Abstract
BACKGROUND:
Home is essential to recovery, and recovery housing can play an important role for individuals seeking a supportive environment. The National Study of Treatment and Addiction Recovery Residences (NSTARR) Project constitutes the largest and most diverse study of recovery housing to date. We describe the development of a national sampling frame to study recovery housing, as well as findings on availability and distribution of recovery housing across the U.S.
METHODS:
Data from publicly available sources and lists maintained by entities tracking recovery housing were compiled. Residences for which locating information was available were geocoded and linked with U.S. Census data and drug and alcohol mortality data. We used hot spot analysis and multilevel models to describe the geographic distribution of recovery residences and assess whether residences are located in areas of high need.
RESULTS:
The NSTARR database contains information on 10,358 residences operated by 3,628 providers in all 50 states. Residences were more likely (p < 0.05) to be in urban areas and in counties with higher substance use mortality; they were less likely to be in economically disadvantaged areas. Recovery housing density also was greater in urban areas and areas with a greater proportion of non-White residents, but lower in economically disadvantaged areas.
CONCLUSIONS:
Despite a wealth of research on some types of recovery housing, critical gaps in the field’s understanding about the nature of recovery housing remain. The NSTARR Project represents an important first step to expand research on recovery housing across the country.
Keywords: recovery, recovery housing, recovery residences, treatment availability, treatment access
1. Introduction
The Substance Abuse and Mental Health Services Administration (SAMHSA) describes recovery as a process through which individuals strive to improve their health and wellness (Substance Abuse and Mental Health Services Administration, 2012). SAMHSA has also delineated four major dimensions that support a lifestyle in recovery, with one dimension being “home”, or having a safe and stable place to live. Recovery housing can play an important role in providing a supportive environment for persons in recovery, yet as recent legislation such as the Excellence in Recovery Housing Act (H.R. 8868, 2019–2020) and its companion bill in the Senate (S. 500 CARA 2.0 Act of 2020, 2019–2020) highlight, critical gaps remain in our understanding of the availability, quality, and effectiveness of recovery housing. The National Study of Treatment and Addiction Recovery Residences (NSTARR) Project represents a critical step in addressing key questions about the availability and nature of recovery housing in the U.S. This paper describes the development of the NSTARR database of recovery residences, initial findings on the availability of recovery housing across the U.S., and how the database will be used to characterize the national recovery housing landscape.
1.1. Recovery housing and its role in supporting those in recovery
Recovery housing is an intervention designed to address the recovering person’s need for a safe and healthy living environment while supplying requisite recovery and peer supports (Substance Abuse and Mental Health Services Administration, 2019). As described by the National Alliance for Recovery Residences (NARR; National Alliance for Recovery Residences, 2015), recovery residences represent a spectrum of living environments and can vary in the type and intensity of services they provide (see Mericle et al., 2014). These residences go by various names including recovery homes, sober homes, sober living environments, Oxford Houses™, and halfway houses. Regardless of what they are called or what types and/or intensities of services provided, a key tenet in recovery housing is reliance on peers living in the same environment to provide support for one another. This is central to the social model of recovery, which highlights the importance of experiential knowledge, peer interaction, and community engagement reflected in a range of settings including Oxford Houses, sober living houses, and therapeutic communities (Borkman, 1998).
1.2. History and evidence base for recovery housing
Recovery housing has been central to the evolution of addiction treatment and recovery in the United States. Residential settings like “inebriate homes” and asylums in the mid-nineteenth century gave rise to the modern addiction recovery movement (White, 2002, 2014). Reviews of the effectiveness of recovery housing generally characterize the supporting evidence as moderate to strong (Kelly, 2018; Reif et al., 2014), noting that recovery housing can enhance clinical and recovery outcomes and reduce costs to society in terms of health care expenditures, criminal justice involvement, and decreased productivity. Despite these strong findings, the impact of this research is undermined by the small number of studies conducted to date on diverse types of recovery housing. Research on Oxford Houses has been conducted in various locations across the U.S. (Ferrari et al., 2004; Jason et al., 2007), but the Oxford House model represents just one type of recovery residence. Research on sober living houses, another model of recovery housing, has primarily focused on residences in California (Polcin et al., 2010; Polcin et al., 2018). Moreover, a major gap in the literature is the lack of consistency in defining essential characteristics and program elements that can be used to identify evidence-based recovery housing practices.
1.3. NSTARR Project Aims
To begin addressing these gaps in the literature, the NSTARR Project created a national database of recovery residences, with the ultimate goal of developing a comprehensive sampling frame to survey a random sample of recovery residences stratified by state to characterize essential features of different types of recovery residence. Residences in the database were geocoded and linked with community information. This paper presents an overview of the development of the NSTARR database and provides the first set of findings on the national geographic distribution of recovery residences. We present national and state-level hot spot analyses to identify places with more (or less) recovery housing than expected based on the underlying population distributions. We also identify urban-rural differences in availability of recovery housing and assess whether residences are located in areas where they might be needed most, using alcohol- and drug-involved mortality rates to indicate a need for recovery housing.
2. Methods
2.1. Developing the NSTARR database
To ensure we could conduct a nationally representative survey of recovery residences, we first needed to develop a national sampling frame. As no such resource existed, we compiled information from a variety of sources and cataloged individual residences and the organizations that operate them. Database fields include the name and location of the residence, contact information, the primary source of information about the residence, and basic information about the population served (e.g., residents’ gender, number of beds, whether residents can bring children). Corresponding location and contact information also were collected for the organizational entity operating each residence.
We began in January 2020 by downloading information available in the Oxford House directory on the Oxford House website (https://www.oxfordhouse.org). We also downloaded information on substance use treatment facilities that operated halfway houses identified in the SAMHSA Treatment Locator (https://findtreatment.samhsa.gov). This information is compiled from responses to the National Survey of Substance Abuse Treatment Services and the National Mental Health Services Survey, which collect facility-level information. Each halfway house was treated as a unique residence in our database. To gather information on the organization operating each facility, we reviewed facility websites to determine whether a given facility was operated by another entity. In the process of reviewing these websites, we also gathered information about other residences operated by the organization. Additional residences were added if they were described as being a distinct location also defined as a halfway house, sober living house/residence, recovery residence, recovery housing, supportive housing, transitional housing, or supportive living environment. We limited inclusion of newly identified residences to those serving individuals with substance use disorders that included some amount of locating or contact information for the residence. We also collected information on residences from state-level Affiliates of NARR, many of which list information on certified residences and providers of recovery housing on their websites. The amount and nature of information maintained or that could be collected varied, so representatives of NARR Affiliates also were contacted to ensure comprehensive information about recovery housing within their state.
Finally, to ensure that our database contained information on residences that may not be chartered by Oxford House, operated as a halfway house, or contained in information collected by NARR Affiliates, we also reviewed a variety of other resources. Some of these resources were suggested by key stakeholders serving as study consultants, and others were online directories of services for individuals seeking help for substance use disorders, or for sober living, more specifically (see Supplemental Table 1). Listings from these directories of unknown or questionable quality were carefully vetted by comparing the information with details already in our database, searching the Treatment Locator to verify whether the facility provided halfway housing, and visiting identified websites for a given facility/residence to verify the listing did indeed represent a recovery residence. When visiting websites for a residence, we followed similar protocols used when reviewing websites identified through the SAMHSA Treatment Locator.
2.2. Geocoding process and measures
House locations were geocoded using ArcGIS (version 10.8.1; Esri, 2020). Of the 10,358 houses in the database, 60.8% were matched at the street level and 25.6% were matched at the ZIP code level, with 13.6% unmatched due to missing address information. Using spatial joins, we assigned county FIPS codes to each geocoded address. We then linked the recovery housing locations with county-level data on urbanicity, alcohol- and drug-involved mortality, and demographic characteristics.
Recovery housing availability was measured by an indicator of any recovery housing (versus none) in a given county, a count of recovery residences in each county, and a count of residences per 100,000 population. As described below, the dichotomous indicator and basic count were used as outcomes in the regression models, and the residence density count was used for the hot spot analyses.
Urbanicity classification was based on the U.S. Department of Agriculture’s (USDA) 2013 Rural-Urban Continuum Codes (RUCC; Ingram & Franco, 2014). These codes distinguish metropolitan counties by population size and nonmetropolitan counties by both degree of urbanization and adjacency to a metro area (United States Department of Agriculture, 2019). We classified areas as urban (RUCC 1–3), adjacent rural (RUCC 4, 6, 8), or non-adjacent rural (RUCC 5,7,9).
Mortality, an indicator of service need, was defined using county-level age-standardized alcohol- and/or drug-involved mortality rates from 2009–2019 (combined). Multiple causes of death data were downloaded from the Centers for Disease Control and Prevention’s WONDER tool (Centers for Disease Control and Prevention, 2020). We included all deaths with any mention of alcohol or drugs in the death record, selecting all underlying causes of death, with alcohol- and/or drug-related as a multiple cause of death. The ICD-10 codes used to indicate alcohol- and drug-related causes of death are in the Supplemental Appendix. Mortality data was sparse through the Great Plains and in some parts of the Southeast, so we coded suppressed and unreliable values at the midpoint of the thresholds for disclosure. Suppressed values were recoded as 5 deaths/100,000 and unreliable values were recoded as 10 deaths/100,000 population.
County demographic characteristics were based on the 2015–2019 American Community Survey (ACS), which is the latest data available for small areas (including some rural counties with low population counts). We included the proportion of county residents with household incomes below 150% of the federal poverty guidelines and the proportion of residents reporting their race/ethnicity as anything other than non-Hispanic White (Asian, Pacific Islander, American Indian/Alaskan Native, Black/African American, Hispanic of any race; hereafter, referred to as non-White residents).
2.3. Analyses
2.3.1. Hot spot analyses
National and state-level hot spot analyses were conducted in ArcGIS to assess clustering of recovery residences across the country. We first used optimized hot spot analysis to identify hot spots and cold spots for recovery housing within counties, nationally. The Optimized Hot Spot Analysis tool uses Getis-Ord Gi* statistics (Getis & Ord, 1992) to detect areas with statistically significant hot spots (counties with higher counts of recovery residences surrounded by counties with similarly high counts) and cold spots (counties with low counts of recovery residences surrounded by other counties with low counts). The tool automatically aggregates incident data (here, locations of recovery residences), identifies the correct scale for analysis, and accounts for multiple testing and spatial dependence. The default aggregation method is to count incident points within fishnet polygons, which are displayed on the maps. A second hot spot analysis utilized the general Hot Spot Analysis tool to identify local areas within each state with a larger (hot spot) or smaller (cold spot) average recovery residence count than the global average for the state. This analysis also used Getis-Ord Gi* statistics to detect areas with high or low clustering values among spatially contiguous counties. The maps present a range of precision, spanning 90% to 99% confidence intervals for the hot and cold spots (see Figures 1 & 2).
Figure 1.
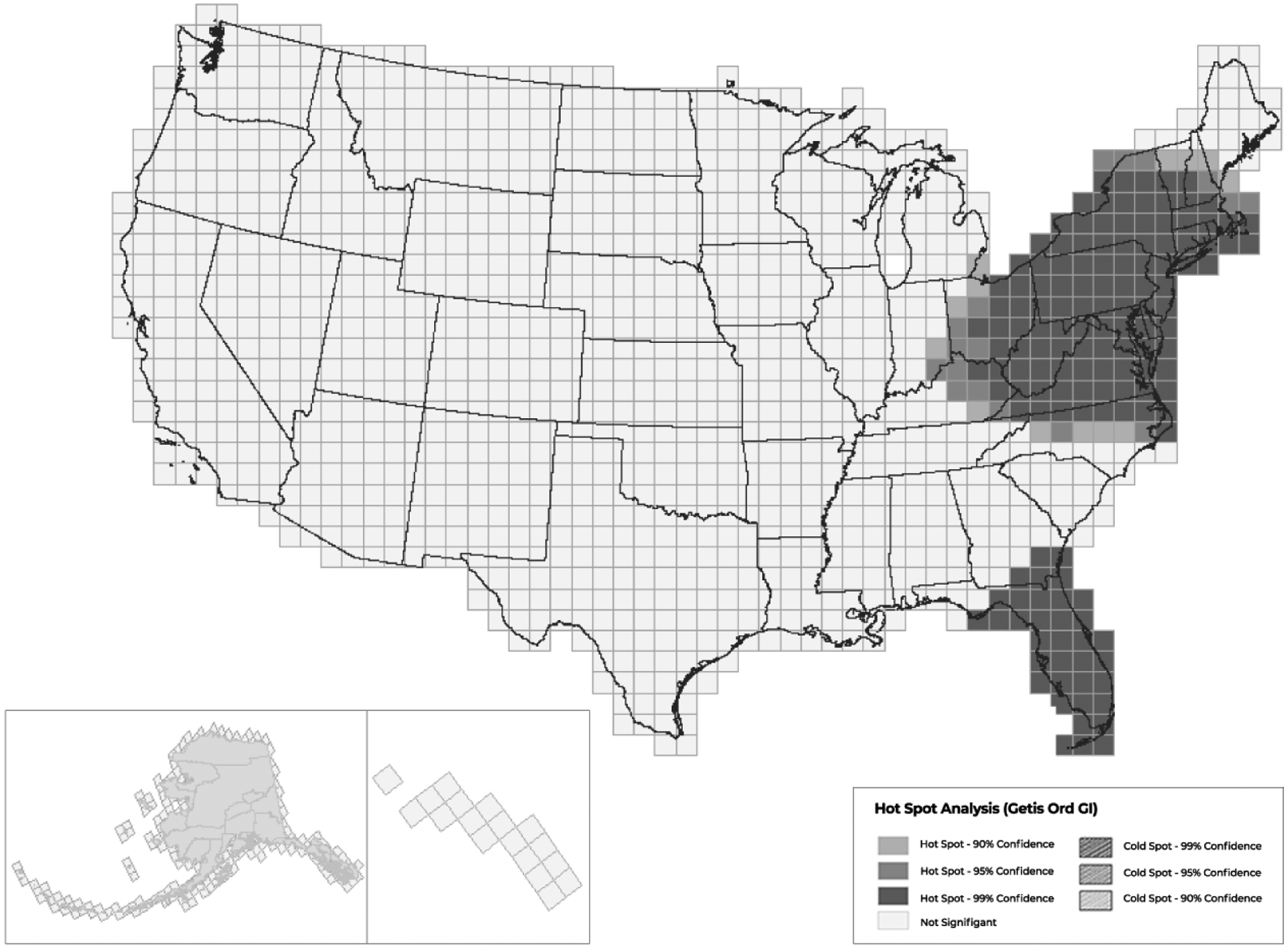
National Optimized Hot Spot Analysis of Recovery Residence Locations, 2019
Figure 2.
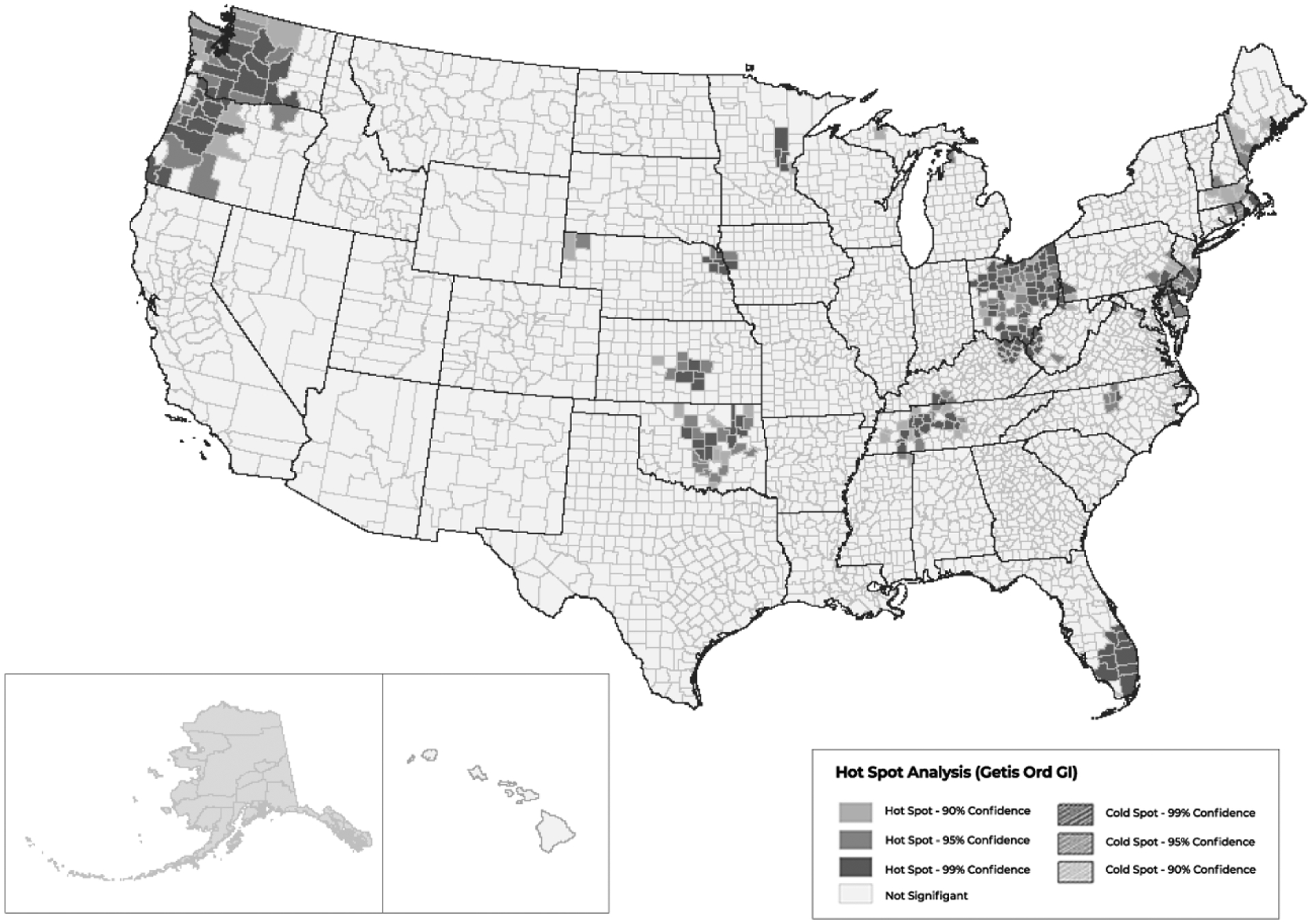
State-level Getis-Ord Hot Spot Analysis of Recovery Residences by County, 2019
2.3.2. Multilevel regression models
Associations with urbanicity, mortality, and county demographics were assessed using unadjusted and adjusted multilevel models with all covariates entered simultaneously. Logistic regression was used for the indicator of any recovery housing (versus none), and a second set of negative binomial regression models were used for the count of recovery residences in each county (limited to counties with at least one recovery residence). All regression models accounted for clustering of counties within states to adjust for unmeasured factors that vary between states (i.e., many key decisions about housing, mental health, and substance use treatment services are made at the state level) and were conducted using Stata (version 16.1; StataCorp., 2019).
3. Results
3.1. Residence information
Between January 2020 and January 2021, 10,358 distinct recovery residences were identified, representing 3,628 different recovery housing providers in each of the 50 U.S. states and Washington, D.C. Most (79%) of the residences were part of an organization that operated multiple residences, with 53% being affiliated with an organization that operated five or more residences. The largest (35%) source of information on recovery residences was the state-level NARR Affiliates, which contributed information on NARR-certified residences as well as non-certified residences (included in “Other” category). The Oxford House website was the next largest (26%) source of information. Information contained in the SAMHSA Treatment Locator also was important, as it contributed to direct identification of another 1,406 residences (14%), as well as residences in the “Other” category that were found by reviewing websites of facilities in the Treatment Locator. The amount of information about each residence available from these sources varied. Residences identified through the Oxford House website and the Treatment Locator resulted in the highest percent of residences with geolocating information. However, across sources, street or zip code was collected on 87% of residences. Details are provided in Supplemental Table 1.
3.2. Geographic distribution of recovery housing
Table 1 provides state-level descriptive information about recovery housing availability and alcohol- and drug-involved mortality as an indicator of service need. Seven of the ten states with the highest mortality rates are in the bottom half of the national ranking on recovery housing availability per capita (New Mexico, Wyoming, Montana, Colorado, South Dakota, North Dakota and Arizona), and these are all sparsely populated Western and Great Plains states. However, Oregon and Oklahoma also have high mortality rates, but are in the top 10% of states in terms of recovery housing availability per capita.
Table 1.
State-level Descriptive Statistics on Recovery Residences
| State | Total Population | Total # of Recovery Residences | % Residences Geocoded | Geocoded Residences in Urban Counties | Houses Per 100,000 Population | Age-Adjusted Alcohol/Drug Mortality Rate per 100,000 Population | Recovery Housing Availability per Capita (Rank) | Mortality Rate (Rank) |
|---|---|---|---|---|---|---|---|---|
| Alabama | 4,876,250 | 30 | 97% | 93.1% | 0.62 | 10.5 | 51 | 51 |
| Alaska | 737,068 | 25 | 84% | 61.9% | 3.39 | 35.9 | 21 | 3 |
| Arizona | 7,050,299 | 185 | 41% | 100.0% | 2.62 | 25.9 | 27 | 9 |
| Arkansas | 2,999,370 | 20 | 90% | 83.3% | 0.67 | 13.8 | 50 | 42 |
| California | 39,283,496 | 757 | 54% | 97.6% | 1.93 | 19.7 | 35 | 22 |
| Colorado | 5,610,349 | 137 | 81% | 96.4% | 2.44 | 29.8 | 29 | 6 |
| Connecticut | 3,575,074 | 118 | 80% | 86.2% | 3.30 | 15.8 | 23 | 38 |
| Delaware | 957,248 | 104 | 100% | 100.0% | 10.86 | 19.8 | 1 | 21 |
| District of Columbia | 692,683 | 47 | 89% | 100.0% | 6.79 | 25.5 | 6 | 11 |
| Florida | 20,901,636 | 2042 | 97% | 99.8% | 9.77 | 16.9 | 2 | 33 |
| Georgia | 10,403,847 | 82 | 49% | 70.0% | 0.79 | 11.9 | 48 | 49 |
| Hawaii | 1,422,094 | 63 | 100% | 88.9% | 4.43 | 11.9 | 14 | 47 |
| Idaho | 1,717,750 | 21 | 86% | 94.4% | 1.22 | 23.3 | 44 | 17 |
| Illinois | 12,770,631 | 156 | 92% | 94.4% | 1.22 | 14 | 44 | 40 |
| Indiana | 6,665,703 | 118 | 97% | 83.3% | 1.77 | 17.1 | 37 | 30 |
| Iowa | 3,139,508 | 32 | 100% | 68.8% | 1.02 | 19.4 | 47 | 24 |
| Kansas | 2,910,652 | 131 | 99% | 77.7% | 4.50 | 17.4 | 13 | 28 |
| Kentucky | 4,449,052 | 202 | 95% | 81.8% | 4.54 | 18.6 | 12 | 25 |
| Louisiana | 4,664,362 | 165 | 96% | 99.4% | 3.54 | 13.3 | 19 | 44 |
| Maine | 1,335,492 | 111 | 68% | 86.7% | 8.31 | 20.6 | 3 | 20 |
| Maryland | 6,018,848 | 337 | 36% | 99.2% | 5.60 | 15.1 | 9 | 39 |
| Massachusetts | 6,850,553 | 290 | 91% | 98.5% | 4.23 | 16.7 | 15 | 35 |
| Michigan | 9,965,265 | 199 | 96% | 86.5% | 2.00 | 16.4 | 34 | 37 |
| Minnesota | 5,563,378 | 190 | 50% | 84.2% | 3.42 | 22.3 | 20 | 18 |
| Mississippi | 2,984,418 | 38 | 97% | 62.2% | 1.27 | 12.3 | 42 | 45 |
| Missouri | 6,104,910 | 167 | 38% | 92.1% | 2.74 | 16.4 | 25 | 36 |
| Montana | 1,050,649 | 8 | 75% | 50.0% | 0.76 | 30.8 | 49 | 4 |
| Nebraska | 1,914,571 | 77 | 92% | 81.7% | 4.02 | 17 | 18 | 31 |
| Nevada | 2,972,382 | 33 | 79% | 96.2% | 1.11 | 23.9 | 46 | 16 |
| New Hampshire | 1,348,124 | 57 | 68% | 64.1% | 4.23 | 19.6 | 15 | 23 |
| New Jersey | 8,878,503 | 203 | 95% | 100.0% | 2.29 | 11.9 | 30 | 48 |
| New Mexico | 2,092,454 | 44 | 73% | 90.6% | 2.10 | 43.3 | 31 | 1 |
| New York | 19,572,320 | 244 | 96% | 87.2% | 1.25 | 13.4 | 43 | 43 |
| North Carolina | 10,264,876 | 345 | 93% | 94.1% | 3.36 | 17.4 | 22 | 29 |
| North Dakota | 756,717 | 12 | 75% | 66.7% | 1.59 | 27.6 | 41 | 8 |
| Ohio | 11,655,397 | 577 | 98% | 78.0% | 4.95 | 18.2 | 11 | 26 |
| Oklahoma | 3,932,870 | 319 | 100% | 81.5% | 8.11 | 25.5 | 5 | 10 |
| Oregon | 4,129,803 | 339 | 99% | 92.6% | 8.21 | 29.8 | 4 | 5 |
| Pennsylvania | 12,791,530 | 347 | 98% | 98.5% | 2.71 | 12.1 | 26 | 46 |
| Rhode Island | 1,057,231 | 56 | 89% | 100.0% | 5.30 | 25.5 | 10 | 12 |
| South Carolina | 5,020,806 | 89 | 99% | 98.9% | 1.77 | 16.9 | 37 | 34 |
| South Dakota | 870,638 | 15 | 93% | 78.6% | 1.72 | 29.7 | 39 | 7 |
| Tennessee | 6,709,356 | 278 | 94% | 93.1% | 4.14 | 18 | 17 | 27 |
| Texas | 28,260,856 | 583 | 92% | 99.3% | 2.06 | 13.8 | 33 | 41 |
| Utah | 3,096,848 | 59 | 95% | 91.1% | 1.91 | 17 | 36 | 32 |
| Vermont | 624,313 | 18 | 78% | 57.1% | 2.88 | 24.1 | 24 | 15 |
| Virginia | 8,454,463 | 216 | 100% | 99.5% | 2.55 | 11.6 | 28 | 50 |
| Washington | 7,404,107 | 452 | 87% | 93.9% | 6.10 | 24.3 | 7 | 13 |
| West Virginia | 1,817,305 | 110 | 85% | 81.7% | 6.05 | 24.2 | 8 | 14 |
| Wisconsin | 5,790,716 | 98 | 99% | 77.3% | 1.69 | 21.2 | 40 | 19 |
| Wyoming | 581,024 | 12 | 100% | 16.7% | 2.07 | 37.1 | 32 | 2 |
Note. Alcohol- and drug-involved mortality included all deaths as underlying causes of death and the selected ICD-10 Codes for contributing cause of death. See Supplemental Appendix for the list of codes.
Approximately 30% of U.S. counties contained at least one recovery residence. The national hot spot analysis (Figure 1) revealed clustering of recovery residences in the northeastern portion of the country, through most of New England and into the Midwest and Mid-Atlantic regions. Another hot spot covered most of Florida. There were no statistically significant cold spots identified. That is, despite lower availability of recovery residences in some Western and Great Plains states (indicated by recovery housing per capita), given the underlying population distributions, there were no areas highlighted as being low-density clusters of counties underserved by recovery housing.
Figure 2 shows within-state hot spots that were not identified in the national analysis. These clusters indicate where spatial distribution of houses did not occur randomly. For example, there were hot spots in Western and coastal areas of Washington and Oregon, in Oklahoma, Kansas and Tennessee, as well as in small sections of Nebraska, Iowa, and Minnesota, that were not highlighted in the national analysis. Further, the large northeastern hot spot from the national analysis was revealed to be most evident in Ohio, New Jersey, Delaware, Massachusetts and Rhode Island, and the Florida hot spot was localized to the southern part of the state.
3.3. Correlates of recovery housing availability
Figure 3 depicts the spatial distribution of recovery housing relative to urbanicity. Most recovery residences were located in urban areas, with 38 states having over 80% of their recovery housing located in urban counties. Figure 4 depicts recovery housing relative to alcohol- and drug-involved mortality. There were counties in the Southwest (Arizona, New Mexico, southern Colorado), Northwest (Montana), and Appalachia (West Virginia) where the alcohol- and/or drug-involved mortality rates were relatively high (greater than 108 deaths/100,000 population) but there were no recovery residences.
Figure 3.

National Distribution of Recovery Residences by Urbanicity, 2019
Figure 4.
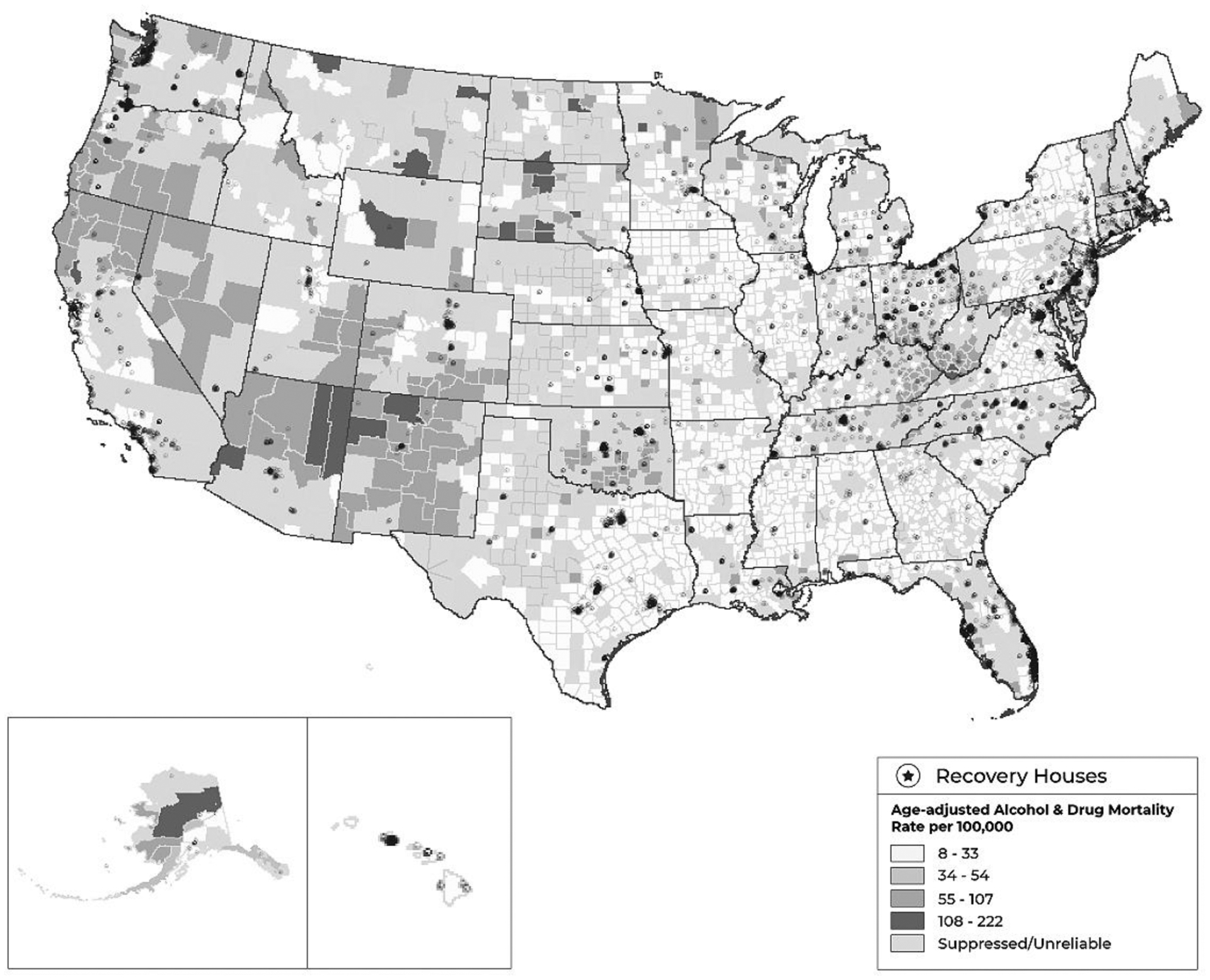
National Distribution of Recovery Residences in 2019, by Age-adjusted Alcohol- and/or Drug-involved Mortality Rate (2009–2019)
Note. Alcohol- and drug-involved mortality included all deaths as underlying causes of death and the selected ICD-10 Codes for contributing cause of death. See Supplemental Appendix for the list of codes.
The unadjusted multilevel logistic regression models (Table 2) showed reduced odds of having at least one recovery residence in counties that were rural (for those adjacent to urban areas, as well as for those not adjacent to urban areas) and those with higher proportions of low-income residents, and increased odds of having at least one recovery residence in counties with higher alcohol-/drug-involved mortality rates. These associations held in the fully adjusted model as well. The proportion of non-White residents was not associated with having at least one recovery residence in the county.
Table 2.
Models Examining Associations between Urbanicity/Rurality, Mortality, and Population Demographics with Recovery Housing Availability and Density
| Availability of Any Recovery Residences (N=3142 counties) | Recovery Housing Density (N=929 counties with at least one recovery residence) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted Models | Adjusted Model | Unadjusted Models | Adjusted Model | |||||||||
| OR | SE | p | aOR | SE | p | Coeff | SE | p | Coeff | SE | p | |
| Urbanicity (urban as reference) | ||||||||||||
| Adjacent rural | 0.163 | 0.026 | <0.001 | 0.184 | 0.032 | <0.001 | −10.19 | 1.953 | <0.001 | −8.695 | 1.699 | <0.001 |
| Non-adjacent rural | 0.109 | 0.021 | <0.001 | 0.127 | 0.027 | <0.001 | −9.799 | 1.697 | <0.001 | −8.889 | 1.589 | <0.001 |
| Mortality | 1.014 | 0.003 | <0.001 | 1.020 | 0.003 | <0.001 | −0.002 | 0.034 | 0.955 | 0.045 | 0.028 | 0.113 |
| Proportion below 150% poverty | 0.943 | 0.008 | <0.001 | 0.970 | 0.008 | <0.001 | −0.224 | 0.089 | 0.012 | −0.176 | 0.088 | 0.046 |
| Proportion non-White residents | 1.000 | 0.001 | 0.543 | 1.000 | 0.001 | 0.681 | 0.063 | 0.021 | 0.002 | 0.059 | 0.019 | 0.002 |
Notes. Multilevel models were employed to take into account the nested structure of the data. The models include two levels, with county-level recovery house availability nested within states. Unadjusted models assess relationships between county-level characteristics with recovery housing in separate models. The adjusted model includes all county-level characteristics in the same model.
The unadjusted multilevel negative binomial regression models (also Table 2) showed the count of recovery residences in those counties with at least one such facility was negatively associated with rural status and proportion of low-income residents, and recovery housing density also was positively associated with the proportion of non-White residents. These associations held in the fully adjusted model. Alcohol-/drug-involved mortality was not associated with recovery housing density. Sensitivity analyses showed similar findings in the adjusted models for both indicators of recovery housing availability when setting suppressed and unreliable mortality data to 0 or, separately, to missing (data available upon request).
4. Discussion
4.1. Need for routine collection of information on recovery housing
We identified 10,358 recovery residences of various types across the country, employing methods that fostered exhaustiveness and careful vetting to ensure the most accurate accounting of recovery housing availability to date. However, the amount of information that we were able to collect from extant sources was highly variable and the recovery residence landscape is constantly changing (Mericle et al., 2015). The National Survey of Substance Abuse Treatment Services (NSSATS), which serves as the source for information contained in the SAMHSA Treatment Locator, provides an annual census of facilities offering substance use treatment and has been used as the sampling frame in a variety of studies examining aspects of the substance use treatment system (Arria et al., 2013; Cochran et al., 2007; Mericle et al., 2018; Roman and Johnson, 2002; Timko et al., 2012). Although halfway houses have been queried in the NSSATS since its inception, and more recent versions of the survey have included the term “sober home” in this question, more purposefully identifying and including questions on recovery residences could ensure the Treatment Locator could be used to access and study recovery housing much in the same way that this resource is used by the public and by researchers with respect to substance use treatment. Including data on recovery housing as part of these ongoing survey efforts also would highlight recovery housing’s role in a robust and comprehensive substance use service delivery system.
4.2. Gaps in availability
Certain states showed areas of higher concentrations of recovery housing relative to surrounding areas. These hot spots may reflect communities friendlier to recovery housing, either through policy or because there are providers who have served to “seed” regions and help foster proliferation of recovery housing. As has been found with respect to substance use treatment (Cummings et al., 2014), urbanicity was associated with increased odds of having any recovery housing, as well as a greater density of recovery residences in counties that had at least one identified recovery residence. Urbanicity may be driving this phenomenon, but there may also be a relationship between substance use treatment programs and recovery housing, as some geographic regions, referred to as “recovery destinations,” have many recovery residences precisely because there are many treatment programs.
While homelessness and substance use are most concentrated in urban areas (Henry et al., 2021), unhoused and marginally housed individuals in rural communities face unique challenges (Shamblin et al., 2012), and the ongoing high rates of opioid use have highlighted unmet need within these communities (Albright et al., 2020; Moody et al., 2017). High alcohol- and drug-involved mortality rates in rural areas also highlight a need for recovery support services outside urban areas.
Multilevel analyses also showed consistent associations between a greater proportion of low-income residents and reduced availability of recovery housing. While this finding may reflect that some types of recovery residences, such as Oxford Houses, seek stable neighborhoods that may contribute to recovery capital (Ferrari et al., 2006), this also may indicate a need for low-cost recovery housing to support economically-disadvantaged people as they establish and maintain recovery from alcohol and drug problems. Residing in low-income neighborhoods and places with many triggers for substance use, such as bars or liquor stores, during the early phases of recovery may contribute to relapse (Karriker-Jaffe et al., 2020; Kerr and Subbaraman, in press). Community-level disadvantage also is associated with reduced initiation of formal substance use treatment (Acevedo et al., 2018), but it is possible that improved availability of recovery housing in low-income communities could help fill a need for services to support people across the recovery spectrum.
Contrary to national studies of Medicaid substance use treatment facilities (Cummings et al., 2014), as well as one prior localized study of recovery housing availability (Mericle et al., 2016), our national data on recovery housing do not suggest gaps in availability in communities with a high proportion of non-White residents. In fact, our data show that a greater proportion of non-White residents was associated with a higher density of recovery residences in counties with at least one such facility. This suggests that recovery residences are available in diverse communities across the country. Further research should establish whether there is differential utilization (or under-utilization) of recovery housing by demographic subgroups.
4.3. Addressing acute needs and seeding prevention
Higher alcohol-/drug-related mortality rates were associated with increased odds that a county would have at least one recovery residence. This finding is promising, as it suggests recovery housing is located in communities with greater need. However, when focusing on counties that had at least one recovery residence, mortality rates were not associated with the density of recovery housing. Future research could help inform service planning to ensure that urban areas with higher population densities and greater alcohol- and drug-associated mortality are appropriately resourced.
Recovery housing and other peer-based recovery support services can augment existing treatment services to address these challenges (Ashford et al., 2019) and build recovery-oriented systems of care (ROSC; Sheedy and Whitter, 2009) within communities. However, as highlighted in the recovery ready ecosystems model and the recovery ready communities framework (Ashford et al., 2020), careful assessment of resources, which would include recovery housing, across systems of care and at different ecological levels is needed to support individuals in recovery, as well as to seed prevention efforts. Future NSTARR work will examine data on local alcohol and drug treatment availability, on- and off-premise retail alcohol outlets, and crime in relation to recovery housing.
4.4. Limitations and next steps
While we were able to collect information on over ten thousand residences in all states and Washington, D.C. from a wide variety of sources, there may be residences missing from our database because they are unknown to these sources. Selection bias may affect results, as there are may be recovery residences of varying quality that do not wish to participate in the SAMHSA Treatment Locator or to become a member of a NARR affiliate. Furthermore, some states incentivize or mandate licensing or certification of recovery homes, which likely influences variation in both recovery housing quantity and quality across states. Some owners and operators also may be more skeptical of governmental or agency oversight and choose not to participate in certification and licensing. Thus, the prevalence of recovery housing may be under-estimated. Additionally, if the prevalence of recovery housing has been differentially under-estimated in places with high alcohol- and/or drug-involved mortality rates, the relationship between recovery housing availability and mortality may be under-estimated as well. Further, these analyses represent one point in time, and some residences may have closed by the time we found them, due to lags in updating of online resources. However, we anticipate additions to these sources would be similarly lagged. We can examine this more closely as we document changes to our database over the course of the study.
Approximately 13% of identified residences were not included in our analyses because we were missing information to identify the county where they were located. Residences sourced from the Oxford House website and the Treatment Locator had the most complete data, so findings on the distribution and availability of recovery housing may best apply to these residences. More than half (57%) of the residences with missing locating information were members of NARR Affiliates, some of which did not collect this level of detail on their membership or could not share it with other entities. That members of NARR Affiliates are under-represented is unfortunate because, unlike residences that are unknown to traditional recovery information sources because they are trying to stay “under the radar,” members of NARR Affiliates are inspected and certified as adhering to national quality standards. Finally, while this work speaks to the availability of recovery housing, it cannot speak to the nature or quality of recovery housing across the country.
Many of these limitations will be addressed as the NSTARR Project progresses. The nationally representative survey will draw a state-stratified random sample of residences to describe the nature of recovery housing and to examine factors associated with evidence-based practices. As we contact residences and present findings, we will continue collecting information about residences not presently in the database and refining information on previously identified residences. Finally, we will archive de-identified survey data and study documentation, including procedures used to develop the database, so this work can be replicated and used to inform regular surveillance of recovery housing.
Summary and conclusions
Recovery housing can be a critical resource for those with substance use disorders who lack safe or otherwise supportive environments. Although recovery housing exists in all 50 states and Washington, D.C., we found it is largely concentrated in urban areas, potentially leaving rural areas under-resourced. Prior research points to the effectiveness of some types of recovery housing, yet is limited to certain types or models of recovery housing and to certain geographic regions. The NSTARR Project has the potential to better characterize recovery housing, increase the generalizability of prior research, and facilitate future research on recovery housing effectiveness, comparative effectiveness, and cost-effectiveness.
Supplementary Material
Highlights.
The NSTARR Project characterizes availability of recovery housing in the U.S.
Rural and disadvantaged communities are underserved by recovery housing.
Substance-related mortality is associated with increased odds of recovery housing.
Acknowledgements
In addition to the funders, the authors would like to acknowledge the recovery residence operators who make information about their recovery residences publicly available, Laya Cooperman who helped to collect this information, and Lee Ann Kaskutas who has provided guidance on this project from its outset.
Role of Funding Source
Work on this manuscript was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to the Public Health Institute (R01AA027782; Mericle, PI). The funding agency had no role in the writing of the report or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflicts declared.
Contributor Information
Amy A. Mericle, Alcohol Research Group at the Public Health Institute.
Deidre Patterson, Alcohol Research Group at the Public Health Institute.
Jason Howell, RecoveryPeople.
Meenakshi Sabina Subbaraman, Alcohol Research Group at the Public Health Institute.
Adrienne Faxio, Alcohol Research Group at the Public Health Institute.
Katherine J. Karriker-Jaffe, RTI International.
References
- Acevedo A, Panas L, Garnick DW, Acevedo-Garcia D, Miles J, Ritter G, Campbell K, 2018. Disparities in the treatment of substance use disorders: does where you live matter? J. Behav. Health Serv. Res 45, 533–549. 10.1007/s11414-018-9586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albright DL, McDaniel JT, Diehr AJ, Paxton J, Bresett J, Moss A, 2020. Small area estimation of opioid abuse and comorbid psychological distress among females living in the thirteen Appalachian region states. Traumatology 26, 61–67. 10.1037/trm0000202. [DOI] [Google Scholar]
- Arria AM, Mericle AA, Rallo D, Moe J, White WL, Winters KC, O’Connor G, 2013. Integration of parenting skills education and interventions in addiction treatment. J. Addict. Med 7, 1–7. 10.1097/ADM.0b013e318270f7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashford RD, Brown AM, Ryding R, Curtis B, 2020. Building recovery ready communities: the recovery ready ecosystem model and community framework. Addict. Res. Theory 28, 1–11. 10.1080/16066359.2019.1571191. [DOI] [Google Scholar]
- Ashford RD, Meeks M, Curtis B, Brown AM, 2019. Utilization of peer-based substance use disorder and recovery interventions in rural emergency departments: patient characteristics and exploratory analysis. Journal of Rural Mental Health 43, 17–29. 10.1037/rmh0000106. [DOI] [Google Scholar]
- Borkman T, 1998. Resident self-governance in social model recovery programs. Contemp. Drug Probl 25, 741–771. 10.1177/009145099802500405. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention, About Multiple Cause of Death, 1999–2019. URL (https://wonder.cdc.gov/mcd-icd10.html) (accessed on 8. 9.21).
- Centers for Disease Control and Prevention, Wide-Ranging Online Data for Epidemiologic Research (WONDER). URL (https://wonder.cdc.gov) (accessed on 6. 23.20).
- Cochran BN, Peavy KM, Robohm JS, 2007. Do specialized services exist for LGBT individuals seeking treatment for substance misuse? A study of available treatment programs. Subst. Use Misuse 42, 161–176. 10.1080/10826080601094207. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Wen H, Ko M, Druss BG, 2014. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry 71, 190–196. 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esri, 2020. ArcGIS Desktop: Release 10.8.1.
- Ferrari JR, Jason LA, Blake R, Davis MI, Olson BD, 2006. ‘This is my neighborhood’: comparing United States and Australian Oxford House neighborhoods. J. Prev. Interv. Community 31, 41–49. 10.1300/J005v31n01_04. [DOI] [PubMed] [Google Scholar]
- Ferrari JR, Jason LA, Davis MI, Olson BD, Alvarez J, 2004. Similarities and differences in governance among residents in drug and/or alcohol misuse recovery: self vs. staff rules and regulations. Ther. Communities 25, 185–198. [Google Scholar]
- Getis A, Ord JK, 1992. The analysis of spatial association by use of distance statistics. Geogr. Anal 24, 189–206. 10.1111/j.1538-4632.1992.tb00261.x. [DOI] [Google Scholar]
- H.R.8868 – 116th Congress (2019–2020): Excellent in Recovery Housing Act. (2020, December 3), https://www.congress.gov/bill/116th-congress/house-bill/8868?s=1&r=2.
- Henry M, de Sousa T, Roddey C, Gayen S, Bednar TJ, Abt Associates, 2021. The 2020 Annual Homeless Assessment Report (AHAR) to Congress. The U.S. Department of Housing and Urban Development. Office of Community Planning and Development. URL (https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf) (accessed on 7.23. 21). [Google Scholar]
- Ingram DD, Franco SJ, 2014. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2, 166. URL (https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf) (accessed on 8.21.21) [PubMed] [Google Scholar]
- Jason LA, Davis MI, Ferrari JR, 2007. The need for substance abuse after-care: longitudinal analysis of Oxford House. Addict. Behav 32, 803–818. 10.1016/j.addbeh.2006.06.014. [DOI] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ, Witbrodt J, Mericle AA, Polcin DL, Kaskutas LA, 2020. Testing a socioecological model of relapse and recovery from alcohol problems. Subst. Abuse 14, 1178221820933631. 10.1177/1178221820933631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J, 2018. SAMHSA Recovery Research and Evaluation Technical Expert Panel Summary Report. URL (http://www.williamwhitepapers.com/pr/dlm_uploads/SAMHSA-Recovery-Research-Report-2018.pdf) (accessed on 6.15.21).
- Kerr WC, Subbaraman MS, in press. Alcohol control policy and regulations to promote recovery from alcohol use disorder [Chapter 19]. In: Tucker JA, Witkiewitz K (Eds.), Dynamic Pathways to Recovery from Alcohol Use Disorder: Meaning and Methods. Cambridge University Press, New York. pp. 346–363. [Google Scholar]
- Mericle AA, de Guzman R, Hemberg J, Yette E, Drabble L, Trocki K, 2018. Delivering LGBT-sensitive substance use treatment to sexual minority women. J. Gay Lesbian Soc. Serv 30, 393–408. 10.1080/10538720.2018.1512435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle AA, Karriker-Jaffe KJ, Gupta S, Sheridan DM, Polcin DL, 2016. Distribution and neighborhood correlates of sober living house locations in Los Angeles. Am. J. Community Psychol 58, 89–99. 10.1002/ajcp.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle AA, Miles J, Cacciola J, 2015. A critical component of the substance abuse continuum of care: recovery homes in Philadelphia. J. Psychoactive Drugs 47, 80–90. 10.1080/02791072.2014.976726. [DOI] [PubMed] [Google Scholar]
- Mericle AA, Miles J, Cacciola J, Howell J, 2014. Adherence to the social model approach in Philadelphia recovery homes. Int. J. Self Help Self Care 8, 259–275. 10.2190/SH.8.2.g. [DOI] [Google Scholar]
- Moody L, Satterwhite E, Bickel WK, 2017. Substance use in rural Central Appalachia: Current status and treatment considerations. Rural Mental Health 41, 123–135. 10.1037/rmh0000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Recovery Residences, 2015. Recovery Residence Quality Standards. URL (https://narronline.org/wp-content/uploads/2015/10/National-Recovery-Residence-Quality-Standards-Oct-7-2015.pdf) (accessed on 6.15 2021).
- Polcin DL, Korcha R, Bond J, Galloway G, 2010. What did we learn from our study on sober living houses and where do we go from here? J. Psychoactive Drugs 42, 425–433. 10.1080/02791072.2010.10400705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL, Korcha R, Witbrodt J, Mericle AA, Mahoney E, 2018. Motivational Interviewing Case Management (MICM) for persons on probation or parole entering sober living houses. Crim. Justice Behav 45, 1634–1659. 10.1177/0093854818784099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif S, George P, Braude L, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME, 2014. Recovery housing: assessing the evidence. Psychiatr. Serv 65, 295–300. 10.1176/appi.ps.201300243. [DOI] [PubMed] [Google Scholar]
- Roman PM, Johnson JA, 2002. Adoption and implementation of new technologies in substance abuse treatment. J. Subst. Abuse Treat 22, 211–218. 10.1176/appi.ps.201300243. [DOI] [PubMed] [Google Scholar]
- Shamblin SR, Williams NF, Bellaw JR, 2012. Conceptualizing homelessness in rural Appalachia: understanding contextual factors relevant to community mental health practice. Journal of Rural Mental Health 36, 3–9. 10.1037/h0095809. [DOI] [Google Scholar]
- Sheedy CK, Whitter M, 2009. Guiding Principles and Elements of Recovery-Oriented Systems of Care: What do we know from the research? [HHS Publication No. (SMA) 09–4439]. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration. URL (https://www.naadac.org/assets/2416/sheedyckwhitterm2009_guiding_principles_and_elements.pdf) (accessed on 5.1.21) [Google Scholar]
- S.5000 – 116th Congress (2019–2020): CARA 2.0 Act of 2020. (2020, December 10). https://www.congress.gov/bill/116th-congress/senate-bill/5000/text
- StataCorp., 2019. Stata Statistical Software: Release 16. StataCorp LLC, College Station, TX. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2012. SAMHSA’s Working Definition of Recovery. URL (https://store.samhsa.gov/sites/default/files/d7/priv/pep12-recdef.pdf) (accessed on 7.31.21)
- Substance Abuse and Mental Health Services Administration, 2019. Recovery Housing: Best Practices and Suggested Guidelines. URL (https://www.samhsa.gov/sites/default/files/housing-best-practices-100819.pdf) (accessed on 6.30.21) [Google Scholar]
- Timko C, Valenstein H, Lin PY, Moos RH, Stuart GL, Cronkite RC, 2012. Addressing substance abuse and violence in substance use disorder treatment and batterer intervention programs. Subst. Abuse Treat. Prev. Policy 7, 37. 10.1186/1747-597X-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Agriculture, Rural-Urban Commuting Area Codes. URL (https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx) (accessed on 4. 16.21)
- White WL, 2002. Addiction treatment in the United States: Early pioneers and institutions. Addiction 97, 1087–1092. 10.1046/j.1360-0443.2002.00180.x-i1. [DOI] [PubMed] [Google Scholar]
- White WL, 2014. Slaying the Dragon: The History of Addiction Treatment and Recovery in America. Chestnut Health Systems/Lighthouse Institute. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


