Abstract
The objective measurement of fatigue is of critical relevance in areas such as occupational health and safety as fatigue impairs cognitive and motor performance, thus reducing productivity and increasing the risk of injury. Wearable systems represent highly promising solutions for fatigue monitoring as they enable continuous, long-term monitoring of biomedical signals in unattended settings, with the required comfort and non-intrusiveness. This is a p rerequisite for the development of accurate models for fatigue monitoring in real-time. However, monitoring fatigue through wearable devices imposes unique challenges. To provide an overview of the current state-of-the-art in monitoring variables associated with fatigue via wearables and to detect potential gaps and pitfalls in current knowledge, a systematic review was performed. The Scopus and PubMed databases were searched for articles published in English since 2015, having the terms “fatigue,” “drowsiness,” “vigilance,” or “alertness” in the title, and proposing wearable device-based systems for non-invasive fatigue quantification. Of the 612 retrieved articles, 60 satisfied the inclusion criteria. Included studies were mainly of short duration and conducted in laboratory settings. In general, researchers developed fatigue models based on motion (MOT), electroencephalogram (EEG), photoplethysmogram (PPG), electrocardiogram (ECG), galvanic skin response (GSR), electromyogram (EMG), skin temperature (Tsk), eye movement (EYE), and respiratory (RES) data acquired by wearable devices available in the market. Supervised machine learning models, and more specifically, binary classification models, are predominant among the proposed fatigue quantification approaches. These models were considered to perform very well in detecting fatigue, however, little effort was made to ensure the use of high-quality data during model development. Together, the findings of this review reveal that methodological limitations have hindered the generalizability and real-world applicability of most of the proposed fatigue models. Considerably more work is needed to fully explore the potential of wearables for fatigue quantification as well as to better understand the relationship between fatigue and changes in physiological variables.
Keywords: fatigue monitoring, wearable, occupational health and safety, signal quality assessment, validation, physiological signal, machine learning, imbalanced datasets
Introduction
Fatigue, often defined as a decrement in mental and/or physical performance caused by cognitive overload, physical exertion, sleep deprivation, circadian phase/circadian rhythm disruption, or illness (International Civil Aviation Organization, 2012; Tanaka et al., 2015; Mohanavelu et al., 2017), has been a topic of research since the 1860ies. Various definitions of fatigue have been proposed in different scientific disciplines, however, none of them is applicable to all of these disciplines (Yung, 2016). Mainly the multidimensionality, interaction of different variables and in many cases, the subjective nature of perception of fatigue have not allowed to provide a unified definition.
Fatigue can develop in response to physiological challenges or pathophysiological changes. Fatigue has been classified according to its genesis as central (i.e., caused by impaired function of the central nervous system) or peripheral (i.e., caused by impaired function of the peripheral nervous or neuro-muscular system); but also according to the type of load as physical (i.e., of physical etiology, resulting from physical effort and leading to a decrease in physical performance) or mental (i.e., of psychological etiology, resulting from sustained cognitive activity and leading to a reduction in cognitive and behavioral performance) (Aaronson et al., 1999; Cavuoto and Megahed, 2016; Aryal et al., 2017). The latter classification is most commonly used, although other categorization methods have been proposed (Aaronson et al., 1999; Desmond and Hancock, 2001).
Fatigue quantification is of crucial relevance in areas such as occupational health and safety. Apart from being a physiological response of the human body possibly preventing it's overload, fatigue is a symptom associated with several diseases and health conditions (Casillas et al., 2006; Harris et al., 2009; Rudroff et al., 2016; Nassif and Pereira, 2018; O'Higgins et al., 2018; Cortes Rivera et al., 2019). Fatigue impairs cognitive and/or motor performance, reducing work efficiency, productivity, and product quality, as well as increasing risks for injury and fatality (Folkard, 2003; Cavuoto and Megahed, 2016; Yung, 2016). This fact renders fatigue a subject of utmost importance for work safety in occupational settings as, for instance, transportation, mining, aviation, or construction. As reported by police records, globally, 1–4% of the registered road crashes occur due to sleepiness and fatigue (Li et al., 2018). These estimates are nonetheless deemed to underrate the impact of fatigue on road safety, partially due to the inability to assess drivers' fatigue at the crash scene. Questionnaires, naturalistic observation studies, and in-depth investigation indicate that the actual value is around 10–20% of road crashes (European Commission, 2018). That share rises to 20–50%, when considering only commercial vehicle accidents (Davidović et al., 2018). Long working hours, and consequent fatigue and stress, were found to increase the hazard rate among US workers (Dembe, 2005). Furthermore, fatigue is involved in 4–8% of aviation mishaps (Caldwell, 2005).
These facts show the important role of continuous monitoring of the level of fatigue in an accurate and unobtrusive manner for early detection and management of fatigue. Among existing technologies, wearable sensors may meet these requirements. Wearables enable continuous, long-term monitoring, paving the way for the development of accurate models for fatigue monitoring in real-time. Therefore, their application for fatigue monitoring is highly promising.
Although several approaches have already been proposed for fatigue detection and monitoring, no gold standard measure of fatigue exists. Existing non-invasive methods are mainly based on five measuring principles: subjective measures, performance-related methods, biomathematical models, behavioral-based methods, and physiological signal-based methods of which not all are useful for online-monitoring during work or leisure.
Subjective Measures
Subjective measures consist of assessing self-reported fatigue through questionnaires and scales (Shahid et al., 2010; Gawron, 2016). These are not useful in the context of online monitoring, however, they provide insights into mental and emotional processes underlying performance in a task. Subjective measures are therefore helpful as gold-standards to compare with results of fatigue models.
Performance-Related Methods
Performance-related methods rely on the fact that subjects' cognitive and consequently motor performance on specific tasks reflects their level of fatigue. These methods consist of conducting tests to assess subjects' task performance, with emphasis on cognitive skills (e.g., vigilance, hand-eye coordination, sustained attention, reaction time) using neuro-behavioral tasks (Dawson et al., 2014; Honn et al., 2015). Despite being easy to standardize, also performance-related methods cannot be used to detect development of fatigue in real-time to allow preventive measures before an incident happens (Balkin et al., 2011; Huang et al., 2018; Zhang Y. et al., 2018).
Biomathematical Models
Biomathematical models predict subjects' level of fatigue based on information regarding sleep-wake times, work-rest pattern as well as circadian cycle. They are typically used for fatigue risk assessment in civil and military aviation. These models have been developed based on data collected during partial and total sleep deprivation studies. To avoid reliance on self-reports and to increase the reliability of estimates of sleep/wake times, wrist-mounted actigraphy has been employed (Hursh et al., 2004).
Although biomathematical models predict fatigue with moderate success (Chandler et al., 2013), they have several limitations (Dawson et al., 2011) being based on cohort data, i.e., they are not able to predict fatigue at the individual level since individual needs for sleep, circadian rhythms, and responses to fatigue are different. Also, the type of task performed is not considered. To overcome this limitation, the inclusion of information regarding an individual, such as biological and psychological factors, and the performed task/context has been proposed (Chandler et al., 2013). Also, more recent models predict several additional performance- and sleep-related metrics but reliability of such predictions has not yet been proved (Bendak and Rashid, 2020).
Behavioral-Based Methods
Behavioral-based methods follow an observational approach to detect fatigue and include external signs, such as yawning, sighing, eyes closure, or head nodding. As a result, technologies in this category frequently use metrics related to eye movements (EYE), head motion, and facial expression as input features (Dababneh et al., 2016; Sampei et al., 2016; Hu and Lodewijks, 2020). For this, computer vision technologies, especially cameras and eye trackers, have been widely employed for fatigue monitoring through this measuring principle. These solutions have been used in the transport and mining industries.
Although behavioral-based methods are not intrusive, allowing real-time fatigue monitoring almost without requiring faction from subjects, they detect fatigue only upon the appearance of its first signs, which may be too late to avoid exposure to fatigue-related risk (Balkin et al., 2011). Furthermore, computer vision technologies are sensitive to environmental factors (e.g., light).
Physiological Signal-Based Methods
Physiological signal-based methods detect the onset of fatigue based on changes in subjects' physiological responses such as brain activity measured by electroencephalogram (EEG), heart rate (HR), or electromyogram (EMG). Electroencephalogram, for example, has been considered the gold standard for vigilance (Zhang et al., 2017; Zhou et al., 2018) and driver drowsiness detection (Hu et al., 2013; Sikander and Anwar, 2019; Hu and Lodewijks, 2020).
Taking physiological signals as indicators of fatigue enables objective, real-time fatigue monitoring at the individual level. However, changes in physiological variables in response to stressors and fatigue vary within and between individuals, which complicates the detection of abnormal conditions. Despite subjects having little control over their physiological signals, these are susceptible to several other factors, such as environmental conditions, emotions, and pathophysiological issues. For these reasons, the sensitivity and reliability of fatigue detection/prediction based on physiological signals, especially in real life settings, is still unclear (Balkin et al., 2011).
This work presents a review on the state-of-the-art in fatigue monitoring through wearable devices and associated measures of fatigue in addition to existing reviews on fatigue research that focus on specific application domains (e.g., Sikander and Anwar, 2019; Bendak and Rashid, 2020; Hu and Lodewijks, 2020) disregarding the type of technology used for fatigue quantification. Therefore, it is our purpose to provide an overview of fatigue monitoring approaches regardless of their application domain and the casual mechanisms behind fatigue, giving particular emphasis to the use of wearable technology. Strengths and weaknesses of current approaches to measure fatigue based on data acquired by wearable devices as well as limitations and existing opportunities in this field of research will be discussed.
Methods
A literature search was performed in Scopus and PubMed databases covering the period from 1 January 2015 to 7 October 2020. Only articles in English, having the terms “fatigue,” “drowsiness,” “vigilance,” or “alertness” in their titles and the term “wearable” in any field were considered.
Inclusion criteria for this review were (a) studies proposing non-invasive, inter-subject approaches for fatigue quantification, (b) describing the methodology to develop the fatigue index or model, and (c) assessing model/index performance. Given the scope of this review, included studies should not merely propose wearable systems for fatigue monitoring, but also provide evidence to support their use for such application. Accordingly, studies investigating methods for fatigue quantification that did not use wearable systems to acquire data and those that explore the suitability of a given parameter or variable as a fatigue indicator without proposing a fatigue model/index or assessing its performance were dismissed.
A wearable device was defined as a small electronic device consisting of one or more sensors and a data logger intended to be worn on or attached to a single body location when the connection between sensors and logger is not wireless. The focus was on inter-subject, i.e., subject-independent, approaches due to their superior generalization ability compared to intra-individual approaches (i.e., based on data obtained from individual study participants).
No review protocol has been established. One reviewer inspected titles and abstracts of retrieved articles to identify potentially relevant publications. The full-text of the identified articles were then assessed for eligibility by two reviewers. Disagreements between reviewers were resolved by consensus. The following data were extracted from the selected articles: type of fatigue investigated and field of application; fatigue-inducing task; proposed approach to quantify fatigue and its performance metrics; reference measures of fatigue; wearable device used for data acquisition, variables monitored, and sensors' position; study design (i.e., in laboratory and/or real-world settings); and number of participants.
To assess the risk of bias of included studies, we have developed a component approach as recommended by the PRISMA statement (Liberati et al., 2009). This approach was founded on methodological aspects influencing models' or indices' performance. The contemplated aspects were identified based on existing empirical evidence and careful reasoning. Study characteristics used to support reviewers' judgment were selected by discussion and consensus among all review authors. A detailed description of the developed risk of the basis assessment tool as well as the rationale behind this is provided in Supplementary Table 1. In summary, we have considered a total of seven different components to assess the risk of bias of included articles:
Presence of a task to induce fatigue, named fatigue inducement.
Presence of validated fatigue reference measures, named validity of reference.
Application of strategies to handle imbalanced data distribution, if existing, named balanced dataset.
Application of strategies for cross-validation.
Validity of the wearable devices used to acquire the data, named validity of outcomes data. In the scope of this review, a device was considered valid if at least one validation study has been published in a peer-review journal, not exclusively authored by the device's developer or vendor (Byrom et al., 2018). A list of identified validation studies is provided in Supplementary Table 2.
Application of strategies to identify as well as to remove noise and artifacts from the acquired data, named signal quality assessment.
Number of participants included in the study. We have set the minimum acceptable number of participants in a study to 8 subjects.
The risk of bias judgments were made by one reviewer and checked by another. Studies were classified into three categories, low, unclear and high risk of bias, based on the components previously listed. Similarly to the Cochrane Collaboration's tool (Higgins et al., 2011), studies with low risk of bias in all components were deemed to be of low risk of bias, studies with low or unclear risk of bias for all components were deemed to be of unclear risk and those with a high risk of bias for one or more components were deemed to be of high risk of bias.
For the sake of clarity, selected articles were categorized according to the type of fatigue they address. Articles were grouped into four categories: mental fatigue, drowsiness, physical fatigue, or muscle fatigue (Williamson et al., 2011). The following definitions were applied:
Mental fatigue—decrease in mental performance as a result of cognitive overload (due to task duration and/or workload), independent of sleepiness (Borragán et al., 2017; Hu and Lodewijks, 2020).
Drowsiness—fatigue arising from sleep- and circadian rhythm-related factors (e.g., sleep deprivation, circadian rhythm disruption), monotony or low task workload (Hu and Lodewijks, 2020).
Physical fatigue—decline in overall physical performance caused by physical exertion (Zhang et al., 2019a).
Muscle fatigue—decrease in an isolated muscle performance due to reduced contractile activity (Allen et al., 2008; Wan et al., 2017).
Hereafter, the term fatigue presented in italic refers to fatigue in general. Articles addressing vigilance detection were considered as well but did not define an own category. This is because vigilance has been defined as the ability to sustain attention over prolonged time periods (Oken et al., 2006), and decrements in vigilance are strongly associated with fatigue onset but it cannot be considered as an individual type of fatigue.
Results
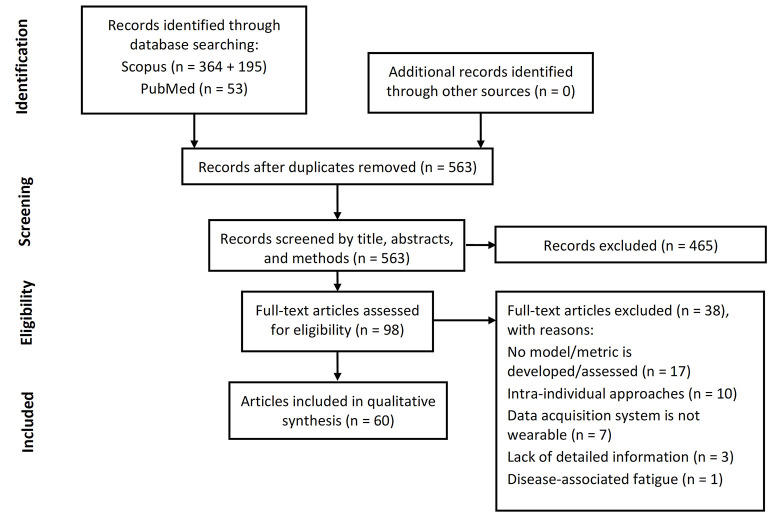
A total of 612 articles were retrieved in the literature search. After removing duplicates 563 remained. Of the identified articles, 465 were discarded during the screening phase due to lack of part of the inclusion criteria. The full text of the remaining 98 articles was assessed for eligibility. Of these, 38 were excluded for not developing a fatigue model/index or not assessing its performance (n = 17), proposing intra-individual approaches (n = 10), not using a wearable system to acquire data (n = 7), or lacking detailed information regarding the procedure used for model/index development (e.g., type of data used to develop the model, data acquisition system, etc., n = 3). Articles addressing disease-associated fatigue (Motta et al., 2016) were deemed to be outside the scope of this review and were therefore excluded (n = 1). Thus, 60 articles were included in this review: 26 conference proceedings and 34 journal articles. The articles selection process is summarized in Figure 1.
Figure 1.
PRISMA flowchart. Flow of information through the different phases of articles selection process.
For maximum clarity, each article has been assigned a unique number by which it will be referred to throughout this work. Table 1 provides the list of included articles. Among them, eight address mental fatigue (#1–#8), three vigilance detection (#9–#11), 34 drowsiness (#7, #12–#44), 12 physical fatigue (#45–#56), and four muscle fatigue (#57–#60). A total of 59 different studies are included in the present review as article #46 acknowledged the use of previously collected data (from #53).
Table 1.
List of included studies with the respective number and citation information, starting from studies addressing mental fatigue (#1–#8), followed by studies addressing vigilance detection (#9–#11), drowsiness (#12–#44), physical fatigue (#45–#56) and, lastly, muscle fatigue (#57–#60).
| No. | Citation | Title of Paper |
|---|---|---|
| 1 | Zeng et al., 2020 | Nonintrusive monitoring of mental fatigue status using epidermal electronic systems and machine-learning algorithms |
| 2 | Li et al., 2020 | Identification and classification of construction equipment operators' mental fatigue using wearable eye-tracking technology |
| 3 | Lamti et al., 2019 | Mental fatigue level detection based on event related and visual evoked potentials features fusion in virtual indoor environment |
| 4 | Zhang Y. et al., 2018 | A deep temporal model for mental fatigue detection |
| 5 | Lee et al., 2019b | Emotion and fatigue monitoring using wearable devices |
| 6 | Huang et al., 2018 | Detection of mental fatigue state with wearable ECG devices |
| 7 | Choi et al., 2018 | Wearable device-based system to monitor a driver's stress, fatigue, and drowsiness |
| 8 | Al-Libawy et al., 2016 | HRV-based operator fatigue analysis and classification using wearable sensors |
| 9 | Samima et al., 2019 | Estimation and quantification of vigilance using ERPs and eye blink rate with a fuzzy model-based approach |
| 10 | Wang et al., 2019 | Detecting and measuring construction workers' vigilance through hybrid kinematic-EEG signals |
| 11 | Chen et al., 2018 | Developing construction workers' mental vigilance indicators through wavelet packet decomposition on EEG signals |
| 12 | Ko et al., 2020 | Eyeblink recognition improves fatigue prediction from single-channel forehead EEG in a realistic sustained attention task |
| 13 | Sun et al., 2020 | Recognition of fatigue driving based on steering operation using wearable smart watch |
| 14 | Foong et al., 2019 | An iterative cross-subject negative-unlabeled learning algorithm for quantifying passive fatigue |
| 15 | Wen et al., 2019 | Recognition of fatigue driving based on frequency features of wearable device data |
| 16 | Zhang M. et al., 2018 | An application of particle swarm algorithms to optimize hidden markov models for driver fatigue identification |
| 17 | Zhang et al., 2017 | Design of a fatigue detection system for high-speed trains based on driver vigilance using a wireless wearable EEG |
| 18 | Fu et al., 2016 | Dynamic driver fatigue detection using hidden markov model in real driving condition |
| 19 | Boon-Leng et al., 2015 | Mobile-based wearable-type of driver fatigue detection by GSR and EMG |
| 20 | Ko et al., 2015 | Single channel wireless EEG device for real-time fatigue level detection |
| 21 | Kundinger and Riener, 2020 | The potential of wrist-worn wearables for driver drowsiness detection: a feasibility analysis |
| 22 | Kundinger et al., 2020a | Assessment of the potential of wrist-worn wearable sensors for driver drowsiness detection |
| 23 | Kundinger et al., 2020b | Feasibility of smart wearables for driver drowsiness detection and its potential among different age groups |
| 24 | Gielen and Aerts, 2019 | Feature extraction and evaluation for driver drowsiness detection based on thermoregulation |
| 25 | Mehreen et al., 2019 | A hybrid scheme for drowsiness detection using wearable sensors |
| 26 | Kim and Shin, 2019 | Utilizing HRV-derived respiration measures for driver drowsiness detection |
| 27 | Kartsch et al., 2019 | Ultra low-power drowsiness detection system with BioWolf |
| 28 | Lee et al., 2019a | Using wearable ECG/PPG sensors for driver drowsiness detection based on distinguishable pattern of recurrence plots |
| 29 | Dhole et al., 2019 | A novel helmet design and implementation for drowsiness and fall detection of workers on-site using EEG and random-forest classifier |
| 30 | Ogino and Mitsukura, 2018 | Portable drowsiness detection through use of a prefrontal single-channel electroencephalogram |
| 31 | Nakamura et al., 2018 | Automatic detection of drowsiness using in-ear EEG |
| 32 | Zhou et al., 2018 | Vigilance detection method for high-speed rail using wireless wearable EEG collection technology based on low-rank matrix decomposition |
| 33 | Lemkaddem et al., 2018 | Multi-modal driver drowsiness detection: a feasibility study |
| 34 | Li and Chung, 2018 | Combined EEG-gyroscope-tDCS brain machine interface system for early management of driver drowsiness |
| 35 | Li et al., 2015 | Smartwatch-based wearable EEG system for driver drowsiness detection |
| 36 | Li and Chung, 2015 | A context-aware EEG headset system for early detection of driver drowsiness |
| 37 | Lee et al., 2016 | Standalone wearable driver drowsiness detection system in a smartwatch |
| 38 | Leng et al., 2015 | Wearable driver drowsiness detection system based on biomedical and motion sensors |
| 39 | Zhang S. et al., 2018 | Low-power listen based driver drowsiness detection system using smartwatch |
| 40 | Cheon and Kang, 2017 | Sensor-based driver condition recognition using support vector machine for the detection of driver drowsiness |
| 41 | Rohit et al., 2017 | Real-time drowsiness detection using wearable, lightweight brain sensing headbands |
| 42 | Niwa et al., 2016 | A wearable device for traffic safety - a study on estimating drowsiness with eyewear, JINS MEME |
| 43 | Ha and Yoo, 2016 | A multimodal drowsiness monitoring ear-module system with closed-loop real-time alarm |
| 44 | Lee et al., 2015 | Smartwatch-based driver alertness monitoring with wearable motion and physiological sensor |
| 45 | Sedighi Maman et al., 2020 | A data analytic framework for physical fatigue management using wearable sensors |
| 46 | Nasirzadeh et al., 2020 | Physical fatigue detection using entropy analysis of heart rate signals |
| 47 | Torres et al., 2020 | Detection of fatigue on gait using accelerometer data and supervised machine learning |
| 48 | Khan et al., 2019 | A novel method for classification of running fatigue using change-point segmentation |
| 49 | Ameli et al., 2019 | Quantitative and non-invasive measurement of exercise-induced fatigue |
| 50 | Zhang et al., 2019b | Automated monitoring of physical fatigue using jerk |
| 51 | Tsao et al., 2019 | Using non-invasive wearable sensors to estimate perceived fatigue level in manual material handling task |
| 52 | Wang et al., 2018 | A heterogeneous ensemble learning voting method for fatigue detection in daily activities |
| 53 | Sedighi Maman et al., 2017 | A data-driven approach to modeling physical fatigue in the workplace using wearable sensors |
| 54 | Aryal et al., 2017 | Monitoring fatigue in construction workers using physiological measurements |
| 55 | Li et al., 2017 | A neuro-fuzzy fatigue-tracking and classification system for wheelchair users |
| 56 | Buckley et al., 2017 | Binary classification of running fatigue using a single inertial measurement unit |
| 57 | Karvekar et al., 2019 | A data-driven model to identify fatigue level based on the motion data from a smartphone |
| 58 | Papakostas et al., 2019 | Physical fatigue detection through EMG wearables and subjective user reports - a machine learning approach toward adaptive rehabilitation |
| 59 | Nourhan et al., 2017 | Detection of muscle fatigue using wearable (MYO) surface electromyography based control device |
| 60 | Mokaya et al., 2016 | Burnout: a wearable system for unobtrusive skeletal muscle fatigue estimation |
Studies have examined the use of wearable technologies for fatigue quantification in occupational settings as well as for healthcare, sports, and exercise applications. Among these, fatigue in occupational settings, and in particular fatigue in transportation, has been the most extensively researched topic. In 44 of the 59 selected studies, authors propose systems for fatigue monitoring in occupational settings (Table 2). From the 44 studies targeting occupational settings, 29 introduce methods for fatigue detection in transportation, of which 27 address driver drowsiness monitoring (#7, #12–#16, #18–#24, #26, #28, #33–#44). High-speed train driver's drowsiness (#17, #32) has also been investigated.
Table 2.
Application domain of wearable systems proposed in the included studies according to the concept they investigate.
| Type of fatigue/Application field | General-purpose | Healthcare | Sport and exercise | Transportation | Other occupations | Other applications | Total # studies |
|---|---|---|---|---|---|---|---|
| Mental fatigue | #5 | #4 | #7 | #1, #2, #6, #8 | #3 | 8 | |
| Vigilance detection | #9 | #10, #11 | 3 | ||||
| Drowsiness | #25, #30, #31 | #7, #12–#24, #26, #28, #32–#44 | #27, #29 | 34 | |||
| Physical fatigue | #47 | #52, #55 | #48, #49, #56 | #45, #46, #50, #51, #53, #54 | 11* | ||
| Muscle fatigue | #58 | #60 | #57, #59 | 4 | |||
| Total # studies | 6 | 4 | 4 | 29* | 15* | 1 | 59* |
Article #7 addresses both drowsiness and mental fatigue; articles #46 and #53 use data from the same study.
The application of wearable systems to monitor fatigue has been also foreseen in heavy industries such as construction (#2, #10, #11, #50, #54) and manufacturing (#45, #53) as well as in other occupations involving manual material handling tasks (#51). The prevention of work-related musculoskeletal disorders (#57, #59) along with overwork-related disorders (#6), and the monitoring of workers in mentally demanding occupations (#1) such as pilots and surgeons, are also among occupation-related applications for this type of technology.
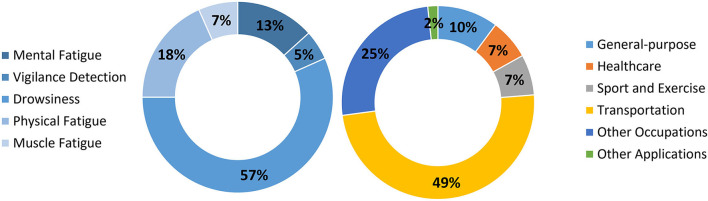
The remaining fatigue monitoring studies were allocated to the other application domains such as sport and exercise (#48, #49, #56, #60), brain-computer interfaces (#3) as well as healthcare (#4). Fatigue monitoring in rehabilitation (#58), prevention of fatigue-induced falls and injuries (#52), and monitoring of manual wheelchair users' fatigue (#55) are some examples of healthcare-related applications. Figure 2 gives an overview of the proportion of research in wearable technologies for fatigue monitoring according to the type of fatigue and systems' application domains.
Figure 2.
Type of fatigue and technology application domain.
The current literature emphasizes the use of wearable systems to acquire subjects' physical and physiological data, which lays the foundation for fatigue quantification through behavioral- and physiological signal-based methods. Thus, the various approaches proposed for fatigue monitoring using wearable devices over the last five years fall within one of these two methods for fatigue quantification. A summary of study characteristics is given separately for each category of fatigue in Tables 3–7.
Table 3.
Summary of characteristic of studies that investigated mental fatigue quantification using wearable devices.
| No. | Type of study | # of participants | Fatiguing task | Task duration | Input data | Reference measure | Modeling approach | Output | Model performance |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Lab | 3 | Mental arithmetic operations, reading professional literature | 60 min | ECG, GSR, RES | Subjective self-report questionnaires, reaction time test | Decision Trees | 3 levels | ACC >84% |
| 2 | Lab | 6 | Excavation operating simulation | 60 min | Eye movement | SSS, NASA-TLX, task performance | SVM | 3 levels | ACC = 85% precision = 86.6% recall = 85.9% F1 score = 85.1% |
| 3 | Lab | 10 | Virtual navigation | 90 min | EEG | NASA-TLX | Dempster–Shafer fusion technique | 4 Levels | F-score = 60–80% |
| 4 | Field | 6 | Not stated | Not stated | PPG, GSR, TSk | CFQ | Deep convolutional autoencoding memory network | Binary | ACC = 82.9% |
| 5 | Lab | 10 | Not stated | Not stated | GSR, PPG | Likert scale | Multilayer neural networks | 4 levels | ACC = 71.2% |
| 6 | Lab | 29 | Quiz with 55 questions | 54 ± 8 min | ECG | CFQ | K-nearest neighbors | Binary | ACC = 75.5% AUC = 0.74 |
| 7 | Lab | 28 | Simulated driving | 150 min | GSR, PPG, TSk, motion | Not stated | SVM | 4 states (normal, stressed, fatigued and/or drowsy) | ACC = 68.31% (4 states)/ ACC = 84.46% (3 states) |
| 8 | Field | 6 | Not stated | Not stated | ECG, TSk | HRV metric | SVM | Binary | ACC = 94.3%* |
ECG, electroencephalogram; EEG, electroencephalogram; GSR, galvanic skin response; PPG, photoplethysmogram; RES, respiration; TSk, skin temperature; CFQ, the Chalder fatigue scale; HRV, heart rate variability; NASA-TLX, NASA task load index; SSS, Stanford sleepiness scale; SVM, support vector machine; ACC, accuracy; AUC, area under the receiver operating characteristic curve.
Calculated average of classes (97.2% for alert, and 91.3% for fatigued state).
Study Design
The vast majority of the studies were conducted in laboratory environments (n = 54). Studies involved 3–50 subjects, with an average of 14 participants. They focus particularly on short-term monitoring, however, three studies explored long-term fatigue monitoring in real-world settings (six weeks of monitoring in #4, 30 days in #8, and one week in #30). Although the use of selected tasks to induce fatigue was found to be prevalent (in 54 studies), none of the long-term studies reported the type of fatigue-inducing tasks subjects performed over the monitoring period.
Fatigue-Inducing Tasks
Fatigue-inducing tasks varied greatly among studies, not only due to the type of fatigue investigated, but also in view of the system's final application (see Tables 3–7, columns “Fatiguing task” and “Task duration”). Among them, simulated tasks were found to be predominant, especially in studies exploring driver drowsiness (Table 5). Resemblance to real-world settings and avoidance of the risk associated with drowsy driving are the main reasons for this preference.
References Measures of fatigue
The included articles used several reference measures of fatigue. Like fatigue-inducing tasks, gold-standard measures differed between studies, even among those investigating the same type of fatigue (see Tables 3–7, column “Reference measure”). Few studies did not use any reference measure for fatigue based on the assumption that subjects would be in a non-fatigued state before performing the fatigue-inducing task, and in a fatigued state right after the task. However, the use of reference measures of fatigue provides a means to confirm the success in inducing fatigue.
Reference measures used in the studies comprised of validated questionnaires and scales as well as other subjective assessments; behavioral-based measures, either based on direct observation by investigators or a physician, or based on video recordings; performance measures, including task performance and reaction time; and physiological-based measures derived from HR and HR variability (HRV), EEG, EMG as well as blood lactate levels.
Each of these fatigue measurement methods has its own limitations. In particular, subjective scales and questionnaires can give different outcomes for similar physiological changes between subjects. To cope with this limitation, Karvekar et al. (#57) used a short perception of the exertion calibration process to improve consistency among subjects.
Fatigue Quantification Approaches
In most of the articles, the authors have proposed several fatigue models and compared their performance. Only the models considered to perform the best are presented in this review. From the included articles, 53 have proposed learning algorithms to model fatigue (see Tables 3–7, column “Modeling approach”). Within those learning algorithms, supervised machine learning approaches are prevalent, in particular support vector machines. Supervised learning consists of using input-output paired samples to infer the function that maps the input data (i.e., physiological and motion data) to the output (i.e., fatigue level). It relies on the availability of labeled data, and thus requires the use of a gold-standard measure of fatigue.
The labeling of datasets is usually done manually. However, Li et al. (#2) have proposed an automatic data labeling method based on Toeplitz Inverse Covariance-based Clustering (TICC). This clustering method identifies repeated patterns in multivariable time series and clusters time series subsequences accordingly, enabling automatic data labeling. In their work, 3 levels of mental fatigue were inferred based on TICC, namely low level, transition phase, and high level. Foong et al. (#14) have approached the problem of fatigue detection from a different perspective. They labeled a small amount of data acquired while subjects were in an alert state (positive class) and used features from these data to iteratively extract, from an unlabelled dataset, drowsy data (negative class). When using this algorithm, referred to as iterative negative-unlabelled learning algorithm, gold-standard values of subjects' fatigue level are no longer necessary. Foong argued that labeling alert data is easier and more precise than labeling fatigue states.
Most research has addressed fatigue quantification as a binary classification problem, meaning that proposed solutions determine the presence or absence of fatigue at a given point in time (see Tables 3–7, column “Output”). On the other hand, some researchers have addressed it as a multilevel problem (n = 13), considering three to five discrete levels of fatigue. Studies exploring both approaches (#21, #33, #34, #57) have found that the binary approach tends to result in better performance, even though reported improvement in accuracy ranges from <1 to 30%.
To differentiate fatigue in discrete levels, researchers have often set decision rules based on reference measure thresholding. It is of interest to note that studies using the same reference measure of fatigue still diverge on the measurement frequency and applied thresholds. As shown in Table 8, this was the case for the Karolinska Sleepiness Scale (KSS), the most used scale among studies investigating drowsiness (Table 5). Karolinska Sleepiness Scale was recorded at intervals of 1–10 min and subjects were deemed drowsy if their ratings were equal or higher than 5/9, 7/9, or 9/9, depending on the study. This divergence can also be observed in studies using Borg's RPE, a scale commonly used in studies exploring physical fatigue (Table 6).
Table 5.
Summary of characteristic of studies that investigated drowsiness quantification using wearable devices.
| No. | Type of study | # of participants | Fatiguing task | Task duration | Input data | Reference measure | Modeling approach | Output | Model performance |
|---|---|---|---|---|---|---|---|---|---|
| 7 | Lab | 28 | Simulated monotonous driving | 120 min | GSR, PPG, TSk, motion | Video-based reference | SVM | 4 states (normal, stressed, fatigued and/or drowsy) | ACC = 68.31% (4 states)/ ACC = 84.46% (3 states) |
| 12 | Lab | 15 | Simulated night-time highway driving (lane-departure paradigm) | 60 min | EEG (brain activity and eye blinking) | Reaction time | Multiple Linear regression | Binary | Se = 58% Sp = 73% ACC = 68% |
| 13 | Lab | 10 | Simulated highway driving | Not stated | Motion | Video-based reference, KSS | SVM | Binary | ACC = 83.3% |
| 14 | Lab | 29 | Target hitting game (alertness activity) and simulated driving | 7 min + 60 min | EEG | KSS | Iterative negative-unlabelled learning algorithm | Subject's most fatigued block | ACC = 93.8% |
| 15 | Lab | 10 | Simulated driving | 90 min | Motion | Video-based reference | SVM | Binary | ACC = 82.6% |
| 16 | Lab | 20 | Simulated driving | 120 min | Eye movement | Real fatigue probability calculated based on heart rate test and subjective evaluation | HMM | Binary | ACC = 80% |
| 17 | Lab | 10 | Simulated train driving while sleep deprived | Not stated | EEG | Investigator's observation | SVM | Binary | ACC = 90.7% Se = 86.8% FP = 5.4% |
| 18 | Field | 12 | Real highway driving | 210 min | EEG, EMG, RES, context | Not stated | First order HMM | Probabilities of fatigue | AUC = 0.84* |
| 19 | Lab | 6 | Not stated | Not stated | EMG, GSR | KSS, physician observation | SVM | Binary | Precision rate = 92% |
| 20 | Lab | 15 | Simulated driving | 60 min | EEG | Reaction time | Linear regression model | Reaction time | ACC = 93.9% RMSE = 219.98 ms |
| 21 | Lab | 28 | Level-2 automated ride | 45 min | PPG | KSS | KNN | Binary/3 levels | ACC = 99.4% F-score = 0.99/ ACC = 98.5% F-score = 0.99 |
| 22 | Lab | 27 | Simulated automated ride | 45 min | PPG | Weinbeer scale, micro-sleep events (based on eye closure duration) | Decision Stump | Binary | ACC = 73.4% F-score = 0.74** |
| 23 | Lab | 10 (study A)/30 (study B) | Simulated monotonous driving under sleep deprivation/simulated monotonous driving | 60 min/45 min | PPG | KSS and video-based reference/KSS | Subspace KNN | Binary | ACC = 99.9% Se = 100% Sp = 100% precision = 100% NPV = 100% |
| 24 | Lab | 19 | Simulated monotonous driving under different lightning conditions and levels of communication between subjects and researcher | 90–150 min | TSk | SSS | Decision Trees | Binary | Se = 77.8% Sp = 100% ACC = 88.9% |
| 25 | Lab | 50 | Watching a 3D rotating screen saver while sitting on a comfortable seat and sleep deprived | 20 min | EEG (brain activity and eye blinking), motion | KSS | SVM with linear kernel | Binary | ACC = 86.5% (LOOCV)/ ACC = 92% Se = 88% Sp = 96% precision = 95.6% (Hold-out validation) |
| 26 | Lab | 6 | Simulated driving | 60 min | ECG | Video-based reference | SVM regression | Binary | AUC = 0.95 |
| 27 | Lab | 3 | Simulating drowsy state in the late night | 5 times per state (approx. 4 min in total) | EEG (brain activity and eye blinking), motion | Parameters threshold determined by authors | Nearest Centroid Classifier based on K-means clustering | 5 levels | ACC = 83% |
| 28 | Lab | 6 | Simulated driving | 60–120 min | ECG/PPG | Video-based reference | Convolutional neural network | Binary | ACC = 70%/64% precision = 71%/71% recall = 85%/78% F-score = 77%/71% |
| 29 | Lab | 4 | Hand-eye-coordination game in a sleep deprived condition | approx. 8 min (500 s) | EEG | Not stated | Random forest | 3 states (normal, sleepy, fallen) | ACC = 98% |
| 30 | Field | 29 | Not stated | Not stated | EEG | KSS | SVM with radial basis function kernel | Binary | precision = 73.5% Se = 88.7% Sp = 45.2% ACC = 72.7% F-score = 80.4% |
| 31 | Lab | 23 | 4 naps while sleep deprived | 20 min each nap | EEG | Clinician scoring (based on EEG data) | SVM with radial basis function kernel | Binary | ACC = 80% Kappa coefficient = 0.53 |
| 32 | Lab | 10 | Simulated high-speed train driving while sleep deprived | Not stated | EEG | Not stated | Robust principal component analysis algorithm | Binary | ACC = 99.4% |
| 33 | Lab | 15 | Simulated driving | 60 min | PPG | KSS, reaction time, total overrun area | KNN | Binary/3 levels | ACC = 93%/75% |
| 34 | Lab | 17 | Simulated monotonous driving | 60 min | EEG, motion | Wierwille scale | linear SVM | Binary/5 levels | ACC = 96.2%/93.7% |
| 35 | Lab | 20 | Simulated monotonous driving | 60 min | EEG | PERCLOS, number of adjustments on steering wheel | SVM-based posterior probabilistic model | 3 levels (alert, early warning, full warning) | ACC = 89%*** |
| 36 | Lab | 6 | Simulated monotonous driving | 60 min | EEG, motion | Wierwille scale | SVM with linear kernel | Binary | ACC = 96.2% Se = 96.5% Sp = 95.6% |
| 37 | Lab | 20 | Simulated driving | 60 min | Motion | KSS (rated by observer and confirmed by participant) | SVM | 5 levels | ACC = 98.2% |
| 38 | Lab | 20 | Simulated driving | 60 min | PPG, GSR, motion | KSS (rated by observer and confirmed by participant) | SVM | 5 levels | ACC = 98.3% |
| 39 | Lab | 4 | Simulated driving | Not stated | PPG, motion | Video-based reference, driver's physical state | SVM with radial basis function kernel | Binary | ACC = 94.4% precision-recall score = 96.4% |
| 40 | Lab | 10 | Watching the photographed actual road video before and after doing a PVT | 50 min | PPG | Not stated | SVM | Binary | ACC = 96.3% recall = 94.7% precision = 97.8% |
| 41 | Lab | 23 | Simulated driving while sleep deprived | 60 min | EEG | Not stated | SVM with temporal aggregation | Binary | ACC = 87% |
| 42 | Lab | 45 | Sit on a chair and watch a movie of night driving while holding a steering wheel | 80 min | EOG | Video-based reference | Random forest | Binary | ACC = 80% |
| 43 | Lab | Unclear | Sleep deprivation (4 h of sleep) | 20 min | EEG, NIRS | Oxford Sleep Resistance Test | 3rd order polynomial SVM | 3 levels (1, 2, or 3 consecutive missed stimulus) | ACC = 77.3%**** |
| 44 | Lab | 12 | Simulated driving | 480 min | PPG, motion | Observation, KSS (rated by observer) | Mobile-based SVM | Binary | ACC = 95.8% |
ECG,electroencephalogram; EEG,electroencephalogram; EMG,electromyogram; EOG,electrooculogram; GSR,galvanic skin response; NIRS,near-infra-red spectroscopy; PPG,photoplethysmogram; RES,respiration; TSk,skin temperature; PVT,psychomotor vigilance test; KSS,Karolinska Sleepiness Scale; PERCLOS,percentage of eye closure; SSS,Stanford Sleepiness Scale; KNN,k-nearest neighbors; HMM,hidden Markov model; SVM,Support Vector Machine; ACC,accuracy; AUC,area under the receiver operating characteristic curve; FP,false positive; LOOCV,leave-one-out cross-validation; NPV,negative predictive value; RMSE,root mean square error; Se,sensitivity; Sp,specificity.
Calculated average among all subjects (AUC between 0.734 and 0.960).
Calculated average of classes (0.82 for non-drowsy and 0.65 drowsy class).
Average of the 3 states (91.25% for alert, 83.8% for early-warning group, and 91.9% for full warning group).
Calculated average of classes (88.1 for 1, 77.9 for 2, and 65.9 for 3 missed stimulus).
Table 6.
Summary of characteristic of studies that investigated physical fatigue quantification using wearable devices.
| No. | Type of study | # of participants | Fatiguing task | Task duration | Input data | Reference measure | Modeling approach | Output | Model performance |
|---|---|---|---|---|---|---|---|---|---|
| 45 | Lab | 15/13 | Simulated manual material handling task/Supply pick-up and insertion task | 180 min | Motion, age/ECG | Borg's RPE | Random forest | Binary | Se = 84.7/82.0% Sp = 86.4/88.9% ACC = 85.5/85.4% G-mean = 0.85/0.85 Consistency = 0.15/0.10 |
| 46 | Lab | 8 | Part assembly task, supply pick-up, and insertion task, manual material handling task | 180 min | ECG | Borg's RPE | Random Forest | Binary | ACC = 69.4–90.4% Se = 66.2–82.3% Sp = 71.7–96.2% AUC = 0.86–0.88 |
| 47 | Lab | 9 | 25 m shuttle sprint | Until sprint time decrement of 5% for two consecutive tests | Motion | Not stated | SVM | Binary | ACC = 90% Cohen's kappa = 0.75 |
| 48 | Lab | 12 | Incremental treadmill running test | Time to exhaustion | EMG | Blood lactate samples | Random Forest | 3 states (aerobic, anaerobic and recovery phase) | AUC = 0.86 |
| 49 | Lab | 20 | Treadmill running program, L-drill and step test, crunch and jumps, sit to stand up, and push-up | 7.5 min | Motion | Rate of perceived exertion a day after the protocol | Fatigue score | Binary |
r = 0.95 (male) r = 0.70 (female) |
| 50 | Lab | 6 | Wall building/two bricklaying activities | Approx. 30 min/50 min | Motion | Not stated | SVM with quadratic kernel/SVM with medium gaussian kernel | Binary | ACC = 79.2%/ ACC = 65.9% |
| 51 | Lab | 6 | Lifting/lowering and turning task in 2 different paces (quick/slow) | 5 min each task | RES, GSR, PPG | Borg's RPE | Linear regression model | 3 levels of fatigue | Correct rate = 66.7% Absolute difference = 1.9 R2 = 0.39 |
| 52 | Lab | 15 | Jumping rope consecutively | 5 min (repeated until exhaustion) | Motion, age, height, weight | Maximum rope number | Heterogeneous ensemble learning voting method | Binary | ACC = 92% Precision = recall = = F1-score = 0.73 |
| 53 | Lab | 8 | Simulated manufacturing tasks | 180 min | ECG, motion | Borg's RPE | Least absolute shrinkage and selection operator model | Binary/RPE prediction | Se = 1, Sp = 0.79/ MAE = 2.16 |
| 54 | Lab | 12 | Simulated construction activity | 200 trials (approx. 150 min) | TSk, ECG, personal information | Borg's RPE | Boosted trees | 4 levels | ACC = 82.6% |
| 55 | Lab | 8 | Propel a wheelchair at a constant speed of 1.6 m/s | Until being unable to meet the required speed | ECG, EMG, motion | Self-reported fatigue | Neuro-fuzzy classifier | 3 levels | ACC = 80% |
| 56 | Field | 21 | The Beep test or Pacer test until exhaustion | Time to exhaustion or Borg's RPE ≥18 | Motion | Borg's RPE | Random Forest | Binary | ACC = 75% Se = 73% Sp = 77% F1-score = 75% |
ECG,electroencephalogram; EMG,electromyogram; GSR,galvanic skin response; PPG,photoplethysmogram; RES,respiration; TSk,skin temperature; RPE,ratings of perceived exertion; SVM,Support Vector Machine; ACC,accuracy; AUC,area under the receiver operating characteristic curve; MAE,mean absolute error; r,correlation coefficient; R2, R-squared; Se, sensitivity; Sp, specificity.
In #8, Al-Libawy et al. used individualized thresholds. Besides, Kim and Shin (#26) considered a subject to be fatigued from the first moment a drowsy event was detected until the end of the experiment. They assumed that subjects' drowsiness states will maintain if no action is taken against it.
Two studies (#30 and #53) have investigated the influence of the reference measure thresholds on the performance of supervised learning algorithms. Both studies have found that algorithms' performance alters according to the thresholds considered, and in #30 authors concluded that model performance improved when using the thresholds that maximize the distance between alert and drowsy states. Besides, #53 has shown that those thresholds can also alter the subset of predictors deemed relevant for fatigue level prediction.
As an alternative to classification, some studies have proposed solutions to monitor fatigue in a continuous manner, which does not require setting thresholds. This can be achieved through the prediction of fatigue indicators, e.g., reaction times or fatigue scale ratings, using regression models (see #20, #48, and #60). A Hidden Markov model (HMM, #16) and a vigilance index (#11) have also been proposed for the same purpose.
A few studies combined the continuous with the binary (#53) or multilevel (#10) approaches, instead of approaching the fatigue quantification problem from a single perspective. Two other studies proposed models to detect not only fatigue, but also other states strongly linked to safety and performance, for instance, stress and fall detection (#7, #29). Apart from learning algorithms, indices calculated based on the monitored parameters (#10, #11, #49) have also been developed for fatigue monitoring purposes. Furthermore, different statistical modeling techniques, namely Hidden Markov modeling, Dempster-Shafer Fusion technique, and Fuzzy logic, have been explored as described below.
The HMM describe the probability of transition between discrete, unobservable (hidden) states, based on observable parameters generated by those states (Wallisch et al., 2009). Such models have been widely applied for predicting sequences and time series due to their capability of modeling dynamic processes. This is the reason why #16 and #18 have developed HMM for fatigue monitoring.
Lamti el al. (#3) have proposed a Dempster-Shafer Fusion technique to determine subjects' fatigue levels. This technique allowed the fusion of features from data acquired by different sensors in a way that data uncertainties and heterogeneity were considered, thus providing a more robust estimation of fatigue levels.
Lastly, Samima et al. (#9) has proposed a fuzzy logic-based system for vigilance level monitoring. Fuzzy logic enables the numeric quantification of the different transitional levels between two opposite states, in this case, non-vigilance and vigilance. Samima's algorithm represents another approach to address fatigue as a continuous variable. Although the numerical values were grouped into four (no, more, moderate, or high) vigilance levels for the sake of model validation, the proposed model was found to be effective. A similar approach has been proposed by Li et al. (#35), who developed a support vector machine-based posterior probabilistic model which estimates driver drowsiness probability in values ranging from 0 to 1.
Performance of Proposed Measures
The proposed approaches were found to perform very well in detecting fatigue, as seen in Tables 3–7, column “Model performance.” Reported accuracies range from approximately 70% to up to 100%. Despite such promising results, the performance of the proposed models on independent datasets has been assessed quantitatively in only one study. Kundinger et al. (#23) trained their models using different datasets which included data of young and/or old people. They evaluated models' performance in datasets other than the one used for model development and noticed that it results in lower accuracies, even when both datasets included data from people of the same age group. From the proposed approaches, four (#12, #27, #34, #35) were tested for real-time monitoring, revealing high accuracies for all approaches.
Table 7.
Summary of characteristic of studies that investigated muscle fatigue quantification using wearable devices.
| No. | Type of study | # of participants | Fatiguing task | Task duration | Input data | Reference measure | Modeling approach | Output | Model performance |
|---|---|---|---|---|---|---|---|---|---|
| 57 | Lab | 24 | 2-min squatting at 8 squats/min | Time until Borg's RPE ≥17 | Motion | Borg's RPE | Support vector machine | Binary/4 levels | ACC = 91/61% |
| 58 | Lab | 10 | Shoulder flexion, shoulder abduction, elbow extension performed using a Barrett WAM arm | Time until self-reported fatigue + 10 s (3 repetitions per exercise) | EMG | Self-report | Gradient Boosting | Binary |
F1-score = 70.4–76.6% Success rate = 73–74% |
| 59 | Lab | 3 | Muscle fatiguing exercise | Time until self-reported fatigue | EMG | Not stated | Backpropagation neural networks | Binary | ACC = 100% |
| 60 | Field | 5 | Isotonic/isometric bicep curl, Isotonic/isometric leg extension | Time until failure (1–2 min) | Motion | Gradient of the Dimitrov spectral index (based on EMG) | Regression tree model | Gradient of the relative change in the Dimitrov spectral fatigue index | Error <15% |
EMG,electromyogram; RPE,ratings of perceived exertion; ACC,accuracy.
Fatigue Monitoring Systems
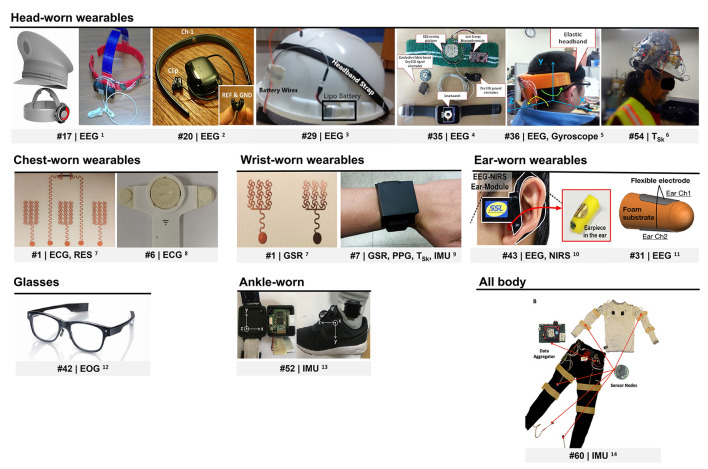
Several wearable devices have been used to obtain data regarding subjects' fatigue level. Researchers have either employed wearable sensors available on the market or devised their own systems (n = 22, see Supplementary Table 4, column “Data acquisition system”). Figure 3 presents some of the devised wearable devices.
Figure 3.
Wearables devised for fatigue monitoring. ECG, electrocardiogram; EEG, electroencephalogram; EOG, electrooculogram; GSR, galvanic skin response; IMU, inertial motion unit; NIRS, near-infra-red spectroscopy; PPG, photoplethysmography; RES, respiration; TSk, skin temperature. 1Reprinted from Zhang et al. (2017). 2© (2015) IEEE. Reprinted, with permission, from Ko et al. (2015). 3Reprinted from Dhole et al., (2019). © (2019) with permission from Elsevier. 4© (2015) IEEE. Reprinted, with permission, from Li et al. (2015). 5Reprinted from Li and Chung (2015). 6Reprinted from Aryal et al. (2017). © (2017) with permission from Elsevier. 7Reprinted (adapted) with permission from Zeng et al. (2020). © (2020) American Chemical Society. 8Reprinted from Huang et al. (2018). © (2018), with permission from Elsevier. 9© (2018) IEEE. Reprinted, with permission, from Choi et al. (2018). 10© (2016) IEEE. Reprinted, with permission, from Ha and Yoo, (2016). 11© (2018) IEEE. Reprinted, with permission, from Nakamura et al. (2018). 12Republished with permission of SAE International, from Niwa et al. (2016); permission conveyed through Copyright Clearance Center, Inc. 13Reprinted with permission of Fuji Technology Press Ltd., from (Wang et al., 2018). 14© (2016) IEEE. Reprinted, with permission, from Mokaya et al. (2016).
Motion (MOT) as measured by inertial measurement units (IMUs) and other motion sensors, EEG, photoplethysmography (PPG), electrocardiogram (ECG), galvanic skin response (GSR), and EMG are among the most investigated signals for fatigue level estimation. While less extensively studied, skin temperature (Tsk), respiration (RES), EYE, including oculometry and pupillometry, electrooculogram (EOG), as well as near infra-red spectroscopy (NIRS) were also found to be relevant for fatigue detection.
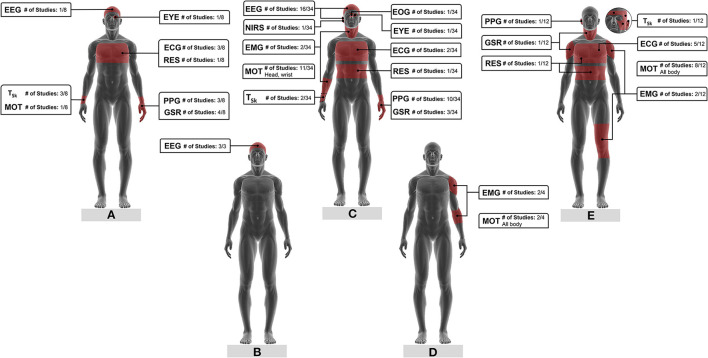
Signals as well as respective measurement locations varied with the type of fatigue investigated but were rather consistent among different studies. Figure 4 shows the physiological and motion signals used to monitor the different types of fatigue, their measurement location, and the number of studies that have explored those signals.
Figure 4.
Physiological and motion signals for (A) mental fatigue, (B) vigilance, (C) drowsiness, (D) muscle fatigue, (E) physical fatigue monitoring and respective measurement locations. The fraction number in the boxes represents the number of studies on a specific signal based on the total literature reviewed on that type of fatigue. ECG, electroencephalogram; EEG, electroencephalogram; EMG, electromyogram; EOG, electrooculogram; EYE, eye movement; GSR, galvanic skin response; MOT, motion; NIRS, near-infra-red spectroscopy; PPG, photoplethysmogram; RES, respiration; TSk, skin temperature.
Electroencephalogram is the most prominent signal for drowsiness monitoring (see Figure 4C; Table 5, column “Input data”). Furthermore, all the three studies investigating vigilance monitoring developed models and indices based on EEG data (see Figure 4B; Table 4, column “Input data”). Spectral power changes in the different frequency bands (#10–#12, #14, #17, #18, #20, #25, #27, #30, #32, #34 to #36, #41, #43) and event-related potentials (#3, #9) of EEG signals collected by wearable EEG systems contain valuable information on subjects' drowsiness, vigilance, and mental fatigue levels.
Table 4.
Summary of characteristic of studies that investigated vigilance detection quantification using wearable devices.
| No. | Type of study | # of participants | Fatiguing task | Task duration | Input data | Reference measure | Modeling approach | Output | Model performance |
|---|---|---|---|---|---|---|---|---|---|
| 9 | Lab | 10 | Two-phase Mackworth Clock Test | 30 min | EEG (brain activity and eye blinking) | Performance | Fuzzy logic | 4 levels | ACC = 95% |
| 10 | Lab | 10 | Three-trial construction task (moving two mental tubes to a predefined location) | Not stated | EEG | NASA-TLX and EEG-vigilance stage model | Vigilance ratio index | Continuous vigilance level/3 levels | r = 0.73/r = 0.75 |
| 11 | Lab | 10 | Three-trial construction task (moving two mental tubes to a predefined location) | Not stated | EEG | EEG-based benchmark | Vigilance ratio index | Continuous vigilance level | Cosine similarity = 0.90–0.92 |
EEG, electroencephalogram; NASA-TLX, NASA Task Load Index; ACC, accuracy; r, correlation coefficient.
Almost all studies acquired EEG data from headbands (Supplementary Table 4, column “Data acquisition system”). Electroencephalogramelectrodes were placed on several brain regions, particularly on frontal (#12, #14, #29, #30) and occipital lobes (#18, #34, #35, #36). Researchers designed headbands with mainly two to three dry (#20, #27, #34, #35, #36) or wet (#29) electrodes, although systems with more channels were also proposed. Two studies presented an eight-channel EEG system with stainless steel (#17) and Ag–AgCl (#32) dry electrodes embedded in a train driver's cap (Figure 3). Besides, Dhole et al. (#29) integrated their EEG monitoring system into a safety helmet (Figure 3) which houses an IMU and a wireless transmission setup. Motion sensors were likewise included in the systems proposed by three other studies (IMU in #27, three-axis gyroscope in #34 and #36).
Nakamura et al. (#31) and Ha and Yoo (#43) devised wearable systems for in-ear EEG monitoring (Figure 3). The first system consists of a wearable in-ear sensor made of viscoelastic foam with two flexible cloth EEG electrodes constructed out of conductive fabric. Nakamura and coworkers showed that a drowsiness classification model trained on their system's data performs almost as well as a model developed based on a scalp EEG headset (average difference in accuracy of approximately 6%). The second system, in turn, monitors EEG and NIRS simultaneously. It is composed of an earpiece with two fabric electrodes for EEG monitoring and NIRS driver, and an ear hook for NIRS monitoring. Ha and Yoo's work revealed that oxyhemoglobin concentration in the brain, measured by in-ear NIRS, also provides information on human drowsiness. Their findings also indicate that the use of in-ear EEG in combination with in-ear NIRS improves drowsiness detection accuracy.
Several studies found that pulse intervals, HR, and HRV derived from PPG signals collected by wearables are relevant predictors of drowsiness (Figure 4C) and mental fatigue (Figure 4A). In those studies, PPG data was acquired from subjects' wrists or fingers using mainly commercial devices, although some employed self-made systems (#5, #7, #38, #44). Choi et al. (#7) designed a multi-sensor wrist band with PPG and Tsk sensors, GSR electrodes, as well as motion sensors (acceleration and rate of rotation) to monitor driving stress, fatigue, and drowsiness (Figure 3).
Studies also showed that wearable ECG sensors can be applied for fatigue detection. ECG signals were acquired by chest strap HR monitors, except in studies #1 and #6. Zeng et al. (#1) designed epidermal electronic sensors. They fabricated filamentary serpentine mesh electrodes made of copper and a graphite-based strain sensor for simultaneous ECG, GSR, and RES monitoring (Figure 3). These sensors are applied on the skin in the form of temporary tattoos. Huang et al. (#6) used a single-channel ECG patch to acquire the data (Figure 3).
Physical and mental fatigue were found to significantly affect subjects' HR, HRV, RR intervals as well as respective spectral power and dynamics. Lee et al. (#28) investigated the use of different types of recurrence plots to detect drowsiness. Those plots were constructed using pulse intervals from PPG or RR intervals. Their results suggest that recurrence patterns, known for capturing non-linear dynamics of HRV, are reliable predictors of drowsiness.
Wearable systems with GSR electrodes located at the wrist (#4, #7), hand palms (#1), fingers (#5, #19, #38), neck, and shoulders (#51) were exploited to monitor drowsiness, mental, and physical fatigue. GSR attributes such as its average, standard deviation, number of peaks, their magnitude, and duration, as well as information regarding signal frequency spectrum were used as predictors of fatigue. Skin conductance variations also served as indicators of drivers' stress (#7, #38).
The few studies exploring EMG signals showed that wearable EMG sensors could successfully monitor physical and muscle fatigue based on a single variable. Electromyogram signals combined with other variables (e.g., EEG, RES, GSR) also detects drowsiness. Data were acquired from arm (#19, #55, #58, #59), leg (#48), and neck (#18) muscles. While some studies collected EMG signals using conventional electrodes, wireless, dry electrodes (#48, #58, #59) were also applied.
Average Tsk, its standard deviation (#4, #7, #8), slope (#24), and power spectral density (#8), have been shown to provide information on mental fatigue and drowsiness levels. All these studies measured Tsk using wrist-worn sensors. Aryal et al. (#54) took a different approach by estimating perceived physical fatigue from thermoregulatory changes monitored by temperature sensors on the face. Tsk data were acquired from subjects' temple, forehead, cheek, and ear using non-contact infra-red temperature sensors fitted into a construction safety helmet (Figure 3). Their results suggest that Tsk, especially measured at the temple, can be more useful to model physical fatigue than heart rate data.
In addition to the physiological signals already mentioned, RES, EYE, and EOG have been investigated. Breathing rate (#1, #51), peak voltage (#51), and mean frequency power (#18) of RES signals were derived from wearable sensors placed on chest and/or abdomen area. These features can be combined with other physiological signals to estimate individuals' drowsiness and mental and physical fatigue levels.
Eye movement-related features extracted from eye-tracking headsets (#2, #16) were applied for mental fatigue and drowsiness detection. Niwa et al. (#42) extracted such information from a glasses-like wearable EOG device (see Figure 3). Moreover, studies #9, #12, #25, and #27, used blink-induced artifacts that contaminate EEG recordings to derive information regarding blink rate, amplitude, and duration. This approach was found to improve vigilance and drowsiness level prediction without requiring additional equipment.
Motion tracking has a preponderant role in physical and muscle fatigue as well as drowsiness detection. While whole-body motion was recorded for physical and muscle fatigue (Figures 4D,E), head and wrist movements seem to be the focus for drowsiness detection (Figure 4C). Information relating to body motion, posture, gait patterns, and drivers' steering behaviors (#13, #44) have been estimated from wearable inertial sensors. Kinetic energy, a measure of the energy required to conduct motions (#49); jerk, which is the time derivate of acceleration signals (#50, #53); joint angles (#49); Euler angles (#56) are some of the researched features.
Among the systems used to acquire motion data are mobile phones (#47, # 57), smart watches (#13, #15, #37, #38, #39, #44), head (#25, #27, #34, #36), and ankle bands (#52, Figure 3). Mokaya et al. (#60) developed Burnout, a wearable sensor network comprised of 10 lightweight sensor nodes embedded in fitted clothing (see Figure 3). Each sensor node contained a 3-axis accelerometer able to sense muscle vibration and detect body movement.
To cope with the inter-subject variability in fatigue development and its impact on individuals' motion and physiological signals, some studies (#2, #7, #52) normalized the acquired data prior to model construction. In Choi's work (#7), four methods of normalization were used. The normalization method was determined for each feature as the one that maximizes the separability between classes.
The use of demographic attributes, such as age, height, weight (#45, #52); contextual information, for instance, sleep quality, circadian rhythm, and work condition (#18); as well as the duration of work and years of working experience (#54), in combination with physiological and motion parameters, has been shown to enhance fatigue models performance. Aryal et al. (#54) found that the use of personal information improved their model accuracy by 15%.
Maman's study (#45) has shown that the relevance of different fatigue predictors varies with the task being performed. In their work, the same methodology was applied to data acquired while subjects were performing different manufacturing tasks. Maman et al. found that the features remaining after the selection process was different for the two tasks investigated.
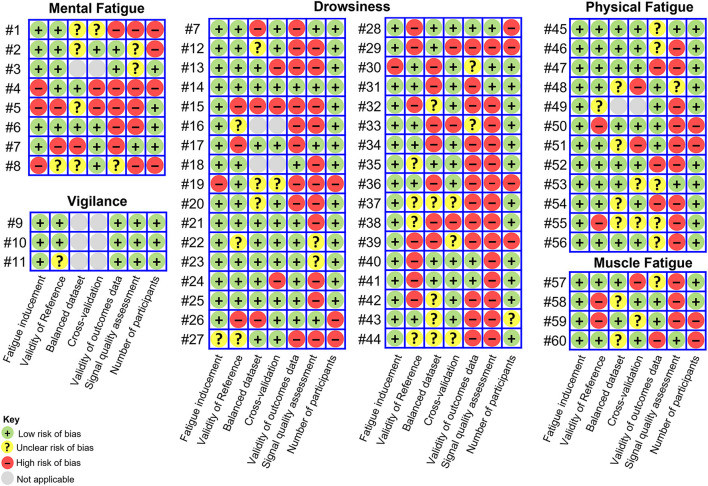
Risk of Bias Assessment
The risk of bias of included studies is depicted in Figure 5. Only few studies fell within the low (#9, #10, #14) or unclear risk of bias (#3, #11, #22, #23, #45, #53) categories. All the remaining studies were assigned to the high risk of bias category according to the criteria described in the Methods section.
Figure 5.
Risk of bias assessment. Studies with low risk of bias in all components were deemed to be of low risk of bias, studies with low or unclear risk of bias for all components were deemed to be of unclear risk and those with high risk of bias for one or more components were deemed to be of high risk of bias.
Signal quality assessment was found to be the most neglected of the methodological aspects contemplated in the risk of bias assessment. Noise and artifacts arising from several sources have an influence on data quality and wearable systems are particularly susceptible to motion artifacts (Mihajlovic et al., 2015; Boudreaux et al., 2018; Choksatchawathi et al., 2020). While these facts are well known, only few studies (n = 8) identified low-quality signal segments with the purpose of excluding those segments from further analysis or reconstructing them. Some researchers assessed the data visually and manually removed artifacts (#45, #53, #60), while others used automatic approaches.
The automatic approaches consisted of feasibility rules applied through thresholding or combination of decision rules. Those rules were either based on changes in signal amplitude and shape (#14, #31) or on the physiological feasibility of parameters derived from the signal as compared to reference values in healthy subjects (#26, #28). Choi et al. (#7) applied a sequence of four decision rules to identify valid data segments from the acquired PPG signal. Their algorithm detected irregularities in the measured pulse intervals due to false peaks, evaluated the similarity between consecutive pulses, and assessed the amount of device motion during data acquisition. Choi reported in their article an average improvement of more than 7% in pulse detection after applying the algorithm. In their work, low-quality signal segments were removed without replacement. Conversely, one study used cubic interpolation (#26) and another the neighbors mean (#28) to reconstruct the signal after the exclusion of noisy data points.
Instead of assessing the quality of the acquired data, some studies applied more sophisticated noise removal algorithms and signal reconstruction techniques to ensure high data quality. Independent component analysis (#9) was to decompose EEG signals and reconstruct signals without artifacts by removing the artifactual components. Wavelet decomposition was also investigated for the same purpose (#17, #30). In studies #10 and #11, principal component analysis was used to select the most effective EEG channels, which were 14 in total. Signals from the selected channels were then averaged to remove artifacts.
In fatigue studies, the amount of data acquired while subjects are in a non-fatigued state tends to exceed the amount of data acquired while in a fatigued state. Since fatigue is the concept of interest, this imbalance needs to be addressed and was for that reason included in the risk of bias assessment. To avoid the creation of imbalanced datasets in the first place, some researchers have acquired data while subjects were rested and fatigued, following a similar methodology. However, imbalances can be corrected through resampling the data.
Maman (#53) explored the use of random under-sampling (removes cases from the majority class) and synthetic minority over-sampling (generates synthetic examples of the minority class by interpolation; Kotsiantis et al., 2006) to equalize the amount of data acquired in a non-fatigued and fatigued states. In their work, the use of random under-sampling resulted in better performance. Synthetic minority over-sampling was also used by Kundinger et al. (#21, #22), while Wang (#52) explored oversampling (duplicates cases from the minority class).
It is also possible to address the dataset imbalance problem at the algorithm level. Zhang (#4) constructed a one-class classifier, named Deep Convolutional Autoencoding Memory network, whose data training process is only based on non-fatigue data. This model learns patterns in time series of non-fatigue data and classifies outliers as data recorded under fatigue state. More detailed information on the risk of bias assessment of the included studies can be found in Supplementary Materials.
Discussion
This review aimed at presenting the state-of-the-art of fatigue monitoring through wearable devices. A considerable amount of the current literature on the selected topic pays particular attention to drowsiness monitoring for occupational purposes, especially within the transportation industry (Figure 2). Other potential application domains foreseen for such kind of technology stretch across healthcare and sport industries (Table 2).
Overall, fatigue studies have been mainly short-term studies, conducted in laboratory settings. The tasks used to induce fatigue, selected reference measures and other methodological aspects differed considerably between studies. Researchers have used wearables available in the market or devised their own systems to acquire physiological and motion data and, based on these, detect fatigue. Supervised machine learning models, and more specifically, binary classification models, are predominant among the proposed fatigue quantification approaches.
Considering that wearables enable continuous, unobtrusive long-term monitoring, it is surprising that most of the articles only reported short-term laboratory studies. A possible explanation for this finding is shown by the main limitation of the three studies exploring long-term monitoring of fatigue in free-living environments (#4, #8, #30). It is the lack of information regarding the tasks performed by the participants over the monitoring period. As shown in Maman's study (#45), fatigue development is task-dependent (Richter et al., 2005; Yung and Wells, 2017), therefore, information regarding fatigue-inducing tasks plays a pivotal role in determining the validity domain of developed models.
Additionally, in real-world settings the acquisition of reference values of fatigue is further aggravated, particularly when using scales and questionnaires. Obtaining reference values in intervals of 2 h or three times a day, as applied in studies #4 and #30, might be inappropriate when aiming at developing a fatigue monitoring system for safety-related applications, for instance. At the same time, there is a lack of valid reference measures which can provide a continuous estimate of an individual's fatigue level non-intrusively. Hence, considerations regarding fatigue-inducing tasks and reference measures to be used are a major challenge in fatigue research.
Most of the included studies used fatigue-inducing tasks. Those tasks varied markedly from study to study, depending on the type of fatigue investigated and technology final application. Simulated tasks have been commonly used, particularly in studies investigating driver drowsiness. Despite resembling real settings, simulation environments cannot reproduce its complexity and dynamism (Techera et al., 2018). Additionally, subjects' effort and perception of risk are reduced in simulated environments (Sahayadhas et al., 2012). The effectiveness of the tasks used to induce fatigue is key for fatigue research in laboratory settings and depends to some extent on participants' engagement in those tasks. For this reason, Huang et al. (#6) offered monetary rewards to better motivate the participants. In general, the selection of fatigue-inducing tasks and their duration lacked scientific basis. Thus, questions can be raised regarding the feasibility of certain tasks which have been used.
Reference measures of fatigue also differed among studies. Some researchers neglected the use of ground truth measures of fatigue relying on the assumption that participants would be rested before performing the fatigue-inducing task and fatigued after that. Foong et al. (#14) questioned this assumption with regard to drowsiness. In their work, participants performed a hitting game prior to the fatigue-inducing task to ensure subjects were in an alert state at the start of the experiment. As noted by Ko et al. (#12), drowsiness does not evolve linearly in time, and the same can be stated with regard to fatigue in general. Indeed, there is a time-on-task effect on fatigue (Richter et al., 2005). Yet, for reasons unrelated to the study protocol, subjects may either be fatigued before performing the fatigue-inducing task or they may not become fatigued in case of high-performing individuals or if the selected task is not effective in inducing fatigue. For instance, Aryal et al. (#54) recognized, based on reference measures, that the selected fatiguing task failed to induce mental fatigue and consequently limited the scope of their investigation to physical fatigue. Therefore, the premise that subjects are rested/fatigued prior to/after the fatigue-inducing task might be a flawed one and does not justify neglecting the use of reference measures of fatigue.
Much of the literature has addressed fatigue monitoring as a binary classification problem. Considering that the major application foreseen for such a technology is fatigue risk management in occupational settings, detecting the occurrence of fatigue is not as relevant as detecting the transition to such a state (Li et al., 2020). That transition phase is crucial to prevent fatigue-related accidents since it is when corrective actions must be taken. Therefore, although applying reference measure thresholds which maximize the separability between rested and fatigued states might result in better model performance, it limits models' ability to detect the early onset of fatigue. In this sense, multilevel or continuous approaches might better address fatigue monitoring. However, the number of studies proposing such approaches is relatively low (n = 23).
Regardless the approach followed to address fatigue monitoring, the selection of the ground truth measure of fatigue and respective thresholds is crucial. It dictates the standard by which proposed models will be developed and assessed. The observed divergence between the reference measure thresholds applied in the included studies, even among those investigating the same type of fatigue for the same application (e.g., papers addressing driver drowsiness monitoring which used the KSS, see Table 8), reflects a lack of consensus regarding the adequate threshold to consider a given fatigue level as risky or unsafe. This divergence may be due to the lack of evidence on the association between a given fatigue level, task performance, and the related safety outcomes (Williamson et al., 2011).
Table 8.
Subjective scales used in the different studies: measurement frequency and fatigue thresholds.
| Reference measure | No. | Measure frequency | Measure threshold |
|---|---|---|---|
| Karolinska sleepiness scale | 14 | 10 min | Not stated |
| 19 | 3 min | Not stated | |
| 25 | 1 min | Not stated | |
| 13 | 10 min | Alert: ≤3; Fatigue: ≥7 | |
| 21 | 5 min | Alert: ≤4; Fatigue: ≥5 | |
| 23 | 5 or 10 min | Alert: ≤4; Fatigue: ≥7 | |
| 30 | 3 times/day | Alert: <3; Fatigue: >7 | |
| 33 | 5 min | Alert: ≤8; Fatigue: = 9 | |
| 18 | Not stated | Alert: <3; Transition: 3–5; Fatigue: 5–7 | |
| 22 | 5 min | Alert: ≤4; Transition: 5–6; Fatigue: ≥7 | |
| 33 | 5 min | Alert: ≤7; Transition: = 8; Fatigue: = 9 | |
| 37 | Unclear | Level 1: 1–2; Level 2: 3–4; Level 3: 5–6; Level 4: 7–8; Level 5: 9 | |
| 38 | Unclear | Level 1: 1–2; Level 2: 3–4; Level 3: 5–6; Level 4: 7–8; Level 5: 9 | |
| Borg's rating of perceived exertion | 45 | 10 min | 13 |
| 46 | 1 h | 15 | |
| 53 | 10 min | 15 | |
| 56 | Unclear | 18 | |
| 58 | After each fatiguing task set | No fatigue: <7; Fatigue: ≥15 | |
| 51 | 1 min | Low: ≤9.5; Medium: 9.5–13.5; High: 13.5 | |
| 54 | Unclear | Low: 6–11; Medium: 12–14; High: 15–16; Very high ≥17 | |
| 58 | After each fatiguing task set | No: <7; Low: ≥7; Medium: ≥11; High: ≥15 |
Models considering fatigue accumulation and recovery are lacking. Only few studies considered the temporal variation of fatigue predictors. Fatigue development is a dynamic process, and individuals' fatigue level at a given point in time is not independent from their state at previous time points. Therefore, as noted by Fu (#18), the assumption of independent and identically distributed data, commonly applied in learning algorithms, is a poor one in the case of fatigue.
Despite their constraints, the performance of the proposed models was very high. Binary classification models performed particularly well. Yet, this promising set of results should be interpreted with caution as most of the models have not been tested in independent datasets.
Furthermore, previous studies have given little attention to the data imbalance problem. Although some studies report the number of data samples used to train the models, half of the studies using learning algorithms either omitted that information or acknowledged the use of imbalanced datasets (Figure 5). Just a few researchers reported strategies to cope with class imbalance. Thus, there is the risk that models were developed using imbalanced datasets, which implies that reported accuracies may overestimate models' performance, especially classification models performance (Luque et al., 2019).
In some works, data have been acquired prior to and right after subjects performed the fatiguing task. While being a useful method to ensure the creation of balanced datasets, the acquired data does not contain information regarding fatigue mechanisms. Consequently, models developed using those datasets can be relevant to analyze which and how the monitored variables change due to fatigue but have limited applicability in domains where continuous, long-term monitoring is necessary.
A third aspect weakening the reliability of some of the proposed models is the very little effort made to ensure the acquisition of high-fidelity signals. Only 21 studies used exclusively validated data acquisition systems, and even fewer removed artifacts or noisy signal segments (Figure 5). The exclusion of low-quality data is of particular importance because it is well known that wearable devices are susceptible to noise and artifacts arising from several factors, especially sensors' movement (Shirmohammadi et al., 2016). Thus, most of the proposed fatigue models and indices were constructed based on data of limited reliability.
We found that a wide variety of physiological and motion signals have been recorded for the purpose of fatigue quantification. Signals' measurement location did not differ considerably, but their relevance and pre-eminence for fatigue monitoring depended on the type of fatigue explored (Figure 4). Even though several signals have been monitored, there has been little attempt to understand how those signals change with fatigue onset and which data features better represent it. We believe this explains the great variability of features derived from the monitored signals. The task dependency of fatigue development and its impact on subjects' physiological and motion signals further contributes to that variability.
Together, the findings of this review reveal as much about the complexity involved in fatigue monitoring using wearable sensors as about the lack of standardization in this field of research. To ensure generalization to real-world settings, proposed approaches must be developed based on data acquired under realistic conditions. At the same time, models construction demands more controlled conditions. In addition, fatigue development is a dynamic process and its impact on subjects' performance depends on the task being performed. Such requirements demand research conducted in close collaboration with industry, the end user of developed technologies.
Researchers should be aware of current issues highlighted in the literature. Accordingly, future studies aiming at developing reliable wearable fatigue monitoring systems should consider the following methodological aspects:
When designing a study, care should be exercised when selecting the fatiguing tasks as well as their duration and workload. They should resemble the target application context and be well-founded on existing evidence.
The validity and reliability of the data acquisition systems should be assessed prior to recording the data for model construction. Acquired data should be pre-processed to correct recoverable disturbances and, afterwards, analyzed using a signal quality assessment algorithm to detect remaining low-quality signal segments and outliers (Naseri and Homaeinezhad, 2015). This approach allows the evaluation of the effectiveness of techniques applied to reconstruct acquired signals.
It is important to use validated reference measures of fatigue. In their review, Hu et al. (Hu and Lodewijks, 2020) advise the use of more than one reference measure of fatigue to cope with the multidimensionality of this concept. Another advantage of using several reference measures is that it allows the evaluation of the agreement between the type of fatigue induced by selected fatiguing tasks and the one of interest.
Techniques to handle data imbalances and cross-validation need to be implemented, if applicable. It allows the unbiased estimation of models' performance. Besides, the amount of data samples used for model development should be clearly reported.
The etiology of fatigue is multifactorial, and physiological and motion responses reflect the integration of various factors. Therefore, the impact of confounding factors (e.g., emotional state, health condition, or even other types of fatigue apart from the one of interest, etc.) should be considered and assessed.
The potential of wearables for fatigue monitoring has not yet been explored fully. Long-term studies, in which fatigue is monitored continuously in real-world environments are lacking. However, for such applications, preceding studies about the development of reliable models in laboratory settings and the subsequent implementation in free-living environments are needed. This enables model validation and, at the same time, provides new insights into the impact of fatigue on individuals' performance and related outcomes.
Long-term studies would also allow the investigation of fatigue dynamics. Given the intra- and inter-subject variability in fatigue responses, large amounts of data are needed to better understand the relationship between fatigue and non-invasive measures. By enabling remote, continuous monitoring, wearables play an important role in harnessing these data (Park and Jayaraman, 2017, 2021).
Limitations
To facilitate the identification of studies whose primary aim was to monitor fatigue, a limited number of search terms was selected. We are fully aware, that a more open search strategy and the inclusion of MeSH terms could have increased the number of retrieved articles. Nevertheless, we are convinced that the most relevant articles dealing with monitoring of fatigue have been detected. Moreover, included studies are of limited comparability, hindering in-depth comparison between proposed fatigue monitoring approaches.
Several criteria were defined in the scope of this review due to the lack of well-defined criteria in the existing literature. For instance, datasets were deemed imbalanced when having a samples' proportion more extreme than 60/40. Although arbitrary, those criteria were based on common sense and empirical evidence. Besides, the criterion set to characterized devices as validated or not does not consider aspects regarding devices' reliability and responsiveness. Although they are crucial for device validation, the assessment of device's validity is usually the first step of the validation process. Thus, we are aware that criteria could be further refined.
The present work provides an overview on wearable-based approaches to monitor fatigue. While summarizing proposed approaches and major findings, aspects relating to sensors location biases and physiological responses to fatigue could not be covered in this review. For instance, although wrist worn GSR sensors for fatigue monitoring, there is evidence suggesting that GSR measurements from the wrist are biased indicators of arousal (Tsiamyrtzis et al., 2016). Included studies seldom justify the placement of sensors in the body. In the same way, other factors not covered in this review may have a biasing effect on the reported findings.
Conclusion
This review has found that the generalizability of much-published research on fatigue monitoring through wearables is problematic. The lack of standardization in methods to induce, measure and model fatigue limits comparability between studies. A joint effort must be done to find consensus and set adequate standards in this research field.
Research in fatigue monitoring through wearables has been focused on the performance of developed measures, while ignoring the underlying mechanisms. Considerably more work will need to be done to design appropriate fatigue-inducing tasks, as well as to study the effect of fatigue on parameters derived from physiological/motion signals measured non-invasively.
Ensuring the acquisition of high-fidelity data, by using validated data acquisition systems and implementing signal quality assessment strategies, should be a priority. Ultimately, no accurate and interpretable fatigue measure can be developed based on data not representing the concept aimed at. More research is also required to construct measures considering the temporal dynamics of fatigue.
Lastly, long-term studies are lacking, which indicates that wearables have not been used to their full potential in fatigue research area. Wearables enable continuous, long-term monitoring in an unobtrusive manner. The development of reliable wearable fatigue monitoring systems and their implementation in real-world settings creates a unique opportunity to better understand fatigue and its impact on subjects' performance.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
NA, SA, CS, and RR contributed to conception of the manuscript. NA performed the systematic search and data extraction. NA and SA assessed articles for eligibility and made the risk of bias judgments. SA, CS, and RR supervised NA's work. All authors contributed to the development of the risk of bias assessment tool, discussed the results, and contributed to the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank Dr. Daniel Onwude for his valuable comments and suggestions.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2021.790292/full#supplementary-material
References
- Aaronson L. S., Teel C. S., Cassmeyer V., Neuberger G. B., Pallikkathayil L., Pierce J., et al. (1999). Defining and measuring fatigue. Image J. Nurs. Scholarsh. 31, 45–50. 10.1111/j.1547-5069.1999.tb00420.x [DOI] [PubMed] [Google Scholar]
- Allen D. G., Lamb G. D., Westerblad H. (2008). Skeletal muscle fatigue: cellular mechanisms. Physiol. Rev. 88, 287–332. 10.1152/physrev.00015.2007 [DOI] [PubMed] [Google Scholar]
- Al-Libawy H., Al-Ataby A., Al-Nuaimy W., Al-Taee M. A. (2016). HRV-based operator fatigue analysis and classification using wearable sensors, in 2016 13th International Multi-Conference on Systems, Signals and Devices (SSD) (Leipzig: IEEE; ), 268–273. 10.1109/SSD.2016.7473750 [DOI] [Google Scholar]
- Ameli S., Naghdy F., Stirling D., Naghdy G., Aghmesheh M. (2019). Quantitative and non-invasive measurement of exercise-induced fatigue. Proc. Inst. Mech. Eng. P J. Sport. Eng. Technol. 233, 34–45. 10.1177/1754337118775548 [DOI] [Google Scholar]
- Aryal A., Ghahramani A., Becerik-Gerber B. (2017). Monitoring fatigue in construction workers using physiological measurements. Autom. Constr. 82, 154–165. 10.1016/j.autcon.2017.03.003 [DOI] [Google Scholar]
- Balkin T. J., Horrey W. J., Graeber R. C., Czeisler C. A., Dinges D. F. (2011). The challenges and opportunities of technological approaches to fatigue management. Accid. Anal. Prev. 43, 565–572. 10.1016/j.aap.2009.12.006 [DOI] [PubMed] [Google Scholar]
- Bendak S., Rashid H. S. J. (2020). Fatigue in aviation: a systematic review of the literature. Int. J. Ind. Ergon. 76, 102928. 10.1016/j.ergon.2020.10292829615937 [DOI] [Google Scholar]
- Boon-Leng L., Dae-Seok L., Boon-Giin L. (2015). Mobile-based wearable-type of driver fatigue detection by GSR and EMG, in TENCON 2015 - 2015 IEEE Region 10 Conference (Macao: IEEE; ), 1–4. 10.1109/TENCON.2015.7372932 [DOI] [Google Scholar]
- Borragán G., Slama H., Bartolomei M., Peigneux P. (2017). Cognitive fatigue: a time-based Resource-sharing account. Cortex 89, 71–84. 10.1016/j.cortex.2017.01.023 [DOI] [PubMed] [Google Scholar]
- Boudreaux B. D., Hebert E. P., Hollander D. B., Williams B. M., Cormier C. L., Naquin M. R., et al. (2018). Validity of wearable activity monitors during cycling and resistance exercise. Med. Sci. Sports Exerc. 50, 624–633. 10.1249/MSS.0000000000001471 [DOI] [PubMed] [Google Scholar]
- Buckley C., O'Reilly M. A., Whelan D., Farrell A. V., Clark L., Longo V., et al. (2017). Binary classification of running fatigue using a single inertial measurement unit, in 2017 IEEE 14th International Conference on Wearable and Implantable Body Sensor Networks (BSN) (Eindhoven: IEEE; ), 197–201. 10.1109/BSN.2017.7936040 [DOI] [Google Scholar]
- Byrom B., Watson C., Doll H., Coons S. J. S. J., Eremenco S., Ballinger R., et al. (2018). Selection of and evidentiary considerations for wearable devices and their measurements for use in regulatory decision making: recommendations from the ePRO consortium. Value Heal. 21, 631–639. 10.1016/j.jval.2017.09.012 [DOI] [PubMed] [Google Scholar]
- Caldwell J. A. (2005). Fatigue in aviation. Travel Med. Infect. Dis. 3, 85–96. 10.1016/j.tmaid.2004.07.008 [DOI] [PubMed] [Google Scholar]
- Casillas J. M., Damak S., Chauvet-Gelinier J. C., Deley G., Ornetti P. (2006). Fatigue in patients with cardiovascular disease. Ann. Réadapt. Méd. Phys. 49, 392–402. 10.1016/j.annrmp.2006.04.003 [DOI] [PubMed] [Google Scholar]
- Cavuoto L., Megahed F. (2016). Understanding fatigue and the implications for worker safety, in ASSE Professional Development Conference and Exposition 2016 (Atlanta, GA: American Society of Safety Engineers; ) 16–19. [Google Scholar]
- Chandler J. F., Arnold R. D., Phillips J. B., Turnmire A. E. (2013). Predicting individual differences in response to sleep loss: application of current techniques. Aviat. Space Environ. Med. 84, 927–937. 10.3357/ASEM.3581.2013 [DOI] [PubMed] [Google Scholar]
- Chen J., Lin Z., Guo X. (2018). Developing construction workers' mental vigilance indicators through wavelet packet decomposition on EEG signals, in Construction Research Congress 2018 (Reston, VA: American Society of Civil Engineers; ), 51–61. 10.1061/9780784481288.006 [DOI] [Google Scholar]
- Cheon S.-P., Kang S.-J. (2017). Sensor-based driver condition recognition using support vector machine for the detection of driver drowsiness, in 2017 IEEE Intelligent Vehicles Symposium (IV) (Redondo Beach, CA: IEEE; ), 1517–1522. 10.1109/IVS.2017.7995924 [DOI] [Google Scholar]
- Choi M., Koo G., Seo M., Kim S. W. (2018). Wearable device-based system to monitor a driver's stress, fatigue, and drowsiness. IEEE Trans. Instrum. Meas. 67, 634–645. 10.1109/TIM.2017.277932927295638 [DOI] [Google Scholar]
- Choksatchawathi T., Ponglertnapakorn P., Ditthapron A., Leelaarporn P., Wisutthisen T., Piriyajitakonkij M., et al. (2020). Improving heart rate estimation on consumer grade Wrist-Worn device using post-calibration approach. IEEE Sens. J. 20, 7433–7446. 10.1109/JSEN.2020.297919127295638 [DOI] [Google Scholar]
- Cortes Rivera M., Mastronardi C., Silva-Aldana C., Arcos-Burgos M., Lidbury B. (2019). Myalgic encephalomyelitis/chronic fatigue syndrome: a comprehensive review. Diagnostics 9, 91. 10.3390/diagnostics9030091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dababneh L., Sharaf A. M., El-Gindy M. (2016). Real-time non-intrusive monitoring and prediction of driver distraction. Int. J. Veh. Syst. Model. Test. 11, 193–216. 10.1504/IJVSMT.2016.080865 [DOI] [Google Scholar]
- Davidović J., Pešić D., Antić B. (2018). Professional drivers' fatigue as a problem of the modern era. Transp. Res. F Traffic Psychol. Behav. 55, 199–209. 10.1016/j.trf.2018.03.010 [DOI] [Google Scholar]
- Dawson D., Ian Noy Y., Härmä M., Kerstedt T., Belenky G. (2011). Modelling fatigue and the use of fatigue models in work settings. Accid. Anal. Prev. 43, 549–564. 10.1016/j.aap.2009.12.030 [DOI] [PubMed] [Google Scholar]
- Dawson D., Searle A. K., Paterson J. L. (2014). Look before you (s)leep: evaluating the use of fatigue detection technologies within a fatigue risk management system for the road transport industry. Sleep Med. Rev. 18, 141–152. 10.1016/j.smrv.2013.03.003 [DOI] [PubMed] [Google Scholar]
- Dembe A. E. (2005). The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup. Environ. Med. 62, 588–597. 10.1136/oem.2004.016667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmond P. A., Hancock P. A. (2001). Active and passive fatigue states, in Stress, Workload, and Fatigue, eds Desmond P. A., Hancock P. A. (Mahwah, NJ: Lawrence Erlbaum Associates Publishers; ), 455–465. 10.1201/b12791-3.1 [DOI] [Google Scholar]
- Dhole S. R., Kashyap A., Dangwal A. N., Mohan R. (2019). A novel helmet design and implementation for drowsiness and fall detection of workers on-site using EEG and Random-Forest Classifier. Proc. Comput. Sci. 151, 947–952. 10.1016/j.procs.2019.04.132 [DOI] [Google Scholar]
- European Commission (2018). Fatigue. Available online at: https://ec.europa.eu/transport/road_safety/sites/default/files/pdf/ersosynthesis2018-fatigue.pdf (accessed March 30, 2021).
- Folkard S. (2003). Shift work, safety and productivity. Occup. Med. 53, 95–101. 10.1093/occmed/kqg047 [DOI] [PubMed] [Google Scholar]
- Foong R., Ang K. K., Zhang Z., Quek C. (2019). An iterative cross-subject negative-unlabeled learning algorithm for quantifying passive fatigue. J. Neural Eng. 16, 056013. 10.1088/1741-2552/ab255d [DOI] [PubMed] [Google Scholar]
- Fu R., Wang H., Zhao W. (2016). Dynamic driver fatigue detection using hidden Markov model in real driving condition. Expert Syst. Appl. 63, 397–411. 10.1016/j.eswa.2016.06.042 [DOI] [Google Scholar]
- Gawron V. J. (2016). Overview of self-reported measures of fatigue. Int. J. Aviat. Psychol. 26, 120–131. 10.1080/10508414.2017.1329627 [DOI] [Google Scholar]
- Gielen J., Aerts J.-M. (2019). Feature Extraction and Evaluation for Driver Drowsiness Detection Based on Thermoregulation. Appl. Sci. 9, 3555. 10.3390/app9173555 [DOI] [Google Scholar]
- Ha U., Yoo H.-J. (2016). A multimodal drowsiness monitoring ear-module system with closed-loop real-time alarm, in 2016 IEEE Biomedical Circuits and Systems Conference (BioCAS) (Shanghai: IEEE; ), 536–539. 10.1109/BioCAS.2016.7833850 [DOI] [Google Scholar]
- Harris M., Glozier N., Ratnavadivel R., Grunstein R. R. (2009). Obstructive sleep apnea and depression. Sleep Med. Rev. 13, 437–444. 10.1016/j.smrv.2009.04.001 [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Altman D. G., Gotzsche P. C., Juni P., Moher D., Oxman A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928–d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honn K. A., Riedy S. M., Grant D. A. (2015). Validation of a portable, touch-screen psychomotor vigilance test. Aerosp. Med. Hum. Perform. 86, 428–434. 10.3357/AMHP.4165.2015 [DOI] [PubMed] [Google Scholar]
- Hu S., Zheng G., Peters B. (2013). Driver fatigue detection from electroencephalogram spectrum after electrooculography artefact removal. IET Intell. Transp. Syst. 7, 105–113. 10.1049/iet-its.2012.0045 [DOI] [Google Scholar]
- Hu X., Lodewijks G. (2020). Detecting fatigue in car drivers and aircraft pilots by using non-invasive measures: the value of differentiation of sleepiness and mental fatigue. J. Safety Res. 72, 173–187. 10.1016/j.jsr.2019.12.015 [DOI] [PubMed] [Google Scholar]
- Huang S., Li J., Zhang P., Zhang W. (2018). Detection of mental fatigue state with wearable ECG devices. Int. J. Med. Inform. 119, 39–46. 10.1016/j.ijmedinf.2018.08.010 [DOI] [PubMed] [Google Scholar]
- Hursh S. R., Redmond D. P., Johnson M. L., Thorne D. R., Belenky G., Balkin T. J., et al. (2004). Fatigue models for applied research in warfighting. Aviat. Sp. Environ. Med. 75(3 Suppl):A44–53; discussion A54–60. [PubMed] [Google Scholar]
- International Civil Aviation Organization (2012). Fatigue Risk Management Systems Manual for Regulators. Available online at: www.icao.int (accessed July 14, 2021).
- Kartsch V., Benatti S., Guermandi M., Montagna F., Benini L. (2019). Ultra low-power drowsiness detection system with BioWolf, in 2019 9th International IEEE/EMBS Conference on Neural Engineering (NER) (San Francisco, CA: IEEE; ), 1187–1190. 10.1109/NER.2019.8717070 [DOI] [Google Scholar]
- Karvekar S., Abdollahi M., Rashedi E. (2019). A data-driven model to identify fatigue level based on the motion data from a smartphone, in 2019 IEEE Western New York Image and Signal Processing Workshop (WNYISPW) (Rochester, NY: IEEE; ), 1–5. 10.1109/WNYIPW.2019.8923100 [DOI] [Google Scholar]
- Khan T., Lundgren L. E., Järpe E., Olsson M. C., Viberg P. (2019). A novel method for classification of running fatigue using change-point segmentation. Sensors (Switzerland) 19, 4729. 10.3390/s19214729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Shin M. (2019). Utilizing HRV-derived respiration measures for driver drowsiness detection. Electronics 8, 669. 10.3390/electronics8060669 [DOI] [Google Scholar]
- Ko L.-W., Komarov O., Lai W.-K., Liang W.-G., Jung T.-P. (2020). Eyeblink recognition improves fatigue prediction from single-channel forehead EEG in a realistic sustained attention task. J. Neural Eng. 17, 036015. 10.1088/1741-2552/ab909f [DOI] [PubMed] [Google Scholar]
- Ko L.-W., Lai W.-K., Liang W.-G., Chuang C.-H., Lu S.-W., Lu Y.-C., et al. (2015). Single channel wireless EEG device for real-time fatigue level detection, in 2015 International Joint Conference on Neural Networks (IJCNN) (Killarney: IEEE; ), 1–5. 10.1109/IJCNN.2015.7280817 [DOI] [Google Scholar]
- Kotsiantis S., Kanellopoulos D., Pintelas P. (2006). Handling imbalanced datasets: a review. GESTS Int. Trans. Comput. Sci. Eng. 30, 25–36. [Google Scholar]
- Kundinger T., Riener A. (2020). The potential of wrist-worn wearables for driver drowsiness detection: a feasibility analysis, in Proceedings of the 28th ACM Conference on User Modeling, Adaptation and Personalization (New York, NY: ACM; ), 117–125. 10.1145/3340631.3394852 [DOI] [Google Scholar]
- Kundinger T., Sofra N., Riener A. (2020a). Assessment of the potential of wrist-worn wearable sensors for driver drowsiness detection. Sensors 20, 1029. 10.3390/s20041029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kundinger T., Yalavarthi P. K., Riener A., Wintersberger P., Schartmüller C. (2020b). Feasibility of smart wearables for driver drowsiness detection and its potential among different age groups. Int. J. Pervasive Comput. Commun. 16, 1–23. 10.1108/IJPCC-03-2019-0017 [DOI] [Google Scholar]
- Lamti H. A., Ben Khelifa M. M., Hugel V. (2019). Mental fatigue level detection based on event related and visual evoked potentials features fusion in virtual indoor environment. Cogn. Neurodyn. 13, 271–285. 10.1007/s11571-019-09523-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee B.-G., Lee B.-L., Chung W.-Y. (2015). Smartwatch-based driver alertness monitoring with wearable motion and physiological sensor, in 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) (Milan: IEEE; ), 6126–6129. 10.1109/EMBC.2015.7319790 [DOI] [PubMed] [Google Scholar]
- Lee B.-L., Lee B.-G., Chung W.-Y. (2016). Standalone wearable driver drowsiness detection system in a smartwatch. IEEE Sens. J. 16, 5444–5451. 10.1109/JSEN.2016.256666727295638 [DOI] [Google Scholar]
- Lee H., Lee J., Shin M. (2019a). Using wearable ECG/PPG sensors for driver drowsiness detection based on distinguishable pattern of recurrence plots. Electronics 8, 192. 10.3390/electronics8020192 [DOI] [Google Scholar]
- Lee J.-S. S., Bae Y.-S. S., Lee W., Lee H., Yu J., Choi J.-P. P. (2019b). Emotion and fatigue monitoring using wearable devices, in Lecture Notes in Electrical Engineering Lecture Notes in Electrical Engineering, eds Hwang S. O., Tan S. Y., Bien F. (Singapore: Springer Singapore; ), 91–96. 10.1007/978-981-13-0311-1_17 [DOI] [Google Scholar]
- Lemkaddem A., Delgado-Gonzalo R., Turetken E., Dasen S., Moser V., Gressum C., et al. (2018). Multi-modal driver drowsiness detection: a feasibility study, in 2018 IEEE EMBS International Conference on Biomedical and Health Informatics (BHI) (Las Vegas, NV: IEEE; ), 9–12. 10.1109/BHI.2018.8333357 [DOI] [Google Scholar]
- Leng L. B., Lee B. G., Chung W.-Y. (2015). Wearable driver drowsiness detection system based on biomedical and motion sensors, in 2015 IEEE SENSORS (Busan: IEEE; ), 1–4. 10.1109/ICSENS.2015.7370355 [DOI] [Google Scholar]
- Li G., Chung W.-Y. (2015). a context-aware EEG headset system for early detection of driver drowsiness. Sensors 15, 20873–20893. 10.3390/s150820873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Chung W.-Y. (2018). Combined EEG-gyroscope-tDCS brain machine interface system for early management of driver drowsiness. IEEE Trans. Hum. Mach. Syst. 48, 50–62. 10.1109/THMS.2017.275980827295638 [DOI] [Google Scholar]
- Li G., Lee B.-L., Chung W.-Y. (2015). Smartwatch-based wearable EEG system for driver drowsiness detection. IEEE Sens. J. 15, 7169–7180. 10.1109/JSEN.2015.247367927295638 [DOI] [Google Scholar]
- Li J., Li H., Umer W., Wang H., Xing X., Zhao S., et al. (2020). Identification and classification of construction equipment operators' mental fatigue using wearable eye-tracking technology. Autom. Constr. 109, 103000. 10.1016/j.autcon.2019.103000 [DOI] [Google Scholar]
- Li W., Hu X., Gravina R., Fortino G. (2017). A neuro-fuzzy fatigue-tracking and classification system for wheelchair users. IEEE Access 5, 19420–19431. 10.1109/ACCESS.2017.273092027295638 [DOI] [Google Scholar]
- Li Y., Yamamoto T., Zhang G. (2018). Understanding factors associated with misclassification of fatigue-related accidents in police record. J. Safety Res. 64, 155–162. 10.1016/j.jsr.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P. A., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 62, e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- Luque A., Carrasco A., Martín A., de las Heras A. (2019). The impact of class imbalance in classification performance metrics based on the binary confusion matrix. Pattern Recognit. 91, 216–231. 10.1016/j.patcog.2019.02.023 [DOI] [Google Scholar]
- Mehreen A., Anwar S. M., Haseeb M., Majid M., Ullah M. O. (2019). A hybrid scheme for drowsiness detection using wearable sensors. IEEE Sens. J. 19, 5119–5126. 10.1109/JSEN.2019.290422227295638 [DOI] [Google Scholar]
- Mihajlovic V., Grundlehner B., Vullers R., Penders J. (2015). Wearable, wireless EEG solutions in daily life applications: what are we missing? IEEE J. Biomed. Heal. Informatics 19, 6–21. 10.1109/JBHI.2014.2328317 [DOI] [PubMed] [Google Scholar]
- Mohanavelu K., Lamshe R., Poonguzhali S., Adalarasu K., Jagannath M. (2017). Assessment of human fatigue during physical performance using physiological signals: a review. Biomed. Pharmacol. J. 10, 1887–1896. 10.13005/bpj/1308 [DOI] [Google Scholar]
- Mokaya F., Lucas R., Noh H. Y., Zhang P. (2016). Burnout: a wearable system for unobtrusive skeletal muscle fatigue estimation, in 2016 15th ACM/IEEE International Conference on Information Processing in Sensor Networks (IPSN) (Vienna: IEEE; ), 1–12. 10.1109/IPSN.2016.7460661 [DOI] [Google Scholar]
- Motta C., Palermo E., Studer V., Germanotta M., Germani G., Centonze D., et al. (2016). Disability and fatigue can be objectively measured in multiple sclerosis. PLoS ONE 11, e0148997. 10.1371/journal.pone.0148997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura T., Alqurashi Y. D., Morrell M. J., Mandic D. P. (2018). Automatic detection of drowsiness using in-ear EEG, in 2018 International Joint Conference on Neural Networks (IJCNN) (Rio: IEEE; ), 1–6. 10.1109/IJCNN.2018.8489723 [DOI] [Google Scholar]
- Naseri H., Homaeinezhad M. R. (2015). Electrocardiogram signal quality assessment using an artificially reconstructed target lead. Comput. Methods Biomech. Biomed. Eng. 18, 1126–1141. 10.1080/10255842.2013.875163 [DOI] [PubMed] [Google Scholar]
- Nasirzadeh F., Mir M., Hussain S., Tayarani Darbandy M., Khosravi A., Nahavandi S., et al. (2020). Physical fatigue detection using entropy analysis of heart rate signals. Sustainability 12, 2714. 10.3390/su12072714 [DOI] [Google Scholar]
- Nassif D. V., Pereira J. S. (2018). Fatigue in Parkinson's disease: concepts and clinical approach. Psychogeriatrics 18, 143–150. 10.1111/psyg.12302 [DOI] [PubMed] [Google Scholar]
- Niwa S., Yuki M., Noro T., Shioya S., Inoue K. (2016). A wearable device for traffic safety - a study on estimating drowsiness with eyewear, JINS MEME, in SAE Technical Paper 2016-01-0118. SAE 2016 World Congress and Exhibition (Detroit, MI: ). 10.4271/2016-01-0118 [DOI] [Google Scholar]
- Nourhan T. M., Piechnick M., Falkenberg J., Nazmy T. (2017). Detection of muscle fatigue using wearable (MYO) surface electromyography based control device, in 2017 8th International Conference on Information Technology (ICIT) (Amman: IEEE; ), 44–49. 10.1109/ICITECH.2017.8079913 [DOI] [Google Scholar]
- Ogino M., Mitsukura Y. (2018). Portable drowsiness detection through use of a prefrontal single-channel electroencephalogram. Sensors 18, 4477. 10.3390/s18124477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Higgins C. M., Brady B., O'Connor B., Walsh D., Reilly R. B. (2018). The pathophysiology of cancer-related fatigue: current controversies. Support. Care Cancer 26, 3353–3364. 10.1007/s00520-018-4318-7 [DOI] [PubMed] [Google Scholar]
- Oken B. S., Salinsky M. C., Elsas S. M. (2006). Vigilance, alertness, or sustained attention: physiological basis and measurement. Clin. Neurophysiol. 117, 1885–1901. 10.1016/j.clinph.2006.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papakostas M., Kanal V., Abujelala M., Tsiakas K., Makedon F. (2019). Physical fatigue detection through EMG wearables and subjective user reports - a machine learning approach towards adaptive rehabilitation, in Proceedings of the 12th ACM International Conference on PErvasive Technologies Related to Assistive Environments (New York, NY: ACM; ), 475–481. 10.1145/3316782.3322772 [DOI] [Google Scholar]
- Park S., Jayaraman S. (2017). The wearables revolution and Big Data: the textile lineage. J. Text. Inst. 108, 605–614. 10.1080/00405000.2016.1176632 [DOI] [Google Scholar]
- Park S., Jayaraman S. (2021). Wearables: fundamentals, advancements, and a roadmap for the future, in Wearable Sensors, ed Sazonov E. (London; Cambridge, MA; San Diego, CA; Oxford: Academic Press; ), 3–27. 10.1016/B978-0-12-819246-7.00001-2 [DOI] [Google Scholar]
- Richter S., Marsalek K., Glatz C., Gundel A. (2005). Task-dependent differences in subjective fatigue scores. J. Sleep Res. 14, 393–400. 10.1111/j.1365-2869.2005.00473.x [DOI] [PubMed] [Google Scholar]
- Rohit F., Kulathumani V., Kavi R., Elwarfalli I., Kecojevic V., Nimbarte A. (2017). Real-time drowsiness detection using wearable, lightweight brain sensing headbands. IET Intell. Transp. Syst. 11, 255–263. 10.1049/iet-its.2016.0183 [DOI] [Google Scholar]
- Rudroff T., Kindred J. H., Ketelhut N. B. (2016). Fatigue in multiple sclerosis: misconceptions and future research directions. Front. Neurol. 7, 122. 10.3389/fneur.2016.00122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahayadhas A., Sundaraj K., Murugappan M. (2012). Detecting driver drowsiness based on sensors: a review. Sensors 12, 16937–16953. 10.3390/s121216937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samima S., Sarma M., Samanta D., Prasad G. (2019). Estimation and quantification of vigilance using ERPs and eye blink rate with a fuzzy model-based approach. Cogn. Technol. Work 21, 517–533. 10.1007/s10111-018-0533-8 [DOI] [Google Scholar]
- Sampei K., Ogawa M., Torres C., Sato M., Miki N. (2016). Mental fatigue monitoring using a wearable transparent eye detection system. Micromachines 7, 20. 10.3390/mi7020020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedighi Maman Z., Alamdar Yazdi M. A., Cavuoto L. A., Megahed F. M. (2017). A data-driven approach to modeling physical fatigue in the workplace using wearable sensors. Appl. Ergon. 65, 515–529. 10.1016/j.apergo.2017.02.001 [DOI] [PubMed] [Google Scholar]
- Sedighi Maman Z., Chen Y.-J., Baghdadi A., Lombardo S., Cavuoto L. A., Megahed F. M. (2020). A data analytic framework for physical fatigue management using wearable sensors. Expert Syst. Appl. 155, 113405. 10.1016/j.eswa.2020.11340534640722 [DOI] [Google Scholar]
- Shahid A., Shen J., Shapiro C. M. (2010). Measurements of sleepiness and fatigue. J. Psychosom. Res. 69, 81–89. 10.1016/j.jpsychores.2010.04.001 [DOI] [PubMed] [Google Scholar]
- Shirmohammadi S., Barbe K., Grimaldi D., Rapuano S., Grassini S. (2016). Instrumentation and measurement in medical, biomedical, and healthcare systems. IEEE Instrum. Meas. Mag. 19, 6–12. 10.1109/MIM.2016.757906327295638 [DOI] [Google Scholar]
- Sikander G., Anwar S. (2019). Driver fatigue detection systems: a review. IEEE Trans. Intell. Transp. Syst. 20, 2339–2352. 10.1109/TITS.2018.286849927295638 [DOI] [Google Scholar]
- Sun D., Huang Y., Zhao M., Chen D., Han W. (2020). Recognition of fatigue driving based on steering operation using wearable smart watch, in Green, Smart and Connected Transportation Systems. Lecture Notes in Electrical Engineering, eds Wang W., Baumann M., Jiang X. (Singapore: Springer; ), 235–248. 10.1007/978-981-15-0644-4_18 [DOI] [Google Scholar]
- Tanaka M., Tajima S., Mizuno K., Ishii A., Konishi Y., Miike T., et al. (2015). Frontier studies on fatigue, autonomic nerve dysfunction, and sleep-rhythm disorder. J. Physiol. Sci. 65, 483–498. 10.1007/s12576-015-0399-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Techera U., Hallowell M., Littlejohn R., Rajendran S. (2018). Measuring and predicting fatigue in construction: empirical field study. J. Constr. Eng. Manag. 144, 1–9. 10.1061/(ASCE)CO.1943-7862.0001513 [DOI] [Google Scholar]
- Torres D. A., Josand N. A., Eacute N. A., Adand N. A., Aacute N. A., Hernand N., et al. (2020). Detection of fatigue on gait using accelerometer data and supervised machine learning. Int. J. Grid Util. Comput. 11, 474. 10.1504/IJGUC.2020.108475 [DOI] [Google Scholar]
- Tsao L., Ma L., Papp C.-T. (2019). Using non-invasive wearable sensors to estimate perceived fatigue level in manual material handling tasks, in Advances in Intelligent Systems and Computing, ed Ahram T. Z. (Cham: Springer International Publishing; ), 65–74. 10.1007/978-3-319-94619-1_7 [DOI] [Google Scholar]
- Tsiamyrtzis P., Dcosta M., Shastri D., Prasad E., Pavlidis I. (2016). Delineating the operational envelope of mobile and conventional EDA sensing on key body locations, in Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (New York, NY: ACM; ), 5665–5674. 10.1145/2858036.2858536 [DOI] [Google Scholar]
- Wallisch P., Lusignan M., Benayoun M., Baker T. I., Dickey A. S., Hatsopoulos N. G. (2009). Markov models, in Matlab for Neuroscientists, eds Wallisch P., Lusignan M., Benayoun M., Baker T. I., Dickey A. S., Hatsopoulos N. G. (Elsevier; ), 283–290. 10.1016/B978-0-12-374551-4.00025-7 [DOI] [Google Scholar]
- Wan J., Qin Z., Wang P., Sun Y., Liu X. (2017). Muscle fatigue: general understanding and treatment. Exp. Mol. Med. 49, e384. 10.1038/emm.2017.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Li H., Chen J. (2019). Detecting and measuring construction workers' vigilance through hybrid kinematic-EEG signals. Autom. Constr. 100, 11–23. 10.1016/j.autcon.2018.12.018 [DOI] [Google Scholar]
- Wang L., Huang Z., Hao S., Cheng Y., Yang Y. (2018). A heterogeneous ensemble learning voting method for fatigue detection in daily activities. J. Adv. Comput. Intell. Intell. Informatics 22, 88–96. 10.20965/jaciii.2018.p0088 [DOI] [Google Scholar]
- Wen Sun, Zhao, Chen (2019). Recognition of fatigue driving based on frequency features of wearable device data, in 2019 3rd International Symposium on Autonomous Systems (ISAS) (Shanghai: IEEE; ), 171–176. 10.1109/ISASS.2019.8757779 [DOI] [Google Scholar]
- Williamson A., Lombardi D. A., Folkard S., Stutts J., Courtney T. K., Connor J. L. (2011). The link between fatigue and safety. Accid. Anal. Prev. 43, 498–515. 10.1016/j.aap.2009.11.011 [DOI] [PubMed] [Google Scholar]
- Yung M. (2016). Fatigue at the Workplace : Measurement and Temporal Development. Thesis, UWSpace. [Google Scholar]
- Yung M., Wells R. P. (2017). Documenting the temporal pattern of fatigue development. IISE Trans. Occup. Ergon. Hum. Factors 5, 115–135. 10.1080/24725838.2017.1373714 [DOI] [Google Scholar]
- Zeng Z., Huang Z., Leng K., Han W., Niu H., Yu Y., et al. (2020). Nonintrusive monitoring of mental fatigue status using epidermal electronic systems and machine-learning algorithms. ACS Sensors 5, 1305–1313. 10.1021/acssensors.9b02451 [DOI] [PubMed] [Google Scholar]
- Zhang L., Diraneyya M. M., Ryu J., Haas C., Abdel-Rahman E. (2019b). Automated monitoring of physical fatigue using jerk, in Proceedings of the 36th International Symposium on Automation and Robotics in Construction, ISARC 2019 (Banff, AB: ), 989–997. 10.22260/ISARC2019/0132 [DOI] [Google Scholar]
- Zhang L., Diraneyya M. M., Ryu J., Haas C. T., Abdel-Rahman E. M. (2019a). Jerk as an indicator of physical exertion and fatigue. Autom. Constr. 104, 120–128. 10.1016/j.autcon.2019.04.016 [DOI] [Google Scholar]
- Zhang M., Zhai X., Zhao G., Chong T., Wang Z. (2018). An application of particle swarm algorithms to optimize Hidden Markov Models for driver fatigue identification*, in 2018 IEEE Intelligent Vehicles Symposium (IV) (Changshu: IEEE; ), 25–30. 10.1109/IVS.2018.8500357 [DOI] [Google Scholar]
- Zhang S., He H., Wang Z., Gao M., Mao J. (2018). Low-power listen based driver drowsiness detection system using smartwatch, in Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) (Springer International Publishing; ) 453–464. 10.1007/978-3-030-00018-9_40 [DOI] [Google Scholar]
- Zhang X., Li J., Liu Y., Zhang Z., Wang Z., Luo D., et al. (2017). Design of a fatigue detection system for high-speed trains based on driver vigilance using a wireless wearable EEG. Sensors 17, 486. 10.3390/s17030486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Chen Y., Pan Z. (2018). A deep temporal model for mental fatigue detection, in 2018 IEEE International Conference on Systems, Man, and Cybernetics (SMC) (Miyazaki: IEEE; ), 1879–1884. 10.1109/SMC.2018.00325 [DOI] [Google Scholar]
- Zhou X., Yao D., Zhu M., Zhang X., Qi L., Pan H., et al. (2018). Vigilance detection method for high-speed rail using wireless wearable EEG collection technology based on low-rank matrix decomposition. IET Intell. Transp. Syst. 12, 819–825. 10.1049/iet-its.2017.0239 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.