Abstract
The exposure to Brucella species is an occupational hazard for veterinary personnel in India. In our previous study, paraveterinarians and animal handlers were found to be at higher risk of being seropositive. In the present study, we further investigate comparative exposure risk to brucellosis amongst the veterinary professionals, identify risk factors, and evaluate the perceptions and practices towards using adequate personal protective equipment (PPE) while attending high risk veterinary interventions. A cross-sectional study was conducted amongst veterinary personnel in the Punjab state of India. Logistic and negative binomial regression models were constructed to interpret the influence of categorical and numerical variables on prevalence of brucellosis and the adequacy of PPE use, respectively. Compared to veterinarians, animal handlers were less likely to consider veterinary practice in sheep and goats (odds ratio [OR] 0.3; 95% confidence interval [CI]: 0.2–0.7) or assisting in obstetric interventions (OR 0.3, 95% CI 0.1–0.8) as potential exposures. They were less aware of the signs and symptoms of the disease in humans (OR 0.05, 95% CI 0.02–0.14) and of the availability of vaccines for cattle (OR 0.07, 95% CI 0.01–0.3) than the veterinarians, and were least likely of the three groups to recommend vaccination of cattle against brucellosis to animal owners (OR 0.1, 95% CI 0.02–0.3). Compared to veterinarians, they were also less likely to consider zoonotic risk (OR 0.4, 95% CI 0.2–0.8) or better efficiency (OR 0.1, 95% CI 0.05–0.4) as enablers of PPE use during veterinary procedures. Of the three occupational groups, animal handlers were also less likely to use adequate PPE during high-risk veterinary exposures, although they were found to have handled the highest number of cases of abortion. The average use of adequate PPE during high-risk interventions in one month preceding this study was lowest for animal handlers. Veterinary personnel with a higher rate of PPE use during high-risk veterinary interventions were likely to obtain information on brucellosis from government sources (p = 0.06) and felt that PPE use enhanced their professional efficiency (Incidence rate ratio [IRR] 3.3, 95% CI 1.5–8.1) compared to those who were less likely to use adequate PPE. We recommend concerted efforts to increase awareness amongst veterinary personnel, particularly amongst animal handlers, regarding brucellosis and the importance of biosecurity measures in veterinary practice. Designing training courses on the importance of PPE use along with formulation of biosecurity guidelines at local levels could help reduce the prevalence of the disease in veterinary personnel.
Keywords: Brucellosis, India, Occupational exposure, Veterinarians, Para-veterinarians, Animal handlers, PPE
1. Introduction
Brucellosis is one of the seven most neglected diseases in the world with the true incidence of the disease estimated to be 5,000,000 to 12,500,000 cases annually [1]. Except for few high-income countries, the disease is prevalent worldwide, but remains widely underreported in the low-income countries where it is responsible for substantial health, economic and livelihood burdens [2]. In India,brucellosis not only affects livestock populations but is also an important occupational hazard for humans associated with livestock-related activities [[3], [4], [5], [6]]. The economic burden of the disease in the country is reported to cause a median loss of US$ 3.43 billion in the livestock population, of which more than 95% is attributed to the bovine industry [7]. Singh, Khatkar, Aulakh, Gill and Dhand [8] estimated the annual impact of human brucellosis to be US $ 10.46 million and 177,601 disability-adjusted life-years (DALYs; 95% CI 152 695–214 764) at the rate of 0.15 (95% CI: 0.13–0.17) DALYs per thousand persons per year in India.
The enormous size of the dairy sector in India and its accelerated growth demands an efficient veterinary coverage including but not limited to animal health advice, artificial insemination, injuries, pregnancy diagnosis, abortion handling, calving assistance, retention of placenta and vaccinations against infectious diseases [9,10]. The veterinary services fall under the administrative control of state governments and most states have three types of animal health service providers namely, (a) qualified registered veterinarians, (b) para-veterinarians, and (c) animal handlers [9]. Para-veterinarians perform a role similar to veterinary nurses and are usually called veterinary pharmacists in India, but we refer to them as para-veterinarians in this manuscript for the international audience. The para-veterinarians typically undergo training for one or two years to obtain a diploma butanimal handlers do not require any formal training. Their main job is to assist veterinarians and para-veterinarians, but with experience, most perform some routine tasks.
The veterinary professionals are vulnerable to contract brucellosis due to their constant exposure to infected animals. High seroprevalence of Brucella antibodies has been reported from veterinarians and para-veterinarians [11,12]. The usual clinical symptoms include undulant fever, joint pain, night sweats and weakness but the disease can persist and progress to a chronically incapacitating stage with severe complications [13]. Repeated contact with infected livestock places these occupations in the high-risk category for Brucella infection [14,15].
A disparity in the infection status within veterinary personnel was demonstrated in our previous investigation, where animal handlers were found to be at a greater risk of brucellosis infection than veterinarians and para-veterinarians [6]. The finding is reinforced by the studies conducted elsewhere in India reporting prevalence of Brucella infection in veterinary practitioners and their inadequate adherence to biosecurity measures in veterinary practice [11,16,17]. However, we suggested further investigations to clarify the association of personal protective equipment (PPE) use and brucellosis prevalence amongst the veterinary professionals, as unexpectedly, those using PPE were found more likely to be positive for brucellosis [6]. Further, despite a number of studies reporting prevalence of brucellosis in veterinary personnel, few studies have been undertaken to analyse the reasons that lead to the difference in disease prevalence amongst veterinarians, para-veterinarians and animal handlers/inseminators.
The religious and traditional practices of communities in India, meagre resources for justifiable compensation to the farmers, ban on cow slaughter, ineffective surveillance, and absence of effective treatment against brucellosis leaves vaccination of livestock as the only option to prevent and control the disease, which is also a cost-effective option [18,19]. Veterinary personnel who play a pivotal role in vaccinating livestock can be accidentally exposed to infections through needlestick injuries [6]. However, non-adherence to personal protective equipment (PPE) usage by the veterinary personnel while attending to various procedures such as retained placenta, dystocia, pregnancy diagnosis and artificial insemination appears to be the main reason for the occupational exposure in veterinarians [9]. Generating knowledge to enable better control of endemic brucellosis in livestock and the risk of occupational exposure in humans can reduce the burden of disease in both populations within a One Health framework. In brucellosis endemic settings such as India, this is likely the most efficient approach to addressing this problem, since disease control resources are scarce and benefits needs to be demonstrated in both sectors.
This study was undertaken in the all the tehsils (subdistricts) of Ludhiana district in the state of Punjab, India with an objective to (a) compare exposure of three occupational groups of the veterinary professional to brucellosis, and (b) identify differences in perception and practices regarding the use of PPE during high-risk veterinary interventions amongst the three occupational groups.
2. Methods
2.1. Study design
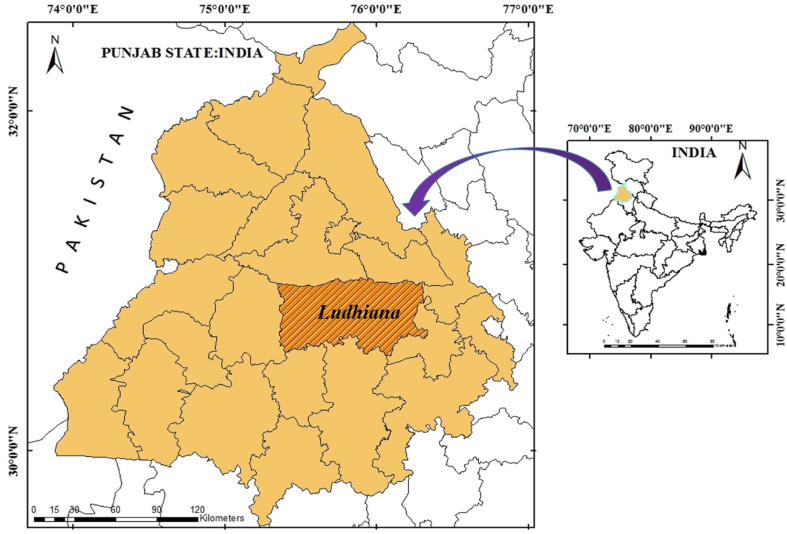
The design of this cross-sectional study has been described in detail elsewhere [6]. Briefly, a census study of government veterinary personnel working with livestock in the Ludhiana district of the Punjab state of India was conducted (Fig. 1). This state is located in the North West, bordering Pakistan. A detailed questionnaire was designed requesting information about participant demographic factors, potential risk and exposure factors for brucellosis infection in veterinary practice, and infection control perceptions and practices, including PPE use.
Fig. 1.
Study area for the comparison of brucellosis prevalence amongst the veterinary personnel in Ludhiana district of Punjab state, India.
This study was approved by the Human Ethics Committee of The University of Sydney, Australia (Approval number 2015/206). Informed consent was obtained from all individual participants included in the study. A copy of the questionnaire is available from the corresponding author upon request. The questionnaire was available both in English and Punjabi, the local language of the state.
2.2. Data handling and study variables
Data from questionnaires were entered into an Excel spreadsheet (Microsoft Office Excel 2007). Data were cleaned, examined for missing values and checks were conducted for frequency, range and logic to prepare the data for analyses. All further statistical analyses were conducted in R programming environment [20].
The study considered 43 categorical explanatory variables of the response of the three occupational groups of veterinary personnel towards the likelihood of brucellosis exposure risk, awareness of human Brucella infection and animal vaccination; enablers and barriers to PPE use during veterinary practice; concerns about contracting brucellosis during professional work; and adequacy of PPE use during high-risk procedures in the veterinary profession. The explanatory variables included (a) six demographic factors, (b) three risk factors for brucellosis infection, (c) information sources for brucellosis, (d) five variables regarding the perceived likelihood of brucellosis exposure risk concerning contact with various animal species during veterinary practice, (e) eight variables regarding the perceived likelihood of brucellosis exposure risk concerning the procedures (such as handling of body fluids and discharges) encountered during the veterinary practice [21], (f) five variables regarding knowledge on human brucellosis infection and animal vaccination, (g) four variables that enable the use of PPE during potential high-risk veterinary practice, (h) five variables that potentially restrict the use of PPE during veterinary practice, (i) three variables regarding the perceived level of concern towards contracting brucellosis and (j) three variables regarding perceived adequacy of PPE use while attending high-risk veterinary procedures. Furthermore, 11 numeric explanatory variables were considered to measure PPE use by veterinary personnel during high-risk veterinary practice situations.
The variables ‘age' and ‘experience’ were originally collected as continuous data expressed in years; however, they were converted into categorical data for logistic regression analysis. These variables were divided into equal range of years for ‘age’ and ‘experience’. The variable ‘age’ was divided into 4 groups, namely, ‘A’ (20–30 years), ‘B’ (31–40 years), ‘C’ (41–50 years) and ‘D’ (50+ years). Similarly, the variable ‘experience’ was divided into 5 groups, namely, ‘A’ (0–9 years), ‘B’ (10–18 years), ‘C’ (19–27 years), ‘D’ (28–36 years) and ‘E’ (37–45 years).
The 5-point Likert scale used to describe the level of likelihood or concern towards the exposure of brucellosis was modified into a dichotomous scale by combining the former three categories, “A little likely”,”Likely”, “Very Likely”/ “A little concerned” “Concerned”, “Very concerned” into “Likely”/”Concerned”, and the latter two categories, that is, “Not at all likely”, “Unlikely”/ “Not at all concerned”, “Not concerned” into “Unlikely”/ “Not concerned”.
The outcome variables concerning the adequacy of PPE use in three different high-risk scenarios were derived from several questions asking whether different types of PPE were used in the scenario. The scenarios were (i) PPE use when performing conception or parturition procedures (overall OR gown AND disposable gloves is adequate); (ii) PPE use when handling an aborted foetus or stillbirth (gown AND gloves AND[surgical mask OR goggles OR face shield]is adequate), and (iii) PPE use when handling a retained placenta (gown AND gloves AND [mask OR goggles]is adequate).The number of high-risk situations when adequate PPE was used was scored 0–3 for the three high risk situations.This was used as an outcome for the negative binomial model. The adequacy of PPE use was based on the 2015 ‘Compendium of veterinary standard precautions for zoonotic disease prevention in veterinary personnel’ [22].
2.3. Descriptive analyses
The distributions of categorical and numeric variables were assessed with frequency tables and box-and-whisker plots, respectively. Missing values were noted. Further, we examined contingency tables of the categorical explanatory variables and box-and-whiskerplots of the continuous explanatory variables by occupation. The contingency tables were examined for cells with low or zero values and the distributions of continuous variables were assessed for normality.
2.4. Demographic variables, risk factors and information source variability amongst the occupational groups
The comparisons amongst the three occupations of the veterinary profession for demographic variables, risk factors and sources of information on brucellosis was carried out by chi-squared test.
2.5. Comparisons of veterinary experience and work practices amongst occupational groups
The variability within the occupations of the veterinary personnel on numeric explanatory variables such as ‘experience (years in practice)’ or variables that describe the frequency of exposure to specific high-risk veterinary practices were analysed using Kruskal-Wallis test.
2.6. Regression analysis for categorical outcome variables
Univariable logistic regression analysis of the various response variables with the variable ‘occupation’ was carried out by fitting generalized linear models using the ‘binomial’ family function in ‘R’ programming environment. In addition to the ‘occupation’, each response variable was also assessed against other demographic factors, viz. age, gender, type of practice, location of practice and years of experience.The final multivariable model was adjusted for those variables that yielded a p-value of <0.25 on univariable analysis and the final odds ratios (OR) were adjusted accordingly for occupation.
2.7. Regression analysis of numeric outcome variables
The association of explanatory variables with the frequency of high-risk situations when adequate PPE was used by the veterinary personnel during veterinary clinical practice was performed by negative binomial regression analysis with a log link function. All variables were assessed for missing values and only those variables with less than 5% missing values were considered for the analyses.
Initially, univariable analyses were performed and those explanatory variables that yielded a p-value of <0.25 (based on the likelihood-ratio chi-square test) were considered for initial multivariable model building.The final multivariable negative binomial regression models were constructed by stepwise elimination of variables that yielded the highest p-values.Only those variables thatwere considered to be of statistical significance (p-value ≤ 0.05) were retained in the final model. Any collinearity between the explanatory variables in the final model was tested by estimating the generalized variation inflation factor (GVIF) using the function ‘vif’ of ‘R' package ‘car' [23]. A value of GVIF less than 5 was considered acceptable. Model adequacy was assessed using the likelihood ratio chi-square goodness of fit statistic and graphical assessment of the distribution of residuals using the R package ‘DHARMa’[24].
3. Results
3.1. Demographic variables
The frequency distributions of demographic variables in this study have been described elsewhere (Proch et al., 2018). Briefly, a total of 296 participants were administered the questionnaire, of whom 45.3% (134) were para-veterinarians, 22.6% (67) were veterinarians and 32.1% (95) were animal handlers. Most respondents were males (93.6%), belonged to the age group 31–40 years (34.8%), resided in rural areas (66.6%) and attended a mix of veterinary practice that included large and small animals (87.2%). A small proportion (4.1%) of participants reported previous needle stick injury during cattle vaccination for brucellosis or to have been potentially exposed to the disease due to consumption of raw milk (11.9%), and more than half of the respondents (56.8%) reared animals at home. The frequency distributions of demographic characteristics of the participants, brucellosis risk factors and main information source by occupation are presented in Table 1.
Table 1.
Contingency tables and Chi-square test results for cross-tabulations of demographic and brucellosis risk factors with occupation in a study of veterinary personnel in India (n = 296).
| Parameters | Categories | Total N (%) | Occupation n (%) |
χ2p value | ||
|---|---|---|---|---|---|---|
| Veterinarians | Para-veterinarians | Handlers | ||||
| Total participants | 296 (100.0) | 67 (22.6) | 134 (45.3) | 95 (32.1) | – | |
| Demographic factors | ||||||
| Tehsil (region) | A(Jagraon) | 55 (18.6) | 9 (13.4) | 24 (17.9) | 22 (23.2) | 0.50 |
| B(Khanna) | 30 (10.1) | 7 (10.5) | 13 (9.7) | 10 (10.5) | ||
| C(Ludhiana) | 83 (28.0) | 21 (31.3) | 36 (26.9) | 26 (27.4) | ||
| D(Payal) | 35 (11.8) | 12 (17.9) | 16 (11.9) | 7 (7.4) | ||
| E(Raikot) | 47 (15.9) | 10 (14.9) | 19 (14.2) | 18 (19.0) | ||
| F(Samrala) | 46 (15.6) | 8 (12.0) | 26 (19.4) | 12 (12.6) | ||
| Age (years) | 20–30 | 38 (12.8) | 7 (10.5) | 19 (14.2) | 12 (12.6) | <0.001 |
| 31–40 | 103 (34.8) | 22 (32.8) | 45 (33.6) | 36 (37.9) | ||
| 41–50 | 59 (19.9) | 25 (37.3) | 11 (8.2) | 23 (24.2) | ||
| 50+ | 96 (32.4) | 13 (19.4) | 59 (44.0) | 24 (25.3) | ||
| Experience (years) | 0–9 | 87 (29.4) | 21(31.4) | 32 (23.9) | 34 (35.8) | <0.001 |
| 10–18 | 87 (29.4) | 23(34.3) | 34 (25.4) | 30 (31.6) | ||
| 19–27 | 43(14.6) | 14 (20.9) | 17 (12.6) | 12 (12.6) | ||
| 28–36 | 71(23.9) | 9 (13.4) | 49 (36.6) | 13 (13.7) | ||
| 37–45 | 8 (2.7) | 0 | 2 (1.5) | 6 (6.3) | ||
| Location of work | Urban | 67 (22.6) | 7 (10.5) | 31 (23.1) | 29 (30.5) | 0.053 |
| Rural | 197 (66.6) | 51 (76.1) | 88 (65.7) | 58 (61.1) | ||
| Urban + rural | 32(10.8) | 9 (13.4) | 15 (11.2) | 8 (8.4) | ||
| Practice type | Large animals | 37 (12.8) | 7 (10.9) | 21 (15.8) | 9 (9.7) | 0.35 |
| Mixed practice | 253 (87.2) | 57 (89.1) | 112 (84.2) | 84 (90.3) | ||
| Gender | Male | 276 (93.6) | 53 (79.1) | 133 (100.0) | 90 (94.7) | <0.001* |
| Female | 19 (6.4) | 14 (20.9) | 0 (0.0) | 5 (5.3) | ||
| Brucellosis risk factors | ||||||
| Brucella needle stick injury | No | 280 (95.9) | 64 (95.5) | 127 (96.9) | 89 (94.7) | 0.048* |
| Yes | 12 (4.1) | 3 (4.5) | 4 (3.1) | 5 (5.3) | ||
| Animals at home | No | 168 (56.8) | 50 (74.6) | 70 (52.2) | 48 (50.5) | 0.004 |
| Yes | 128 (43.2) | 17 (25.4) | 64 (47.8) | 47 (49.5) | ||
| Consumes raw milk | No | 260 (88.1) | 64 (97.0) | 121 (90.3) | 75 (78.9) | 0.001 |
| Yes | 35 (11.9) | 2 (3.0) | 13 (9.7) | 20 (21.1) | ||
| Source of information about brucellosis | ||||||
| Mainbrucellosis information source | People | 104 (35.1) | 7 (10.5) | 31 (23.1) | 66 (69.5) | <0.001 |
| Government | 41 (13.9) | 8 (11.9) | 18 (13.4) | 15 (15.8) | ||
| Journals/books | 151 (51.0) | 52 (77.6) | 85 (63.4) | 14 (14.7) | ||
The distribution of the respondents across the three occupations varied significantly by age (p < 0.001), experience (p < 0.001), gender (p < 0.001), main information source of brucellosis (p < 0.001) and risk factors, such as Brucella needle stick injury (p < 0.048), having animals at home (p = 0.004), and consuming raw milk (p < 0.001). All para-veterinarians were males, compared to 94.7% males amongst handlers and 79.1% of males amongst veterinarians (p < 0.001). A large proportion (44.0%) of para-veterinarians was over 50 years old, compared to handlers (25.3%) handlers and veterinarians (19.4%) in the same age group (p < 0.001). The highest proportions of animal handlers kept animals at home (49.5%) and consumed raw milk (21.1%). However, only 14.7% used academic journals and books as their main source of brucellosis information, compared to veterinarians (77.6%) and handlers (63.4%),who obtained disease information via other people (69.5%, Table 1).
The number of years in practice and the frequency of exposure to specific veterinary interventions differed by occupation (Table 2). The number of years of experience varied significantly between the personnel (p = 0.01); on average, para-veterinarianswere the most experienced group (20.0 years) followed by handlers (16.3 years) and veterinarians (15.9 years).
Table 2.
Descriptive data of veterinary experience in years and the frequency of potential exposure in one month during the study of comparative risks of brucellosis exposure to the veterinary personnel in the state of Punjab, India in 2015.
| Variable | Veterinarians (n = 67) | Para-veterinarians (n = 134) | Handlers (n = 95) | p-Value⁎ |
|---|---|---|---|---|
| Experience | ||||
| Median (IQR) (years) | 16 (8–20) | 20 (10−30) | 12 (8–20) | |
| Mean and range, (years) | 15.9(0–34) | 20.0 (1–38) | 16.3 (2–45) | 0.01 |
| Potential exposure situations (during the previous one month) | ||||
| Parturition cases handled | ||||
| Median (IQR) | 1 (0–3) | 3 (1–5) | 2 (0–4) | |
| Mean and range, number of cases | 2.15 (0−20) | 6.55 (0−100) | 3.83 (0–60) | <0.001 |
| Retained placenta removal | ||||
| Median (IQR) | 0 (0–2) | 4 (1–5) | 5 (0–5) | |
| Mean and rangenumber of cases | 1.54 (0–15) | 3.79 (0–50) | 2.92 (0−30) | <0.001 |
| Aborted foetus cases handled | ||||
| Median (IQR) | 0 (0–1) | 0 (0–2) | 0 (0–3) | |
| Mean and rangenumber of cases | 0.8 (0–20) | 1.9 (0–50) | 2.08 (0–40) | <0.001 |
| Stillbirth cases handled | ||||
| Median (IQR) | 0 (0–0) | 2 (0–4) | 0 (0–3) | |
| Mean and rangenumber of cases | 0.4 (0–20) | 3.04 (0–35) | 1.93 (0–20) | <0.001 |
| Infertility cases handled | ||||
| Median (IQR) | 9 (3–15) | 7 (4–14) | 1 (0–5) | |
| Mean and rangenumber of cases | 11.3 (0–72) | 9.82 (0–100) | 4.97 (0–100) | <0.001 |
| Artificial inseminations performed | ||||
| Median (IQR) | 30 (10–80) | 48 (20–90) | 5 (0–18) | |
| Mean and rangenumber of cases | 51.2 (0–250) | 59.9 (0–500) | 22.3 (0–140) | <0.001 |
Kruskal wallis test.
On average, para-veterinarians were also found to attend the greatest number of high-risk interventions during the past month, such as performing artificial inseminations (59.9), handling stillbirth (3.79) and parturition (6.55) cases compared to handlers and veterinarians (p < 0.001). Abortion cases were most attended by the handlers (p < 0.001), while veterinarians handled the most infertility cases (p < 0.001) during the past month.
3.2. Univariable and multivariable binary regression analyses
The analyses of variables related to perceived likelihood of brucellosis exposure risk are shown in Table 3, Table 4, Table 5, Table 6 and Suplementary Tables 1 & 2.
-
(a)
Brucellosis exposure risk due to veterinary practice in different animal species:
The multivariable model showed that compared to veterinarians, para-veterinarians (OR 0.4, 95%CI 0.2–0.8) and animal handlers (OR 0.3, 95%CI 0.2–0.7) were less likely to consider sheep and goat practice a potential brucellosis exposure (p = 0.004); and the animal handlers were also likely to believe that small animal practice exposed them to brucellosis (OR 0.5, 95% CI 0.3–0.9) (Table 3).
-
(b)
Brucellosis exposure risk due to the handling of different routine procedures (such as handling body fluids, discharges) during veterinary practice: Animal handlers were more likely to perceive contact with animal saliva as a potential exposure risk compared to the veterinarians (OR 2.3, 95%CI 1.3–5.2, p = 0.02), and to the contrary, consider assisting in conception/parturition procedures less likely (OR 0.3, 95%CI 0.1–0.8, p = 0.01) as potential brucellosis exposure risk (Table 4).
-
(c)
Knowledge about human brucellosis infection and animal vaccination: The difference between three occupational groups of veterinary personnel with regards to their knowledge of human brucellosis infection and animal vaccinations are presented in Table 5. Compared to veterinarians, animal handlers were less likely to be aware of signs and symptoms of human brucellosis; have been tested for brucellosis; knew about the availability of brucella vaccine against cattle; recommend vaccination of animals against brucellosis; and have vaccinated the female calves against brucellosis, respectively. Para-veterinarians were also less likely to be aware of the availability of brucellosis vaccine for cattle (OR 0.2, 95%CI 0.04–0.9) compared to the veterinarians. While all veterinarians (100%) would recommend to animal owners to get their animals vaccinated, 84% of para-veterinarians and only 76.6% of animal handlers would do so. Collinearity was observed between the two strongly positively correlated variables ‘age' and ‘experience' while constructing the final multivariable model for ‘awareness of signs and symptoms of human brucellosis' for the different occupations with the GVIF 17.5 for ‘age' and 16.1 for ‘experience' respectively (χ2 = 315.7, df = 12, p-value<0.001). The proportion of veterinarians (64.2%), who undertook Brucella testing was higher than that of the para-veterinarians (57.7%) or animal handlers (21.1%), but animal handlers were significantly more likely to test positive compared to the veterinarians (OR 5.7, 95%CI 1.2–33.7, p = 0.03).
-
(d)
Enablers and barriers to PPE use during veterinary procedures: The results of tests of association and multivariable analysis to investigate the likely enablers and barriers of PPE use while attending veterinary procedures are presented in Table 6. Compared to veterinarians, the animal handlers (65.9%) were least likely to feel that the use of PPE enhanced their efficiency, while more para-veterinarians (72.9%) felt otherwise. Similarly, previous experience with zoonotic diseases was an unlikely enabler for animal handlers to use PPE compared to veterinarians. More veterinarians (40.0%) and para-veterinarians (36.1%) were encouraged by their previous experience of zoonotic diseases to use PPE in routine situations as they perceived zoonotic infection risk to their lives more than animal handlers (21.1%).
An investigation into the likely barriers to PPE use by veterinary personnel while attending routine veterinary procedures revealed that compared to the veterinarians, animal handlers/para-veterinarians were less likely to use PPE due to time constraints or cost constraints or due to heat stress.
-
(e)
Level of concern regarding contracting brucellosis infection through veterinary work: Animal handlers were less likely to feel concerned about contracting brucellosis infection (Supplementary Table 1).
-
(f)
Level of the adequacy of PPE use during high-risk veterinary interventions:Compared to veterinarians, animal handlers were less likely to use adequate PPE during the three high-risk veterinary interventions, namely conception/parturition cases, abortion/stillbirth zcases and manual removal of retained placenta. Para-veterinarians were also less likely to use adequate PPE than veterinarians (Supplementary Table 2).
Table 3.
Test of association and multivariable logistic regression analyses of perceived likelihood of brucellosis exposure risk with respect to contact with various animal species during veterinary practice in the study on comparative exposure risk to brucellosis amongst veterinary personnel in Punjab, India during 2015.
| Number of participants | Likely (%) | Univariable analysis/ test of association |
Multivariable analyses |
Model adjustment⁎ | |||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | Adjusted OR |
P value | ||||
| (95%CI) | |||||||
| Q. What do you think is your likelihood of exposure to brucellosis from small animal (dog/cat) practice? | 0.06 | 0.1 | Adjusted for gender | ||||
| Animal Handler | 88 | 31(35.2) | 0.5 (0.3–1.0) | 0.5 (0.3–0.9) | |||
| Para-veterinarians | 130 | 42(32.3) | 0.4(0.2–0.8) | 0.6(0.3–1.1) | |||
| Veterinarian | 62 | 32(51.6) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from cattle practice? | 0.001 | 0.008 | Adjusted for tehsil, location and age | ||||
| Animal Handler | 92 | 85 (92.4) | 0.6 (0.1–2.3) | 0.6 (0.1–3.3) | |||
| Para-veterinarians | 134 | 134 (100) | – | – | |||
| Veterinarian | 67 | 64 (95.5) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from equine practice? | 0.09 | 0.2 | Adjusted for gender | ||||
| Animal Handler | 89 | 22 (24.7) | 0.5 (0.2–1.0) | 0.5 (0.3–1.1) | |||
| Para-veterinarians | 132 | 33 (25.0) | 0.5 (0.3–1.0) | 0.6 (0.3–1.1) | |||
| Veterinarian | 89 | 24 (39.3) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from swine practice? | 0.09 | 0.15 | Adjusted for gender | ||||
| Animal Handler | 87 | 18 (20.7) | 0.5 (0.2–1.0) | 0.6 (0.3–1.2) | |||
| Para-veterinarians | 128 | 30 (23.4) | 0.5 (0.3–1.0) | 0.5 (0.2–1.1) | |||
| Veterinarian | 61 | 22 (36.1) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from sheep and goat practice? | 0.006 | 0.004 | Adjusted for tehsil and age | ||||
| Animal Handler | 87 | 30 (34.5) | 0.4 (0.2–0.7) | 0.3 (0.2–0.7) | |||
| Para-veterinarians | 131 | 52 (39.7) | 0.4 (0.2–0.8) | 0.4 (0.2–0.8) | |||
| Veterinarian | 64 | 38 (59.4) | Ref | Ref | |||
The association was individually tested for each demographic predictor and only the factors that yielded p value of ≤ 0.25 were adjusted in the final model for association of the occupation with the response variable.
Table 4.
Test of association and multivariable logistic regression analyses of perceived likelihood of brucellosis exposure risk with respect to the various procedures encountered during the veterinary practice in the study on comparative exposure risk to brucellosis amongst veterinary personnel in Punjab, India during 2015.
| Number of participants | Likely n (%) | Univariable analysis/ test of association |
Multivariable analyses |
Model adjustment⁎ | |||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | Adjusted OR (95%CI) | P value | ||||
| Q. What do you think is your likelihood of exposure to brucellosis from contact with animal faeces/urine? | Adjusted for age, gender and rurality | ||||||
| Animal Handler | 90 | 54(60.0) | 1.0 (0.5–1.9) | 0.5 | 1.0 (0.5–2.1) | 0.4 | |
| Para-veterinarians | 131 | 70(53.4) | 0.8 (0.4–1.4) | 0.7 (0.3–1.4) | |||
| Veterinarian | 65 | 39(60.0) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from contact with animal blood? | Adjusted for gender and tehsil | ||||||
| Animal Handler | 91 | 67 (73.6) | 0.9 (0.5–1.9) | 0.7 | 0.9 (0.3–1.7) | 0.7 | |
| Para-veterinarians | 134 | 93 (69.4) | 0.8 (0.4–1.5) | 0.7(0.3–1.5) | |||
| Veterinarian | 67 | 50 (74.6) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from contact with animal saliva? | |||||||
| Animal Handler | 90 | 63 (70.0) | 2.3 (1.2–4.4) | 0.04 | 2.6 (1.3–5.2) | 0.02⁎ | Adjusted for tehsil and rurality |
| Para-veterinarians | 134 | 78 (58.2) | 1.3 (0.7–2.4) | 1.5 (0.8–2.8) | |||
| Veterinarian | 67 | 34 (50.7) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis from contact with animal bodily fluids? | Adjusted for age and experience | ||||||
| Animal Handler | 92 | 76 (82.6) | 0.8 (0.4–2.0) | 0.3 | 0.9 (0.4–2.3) | 0.5 | |
| Para-veterinarians | 133 | 119 (89.5) | 1.5 (0.6–3.6) | 1.5 (0.6–3.7) | |||
| Veterinarian | 66 | 56 (84.9) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis while performing post-mortems? | Adjusted for gender, age and experience | ||||||
| Animal Handler | 91 | 77 (84.6) | 0.9 (0.3–2.1) | 0.3 | 0.9 (0.3–2.3) | 0.5 | |
| Para-veterinarians | 132 | 120 (90.9) | 1.6 (0.6–4.0) | 1.4 (0.5–4.1) | |||
| Veterinarian | 66 | 57(86.4) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis while assisting conception/parturition? | |||||||
| Animal Handler | 91 | 71 (78.0) | 0.3 (0.1–0.8) | 0.008 | 0.3 (0.1–0.8) | 0.01 | Adjusted for gender and tehsil |
| Para-veterinarians | 134 | 122 (91.0) | 0.8 (0.3–2.5) | 0.7 (0.2–2.4) | |||
| Veterinarian | 66 | 61 (92.4) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis on contact with healthy animals? | |||||||
| Animal Handler | 87 | 32 (36.8) | 0.6 (0.3–1.2) | 0.2 | 0.7 (0.3–1.3) | 0.2 | Adjusted for age and rurality |
| Para-veterinarians | 131 | 46 (35.1) | 0.6 (0.3–1.1) | 0.6 (0.3–1.1) | |||
| Veterinarian | 65 | 31(47.7) | Ref | Ref | |||
| Q. What do you think is your likelihood of exposure to brucellosis on contact with sick animals? | |||||||
| Animal Handler | 90 | 67 (74.4) | 0.5 (0.2–1.2) | 0.6 | 0.5 (0.2–1.2) | 0.4 | Adjusted for experience |
| Para-veterinarians | 134 | 117 (87.3) | 1.2 (0.5–2.8) | 1.5 (0.6–3.6) | |||
| Veterinarian | 90 | 57 (85.1) | Ref | Ref | |||
The association was individually tested for each demographic predictor and only the factors that yielded p value of ≤ 0.25 were adjusted in the final model for association of the occupation with the response variable.
Table 5.
Test of association and multivariable logistic regression analyses of knowledge and experience regarding human brucellosis infection and animal vaccination amongst veterinary personnel in Punjab, India during 2015.
| Number of participants | Likely n (%) | Univariable analysis/ test of association |
Multivariable analyses |
Model adjustment⁎ | |||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | Adjusted OR (95%CI) | P value | ||||
| Q. Are you aware of the signs and symptoms of brucellosis? | |||||||
| Animal Handler | 93 | 38 (40.9) | 0.06 (0.02–0.15) | <0.001 | 0.05 (0.02–0.14) | <0.001 | Adjusted for tehsil and experience |
| Para-veterinarians | 130 | 117 (90.0) | 0.7 (0.2–2.1) | 0.6 (0.2–1.9) | |||
| Veterinarian | 67 | 62 (92.5) | Ref | Ref | |||
| Q. Have you ever been tested for brucellosis? | |||||||
| Animal Handler | 93 | 20 (21.1) | 0.1 (0.07–0.3) | <0.001 | 0.1 (0.03–0.2) | <0.001 | Adjusted for age, gender and tehsil |
| Para-veterinarians | 130 | 75 (57.7) | 0.8 (0.4–1.4) | 0.5 (0.2–1.0) | |||
| Veterinarian | 67 | 43 (64.2) | Ref | Ref | |||
| Q. Do you know that vaccine for brucellosis is available for cattle? | |||||||
| Animal Handler | 94 | 69 (73.4) | 0.1 (0.04–0.4) | <0.001 | 0.07 (0.01–0.3) | <0.001 | Adjusted for gender |
| Para-veterinarians | 132 | 118 (89.4) | 0.4 (0.1–1.4) | 0.2 (0.04–0.9) | |||
| Veterinarian | 66 | 64 (95.5) | Ref | Ref | |||
| Q. Do you recommend animal owners to vaccinate their animals against brucellosis? | |||||||
| Animal Handler | 94 | 72 (76.6) | 0.1 (0.02–0.3) | <0.001 | 0.1 (0.02–0.3) | <0.001 | Adjusted for age and tehsil |
| Para-veterinarians | 132 | 128 (84.0) | Ref | Ref | |||
| Veterinarian | 66 | 66 (100.0) | – | – | |||
| Q. Have you ever vaccinated females calves against brucellosis? | |||||||
| Animal Handler | 95 | 38 (40) | 0.2 (0.1–0.4) | <0.001 | 0.2 (0.1–0.4) | <0.001 | Adjusted for tehsil |
| Para-veterinarians | 131 | 110 (84.0) | 1.6 (0.8–3.4) | 1.8 (0.9–3.9) | |||
| Veterinarian | 67 | 51 (76.1) | Ref | Ref | |||
The association was individually tested for each demographic predictor and only the factors that yielded p value of ≤ 0.25 were adjusted in the final model for association of the occupation with the response variable.
Table 6.
Test of association and multivariable binary logistic regression analyses of PPE perception and practices amongst veterinary personnel in Punjab, India during 2015.
| Number of participants | Likely (%) | Univariable analysis/ test of association |
Multivariable analyses |
Model adjustment⁎ | |||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P value | Adjusted OR (95%CI) | P value | ||||
| Enablers to PPE use | |||||||
| Q.Does the risk to your life due to zoonotic diseases encourage you to use PPE? | |||||||
| Animal Handler | 93 | 78(83.9) | 0.2 (0.1–0.4) | 0.03 | 0.2 (0.1–0.4) | <0.001 | Adjusted fortehsil and experience |
| Para-veterinarians | 133 | 123 (92.5) | 1.6 (0.8–3.4) | 1.9 (0.9–4.2) | |||
| Veterinarian | 67 | 64 (95.5) | Ref | Ref | |||
| Q. Does your previous experience with brucellosis due to zoonotic diseases encourage you to use PPE? | |||||||
| Animal Handler | 90 | 19(21.1) | 0.4 (0.2–0.8) | 0.02 | 0.4 (0.2–0.8) | 0.03 | Adjusted for age,tehsil, experience |
| Para-veterinarians | 133 | 48 (36.1) | 0.8 (0.5–1.6) | 0.7 (0.4–1.4) | and rurality | ||
| Veterinarian | 65 | 26 (40.0) | Ref | Ref | |||
| Q. Does using PPE helps you to perform efficiently? | |||||||
| Animal Handler | 91 | 60(90.9) | 0.2 (0.1–0.5) | <0.001 | 0.1 (0.05–0.4) | <0.001 | Adjusted for age, tehsil, and rurality |
| Para-veterinarians | 133 | 97 (72.9) | 0.3 (0.1–0.7) | 0.2 (0.1–0.6) | |||
| Veterinarian | 66 | 60 (65.9) | Ref | Ref | |||
| Q. Does using PPE enables to keep your clothes clean? | |||||||
| Animal Handler | 91 | 62(68.1) | 0.5 (0.2–1.1) | 0.12 | 0.5 (0.2–1.1) | 0.09 | Adjusted for age, tehsil, experience |
| Para-veterinarians | 133 | 90 (67.7) | 0.5 (0.2–1.0) | 0.4 (0.2–0.9) | and rurality# | ||
| Veterinarian | 67 | 54 (80.6) | Ref | Ref | |||
| Barriers to PPE use | |||||||
| Q. Does the constraint of time discourage the use of PPE? | |||||||
| Animal Handler | 90 | 16(17.8)) | 0.2 (0.1–0.5) | <0.001 | 0.3 (0.1–0.5) | <0.001 | Adjusted for age and rurality |
| Para-veterinarians | 132 | 25 (18.9) | 0.2 (0.1–0.5) | 0.3 (0.1–0.6) | |||
| Veterinarian | 64 | 32 (48.5) | Ref | Ref | |||
| Q. Does the cost of PPE discourage you from using PPE? | |||||||
| Animal Handler | 90 | 36(40.0) | 0.4 (0.2–0.8) | 0.009 | 0.4 (0.2–0.8) | 0.02 | Adjusted for gender and tehsil |
| Para-veterinarians | 134 | 55 (41.0) | 0.4 (0.2–0.8) | 0.4 (0.2–0.8) | |||
| Veterinarian | 66 | 41 (62.1) | Ref | Ref | |||
| Q. Does the heat stress discourage you from using PPE? | |||||||
| Animal Handler | 90 | 24(26.7) | 0.5 (0.3–1.0) | 0.06 | 0.5 (0.2–0.9) | 0.03 | Adjusted for gender and tehsil |
| Para-veterinarians | 133 | 33 (24.8) | 0.5 (0.2–0.9) | 0.4(0.2–0.8) | |||
| Veterinarian | 66 | 27 (40.9) | Ref | Ref | |||
| Q. Does safety concerns such as poor visibility discourage you from using PPE? | |||||||
| Animal Handler | 89 | 27(30.3) | 0.7 (0.4–1.5) | 0.12 | 0.7 (0.3–1.3) | 0.24 | Adjusted for tehsil |
| Para-veterinarians | 131 | 36 (27.5) | 0.6 (0.3–1.2) | 0.6 (0.3–1.1) | |||
| Veterinarian | 75 | 24 (36.9) | Ref | Ref | |||
| Q. Does the concern for an adverse reaction from the animals discourage you from using PPE? | No multivariable model was attempted as none of the demographic variables | ||||||
| Animal Handler | 89 | 19 (21.3) | 0.8 (0.4–1.7) | 0.8 | yielded p value of ≤ 0.25 | ||
| Para-veterinarians | 132 | 33 (25.0) | 1.0 (0.5–1.9) | ||||
| Veterinarian | 66 | 17 (25.8) | Ref | ||||
The association was individually tested for each demographic predictor and only the factors that yielded p value of ≤ 0.25 were adjusted in the final model for association of the occupation with the response variable.
3.3. Negative binomial regression analyses
The mean number of high-risk veterinary interventions when adequate PPE was used during the past month was found to be the lowest for animal handlers. PPE use while attending high-risk veterinary interventions was found highest by veterinarians followed by para-veterinarians (Table 7).
Table 7.
Negative binomial univariable and multivariable regression analyses for incident rates on exposure to high-risk situations based on the level of PPE use by the veterinary personnel in Punjab, India 2015.
| Variable | Number | Mean (SD) | Estimate |
IRRa (95%CI) |
P value |
Estimate |
Adjusted IRRb (95%CI) |
P value |
|---|---|---|---|---|---|---|---|---|
| Univariable model | Multivariable model | |||||||
| Occupation | ||||||||
| Intercept | −0.4 (0.2) | <0.001 | −1.5 (0.5) | <0.001 | ||||
| Animal Handler | 95 | 0.05 (0.4) | −2.5 (0.3) | 0.08 (0.02–0.2) | −2.3 (0.5) | 0.1 (0.03–0.3) | ||
| Para-veterinarians | 134 | 0.5 (0.9) | −0.4 (0.5) | 0.7 (0.4–1.2) | −0.2 (0.3) | 0.8 (0.4–1.5) | ||
| Veterinarian | 67 | 0.7 (1.1) | – | Ref | – | Ref | ||
| PPE use encouraged by the ability to perform efficiently | ||||||||
| Intercept | −2.1 (0.4) | |||||||
| Low | 73 | 0.1 (0.4) | Ref | 0.001 | Ref | 0.004 | ||
| High | 217 | 1.0 (0.9) | 1.4 (0.4) | 3.9 (1.8–9.4) | 1.2 (0.4) | 3.2 (1.4–7.6) | ||
| Information source | ||||||||
| Intercept | −2.1 (0.3) | |||||||
| People | 41 | 0.5 (0.9) | Ref | 0.006 | ||||
| Government | 151 | 0.5 (0.9) | 1.3 (0.5) | 3.6 (1.4–9.5) | ||||
| Journals/books | 104 | 0.1 (0.5) | 1.3 (0.4) | 4.3 (2.1–9.0) | ||||
| Age | ||||||||
| Intercept | −0.6 (0.4) | 0.14 | ||||||
| 20–30 | 38 | 0.6 (1.0) | Ref | |||||
| 31–40 | 103 | 0.3 (0.7) | −0.7 (0.4) | 0.5 (0.3–1.1) | ||||
| 41–50 | 59 | 0.3 (0.7) | −0.7 (0.5) | 0.5 (0.2–1.3) | ||||
| 50+ | 96 | 0.5 (0.9) | −0.1 (0.4) | 0.9 (0.4–2.1) | ||||
| PPE use encouraged by zoonotic risk | ||||||||
| Intercept | −2.6 (0.8) | 0.03 | ||||||
| Low | 28 | 0.1 (0.3) | ||||||
| High | 265 | 0.4 (0.9) | 1.8 (0.8) | 5.9 (1.4–39.7) | ||||
| Performed AI last month | 0.09 | |||||||
| Intercept | −1.4 (0.3) | |||||||
| No | 74 | 0.2 (0.7) | Ref | |||||
| Yes | 222 | 0.4 (0.9) | 0.6 (0.4) | 1.8 (0.9–3.8) | ||||
| PPE use encouraged by past experience | ||||||||
| Intercept | −1.1 (0.2) | 0.1 | ||||||
| Low | 195 | 0.3 (0.7) | Ref | |||||
| High | 93 | 0.5 (1.0) | 0.5 (0.3) | 1.6 (0.9–3.0) | ||||
| Brucellosis tested | ||||||||
| Intercept | −1.2 (0.2) | 0.1 | ||||||
| No | 154 | 0.3 (0.8) | Ref | |||||
| Yes | 138 | 0.5 (0.9) | 0.5 (0.3) | 1.6 (0.9–2.9) | ||||
| PPE use discouraged by time constraints | 0.1 | |||||||
| Intercept | −1.1 (0.2) | |||||||
| Low | 215 | 0.3 (0.8) | Ref | |||||
| High | 73 | 0.5 (1.0) | 0.5 (0.3) | 1.6 (0.8–3.0) | ||||
| PPE use encouraged by keeping the clothes clean | ||||||||
| Intercept | −1.2 (0.3) | 0.2 | ||||||
| Low | 85 | 0.3 (0.7) | Ref | |||||
| High | 206 | 0.4 (0.9) | 0.4 (0.3) | 1.5 (0.8–2.8) | ||||
| Attended infertility cases in last month | ||||||||
| Intercept | −1.2 (0.3) | 0.13 | ||||||
| No | 80 | 0.2 (0.7) | Ref | |||||
| Yes | 216 | 0.4 (0.9) | 0.5 | 1.7 (0.8–3.4) | ||||
IRR = Incidence rate ratio.
Adjusted for ‘PPE use encouraged by the ability to perform efficiently’.
All explanatory variables were tested against the outcome variable of ‘number of high-risk veterinary interventions when adequate PPE was used' using univariable negative binomial? regression analyses. Eleven explanatory factors yielded the p-value of <0.25 and were included in the initial multivariable negative binomial regression model. Only twovariables (three descriptive and one enabler of the PPE use) were retained in the final multivariable model (Table 7). The model was found to be stable when checked for goodness of fit using ‘R' package ‘DHARMa', where the model residuals were found distributed normally with non-significant deviation (Dispersion test: p = 0.3; Kolmogorov-Smirnov test: p = 0.9).
The incident rate ratios derived from the final multivariable model revealed that the lowest use of PPE during high-risk interventions was by animal handlers followed by para-veterinarians,when compared to the veterinarians (p < 0.001). The participants who felt that use of PPE during high-risk veterinary interventions enhance their professional efficiency were also found to have high PPE use rates (IRR 3.3, 95%CI 1.5–8.1, p = 0.003), compared to those participants who felt otherwise.
4. Discussion
A high prevalence of brucellosis has been reported in veterinary personnel globally (including India) as they are at risk of frequent exposure to infected animals [4,25,26]. In the present study, we further the findings of Proch, Singh, Schemann, Gill, Ward and Dhand [6] by comparing brucellosis prevalence and risk factors for three occupational groups within the veterinary profession, and assess their perceptions and practices towards the use of PPE during high-risk exposures in the course of veterinary practice in the state of Punjab, India. In response to the structured questionnaire the highest proportion of animal handlers (31.25%) admitted testing positive for Brucella infection compared to the para-veterinarians (11.11%) or the veterinarians (7.5%), although the number of animal handlers who undertook testing (20 of 67) for brucellosis was the lowest of the three occupational groups [6].
The disinclination to seek testing by animal handlers is supported by the finding that compared to veterinarians or para-veterinarians, the former were less likely to be aware of signs and symptoms of human brucellosis, or most likely to perceive exposure to animal saliva as a potential infection risk. Further, they were less likely to consider sheep and goat practice or assisting in parturition/conception procedures as potential brucellosis exposure risk. They were also less likely to consider exposure to sick animals as a potential infection risk and consequently least likely to recommend vaccinations against brucellosis for cattle.A higher prevalence of brucellosis infection in animal handlers compared to veterinarians and para-veterinarians has been reported in other states of India, such as Odisha [27] and Karnataka [17], although to the contrary in an earlier study in the same area as this current investigation the prevalence in animal handlers was found to be less than that for samples originating from veterinarians and para-veterinarians [11]. Animal workers were also found to have a higher prevalence than cattle breeders in Namibe Province, Angola while no significant difference in the prevalence between different occupations was reported from the Khyber Pakhtunkhwa region of Pakistan [28].
Some studies have reported an association between low education levels and awareness of human brucellosis in Asia, such as in Pakistan [29], Tajikistan [30] and Middle East Asia [31]. Knowledge about brucellosis transmission was also found lacking in a study in Karnataka [17] and Assam state in India [32]. All the animal handlers included in the present study had a high school level education and despite their occupation requiring interaction with animals, presumably, they are not equipped with relevant knowledge regarding zoonotic diseases. Further, the study highlighted that the main source of information on brucellosis for animal handlers was through people (69.5%), and only 14.7% reportedly referred to books/journals, as opposed to 77.6% of veterinarians and 63.4%of para-veterinarians. This could be because animal handlers are not exposed to any training in veterinary sciences in the course of their vocation.
The lower likelihood of reliance on government sources for information on the disease compared to other sources could possibly be attributed to the absence of formal vocational training in veterinary sciences across all occupational groups (Table 1). It is recommended that periodic professional training courses be introduced that could increase the knowledge of the animal handlers and para-veterinarians alike in addition to periodic release of newsletters regarding the disease. It would also help to enhance their professional skills.
Interestingly, older participants and males were more likely to have been tested for brucellosis than the younger and female respondents. While the length of service implies that older participants had a chance of being tested at some point in their career,the gender disparity should be read with caution as only a few female veterinary personnel participated in the survey. Amongst the various tehsils (sub-districts), the veterinary personnel from Khanna were least likely to have been tested for brucellosis. Although it may imply a lack of awareness about human brucellosis in Khanna, there could be other plausible reasons such as lack of availability of testing facilities that were not investigated in this study and must form part of future studies.
Not surprisingly, in the multivariable models constructed to assess the enablers of PPE use during veterinary practice, being an animal handler compared to being a veterinarian was protective (Table 6). That a significant number of animal handlers were indifferent to the risk of Brucella infection to their lives (OR 0.2), only implies that compared to veterinarians, the former were not encouraged to improve their professional efficiency (OR 0.1) by using PPE during veterinary procedures. Only a few of them (21.1%) learnt to use PPE based on their previous experience of zoonotic diseases.
Unexpectedly, in a notable finding of [6], the veterinary personnel using PPE while attending sick animals were found to be more likely to be seropositive than others. While the potential reasons for the finding were elaborated in the publication, elsewhere individuals involved in veterinary practice have been reported to suffer from zoonotic infections when they fail to adhere to healthy biosecurity practices such as using adequate PPE while attending sick animals [26,33,34]. In the present study, the comparative risk based on adequacy of PPE use during high risk veterinary situations amongst the three occupations of the veterinary profession was analysed. It is a matter of great concern that the rate of PPE use across all professions in this study was found to be grossly inadequate (Supplementary Table 2). The inadequate PPE use by the animal handlers compared to veterinarians can again be attributable to a lack of awareness of not only brucellosis but also other potential zoonotic infections. It could be that their previous exposures to zoonotic infections could have gone unnoticed in the absence of any institutionalised testing or active surveillance. It is suggested that a serosurvey of animal handlers should be conducted to investigate previous or current affections such as pyrexia of unknown origin [35], as it could reflect the magnitude of clinical/subclinical zoonotic infections amongst this group of veterinary personnel.
Given the finding that the likelihood of animal handlers testing positive is higher than veterinarians or para-veterinarians, it is not surprising that on average they attended a higher number of potentially high-risk veterinary interventions such as ‘handling of abortedfoetus’ (mean-2.08) than veterinarians (mean-0.8) or the para-veterinarians (mean-1.9). They also handled a significantly higher number of stillbirth cases, removals of retained placentaand parturition cases than the veterinarians (Table 2). A higher frequency of exposure to high-risk interventions and the demonstrated negligible use of PPE compared to veterinarians and para-veterinarians during such interventions (Supplementary Table 2) makes animal handlers the most vulnerable occupation of the three veterinary personnel considered in this study.The little concern demonstrated by the animal handlers regarding the transmission of infection to their colleagues or staff during their routine work (Supplementary Table 1) could also be a serious impediment to the success of any brucellosis control programme in the state.
An important risk to the vaccinators during a brucellosis vaccination programme is needle-stick injuries and accidental inoculations of livestock Brucella vaccines [36]. A long-term adverse reaction due to accidental inoculation of the RB51 brucellosis vaccine has been reported [37]. It has also necessitated the introduction of ‘needle stick injury avoidance protocols’, which are recommended as essential practices for carrying out brucella vaccination programmes in cattle [38]. However, in our study, needle-stick injury during vaccination campaigns was experienced by only 12 respondents (4.1%), of which the majority were animal handlers (Table 1). On the contrary, a significant proportion (26.6%) of animal handlers were unaware of the availability of vaccinations for cattle (Table 5). It is not surprising that the relationship between the animal handlers not recommending vaccination against brucellosis in cattle, and those who experienced needlestick injuries was not significant. We reason that a larger proportion of animal handlers experiencing needle stick injuries could be because they are at the forefront of any government-sponsored brucellosis control vaccination campaign owing to their farther reach in the rural and remote areas. We recommend that a change in the perception of brucellosis vaccination in animals should be facilitated by increasing awareness and improved disease control practices such as adherence to ‘needle stick injury avoidance protocols’, highly recommended for the success of the recently launched brucellosis eradication scheme by the Government of India (https://dahd.nic.in/about-us/divisions/livestock-health).
In addition to the significant variation between the three veterinary occupations, the variable ‘information source' was found to significantly (p = 0.006) influence the PPE use during the high-risk gynaecological and obstetric interventions in the univariable analysis, although it was only marginally non-significant (p = 0.06) when included the multivariable model (Table 7). This implies that the individuals who were most likely to use PPE during such interventions were likely to obtain information regarding brucellosis from formal sources such as government channels (OR = 2.5) or through books/journals (OR = 2.4). As the study has indicated that animal handlers are least likely to use PPE during high risk interventions, this finding only reinforces the dependence of animal holders on obtaining information from people which is an informal communication medium. As discussed previously, para-veterinarians and veterinarians are comparatively more oriented towards formal channels of information presumably due to their formal vocation into the veterinary profession. Mostly, animal handlers start as ‘helpers' to the para-veterinarians and veterinarians and later start to perform some interventions independently. It must be accepted that they fill an essential gap in the animal husbandry services in remote villages that are beyond the reach of veterinarians and para-veterinarians. Formal training and inclusion of biosecurity principles in their training curriculum will go a long way to help them adapt to healthy biosecurity practices during veterinary practice.
Admittedly, analysis of the potential barriers for adequate PPE use during high-risk veterinary interventions gives a false impression that animal handlers are not restricted by the barriers considered in the study, as they all return protective OR in the multivariable logistic regression model. It is a serious limitation of this study because the animal handlers who reported as less likely to be affected by thepotential barriers to PPE use such as time, cost or constraint of heat stress (Table 6), were in fact least likely to use PPE to enhance efficiency during high-risk interventions (Table 7). We recommend that future studies should take into account opinions on the potential barriers only from those participant groups which have a minimum score for the adequacy of PPE use. Further, self-reported behaviour may not reflect the actual practice of the respondents, a limitation akin to the questionnaire surveys [39]. This could be resolved by observing the behaviour of the participants, but the study was restricted by time constraints. We recommend further studies to investigate the inconsistencies between self-reported and the observed practice of PPE use. The inclusion of fewer female participants across the three occupations is another limitation of this study.
It would be informative to reassess the prevalence and perception of brucellosis in India following the launch of a nationwide programme for brucellosis eradication in 2019. Within this program, brucella vaccination for livestock is being made available free. It is an ambitious project, and this current study underscores that in addition to vaccination, the strategy for brucellosis control requires collateral efforts such as improved disease and biosecurity awareness amongst veterinary personnel. A biosecurity protocol at the local level that provides guidelines for PPE use together with initiating measures to enhance afforaadability and availability of PPE is arguably the first step to reduce this occupational hazard amongst veterinary personnel.
5. Conclusion
The frequent exposure of veterinary personnelto infected animals places themat highrisk to contract brucellosis. However, the prevalence of the disease varies amongst the different occupations within the veterinary profession. The risk of exposure to Brucella organisms is significantly higher for animal handlers compared to para-veterinarians and veterinarians. Despite the high exposure risk and the highest prevalence amongst the veterinary personnel, this study highlights the disinclination of animal handlers to get tested for brucellosis andthe minimal use of PPE while attending high-risk veterinary interventions. We recommend that animal handlers should be brought into the ambit of personneltrained through government efforts towardsthe importance of biosecurity measures in veterinary practice. The study also brings to light the barriers to PPE use by the veterinary personnel, such as severe weather conditions, cost and time constraints. Although this study was conducted in the state of Punjab, the circumstances in other states of India are similar.
Author statement
Brucellosis is one of the most important zoonotic diseases prevalent in India. It causes substantial health and economic impact in humans. The disease is most prevalent in veterinary personnel owing to their frequent exposure to diseased livestock during their work. Following an earlier study on prevalence of the brucellosis amongst different veterinary personnel, this study analyses the risk factors of brucellosis amongst veterinary professionals and their practices regarding adequate PPE use when attending high risk veterinary procedures. The disease prevalence was found to be highest in the animal handlers, but they were less likely to be aware of the signs and symptoms of the disease or to recommend vaccination against brucellosis to the livestock owners than veterinarians and the para-veterinarians. They were also less likely to adhere to adequate PPE use during high-risk veterinary interventions. We recommend increasing awareness of the disease and biosecurity practices amongst animal handlers to reduce the risk of contracting zoonotic diseases during their work.
Declaration of Competing Interest
None declared.
Acknowledgements
This study was funded by the University of Sydney's International Program Development Fund. The authors are grateful to all the veterinary personnel who participated in the study Support provided by the Animal Husbandry Department Punjab is thankfully acknowledged.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2021.100367.
Appendix A. Supplementary data
Supplementary material
References
- 1.Hull N.C., Schumaker B.A. Comparisons of brucellosis between human and veterinary medicine. Infect. Ecol. Epidemiol. 2018;8(1):1500846. doi: 10.1080/20008686.2018.1500846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franc K., Krecek R., Häsler B., Arenas-Gamboa A. Brucellosis remains a neglected disease in the developing world: a call for interdisciplinary action. BMC Public Health. 2018;18(1):1–9. doi: 10.1186/s12889-017-5016-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhand N.K., Gumber S., Singh B.B., Aradhana M.S., Bali H., Kumar D.R., Sharma J., Singh K.S. Sandhu. A study on the epidemiology of brucellosis in Punjab (India) using Survey Toolbox. Rev. Sci. Tech. 2005;24(3):879–885. [PubMed] [Google Scholar]
- 4.Mantur B.G., Amarnath S.K. Brucellosis in India—a review. J. Biosci. 2008;33(4):539–547. doi: 10.1007/s12038-008-0072-1. [DOI] [PubMed] [Google Scholar]
- 5.Young E.J. Human brucellosis. Rev. Infect. Dis. 1983;5(5):821–842. doi: 10.1093/clinids/5.5.821. [DOI] [PubMed] [Google Scholar]
- 6.Proch V., Singh B.B., Schemann K., Gill J.P.S., Ward M.P., Dhand N.K. Risk factors for occupational Brucella infection in veterinary personnel in India. Transbound. Emerg. Dis. 2018;65(3):791–798. doi: 10.1111/tbed.12804. [DOI] [PubMed] [Google Scholar]
- 7.Singh B.B., Dhand N.K., Gill J.P.S. Economic losses occurring due to brucellosis in Indian livestock populations. Prevent. Vet. Med. 2015;119(3–4):211–215. doi: 10.1016/j.prevetmed.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Singh B.B., Khatkar M.S., Aulakh R.S., Gill J.P.S., Dhand N.K. Estimation of the health and economic burden of human brucellosis in India. Prevent. Vet. Med. 2018;154:148–155. doi: 10.1016/j.prevetmed.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 9.Singh J., Singh B.B., Tiwari H.K., Josan H.S., Jaswal N., Kaur M., Kostoulas P., Khatkar M.S., Aulakh R.S., Gill J.P.S. Using dairy value chains to identify production constraints and biosecurity risks. Animals. 2020;10(12):2332. doi: 10.3390/ani10122332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landes M., Cessna J., Kuberka L., Jones K. United States Department of Agriculture; 2017. India's Dairy Sector: Structure, Performance, and Prospects. [Google Scholar]
- 11.Yohannes Gemechu M., Gill J. Paul Singh. Seroepidemiological survey of human brucellosis in and around Ludhiana, India. Emerg. Health Threats J. 2011;4(1):7361. doi: 10.3402/ehtj.v4i0.7361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deepthy B. Department of Biotechnology and Microbiology. Kannur University; Kannur: 2012. Serodiagnostic study of animal handlers for brucellosis. (p. 3.8, MB) [Google Scholar]
- 13.Smits H.L., Kadri S.M. Brucellosis in India: a deceptive infectious disease. Indian J. Med. Res. 2005;122(5):375. [PubMed] [Google Scholar]
- 14.Leggat P.A., Smith D.R., Speare R. Exposure rate of needlestick and sharps injuries among Australian veterinarians. J. Occup. Med. Toxicol. 2009;4(1):1–6. doi: 10.1186/1745-6673-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kutlu M., Ergonul O., Sayin-Kutlu S., Guven T., Ustun C., Alp-Cavus S., Ozturk S.B., Acicbe O., Akalin S., Tekin R. Risk factors for occupational brucellosis among veterinary personnel in Turkey. Prevent. Vet. Med. 2014;117(1):52–58. doi: 10.1016/j.prevetmed.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Mrunalini N., Reddy M., Ramasastry P., Rao M. Seroepidemiology of human brucellosis in Andhra Pradesh. Ind. Vet. J. 2004;81(7):744–747. [Google Scholar]
- 17.Shome R., Kalleshamurthy T., Shankaranarayana P.B., Giribattanvar P., Chandrashekar N., Mohandoss N., Shome B.R., Kumar A., Barbuddhe S.B., Rahman H. Prevalence and risk factors of brucellosis among veterinary health care professionals. Pathogens Global Health. 2017;111(5):234–239. doi: 10.1080/20477724.2017.1345366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhand N.K., Singh J., Josan H.S., Singh B.B., Jaswal N., Tiwari H.K., Kostoulas P., Khatkar M.S., Aulakh R.S., Kaur M. The feasibility and acceptability of various bovine brucellosis control strategies in India. Prevent. Vet. Med. April 2021;189 doi: 10.1016/j.prevetmed.2021.105291. Special Issue SVEPM : 2020. [DOI] [PubMed] [Google Scholar]
- 19.Singh B.B., Kostoulas P., Gill J.P.S., Dhand N.K. Cost-benefit analysis of intervention policies for prevention and control of brucellosis in India. PLoS Negl. Trop. Dis. 2018;12(5) doi: 10.1371/journal.pntd.0006488. (e0006488-e0006488) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.R Core Team . Foundation for Statistical Computing; Vienna, Austria: 2019. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 21.Lakatos B., Knotek Z., Farkas J., Adam E., Dobay O., Nasz I. Adenovirus infection in cats. An epidemiological survey in the Czech Republic. Acta Vet. Brno. 1999;68(4):275–280. [Google Scholar]
- 22.Williams C.J., Scheftel J.M., Elchos B.L., Hopkins S.G., Levine J.F. Compendium of veterinary standard precautions for zoonotic disease prevention in veterinary personnel: National Association of State Public Health Veterinarians: Veterinary Infection Control Committee 2015. J. Am. Vet. Med. Assoc. 2015;247(11):1252–1277. doi: 10.2460/javma.247.11.1252. [DOI] [PubMed] [Google Scholar]
- 23.John Fox S. Third ed. Sage; Thousand Oaks, CA: 2019. Weisberg, an {R} Companion to Applied Regression. [Google Scholar]
- 24.Hartig F. 2020. DHARMa: Residual Diagnostics for Hierarchical (Multi-level / Mixed) Regression Models. [Google Scholar]
- 25.Agasthya A.S., Isloor S., Prabhudas K. Brucellosis in high risk group individuals. Indian J. Med. Microbiol. 2007;25(1):28–31. doi: 10.4103/0255-0857.31058. [DOI] [PubMed] [Google Scholar]
- 26.Baker W.S., Gray G.C. A review of published reports regarding zoonotic pathogen infection in veterinarians. J. Am. Vet. Med. Assoc. 2009;234(10):1271–1278. doi: 10.2460/javma.234.10.1271. [DOI] [PubMed] [Google Scholar]
- 27.Priyadarshini A., Sarangi L., Palai T., Panda H., Mishra R., Behera P. Brucellosis in cattle and occupationally exposed human beings: a Serosurvey in Odisha, India. J. Pure Appl. Microbiol. 2013;7:3255–3260. [Google Scholar]
- 28.Khan A., Shafee M., Khan N., Rahman A., Rafiullah R., Ali I., Khan I., Ur Rahman S. Incidence of brucellosis in aborted animals and occupationally exposed veterinary professionals of Bannu, Khyber Pakhtunkhwa, Pakistan. Wētchasān sattawaphāet. 2018;48(1):47–54. [Google Scholar]
- 29.Arif S., Thomson P.C., Hernandez-Jover M., McGill D.M., Warriach H.M., Heller J. Knowledge, attitudes and practices (KAP) relating to brucellosis in smallholder dairy farmers in two provinces in Pakistan. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0173365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lindahl E., Sattorov N., Boqvist S., Magnusson U. A study of knowledge, attitudes and practices relating to brucellosis among small-scale dairy farmers in an urban and peri-urban area of Tajikistan. PLoS One. 2015;10(2) doi: 10.1371/journal.pone.0117318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bagheri Nejad R., Krecek R.C., Khalaf O.H., Hailat N., Arenas-Gamboa A.M. Brucellosis in the Middle East: current situation and a pathway forward. PLoS Negl. Trop. Dis. 2020;14(5) doi: 10.1371/journal.pntd.0008071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deka R.P., Magnusson U., Grace D., Shome R., Lindahl J.F. Knowledge and practices of dairy farmers relating to brucellosis in urban, peri-urban and rural areas of Assam and Bihar, India. Infect. Ecol. Epidemiol. 2020;10(1):1769531. doi: 10.1080/20008686.2020.1769531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khillare R.S., Bhave S.S. Occupational hazards associated with veterinarians and their control measures. J. Foodborne Zoonot. Dis. 2018;6(02):13–17. [Google Scholar]
- 34.Robin C., Bettridge J., McMaster F. Zoonotic disease risk perceptions in the British veterinary profession. Prevent. Vet. Med. 2017;136:39–48. doi: 10.1016/j.prevetmed.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nareaho A., Puomio J., Saarinen K., Jokelainen P., Juselius T., Sukura A. Feline intestinal parasites in Finland: prevalence, risk factors and anthelmintic treatment practices. J. Feline Med. Surg. 2012;14(6):378–383. doi: 10.1177/1098612X12439257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Langley R.L., Pryor W.H., Jr., O’Brien K.F. Health hazards among veterinarians: a survey and review. J. Agromed. 1995;2(1):23–52. [Google Scholar]
- 37.Ashford D.A., di Pietra J., Lingappa J., Woods C., Noll H., Neville B., Weyant R., Bragg S.L., Spiegel R.A., Tappero J. Adverse events in humans associated with accidental exposure to the livestock brucellosis vaccine RB51. Vaccine. 2004;22(25–26):3435–3439. doi: 10.1016/j.vaccine.2004.02.041. [DOI] [PubMed] [Google Scholar]
- 38.Weese J.S., Jack D.C. Needlestick injuries in veterinary medicine. Can. Vet. J. 2008;49(8):780. [PMC free article] [PubMed] [Google Scholar]
- 39.Jenner E.A., Fletcher B.C., Watson P., Jones F., Miller L., Scott G. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J. Hosp. Infect. 2006;63(4):418–422. doi: 10.1016/j.jhin.2006.03.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material