Abstract
Objectives:
Aberrant automated blood pressure readings during Caesarean Delivery (CD) may lead to disruptions in monitoring. The present study compared the frequency of aberrant blood pressure (BP) readings across two types of commercially available blood pressure monitoring systems in use during Caesarean Delivery.
Methods:
This was a retrospective observational study using two comparable patient cohorts that resulted from simultaneous introduction of two types of monitors into a single obstetric surgical center in which similar patients were treated for the same surgical procedure by the same set of clinicians during the same year. Our primary hypothesis was that aberrant readings were significantly associated with the type of monitor being used for blood pressure measurement, controlling for a variety of relevant covariates as specified in the analytic plan
Results:
A total of 1418 Cesarean Delivery (CD) patients met inclusion criteria. Gaps of at least 6 minutes in machine-captured BP readings occurred in 159 (21.1%) of cases done in the Operating Room (OR) using a Datex-Ohmeda monitor vs 183 (27.5%) of cases in the ORs using Phillips monitors (p=0.005). In multivariable logistic regression analysis, the relative odds of the occurrence of monitoring gaps was 35% higher in rooms with the Phillips BP monitors as compared to the Datex-Ohmeda monitor while controlling for pre-specified covariates (OR=1.35, 95% CI=1.04 – 1.74, p=0.02).
Conclusion:
The present analysis suggests that aberrant BP readings for parturients undergoing CD are significantly different between the two types of automated BP monitoring systems used in the ORs at our institution.
Keywords: Blood pressure, Artifact Detection, Shivering, Monitoring Gaps, Cesarean Delivery
Introduction:
Practice standards from major professional organizations mandate that arterial blood pressure (BP) should be measured at least every five minutes during the intraoperative phase of care.[1] Because blood pressure measurement is a critical aspect of anesthetic vital sign monitoring, it is important that monitors designed to measure BP should be resistant to potential artifacts from sources including shivering or other commonly encountered sources of interference that may occur during routine patient care. Presently available automated, non-invasive oscillometric blood pressure (NIBP) monitors rely on proprietary algorithms to infer systolic and diastolic blood pressures, and there is very little published research comparing reliability of these commercially available systems[2] in the context of routine intraoperative care of parturients during Caesarean Delivery, a population particularly prone to shivering artifacts.[3] Nevertheless, automated monitors have compared favorably with manual sphygmomanometry in the office setting.[4]
After renovations at our tertiary care hospital during the late summer of 2018, three adjacent obstetric surgical suites (ORs) were equipped with two different brands of automated NIBP monitors. One OR was equipped with a Datex-Ohmeda S5 Anesthesia Physiologic Monitoring system utilizing Welch Allyn Non-Invasive Blood Pressure (NIBP) cuffs, and two ORs were equipped with a Philips Intellivue MX800 NIBP monitoring system with Phillips NIBP cuffs. Both NIBP monitors are included in monitoring systems that are regulated by FDA and approved for use in humans. In August of 2019, approximately one year after the installation had been completed, providers suggested that they had observed a higher prevalence of unreadable or otherwise aberrant NIBP readings in the context of patients undergoing anesthetics for Caesarean Delivery (CD) when these procedures took place in the rooms with the Phillips system as compared to the adjacent room with the Datex-Ohmeda system. Company representatives were consulted regarding these possible aberrancies and confirmed that the monitors were not physically defective. While the subjective experience of providers was taken seriously, the extent of differences in aberrant BP between the two systems in adjacent rooms was anecdotal without quantitative documentation. In response, we undertook, and herein report, an analysis of the prevalence of significant NIBP gaps in measurement and other likely blood pressure artifacts as encountered during CD with the use of these two monitoring systems.
Methods:
This retrospective observational study was conducted using data from our local perioperative research and quality data repository with waiver of consent under an approved IRB protocol most recently renewed on April 15, 2019 (HIC#1206010438). The repository also forms the local dataset for our site participation in the Multicenter Perioperative Outcomes Group (MPOG) consortium. The MPOG data collection methods have been previously described (see www.mpog.org).[5–7] The process includes automated collection of all machine-captured intraoperative blood pressures into a dedicated local perioperative data repository. This repository undergoes quality control common across MPOG centers and includes local case by case validation of a random sample of cases by subject-matter experts on a monthly basis. The same local repository has been used in the production of several multicenter peer reviewed manuscripts. [8–10] The analytic plan for the present analysis was publicly registered on the website of the Open Science Framework (url:https://osf.io/2t9u6) on September 11, 2019, with addition of baseline temperature as an important covariate following publication of the initial protocol. The manuscript was prepared in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.[11]
The present analysis sought to take advantage of the similar patient cohorts that resulted from simultaneous introduction of the two types of monitors into a single obstetric surgical center in which comparable patients were treated for the same surgical procedure by the same set of clinicians during the same time period. Our primary hypothesis was that aberrant readings were significantly associated with the type of monitor being used for NIBP measurement, controlling for a variety of relevant covariates as specified in the a priori analytic plan as described below.
Inclusion criteria consisted of all Caesarean Deliveries contained in our perioperative database that occurred at the study institution in the 3 relevant operating rooms from 9/6/18 through 9/5/2019. Data collected included all machine-captured NIBP measurements occurring between “anesthesia release” time and “procedure ending” time – two structured fields collected on every OR case in the Electronic Health Record at our institution. No applicable cases were excluded.
The primary endpoint was the prevalence of cases in which a BP monitoring gap occurred, defined as a gap between machine-captured NIBP readings of greater than six minutes. The six minute timeframe represents 3-times the typical two-minute interval for automated NIBP cuff reading that is the customary machine setting in these operating rooms. Six minutes also exceeds the maximum interval for intraoperative arterial BP measurement as stated by the ASA. While there is no agreed standard for the acceptable number of aberrant readings, the present study focused on the comparative reliability of the two systems in place. Alternative definitions of aberrant or unusually high NIBP readings were also considered and then combined to determine the prevalence of cases in which any of the following occurred: a) any gap of more than 6 minutes in duration, b) any unusually high NIBP reading > 160mmHg systolic or > 100 diastolic, or c) a low pulse pressure wherein the difference between the systolic and diastolic blood pressures was ≤ 20mmHg. Finally, a secondary endpoint was defined as the number of > 6 minutes gaps per hour of case-time occurring across the two types of monitoring systems.
In order to assess the validity of this pseudo-randomized natural experiment, we performed an analysis of patient characteristics between the OR suites containing the two alternative monitors. Specifically, we planned a priori to compare the following variables to understand potential covariate balance: Age, ASA Physical Status, BMI (calculated as the weight in kilograms divided by the square of the height in meters), Case Duration between “anesthesia release” through the event “procedure ending”, Oxytocin use, the Use of Other Uterotonics (methylergonovine, carboprost, misoprostol), Estimated Blood Loss, Type of Anesthesia (General vs. regional), ASA PS Emergency Modifier, and Baseline Temperature.
After univariate comparisons of the endpoints and an assessment of covariate balance above, we planned for a multivariable logistic regression analyses to be conducted, including the above putative confounders as independent variables in the analysis of the binary primary endpoints.
Sample Size Justification:
For the primary analysis, we estimated that a sample size of 1000 (500 in each group) would be sufficient to have 80% power to detect a difference in the primary outcome of 15% vs. 22% at an alpha of 0.05.
Results:
A total of 1418 Caesarean Delivery patients met inclusion criteria. The mean (SD) age in years was 32.4 (5.4) with no significant difference in age between the two groups (32.7 (5.4) in the Datex-Ohmeda room vs. 32.2 (5.5) years in the Phillips rooms). Mean procedure time was 67.1 (26.7) minutes and again did not differ significantly between the two room types (66.2 (24.5) vs. 68.1 (28.9), respectively; p=0.18). Due to a higher than expected rate of missing values of patient height, BMI was unable to be calculated for 27% of the cohort, was more frequently missing from the Phillips group, and was excluded from analyses. Similarly, estimated blood loss was missing from 14% of the cohort and was excluded. The proportion of patients with missing values for estimated blood loss was not significantly different between the two groups. Finally, the ASA Physical Status Emergency modifier was poorly penetrant (with only one case), so this was also eliminated from the multivariable analysis with retention of General Anesthesia vs. Spinal Anesthesia as a highly correlated replacement for emergency status.
As expected, most CD cases were performed under neuraxial anesthesia which is commonly associated with patient shivering. Standard protocols in the present cohort included the use of underbody forced warm air devices and warm blankets placed over the patients’ arms and chest.
In univariate analyses, the majority of other covariates were well-balanced or showed clinically trivial differences between the two monitoring groups. Although over 98% of the cohort was classified as ASA Physical Status 2 or 3, the number of ASA 2 vs. 3 was different between the two BP groups. Also, uterotonics other than oxytocin were less frequently used in the Datex-Ohmeda OR vs the Phillips ORs (10.6% vs.15.6% of cases, p=0.005). Finally, patients’ baseline temperatures were warmer by 0.2 degrees in the Phillips ORs (97.9 vs. 98.1 F; p<0.001). A comparison of all univariate predictors between the two monitor types is listed in Table 1.
Table 1:
Description of cohort characteristics for patients undergoing Caesarean Delivery in Operating Rooms with the two types of monitors.
| Variable | OR 1 (Datex-Ohmeda) N=753 | OR 2 and 3 (Phillips) N=665 | Total N=1418 | |
|---|---|---|---|---|
| Age (years) | Mean (SD) | 32.7 (5.4) | 32.2 (5.5) | 32.4 (5.4) |
| BMI (kg/m2) | Mean (SD) | 34.5 (7.4) | 34.6 (7.0) | 34.5 (7.3) |
| N (N Missing) | 603 (150) | 436 (229) | 1039 (379) | |
| Temperature (F) | Mean (SD) | 97.9 (0.6) | 98.1 (0.7) | 98.0 (0.6) |
| N (N Missing) | 723 (30) | 633 (32) | 1356 (62) | |
| Procedure Time (minutes) | Mean (SD) | 66.2 (24.5) | 68.1 (28.9) | 67.1 (26.7) |
| Estimated Blood Loss (mL) | Mean (SD) | 772.2 (368.6) | 794.0 (370.0) | 782.4 (369.3) |
| N (N Missing) | 648 (105) | 571 (94) | 1219 (199) | |
| General Anesthesia | No | 725 (96.3%) | 626 (94.1%) | 1351 (95.3%) |
| Yes | 28 (3.7%) | 39 (5.9%) | 67 (4.7%) | |
| ASA Physical Status | 1 | 2 (0.37%) | 1 (0.2%) | 3 (0.2%) |
| 2 | 556 (73.8%) | 436 (65.6%) | 992 (70.0%) | |
| 3 | 187 (24.8%) | 224 (33.7%) | 411 (29.0%) | |
| 4 | 8 (1.1%) | 4 (0.6%) | 12 (0.9%) | |
| ASA Physical Status Emergency Modifer | No | 752 (99.9%) | 665 (100.0%) | 1417 (99.9%) |
| Yes | 1 (0.1%) | 0 (0.0%) | 1 (0.1%) | |
| Oxytocin Administration | No | 514 (68.3%) | 462 (69.5%) | 976 (68.8%) |
| Yes | 239 (31.7%) | 203 (30.5%) | 442 (31.2%) | |
| Uterotonic other than Oxytocin | No | 673 (89.4%) | 561 (84.4%) | 1234 (87.0%) |
| Yes | 80 (10.6%) | 104 (15.6%) | 184 (13.0%) |
For the primary analysis, gaps of at least 6 minutes in machine-captured BP readings occurred in 159 (21.1%) of cases done in the Datex-Ohmeda location vs 183 (27.5%) of cases using the Phillips monitor (see Table 2). This difference represented a 29.7% relative increase in the likelihood of a monitoring gap in the latter group and also demonstrated statistical significance (p=0.005).
Table 2:
Univariate comparison of outcomes between the two monitor types:
| Univariate Outcomes: | OR 1 (Datex-Ohmeda) N=753 | OR 2 and 3 (Phillips) N=665 | Total N=1418 | P-value For Difference | |
|---|---|---|---|---|---|
| BP GAP > 6 Minutes | No | 594 (78.9%) | 482 (72.5%) | 1076 (75.9%) | 0.005 |
| Yes | 159 (21.1%) | 183 (27.5%) | 342 (24.1%) | ||
| Systolic >160 or Diastolic>100 | No | 414 (55.0%) | 283 (42.6%) | 697 (49.2%) | <0.001 |
| Yes | 339 (45.0%) | 382 (57.4%) | 721 (50.9%) | ||
| Pulse Pressure <= 20 mmHg | No | 460 (61.1%) | 332 (49.9%) | 792 (55.9%) | <0.001 |
| Yes | 293 (38.9%) | 333 (50.1%) | 626 (44.2%) |
Using our a priori alternative definition of aberrant or unusually high BP readings described above, at least one such aberrant reading occurred more often in the Phillips cases vs. the Datex-Ohmeda cases (526 (68.5%) of Datex-Ohmeda cases vs. 525 (79.0%) of Phillips cases, p<0.0001).
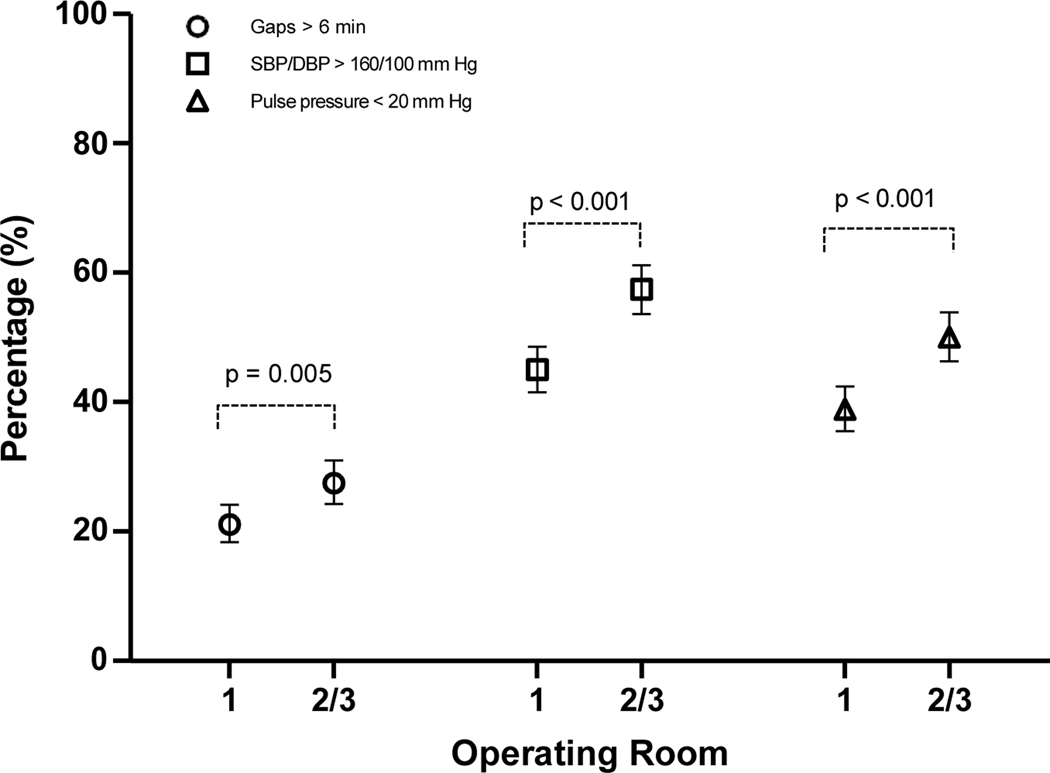
When divided into the three individual types of BP aberrancy or unusually high readings that were analyzed, a similar result was seen regardless of type of artifact. Comparing the Datex-Ohmeda vs. Phillips BP monitoring sites, systolic BP > 160mmHg or diastolic BP >100mmHg were encountered in 339 (45.0%) of Datex-Ohmeda cases vs. 382 (57.4%) of Phillips cases; p<0.001). Low pulse pressures of less than 20mmHg difference between SBP and DBP occurred in 293 (38.9%) of Datex-Ohmeda cases and 333 (50.1%) of Phillips cases; p<0.001). See Figure 1 for pairwise analyses of each type of BP aberrancy.
Figure 1:
Comparison of prevalence of three types of likely aberrant Blood Pressure readings. (OR 1 had a Datex-Ohmeda S5 Monitor and ORs 2 and 3 had a Phillips Intellivue MX800 Monitor System.)
In the pre-specified secondary analysis of number of gaps in BP measurement per hour of case between the two types of monitors, once again the Datex-Ohmeda location demonstrated fewer time-adjusted gaps than the Phillips locations (Wilcoxon Rank Sum Test mean ranks were 687 vs 735; p for difference =0.003).
Following the above univariate analyses, we performed a multivariable logistic regression analysis to measure the odds of at least one 6-minute BP monitoring gap occurring in a case while controlling for the following covariates: patient age, procedure time, preoperative temperature, ASA PS (1–2 vs 3–4), use of a uterotonic other than oxytocin, use of oxytocin, and general vs. neuraxial anesthesia. This multivariable logistic analysis demonstrated that the relative odds of the occurrence of monitoring gaps was 35% higher in rooms with the Phillips BP monitors as compared to the Datex-Ohmeda monitor while controlling for the above covariates (OR=1.35, 95% CI=1.04 – 1.74, p=0.02). (See Table 3)
Table 3:
Multivariable Logistic Regression Results Demonstrating Adjusted Odds of at Least One 6-minute Gap in BP Readings.
| Variables | Odds Ratio (95% CI) | P-value |
|---|---|---|
| Phillips OR vs Datex-Ohmeda OR | 1.349 (1.044 – 1.743) | 0.02 |
| Age, years | 0.989 (0.966 – 1.013) | 0.38 |
| Procedure Time, min | 1.01 (1.005 – 1.014) | <.0001 |
| Temperature | 0.972 (0.795 – 1.188) | 0.78 |
| ASA, (3–4 vs 1–2) | 1.261 (0.961 – 1.656) | 0.095 |
| Uterotonic Other than Oxytocin, (Yes vs No) | 1.54 (1.085 – 2.186) | 0.016 |
| Oxytocin status, (Yes vs. No). | 1.178 (0.9 – 1.544) | 0.23 |
| General Anesthesia, (Yes vs No) | 0.629 (0.328 – 1.205) | 0.16 |
As a sensitivity analysis, we sought to investigate when in the course of the anesthetics the suspected aberrancies were occurring. If indeed, providers were correct that shivering artifact was a major contributor, it would be expected that such artifacts would be associated with the first third of the anesthetic period, a time in which induction of spinal anesthesia is achieved or during which the conversion from epidural analgesia to anesthesia after failed vaginal delivery occurs.. Accordingly, each case was divided into three equal epochs, and the distribution of each type of suspected aberrancy was examined. The post hoc analysis demonstrated that the majority of each type of aberrancy in both types of rooms indeed occurred during the first of the three epochs (see Table 4).
Table 4:
Timing of aberrancies in regard to when they occurred during cases.
| Blood Pressure Aberrancy By Epoch | ||
|---|---|---|
| OR 1 | OR 2 & 3 | |
| N (%) | N (%) | |
| >6 Minute Gap | ||
| First Epoch | 165 (66.3) | 217 (58.8) |
| Second Epoch | 13 (5.2) | 33 (8.9) |
| Third Epoch | 71 (28.5) | 119 (32.2) |
| Low Pulse Pressure | ||
| First Epoch | 396 (54.2%) | 471 (50.2%) |
| Second Epoch | 106 (14.5%) | 132 (14.1%) |
| Third Epoch | 229 (31.3%) | 335 (35.7%) |
| Systolic >160mmHg or Diastolic > 100mmHg | ||
| First Epoch | 689 (52.2) | 858 (52.0) |
| Second Epoch | 201 (15.2) | 283 (17.2) |
| Third Epoch | 430 (32.6) | 508 (30.8) |
Discussion:
The present study provides quantitative evidence in support of practitioners’ impressions that aberrant BP readings were obtained in a higher proportion of cases in obstetric ORs where Phillips monitors were utilized as compared to a Datex-Ohmeda monitor. The historical use of two monitoring systems in adjacent ORs allowed the dataset used for this analysis to result in highly similar cohorts[12] and thus may provide a level of credence that may not exist in other types of retrospective observational studies.[13] Other strengths include public registration and adherence to a published analytic plan,[14] after accounting for high missingness of two covariates. One limitation of this study includes the possibility that results may have been distorted by differences in the accuracy of provider intraoperative charting. For example, given the care patterns in place at our institution, we suspect that a higher number of parturients were administered exogenous oxytocin than was charted in our dataset. However, we note with reassurance that the lack of oxytocin charting was essentially identical across the room types, suggesting that any misclassification of this covariate would have been non-differential between patient groups. Given that oxytocin administration did not appear to be significantly associated with the primary outcome, we suggest that significant distortion in conclusions regarding the primary outcome analysis are unlikely to have resulted from mischarting oxytocin administration. Further, we emphasize as a particular strength of this study that the primary outcome that depended on BP measurements was a machine-captured variable automatically captured into our dataset and not prone to provider charting inaccuracies.
Although the strength of our approach to identify highly similar historical cohorts is notable, we continue to emphasize that the data described herein remain fundamentally retrospective and observational in nature, and thus the observed association between aberrant BP readings and rooms where one type of monitor was used as compared to another cannot establish causation. Due to its retrospective nature, the data were subject to a variety of missing variables, including nondifferential missingness of BMI from the two groups. Moreover, the present study was not designed to establish the underlying source within either monitor for the observed differences in artefactual BP readings. While speculative, several practitioners at our hospital have suggested that the aberrant readings are often seen in the context of shivering patients, a common occurrence among parturients receiving neuraxial anaesthetics for CD that has received substantial attention in the anesthesia literature.[3, 15] This suspicion is consistent with the finding that the majority of aberrancies occurred during the first third of the anesthetic, a time when shivering would typically be most common. If the suggested connection of aberrant BP readings with the occurrence of shivering is correct, improved accommodation of shivering into the automated algorithms of commercial BP monitors should be an important target for future quality improvement of these devices.
Beyond our primary analyses, we wish to note two further interesting observations from our dataset. First, it is notable that across all three ORs in this study, providers saw monitoring gaps of at least 6 minutes in many cases. Even the “best” room still saw more than one in five cases include at least one monitoring gap, suggesting that both types of monitors examined in this study may benefit from improvements in their algorithms to improve dependability and accuracy. The further observation that the timing of the majority of these aberrancies occurred in the first third of the anesthetic further highlights their potential importance. At the very time when instability is most common and during which placental blood flow remains critical for fetal outcomes, the monitors on which practitioners are depending were observed to fail with alarming frequency.
Second, of the three types of likely aberrant readings that we included in our analysis, the largest difference between the monitors in relative terms was in the proportion of cases where at least one reading showed a pulse pressures less than 20mmHg. The absolute difference in this type of aberrancy between the two types of BP monitors was 11.2% of cases. This difference would suggest that for every nine cases taking place in an OR equipped with the Datex-Ohmeda monitor as compared to the Phillips monitor, one fewer case would experience an automated BP reading containing a pulse pressure <20mmHg. We believe this observation suggests the existence of a clinically relevant difference between the two automated BP systems that deserves dedicated prospective study as well as further validation in multicenter observational cohorts.
In conclusion, the present study suggests that aberrant BP readings for parturients undergoing CD are significantly different between the two types of automated BP monitoring systems that were used in the ORs at our institution.
Acknowledgments
Funding: Dr. Feng Dai who contributed to the analysis of the present manuscript is supported in part by CTSA Grant Number UL1RR024139 from the National Center for Research Resources and the National Center for Advancing Translational Science, components of the National Institutes of Health (NIH). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or the United States government.
Footnotes
Conflicts of Interest: Dr. Schonberger reports holding common stock in Johnson & Johnson, a publicly traded diversified manufacturer of healthcare products. Yale University receives funding from Merck, Inc. for a study unrelated to the present manuscript on which Drs. Bardia and Schonberger are principle investigator and co-investigator, respectively. No other authors report competing interests.
References:
- [1].STANDARDS FOR BASIC ANESTHETIC MONITORING; American Society of Anesthesiologists Committee on Practice Parameters. 2015. [Google Scholar]
- [2].Gerin W, Schwartz AR, Schwartz JE, Pickering TG, Davidson KW, Bress J, et al. Limitations of current validation protocols for home blood pressure monitors for individual patients. Blood Pressure Monitoring. 2002;7:313–8. [DOI] [PubMed] [Google Scholar]
- [3].Crowley LJ, Buggy DJ. Shivering and neuraxial anesthesia. Regional Anesthesia & Pain Medicine. 2008;33:241–52. [DOI] [PubMed] [Google Scholar]
- [4].Roerecke M, Kaczorowski J, Myers MG. Comparing Automated Office Blood Pressure Readings With Other Methods of Blood Pressure Measurement for Identifying Patients With Possible Hypertension: A Systematic Review and Meta-analysis. JAMA Internal Medicine. 2019;179:351–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Colquhoun DA, Shanks AM, Kapeles SR, Shah N, Saager L, Vaughn MT, et al. Considerations for Integration of Perioperative Electronic Health Records Across Institutions for Research and Quality Improvement: The Approach Taken by the Multicenter Perioperative Outcomes Group. Anesth Analg. 2020;130:1133–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kheterpal S. Clinical research using an information system: the multicenter perioperative outcomes group. Anesthesiology Clinics. 2011;29:377–88. [DOI] [PubMed] [Google Scholar]
- [7].Mathis MR, Dubovoy TZ, Caldwell MD, Engoren MC. Making Sense of Big Data to Improve Perioperative Care: Learning Health Systems and the Multicenter Perioperative Outcomes Group. J Cardiothorac Vasc Anesth. 2020;34:582–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kheterpal S, Vaughn MT, Dubovoy TZ, Shah NJ, Bash LD, Colquhoun DA, et al. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER): A Multicenter Matched Cohort Analysis. Anesthesiology. 2020;132:1371–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Larach MG, Klumpner TT, Brandom BW, Vaughn MT, Belani KG, Herlich A, et al. Succinylcholine Use and Dantrolene Availability for Malignant Hyperthermia Treatment: Database Analyses and Systematic Review. Anesthesiology. 2019;130:41–54. [DOI] [PubMed] [Google Scholar]
- [10].Lee LO, Bateman BT, Kheterpal S, Klumpner TT, Housey M, Aziz MF, et al. Risk of Epidural Hematoma after Neuraxial Techniques in Thrombocytopenic Parturients: A Report from the Multicenter Perioperative Outcomes Group. Anesthesiology. 2017;126:1053–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Vandenbroucke JP, Elm Ev, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Annals of Internal Medicine. 2007;147:W-163-W-94. [DOI] [PubMed] [Google Scholar]
- [12].Schonberger RB, Dutton RP, Dai F. Is There Evidence for Systematic Upcoding of ASA Physical Status Coincident with Payer Incentives? A Regression Discontinuity Analysis of the National Anesthesia Clinical Outcomes Registry. Anesth Analg. 2016;122:243–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Schonberger RB, Gilbertsen T, Dai F. The problem of controlling for imperfectly measured confounders on dissimilar populations: a database simulation study. J Cardiothorac Vasc Anesth. 2014;28:247–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kharasch ED. Observations and Observational Research. Anesthesiology. 2019;131:1–4. [DOI] [PubMed] [Google Scholar]
- [15].Saito T, Sessler DI, Fujita K, Ooi Y, Jeffrey R. Thermoregulatory effects of spinal and epidural anesthesia during cesarean delivery. Regional Anesthesia & Pain Medicine. 1998;23:418–23. [DOI] [PubMed] [Google Scholar]