Abstract
Background:
Cardiovascular complications of the coronavirus disease 2019 (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2), have been documented both in the acute phase and in convalescence. One such complication is the formation of the left ventricular (LV) thrombus. There is a lack of clarity regarding the incidence, risk factors, and management of this complication.
Aim:
The aim of the study is to identify the clinical presentation, risk factors and outcome of COVID-19 patients with left ventricular thrombus (LVT).
Methods:
A literature search was conducted to identify all case reports of COVID-19 with LVT in PubMed/Medline, Embase, Web of Science, and Google Scholar.
Results:
Among the 65 patients identified, 60 had LVT, either at admission, or during the acute phase of the illness. Six patients with mild symptoms during the acute phase of viral illness had only the COVID-19 antibody test positivity at the time LV thrombus was detected. Few of the patients (23.1%) had no comorbidities. The mean age of the patients was 52.8 years, and the youngest patient was 4 years old. This suggests that LVT formation can occur in young COVID-19 patients with no co-morbid conditions. Most of the patients (69.2%) had more than one site of thrombosis. A mortality rate of 23.1% was observed in our review, and ST-elevation myocardial infarction (STEMI) was diagnosed in 33.3% of those who died.
Conclusions:
A high degree of suspicion for LVT must be maintained in patients with known cardiac disease and those with new-onset arterial or venous thromboembolism, and such patients may benefit from a screening echocardiography at admission.
Relevance for Patients:
The patients with preexisting cardiovascular disease must take added precautions to prevent acquiring COVID-19 infection as there is a higher risk of developing LV thrombus. In patients who develop LVT in COVID-19, mortality rate is higher.
Keywords: coronavirus disease 2019, severe acute respiratory syndrome, coronavirus 2, coronavirus, left ventricular thrombus, acute coronary syndrome, thrombosis, thromboembolism, echocardiogram
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or the novel coronavirus-2019 (nCoV-19), which was identified from Wuhan, China, is responsible for the coronavirus disease 2019 (COVID-19), which has caused nearly 4.3 million deaths worldwide. According to a meta-analysis from China, pre-existing cardiovascular disease is a predisposing factor for higher morbidity and mortality in COVID-19 [1]. Although acute respiratory failure and sepsis have been reported as the leading causes of death in COVID-19, direct and indirect cardiovascular complications such as myocardial injury, arrhythmia, acute coronary syndrome, and thromboembolism may also mortality. The mechanism of cardiac injury in COVID-19 may be ischemic or non-ischemic [2]. Thromboembolic complications are increasingly being reported as a complication of COVID-19 infection. The activation of endothelial cells by viral particles is thought to be the primary mechanism for thrombus development. The incidence of thrombosis in hospitalized non-critically ill patients is approximately 2.6% and is higher in critically ill patients (35.3%) [3]. During the pandemic the incidence of left ventricular thrombus (LVT) among patients presenting with myocardial infarction, it has reportedly increased [4]. This review aims to study the clinical presentations, risk factors, and outcomes of patients with COVID-19 who had presented with an LVT.
2. Methods
2.1. Eligibility criteria
This study included all patients with COVID-19 with LVT during any stage of illness. Case reports, mini-reports, and case series with individual patient details were pooled to assess clinical manifestations, imaging features, laboratory investigations, and outcomes. The diagnosis of COVID-19 was based on microbiological, radiology or serological tests.
2.2. Selection strategy
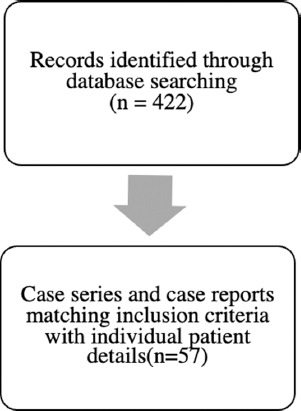
This review included articles on COVID-19 and LVT published in PubMed, Medline, Embase, Web of Science, and Google scholar till 16th August 2021. The search terms used in the MeSH database, Web of science research assistant and Embase search were ‘“COVID-19” and “LVT”, “2019 nCoV” and “LVT”, and “SARS-CoV-2” and “LVT. In Google scholar, the terms “COVID-19 and LVT” were used and articles were sorted by relevance from 2019 onward. A total of 422 articles were identified. After eliminating duplicate articles, non-English articles and case reports with intracardiac thrombus at sites other than the left ventricle, a total of 62 articles (both case series and case reports) were identified. Five articles were eliminated because the diagnosis of COVID-19 could not be made with certainty. Authors were contacted to clarify aspects of the case reports that were vague. Full text was available for all 57 mansucripts that were finally included in the review. Data from all case reports and case series were pooled and analyzed. The findings of this analysis were compared to the other studies reported in the literature (Figure 1). Two independent clinicians were involved in the screening of the articles.
Figure 1. PRISMA flow chart of search.
3. Results
Case reports and case series of a total of 65 COVID-19 patients with LVT were identified. Among them, 66.2% were male and the mean age was 52.8 years. Most of the cases were reported from the United States of America (USA).
3.1. Clinical features
The diagnosis of COVID-19 was made by reverse transcriptase-polymerase chain reaction (RT-PCR) of nasopharyngeal swab in 35 patients (53.8%), PCR of myocardial biopsy sample in one patient (1.5%), SARS CoV2 antibodies in six patients (9.2%), SARS CoV-2 rapid antigen test in one (1.5%) and computed tomography (CT) of the thorax in two patients (3.1%). The initial presenting symptom was dyspnea in 42 patients (64.6%), fever in 29 (44.6%), cough in 29 (44.6%), chest pain in 16 patients (24.6%), gastrointestinal symptoms such as vomiting and diarrhoea in six patients (9.2%), and neurological deficits in seven (10.7%). Twenty patients (30.8%) presented with hypoxia, one of whom was in shock, and COVID-19 pneumonia was present in 44 patients (67.7%). In 20 patients (30.8%), the mode of diagnosis of COVID-19 was not specified. The diagnosis of LVT was made at the time of admission in 37 patients (56.9%). Among the rest, LVT was detected between days one and 30 of hospital admission.
3.2. Risk factors
The most common comorbidity seen was pre-existing heart disease which was present in 14 (21.5%) patients, wherein chronic heart failure with reduced ejection fraction and pre-existing coronary artery disease was observed in eight (12.3%) and six (9.2%) patients, respectively. Diabetes mellitus, hypertension, dyslipidemia, obesity, and obstructive airway disease were seen in eleven (16.9%), nine (13.8%), six (9.2%), four (6.1%), and eight (12.3%) patients, respectively. Fifteen patients (23.1%) had no comorbidities, and in eight patients (12.3%) comorbidities were not reported.
3.3. Lab reports and imaging
C-reactive protein (CRP) was reported in 29 patients (44.6%) and was elevated (>10 mg/L) in 27 of them (41.5%). Troponin was reported in 34 patients (52.3%) at admission and was elevated (>0.14 μg/L) in 22 (33.8%). D-dimer was elevated (>500 ng/ml fibrinogen equivalent units) in 29 (44.6%) of the 35 patients for whom it was reported, and 23 patients (35.4%) had elevated brain natriuretic peptide.
Electrocardiogram (ECG) was reported in 39 patients (60%). Fourteen of them (21.5%) had ST-segment changes at admission (Table 1). Nineteen of them (29.2%) underwent coronary angiography (CAG), seven of whom (10.8%) had thrombi in either the right coronary artery or left anterior descending artery. Lung involvement by COVID-19 was present in 45 patients (69.2%), which was demonstrated by either chest roentgenogram (X-ray), or CT thorax, or both. CT pulmonary angiogram showed pulmonary embolism in 11 patients (16.9%), four of whom had right ventricular thrombus as well. One patient had the presence of inferior vena caval, renal, and iliac vessel thrombosis [5]. The presence of LVT was identified by 2D echocardiogram in 40 patients (61.5%), CT thorax in twelve patients (18.5%), cardiac magnetic resonance imaging (MRI) in nine patients (13.8%), and ventriculography in one patient (1.5%). Apical thrombus was present in 36 patients (55.4%), while the site of thrombus was not specified in 29 patients. Eight patients (12.3%) had ventricular aneurysms, and five had biventricular thrombi (7.7%). LV dysfunction and reduced ejection fraction were noted in 44 patients (67.7%).
Table 1. Summary of laboratory findings in COVID-19 patients with the left ventricular thrombus.
| Reference | BNP (ng/ml) | CRP (mg/L) | Troponin T (mcg/L) | D-dimer (ng/ml) | |
|---|---|---|---|---|---|
| 1 | Mahdavi [57] | 8827 | No data | No data | No data |
| 2 | Bigdelian [58] | No data | 11 | No data | 2000 |
| 3 | Bigdelian [58] | No data | 29 | No data | 490 |
| 4 | Materna [59] | Elevated | Elevated | Elevated | Elevated |
| 5 | Schroder [60] | 17950 | 301 | 2.18 | 3800 |
| 6 | Munoz [61] | 34 | No data | 0.12 | 390 |
| 7 | Agarwal [62] | 5166 | Normal | 1.326 | 2630 |
| 8 | Iguina [8] | 1000 | No data | 0.34 | 856 |
| 9 | Hodson [62] | No data | No data | No data | No data |
| 10 | Capaccione [64] | No data | No data | No data | 500 |
| 11 | Ranard [64] | 315 | 5.96 | 0.386 | 500 |
| 12 | Kihira [66] | No data | No data | No data | 700 |
| 13 | Ziaie [11] | 23000 | 103 | No data | 1350000 |
| 14 | Amin [67] | No data | No data | No data | No data |
| 15 | El Aidouni [68] | No data | 114 | 0.1 | No data |
| 16 | Paolo Rubartelli [69] | 1702 | No data | 0.116 | 5004 |
| 17 | Jadhav [70] | No data | No data | No data | No data |
| 18 | Jariwala [71] | No data | No data | Elevated | 2322 |
| 19 | Hammam [72] | 2215 | 147 | 0.734 | 3.4 |
| 20 | Ceci Bonello [73] | No data | 115 | 0.504 | 5483 |
| 21 | Garg [74] | No data | 118 | 0.91 | 8100 |
| 22 | Hudowenz [75] | 12,232 | 130 | 3.264 | No data |
| 23 | Jadhav [70] | 5080 | No data | 1.81 | No data |
| 24 | Mitevska [9] | 6700 | 45 | No data | No data |
| 25 | Venkataraman Pranav [76] | No data | 50 | 0.181 | No data |
| 26 | Alizadehasl [787] | No data | No data | No data | No data |
| 27 | Sharma [78] | No data | 374 | 2.54 | No data |
| 28 | Ramalho [79] | 30.39 | 641 | 0.628 | No data |
| 29 | Gravinay [80] | 900 | 270 | 2900 | |
| 30 | Ford [81] | 588 | No data | 0.066 | No data |
| 31 | Jariwala [71] | No data | No data | No data | 7809 |
| 32 | Servato [82] | l7460 | 123.5 | low | low |
| 33 | Jeon [5] | No data | No data | No data | No data |
| 34 | Imaeda [83] | 683.4 | 22.9 | 0.028 | 3000 |
| 35 | Malaweera [84] | No data | No data | No data | 7480 |
| 36 | Jariwala [85] | No data | No data | No data | 6548 |
| 37 | Zheng [86] | 11,463 | No data | 0.05 | na |
| 38 | Ferguson [10] | No data | 405 | No data | 508 |
| 39 | John [87] | No data | No data | 0.01 | 629 |
| 40 | Ozer [88] | 34824 | 197 | 0.05 | 20000 |
| 41 | Farouji [89] | 517 | 144 | negative | 64,000 |
| 42 | Tadayoni [90] | No data | No data | No data | No data |
| 43 | Byer [91] | No data | No data | No data | No data |
| 44 | Soltani [92] | No data | No data | 937 | No data |
| 45 | M Ignaszewski [93] | No data | No data | No data | No data |
| 46 | Jadhav [70] | No data | No data | No data | No data |
| 47 | Jadhav [70] | No data | No data | No data | No data |
| 48 | Iqbal Phool [94] | No data | 170.4 | 0.189 | 3370 |
| 49 | Jariwala [721] | No data | No data | Elevated | 4566 |
| 50 | Singh [95] | No data | No data | No data | 4558 |
| 51 | Castro [96] | No data | 164 | No data | No data |
| 52 | Mandal [97] | No data | 54 | No data | No data |
| 53 | Calvi [91] | No data | No data | No data | No data |
| 54 | Nanthatanti [98] | No data | No data | No data | 1548 |
| 55 | Azhar [99] | >20000 | No data | 0.04 | No data |
| 58 | Meriem Boui [100] | No data | 115 | 2.45 | 11200 |
| 57 | Gozgec [101] | No data | No data | No data | No data |
| 58 | Bernardi [7] | 8999 | 14.2 | 0.775 | 2931 |
| 59 | Calvi [91] | No data | No data | No data | 2931 |
| 60 | Furtney Joshua [102] | No data | No data | No data | No data |
| 61 | Alfaki [103] | 1830 | No data | 6.89 | >20.00 |
| 62 | Patell [6] | No data | No data | No data | No data |
| 63 | Sonaglioni [104] | >20,000 | 111 | 0.08 | 17,108 |
| 64 | Fenton [105] | No data | 412 | 0.354 | No data |
| 65 | Jariwala [71] | No data | No data | No data | 13453 |
BNP: Brain natriuretic peptide; CRP: C- reactive protein
3.4. Outcome
More than one site of thrombus formation was noted in 45 (69.2%) patients. Stroke was a complication in 14 patients (21.5%), acute coronary syndrome in 15 (23.1%), pulmonary embolism in 11 (16.9%), and peripheral arterial embolism in eight (12.3%) (Table 2). One patient had central retinal artery occlusion [6], and three had peripheral venous embolism (4.6%). Four patients (6.2%) had renal infarcts, among whom two had splenic infarction as well. Isolated splenic infarction was seen in two patients (3.1%). The cause of thrombosis could be attributed to an acute coronary event in 15 patients (23.1%). MRI confirmed viral myocarditis in eight patients (12.3%) and one patient developed takotsubo cardiomyopathy [7]. Thrombophilia workup showed anti-phosphatidyl serine antibodies in one patient [8], and the presence of heterozygous mutations for Factor V Leiden, prothrombin and PAI-1 antibodies in another [9] Heparin-induced thrombocytopenia (HIT) was suspected in one patient; however, antibodies were negative [10]. One patient who developed LVT was later diagnosed with hyper-eosinophilic syndrome [11]. Three patients (4.6%) with LVT had no previous or ongoing cardiac or coagulation abnormalities. All patients were treated with low molecular weight heparin, which was later modified to coumarins or novel oral anticoagulants. The overall mortality was 23.1%. Five of the 15 patients who died had ST-elevation on ECG, either during diagnosis or during the course of hospital admission. All patients who died were hypoxic at admission or immediately after. Among the 50 patients who survived, follow-up data was available for 30, all of whom had a decreased or complete dissolution of the thrombus. Five patients underwent thrombus extraction by either CAG guided thrombolysis with peripheral extraction, or surgical LV thrombectomy, and had no recurrence during follow-up.
Table 2. Outcomes of patients presenting with left ventricular thrombus.
| Outcome | n (%) |
|---|---|
| Myocardial infarction | 15 (23.1) |
| New onset heart failure | 16 (24.6) |
| Myocarditis | 8 (12.3) |
| Takotsubo cardiomyopathy | 1 (1.5) |
| Biventricular thrombus | 5 (7.7) |
| Cerebrovascular accident | 14 (21.5) |
| Peripheral arterial embolism | 8 (12.3) |
| Deep vein thrombosis | 5 (7.7) |
| Pulmonary embolism | 11 (16.9%) |
| Organ involvement | |
| Renal | 4 (6.2) |
| Splenic | 4 (6.2) |
| Hepatic | 1 (1.5) |
| Eye | 1 (1.5) |
4. Discussion
Among the underlying etiologies for LVT formation, the most common was dilated cardiomyopathy followed by myocardial infarction [12]. Both right and LVT formation have been reported in patients with COVID-19, with the latter being more common. A study conducted among 3334 hospitalized patients with COVID-19 in New York showed that the incidence of thrombotic complications was 16%, 11% of which were arterial thrombosis, and 6.2% were venous [13]. This is higher than what was observed during the influenza pandemic of 2009, when the overall incidence of thrombotic complications was 5.9% [14]. The risk of myocarditis was higher in COVID-19 when compared to influenza (Table 3) [15]. In a Danish nationwide study which followed-up COVID-19 cases, the incidence of myocardial infarction was 5 times higher in the 14 days following the diagnosis of COVID-19, compared to 180 days prior [16].
Table 3. Summary of case reports of patients with COVID-19 with the left ventricular thrombus.
| Reference | Age | Sex | Comorbidities | Diagnosis | Mode of diagnosis | Resolution of thrombus | |
|---|---|---|---|---|---|---|---|
| 1 | Mahdavi [57] | 4 | F | Nil | LV thrombus, myocarditis | MRI | Expired |
| 2 | Bigdelian [58] | 8 | F | Orthopedic surgery few weeks back | Biventricular thrombus, pulmonary embolism | Echo | Surgical thrombectomy |
| 3 | Bigdelian [58] | 11 | F | Nil | Biventricular thrombus | Echo | Surgical thrombectomy |
| 4 | Materna [59] | 17 | M | Nil | LV thrombus with CVA | Echo | Extracted, no recurrence. LV function normalized in 42 hrs |
| 5 | Schroder [60] | 17 | M | Nil | LV thrombus, MIS-C | Echo | 9 days |
| 6 | Munoz [61] | 18 | M | Nil | Myocarditis, LV thrombus | Echo followed by MRI | Non-compliant with treatment, persistent at several months |
| 7 | Agarwal [62] | 26 | M | Nil | Biventricular thrombus, non-obstructive MI, new onset heart failure | Echo followed by MRI | 12 days |
| 8 | Iguina [8] | 27 | F | DM, PCOS on OCP | LV thrombus with CVA and APS antibodies | Echo | Not known |
| 9 | Hodson [63] | 29 | M | asthma | Myopericarditis and LV thrombus | Echo followed by MRI | No data |
| 10 | Capaccione [64] | 35 | M | intermittent asthma, mild obesity | CVA, NSTEMI, LV thrombus | Echo | 6 days |
| 11 | Ranard [65] | 35 | M | asthma, obesity | CVA, NSTEMI, LV thrombus | Echo followed by MRI | Reduced size at 6 days |
| 12 | Kihira [66] | 37 | M | Nil | LV thrombus with CVA | Echo | Not known |
| 13 | Ziaie [11] | 39 | F | Asthma | LV thrombus with HES | Echo | 8 days |
| 14 | Amin [67] | 39 | F | Asthma | LV thrombus, myocarditis | Echo | 3 days |
| 15 | El Aidouni [68] | 40 | F | Psychosis | LV thrombus, DVT peripheral arterial embolism | Echo | Not known |
| 16 | Paolo Rubartelli [69] | 43 | M | HfrEF, EF=48 | Myocarditis, LV thrombus, pulmonary artery DVT, IVC thrombus, renal infarct | CT Angiogram followed by echo | More than 4 months |
| 17 | Jadhav [70] | 43 | M | Not known | IWMI, LV thrombus | Echo | Persistent thrombus at 20 days |
| 18 | Jariwala [71] | 45 | M | DM, smoker | LV thrombus with STEMI, homocysteinemia | Echo followed by MRI | 30 days |
| 19 | Hammam [72] | 47 | F | Nil | LV thrombus peripheral arterial thrombus, DVT | Echo | 30 days, LVEF improved to 30% |
| 20 | Ceci Bonello [73] | 47 | M | DM, DLP | LV thrombus with CVA, splenic, renal infarct, peripheral arterial infarcts | Echo | Surgical thrombectomy |
| 21 | Garg [74] | 48 | F | HTN | STEMI, LV thrombus, CVA | Echo | Expired |
| 22 | Hudowenz [75] | 48 | M | Asthma | Myocarditis, LV thrombus | MRI | 90 days |
| 23 | Jadhav [70] | 48 | F | DM, HTN | AWMI, LV thrombus | Echo | 15 days |
| 24 | Mitevska [9] | 48 | M | Nil | Biventricular thrombus, pulmonary embolism, DVT | Echo | Not known |
| 25 | Venkataraman Pranav [76] | 49 | M | No data | STEMI, LV thrombus | Echo | Not known |
| 26 | Alizadehasl [77] | 49 | F | Nil | LV thrombus | Echo | No details |
| 27 | Sharma [78] | 50 | M | DM, DLP in admission | STEMI, LV thrombus, peripheral arterial thrombus | Echo | Expired |
| 28 | Ramalho [79] | 50 | M | DM, DLP | new onset DCM, LV thrombus | Echo | 2 months |
| 29 | Gravinay [80] | 51 | M | No data | Myocarditis, LV thrombus | MRI | No data |
| 30 | Ford [81] | 53 | M | DLP | CVA with LV thrombus and myocarditis, possible chagas | Echo | Not known |
| 31 | Jariwala [71] | 54 | M | DM, smoker | LV thrombus with STEMI | Echo | LV thrombectomy done |
| 32 | Servato [82] | 55 | M | Obesity, OSA on CPAP | LV thrombus, myocarditis | Echo | 7 days |
| 33 | Jeon [5] | 55 | M | Not known | LV, pulmonary embolism, liver, kidney, spleen | Echo | 1 month |
| 34 | Imaeda [83] | 56 | M | DCM. EF-30 | LV thrombus | CTPA followed by echo confirmation | 8 days |
| 35 | Malaweera [84] | 56 | M | CAD, LV thrombus received 1yr anticoagulation | LV thrombus, spontaneous pneumothorax, pulmonary embolism | CTPA | Not known |
| 36 | Jariwala [85] | 56 | M | Chronic pancreatitis | LV thrombus | CTPA | Expired |
| 37 | Zheng [86] | 57 | M | DM, HTN, non-ischemic DCM, rEF | CVA, LV thrombus | Echo | Not known |
| 38 | Ferguson [10] | 58 | M | HTN, obesity, previous smoker | Biventricular thrombus, pulmonary embolism, peripheral arterial thrombosis | CTPA | Not known |
| 39 | John [87] | 58 | M | Nil | LV thrombus with STEMI | Echo | 6 weeks, normal EF at 5 months |
| 40 | Ozer [88] | 58 | M | DM, HTN | Biventricular thrombi, DVT, myocarditis | CTPA | Pt expired |
| 41 | Farouji [89] | 60 | M | HFrEF, epilepsy, and schizophrenia, active smoker, | LV thrombus, pulmonary embolism | CTPA followed by echo confirmation | Reduced size at 6 weeks |
| 42 | Tadayoni [90] | 61 | M | HOCM, LV aneurysm, GBS post COVID | LV thrombus, GBS | Echo | Not known |
| 43 | Byer [91] | 62 | F | Ischemic DCM | LV thrombus, | Echo | Not known |
| 44 | Soltani [92] | 63 | F | Smoker, emphysema | Biventricular thrombi, pulmonary embolism, STEMI | Ventriculography followed by cardiac CT | Expired |
| 45 | Ignaszewski [93] | 63 | M | Nil | STEMI, LV thrombus, HF | Echo followed by MRI | Not known |
| 46 | Jadhav [70] | 63 | M | No data | AWMI, LV thrombus, CVA | Echo | Expired |
| 47 | Jadhav [70] | 64 | F | No data | LV thrombus with CVA | Echo | Expired |
| 48 | Iqbal Phool [94] | 65 | M | Nil | CVA, LV thrombus | Echo | 1 month |
| 49 | Jariwala [71] | 67 | M | DM, reformed smoker | LV thrombus with STEMI | Echo | 2 weeks |
| 50 | Singh [95] | 69 | F | Pulmonary embolism on apixaban | LV thrombus with CVA | Echo | Expired |
| 51 | Castro [96] | 70 | F | HTN | LV thrombus | Echo | Expired |
| 52 | Mandal [97] | 70 | F | CAD s/p CABG and LV aneurysm resection, COPD | LV thrombus with splenic infarct, peripheral arterial infarcts | CTPA | Not known |
| 53 | Calvi [91] | 70 | M | CAD, HFrEF 33%, Lt pneumonectomy for adenocarcinoma lung | LV thrombus, VA, splenic infarct | Echo followed by CT | 12 days |
| 54 | Nanthatanti [98] | 71 | M | HTN, DLP, CAD | LV thrombus, | CTPA followed by echo confirmation | Not known |
| 55 | Azhar [99] | 71 | F | Not known | LV thrombus, DVT pulmonary embolism | CT angiogram followed by echo | Not known |
| 56 | Boui [100] | 73 | M | Gout | LV thrombus, pulmonary embolism, renal thrombus | CTPA followed by echo confirmation | 55 days |
| 57 | Gozgec [101] | 74 | F | Nil | LV thrombus, | CT | Expired |
| 58 | Bernardi [7] | 74 | M | DM, HTN, DLP | LV thrombus with Takotsubo syndrome | Echo followed by MRI | 14 days |
| 59 | Calvi [91] | 74 | M | Nil | LV thrombus, | Echo followed by MRI | 13 days |
| 60 | Furtney Joshua [102] | 78 | F | Not known | LV thrombus | Echo | Not known |
| 61 | Alfaki [103] | 79 | M | Non-ischemic cardiomyopathy, EF-45-50 | LV thrombus, pulmonary embolism | Echo | Expired |
| 62 | Patell [6] | 80 | F | Not known | LV thrombus with CRAO | Echo | Not known |
| 63 | Sonaglioni [104] | 80 | F | CAD, HFrEF, CKD | Biventricular thrombus | Echo | Expired |
| 64 | Fenton [105] | 82 | M | Nil, smoking history | STEMI, LV thrombus | Echo | Expired |
| 65 | Jariwala [71] | 85 | M | HTN, CAD, | LV thrombus, CVA, carotid artery thrombus | Echo | Expired |
CABG: Coronary artery bypass grafting, CAD: Coronary artery disease, CAG: Coronary angiography, CMR: Cardiac magnetic resonance imaging, CRAO: Central retinal artery occlusion,
CT: Computed tomography, CTPA: Computed tomography with pulmonary angiogram, CVA: Cerebrovascular accident, DCM: Dilated cardiomyopathy, DLP: Dyslipidemia, DM: Diabetes mellitus, DVT: Deep vein thrombosis, HFrEF: Heart failure with reduced Ejection fraction, HTN: Hypertension, LV: Left ventricle, MRI: Magnetic resonance imaging, NSTEMI: Non-ST segment elevation myocardial infarction, OSA: Obstructive sleep apnea, PTCA: Percutaneous transluminal coronary angioplasty, STEMI: ST segment elevation myocardial infarction
Since the rates of LVT in acute myocardial infarction and acute idiopathic myocarditis were 45% and 61.9%, respectively, a similar or higher incidence can be expected in COVID-19 [17]. This is supported by the observation that patients with concomitant COVID-19 and STEMI had worse left ventricular function, myocardial blush grade, higher incidence of multivessel disease, and stent thrombosis when compared to non-COVID-19 patients [18,19]. STEMI was the initial presentation in 69.2% of the patients with COVID-19, in an Egyptian study of 26 patients [19]. In our review, symptoms of typical anginal pain, as the presenting symptom were noted in nine patients (31%).
Post-infarct complications can lead to severe morbidity and mortality in these patients; however, the mortality from acute myocardial infarction has decreased after the incidence of percutaneous coronary intervention (PCI). The incidence of LVT post-acute myocardial infarction was 17% in the pre-PCI era, with an incidence as high as 34% in patients with anterior MI [20]. After the introduction of primary PCI, the incidence of LVT has fallen drastically, with incidence rates as low as 1.6% [21]. However, meta-analyses have found the rates to be between 7.5 and 9.1% in anterior MI [22].
Higher rates of thrombus formation were found in patients with anterior MI, low ejection fraction, severe apical wall motion abnormality, and worse TIMI flow rates.
4.1. Pathogenesis
The incidence of thrombotic complications may be higher in patients diagnosed with COVID-19 due to one of the following reasons.
The direct effects of the SARS-CoV2 virus, such as inhibition of interferon production and cytopathic effects on the CD4 cells leading to CD4+ lymphopenia, may stimulate downstream activation of proinflammatory macrophages and polymorphs, resulting in the release of prothrombotic cytokines and activation of platelets [23].
Infections such as COVID-19 can stimulate inflammatory activity inside an atheromatous plaque by activating macrophages and T-cells leading to a disruption of the plaque surface, exposure of its underlying thrombogenic elements and the formation of a thrombus [24].
Direct effects on the myocardium and COVID-19 induced myocarditis have been reported in 1% of all hospital admission [25]. In autopsy specimens, cardiac injury was noted in as many as 35%, with 13% showing lymphocytic myocarditis [26].
COVID-induced hypoxia may contribute to increased circulatory demand in the form of a compensatory increase in heart rate to maintain tissue oxygenation. Sustained hypoxia can lead to an increased production of transcription factors such as Nuclear Factor-kb and Hypoxia-inducible Factor-1, leading to further the inflammatory cascade and thrombosis [27].
COVID-19 has been shown to stimulate the production of neutrophil extracellular traps, which contribute to an increased risk of microvascular and venous thrombus formation [28]. In neutrophils incubated with the SARS-CoV2, increased levels of reactive oxygen species and serum levels of cell-free DNA, myeloperoxidase-DNA, and citrullinated histone H3 have been seen [29]. The virus exhibits tropism for angiotensin-converting enzyme -2 (ACE-2), which is found in type II epithelial cells of the lung, heart, kidneys, intestines, and blood vessels. In the heart, the receptor has been found on the pericytes, myocytes, and endothelial cells [30]. Higher concentrations of ACE- 2 may be found in the pericytes of patients with heart failure [31]. This may predispose these patients to a higher incidence of cardiac involvement. Direct cytopathic effects on the cardiac endothelial cells may be responsible for endothelial cell injury, apoptosis, and resultant thrombosis [32]. In response to viral replication, the host defence mechanism attempts to downregulate the levels of ACE-2 in the heart. This can, in turn, lead to an increase in the prothrombotic and proinflammatory effects of angiotensin II, leading to the formation of thrombosis and an increase in troponins, which in turn is associated with a poorer prognosis [33].
Prolonged hospitalization, ICU admission, and intubation are risk factors contributing to immobilization and venous stasis.
Antiphospholipid antibody syndrome is a prothrombotic autoimmune disease due to the presence of antiphospholipid antibodies, such as lupus anticoagulant (LA) anticardiolipin antibodies LA, or anti-b2glycoprotein-1. COVID-19 has been associated with detecting antiphospholipid antibodies in at least 52% of the patients [34]. The pathogenesis behind this finding can be attributed to molecular mimicry between the spike protein of the SARS CoV2 and native phospholipids, leading to the generation of antiphospholipid antibodies. Another possible mechanism is the conformational change in b2 glycoprotein induced by the oxidative stress in COVID-induced cytokine release, leading to a neoepitope formation and increased immunogenicity [35].
The increased incidence of Takotsubo cardiomyopathy in the post-COVID-19 period has been observed based on the results of a Cleveland clinic study, with rates as high as 7.7% in all patients with acute coronary syndrome compared to less than 2% before the pandemic [36,37]. This may contribute to the development of mural thrombus, as 3.3% of all patients with Takotsubo syndrome have been found to develop LVT [38].
COVID-19 associated HIT has been proven by the demonstration of elevated HIT antibodies against heparin-PF4 complexes. It leads to increased activation of the complement system, accumulation of C3a complement and increased arterial and venous thrombosis, especially in patients with severe COVID 19 [39].
4.2. Investigations
Echocardiography was the most commonly used imaging modality for detecting LVT. Early identification and treatment of patients with LVT are essential to improve outcomes. Transthoracic echocardiogram (TTE) is usually the initial modality used for evaluating LVT [40]. However, sensitivity is reportedly as low as 21%. Routine echocardiograms may oversee a small mural thrombus, especially when the clinical indication does not warrant a high degree of suspicion [41,42]. This can be improved with intravenous contrast, which raises sensitivity to approximately 64% [43]. Delayed enhanced cardiac MRI (CMR) is the gold standard for evaluating LVT, with a sensitivity of up to 88% and specificity of 99–100% verified by surgical findings, and with the highest detection rates when done 9–12 days after myocardial infarction [44]. Delayed enhancement CMR relies on tissue characterization to detect LVT rather than anatomic appearance, allowing thrombus to be differentiated from myocardial structures regardless of location or morphology [40]. Some studies have reported coronary CT angiography (CCTA) to be comparable to CMR in detecting LVT with advantages including shorter scanning time and widespread availability. Disadvantages of CCTA include increased radiation to patients and the need for intravenous iodinated contrast [45]. In one case study, persistent Staphylococcus bacteremia was detected in a 61-year-old woman with fever and acute meningitis. A transesophageal echocardiogram did not reveal any pathological findings. However, 18F-FDG PET/CT and CMR helped diagnose a left ventricular infected thrombus [46]. Among the modalities of diagnosis, contrast-MRI with late gadolinium enhancement yields accurate results with a sensitivity of 88% and specificity of 99%. This is followed by the cine CMR, contrast TTE, and non-contrast TTE, among the non-invasive methods. Although contrast ventriculography has a high specificity (85–90%), the sensitivity ranges to around 30%, especially immediately after a MI [47]. Fiberoptic cardioscopy is an endoscopic system developed in Japan, and is used to assess the morphology and functionality of the interior of the cardiac chambers and enable minimally invasive procedures [48]. Cardioscopy can detect LVT in 30.2% of the cases, compared to 2.7% with left ventriculography, 7.0% with contrast echocardiogram, and 1.9% with non-contrast echocardiography [49]. No direct study has compared the relative efficacy of cardioscopy over CMR. However, Uchida proposes that cardioscopy may be more valuable in this cause, as it is more sensitive (35.1% vs. 16.3%, P<0.01), and can also detect the characteristics of the thrombus, such as morphology and color. In the present pandemic, due to the need for sophisticated equipment and the ability to visualize only 4-5 sections of the LV, non-invasive diagnostic tests may be preferred for ease of access and availability.
4.3. Management
All patients with cardiovascular comorbidities, who receive medical care at home, should be closely assessed for disease worsening and need for hospitalization [50]. Patients who require hospitalization and those who require critical care should receive routine thromboprophylaxis. TTE is indicated in hospitalized patients with cardiac comorbidities or high clinical suspicion, especially those with raised troponins and D-dimer values. These correlate with a higher risk of detecting critical findings on the echocardiogram and may necessitate a change in treatment strategy [51,52].
In hospitalized patients, unfractionated heparin (UFH) or LMWH may be preferred over direct oral anticoagulants due to the lower risk of drug-interaction with antivirals or steroids. Using heparin in the form of UFH or LMWH improved the 28-day mortality in hospitalized patients with COVID-19, who had D-dimer above 3000 ng/ml [53,54]. Extended post-discharge thromboprophylaxis is recommended only in patients with a high risk of post-discharge thrombosis. In the pre-COVID-19 period, studies on LVT demonstrated that the median time to thrombus regression was 103 days, irrespective of the anticoagulant given [55]. There was no difference in the rate of embolic or bleeding events among the different anticoagulants [56].
5. Limitations
Most studies on COVID-19 and cardiac complications do not have data on the incidence of LVT; hence, the actual incidence in the real-world setting cannot be estimated. Although preliminary data suggests that there is an association between LVT and COVID-19, one cannot assume that the latter is the cause of the former, in the absence of unequivocal evidence from a large, prospective study. Studies with directed cardiac imaging and a high degree of suspicion are required in COVID-19 patients with documented peripheral arterial or venous embolism to differentiate between small vessel de novo thrombosis and embolism secondary to intra-cardiac thrombosis. Due to a lack of uniformity in clinical, imaging, and laboratory data between the patients included in our review, definite conclusions could not be drawn regarding any parameter that could be considered helpful in screening or assessing patients presenting with LVT. Details of outcomes including ARF, ARDS, CNS injury, mechanical ventilation, duration of stay, hemodialysis, and cost of care have not been reported.
6. Conclusion
Although LVT has high morbidity and mortality in patients with COVID-19, routine screening of patients is not required. With only a few cases reported, the clinical presentation and laboratory parameters necessitating screening for LVT are uncertain. LVT has been commonly reported in the COVID-19 patients with severe infection and underlying myocardial dysfunction. Cardiac screening studies may be necessary for COVID-19 patients with severe infection, elevated coagulation parameters, and comorbidities to rule out mural thrombus, and the possibility of arterial or pulmonary embolism. Bedside screening echocardiogram can be done in patients with preexistent cardiac illness, and moderate to severe COVID-19 at the time of admission.
Further imaging is warranted only if clinical or laboratory parameters suggest increasing severity of disease. Since COVID-19 pneumonia and resultant hypoxia have been associated with an increased risk of thrombosis, thromboprophylaxis must be initiated in all patients with moderate to severe disease. A high index of suspicion should also be maintained in patients presenting with arterial and venous embolism.
Acknowledgments
Authors would like to thank Dr. Bivin V Thomas and Anju Philip for reviewing the article.
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Statement
The article does not contain the participation of any human being and animal.
References
- [1].Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of Comorbidities and its Effects in Patients Infected with SARS-CoV-2:A Systematic Review and Meta-Analysis. Int J Infect Dis. 2020;94:91–5. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mishra AK, Lal A, Sahu KK, Kranis M, Sargent J. Quantifying and Reporting Cardiac Findings in Imaging of COVID-19 Patients. Monaldi Arch Chest Dis. 2020;90:1394. doi: 10.4081/monaldi.2020.1394. [DOI] [PubMed] [Google Scholar]
- [3].Piazza G, Morrow DA. Diagnosis, Management, and Pathophysiology of Arterial and Venous Thrombosis in COVID-19. JAMA. 2020;324:2548–9. doi: 10.1001/jama.2020.23422. [DOI] [PubMed] [Google Scholar]
- [4].de Simone V, Mugnolo A, Zamboni A, Morando G. Myocardial Infarction in COVID-19 Era:A Dramatic Dip into the Past? Mathews J Cardiol. 2020;5:22. [Google Scholar]
- [5].Jeon HD, Patel J, Priester T, Moten M. Left Ventricular Thrombus Caused by COVID-19:How Long to Treat? J Am Coll Cardiol. 2021;77:2013. [Google Scholar]
- [6].Patell R, Bogue T, Koshy A, Bindal P, Merrill M, Aird WC, et al. Postdischarge Thrombosis and Hemorrhage in Patients with COVID-19. Blood. 2020;136:1342–6. doi: 10.1182/blood.2020007938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bernardi N, Calvi E, Cimino G, Pascariello G, Nardi M, Cani D, et al. COVID-19 Pneumonia, Takotsubo Syndrome, and Left Ventricle Thrombi. JACC Case Rep. 2020;2:1359–64. doi: 10.1016/j.jaccas.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Iguina M, Saleh A, Sayeedi I, Danckers M. Recurrent Ischemic Strokes in a Patient with Severe COVID-19 Infection and Phosphatidylserine Antibodies. Chest. 2020;158:A776. [Google Scholar]
- [9].Mitevska I, Nastevska EG, Kandic E, Busljetik O. “Heart Full of Thrombi”:Post COVID-19 Multisite Thrombosis assessed by Echocardiography and Pulmonary CT. Imaging. 2021 https://doi.org/10.1556/1647.2021.00047. [Google Scholar]
- [10].Ferguson K, Quail N, Kewin P, Blyth KG. COVID-19 Associated with Extensive Pulmonary Arterial, Intracardiac and Peripheral Arterial Thrombosis. BMJ Case Rep. 2020;13:e237460. doi: 10.1136/bcr-2020-237460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ziaie N, Maleh PA, Ramandi MM, Pourkia R, Latifi K, Mansouri D. Transient Left Ventricular clot in COVID-19-Related Myocarditis is Associated with Hypereosinophilic Syndrome:A Case Report. Int J Cardiovasc Imaging. 2021;37:3279–83. doi: 10.1007/s10554-021-02317-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Talle MA, Buba F, Anjorin CO. Prevalence and Aetiology of Left Ventricular Thrombus in Patients Undergoing Transthoracic Echocardiography at the University of Maiduguri Teaching Hospital. Adv Med. 2014;2014:731936. doi: 10.1155/2014/731936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in Hospitalized Patients with COVID-19 in a New York City Health System. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bunce PE, High SM, Nadjafi M, Stanley K, Liles WC, Christian MD. Pandemic H1N1 Influenza Infection and Vascular Thrombosis. Clin Infect Dis. 2011;52:e14-7. doi: 10.1093/cid/ciq125. [DOI] [PubMed] [Google Scholar]
- [15].Cates J, Lucero-Obusan C, Dahl RM, Schirmer P, Garg S, Oda G, et al. Risk for in-Hospital Complications Associated with COVID-19 and Influenza-Veterans Health Administration, United States, October 1, 2018-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1528–34. doi: 10.15585/mmwr.mm6942e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Daniel M, Brian C, Caroline SP, Højbjerg LM, Grundtvig SK, Stæhr JJ, et al. Acute COVID-19 and the Incidence of Ischemic Stroke and Acute Myocardial Infarction. Circulation. 2020;142:2080–2. doi: 10.1161/CIRCULATIONAHA.120.050809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Uchida Y, Uchida Y, Sakurai T, Kanai M, Shirai S, Nakagawa O. Cardioscopic Detection of Left Ventricular Thrombi. Circ J. 2011;75:1920–6. doi: 10.1253/circj.cj-11-0248. [DOI] [PubMed] [Google Scholar]
- [18].Choudry FA, Hamshere SM, Rathod KS, Akhtar MM, Archbold RA, Guttmann OP, et al. High Thrombus Burden in Patients with COVID-19 Presenting with ST-Segment Elevation Myocardial Infarction. J Am Coll Cardiol. 2020;76:1168–76. doi: 10.1016/j.jacc.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Alaarag A, Hassan T, Samir S, Naseem M. Clinical and Angiographic Characteristics of Patients with STEMI and Confirmed Diagnosis of COVID-19:An Experience of Tanta University Hospital. Egypt Heart J. 2020;72:68. doi: 10.1186/s43044-020-00103-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Asinger RW, Mikell FL, Elsperger J, Hodges M. Incidence of Left-Ventricular Thrombosis after Acute Transmural Myocardial Infarction. N Engl J Med. 1981;305:297–302. doi: 10.1056/NEJM198108063050601. [DOI] [PubMed] [Google Scholar]
- [21].Mao TF, Bajwa A, Muskula P, Coggins TR, Kennedy K, Magalski A, et al. Incidence of Left Ventricular Thrombus in Patients With Acute ST-Segment Elevation Myocardial Infarction Treated with Percutaneous Coronary Intervention. Am J Cardiol. 2018;121:27–31. doi: 10.1016/j.amjcard.2017.09.010. [DOI] [PubMed] [Google Scholar]
- [22].Robinson AA, Jain A, Gentry M, McNamara RL. Left Ventricular Thrombi after STEMI in the Primary PCI Era:A Systematic Review and Meta-Analysis. Int J Cardiol. 2016;221:554–9. doi: 10.1016/j.ijcard.2016.07.069. [DOI] [PubMed] [Google Scholar]
- [23].Henry BM, Vikse J, Benoit S, Favaloro EJ, Lippi G. Hyperinflammation and Derangement of Renin-Angiotensin-Aldosterone System in COVID-19:A Novel Hypothesis for Clinically Suspected Hypercoagulopathy and Microvascular Immunothrombosis. Clin Chim Acta. 2020;507:167–73. doi: 10.1016/j.cca.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Schiavone M, Gobbi C, Biondi-Zoccai G, D'Ascenzo F, Palazzuoli A, Gasperetti A, et al. Acute Coronary Syndromes and COVID-19:Exploring the Uncertainties. J Clin Med. 2020;9:1683. doi: 10.3390/jcm9061683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Laganà N, Cei M, Evangelista I, Cerutti S, Colombo A, Conte L, et al. Suspected Myocarditis in Patients with COVID-19:A Multicenter Case Series. Medicine (Baltimore) 2021;100:e24552. doi: 10.1097/MD.0000000000024552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Mishra AK, Lal A, Sahu KK, Sargent J. Cardiovascular Factors Predicting Poor Outcome in COVID-19 Patients. Cardiovasc Pathol. 2020;49:107246. doi: 10.1016/j.carpath.2020.107246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Gupta N, Ashraf MZ. Hypoxia Signaling in Cardiovascular Diseases. In: Das KK, Biradar MS, editors. Hypoxia and Anoxia. London: Intech Open; 2018. [Google Scholar]
- [28].Zuo Y, Yalavarthi S, Shi H, Gockman K, Zuo M, Madison JA, et al. Neutrophil Extracellular Traps in COVID-19. JCI Insight. 2020;5:e138999. doi: 10.1172/jci.insight.138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Arcanjo A, Logullo J, Menezes CC, de Souza Carvalho Giangiarulo TC, dos Reis MC, de Castro GM, et al. The Emerging role of Neutrophil Extracellular Traps in Severe Acute Respiratory Syndrome Coronavirus 2 (COVID-19) Sci Rep. 2020;10:19630. doi: 10.1038/s41598-020-76781-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Thum T. SARS-CoV-2 Receptor ACE2 Expression in the Human Heart:Cause of a Post-Pandemic Wave of Heart Failure? Eur Heart J. 2020;41:1807–9. doi: 10.1093/eurheartj/ehaa410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 Expression in Human Heart Indicates New Potential Mechanism of Heart Injury among Patients Infected with SARS-CoV-2. Cardiovasc Res. 2020;116:1097–100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Connors JM, Levy JH. COVID-19 and its Implications for Thrombosis and Anticoagulation. Blood. 2020;135:2033–40. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39:618–25. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Zuo Y, Estes SK, Ali RA, Gandhi AA, Yalavarthi S, Shi H, et al. Prothrombotic Autoantibodies in Serum from Patients Hospitalized with COVID-19. Sci Transl Med. 2020;12:eabd3876. doi: 10.1126/scitranslmed.abd3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Tung ML, Tan B, Cherian R, Chandra B. Anti-Phospholipid Syndrome and COVID-19 Thrombosis:Connecting the Dots. Rheumatol Adv Pract. 2021;5:rkaa081. doi: 10.1093/rap/rkaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Shah RM, Shah M, Shah S, Li A, Jauhar S. Takotsubo Syndrome and COVID-19:Associations and Implications. Curr Probl Cardiol. 2021;46:100763. doi: 10.1016/j.cpcardiol.2020.100763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].John K, Lal A, Mishra A. A Review of the Presentation and Outcome of Takotsubo Cardiomyopathy in COVID-19. Monaldi Arch Chest Dis. 2021;91:1710. doi: 10.4081/monaldi.2021.1710. [DOI] [PubMed] [Google Scholar]
- [38].Katharina JD, Victoria LC, Konrad AS, Barbara ES, Manfred W, Di Vece Davide, et al. Intraventricular Thrombus Formation and Embolism in Takotsubo Syndrome. Arterioscler Thromb Vasc Biol. 2020;40:279–87. doi: 10.1161/ATVBAHA.119.313491. [DOI] [PubMed] [Google Scholar]
- [39].Liu X, Zhang X, Xiao Y, Gao T, Wang G, Wang Z, et al. Heparin-Induced Thrombocytopenia is Associated with a High Risk of Mortality in Critical COVID-19 Patients Receiving Heparin-Involved Treatment. medRxiv. 2020;2020:20076851. [Google Scholar]
- [40].Hur J, Hong YJ, Im DJ, Lee HJ, Kim YJ, Choi BW. Technological Improvements in Cardiac Thrombus Diagnosis. Cardiovasc Imaging Asia. 2017;1:166. [Google Scholar]
- [41].Weinsaft JW, Kim HW, Crowley AL, Klem I, Shenoy C, van Assche L, et al. LV Thrombus Detection by Routine Echocardiography:Insights into Performance Characteristics using Delayed Enhancement CMR. JACC Cardiovasc Imaging. 2011;4:702–12. doi: 10.1016/j.jcmg.2011.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, et al. ST-Segment Elevation in Patients with COVID-19-a Case Series. N Engl J Med. 2020;382:2478–80. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].McCarthy CP, Vaduganathan M, McCarthy KJ, Januzzi JL, Jr, Bhatt DL, McEvoy JW. Left Ventricular Thrombus after Acute Myocardial Infarction:Screening, Prevention, and Treatment. JAMA Cardiol. 2018;3:642–9. doi: 10.1001/jamacardio.2018.1086. [DOI] [PubMed] [Google Scholar]
- [44].Srichai MB, Junor C, Rodriguez LL, Stillman AE, Grimm RA, Lieber ML, et al. Clinical, Imaging, and Pathological Characteristics of Left Ventricular Thrombus:A Comparison of Contrast-Enhanced Magnetic Resonance Imaging, Transthoracic Echocardiography, and Transesophageal Echocardiography with Surgical or Pathological Validation. Am Heart J. 2006;152:75–84. doi: 10.1016/j.ahj.2005.08.021. [DOI] [PubMed] [Google Scholar]
- [45].Mendirichaga R, Fishman JE, Martinez CA. Imaging Modalities for Detection and Treatment of Cardiovascular Thrombus. In: Topaz O, editor. Cardiovascular Thrombus. Ch. 7. Cambridge, Massachusetts, United States: Academic Press; 2018. pp. 99–113. [Google Scholar]
- [46].Vicente AM, García MV, Sancho JJ, Castrejón ÁS. Left Ventricular Infected Thrombus Detected by 18F-FDG PET/CT and MRI in Disseminated Staphylococcus Infection. Clin Nucl Med. 2020;45:957–9. doi: 10.1097/RLU.0000000000003301. [DOI] [PubMed] [Google Scholar]
- [47].Habash F, Vallurupalli S. Challenges in Management of Left Ventricular Thrombus. Ther Adv Cardiovasc Dis. 2017;11:203–13. doi: 10.1177/1753944717711139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Uchida Y. Advances in Percutaneous Cardioscopy for Heart Disease. J Indian Coll Cardiol. 2018;8:200–8. [Google Scholar]
- [49].Uchida Y. Recent Advances in Percutaneous Cardioscopy. Curr Cardiovasc Imaging Rep. 2011;4:317–27. doi: 10.1007/s12410-011-9092-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Gerotziafas GT, Catalano M, Colgan MP, Pecsvarady Z, Wautrecht JC, Fazeli B, et al. Guidance for the Management of Patients with Vascular Disease or Cardiovascular Risk Factors and COVID-19:Position Paper from VAS-European Independent Foundation in Angiology/Vascular Medicine. Thromb Haemost. 2020;120:1597–628. doi: 10.1055/s-0040-1715798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Yuan N, Wu S, Rader F, Siegel RJ. Determining which Hospitalized COVID-19 Patients Require an Urgent Echocardiogram. J Am Soc Echocardiogr. 2021;34:831–8. doi: 10.1016/j.echo.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, et al. Global Evaluation of Echocardiography in Patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949–58. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Mishra AK, Sahu KK, Lal A, Sargent J. Mechanisms of Stroke and the Role of Anticoagulants in COVID-19. J Formos Med Assoc. 2020;119:1721–2. doi: 10.1016/j.jfma.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Yin S, Huang M, Li D, Tang N. Difference of Coagulation Features between Severe Pneumonia Induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2021;51:1107–10. doi: 10.1007/s11239-020-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Lattuca B, Bouziri N, Kerneis M, Portal JJ, Zhou J, Hauguel-Moreau M, et al. Antithrombotic Therapy for Patients With Left Ventricular Mural Thrombus. J Am Coll Cardiol. 2020;75:1676–85. doi: 10.1016/j.jacc.2020.01.057. [DOI] [PubMed] [Google Scholar]
- [56].Zhou K, Zhang X, Xiao Y, Li D, Song G. Effectiveness and safety of direct-Acting oral Anticoagulants Compared to Vitamin K Antagonists in Patients with Left Ventricular Thrombus:A Meta-Analysis. Thromb Res. 2021;197:185–91. doi: 10.1016/j.thromres.2020.11.018. [DOI] [PubMed] [Google Scholar]
- [57].Mahdavi M, Houshmand G, Pouraliakbar H, Mortaz Hejri G. Delayed Diffuse Inflammatory Myocardial Damage in a Child with a History of Systemic Inflammatory Syndrome Related to COVID-19. Eur Heart J. 2021;42:1639–9. doi: 10.1093/eurheartj/ehaa1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Bigdelian H, Sedighi M, Sabri MR, Dehghan B, Mahdavi C, Ahmadi A, et al. Case Report:Acute Intracardiac Thrombosis in Children With Coronavirus Disease 2019 (COVID-19) Front Pediatr. 2021;9:656720. doi: 10.3389/fped.2021.656720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Materna O, Koubský K, Pádr R, Janoušek J. Major Left Ventricular Thrombi in an Adolescent with COVID-19-Associated Inflammatory Syndrome. Eur Heart J. 2021;42:3207. doi: 10.1093/eurheartj/ehab165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Schroder J, Lund MA, Vejlstrup N, Juul K, Nygaard U. Left Ventricular Thrombus in Multisystem Inflammatory Syndrome in Children Associated with COVID-19. Cardiol Young. 2021 doi: 10.1017/S1047951121002456. https://doi.org/10.1017/S1047951121002456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Munoz D, Malik H, Eickenhorst D, Newman S, Varughese C, Ali F. Cardiac Screening in a Young Adult Male Leading to Discovery of Post-COVID Myocarditis with Asymptomatic Large Apical Left Ventricular Thrombus. CASE (Phila) 2021;5:309–12. doi: 10.1016/j.case.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Agarwal S, Al Hashimi H, Agarwal SK, Albastaki U. Possible Association Between Myocardial Infarction with Nonobstructed Coronary Arteries and SARS-CoV-2 Infection. Can Med Assoc J. 2020;192:E1633. doi: 10.1503/cmaj.202106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Hodson DZ, Reinhardt SW, Moore CL. Young Man with Shortness of Breath. Ann Emerg Med. 2021;77:500–58. doi: 10.1016/j.annemergmed.2020.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Capaccione KM, Leb JS, D'souza B, Utukuri P, Salvatore MM. Acute Myocardial Infarction Secondary to COVID-19 Infection:A Case Report and Review of the Literature. Clin Imaging. 2021;72:178–82. doi: 10.1016/j.clinimag.2020.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Ranard LS, Engel DJ, Kirtane AJ, Masoumi A. Coronary and Cerebral Thrombosis in a Young Patient after Mild COVID-19 Illness:A Case Report. Eur Heart J Case Rep. 2020;4:1–5. doi: 10.1093/ehjcr/ytaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Kihira S, Schefflein J, Pawha P, Rigney B, Delman BN, Xuan D, et al. Neurovascular Complications that Can be Seen in COVID-19 Patients. Clin Imaging. 2021;69:280–4. doi: 10.1016/j.clinimag.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Amin A, Sadeghipour P, Chitsazan M. Cardiovascular Disease in the COVID-19 Era:Myocardial Injury and Thrombosis. Pract Cardiol. 2022:737–43. https://doi.org/10.1016/B978-0-323-80915-3.00044-2. [Google Scholar]
- [68].El Aidouni G, Merbouh M, Aabdi M, Bouabdallaoui A, Bkiyar H, Smaili N, et al. Intra Cardiac Thrombus in Critically Ill Patient with Coronavirus Disease 2019:Case Report. Ann Med Surg. 2021;66:102434. doi: 10.1016/j.amsu.2021.102434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Rubartelli P, Toselli A, Camerini A, Lupi G, Romeo M. A Patient with COVID-19 Presenting Multiple Thrombi in the Left Ventricle. Acta Cardiol. 2021;76:211–3. doi: 10.1080/00015385.2020.1826702. [DOI] [PubMed] [Google Scholar]
- [70].Jadhav K, Jariwala P. Intra-Cardiac Thrombus in COVID-19 pandemic-Case Series and Review. Eur J Cardiovasc Med. 2020;6:591–8. [Google Scholar]
- [71].Jariwala P, Punjani A, Boorugu H, Reddy M. Left Ventricular Thrombus in Patients with COVID-19-a Case Series. J Pract Cardiovasc Sci. 2021;7:69. [Google Scholar]
- [72].Hammam R, Abdelaziz B, Anass H, Nabila I, Ouafi NE. Multiple Cardiovascular Complications of COVID-19 Infection in a Young Patient:A Case Report. Pan Afr Med J. 2021;38:192. doi: 10.11604/pamj.2021.38.192.27471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Bonello EC, Casha R, Xerri T, Bonello J, Fsadni C, Azzopardi CM. Multiorgan Thrombosis as a Complication of COVID-19 Pneumonia. BMJ Case Rep. 2021;14:e243953. doi: 10.1136/bcr-2021-243953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Garg A, Hakeem H, Chennu G, Saeed Q, Vucic E, Kats Y, et al. Left Ventricular Mural Thrombi with Multisystem Thrombosis In Patients with COVID-19 and Myocardial Injury:A Case Series. Eur Heart J Case Rep. 2021;5:ytab239. doi: 10.1093/ehjcr/ytab239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Hudowenz O, Klemm P, Lange U, Rolf A, Schultheiss HP, Hamm C, et al. Case Report of Severe PCR-Confirmed COVID-19 Myocarditis in a European Patient Manifesting in Mid January 2020. Eur Heart J Case Rep. 2020;4:1–6. doi: 10.1093/ehjcr/ytaa286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Pranav V, Michael A, Levi M, Faisal D, Raj P, Ahmed A, et al. Successful Treatment of COVID-Related Stemi with Anti-Thrombotic Medical Management. J Am Coll Cardiol. 2021;77(Suppl 18):2015. [Google Scholar]
- [77].Alizadehasl A, Roudbari S, Salehi P, Sistani A, Mostafavi A, Fumani HK, et al. A Case of Multiple Large Left Ventricular Clots in a Patient with COVID-19. Int Cardiovasc Res J. 2021;15:44–7. [Google Scholar]
- [78].Sharma H, George S. Early Left Ventricular Thrombus Formation in a COVID-19 Patient with ST-Elevation Myocardial Infarction. Case Rep Cardiol. 2020;2020:8882463. doi: 10.1155/2020/8882463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Ramalho C, Almeida M, Gomes F, Silva M, Rodrigues S. Cardiac Abnormalities in COVID-19 Patients:Should a Cardiac Echocardiogram be Routine? Eur J Case Rep Intern Med. 2021;8:002559. doi: 10.12890/2021_002559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Gravinay P, Issa N, Girard D, Camou F, Cochet H. CMR and Serology to Diagnose COVID-19 Infection with Primary Cardiac Involvement. Eur Heart J Cardiovasc Imaging. 2021;22:133–3. doi: 10.1093/ehjci/jeaa169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Ford JS, Holmes JF, Jones RF. Cardioembolic Stroke in a Patient with Coronavirus Disease of 2019 (COVID-19) Myocarditis:A Case Report. Clin Pract Cases Emerg Med. 2020;4:332–5. doi: 10.5811/cpcem.2020.6.47856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Servato ML, Valente FX, García-Moreno LG, Casas G, Fernández-Galera R, Burcet G, et al. Intraventricular Conundrum in a SARS-CoV-2-Positive Patient With Elevated Biomarkers of Myocardial Injury. JACC Case Rep. 2021;3:566–72. doi: 10.1016/j.jaccas.2021.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Imaeda S, Kabata H, Shiraishi Y, Kamata H, Tsuruta H, Yuasa S, et al. Left Ventricular Thrombus With COVID-19 Complication in a Patient with Dilated Cardiomyopathy. CJC Open. 2021;3:124–6. doi: 10.1016/j.cjco.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Malaweera A, Papachristidis A, Harding I, Pareek N. Multisystem Manifestations of COVID-19 in a Patient Presenting to a Heart Attack Centre. Eur Heart J Cardiovasc Imaging. 2020;21:1304–4. doi: 10.1093/ehjci/jeaa203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Jariwala PV, Jadhav KP, Aurangabadkar H, Dommata RR. Left Ventricular Thrombus with Normal Systolic Function Secondary to the Novel Prothrombotic Association of Acute on Chronic Calcific Pancreatitis and COVID-19. J Cardiol Cases. 2021 doi: 10.1016/j.jccase.2021.06.010. https://doi.org/10.1016/j.jccase.2021.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Zheng H, Stergiopoulos K, Wang L, Chen L, Cao J. COVID-19 Presenting as Major Thromboembolic Events:Virchow's Triad Revisited and Clinical Considerations of Therapeutic Anticoagulation. Cureus. 2020;12:e10137. doi: 10.7759/cureus.10137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].John S, Hegde S, Hussain S, Bukharovich I, Graham-Hill S, Mallappallil M, et al. COVID-19 Pneumonia Precipitating Acute Anterior Wall Myocardial Infarction With Large Left Ventricular Apical Thrombus. J Med Cases. 2021;12:251–5. doi: 10.14740/jmc3687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Ozer M, Abbasi F, Mahdi M, Goksu SY, Struble E. Massive Biventricular Thrombi Complicating New-Onset Heart Failure in a Patient with Suspected COVID-19. J Cardiol Cases. 2021;24:144–7. doi: 10.1016/j.jccase.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Farouji I, Chan KH, Abanoub R, Guron G, Slim J, Suleiman A. A Rare Case of Co-Occurrence of Pulmonary Embolism and Left Ventricular Thrombus in a Patient with COVID-19. SAGE Open Med Case Rep. 2020;8:1–5. doi: 10.1177/2050313X20974534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Tadayoni A, Adedayo A, Dogar M, Budzikowski AS. Left Ventricular Thrombosis Formation in the Patient with Obstructive Hypertrophic Cardiomyopathy Following SARS-COV-2 Infection a Case Report and Literature Review. J Am Coll Cardiol. 2021;77:1995–5. [Google Scholar]
- [91].Calvi E, Bernardi N, Cimino G, Pascariello G, Faggiano P, Gavazzi E, et al. Unusual Intracardiac Thrombosis in two Patients with Coronavirus Disease 2019 (COVID-19):Case Series. Eur Heart J Case Rep. 2020;5:ytaa518. doi: 10.1093/ehjcr/ytaa518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Soltani M, Mansour S. Biventricular Thrombi Associated With Myocardial Infarction in a Patient with COVID-19. Can J Cardiol. 2020;36:1326.e9–11. doi: 10.1016/j.cjca.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Ignaszewski M, Pandrangi K, Kabbany M, Wilcox JE, Vorovich EE, Tibrewala A, et al. To VAD or Not to VAD:A Case of Durable Left Ventricular Assist Device Implantation in a COVID-19 Patient. J Heart Lung Transplant. 2021;40:S521. [Google Scholar]
- [94].Iqbal P, Laswi B, Jamshaid MB, Shahzad A, Chaudhry HS, Khan D, et al. The Role of Anticoagulation in Post-COVID-19 Concomitant Stroke, Myocardial Infarction, and Left Ventricular Thrombus:A Case Report. Am J Case Rep. 2021;22:e928852. doi: 10.12659/AJCR.928852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Singh G, Attique HB, Gadela NV, Mapara K, Manickaratnam S. COVID-19 Related Arterial Coagulopathy. Cureus. 2020;12:e9490. doi: 10.7759/cureus.9490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Castro RR, da Silveira JG, Castro RR, do Nascimento JS, do Nascimento JK, Dos Santos Moraes Nunes N, et al. COVID-19 and Stroke:A Thromboembolic Hypothesis. Rev Assoc Méd Bras. 2020;66:1476–7. doi: 10.1590/1806-9282.66.11.1476. [DOI] [PubMed] [Google Scholar]
- [97].Mandal S, Gami S, Khadka S, Ray B, Ghimire S. A Case Report on Extensive Arterial Thrombosis:A Rare Complication of COVID-19 Infection. Cureus. 2021;13:e15378. doi: 10.7759/cureus.15378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Nanthatanti N, Phusanti S, Chantrathammachart P, Thammavaranucupt K, Angchaisuksiri P, Sungkanuparph S. Left Ventricular Thrombus and Pulmonary Embolism:A Case Series of Thrombosis in COVID-19 in Thai Patients. Res Pract Thromb Haemost. 2020;4:1224–9. doi: 10.1002/rth2.12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Azhar A, Bk A, Hadzipasic O. In:TP47 TP047 COVID and ARDS Case Reports. New York, United States: American Thoracic Society; 2021. An Interesting Case of COVID-19 Induced Hypercoagulability Manifesting as Pulmonary Embolism and Apical Left Ventricular Thrombus; p. A2441. [Google Scholar]
- [100].Boui M, Hammoune N, Slioui B, Bellasri S, Ben Elhend S, Zouaki Z, et al. Concomitant acute pulmonary embolism, intracardiac thrombus and renal artery thrombosis in COVID-19 patient. Thromb Update. 2021;3:100042. doi: 10.1016/j.tru.2021.100042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Gozgec E, Ogul H, Alay H. Left Ventricular Thrombus in a Patient Infected by COVID-19. Ann Thorac Surg. 2021;111:e67. doi: 10.1016/j.athoracsur.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Joshua F, Steven B, Seri H, Riley J. A rare complication of Delayed Onset Takotsubo Cardiomyopathy in COVID-19. J Am Coll Cardiol. 2021;77(Suppl 18):2213. [Google Scholar]
- [103].Alfaki M, Flemming N, Sittol R, Grant J, Lisung F. Acute Pulmonary Embolism and Myocardial Injury in COVID-19 Patient. Chest. 2020;158:A2134. [Google Scholar]
- [104].Sonaglioni A, Albini A, Nicolosi GL, Rigamonti E, Noonan DM, Lombardo M. Case Report:An Unusual Case of Biventricular Thrombosis in a COVID-19 Patient With Ischemic Dilated Cardiomyopathy:Assessment of Mass Mobility and Embolic Risk by Tissue Doppler Imaging. Front Cardiovasc Med. 2021;8:694542. doi: 10.3389/fcvm.2021.694542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Fenton M, Siddavaram S, Sugihara C, Husain S. Lessons of the Month 3:ST-Elevation Myocardial Infarction and Left Ventricular Thrombus Formation:An Arterial Thrombotic Complication of Severe COVID-19 Infection. Clin Med. 2020;20:437. doi: 10.7861/clinmed.2020-0266. [DOI] [PMC free article] [PubMed] [Google Scholar]


