Abstract
EXECUTIVE SUMMARY The 2020-2021 Academic Affairs Committee was charged to (1) Read all six reports from the 2019-20 AACP standing committees to identify elements of these reports that are relevant to your committee’s work this year; (2) Determine what changes made in colleges and schools of pharmacy during the COVID-19 pandemic should be continued to advance pharmacy education; (3) Develop a realistic model for colleges and schools of pharmacy to share resources to meet the curricular needs of member schools; (4) Create strategies by which colleges and schools of pharmacy can meet current and future workforce development needs particularly in light of the changes in healthcare delivery as a result of the COVID-19 pandemic; (5) Identify salient activities for the Center To Accelerate Pharmacy Practice Transformation and Academic Innovation (CTAP) for consideration by the AACP Strategic Planning Committee and AACP staff. This report provides an overview of changes made in schools and colleges of pharmacy implemented in response to the COVID-19 pandemic that may be continued to advance pharmacy education; a realistic model for colleges and schools of pharmacy to share resources to meet the curricular needs of member schools; and strategies by which schools and colleges of pharmacy can meet current and future workforce development needs, particularly in light of the changes in healthcare delivery as a result of the COVID-19 pandemic. The committee is proposing one policy statement for consideration by the 2021 AACP House of Delegates, four suggestions for consideration by schools and colleges of pharmacy (including two endorsements for suggestions from the 2020-21 Argus Commission), and one recommendation for consideration by AACP for CTAP to implement and oversee.
Keywords: virtual learning, curriculum, workforce, technology, practice advancement
INTRODUCTION AND COMMITTEE CHARGES
According to the Bylaws of the American Association of Colleges of Pharmacy (AACP), the Academic Affairs Committee (AAC) is to address intellectual, social, and personal aspects of pharmacy education and identify practices, procedures, and guidelines which aid faculties in developing students to their maximum potential. President Anne Lin charged the 2020-2021 Academic Affairs Committee to evaluate how pharmacy education is delivered and how pharmacy is practiced, especially in light of changes brought about by the COVID-19 pandemic.1 The specific charges are as follows:
Read all six reports from the 2019-20 AACP standing committees to identify elements of these reports that are relevant to your committee’s work this year.
Determine what changes made in colleges and schools of pharmacy during the COVID-19 pandemic should be continued to advance pharmacy education.
The COVID-19 pandemic demonstrated the need for colleges and schools of pharmacy to share and work together. Develop a realistic model for colleges and schools of pharmacy to share resources to meet the curricular needs of member schools.
Create strategies by which colleges and schools of pharmacy can meet current and future workforce development needs particularly in light of the changes in healthcare delivery as a result of the COVID-19 pandemic
From your work on this year’s charges, identify salient activities for the Center to Accelerate Pharmacy Practice Transformation and Academic Innovation (CTAP) for consideration by the AACP Strategic Planning Committee and AACP staff.
BACKGROUND
The AAC conducted its work primarily using online platforms such as Zoom or GoToMeeting, given the restrictions on travel and in-person meetings brought about by the COVID-19 pandemic. The full committee initially met to discuss a plan for how to address all of the charges. The committee decided to break into three subgroups, with each group focusing on either charge two, three, or four. The full committee subsequently met virtually five more times to check-in on the work of the three subcommittees and perform group brainstorming. In addition, two meetings hosted by AACP and President Anne Lin were attended by members and staff liaisons from all the standing committees to hear updates from each standing committee chair and AACP staff.
Charge one was addressed at the beginning of the committee’s work and was valuable in providing information for this committee’s work to address the charges. The work generated for charges two, three and four serves as the foundation for recommendations to charge five. The 2020-2021 AAC offers one proposed policy statement, one recommendation for consideration by AACP, and several suggestions to schools and colleges of pharmacy related to the committee charges.
This report provides an overview of changes made by schools and colleges of pharmacy in response to the COVID-19 pandemic that may be continued to advance pharmacy education; a realistic model for colleges and schools of pharmacy to share resources to meet the curricular needs of member schools; and strategies by which schools and colleges of pharmacy can meet current and future workforce development needs, particularly in light of the changes in healthcare delivery as a result of the COVID-19 pandemic.
CHARGE 2: Determine what changes made in colleges and schools of pharmacy during the COVID-19 pandemic should be continued to advance pharmacy education
A survey titled “COVID-19 related changes for future pharmacy education” was created and sent out in early November 2020 to Associate Deans for Academic Affairs, Associate Deans for Student Affairs and current student pharmacists enrolled in a PharmD program at AACP member institutions. As of January 2021, the committee received 81 responses, representing 59 different member institutions. There were 54 responses (67%) from Associate Deans for Academic Affairs, 19 responses (23%) from Associate Deans for Student Affairs, and 8 responses (10%) from P3 and P4 student pharmacists. Survey respondents included a similar mix of public and private schools, with 42 and 39 responses respectively. The responses were reviewed by members of the 2020-21 AACP Academic Affairs Committee and compiled into a summary highlighting primary themes.
There were four open-ended questions on the survey:
With regard to the curriculum, what are unique ways that your institution has adapted because of COVID-19? (speak to the following: didactic lectures, laboratories, IPE courses, IPPEs/APPEs)
Of those adaptations from the previous question, which should continue after the pandemic and why?
With regard to student engagement activities, what are unique ways that your institution has adapted because of COVID-19? (speak to the following: orientation, admissions, formal ceremonies, student organizations, co-curricular activities, etc.)
Of those adaptations from the previous question, which should continue after the pandemic and why?
Based on the responses received, schools and colleges of pharmacy showed interest in continuing active learning strategies and team-based learning for student pharmacists. It was also clear that some virtual coursework was expected to continue in the future, particularly for electives, pre-lab work and small group discussions/facilitations. Respondents also noted how hybrid teaching models at schools and colleges of pharmacy have helped student pharmacists with self-directed learning, allowed for more adjunct faculty to teach within curricula, and opened opportunities for alumni and other healthcare providers to participate in interprofessional activities. This model has also allowed students with special needs, illnesses, and excused absences to watch recorded/live classes at home in addition to performing classroom activities remotely as required. It also proved a beneficial method for keeping students on schedule with coursework during inclement weather advisories which may result in school closures. Prioritizing the courses within the pharmacy curriculum that can be delivered in a hybrid teaching model was reported to be the key to delivering an efficient and effective learning environment for students. Strategic use of asynchronous coursework was important, as it was generally agreed that laboratories, IPPEs and APPEs should remain in-person activities unless extenuating circumstances arise.
Specific technologies that were mentioned and utilized to a great extent by survey respondents include:
Course management technology: Blackboard Collaborate Ultra, Canvas, Moodle, InteDashboard, D2L
Lecture capture: Panopto, Camtasia, Tegrity
Audience response systems: TopHat, TurningPoint, iClicker, Poll Everywhere
Electronic testing and proctoring: ExamSoft, Respondus, ExamMonitor or HonorLock
Web conferencing: Zoom, Google Meets, Microsoft Teams, Adobe Connect, WebEx
Document collaboration: Google Docs, SharePoint
Limited use of secure, remote proctoring software was mentioned by many administrators as having been successful this past year, and most stated that it will be continued in some form for students who may not be able to come to the classroom to take an exam. During this past year, of course, this technology was especially useful for minimizing exposure to students who may have felt ill or thought they might have COVID-19. Faculty administrators also mentioned the need for incorporating more digital health into curricula, especially with the expansion of telehealth in practice. As digital therapeutics, remote patient monitoring, and telehealth are fundamentally transforming how health care is delivered and consumed, colleges/schools of pharmacy need to effectively educate student pharmacists in these areas so that they are better prepared for the emerging workforce.
With regard to student engagement activities, many institutions adapted changes for admissions, including virtual interviews and pre-admission events. It was found that this increased overall turnout and allowed for students to interview who might not have otherwise been able to travel to campus. Many institutions also reported waiving the requirement for the Pharmacy College Admission Test (PCAT) based on the inability for applicants to take the exam, and some planned to continue this practice for the future. These changes align with the data AACP collected for the COVID-19 Pharmacy School Admission Policies report in spring 2021 for the 2021-2022 admissions cycle, which found 33% of institutions did not require the PCAT, 7% continued to require the PCAT, and the remaining 60% had the PCAT conditionally required, optional, or recommended.2
Many orientation activities for incoming students were offered virtually during the pandemic and are recommended to be continued in this manner. Money can be saved by eliminating print materials for students as well as reducing the need for snacks and meals. The means to communicate and gather in different forms/venues for student organizations were also found to be successful with virtual engagement. These included electronic newsletters and hybrid models for meetings. Use of virtual and in-person meetings allowed for adjunct faculty and alumni to participate while also increasing the pool of speakers available for student organization meetings. This model also decreased the need for on-campus rooms, organizations competing for space, and the burden of scheduling rooms. Additionally, ceremonies that were once in-person only were recommended to continue to be offered using a hybrid model to allow more family, friends, and potentially faculty, staff, and guest speakers to participate and join in the festivities. These may occur over platforms offering live streaming such as YouTube or Facebook Live, with an added bonus of being able to record.
Survey respondents also recommended continuing to allow for student advising and office hours to be offered virtually. This allowed for greater flexibility and increased opportunities to meet with students who may commute, be on rotations, and/or help students that have other struggles with meeting with faculty and staff in-person. Respondents also recommended to continue increased town hall forums to maintain engagement with students.
Offering students the ability to connect with employers and prepare for jobs and post-graduate positions changed as well during the pandemic and was recommended to continue. This included having a hybrid career fair event to connect employers with students. Additionally, students learned the value of having virtual mock interviews to prepare for real ones to obtain positions after graduation. With the ever-changing job market, these modalities helped students connect in new ways and increase the opportunities for their future.
SUGGESTION 1. Schools and colleges of pharmacy should continue to investigate where the virtual or hybrid model is most beneficial with regard to curricula and student engagement, while still meeting ACPE standards. Future research and scholarly activities should be conducted to determine if evidence supports continuing pandemic-related adaptations for curricular and student engagement to advance pharmacy education.
CHARGE 3: The COVID-19 pandemic demonstrated the need for colleges and schools of pharmacy to share and work together. Develop a realistic model for colleges and schools of pharmacy to share resources to meet the curricular needs of member schools.
The start of the COVID-19 pandemic abruptly changed the delivery of pharmacy education, including didactic, experiential, and co-curricular experiences. This sudden change prompted many questions regarding the availability of curricular resources to ensure continuity of exceptional pharmacy education. Committee members were charged to explore models for sharing resources to meet curricular needs of member schools – not just regarding content but also in terms of faculty expertise. The ability for schools and colleges of pharmacy to obtain expertise related to educational content remains a continual need within the Academy. For example, should a faculty member become unexpectedly unavailable or gaps in educational programs required to meet accreditation standards be identified, schools and colleges of pharmacy may seek to formally partner with another institution to deliver the educational content in place of hiring a new faculty member. Additionally, financial constraints may limit the ability to hire a full-time employee but may allow for the contractual “purchasing” of faculty time to teach specific coursework.
Committee members initially researched available models to share educational content, including those outside of pharmacy education. MedEdPORTAL provides one such example of a curation of teaching and learning resources for health professionals.3 Discussion also ensued regarding possible engagement with other health professional programs and professional organizations. Ultimately, committee members refocused the search to determine how schools and colleges of pharmacy could collaborate to extend resources to other programs beyond educational content to include faculty, teaching, and experiential site connections.
Ideally, the soon-to-be developed AACP Center to Accelerate Pharmacy Transformation and Academic Innovation (CTAP) can help to facilitate the sharing of resources in an organized manner. However, until this Center is fully operational, a short-term solution needs to be identified. Committee members felt that utilizing AACP Connect for this purpose would allow members easy access to content, since anyone can choose which communities to join. A variety of Connect Communities are currently available for sharing resources and posting discussions. Special Interest Groups (SIGs) and Sections of AACP coordinate content within specific Connect Communities, and still other groups provide resources for identified needs of the organization. These communities allow members to post questions and engage in discussions as well as share documents and resources. Developing a new Connect Community called the “Pharmer’s Market” was discussed; however, this would create yet another location within AACP Connect for members to search and post resources. It would also require new leadership (chair, knowledge management secretary, content users, etc.) from year-to-year to continue engaging members and curating resources.
As such, the committee approached the AACP Curriculum SIG as a resource partner to integrate the “Pharmer’s Market” into an already existing community. Enhancements within this particular SIG will allow easier organization and submission of resources into appropriate categories. Search processes will be improved, particularly with expanding options for tagging documents and posts within AACP Connect. Communications will focus on encouraging AACP members to join the Curriculum SIG and begin contributing to discussions and library resources. Faculty will be encouraged to post individual teaching needs at their institution in order to connect with other faculty who may be able to assist. Current recommendations for organization of content include:
Didactic curriculum (required and elective opportunities)
Co-curriculum
Experiential education
Interprofessional education
Other (student skills, competencies, online teaching and learning tools)
As previously mentioned, the ideal plan is for CTAP to eventually serve as a clearinghouse for member institutions willing to share educational offerings (eg, courses, rotations) to help meet the curricular needs of other member institutions on a regular and consistent basis. Information that would be collected would include: type of educational offering (ie, module, course, rotation, etc.); semester availability for the course to be offered to the outside institution; basic outline/syllabus of content; applicable ACPE standards met by the offering; name and contact information of institution representative. Prior to agreeing to post information, institutions offering content should: ensure willingness and availability of faculty member(s) to offer course/content in the listed semester; ensure collaborators share enough relevant information/documentation to satisfy ACPE and university requirements; obtain department chair approval to allocate time for faculty member to teach the additional content; obtain CEO Dean buy-in to engage in a contractual agreement with another institution; determine a reasonable cost for providing the offering and agree upon an internal financial plan for the department/institution.
In order to maintain an accurate and up-to-date online database, AACP will need to confirm the educational offerings each year. Institutions will be asked to confirm all elements of the posting or offer updates as needed. Institutions who fail to update their offering will have it removed and be required to resubmit. In addition, this process should be reassessed on an ongoing basis to ensure efficiency and effectiveness in meeting member needs. An assessment of utilization and cost should be conducted each year in order to determine effectiveness and sustainability. Potentially, a small charge could be instituted to post an offering or for those offerings that are utilized by member institutions.
POLICY 1. AACP supports the collaboration and sharing of educational resources among member institutions and seeks to serve as a clearinghouse to assist member institutions with meeting curricular and educational needs and promoting academic innovation and collaboration.
RECOMMENDATION 1. AACP should, through the Center to Accelerate Pharmacy Transformation and Academic Innovation, serve as a clearinghouse to assist member institutions with meeting curricular and educational needs.
CHARGE 4: Create strategies by which colleges and schools of pharmacy can meet current and future workforce development needs particularly in light of the changes in healthcare delivery as a result of the COVID-19 pandemic
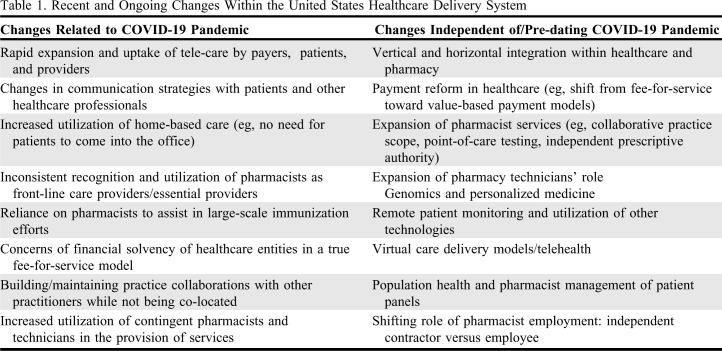
Changes in how healthcare is delivered and reimbursed in the United States (US) have been continually implemented over the years in response to increasing expectations from healthcare consumers in the areas of convenience, affordability, and quality.4 Additionally, Gen Xers and Millennials adopt technology at an increasingly rapid rate as compared to Baby Boomers.5 With an increasingly digitized society, there is a corresponding shift in people’s perspectives on how technology interplays with healthcare (eg, wearable technology, mobile applications, remote patient monitoring), with younger consumers being more likely than any other generation to choose medical providers who offer digital capabilities.4,6,7 Lastly, the COVID-19 pandemic has dramatically altered how the US healthcare delivery system operates by encouraging the incorporation of some of these technologies into routine practice. A summary of some of the most relevant changes identified by the committee can be found in Table 1.
Table 1.
Recent and Ongoing Changes Within the United States Healthcare Delivery System
Strategies by which schools and colleges of pharmacy can meet current and future workforce development needs are abundant. However, with curricular time, faculty and staff time, student stress, and other resources already stretched to the limit, it can be very difficult to envision piling on more. Rather than recommend a one-size-fits-all approach, the committee discussed various strategies that individual schools and colleges of pharmacy could tackle depending on their institution’s specific situation. The four major focus areas include: 1) faculty and staff development, 2) school/college of pharmacy leadership team discussions, 3) education and training for current students, and 4) education and training for alumni and other practitioners.
School/College of Pharmacy Faculty and Staff Development
The changes occurring within the US healthcare delivery system are too important to only be discussed by the curriculum committee or select group of faculty members; rather, an “all hands on deck” approach is required. To start, the topic of “ongoing changes within the US healthcare delivery system and workforce development needs” should be integrated into routine professional development programming targeting all faculty and staff, not just pharmacy practice faculty interested in this topic. This is a topic that impacts the entire academic pharmacy enterprise, from applicant to alumnus. If all faculty and staff are not in tune with this topic, how can one provide sound advice during the admissions process, effectively mentor a student on career preparation, or provide the relevant context to material being taught throughout the entire curriculum? To that extent, these elements should be incorporated into relevant content across the entire curriculum in an integrated manner, not necessarily as an “add-on” topic tucked away within one course. This doesn’t necessarily need to be an arduous task; simply asking oneself “how is this content impacted by ongoing changes in the US healthcare delivery system?” when developing any curricular content would be a good start. In addition to ongoing professional development programming, developing a repository of resources for faculty, staff, and students to easily access could also help ensure these topics are front of mind for everyone. Such a repository could exist on a school website or within the institution’s online learning management system. Lastly, faculty and staff should regularly discuss “how is our program preparing students for future workforce needs?” (eg, component of annual retreat, dedicated agenda topic for one faculty meeting per year).
School/College of Pharmacy Leadership Team Discussions
The program’s leadership team must also dedicate time and energy to discussing this important topic. Not every program will be able to address this issue in the same manner. Therefore, it is imperative for each program to identify their program-specific priorities related to ongoing changes in healthcare delivery and workforce development needs, taking into consideration such aspects as availability of resources, identification of collaborating partners, local/regional practice opportunities and barriers, and the program’s mission, vision, and values. Each school and college of pharmacy should evaluate their impact on pharmacy practice in the region, and leverage their influence wherever and whenever possible to maximize opportunities and remove barriers to pharmacist practice advancement. Focusing only on the pipeline of candidates entering a program will not be of any value if the opportunities for graduates are significantly limited. Lastly, the topic of entrepreneurship should also be considered during the admissions process - is the program-specific recruitment and admissions process encouraging entrepreneurial and “gritty” individuals who are comfortable taking calculated risks and may thrive in a dramatically changing healthcare market, or is the process biased against these individuals in some way?8
Education and Training for Current Students
Career Preparation
Today’s job market requires significantly more time, energy, and structured programming than what has generally been needed or offered by pharmacy programs in the past.9 The residency application process gets more competitive each year, with the number of applicants continuing to exceed the number of positions available.10 Furthermore, employers are not necessarily reaching out to future graduates as aggressively as they have in the past, placing the onus of the job search entirely on the shoulders of the novice student. Schools and colleges of pharmacy should consider collaborating with a career center or career coaching services, or even establish a center of their own if resources allow for it. Within the curriculum and co-curriculum, students must have the ability to develop their “employability skills” and entrepreneurial skills, as these are the characteristics routinely sought after by employers, regardless of practice setting.11,12 In addition, providing some initial instruction and ongoing coaching on interviewing and self-marketing skills would also be tremendously valuable to students. Schools and colleges of pharmacy may consider partnering with their alumni association, state pharmacy association, and/or social media networks to connect students with alumni and other current practitioners for additional mentorship on pharmacy careers and professional development.
Educational Content
As mentioned earlier within this report, the reality of adding more content to an extremely full curricular schedule seems impossible. However, the committee discussed a wide variety of content that would be helpful for incorporating into the curriculum, either integrated within some existing content/activities and/or replacing some outdated content. For example, within the skills lab, replacing one or more face-to-face OSCEs with a tele-video OSCE can provide an opportunity for the student to practice with communication methods used when providing care via telehealth, without requiring any additional time within the curriculum. Some ideas for relevant topic areas to incorporate include:
Identifying and using HIPAA-compliant communication methods
Interacting with and caring for patients virtually
Developing and justifying a telehealth service
Collaborating with other healthcare professionals remotely/virtually
Developing one’s digital knowhow12
Creativity and entrepreneurship12
Reimagining work across the enterprise with digitalization and automation13
Pharmacy informatics, personalized medicine and management principles and capability - shifting from knowledge acquisition to application
How to stay up to date with technology updates and changes in healthcare delivery model
The “Fourth Industrial Revolution” - the intersection of the physical, digital, and biological spheres14,15
Becoming an independent contractor - helping practitioners practice pharmacy without a direct employer
Networking and professional socialization (including via virtual means)
Although there may be a role for elective coursework in these areas, it must be emphasized that these are topic areas and skills that will impact all graduates in the near future, if not now. Another strategy that can be utilized is to develop or adopt an existing certificate program or other readily available training program to be integrated within or in addition to existing curricular content. The source of this programming does not necessarily need to be from within pharmacy; there is plenty available in other fields that can be applied and/or adapted to pharmacy (eg, business, information technology, engineering).
Education and Training for Alumni or Other Practitioners
The 2019-2020 AAC previously identified the ideal principles, characteristics, and design elements of a high-quality workforce development program, in addition to providing an overview of the current mechanisms in place for developing the current workforce.16 Alumni and other pharmacist practitioners can certainly benefit from most if not all of the recommendations provided above under the student emphasis. However, the committee also acknowledged that the existing workforce does have unique needs and circumstances compared to the average student pharmacist. For the existing pharmacy workforce, application-based programming that provides true hands-on practice with these complex topics would be most valuable. Some example topics to consider when offering such programming include:
How to effectively manage people (eg, employees, technicians, pharmacists, other staff, patients)
Best practices for practicing during a health emergency
Best practices for educating oneself in an area that is changing rapidly and information is quickly outdated (eg, COVID-19)
How to develop and maintain a team (with an emphasis on dispersed working environments)
How to engage in true continuous professional development
The format for this programming can vary, depending on the desired outcomes and the amount of resources available. Ideally, the format would include a longitudinal approach, with multiple opportunities for reflective practice and specific feedback. Some example formats to consider may include:
Experiential-type programming: opportunity for practicing pharmacists looking to upskill in a specific area (similar to an APPE, but for practicing pharmacists)
“Part-time” residency (eg, 0.5 FTE x 2 years): opportunity for individuals who have had their hours reduced with their current employer and/or work part-time and have the desire to upskill in a specific area
Professional certificate programs: opportunity to partner with professional associations and/or develop an entirely new program
Graduate certificate programs: offering coursework applicable to pharmacists for university credit that is more robust than a professional certificate, but less intensive than a complete graduate degree program (eg, evaluating research, developing a new clinical service, managed care applications)
Lastly, it is important to also note that the 2019-2020 AAC also recommended AACP convene a stakeholder conference focusing on the need for large-scale pharmacist workforce development.16 Currently AACP is currently in the preliminary planning stages with several other organizations to convene such an event, targeting early 2022 for a meeting date.
SUGGESTION 2. The Academic Affairs Committee endorses the following suggestion proposed by the 2020-2021 Argus Commission: Schools and colleges should develop strong partnerships with professional organizations to provide career development training, with emphasis on chronic disease state management, understanding pay-for-value healthcare financing models, and use of data analytics.
SUGGESTION 3. The Academic Affairs Committee endorses the following suggestion proposed by the 2020-2021 Argus Commission: Academic pharmacy should expand research efforts to identify, define and implement practice models that support interdependent collaborations between medical providers and pharmacists in distant settings (eg, not co-located).
SUGGESTION 4. Schools and colleges of pharmacy should integrate the topics of “ongoing changes within the US healthcare delivery system” and “ongoing workforce development needs” into routine professional development programming targeting ALL faculty and staff (ie, >/= one time per year).
PROPOSED POLICY STATEMENTS, RECOMMENDATIONS AND SUGGESTIONS
Proposed Policy Statement 1. AACP supports the collaboration and sharing of educational resources among member institutions and seeks to serve as a clearinghouse to assist member institutions with meeting curricular and educational needs and promoting academic innovation and collaboration.
Recommendation 1. AACP should, through the Center to Accelerate Pharmacy Transformation and Academic Innovation (CTAP), serve as a clearinghouse to assist member institutions with meeting curricular and educational needs.
Suggestion 1. Schools and colleges of pharmacy should continue to investigate where the virtual or hybrid model is most beneficial with regard to curricula and student engagement, while still meeting ACPE standards. Future research and scholarly activities should be conducted to determine if evidence supports continuing pandemic-related adaptations for curricular and student engagement to advance pharmacy education.
Suggestion 2. The Academic Affairs Committee endorses the following suggestion proposed by the 2020-2021 Argus Commission: Schools and colleges should develop strong partnerships with professional organizations to provide career development training, with emphasis on chronic disease state management, understanding pay-for-value healthcare financing models, and use of data analytics.
Suggestion 3. The Academic Affairs Committee endorses the following suggestion proposed by the 2020-2021 Argus Commission: Academic pharmacy should expand research efforts to identify, define and implement practice models that support interdependent collaborations between medical providers and pharmacists in distant settings (eg, not co-located).
Suggestion 4. Schools and colleges of pharmacy should integrate the topics of “ongoing changes within the US healthcare delivery system” and “ongoing workforce development needs” into routine professional development programming targeting ALL faculty and staff (ie, >/= one time per year).
CONCLUSION
The higher education, healthcare, and pharmacy practice landscapes were all already undergoing significant transformations prior to the pandemic, and will undoubtedly continue to change dramatically in the aftermath of the pandemic. As member institutions enter this “new normal”, it will be important to evaluate the outcomes of all the significant changes and adaptations that have been implemented in the past year in order to know what has been helpful for advancing pharmacy education and retaining those elements. To assist with the long-term aspects of implementing these changes, the committee has proposed one policy statement, one recommendation, and four suggestions related to our charges.
REFERENCES
- 1.Sorensen TD, Lin A. Address of the 2020-2021 president and immediate past president to the first house of delegates at the 2020 virtual annual meeting of the American Association of Colleges of Pharmacy. Am J Pharm Educ. 2020;84(10):8370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.COVID-19 Pharmacy School Admissions Policies. https://www.pharmcas.org/covid-19/. Accessed April 12, 2021.
- 3.Association of American Medical Colleges. MedEdPORTAL 2021. https://www.mededportal.org/. Accessed February 19, 2021.
- 4.Safavi K, Kalis B. Today’s consumers reveal the future of healthcare. Accenture Consulting. https://www.accenture.com/us-en/insights/health/todays-consumers-reveal-future-healthcare. Published February 12, 2019. Accessed April 10, 2021.
- 5.Vogels EA. Millennials stand out for their technology use, but older generations also embrace digital life. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/. Published September 9, 2019. Accessed April 10, 2021.
- 6.Digital’s imprint in health care: changing lives for the better. Stefanini Group. https://stefanini.com/en/trends/news/digital-imprint-in-health-care-changing-lives-for-the-better. Published July 17, 2019. Accessed April 10, 2021.
- 7.Ripton JT. How Millennials and Generation Z are driving the digital healthcare revolution. Am J Manag Care. https://www.ajmc.com/view/how-millennials-and-gen-zers-are-driving-the-digital-healthcare-revolution. Published October 22, 2019. Accessed April 10, 2021.
- 8.Shaikh NF, Nili M, Dwibedi N, Madhavan SS. Initial validation of an instrument for measuring entrepreneurial and intrapreneurial intentions in student pharmacists. Am J Pharm Educ. 2020;84(7):7624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ives RC, Klein KC, Mason NA. Career and professional development services for pharmacy students. Curr Pharm Teach Learn. 2020;12(9):1110-1115. [DOI] [PubMed] [Google Scholar]
- 10.American Society of Health System Pharmacists. Summary results of the Match for positions beginning in 2020 combined Phase I and II applicants. National Matching Services Inc. https://natmatch.com/ashprmp/stats/2020applstats.pdf. Accessed April 10, 2021.
- 11.Medina MS, Schwier NC, Miller JL, Miller MM, Skrepnek GH. Career skills assessment in a doctor of pharmacy curriculum. Am J Pharm Educ. 2018;82(7):6300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The future of the workforce: critical drivers and challenges. Deloitte. https://www2.deloitte.com/content/dam/Deloitte/au/Documents/human-capital/deloitte-au-hc-future-of-workforce-critical-drivers-challenges-220916.pdf. Published July 2016. Accessed April 10, 2021.
- 13.Reimagining Human Resources (HR): the future of the enterprise demands a new future of HR. Deloitte. https://www2.deloitte.com/content/dam/Deloitte/us/Documents/human-capital/us-human-capital-the-future-of-the-enterprise.pdf. Published 2019. Accessed April 10, 2021.
- 14.Schwab K. The Fourth Industrial Revolution: What it means and how to respond. World Economic Forum. https://www.weforum.org/agenda/2016/01/the-fourth-industrial-revolution-what-it-means-and-how-to-respond/. Published January 14, 2016. Accessed April 10, 2021.
- 15.The future of jobs: employment, skills, and workforce strategy for the Fourth Industrial Revolution. World Economic Forum. http://www3.weforum.org/docs/WEF_Future_of_Jobs.pdf. Published January 2016. Accessed April 10, 2021.
- 16.Bzowyckyj AS, Crabtree B, Framson K, et al. Report of the 2019-2020 AACP Academic Affairs Committee: developing the pharmacist workforce for society’s medication use needs in 2030. Am J Pharm Educ. 2020;94(10):8203. [DOI] [PMC free article] [PubMed] [Google Scholar]