Abstract
Introduction
The increasing burden of non-communicable diseases and limited public financing are major challenges facing health care systems in Latin America. Although COVID-19 severely impacted the Brazilian health care system, it is crucial to further characterize the degree of disruption caused to public health efforts, in order to address and manage long term effects of this pandemic. We therefore quantified the demand for preventive and treatment services from the Brazilian Unified Health System (Sistema Único de Saúde/SUS) in 2020 to evaluate potential repercussions of COVID-19 in this setting.
Methods
Using the SUS database, we compared preventative and treatment services rendered in 2020 to the same services rendered from 2017 to 19. We also evaluated the frequency of respiratory infection (RI) diagnoses during the pandemic, relative to the preceding years.
Results
Compared to 2017–19, in 2020 non-urgent medical appointments decreased 1.4-fold (p = 0.0017), dental consultations 2.8-fold (p = 0.05), and immunization coverage 1.5 fold (p = 0.0005). The number of RI visits to SUS ambulatory care units in 2020 was 4.2 times higher than in preceding years (p = 0.0014), with a peak of 280,898 diagnoses in July 2020.
Conclusion
The COVID-19 pandemic appears to have led to a dramatic decline in preventative and treatment services provided by SUS to the Brazilian population. Our findings may aid decision-makers in formulating policies to increase the availability of outpatient services in the aftermath of the pandemic. Counter measures will be critical to avoid a resurgence in vaccine-preventable diseases and complications stemming from non-communicable, chronic health conditions.
Keywords: Public health, Vaccination, COVID-19, Immunization, Public policy
1. Introduction
The SARS-CoV-2 epidemic, first reported in December 2019, soon became a full-scale global pandemic with a devastating impact on Latin America, particularly Brazil. In December 2021, Brazil ranked third in the number of SARS-CoV-2 infections worldwide and second only to the U.S. in number of deaths due to COVID-19 (Center for Systems Science and Engineering (CSSE) at Johns Hopkins University, 2021). The rapid spread of COVID-19 in Brazil was attributable to multiple factors, including urban density, timing of implementation of social distancing policies, and limited testing capacity (Monteiro de Oliveira et al., 2020). A large percentage of the Brazilian population live in urban, low-income settlements, often with minimum sanitation and limited access to private and public health care, which compounded COVID-19 prevention efforts (Rocha et al., 2021; Galassi et al., 2021). In addition, during the current pandemic, an oversaturated health care system often turned patients away from the hospital, contributing to an increasing number of preventable deaths (de Andrade et al., 2020).
Although Brazil historically has maintained a solid public health care system and has experience in managing epidemics such as dengue, Chikungunya, Yellow Fever and Zika virus, pandemic preparedness during COVID-19 suffered immensely due to the lack of a consistent centralized approach in preventing disease spread. Although Brazil always excelled in its national immunization program, the failure to administer effective top-quality vaccines against SARS CoV-2 rapidly facilitated viral spread and mutation, with multiple surges due to variants of concern across the country, leading to a tremendous, unacceptable death toll. Availability of SARS CoV-2 testing in public settings has also been unfortunately inconsistent and limited, while the cost of testing in pharmacies or private laboratories far exceeds what the average citizen can afford. Therefore, the official numbers of COVID-19 cases most certainly greatly underestimate the number of infections given difficulties in accessing testing. Although Brazil has the largest public health network in the world, tertiary care for severely ill COVID-19 patients in critical care units is not universally available with a frequent shortage of beds. The abysmal number of COVID-19 cases in Brazil reflects an unfortunate failure in preventative health care efforts. Consequently, an extraordinary number of COVID-19 cases have ravaged the country and overburdened existing health systems.
The Brazilian Unified Health System, also known as SUS (Sistema Único de Saúde), which, as previously noted, is the largest public health system in the world, is confronting its first pandemic in the 21st century. COVID-19 is likely the most dramatic challenge SUS has ever faced in its 31 years of existence, with the current death toll vastly exceeding that of past Brazilian epidemics (Castro et al., 2021). SUS is responsible for the health care of roughly 75% of Brazilians, and is funded through contributions from federal, state, and municipal budgets, through a health system that encompasses both public and private health care facilities as well as medical providers (Histórico de Cobertura da Saúde da Familia, 2021). Through SUS, health services and commonly-used medications, as well as most vaccines, are offered free of charge to all citizens in the country. SUS also provides laboratory, imaging, and other ancillary services (Histórico de Cobertura da Saúde da Familia, 2021).
One major hallmark in the history of SUS was the development of the Family Health Care Program (FHP) in 1994, which focused on preventative services. Initially developed in northeastern Brazil to improve maternal health and infant outcomes, FHP eventually evolved into a robust program of primary health care delivery involving interdisciplinary teams and community health outreach workers responsible for a vast network of services that provide health care to over 2/3 of the Brazilian population (Macinko and Harris, 2015). Services have gone beyond strict medical care and encompass dental care, nutritional services, social worker support, pharmaceutical services, physical therapy and public health interventions, such as contact tracing and immunizations (Castro et al., 2019). FHP, also known as the Family Health Strategy, has been responsible for the reversal of poor patient outcomes since its inception, including dramatic reductions in infant mortality and adverse pregnancy outcomes (Rocha and Soares, 2010).
Despite challenges since its inception in the 1990s, SUS has improved health equity across the country, increasing life expectancy at birth (Paim et al., 2011) by drastically reducing maternal and childhood mortality, and expanding immunization coverage. Much of its success in improving primary health care access derives from a robust program employing health agents and domiciliary visits. Nevertheless, since the beginning of the COVID-19 pandemic, these achievements have been negatively impacted, especially in states where structural poverty remains a large burden (Szwarcwald et al., 2011). We conducted the present analysis to assess how the COVID-19 pandemic has impacted SUS primary care to anticipate longer term effects of this disruption on public health. We focused on specific health care parameters abstractable from SUS databases in Brazil.
Since March 2020, when the COVID-19 pandemic first struck the country, Brazilians witnessed an unraveling of many of the health benefits achieved by SUS and affiliated FHP services (Takemoto et al., 2020). The present analysis was conducted to evaluate the direct and indirect repercussions of the COVID-19 pandemic on preventive health care services offered by SUS. FHP-affiliated health centers, hospitals and providers are presently battling misinformation, underfunding, and public mistrust, while attempting to maintain the availability of preventative health care for the most vulnerable populations during the pandemic. Such services are crucial for implementation of effective COVID-19 vaccination strategies in addition to overall maintenance of population health.
2. Methods
We evaluated public health records available through the public SUS database (DATASUS) to assess health services provided from the months of March to December each year from 2017 to 2020 for the entire country of Brazil. The following parameters were evaluated: (1) Primary health care services provided by SUS from March 2017 to 2020. These included the average number of monthly medical and dental consultations at SUS primary care facilities, the average number of monthly home visits carried out by health professionals based at SUS primary care facilities, and immunization coverage measured as vaccine doses provided at SUS primary care facilities from 2017 to 2020. We calculated total immunizations for all twelve months of the year because these are impacted by vaccine campaigns, and therefore monthly estimates are not as reflective as yearly estimates; (2) Elective hospitalizations at SUS medical units from March to December 2017–2020. This analysis included evaluation of non-medical emergency procedures performed at SUS and SUS-affiliated facilities from March to December 2017 to 2020; (3) Number of respiratory infections (RI) reported from 2017 to 2020 diagnosed at SUS primary health care facilities from March 2017 to 2020. This parameter was included to gauge the potential impact of SARS CoV-2 respiratory symptoms in ambulatory SUS services across Brazil in 2020 as compared to the average number of visits for respiratory symptoms in the three preceding years.
-
(1)
Evaluation of primary health care services provided by SUS, 2017–2020. Through the SISAB database (Sistema de Informação em Saúde para a Atenção Básica/ Health information federal surveillance system for primary care, which covers all patients registered in SUS) (Sistema de Informação em Saúde para a Atenção Básica (SISAB), 2021), we compiled data on scheduled monthly medical appointments from March 2017 to 2020. Two types of non-emergency scheduled medical appointments were selected: routine consultations and follow-up appointments. We calculated the average number of monthly appointments from March 2017 to 2020 as well as the standard deviation and standard error for each year. The analysis included data from the entire country.
-
(1.1)
Dental Consultations in SUS Primary Care Facilities from 2017 to 2020 were also evaluated. For this analysis, initial dental consultations, follow-up appointments, and maintenance appointments (appointments scheduled six months after dental treatment was completed) were considered. The median number of appointments per month was calculated, with the median monthly number of visits in 2020 compared to the three prior years for all of Brazil.
-
(1.2)
Domiciliary Visits from SUS Primary Care Facilities, 2017 to 2020. Utilizing the same SISAB database, we tallied the number of home visits by healthcare teams for 2020 and compared it with the three prior years by analyzing the average number of monthly home visits from 2017 to 2020. This analysis was performed for the entire country.
-
(1.3)
Immunization coverage as measured by vaccine doses administered at SUS Primary Care Facilities, 2017–2020. For this analysis, surveillance data from the Ministry of Health through the Information Technology Department of the Public Health Care System (DATASUS) (Departamento de Informática do SUS (DATASUS), 2021) was used. We analyzed immunization campaigns all over the country, including the annual “Influenza Vaccination Campaign” period from March 11th to May 31st, which in 2020 was extended until June 30th because of lack of adherence. Doses of vaccines provided in 2020 were compared with the number of doses provided during the three preceding years. The following vaccines which are provided free of cost through SUS were considered: Bacillus Calmette–Guérin (BCG), Yellow Fever, Hepatitis A (HepA), Hepatitis B (Hep B), Influenza (INF), Varicella, Diphtheria & Tetanus toxoid (DT), Diphteria, Tetanus toxoid and Acellular Pertussis (DTaP), Inactivated Polio Vaccine (IPV), Meningococcal C Conjugate (Men-C), Oral Polio Vaccine (OPV), Oral Human Rotavirus Vaccine, Pentavalent Vaccine (DTP whole cell-Hep B-Hib (PRP-T)), Measles, Mumps, Rubella, Varicella (MMRV), and Human Papillomavirus (HPV) quadrivalent gender-specific vaccine. The total number of vaccine doses provided across the years were included in this analysis.
-
(2)
Evaluation of Elective Monthly Hospitalizations at SUS medical units, 2017–2020. Data encompassing elective monthly hospitalizations, including all non-emergency medical procedures from 2017 to 2020 were obtained from surveillance data of the Brazilian Ministry of Health available from DATASUS.
-
(3)
Respiratory Infection (RI) diagnoses reported from 2017 to 2020 at SUS Primary Care Health Facilities. Data was collected from SISAB. Using this database, ICD codes (International Classification of Diseases) and ICHPPC codes (International Classification of Health Problems in Primary Care) presumably associated with COVID-19 and known co-morbidities (Zhu et al., 2020) were collected and analyzed. These included the following codes: ICHPPC (R05) Cough, ICHPPC (R81) Pneumonia, ICD (U04) SARS ICD (U049) Severe Acute Respiratory Syndrome [SARS], Not Specified, ICHPPC (R74) Acute Respiratory Infection, ICHPPC (A03) Fever, ICD (J12) Viral Pneumonia not Classified as other Disease, ICD (J110) Influenza [with Pneumonia, Due to unidentified virus] ICD (J100) Influenza with Pneumonia due to other virus not Influenza identified, ICD (J128) Other Viral Pneumonias, ICD (J129) Viral Pneumonia Unspecified] ICD (J16) Pneumonia due to other infectious microorganisms specified – unclassified, and ICD (J168) Pneumonia due to other infectious microorganisms specified.
We compared the mean number of monthly consultations, home visits, immunizations, admissions, and RIs in 2017–2019 to 2020 using paired t-tests. Statistical analysis was performed using R 4.0.4.
3. Results
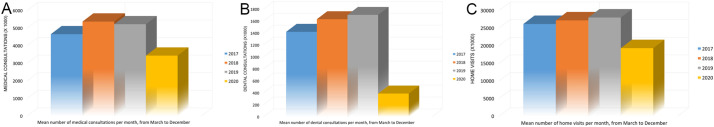
A significant decline in the number of monthly medical consultations in SUS Primary Care Facilities across Brazil was observed when the period of March–December 2017, 2018 and 2019 was compared to the same months in 2020, according to the performance metrics for primary health care services rendered at SUS facilities. As seen in Fig. 1A, there was a decline of roughly 30% in the monthly average of scheduled medical appointments: from 6 million in 2017–2019 to 4.3 million consults per month in 2020 (p = 0.0017). Similarly, an overall decrease in the number of SUS dental consultations was observed in 2020, in comparison to the three prior years (Fig. 1B). The number of average monthly dental consultations increased from 1.6 million in 2017 to 1.9 million in 2018 and remained stable in 2019 at 2 million consults, while in 2020 there was a sharp decline to 658,000 (p = 0.05).
Fig. 1.
A. Mean number of monthly medical consultations at primary health care facilities in Brazil March–December 2017–2020. B. Mean number of monthly dental consultations at primary care facilities in Brazil March–December 2017–2020. C.Title: Mean number of monthly SUS domiciliary visits across Brazil, March–December 2017–2020.
Domiciliary visits from SUS primary care facilities from 2017 to 2020 also decreased in 2020 (Fig. 1). The average monthly number of SUS home visits in 2020 was 231,725,756 (standard deviation, sd = 4,857,837), compared to the average number of visits for the three previous years of 325,302,664 (p = 0.0006). Prior to 2020, there was a yearly increase in the monthly average of domiciliary visits from 313,878,686 (sd = 4,061,518), in 2017, to 326,151,589 (sd = 4,936,025) in 2018 and 335,877,717 (sd = 5,094,383). in 2019.
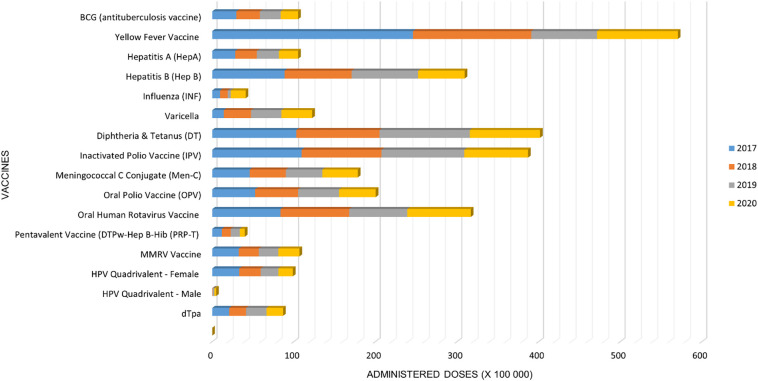
A dramatic decline in vaccination coverage was noted during the COVID-19 pandemic. Between 2017 and 2019, a monthly average of 80,466,342 vaccine doses were provided, as seen in Fig. 2 . In 2017, 90,826,817 (sd = 5,910,907) doses were administered, 78,926,866 doses (s = 3,966,345) in 2018, and 71,645,342 doses (sd = 3,321,479) in 2019. In contrast, in 2020, only 66,006,019 (sd = 2,910,905) vaccine doses were provided to the population, reflecting a 18% decline in vaccine doses administered during the first year of the COVID-19 pandemic (p = 0.0005).
Fig. 2.
Total number of vaccine doses administered by SUS in Brazil from 2017 to 2020.
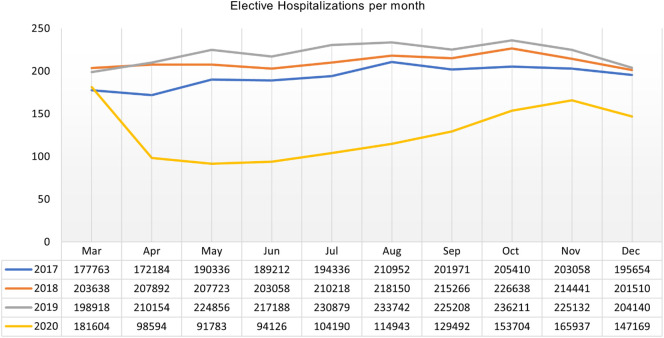
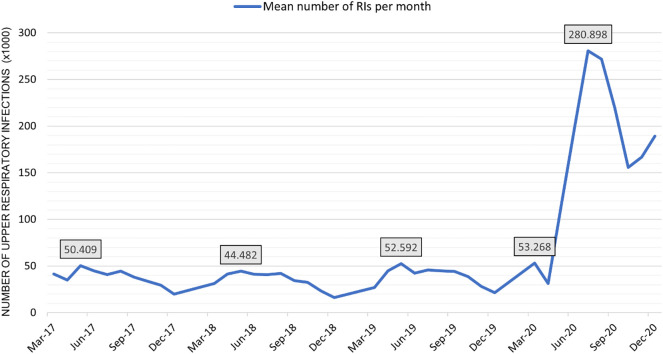
Elective hospitalizations and elective procedures also dramatically declined in 2020 across Brazil as compared to prior years (p = 0.001), as seen in Fig. 3 . The monthly average of elective hospitalizations and procedures in 2017 was 182,272 (sd = 16,820), 205,641 in 2018 205,641 (sd = 13,574), and in 2019, 215,704 (sd = 15,691). In contrast, in 2020, the monthly average of elective hospitalizations and elective procedures was 139, 830 (sd = 38,280). Conversely, in 2020 diagnoses of RIs sharply increased as compared to the three prior years. ICHPPC code R74, which corresponds to Acute Respiratory Infections, had the highest increase in the initial months of 2020 (Fig. 4 ). The average monthly number of RIs reported from SUS ambulatory facilities across Brazil in 2020 was 1,730,475 (sd = 94,298), which was 4.21 times greater than the average number of RIs reported for the previous years: 410,368, p = 0.0014 (411,339, sd = 11,467 in 2017, 385,078, sd = 20,449 in 2018 and 434,695, s = 11,153 in 2019). This increase clearly correlated with the escalation in the number of COVID-19 cases.
Fig. 3.
Number of elective non-emergent admissions to SUS hospital facilities per year from March–December 2017 to 2020.
Fig. 4.
Number of total cases of RIs diagnosed at SUS ambulatory facilities across Brazil from March–December 2017 to 2020.
4. Discussion
COVID-19 cases in Brazil were imported from individuals traveling abroad, with the first cases arising in early March 2020 (Candido et al., 2020). The cases were initially concentrated in the wealthiest municipalities and states. Subsequently, the epidemic rapidly spread throughout the country reaching the most vulnerable communities of Brazil's 5570 municipalities in 26 states and the Federal District (Ribeiro et al., 2020). By March 2021, all 5570 municipalities (100% of the Brazilian territory) had officially reported cases of COVID-19 (Ministério da Saúde, n.d.). Throughout 2020 measures to combat the pandemic in Brazil were relegated to the regional level, with state and county leadership often responsible for the development of medical/therapeutic guidelines. As of December 26, 2021, the country has reported 22.2 million confirmed cases and surpassed 618,000 deaths (Johns Hopkins University and Medicine. Coronavirus Resource Center, 2021). An ongoing major concern is how SUS will manage the unquestionable long-term burden that COVID-19 has placed upon the Brazilian health care system.
SUS is the pillar of health care in Brazil (Massuda et al., 2018). Any deficiencies in services provided by SUS dramatically affect the immediate health of the Brazilian population, likely with long-term effects. We observed an increase in services from 2017 to 2019 with overall increases in monthly medical consultations, dental consultations and home visits performed by SUS in the years preceding the pandemic. Although there were slight variations, with a notable increase between 2017 and 2018, the steep decline in visits noted in 2020 was unparalleled, and is likely attributable to the COVID-19 pandemic. Shut-downs, fear of acquiring COVID-19 in health care settings, and the overburdening of other health sectors led to a dramatic decline in individuals seeking ambulatory health care services. Thus, our analysis of SUS data demonstrates a dramatic decline in health parameters used to gauge delivery of preventative services in 2020. In parallel, it was clear that there was a dramatic increase in diagnoses associated with RIs in SUS ambulatory care across the whole country. Diagnoses in emergency services were not evaluated, because the impact of COVID-19 on emergency care was not captured by the official databases. The pronounced decline in scheduled ambulatory medical and dental appointments, and elective surgical procedures and elective admissions observed in 2020 will likely strain the health care system in the coming years.
The reduction of ambulatory clinical and dental visits in Brazil during the COVID-19 pandemic is likely severely impacting the delivery of health promotion and education, with implications for future generations, compromising, for instance, prenatal care at health care centers (Dashraath et al., 2020). Initial home neonatal visits with support for breastfeeding, usually provided by nurses to mothers unable to go to health care centers, were also adversely affected by the pandemic. In addition to the low number of medical consultations in general, there was a decrease in follow-up consultations to manage chronic diseases such as diabetes and arterial hypertension, thus increasing the likelihood of serious complications for patients suffering from these conditions (Grassi et al., 2020). The lack of home care visits and the increase in the number of COVID-19 cases prevent one-on-one health promotion and health education at community health centers for individuals of all ages (Jeet et al., 2017). This triggers a cascade effect where contact tracing for common infectious diseases is also compromised, as well as household risk assessments and guidance and control management of vector-borne diseases.
Dental care is considered one of the health services most severely affected by the COVID-19 pandemic. The fact that SARS-CoV-2 is transmitted person-to-person by inhalation or ingestion of droplets containing the virus poses a threat to dental health care teams. Most importantly, however, the impossibility of providing proper dental treatment during lockdowns adversely affects dental care. Tooth decay due to dental cavities is the most common noncommunicable disease worldwide (Peres et al., 2019). Reduction of dental assistance for the most vulnerable communities in Brazil may harshly impact the DMFT index of the population, which is an incremental measure of teeth decayed (D), missing (M) and filled (F). SUS provides free dental care for all age groups, from early childhood to seniors, which is subsidized by the federal government. The goal of the SUS oral health program is to evaluate the epidemiological situation of regional populations in order to offer preventive oral care as early as possible and avoid unnecessary increases in the DMFT index. Studies have shown that the prevalence of edentulism is high in Latin America (Kranz et al., 2015; Tyrovolas et al., 2016). These populations also have a disproportionately higher incidence of COVID-19 and are the most affected by the health policies in place. Tooth loss not only has functional, aesthetic, psychological, and social repercussions, but constitutes one of the most significant markers of social inequality among populations (Antunes et al., 2003). With dental care restricted to emergencies and fluoride applications, risk assessments and promotion of oral health care in community settings are severely undermined by the pandemic.
Our analysis showed that the COVID-19 pandemic also reduced elective admissions significantly. The most common elective hospitalizations in Brazil include cataract surgeries, cholecystectomy, and appendectomy, among others (Reis et al., 2021). The shortage of supplies, health personnel and escalating numbers of emergency hospitalizations due to COVID-19 were a consistent burden hampering elective procedures offered by SUS. In our study, by mid-April 2020, these procedures had already declined by 40% even before the peak of the first wave of the pandemic. The decrease in elective admissions is attributable to the shift in the direction of care towards comorbidities brought on by the pandemic, as well as an increased self-perception of risk and fear of contracting COVID-19 in the hospital environment.
A particularly concerning effect of the pandemic on the Brazilian primary care system was the dramatic decline in administration of vaccines in 2020. Reduce rates of vaccination against preventable illnesses may facilitate outbreaks of measles, influenza, diphtheria, and tetanus in the near future. Recent measles outbreaks in Brazil have been associated with a higher prevalence of intentionally unvaccinated individuals (Elidio et al., 2019). This is in stark contrast with prior achievements of Brazil's national immunization program, which over the years eradicated several vaccine preventable illnesses, due to implementation of SUS FHP initiatives (Rocha and Soares, 2010). However, even prior to the pandemic, the Oswaldo Cruz Foundation (FIOCRUZ) estimated that there was a 13.5% (Césare et al., 2020) decline in childhood immunizations in Brazil between 2017 and 2019. The added burden of COVID-19 on immunization coverage across the country requires urgent public health attention.
Finally, with health systems being overwhelmed with SARS-CoV-2 cases, it was not surprising to observe an over 300% increase in RI diagnoses in the SUS ambulatory setting in 2020. These RIs were not coded as COVID-19 cases, likely due to the scarcity of available testing across primary health care facilities. These cases were not counted towards the pandemic burden, which highlights how frequently COVID-19 cases may have been underestimated. Lack of contact tracing and decreases in home visits also made it more difficult to control the spread of SARS CoV-2, with an unprecedented number of new cases identified throughout 2020.
Our study has limitations in that data input into public databases was substantially delayed due to the pandemic, in some regions of Brazil more so than others, which may lead to more conservative estimates than anticipated. Nevertheless, data generated thus far already attests to the severe repercussions the pandemic has had on primary health care. Although much has been publicized about the dramatic effects of COVID-19 on emergency medical services and critical care, the devastating impact of the pandemic on preventative health services may unfortunately become apparent in the years to come. When the country eventually emerges from the COVID-19 abyss, considerable attention should be given to the rescue and re-establishment of primary health care services to protect the population from further harm and neglect.
Availability of data and materials
Data derived for this analysis is publicly available at the Brazilian Ministry of Health Coronavirus Panel at http://COVID.saude.gov.br
Funding
National Institutes of Health/ NIAID AI140718 and the UK Medical Research Council MR/V033530/1. MCC received support from NIH T32MH080634.
Authors' contributions
M.M., T.F., C.R.G, P.B., K.N·S performed the literature review, T.F. performed the dataset analysis. M.M., T.F., K.N·S. interpreted the data. M.M., T.F. and K.N.S wrote the first draft of the manuscript. All authors participated in critical review of the manuscript and contributed to the final manuscript product.
Competing interests
The authors declare that they have no competing interests.
Disclosure of financial conflict of interests
No financial disclosures were reported by the authors of this paper.
Acknowledgments
We confirm that the article content is original and has not been published anywhere, nor is it currently under consideration for publication elsewhere.
References
- Antunes J.L., Pegoretti T., de Andrade F.P., et al. Ethnic disparities in the prevalence of dental caries and restorative dental treatment in Brazilian children. Int. Dent. J. 2003 Feb;53(1):7–12. doi: 10.1111/j.1875-595x.2003.tb00649.x. [DOI] [PubMed] [Google Scholar]
- Candido D.D.S., Watts A., Abade L., et al. Routes for COVID-19 importation in Brazil. J. Travel Med. 2020 May 18;27(3) doi: 10.1093/jtm/taaa042. taaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro M.C., Massuda A., Almeida G., Menezes-Filho N.A., Andrade M.V., et al. Brazil’s unified health system: the first 30 years and prospects for the future. Lancet. 2019 Jul 27;394(10195):345–356. doi: 10.1016/S0140-6736(19)31243-7. (Epub 2019 Jul 11) [DOI] [PubMed] [Google Scholar]
- Castro M.C., Kim S., Barberia L., Ribeiro A.F., Gurzenda S., et al. Spatiotemporal pattern of COVID-19 spread in Brazil. Science. 2021 Apr 14 doi: 10.1126/science.abh1558. eabh1558. (In press) [DOI] [PubMed] [Google Scholar]
- Center for Systems Science and Engineering (CSSE) at Johns Hopkins University COVID-19 Dashboard. 2021. https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Accessed April 29.
- Césare N., Mota T.F., Lopes F.F.L., et al. Longitudinal profiling of the vaccination coverage in Brazil reveals a recent change in the patterns hallmarked by differential reduction across regions. Int. J. Infect. Dis. 2020 Sep;98:275–280. doi: 10.1016/j.ijid.2020.06.092. (Epub 2020 Jun 30) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dashraath P., Nielsen-Saines K., Madhi S.A., Baud D. COVID-19 vaccines and neglected pregnancy. Lancet. 2020 Sep 5;396(10252) doi: 10.1016/S0140-6736(20)31822-5. (Epub 2020 Aug 27) [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Andrade C.L.T., Pereira C.C.A., Martins M., Lima S.M.L., Portela M.C. COVID-19 hospitalizations in Brazil’s unified health system (SUS) PLoS One. 2020 Dec 10;15(12) doi: 10.1371/journal.pone.0243126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Departamento de Informática do SUS (DATASUS) 2021. http://tabnet.datasus.gov.br/cgi/dhdat.exe?bd_pni/dpnibr.def Accessed: April 25.
- Elidio G.A., França G.V.A., Pacheco F.C., et al. Measles outbreak: preliminary report on a case series of the first 8,070 suspected cases, Manaus, Amazonas state, Brazil, February to November 2018. Euro Surveill. 2019 Jan;24(2):1800663. doi: 10.2807/1560-7917.ES.2019.24.2.1800663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galassi F.M., Habicht M.E., Pate F.D., Varotto E. Flying higher than politics: the goal of preventive medicine at the time of the COVID-19 pandemic. Eur. J. Intern. Med. 2021;86:102–103. doi: 10.1016/j.ejim.2020.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassi T., et al. COVID-19, a viral endocrinological disease? Eur. J. Intern Med. 2020 Jul;77:156–157. doi: 10.1016/j.ejim.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Histórico de Cobertura da Saúde da Familia Brasilia, Brazil: Departamento de Atencao Básica. 2021. https://egestorab.saude.gov.br/index.xhtml Accessed April 29.
- Jeet G., Thakur J.S., Prinja S., Singh M. Community health workers for non-communicable diseases prevention and control in developing countries: evidence and implications. PLoS One. 2017 Jul 13;12(7) doi: 10.1371/journal.pone.0180640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins University & Medicine. Coronavirus Resource Center 2021. https://coronavirus.jhu.edu/data/mortality Accessed: April 25.
- Kranz A.M., Preisser J.S., Rozier R.G. Effects of physician-based preventive oral health services on dental caries. Pediatrics. 2015 Jul;136(1):107–114. doi: 10.1542/peds.2014-2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko J., Harris M.J. Brazil’s family health strategy--delivering community-based primary care in a universal health system. N. Engl. J. Med. 2015 Jun 4;372(23):2177–2181. doi: 10.1056/NEJMp1501140. [DOI] [PubMed] [Google Scholar]
- Massuda A., Hone T., Leles F.A.G., de Castro M.C., Atun R. The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Glob. Health. 2018 Jul 3;3(4) doi: 10.1136/bmjgh-2018-000829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministério da Saúde Secretaria de Vigilância em Saúde. Boletim Epidemiológico Especial. Doença pelo Coronavírus COVID19. Semana Epidemiológica 8 (21 a 27/2/2021) https://www.gov.br/saude/pt-br/media/pdf/2021/marco/05/boletim_epidemiologico_COVID_52_final2.pdf Accessed: April 25, 2021.
- Monteiro de Oliveira M., Fuller T.L., Brasil P., Gabaglia C.R., Nielsen-Saines K. Controlling the COVID-19 pandemic in Brazil: a challenge of continental proportions. Nat. Med. 2020 Oct;26(10):1505–1506. doi: 10.1038/s41591-020-1071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paim J., Travassos C., Almeida C., Bahia L., Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011 May 21;377(9779):1778–1797. doi: 10.1016/S0140-6736(11)60054-8. (Epub 2011 May 9) [DOI] [PubMed] [Google Scholar]
- Peres M.A., Macpherson L.M.D., Weyant R.J., et al. Oral diseases: a global public health challenge. Lancet. 2019 Jul 20;394(10194):249–260. doi: 10.1016/S0140-6736(19)31146-8. Erratum in: Lancet. 2019 Sep 21;394(10203):1010. [DOI] [PubMed] [Google Scholar]
- Reis T., Lansingh V., Ramke J., et al. Cataract as a cause of blindness and vision impairment in Latin America: progress made and challenges beyond 2020. Am J. Ophthalmol. 2021 Jan 4;225:1–10. doi: 10.1016/j.ajo.2020.12.022. [DOI] [PubMed] [Google Scholar]
- Ribeiro H.V., Sunahara A.S., Sutton J., Perc M., Hanley Q.S. City size and the spreading of COVID-19 in Brazil. PLoS One. 2020 Sep 23;15(9) doi: 10.1371/journal.pone.0239699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha R., Soares R.R. Evaluating the impact of community-based health interventions: evidence from Brazil’s family health program. Health Econ. 2010 Sep;19(Suppl):126–158. doi: 10.1002/hec.1607. [DOI] [PubMed] [Google Scholar]
- Rocha R., Atun R., Massuda A., Rache B., Spinola P., Nunes L., Lago M., Castro M.C. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob. Health. 2021;9 doi: 10.1016/S2214-109X(21)00081-4. e782-e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sistema de Informação em Saúde para a Atenção Básica (SISAB) 2021. https://sisab.saude.gov.br/ Accessed April 25.
- Szwarcwald C.L., da Mota J.C., Damacena G.N., Pereira T.G. Health inequalities in Rio de Janeiro, Brazil: lower healthy life expectancy in socioeconomically disadvantaged areas. Am. J. Public Health. 2011 Mar;101(3):517–523. doi: 10.2105/AJPH.2010.195453. (Epub 2011 Jan 13) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takemoto M.L.S., Menezes M.O., Andreucci C.B., et al. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int. J. Gynaecol. Obstet. 2020 Oct;151(1):154–156. doi: 10.1002/ijgo.13300. (Epub 2020 Jul 29) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrovolas S., Koyanagi A., Panagiotakos D.B., et al. Population prevalence of edentulism and its association with depression and self-rated health. Sci. Rep. 2016 Nov 17;6:37083. doi: 10.1038/srep37083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Ji P., Pang J., et al. Clinical characteristics of 3062 COVID-19 patients: a meta-analysis. J. Med. Virol. 2020 Oct;92(10):1902–1914. doi: 10.1002/jmv.25884. (Epub 2020 Jun 24) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data derived for this analysis is publicly available at the Brazilian Ministry of Health Coronavirus Panel at http://COVID.saude.gov.br