Abstract
Background
Depression and anxiety are two to four times more prevalent in people with CF (pwCF) than the general population. COVID-19 may exacerbate mental health challenges, increasing demand for psychological services, while decreasing their availability. We assessed the impact of the pandemic on depression and anxiety in pwCF, including how COVID-19 affected the frequency of mental health screening and the types of services provided.
Methods
A 38‐item internet survey, completed in June 2020, assessed how COVID-19 affected: 1) the mental health clinician's role and screening processes; 2) barriers to screening and resource needs; 3) impact of COVID-19 on depression and anxiety, and 4) positive outcomes and confidence in sustaining mental health screening and treatment, including telehealth services, after the pandemic.
Results
Responses were obtained from 131 of the 289 US CF programs. Overall, 60% of programs (n=79) continued mental health screening and treatment, although less frequently; 50% provided individual tele-mental health interventions, and 9% provided telehealth group therapy. Clinically elevated depression symptoms (PHQ-9≥10; moderate to severe), were found in 12% of 785 pwCF, with 3.1% endorsing suicidal ideation. Similarly, elevated anxiety (moderate to severe; GAD-7≥10) was found in 13% of pwCF (n=779).
Conclusions
The COVID-19 pandemic created an opportunity to implement innovative solutions to disruptions in mental health screening and treatment in CF programs. We found that pwCF had increased access to psychological interventions during the pandemic via telehealth, supporting the continued integration of tele-mental health screening and treatment into CF care.
Keywords: Cystic fibrosis, COVID-19, Depression, Anxiety, Telehealth
Abbreviations: CF, cystic fibrosis; CFF, Cystic Fibrosis Foundation; COVID-19, coronavirus disease 2019; GAD-7, generalized anxiety disorder 7-item scale; MHAC, Mental Health Advisory Committee; MHC, mental health coordinator; PHQ-9, patient health questionnaire 9; pwCF, people with CF
1. Introduction
Depression and anxiety are two to four times more prevalent in people with CF (pwCF) than the general population, according to a study of 6088 pwCF ages 12 years through adulthood and 4102 parent caregivers across nine countries [1]. Elevated symptoms of depression were found in 17% of pwCF, 37% of mothers, and 31% of fathers. Elevated anxiety was found in 30% of pwCF, 48% of mothers and 36% of fathers. Depression and anxiety take on greater significance in CF because they negatively impact disease self-management and health outcomes, including worse adherence [2,3], decreased health-related quality of life [4], [5], [6], and increased healthcare costs [7]. A positive depression screen is also associated with more frequent pulmonary exacerbations and increased mortality among adults with CF, particularly in those with severe depressive symptoms [8].
These findings led the Cystic Fibrosis Foundation (CFF) and European Cystic Fibrosis Society to develop international guidelines for mental health in CF which recommend annual screening for depression and anxiety in pwCF ≥12 years and parent caregivers using standardized screening tools. Algorithms were also developed which guide recommendations for evidence-based psychological and/or pharmacological interventions [9]. Implementation of these guidelines has been facilitated by establishing and supporting a standing national advisory committee (Mental Health Advisory Committee; MHAC) and creating grant-funded positions for a Mental Health Coordinator (MHC) in 138 of the 289 US CF programs (between 2015-2019). Beginning in 2020, the CFF expanded funding for an MHC to all CF programs and centers, with the amount of funding dependent on size of the center. In addition, MHCs were asked annually about their needs for training, which were systematically programmed into the national CF conference, further faciliating implementation of mental health screening and treatment as part of their program of CF care. To evaluate guideline dissemination efforts, the MHAC adapted and utilized the Consolidated Framework for Implementation Research [10], which indicated successful implementation across US CF programs [11].
As COVID-19 emerged across the US early in 2020, significant changes were made to healthcare delivery [12]. In CF centers, this included shifting clinic visits from in-person to telehealth and implementing staff redeployments and furloughs. A major aim of this study was to evaluate how these changes have affected implementation of mental health screening and treatment. In addition, the pandemic may have exacerbated mental health challenges for pwCF, who are uniquely vulnerable to a respiratory virus and faced uncertainty and potentially heightened anxiety about its impact on their physical and mental health. Thus, an additional aim was to evaluate the impact of COVID-19 on mental health in pwCF.
Early in the pandemic, several European studies assessed the effects of COVID-19 on pwCF. A survey study in Belgium reported heightened fear of exposure to the virus, increased symptoms of stress and depression, and problems with sleep and concentration [13]. A large Italian study also reported high levels of distress; however, elevated distress was also reported by community controls [14]. In a small, single center study in the UK, pwCF were adherent to “stay at home orders” and avoided outside contacts, but self-reported anxiety increased from 27% to 54% [15]. Similarly, a small intervention study in Italy during their “lockdown” found substantial rates of depression and anxiety in adolescents, young adults, and caregivers, with 20-40% reporting moderate to severe symptoms. These symptoms were mitigated by a four-session cognitive-behavioral telehealth intervention, which reduced stress and depression in both pwCF and parents [16]. Conversely, one study, in Turkey, found lower rates of anxiety in 45 adolescents with CF when compared to age-matched controls [17].
Most of these studies represented single centers, and to date, no studies have investigated the effects of COVID-19 on mental health for pwCF in the US. We sought to determine how COVID-19 affected mental health screening and treatment at CFF-accredited US programs, with an emphasis on the new role telehealth played in healthcare delivery. Barriers to screening and resource needs were documented, as well as the impact of COVID-19 on depression, anxiety, and suicidal thoughts in pwCF. Finally, we evaluated the positive outcomes of mental health screening and treatment, and providers’ confidence in their ability to sustain continued delivery of mental health services both during and after the pandemic.
2. Methods
2.1. Participants and procedure
CFF administered the internet survey via SurveyMonkey® to all 289 accredited US CF programs. The survey was emailed to CF program directors and coordinators (n=700), asking the MHC to complete the survey, if possible. The survey launched May 29, 2020, with a reminder sent on June 12, and closed on June 28, 2020.
2.2. Measure
The survey was developed by the CFF-sponsored MHAC, a multidisciplinary committee comprised of health care professionals (e.g., pulmonologists, psychologists, psychiatrists, social workers, nurses), adults with CF, and a parent of a child with CF. An iterative consensus process was used to create the 38‐item internet survey assessing mental health screening and treatment during the COVID-19 pandemic. Most responses were “check boxes” or numeric data (e.g., characteristics of the center, screening outcomes). Two open-ended questions elicited key barriers to sustaining tele-mental health services during and after the pandemic, and the resources most helpful for MHCs to continue screening and service provision.
2.3. Data analysis
The data were downloaded to SPSS version 26 and anonymized using a CFF-generated ID code, preventing identification of specific programs. Several duplicate entries were found using the ID, however, all but one of these occurrences included an adult and pediatric program at the same location, and were retained in the dataset. One program submitted three responses from different members of the team; the first response, from the MHC, was retained, and the other two were deleted. Data cleaning and coding ensured data quality: entries were checked to eliminate nonsense values and confirm that all values were within appropriate ranges. Multiple frequencies and mean rank ordering of appropriate items were generated. For questions that elicited the percentage of time engaged in activities, means and quartiles were determined. Open-ended responses were coded thematically. To assess reliability, two independent coders (BS, AM) identified and agreed on emergent themes, with a calculation of percent agreement.
3. Results
A total of 131 of the 289 US CF programs responded to the survey: 36% were pediatric programs, 24% adult, and 40% combined programs (pediatric and adult). CF program size was evenly distributed: 29% small programs (≤70 patients), 37% medium (71-140 patients), and 34% large (>140 patients). Similarly, responses were equally distributed across the US, and regional location was not related to response rate. Of these 131 CF programs, 46 (35%) had not received an MHC grant from the CFF between 2015-2019. The MHC's profession and average amount of time currently devoted to their role on the CF team are presented below (Table 1 ).
Table 1.
Descriptive information on MHCs.
| N | % | |
|---|---|---|
| Profession of MHC | ||
| Social Worker | 80 | 64 |
| Psychologist | 27 | 22 |
| Psychiatrist | 1 | 1 |
| Other (e.g., licensed professional counselor) | 17 | 13 |
| MHC: Full or Part-Time | ||
| Full-time | 39 | 30 |
| Part-time | 53 | 40 |
| No MHC* | 22 | 17 |
| Other (e.g., alternate team member devoting time to MHC duties)# | 17 | 13 |
| MHC Time—Pediatric | ||
| Up to 25% | 13 | 14 |
| 26%–50% | 27 | 30 |
| 51%–75% | 8 | 9 |
| 76%–100% | 42 | 47 |
| Mean % | 63 | |
| MHC Time—Adult | ||
| Up to 25% | 23 | 35 |
| 26%–50% | 14 | 21 |
| 51%–75% | 5 | 8 |
| 76%–100% | 24 | 36 |
| Mean % | 52 | |
Legend: The question on time asked specifically about effort (% of full time equivalent) devoted to the role of MHC by those who were currently filling that role.
Represents those who were furloughed or redeployed during the COVID-19 crisis and no one from the team was devoting time to MHC duties
Other member of the team (e.g., nurses, intake coordinators, etc.) who stepped in to fill MHC role
3.1. Impact of COVID-19 on mental health screening processes & MHC roles
In response to the COVID-19 pandemic, many CF programs changed their standard appointment processes, temporarily eliminating in-person visits, or limiting them to those experiencing urgent symptoms. Most programs provided regular CF clinic visits via telehealth. Slightly more than half of the MHC's (57%) continued interacting with patients in the same way as the rest of the clinic, but 43% developed a different schedule of visits or mode of service delivery (e.g., telephone, video telehealth visit), and some were furloughed or had their hours reduced. Many programs continued mental health screening during the pandemic (60%), all of which were using the PHQ-9 and GAD-7. However, the frequency of screening decreased overall during the pandemic, with 60% of centers reporting less frequent screening, 35% reporting the same frequency, and 5% increased frequency. Screening was conducted in a variety of ways, including videoconferencing (38.3%), via telephone (35.8%), in-person (24.7%), and through email (1.2%).
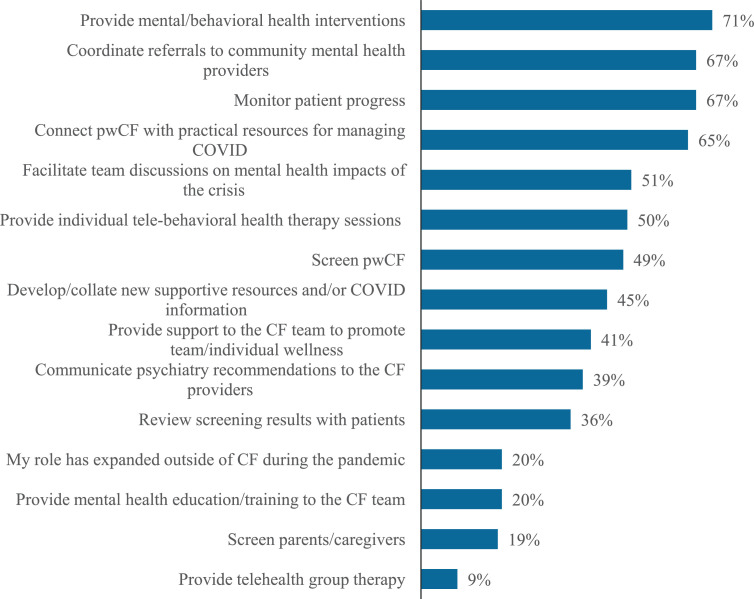
MHCs often continued previous responsibilities during the pandemic, and also took on new roles (Fig. 1 ). MHCs provided mental/behavioral health interventions via telehealth, coordinated referrals to community mental health providers, and monitored patient well-being. In addition, 41% began providing support to the CF team to promote wellness and reduce stress, and 20% offered mental health education training to CF team members. Although sample sizes were too small for comparisons, a consistent pattern emerged: adult programs were providing more of these services than pediatric programs.
Fig. 1.
MHC role during the pandemic.
Despite the substantial reduction in rates of screening, 71% of pwCF with elevated depression symptoms received psychological interventions in clinic and 67% were referred to community providers. This compares favorably with previous MHC survey data across the first 3 years of mental health guideline implementation, pre-pandemic [11,18,19]. In Year 1, with the initiation of MHC grants to 84 CF centers, 33% of patients with elevated symptoms of depression received psychological interventions in clinic and 17% were referred to community providers; in Year 2, interventions in clinic were provided to 75% of those with depressive symptomatology, with 12% referred to the community; in Year 3, when many centers were in their last year of grant support with no certainty of sustaining future funding, 47% of those with elevated symptoms of depression received interventions in clinic, with 31% referred to community providers. CFF subsequently initiated funding to all CF centers, programs, and affiliates to sustain at least part of the MHC role.
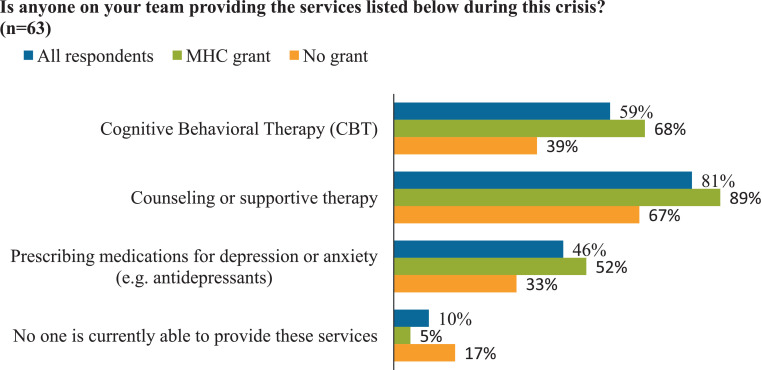
Given that providing tele-mental health interventions was a new role for most MHCs, respondents were asked specifically about the types of services their CF care teams provided. In adult programs, the most common services included providing counseling or supportive therapy (95%) and prescribing medications for depression or anxiety (95%), followed by cognitive behavioral therapy (CBT) (65%). Prescribing medications was less common in pediatric programs (21%); however, counseling (82%) and CBT (54%) were provided by a similar percentage of pediatric programs as adult programs. There were substantial differences in service provision in every category between programs that had been awarded an initial 3-year MHC grant vs. those that had not (Fig. 2 ).
Fig. 2.
Service provision during the pandemic: differences between programs with MHC grant vs no grant.
3.2. Barriers to and resources needed for sustaining mental health screening and treatment
The first open-ended survey question asked about key barriers to sustaining or expanding telehealth services: 91 respondents provided 163 response items. For a majority of coded responses (n=139 of 163), raters’ coding aligned, yielding 82.5% interrater agreement. Discrepancies in coding (n= 24) were resolved by consensus discussion. The top 5 most frequent types of barriers are reported in Table 2 . Although providing psychological interventions was the most important role for the MHC during the pandemic, the greatest number of barriers were reported for delivery of interventions via telehealth. Numerous barriers to utilization of telehealth were documented in the “Provider” and “Technological and Logistic” themes, including access to equipment for mental health providers, lack of telehealth training, and licensure for practicing across state lines (see Table 2).
Table 2.
Key barriers to sustaining or expanding telehealth services.
| Top-Ranked | Total N | |
|---|---|---|
| Provider Factors | 38 | |
| Time | 13 | |
| Lack of telehealth training | 7 | |
| Staffing issues (e.g., furloughs) | 6 | |
| Licensure | 5 | |
| Psychiatry access | 2 | |
| Technological and Logistic Factors | 38 | |
| Access for providers | 12 | |
| Logistics (e.g., obtaining consent) | 11 | |
| Virtual screening | 5 | |
| Technical issues | 4 | |
| Space/privacy | 4 | |
| Patient Factors | 32 | |
| Lack of interest | 13 | |
| Internet access | 12 | |
| Difficulty contacting | 7 | |
| Financial Factors | 29 | |
| Insurance/payment issues | 13 | |
| Funding | 9 | |
| Billing | 7 | |
| CF Team Factors | 14 | |
| Lack of buy-in | 7 | |
| Team functioning (workflow) | 7 |
The second open-ended question asked which resources would be most helpful for the MHC; 76 responses were received. Interrater agreement (73 of 76 responses; 96%) was excellent. Discrepancies (n= 3) were resolved by consensus. The most frequently requested resources were coded into 10 themes, ranked by frequency of endorsement; the top 5 included: 1) Virtual Screening Resources (n=29; 38%), 2) Clinical Resources (n=19, 25%), 3) Access to Telehealth (n= 8; 11%), 4) Financial Support (n= 5; 7%), and 5) Access to Psychiatry (n=4, 5%). The top-ranked need, for Virtual Screening Resources, primarily mentioned electronic screening or integration of screening tools into electronic medical record (EMR). Several types of Clinical Resources were requested, including self-help materials (e.g., CBT booklets for pwCF) and therapy resources (e.g., stress management, telehealth strategies, patient/family handouts). Access to Telehealth included consistent and independent access to virtual technology, with links to the scheduling system. MHCs requested continuation of or increases in funding to cover the time required to maintain their role in screening and treatment.
3.3. Impact of COVID-19 on mental health
Given the potential impact of the pandemic on mental health, symptoms of depression and anxiety, as well as suicidal ideation, were assessed in pwCF. When the survey was deployed, amid the pandemic, respondents reported that 785 pwCF ages 12 through adulthood had been screened for depression and 779 had been screened for anxiety in the year to date, a notable decrease in rates of screening. Importantly, these screening rates reflected only the first six months of 2020. Average screening numbers from the CF Foundation Patient Registry, reported by CF centers beginning in 2015, show that by 2019, over 83% of adolescents and over 90% of adults completed annual mental health screening [20]. Furthermore, the MHC survey in Year 2 of grant funding [18] indicated that 8,566 pwCF were screened in the past 12 months. Given that the COVID-19 survey captured only 6 months of data, we would have expected over 4000 pwCF to be screened by mid-year, however, the COVID-19 data indicates that only 785 and 779 were screened for depression and anxiety, respectively, which represents 18% of the expected screening rate. Clinically elevated depression, in the moderate to severe range (PHQ-9≥10), was identified in 12% of pwCF, with 13% endorsing moderate to severe symptoms of anxiety (GAD-7≥10). Suicidal ideation during the pandemic (assessed with question #9 on the PHQ-9) was endorsed by 3.1% of pwCF. Although direct comparisons are difficult to make given that the COVID-19 survey was based on 6 months of data, in both Years 1 and 2 of the MHC surveys, 52.4% and 49.7% of those screened were in the elevated range, including mild to severe symptomatology, on either or both screeners, and endorsement of suicidal ideation was 2.8% in Year 1, 3.8% in Year 2 and 4% in Year 3 [18,19].
3.4. Positive outcomes & sustainability of mental health screening and treatment
Respondents were asked about the positive outcomes they observed while implementing mental health screening during COVID-19 and how confident they were that screening and treatment could be sustained after the pandemic.
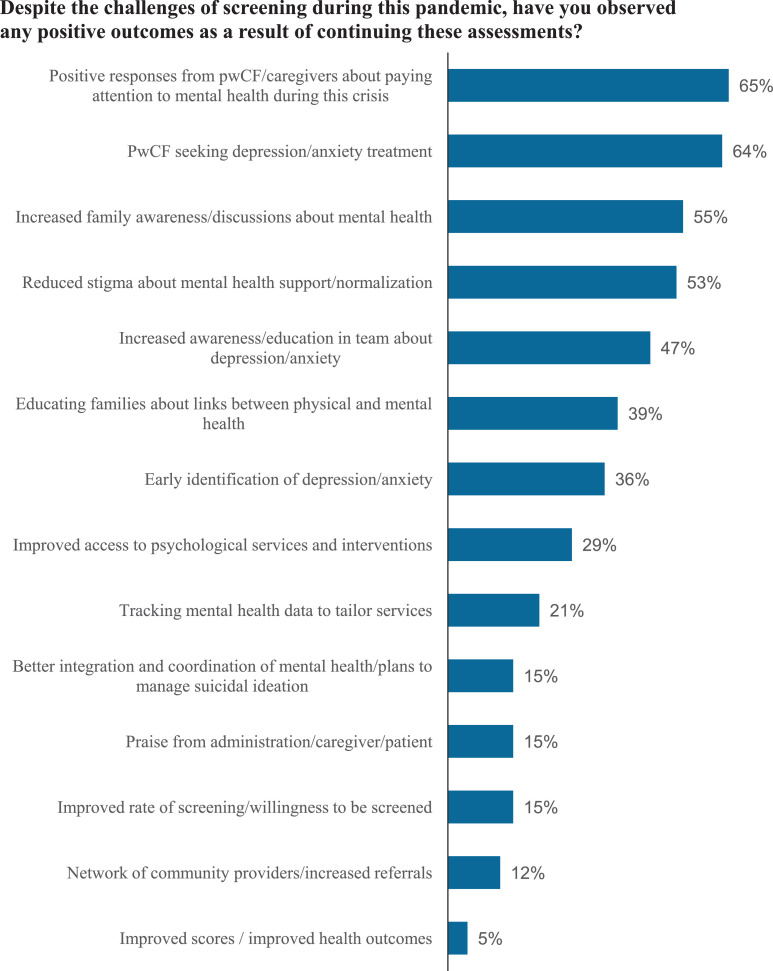
3.4.1. Positive outcomes observed
Respondents rank-ordered the successes they observed in continuing to screen and treat mental health challenges during the COVID-19 pandemic. The 5 highest ranked outcomes included: 1) positive responses from pwCF about attending to their psychological needs, 2) increased willingness to seek treatment for depression and anxiety, 3) increased discussion of mental health challenges among family members, 4) reduced stigma about the need for mental health support, and 5) increased awareness and education among CF team members about the impact of psychological distress (Fig. 3 ). These successes are nearly identical to the top five successes reported in Years 1-3 of the MHC survey, although they appeared in slightly different order [11,18,19].
Fig. 3.
Positive outcomes from continued mental health screening & treatment.
3.4.2. Sustainability
In general, slightly more than half of respondents were “extremely confident” that their program would be sustained after the crisis. Adult programs endorsed a higher level of confidence in sustainability than pediatric programs (65% vs. 58% “extremely confident”), and programs that received an MHC grant rated their confidence in sustainability higher than centers that had not received a grant (60% vs. 52% “extremely confident”).
4. Conclusions
The COVID-19 pandemic led to major disruptions in the delivery of healthcare across the world [12], with most CF programs shifting to telemedicine. The majority of CF clinics reported that only one-quarter of their visits were conducted in-person, with most visits conducted via telehealth. At the time the COVID-19 survey was deployed, MHCs were primarily working part-time: 30% were furloughed or redeployed, and others had their time reduced. At the same time, this crisis led to an expanded MHC role including facilitating team discussions about the impact of COVID-19 on pwCF, and nearly half of MHCs provided psychological support and stress reduction strategies to CF team members. This disruption in care and changes in MHC staffing and effort affected mental health screening and treatment. Rates of screening dropped precipitously in the first six months of the pandemic; 40% of programs stopped screening, and screening rates decreased in 60% of programs that continued screening. These rates represent only 18% of the expected number of screenings over 6 months, based on MHC survey data from 2018 in which 125 CF programs were funded for mental health screening and treatment [18].
Although the pandemic led to rapid, crisis-oriented shifts in healthcare delivery, this disequilibrium also facilitated beneficial changes in systems of care. For example, provision of psychological interventions, as a proportion of those who were screened, compared favorably to our 3 years of MHC survey data; 71% of those elevated in depression at the time of the COVID-19 survey received interventions from the CF team during the pandemic, which was close to the highest rate of intervention provision from the second year of implementation of the MHC grant program (n = 84 CF centers/programs) [18,19]. It appears that MHCs prioritized intervention provision over higher rates of screening. Delivering psychological interventions became the central role for the MHC, and they provided structured, evidence-based interventions, such as CBT, more frequently. However, given the substantial decrease in screening, it is likely that many pwCF were not identified as having elevated symptomatology, and thus, their clinical needs were not met. Furthermore, rates of depression and anxiety in these first 6 months of the pandemic are not comparable to rates prior to COVID-19 because of the decrease in screening, which is foundational to ascertaining those with elevated symptomatology.
The most profound change in mental healthcare delivery during the pandemic was the widespread adoption of telehealth [21]. This mode of service delivery had several obvious advantages, including reducing travel burden and infection risk, and also facilitated access to more formalized psychological interventions, such as CBT. In a recent mental health prioritization survey, both CF community (n=693) and healthcare provider (n=352) respondents rated psychological interventions delivered via telehealth as a high priority for improving mental health outcomes [22]. In addition, a recent CBT intervention study, delivered via telehealth and conducted during the very strict COVID-19 lockdown in Rome, demonstrated both substantial efficacy and high satisfaction in pwCF and caregivers [16].
Importantly, the vast majority of barriers reported by MHCs during the COVID-19 pandemic were related to using telehealth to both screen and provide interventions. The main challenges included access to telehealth training and technology, scheduling of virtual visits, licensure to practice across state lines, and patient internet access. Addressing these barriers should be a priority, given that access to psychological interventions in the community is limited, often not covered by insurance, and frequently unaffordable [23]. Despite the challenges of providing CF care during a pandemic, access to psychological care provided by CF MHCs increased dramatically when delivered via telehealth, a change in clinical practice that could potentially be sustained after the pandemic. Furthermore, evidence is accumulating that delivering psychological interventions via telehealth is feasible, acceptable, and effective for pwCF [16,[24], [25], [26], [27]]. These results also mirror the resource needs documented by MHCs, which included availability of electronic screening programs (digital links with screening tools, EMR links), access to telehealth technology, efficient scheduling, and space and privacy to conduct telehealth sessions. Solving these implementation challenges should be a high priority for CF programs.
Although the pandemic generated fear of exposure to the virus and social isolation, the rates of depression and anxiety among pwCF did not reflect a major upward trend. This survey did not ascertain rates of mild levels of depression and anxiety; however, approximately 12-13% of pwCF reported moderate to severe levels of depression and anxiety, respectively. These rates are similar to those reported at a large Italian CF Center during the pandemic (11.5% for both depression and anxiety) [16] and pre-pandemic rates at a Swedish CF center in which 21% of patients had scored in the moderate to severe range for depression and/or anxiety [28]. Suicidal ideation during the pandemic (3.1%) was also similar to rates reported in Year 1 (2.8%), Year 2 (3.8%), and Year 3 (4%) of MHC surveys, suggesting no apparent increase during the pandemic [11].
Several positive outcomes were associated with continued implementation of mental health screening and treatment, including appreciation from pwCF that the team is paying attention to mental health and addressing it, interest by pwCF in accessing psychological treatment, increased family and CF team awareness and discussion of mental health, and reduced stigma related to mental health challenges. These successes mirrored the top 5 successes reported across the 3 years of MHC surveys [18,19]. Even in the context of a pandemic, pwCF and family members have come to expect that symptoms of depression and anxiety will be identified and treated. This points to the successful integration of mental health services into the care of pwCF. Recent evidence from a survey conducted in Europe and the US with pwCF and caregivers also supports this finding; mental health screening and discussion of results were perceived as signs of caring and support [29].
Most MHCs were confident that mental health screening and treatment could be sustained on a more limited basis through the pandemic, however, concerns were raised about funding, stability of the position, and need for more time. This was supported by notable differences between programs that had received a mental health grant compared to those that had not, including increased provision of CBT, counseling, and prescribing of medications, likely a function of the MHC grant increasing access to clinicians with sufficient availability and expertise to provide these services. MHC grant recipients annually identified important clinical training needs. The CFF-sponsored MHAC responded by systematically programming sessions at the national conference to address these gaps in knowledge, including short courses on evidence-based treatments (e.g., CBT, Acceptance and Commitment Therapy, Dialectical Behavioral Therapy; Psychopharmacology), training to expand clinical skills on how to manage pwCF endorsing suicidal ideation, and strategies to address procedural anxiety and distress. Although a key to sustaining and potentially expanding mental health care delivery by CF teams is a stable, funded mental health position– education and training, growth of clinical intervention skills, and national acceptance of the integration of mental health into CF care could also influence these results. In 2020, CFF began to provide all programs with a level of support dependent on clinic size.
The strengths of this study include being the first to assess how the COVID-19 pandemic affected the mental health of pwCF and delivery of mental health services across the US. Additionally, responding centers were representative nationally by program type, size, and location. The most significant limitation is related to the precipitous drop in mental health screening nationally, which made it difficult to compare rates of depression and anxiety pre- to post-COVID. Given that 60% of centers had decreased their rate of screening, this could have introduced biases in who was screened and how many pwCF were experiencing clinically elevated symptomatology. However, this reduction in screening was a real effect of the pandemic, given that MHCs had reductions in their time and effort. A substantial proportion of MHCs were furloughed or had to reduce their work time, and it appears that they prioritized providing psychological interventions to pwCF presenting with an identified need for care over conducting screening to increase ascertainment. Amid this crisis, the emphasis on psychological support makes sense clinically. In addition, we did not capture all CF centers, programs, and affiliates and thus, it is possible that those that did not respond may have been more overwhelmed by the pandemic, and thus, less able to conduct screening and intervention, with these data representing the best-case scenario. The survey was also administered only once during 2020 and thus, does not reflect changes in service delivery at different phases of the pandemic. Finally, utilization of a cut-off score identifying those in the moderate to severe range of symptomatology may constitute an under-reporting of clinically relevant symptoms falling in the mild range; this made comparisons to previous rates of depression and anxiety in the MHC surveys more difficult.
In summary, the COVID-19 pandemic created an opportunity to implement innovative solutions to disruptions in mental health screening and treatment in CF programs. We found that pwCF had increased access to psychological interventions during the pandemic via telehealth, supporting the continued integration of tele-mental health screening and treatment into CF care.
Declaration of Competing Interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT author statement
Beth A. Smith: Conceptualization, Methodology, Formal analysis,Writing original draft, Writing review & editing. Anna M. Georgiopoulos: Conceptualization, Writing original draft, Writing review & editing. Amy Mueller: Conceptualization, Formal analysis, Writing review & editing.Janice Abbott: Methodology, Data curation, Formal analysis, Writing original draft.Paula Lomas: Conceptualization, Data curation, Writing review & editing.Enid Aliaj: Data curation, Formal analysis. Alexandra L. Quittner: Conceptualization, Methodology, Formal analysis, Writing original draft, Writing review & editing.
Acknowledgements
The Cystic Fibrosis Foundation has supported the activities of the Mental Health Advisory Committee (MHAC), including group meetings. We gratefully acknowledge the valuable input of the MHAC. We also thank the participants for taking the time to complete this survey.
Footnotes
This paper is part of a Supplement supported by the Cystic Fibrosis Foundation.
References
- 1.Quittner AL, Goldbeck L, Abbott J, Duff A, Lambrecht P, Sole A, et al. Prevalence of depression and anxiety in patients with cystic fibrosis and parent caregivers: results of The International Depression Epidemiological Study across nine countries. Thorax. 2014;69(12):1090–1097. doi: 10.1136/thoraxjnl-2014-205983. [DOI] [PubMed] [Google Scholar]
- 2.Smith BA, Modi AC, Quittner AL, Wood BL. Depressive symptoms in children with cystic fibrosis and parents and its effects on adherence to airway clearance. Pediatr Pulmonol. 2010;45(8):756–763. doi: 10.1002/ppul.21238. [DOI] [PubMed] [Google Scholar]
- 3.Barker DH, Quittner AL. Parental depression and pancreatic enzymes adherence in children with cystic fibrosis. Pediatrics. 2016;137(2) doi: 10.1542/peds.2015-2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Havermans T, Colpaert K, Dupont LJ. Quality of life in patients with cystic fibrosis: association with anxiety and depression. J Cyst Fibros. 2008;7(6):581–584. doi: 10.1016/j.jcf.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Riekert KA, Bartlett SJ, Boyle MP, Krishnan JA, Rand CS. The association between depression, lung function, and health-related quality of life among adults with cystic fibrosis. Chest. 2007;132(1):231–237. doi: 10.1378/chest.06-2474. [DOI] [PubMed] [Google Scholar]
- 6.Yohannes AM, Willgoss TG, Fatoye FA, Dip MD, Webb K. Relationship between anxiety, depression, and quality of life in adult patients with cystic fibrosis. Respir Care. 2012;57(4):550–556. doi: 10.4187/respcare.01328. [DOI] [PubMed] [Google Scholar]
- 7.Snell C, Fernandes S, Bujoreanu IS, Garcia G. Depression, illness severity, and healthcare utilization in cystic fibrosis. Pediatr Pulmonol. 2014;49(12):1177–1181. doi: 10.1002/ppul.22990. [DOI] [PubMed] [Google Scholar]
- 8.Schechter MS, Ostrenga JS, Fink AK, Barker DH, Sawicki GS, Quittner AL. Decreased survival in cystic fibrosis patients with a positive screen for depression. J Cyst Fibros. 2021;20(1):120–126. doi: 10.1016/j.jcf.2020.07.020. [DOI] [PubMed] [Google Scholar]
- 9.Quittner AL, Abbott J, Georgiopoulos AM, Goldbeck L, Smith B, Hempstead SE, et al. International committee on mental health in cystic fibrosis: cystic fibrosis foundation and European Cystic Fibrosis Society consensus statements for screening and treating depression and anxiety. Thorax. 2016;71(1):26–34. doi: 10.1136/thoraxjnl-2015-207488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quittner AL, Abbott J, Hussain S, Ong T, Uluer A, Hempstead S, et al. Integration of mental health screening and treatment into cystic fibrosis clinics: evaluation of initial implementation in 84 programs across the United States. Pediatr Pulmonol. 2020;55(11):2995–3004. doi: 10.1002/ppul.24949. [DOI] [PubMed] [Google Scholar]
- 12.Mathews KS, Seitz KP, Vranas KC, Duggal A, Valley TS, Zhao B, et al. Variation in initial U.S. hospital responses to the coronavirus disease 2019 pandemic. Crit Care Med. 2021 doi: 10.1097/CCM.0000000000005013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Havermans T, Houben J, Vermeulen F, Boon M, Proesmans M, Lorent N, et al. The impact of the COVID-19 pandemic on the emotional well-being and home treatment of Belgian patients with cystic fibrosis, including transplanted patients and paediatric patients. J Cyst Fibros. 2020;19(6):880–887. doi: 10.1016/j.jcf.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ciprandi R, Bonati M, Campi R, Pescini R, Castellani C. Psychological distress in adults with and without cystic fibrosis during the COVID-19 lockdown. J Cyst Fibros. 2021;20(2):198–204. doi: 10.1016/j.jcf.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westcott KA, Wilkins F, Chancellor A, Anderson A, Doe S, Echevarria C, et al. The impact of COVID-19 shielding on the wellbeing, mental health and treatment adherence of adults with cystic fibrosis. Future Healthc J. 2021;8(1):e47–e49. doi: 10.7861/fhj.2020-0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graziano S, Boldrini F, Righelli D, Milo F, Lucidi V, Quittner A, et al. Psychological interventions during COVID pandemic: telehealth for individuals with cystic fibrosis and caregivers. Pediatr Pulmonol. 2021 doi: 10.1002/ppul.25413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinar Senkalfa B, Sismanlar Eyuboglu T, Aslan AT, Ramasli Gursoy T, Soysal AS, Yapar D, et al. Effect of the COVID-19 pandemic on anxiety among children with cystic fibrosis and their mothers. Pediatr Pulmonol. 2020;55(8):2128–2134. doi: 10.1002/ppul.24900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quittner A, Hussain S, Muther E, Abbott J, Tillman L, Schechter M, et al. P376 Prevalence and treatment of severe mental health symptoms at 120 cystic fibrosis centres: clinician preparation to intervene and sustain mental health screening. J Cyst Fibros. 2020;19:S161. [Google Scholar]
- 19.Quittner AL, Muther E, Tillman L, Abbott J, Lomas P, Hempstead S, et al. Examining the impact of mental health coordinators in CF centers: barriers & successes over 3 years. P672. Pediatr Pulmonol. 2019.
- 20.Cystic Fibrosis Foundation . 2020. Cystic fibrosis foundation patient registry: 2019 annual data report to the center directors. Bethesda, Maryland. [Google Scholar]
- 21.Sorkin DH, Janio EA, Eikey EV, Schneider M, Davis K, Schueller SM, et al. Rise in use of digital mental health tools and technologies in the United States during the COVID-19 pandemic: survey study. J Med Internet Res. 2021;23(4):e26994. doi: 10.2196/26994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith BA, Georgiopoulos AM, Tillman L, Aliaj E, Riva D, Davis K, et al. P209 Key priorities in mental health research: results of a community and provider survey across the US. J Cyst Fibros. 2021;20:S103. [Google Scholar]
- 23.McCray CI, Rosenberg L. A path forward: mental health and the U.S. pandemic response. J Behav Health Serv Res. 2021;48(2):161–170. doi: 10.1007/s11414-020-09747-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bathgate CJ, Kilbourn KM, Murphy NH, Wamboldt FS, Holm KE. Pilot RCT of a telehealth intervention to reduce symptoms of depression and anxiety in adults with cystic fibrosis. J Cyst Fibros. 2021 doi: 10.1016/j.jcf.2021.07.012. [DOI] [PubMed] [Google Scholar]
- 25.Friedman D QA, Smith B, Schwartz CE, Lee H, Stark RB, Pinsky H, et al. Preventing depression and anxiety: results of a pilot study of a CF-specific CBT intervention for adults with CF. Pediatr Pulmonol. 2019;54(397) [Google Scholar]
- 26.Verkleij M, Georgiopoulos AM, Friedman D. Development and evaluation of an internet-based cognitive behavioral therapy intervention for anxiety and depression in adults with cystic fibrosis (eHealth CF-CBT): an international collaboration. Internet Interv. 2021;24 doi: 10.1016/j.invent.2021.100372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Hayer CV, O’Loughlin CM, Nurse CN, Smith PJ, Stephen MJ. ACT with CF: a telehealth and in-person feasibility study to address anxiety and depressive symptoms among people with cystic fibrosis. J Cyst Fibros. 2021;20(1):133–139. doi: 10.1016/j.jcf.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 28.Jarvholm S, Ericson P, Gilljam M. Patient acceptance and outcome of mental health screening in Swedish adults with cystic fibrosis. Qual Life Res. 2020;29(6):1579–1585. doi: 10.1007/s11136-020-02417-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Landau E, Verkleij M, Graziano S, Quittner AL, Georgiopoulos AM, Smith BA, et al. Mental health screening as an intervention: how patients and caregivers contribute to improving our processes [selected oral abstract workshop presentation by Landau]. 44th European Cystic Fibrosis Conference (ECFS Digital); Virtual; 2021. [Google Scholar]