Abstract
Objective
Emergency clinicians face elevated rates of burnout that result in poor outcomes for clinicians, patients, and health systems. The objective of this single‐arm pilot study was to evaluate the feasibility of a Transcendental Meditation (TM) intervention for emergency clinicians during the coronavirus disease 2019 (COVID‐19) pandemic and to explore the potential effectiveness in improving burnout, sleep, and psychological health.
Methods
Emergency clinicians (physicians, nurses, and physician‐assistants) from 2 urban hospitals were recruited to participate in TM instruction (8 individual or group in‐person and remote sessions) for 3 months. Session attendance was the primary feasibility outcome (prespecified as attending 6/8 sessions), and burnout was the primary clinical outcome. Participant‐reported measures of feasibility and validated measures of burnout, depression, anxiety, sleep disturbance, and stress were collected at baseline and the 1‐month and 3‐month follow‐ups. Descriptive statistics and linear mixed‐effects models were used.
Results
Of the 14 physicians (46%), 7 nurses (22%), and 10 physician‐assistants (32%) who participated, 61% were female (n = 19/32). TM training and at‐home meditation practice was feasible for clinicians as 90.6% (n = 29/32) attended 6/8 training sessions and 80.6% self‐reported meditating at least once a day on average. Participants demonstrated significant reductions in burnout (P < .05; effect sizes, Cohen's d = 0.43–0.45) and in symptoms of depression, anxiety, stress, and sleep disturbance (P values < .001; Cohen's d = 0.70–0.87).
Conclusion
TM training was feasible for emergency clinicians during the COVID‐19 pandemic and led to significant reductions in burnout and psychological symptoms. TM is a safe and effective meditation tool to improve clinicians’ well‐being.
Keywords: burnout, clinician intervention, covid‐19, meditation, nurse burnout, PA burnout, pandemic, physician burnout, pilot study, transcendental meditation, video‐delivery
1. INTRODUCTION
1.1. Background
Emergency medicine (EM) and frontline healthcare clinicians innately manage high‐intensity, high‐risk, and high‐stress clinical scenarios. Unsurprisingly, emergency clinicians face high rates of burnout and exhaustion. Prevalence rates of burnout and psychological stress vary, with some reports suggesting 65% of emergency residents met the criteria for burnout 1 , 2 and another revealing around 85% of emergency medicine nurses experienced burnout and compassion fatigue. 3 , 4 Physician and physician assistants are at equally high risk for burnout. 3 , 5 Burnout often leads to increased medical errors, reduced adherence to safety protocols, increased costs, reduced patient satisfaction, job loss, depression, and substance use, and in severe cases suicide. 6 , 7 , 8 Clinician burnout is relevant not only to a clincian's quality of life but also results in compromised care.
The coronavirus disease 2019 (COVID‐19) pandemic continues to exacerbate emergency clinician well‐being and burnout. The emergency department functions as the initial triage point for many patients with potential COVID‐19 infections, driving higher demand for services, increased vigilance around infection transmission, and greater acuity on shift. Clinicians have experienced increased stress from fear of or actual contraction of COVID‐19 and the overwhelming concerns for infecting loved ones in addition to the ever‐changing clinical landscape, demand, and extended nature of the pandemic. 9 , 10 , 11 , 12 Unsurprisingly, 1 study noted that 53% of healthcare workers report experiencing high levels of burnout during the pandemic. 13 At this time, it is imperative that emergency clinicians receive better support to reduce current and future burnout.
1.2. Importance
Burnout interventions at the system and hospital levels often have the greatest impact; however, clinician‐focused interventions also have been found to provide meaningful improvements in burnout. 14 , 15 , 16 , 17 Meditation and mindfulness interventions are increasingly more accessible in healthcare systems and popular in the mainstream media. These interventions are often low cost, low risk, and easy to practice. 18 A recent meta‐analysis of resilience interventions for healthcare clinicians identified that although meditation results in improvements to clinician resilience, future studies need to evaluate the ability to sustain or maximize intervention effects with interventions that are longer than 1 week and include postintervention support. 19 Transcendental Meditation (TM) is a type of meditation practice that has been well‐documented as a non‐pharmacologic method for stress reduction. 17 , 19 Evidence suggests that meditation‐based interventions such as TM and Mindfulness‐Based Stress Reduction can result in decreased burnout, blood pressure, depression, anxiety, emotional exhaustion, and insomnia and increased resiliency in various clinical populations. 16 , 20 , 21 Mechanistically, it is theorized that the TM practice varies from other mindfulness meditation practices and leads to reduced psychological and physiologic response to stress, evidenced by decreased sympathetic nervous system and hypothalamic‐pituitary‐adrenal axis responsivity and reduced cortisol levels. 22 , 23 Specifically, 2 studies identified that those practicing meditative interventions, such as TM, experienced increased tumor necrosis factor α mRNA, 24 reduced blood pressure, 25 and increased cortical connectivity in emotion and reward systems. 26 Theoretically, reduced stress reactivity decreases anxiety and burnout for clinicians over time. TM training could therefore provide prolonged improvements in resilience and burnout for clinicians.
1.3. Goals of this investigation
Timely support during stressful situations can prevent further worsening of burnout 23 , 27 ; however, burnout interventions during pandemics pose unique challenges for implementation. The objectives of this single‐arm pilot study were to examine whether training emergency clinicians in TM during the COVID‐19 pandemic was feasible and acceptable, and to explore whether TM had an impact on clinician burnout and psychological well‐being at 3 months after initial training.
2. METHODS
2.1. Design and participants
Emergency clinicians were screened and enrolled to engage in this single‐arm pilot study to learn TM and evaluate the feasibility, acceptability, and potential efficacy of this program during the COVID‐19 pandemic. Emergency clinicians completed baseline (1–3 days before meditation training), 1‐month (since the initial training session), and 3‐month (since the initial training session) measures to measure the perceived acceptability and feasibility and to explore the impact of TM practice on clinician burnout and psychological well‐being. The study was approved by the Mass General Brigham Institutional Review Board as exempt. The David Lynch Foundation funded this study and provided certified TM teachers to lead the meditation sessions.
Participants were recruited from one academic tertiary care center (Brigham and Women's Hospital) and an affiliated community center (Brigham and Women's Faulkner Hospital) in Boston, MA, using within‐hospital email listservs and direct contact between a research assistant (Lily Johnsky) and physicians, nurses, and physician assistants to answer relevant questions about participation. Emergency clinicians were recruited between October 2020 and February 2021, and follow‐up for the study was completed by May 2021; study procedures occurred during the second peak of COVID‐19 in Massachusetts (November 2020–May 2021). The study was presented as an opportunity to engage in a free meditation training program that has evidence of improved sleep and wellness. Expected engagement in the 8 training sessions was explicitly described. Emergency clinicians then self‐enrolled in the study by email. Emergency clinicians were eligible if they were full‐time a medical doctor, physician assistant, resident, or nurse, aged 18 years or older, had treated patients with COVID‐19 or were working at locations where patients with COVID‐19 are being treated, were willing and able to complete baseline and poststudy surveys, and were willing to dedicate time to complete the intervention sessions. If participants were on psychoactive medications, they self‐reported being on a stable regimen (no changes to their medication or dosing) for at least 2 months before enrollment. Participants were excluded if they had previous instruction in TM techniques, if they were currently psychiatrically unstable per self‐report, or reported a psychiatric hospitalization in the past 6 months. Together, both hospitals staff a total of 450 clinicians, including physicians, physician assistants, and nurses; yet not all clinicians are full‐time, which was a unique inclusion criterion for the study. All participants provided consent to participate in the study and completed surveys on Research Electronic Data Capture (REDCap) tools hosted by the Mass General Brigham Research Computing Enterprise Research Infrastructure & Services group. 31 , 32 REDCap is a secure, web‐based application designed to support data capture for research studies. 28 , 31 , 32 Clinicians were not provided remuneration.
2.2. Intervention
TM is a simple meditation practice that allows the participant to experience quieter levels of thinking and a sense of restful alertness. The technique advises the use of a repetitive mantra and is practiced sitting with closed eyes. TM was delivered by certified instructors (1 female and 1 male) in the same standardized format used in other TM studies. 20 , 22 , 23 TM instruction was first described in an introductory educational session that all staff members were invited to join. The certified TM instructor described the practice of TM, previous scientific evidence supporting TM's efficacy, and proposed mechanisms of the practice.
The Bottom Line.
Transcendental Meditation (TM) is known to enhance psychological health. This pilot study of 31 healthcare workers demonstrated reductions in reported burnout, depression, anxiety, stress, and sleep disturbance with structured TM sessions. Although lacking a comparison group, this study supports the feasibility of TM and its potential use for improving healthcare worker well‐being.
The core instruction for learning the TM technique was then taught to participants for 4 consecutive days. Sessions 1–4 are fundamental for the successful instruction of the TM technique. The first session was an individual, in‐person session (Session 1) and the 3 subsequent sessions were group, in‐person sessions (Sessions 2–4). Session 1 included a brief personal interview with the instructor along with 1‐on‐1 instruction in the practice of TM. Sessions 2, 3, and 4 involved continued, group instruction, verification of correct practice, and some didactic explanation of TM mechanisms. Participants practiced TM during these sessions and were encouraged to practice TM for 20 minutes twice per day thereafter. After the core instruction (Sessions 1–4), there were 4 maintenance sessions (Sessions 5–8) delivered in a group format held over an encrypted web‐based format (Zoom). These sessions were conducted 2 weeks after the completion of Session 4 and at the 1‐month, 2‐month, and 3‐month follow‐ups. Sessions 5–8 are meant to be supportive in nature and not didactic. As such, participants reviewed their current practice rates, verified correct practice of the TM technique, and shared discussions of personal experiences.
As a primary feasibility outcome of this pilot study, we sought to evaluate whether engaging in a TM intervention was feasible and acceptable for emergency clinicians during the COVID‐19 pandemic. Feasibility was prespecified as attending 6 of the 8 training sessions by 80% of the cohort. Participation of each training session was recorded for each participant by the meditation teacher. We evaluated whether participants practiced meditation after the primary instruction period (Week 1) through the 3‐month follow‐up self‐report assessment. Adherence to at‐home meditation practice has been identified in other TM studies as practicing TM at least once daily for most days of the week. 22 Lastly, participants completed self‐report acceptability and feasibility ratings of the TM training during the 3‐month follow‐up assessment. Acceptability was prespecified with a score of 4 or 5 on a 5‐point Likert scale for ≥80% of the sample. Questions evaluated whether they found the TM training and meditation feasible, whether they enjoyed meditation, and if they would recommend TM to a friend or colleague. As a primary clinical outcome, we explored trends in changes of burnout, in addition to psychological well‐being at baseline (T1), 1 month (T2), and 3 months (T3) after TM training.
2.3. Measures
The Maslach Burnout Inventory (MBI) is a validated and highly used measurement tool to evaluate clinician burnout. 39 The MBI includes the following 3 subscales: emotional exhaustion, depersonalization, and professional accomplishment. Total scores range from 0–100, and higher scores equate to higher ratings of that factor. Depressive symptoms were measured using the Patient Health Questionnaire 8‐item scale (PHQ‐8) 40 ; item 9 evaluating suicidality was removed for this study. Anxiety symptoms were measured using the Generalized Anxiety Disorder 7‐item (GAD‐7) scale. 27 Both the PHQ‐8 and GAD‐7 are highly used, well‐validated measures for depression and anxiety and have been used in previous studies evaluating clinician burnout. Higher scores relate to higher symptoms of anxiety and depression. The 4‐item Perceived Stress Scale (PSS‐4) 33 is a validated measure used to evaluate perceived stress, with higher scores indicating greater stress. Lastly, the patient‐reported outcomes measurement information systems (PROMIS) Sleep Disturbance 8‐item measure was used to evaluate sleep difficulties. 24 This sleep measure has been validated in both clinical and general samples, making it relevant for this clinician cohort of shift workers with inherently variable sleep patterns. Higher scores are associated with higher sleep disturbance.
2.4. Statistical analysis
Frequencies and mean scores were calculated for demographics, attendance, and other self‐report measures of acceptability and feasibility. To explore the impact of TM on burnout and psychological well‐being (MBI, PHQ‐8, GAD‐7, PSS‐4, and PROMIS sleep disturbance), we used a linear mixed‐effects model to compare the scores from T1 to T3 with a random intercept for each participant (fitted by restricted maximum likelihood) to determine whether there were statistically significant changes (T1 vs T2, T1 vs T3) while considering the within‐participant correlation. That is, participants with above (below) average scores at T1 may tend to also have above (below) average scores at T2 and T3, and this linear mixed‐effects model can account for these within‐participant correlations. Data were included for participants who completed at least 2 of the survey assessments (n = 31 of 32). See Appendix 1.
3. RESULTS
A total of 32 participants were enrolled in the study between October 2020 and February 2021, with 31 participants completing training and follow‐up assessments (see Figure 1). Of note, enrollment and study participation continued through the second peak of the COVID‐19 pandemic in Boston, MA. The sample was primarily White (84%, n = 26), 41 years old on average (SD = 10), and slightly more than half were women (61%, n = 19). A variety of emergency clinicians enrolled in the study, including 14 physicians (45%), 10 physician assistants (32%), and 7 nurses (23%). Emergency clinicians reported working an average of 37 hours per week (SD = 11; see Table 1).
FIGURE 1.
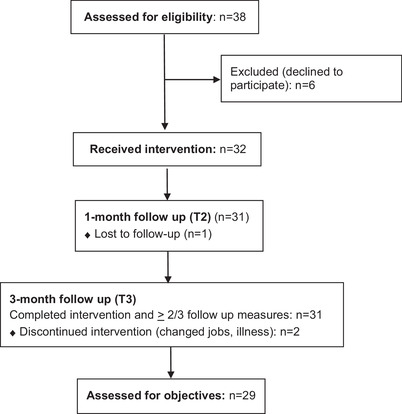
Consort diagram
TABLE 1.
Clinician demographics
| Demographics (n = 31) | Mean (SD) | n (%) |
|---|---|---|
| Age, years | 41.6 (10.4) | |
| Sex, female | 19 (61.3) | |
| Ethnicity | ||
| Hispanic/Latino | 4 (12.9) | |
| Not Hispanic | 25 (80.6) | |
| Unknown | 2 (6.5) | |
| Race | ||
| White | 26 (83.9) | |
| African American | 3 (9.7) | |
| Asian | 2 (6.5) | |
| Native American | – | |
| More than 1 race | – | |
| Education level | ||
| RN/BSN | 6 (19.3) | |
| PA | 8 (25.8) | |
| Master's level | 3 (9.7) | |
| MD or equivalent | 14 (45.2) | |
| Clinician role | ||
| MD | 14 (45.2) | |
| Nurse | 7 (22.6) | |
| PA | 10 (32.3) | |
| Average work hours per week | 37.2 (11.9) | |
| Previous meditation practice | 11 (35.4) | |
| Years practicing | 5.4 (6.0) |
Abbreviations: BSN, bachelor of science in nursing; MD, doctor of medicine; PA, physician's assistant; RN, registered nurse.
3.1. Feasibility and acceptability
TM training was feasible for emergency clinicians during the COVID‐19 pandemic. Of the 32 participants enrolled, 29 (90.6%) participants completed at least 6 of 8 meditation training sessions. Of those, 65.6% (n = 21) attended all 8 sessions. A total of 3 participants were able to only attend 4 or 5 of the 8 sessions (9.4%). Of these, 2 left the study and 1 was lost to follow‐up (1 as a result of COVID‐19 infection). Of the participants, 100% (32/32) completed all 4 in‐person instructional sessions; 4 participants completed abbreviated sessions by phone in place of 1 of these in‐person meetings. Self‐reported feasibility was successful, with 89.7% (n = 26) of the sample reporting that the TM meditation training was feasible/very feasible. Compliance of TM is identified as practicing at least once daily on most days of the week; 81% were compliant with meditations at home. Specifically, approximately half (44.8%, n = 13) reported meditating 5–7 days per week, 41.4% (n = 12) reported meditating 3–4 days per week, and few reported meditating <2 days per week (13.8%, n = 4). The majority reported meditating at least once on days they meditated (89.7%, n = 26), and 10.3% (n = 3) reported meditating 2 times per day.
Regarding the acceptability of the meditation practice, most rated meditation as easy or very easy (75.8%). For acceptability of the intervention training, 95.6% (n = 28) found the TM training to be acceptable, and 93% (n = 27) reported that they would recommend TM to a friend. The majority reported that TM was helpful during the COVID‐19 pandemic (93.1%, n = 27), and most indicated that TM impacted their career positively (65.5%, n = 19). See Table 2 and Figure 2 for complete feasibility and acceptability measures. Emergency clinicians liked the intervention and stated “feeling less anxious, more focused, and sleep[ing] better” and that they felt “less reactive.” Of the participants, 2 described disliking a few aspects of the TM training, indicating that it was “difficult to find time to meditate twice a day” and that they felt the training sessions could have been shortened and in‐person training was difficult. Overall, participants reported feeling more “at ease” and “less stressed/anxious” and “sleeping better.” See Table 3 for further participant reports/quotes.
TABLE 2.
Feasibility and acceptability outcomes for Transcendental Meditation training for emergency clinicians during the COVID‐19 pandemic
| Feasibility and acceptability measures | n (%) |
|---|---|
| Session completion rate (n = 32) | |
| ≥6/8 sessions | 29/32 (90.6) |
| ≤5/8 sessions | 3/32 (9.4) |
| Self‐reported meditation practice (n = 31) | |
| Days per week | |
| 0–2 days | 4 (13.8) |
| 3–4 days | 12 (41.4) |
| 5–7 days | 13 (44.8) |
| Times per day | |
| once/day | 26 (89.7) |
| twice per day | 3 (10.3) |
| Duration | |
| 3–7 minutes | 2 (6.9) |
| 10–15 minutes | 12 (41.4) |
| 20–30 minutes | 15 (51.7) |
| Self‐reported feasibility and acceptability (n = 31) | |
| Recommend TM to a friend | |
| Yes | 27 (93.1) |
| No | 2 (6.9) |
| TM helpful during COVID‐19 | |
| Yes | 27 (93.1) |
| No | 2 (6.9) |
| Does TM impact your career? | |
| Yes | 19 (65.5) |
| No | 2 (6.9) |
| Maybe | 8 (27.6) |
| TM adds to overall well‐being | |
| Yes | 26 (89.7) |
| No | 0 |
| Maybe | 3 (10.3) |
| Continue using TM | |
| Yes | 23 (79.3) |
| No | 0 |
| Maybe | 3 (10.3) |
Note: All feasibility and acceptability ratings, including rates of self‐reported meditation frequency, were reported at the 3‐month follow‐up. Feasibility was prespecified as attendance at 6 of 8 TM training sessions. Acceptability cut‐offs were prespecified at 80%.
Abbreviations: COVID‐19, coronavirus disease 2019; TM, Transcendental Meditation.
FIGURE 2.
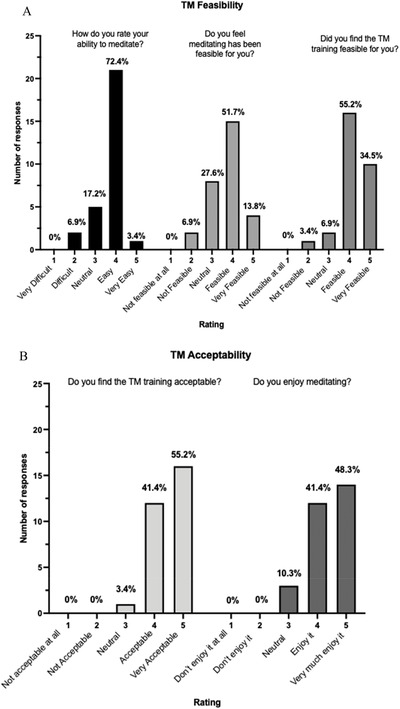
Participants self‐reported feasibility and acceptability measures of Transcendental Meditation practice 3 months following initial training, noting high feasibility and acceptability of this training program during the coronavirus disease 2019 pandemic. Items were scored on a 5‐point Likert scale
TABLE 3.
Participant qualitative feedback
| Themes | Participant quotes |
|---|---|
| Benefits of TM |
• “Clears my mind. I feel that I am thinking more clearly after.” Male, MD • “I feel less anxious, more focused, and I sleep better.” Female, RN • “Turning attention inwardly has a self‐nurturing quality that is rewarding.” Male, MD • “Able to make decisions easier at work and take time to breathe during the stress.” Female, PA‐C • “Makes me a better doctor, teacher, and colleague on shift.” Male, MD • “Many times, I am more relaxed and happy to be at work. This has been quite significant since the COVID pandemic has made work less enjoyable than usual.” Female, MD • “Remain calmer under stress.” Male, MD • “I feel more at ease in general and I think that is very important especially with the type of job I have.” Female, PA‐C • “I feel more at ease in my everyday life. I'm sleeping better than ever and feeling well rested when I wake up.” Female, RN • “Cannot imagine showing up to a shift without TM.” Male, MD |
| Negatives of TM |
• “Difficult to find time to meditate twice a day.” Female, MD • Meditation practice 2x per day—“Hard to be consistent with my schedule.” Male, MD • “Sometimes it's hard to make the time with working 12‐hours shifts.” Female, RN |
Abbreviation: TM, Transcendental Meditation.
3.2. Intervention effects
At baseline, emergency clinicians endorsed elevated burnout, with 74.2% (n = 23) reporting high emotional exhaustion and elevated sleep disturbance. Mean baseline levels of depressive symptoms, anxiety, and perceived stress were also elevated; 7 participants had moderate to severe depressive symptoms (25%), 15 had significant sleep disturbance (50%), and 9 had moderate to severe anxiety (27.1%). After the initial meditation training (Sessions 1–5), emergency clinicians experienced significant reductions in burnout, sleep disturbance, and symptoms of depression, anxiety, and stress. Reductions persisted with significant decreases in all measures of burnout and psychological well‐being at the 3‐month follow‐up. See Figures 3 and 4. In this single‐arm pilot study, meditation training led to significant reductions with medium to large effects on clinician burnout: emotional exhaustion (Cohen's d = 0.45), depersonalization (Cohen's d = 0.43), and professional accomplishment (Cohen's d = 0.43) 3 months after the initial training. Results of this single‐arm cohort also suggested that TM training had medium to large effects on depression (Cohen's d = 0.86), anxiety (Cohen's d = 0.87), perceived stress (Cohen's d = 0.75), and sleep (Cohen's d = 0.70) at 3 months posttest (see Table 3). Qualitatively, most of the participants reported that TM added to their overall well‐being and “feeling more at ease” and that TM positively impacted their career as they noted being able to “make decision[s] easier at work” and feeling like TM “makes me a better doctor, teacher, and colleague on shift” (see Table 4).
FIGURE 3.
(A–H) Effects of TM at baseline and the 1‐month and 3‐month follow‐ups on clinician burnout and psychological well‐being. MBI, Maslach Burnout Inventory; TM, Transcendental Meditation
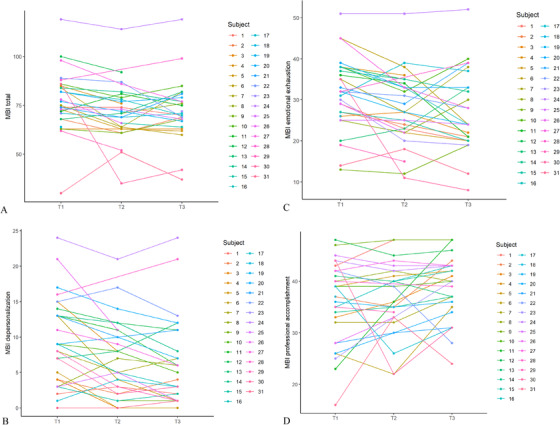
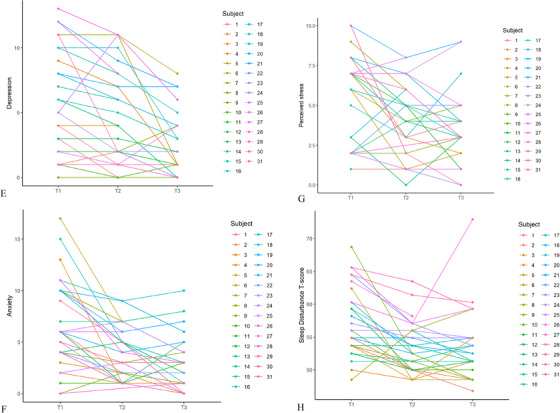
FIGURE 4.
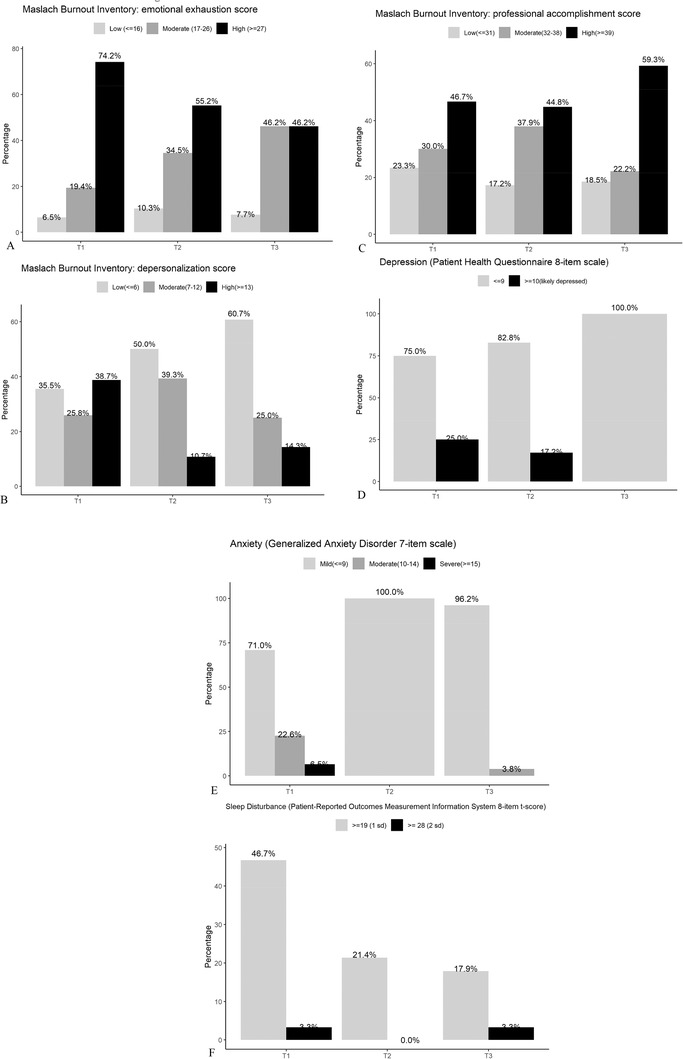
(A–F) Clinical outcomes at baseline and the 1‐month and 3‐month follow‐ups after Transcendental Meditation training
TABLE 4.
Change scores in emergency clinician burnout and psychological well‐being ratings at baseline and 1 and 3 months after TM training
| Measure from T1 to T3 | Cohen's d | b (95% CI) | P |
|---|---|---|---|
| Maslach Burnout Inventory | |||
| Emotional exhaustion subscale | 0.45 | 4.43 (1.67–7.20) | 0.002 |
| Depersonalization subscale | 0.43 | 2.58 (1.35–3.80) | <0.001 |
| Professional accomplishment subscale | 0.43 | −2.71 (−5.24 to −0.18) | 0.036 |
| Depression: PHQ‐8 | 0.86 | 2.98 (1.88–4.09) | <0.001 |
| Anxiety: GAD‐7 | 0.87 | 3.65 (2.38–4.93) | <0.001 |
| Perceived stress: PSS‐4 | 0.75 | 2.10 (1.16–3.03) | <0.001 |
| Sleep disturbance: PROMIS SF sleep 8a | 0.70 | 3.72 (1.80–5.64) | <0.001 |
Abbreviations: CI, confidence interval; GAD‐7, Generalized Anxiety Disorder Scale 7 item; PHQ‐8, Patient Health Questionnaire 8 item; PSS‐4, Perceived Stress Scale 4 item; PROMIS SF, patient‐reported outcomes measurement information systems‐short form; T1, baseline; T3, 3 months after TM training.
3.3. Limitations
Intervention effects should be evaluated with caution as this was a single‐arm pilot study and participants’ TM practice was self‐reported. Future studies should include a randomized trial with an appropriate control group to reduce bias in interpretation and to accurately evaluate the effects of TM on emergency clinician burnout. Mobile phone‐based delivery of TM may increase accuracy in participants’ meditation practice reporting. Anecdotally, participants who practiced more frequently reported greater benefits from TM; however, the study was underpowered to evaluate these relationships. In addition, this study was conducted during the second wave of the pandemic in Massachusetts. Participants may have experienced decreased stress as a result of the availability of the COVID‐19 vaccine; however, symptoms of stress and burnout often increase after the resolution of a stressor or trauma, and this trajectory was not seen in this sample, further emphasizing the potential impact of TM. Levels of burnout were particularly high in this sample, and it may be the case that those who felt more burned out or those with greater interest in meditation were more likely to engage in this intervention, potentially introducing selection bias. Recruitment of participants may have been impacted by the fact that study staff were colleagues, potentially introducing further selection bias. The principal investigator (D.R. Azizoddin) joined the department 3 months before study initiation and knew only 1 eligible participant. The physician assistant coleading the project (N. Kvaternik) knew most of the staff eligible for enrollment. In an effort to reduce bias, the study staff members were not directly involved in recruiting participants to the study, in onboarding, or during meditation sessions. A portion of this sample also reported previous experience with meditation that may have influenced their motivation to engage in the study. It may also be the case that this level of training was not accessible for all clinicians, particularly those with small children. Brief and remote delivery of low‐cost, self‐management interventions may be more accessible for larger cohorts of clinicians. 18 Lastly, the effects on sleep disturbance may be influenced by the fact that all clinicians in this cohort engaged in shift work that can be particularly disruptive to sleep.
4. DISCUSSION
This single‐cohort pilot study found that TM training was feasible and acceptable to emergency clinicians during the COVID‐19 pandemic, and emergency clinicians reported significant reductions in burnout, psychological symptoms, and poor sleep quality. Of this cohort, 90% were able to attend 6 of the 8 sessions, and the majority found TM to be easy to learn and would recommend it to a colleague. Of note, >80% of participants self‐reported compliance and maintenance of their meditation practice for the 3 months after instruction, indicating that meditation at least once daily on most days was a sustainable self‐management tool. Emergency clinicians reported that TM had a significant impact on their feelings of burnout and well‐being and that TM helped to improve their sleep. Emergency clinicians were able to attend, learn, and practice TM during the second peak of the COVID‐19 pandemic. During enrollment, many emergency clinicians identified that attending 4 consecutive sessions was the primary barrier to participation; however, we saw that for clinicians who enrolled, 100% were able to attend the 4 consecutive core TM sessions with minor scheduling modifications.
Identifying accurate yet appropriate timing of burnout interventions either during or after catastrophic events remains complex. Our study sought to evaluate whether a meditation‐based burnout intervention could be delivered and prove effective during a pandemic for frontline emergency healthcare workers. Emotional exhaustion at baseline was higher in this sample compared with other non‐emergency clinician cohorts measured before COVID‐19 35 , 36 and during COVID‐19, 13 with similar burnout rates among 2 other cohorts of emergency nurses and residents. 2 , 4 Higher levels of baseline burnout may be unsurprising as this study occurred during the second wave of the COVID pandemic in Boston, MA—a city that experienced elevated levels of the virus. Although the COVID‐19 vaccine became available in winter 2021 and cases began to decrease in the spring of 2021, it is expected that burnout rates would increase as the pandemic continued. The delivery of TM during the pandemic was highly successful in this sample, with significant reductions in burnout, depression, and other psychological symptoms during the pandemic. After 5 sessions, we demonstrated that participants could effectively practice TM on their own and continued to do so even 3 months after the intervention was complete. The etiology of stress for physicians, nurses, physician assistants, and residents may be heterogenous, yet a commonality among these clinicians is the use of brief, on‐demand TM sessions to boost wellness and mitigate stressors surrounding ED work during COVID‐19. Self‐management interventions can be provided during elongated crises such as the COVID‐19 pandemic, which may reduce the negative impact of burnout on clinicians.
Our anecdotal experiences may be relevant to health systems considering future integration of TM to alleviate issues with burnout, poor sleep quality, and psychological health. In our cohort, emergency clinicians noted being more likely to engage in the intervention training because of the previous scientific evidence supporting the effectiveness of TM, the format of delivery within a research study, and the fact that the study was led by fellow emergency clinicians and researchers. Participants also shared that the TM teachers’ flexibility when scheduling TM sessions increased accessibility of the intervention; flexibility with wellness interventions may increase accessibility of such interventions in healthcare systems generally. Many participants were also concerned about the confidentiality of their self‐reported mental health data and voiced that the research structure of our intervention enhanced privacy. Participants also noted the immediate impact meditation practice had on their levels of anxiety, which likely served as reinforcement to attend follow‐up sessions and engage in a consistent home practice. Participants reported building new relationships with one another after attending group sessions, which may have lasting effects on team building.
To our knowledge, TM has not yet been evaluated for emergency clinicians. TM training can be considered a feasible and effective intervention to support clinician burnout and should be implemented alongside wellness initiatives that focus on hospital‐wide structural and administrative changes, which have been shown to have the largest impact on burnout. 8 , 27 Our findings are consistent with other TM literature that suggests that TM results in significant decreases in anxiety 20 and emotional exhaustion with improvements in resilience, perceived stress, fatigue, and depression in teachers and clinicians. 21 , 24 , 25 , 36 , 37 , 38 Delivery of TM training content online would likely increase the overall scalability of this intervention as the pandemic continues to persist. To truly evaluate the efficacy of TM for clinician burnout and psychological well‐being, future studies should compare TM training with a matched control (eg, relaxation recordings) in a randomized study.
CONFLICT OF INTEREST
Desiree Azizoddin receives funding from the David Lynch Foundation, NIH‐NCI, and the National Palliative Care Research Center Kornfeld Scholars Award. Peter R. Chai is funded by NIH K23DA044874, R44DA051106, DARPA HR001120S0041, eink corporation, Hans and Mavis Lopater Psychosocial Foundation and the Bill and Melinda Gates Foundation. Dr. Chai has a financial interest in Biobot Analytics, a company engaged in the collection and analysis of wastewater to develop epidemiological data. Dr. Chai's interests were reviewed and are managed by Brigham and Women's Hospital and Mass General Brigham in accordance with their conflict of interest policies. The other authors have no conflicts of interest to report.
AUTHOR CONTRIBUTIONS
Desiree R. Azizoddin, Noelia Kvaternik, and Edward W. Boyer conceived the study, designed the trial, and obtained research funding. Desiree R. Azizoddin and Mohammad Adrian Hasdianda supervised the conduct of the trial and data collection. Desiree R. Azizoddin, Noelia Kvaternik, and Lily Johnsky undertook recruitment of the study. Desiree R. Azizoddin and Mohammad Adrian Hasdianda managed the data, including quality control. Guohai Zhou and Desiree R. Azizoddin completed statistical analysis. Desiree R. Azizoddin drafted the manuscript with input from Noelia Kvaternik and Meghan Beck. All authors contributed to the revision of the manuscript.
ACKNOWLEDGMENT
The authors would like to acknowledge all participants for engaging in this pilot trial during the coronavirus disease 2019 pandemic.
Biography
Desiree R. Azizoddin, PsyD, is a member of the Research Faculty at Brigham and Women's Hospital in Boston, Massachusetts.

APPENDIX 1. DETAILS OF THE LINEAR MIXED‐EFFECTS MODEL
1.1.
The model equation is the following:
where Yij is the 1 of the outcomes (Maslach Burnout Inventory [MBI] total, MBI emotional exhaustion, MBI depersonalization, MBI professional accomplishment, depression/PHQ‐8, anxiety/GAD‐7, stress/PSS‐4, or sleep disturbance/PROMIS‐SF sleep 8a t score) from subject i at time j, T2 ij is the dummy variable coding for time T2 (1‐month follow‐up) with T2 ij = 1 if Yij is measured at time T2 and T2 ij = 0 otherwise, T3 ij is the dummy variable coding for time T3 (3‐month follow‐up) with T3 ij = 1 if Yij is measured at time T3 and T3 ij = 0 otherwise, bi is the random subject effect with N(0,) distribution accounting for within‐subject correlation, and eij is the error term with N(0,) distribution. The fixed effects β2 and β3 represent the mean change scores in the outcome, respectively, for T2 versus baseline and T3 versus baseline, and with estimates (95% confidence intervals) and p values presented in Table 3. The residual versus fitted diagnostic plots below show that the models are approximately unbiased for all outcomes with residuals roughly scattered around 0.
Azizoddin DR, Kvaternik N, Beck M, et al. Heal the Healers: A pilot study evaluating the feasibility, acceptability, and exploratory efficacy of a Transcendental Meditation intervention for emergency clinicians during the coronavirus disease 2019 pandemic. JACEP Open. 2021;2:e12619. 10.1002/emp2.12619
Funding and support: The David Lynch Foundation and The National Palliative Care Research Center.
Supervising Editor: Henry Wang, MD, MS.
REFERENCES
- 1. Takayesu JK, Ramoska EA, Clark TR, et al. Factors associated with burnout during emergency medicine residency. Acad Emerg Med. 2014;29:1031–1035. [DOI] [PubMed] [Google Scholar]
- 2. Lin M, Battaglioli N, Melamed M, Mott SE, Chung AS, Robinson DW. High prevalence of burnout among US emergency medicine residents: results from the 2017 National Emergency Medicine Wellness Survey. Ann Emerg Med. 2019;74(5):682–690. [DOI] [PubMed] [Google Scholar]
- 3. Kuhn CM, Flanagan EM. Self‐care as a professional imperative: physician burnout, depression, and suicide. Can J Anaesth. 2017;64(2):158–168. [DOI] [PubMed] [Google Scholar]
- 4. Hooper C, Craig J, Janvrin DR, Wetsel MA, Reimels E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. J Emerg Nurs. 2010;36(5):420–427. [DOI] [PubMed] [Google Scholar]
- 5. Bell RB, Davison M, Sefcik D. A first survey . Measuring burnout in emergency medicine physician assistants. JAAPA. 2002;15(3):1–16. [PubMed] [Google Scholar]
- 6. Bridgeman PJ, Bridgeman MB, Barone J. Burnout syndrome among healthcare professionals. Am J Health Syst Pharm. 2018;75(3):147–152. [DOI] [PubMed] [Google Scholar]
- 7. Embriaco N, Papazian L, Kentish‐barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13:482–488. [DOI] [PubMed] [Google Scholar]
- 8. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. [DOI] [PubMed] [Google Scholar]
- 9. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid‐19 pandemic. BMJ. 2020:368:m1121. [DOI] [PubMed] [Google Scholar]
- 10. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID‐19 outbreak. Lancet Psychiatry 2020;7(4):e15–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Arslan HN, Karabekiroglu A, Terzi O, Dundar C. The effects of the COVID‐19 outbreak on physicians’ psychological resilience levels. Postgraduate Med. 2021;133(2):223–230. [DOI] [PubMed] [Google Scholar]
- 13. Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID‐19 pandemic: a cross‐sectional study. Int Arch Occup Environ Health. 2021;94:1345–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gotink RA, Chu P, Busschbach JJV, Benson H, Fricchione GL, Hunink MGM. Standardised mindfulness‐based interventions in healthcare: an overview of systematic reviews and meta‐analyses of RCTs. PLoS One. 2015;10(4):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15. Maricuţoiu LP, Sava FA, Butta O. The effectiveness of controlled interventions on employees’ burnout: a meta‐analysis. J Occup Organ Psychol. 2016;89(1):1–27. [Google Scholar]
- 16. Janssen M, Heerkens Y, Kuijer W, Van Der Heijden B, Engels J. Effects of mindfulness‐based stress reduction on employees’ mental health: A systematic review. 2018;13(1):1166–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dean DJ, Sabagha N, Rose K, et al. A pilot trial of topical capsaicin cream for treatment of cannabinoid hyperemesis syndrome. Acad Emerg Med. 2020;27(11):e0191332. [DOI] [PubMed] [Google Scholar]
- 18. Holt A. Mindfulness‐Based stress reduction and Transcendental Meditation: current state of research. J Patient Cent Res Rev. 2015;2(2):64–68. [Google Scholar]
- 19. Angelopoulou P, Panagopoulou E. Resilience interventions in physicians: a systematic review and meta‐analysis. Appl Psychol. 2021;00(1):23. [DOI] [PubMed] [Google Scholar]
- 20. Orme‐Johnson DW, Barnes VA. Effects of the transcendental meditation technique on trait anxiety: a meta‐analysis of randomized controlled trials. J Altern Complement Med. 2014;20(5):330–341. [DOI] [PubMed] [Google Scholar]
- 21. Valosek L, Wendt S, Link J, et al. Meditation effective in reducing teacher burnout and improving resilience: a randomized controlled study. Front Educ. 2021;6:1–6. [Google Scholar]
- 22. Nidich S, Mills PJ, Rainforth M, et al. Non‐trauma‐focused meditation versus exposure therapy in veterans with post‐traumatic stress disorder: a randomised controlled trial. Lancet Psychiatry. 2018;5(12):975–986. [DOI] [PubMed] [Google Scholar]
- 23. Elder C, Nidich S, Moriarty F, Nidich R. Effect of transcendental meditation on employee stress, depression, and burnout: a randomized controlled study. Perm J. 2014;18(1):19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lebares CC, Coaston TN, Delucchi KL, et al. Enhanced stress resilience training in surgeons: iterative adaptation and biopsychosocial effects in 2 small randomized trials. Ann Surg. 2021;272(3):424–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scalese R, Jarmanning A. CHARTS: Mass. confirmed coronavirus cases by day. https://www.wbur.org/news/2020/03/09/coronavirus‐cases‐massachusetts‐map. Accessed August 21, 2021.
- 26. Smith JL, Allen JW, Haack C, et al. The impact of app‐delivered mindfulness meditation on functional connectivity and self‐reported mindfulness among health profession trainees. Mindfulness. 2021;12(1):92–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dunne PJ, Lynch J, Prihodova L, et al. Burnout in the emergency department: randomized controlled trial of an attention‐based training program. J Integr Med. 2019;17(3):173–180. [DOI] [PubMed] [Google Scholar]
- 28. Anderson JW, Liu C, Kryscio RJ. Blood pressure response to Transcendental Meditation: a meta‐analysis. Am J Hypertens. 2008;21(3):310–316. [DOI] [PubMed] [Google Scholar]
- 29. Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during COVID‐19 pandemic. BMJ. 2020;368:10–12. [DOI] [PubMed] [Google Scholar]
- 30. Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. JAMA. 2020;323(15):1439–1440. [DOI] [PubMed] [Google Scholar]
- 31. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ribeiro Santiago PH, Nielsen T, Smithers LG, Roberts R, Jamieson L. Measuring stress in Australia: validation of the Perceived Stress Scale (PSS‐14) in a national sample. Health Qual Life Outcomes. 2020;18(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cella D, Yount S, Rothrock N, et al. Developing the patient‐reported outcomes measurement information system (PROMIS). Med Care. 2007;45:S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bell RB, Davison M, Sefcik D. A first survey measuring burnout in emergency. JAAPA. 2002;15(3):40–55. [PubMed] [Google Scholar]
- 36. Kuhn G, Goldberg R, Compton S. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine. Ann Emerg Med. 2009;54(1):106–113.e6. [DOI] [PubMed] [Google Scholar]
- 37. Bonamer JR, Aquino‐Russell C. Self‐care strategies for professional development: transcendental meditation reduces compassion fatigue and improves resilience for nurses. J Nurses Prof Dev. 2019;35(2):93–97. [DOI] [PubMed] [Google Scholar]
- 38. Christman LK, Schroeder J, Abdulla R. Long‐term results from a randomized controlled trial to increase cancer screening among attendees of community health centers. Ann Fam Med. 2005;3(2):109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Maslach C, Jackson S, Leiter M. Maslach Burnout Inventory Manual. 3rd ed. Consulting Psychologists Press; 1996. [Google Scholar]
- 40. Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ‐8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. [DOI] [PubMed] [Google Scholar]


