Abstract
Ischaemic heart disease (IHD) is a major cause of morbidity and mortality worldwide. While there have been major advances in this field, these patients are still a higher risk subgroup. As such, strategies to mitigate risk and tailor secondary prevention measures are of the utmost relevance. Cardiac rehabilitation (CR), encompassing several domains including exercise training, cardiovascular risk factor optimization, nutritional and psychological assessments, as well as other ancillary interventions has shown to be one of the pillars in the contemporary management of patients with IHD. Indeed, CR is associated with several benefits in this population, ranging from functional capacity to improvements in outcomes. Whilst this, there are still several issues concerning the optimal application of CR which are still not fully ascertained, such as lack of referral and completion, as well as questions related to programme design (particularly among patients with multiple comorbidities). In this review, we aim at presenting a pragmatic overview on the current role of CR in the management of individuals with IHD, while also discussing some of the caveats in the current data, as well as future concepts which could help improve the uptake and personalization of this pivotal time-tested intervention.
Keywords: Cardiac rehabilitation, Secondary prevention, Myocardial infarction, Ischaemic heart disease, Cardiovascular diseases
Core Tip: Ischaemic heart disease (IHD) is a leading cause of morbidity and mortality. Cardiac rehabilitation (CR) programmes have evolved over the years, as to provide comprehensive frameworks encompassing several domains of secondary prevention and forming an integral part of the contemporary management of individuals with IHD. Whilst this, the optimal application of these programmes, in diverse subsets of patients, remains an evolving and challenging field. In this review, we present a pragmatic overview on the current data concerning CR in IHD, while also discussing some of the caveats and future perspectives in this topic.
INTRODUCTION
Cardiovascular diseases (CVD) are a major cause of morbidity and mortality worldwide[1-3]. Ischaemic heart disease (IHD) is one of its most common presentations, and though significant advances have been made in terms of both its diagnosis and management, patients with IHD still represent a higher risk subgroup[4-6]. Given this background, strategies focused on optimizing overall secondary preventive measures have been the focus of increased interest[4,7,8].
Cardiac rehabilitation (CR) programmes are one of the pillars of the contemporary management of individuals with IHD, being associated with improvements in both morbidity and mortality[6,7,9,10]. Over the years, these programmes have evolved into comprehensive and multidimensional secondary prevention frameworks encompassing several domains ranging from exercise training (ET) to lifestyle counselling, cardiovascular risk factor (CVRF) optimization, psychological interventions, as well as nutritional support and other ancillary interventions[11,12]. While the central role of CR programmes in the management of IHD is currently consensual, there are still several hinderances concerning its optimal application, as manifest by the diversity in programme designs, availability, and patient enrolment[11,13-15]. Moreover, tailoring of these programmes for traditionally less referred subgroups of patients such as women and the elderly, as well as the role of novel strategies to improve referral and completion are also areas of intense interest[8,16-18].
In this review, we aim at presenting a focused and pragmatic overview of the role of CR programmes in the management of individuals with IHD, as well as reviewing some of the challenges and future perspectives concerning this intervention.
CR IN ISCHAEMIC HEART DISEASE
General concepts
Over the last decades, the important role of exercise in the management of individuals with IHD has come under the spotlight[19,20]. Though its potential role in the modulation of anginous symptoms is often ascribed to the classical work of Heberden in the 18th century, the first descriptions of exercise-based rehabilitation in individuals after a myocardial infarction were only reported several years later, well into the 20th century[19,21,22]. Importantly, these early pioneers had a crucial role in changing the then-current status quo of prolonged immobilization, by reporting on the benefits of exercise (adapted to the individual patient) in this specific setting[19]. Since these pivotal landmarks, several studies have extensively reported on the myriad benefits of ET in individuals with IHD[8,9,23,24].
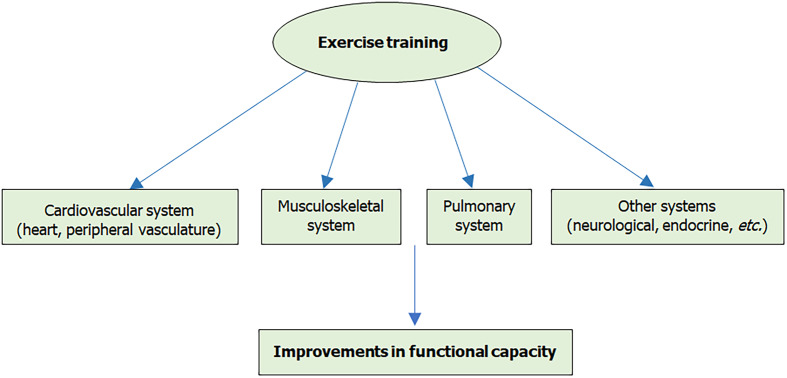
Exercise can have a profound impact on the cardiovascular (CV) system, both in the heart as well as in the peripheral vasculature[10,20,25-27]. Interestingly, though its effect on left ventricular systolic function per se can vary (depending on factors such as the population under study, timing of introduction and type of protocol), data concurs as to the improvements in functional capacity [as assessed by surrogates such as the peak oxygen consumption (pVO2)][20,28-30]. In addition, its impact on other sites such as the pulmonary and musculoskeletal systems should also be kept in mind, particularly when analysing data related to overall functional capacity as well as its impact in the face of the complex multimorbidity patient[20,31-33]. Moreover, and given recent reports illustrating the putative role of inflammation in IHD, the potential modulation of inflammatory pathways by physical activity has also been postulated as being one of the mechanisms underlying the benefits of exercise-based CR[25,34]. Of note, however, that while some mechanistic as well as clinical data have supported this hypothesis, further research is still needed to fully ascertain the potential relative contribution of inflammatory modulation and metabolic substrate utilization to the overall improvements in individuals undergoing CR[25,34-36].
The role of exercise in preventing CVD has been extensively explored, as depicted by the data showing its relevance in reducing the incidence of several pathologies such as heart failure (HF) and mortality[4,37,38]. Interestingly, though some reports have explored the notion that intense ET could potentially lead to detrimental CV effects, as manifest by phenomena ranging from elevations in cardiac biomarkers (such as cardiac troponin and natriuretic peptides) to coronary artery calcification and myocardial fibrosis, data has consistently shown the beneficial effects of moderate regular exercise[27,38-41]. As such, though these factors should be taken into consideration, particularly in terms of exercise prescription and personalization, the plethora of benefits associated with ET should be further highlighted, namely in the setting of IHD[9,10,42] (Figure 1).
Figure 1.
Overview of some of the sites related to the overall effects of exercise training.
CURRENT EVIDENCE CONCERNING CR
As discussed above, there are several potentially beneficial biological effects of ET[25,38,43] (Figure 1). In accordance with these data, it has become one of the central components in the management of IHD[4,6-8]. While the contribution of ET is undisputable, CR programmes have progressively incorporated increasingly different facets, as to provide a comprehensive approach to the individual patient[8,11,12,44]. This progression mirrors the growing complexity of both patients (including multiple comorbidities, the inclusion of older individuals as well as differences in terms of socio-cultural backgrounds) as well as of therapeutic modalities, and as such the need to provide an ever more patient-centred intervention, as to improve outcomes[11,44-46]. Interestingly, as the concept of global CV risk (comprising different CVRF, as well as modulators which could have varying levels of influence) becomes paramount in the CV assessment, the utility of CR in tackling different components of CVD gains additional relevance[4,8,11]. Indeed, reports have shown the benefits of comprehensive programmes, when compared to isolated interventions[44,47]. These concepts are reflected in the current recommendations by different societies, which reinforce the need for CR programmes to include multiple components, as to provide optimal risk management strategies[11,48-50]. In this regard, the European Association of Preventive Cardiology (EAPC) has recently provided guidance on the core components of CR programmes in individuals with IHD (as well as in other CVD), while also presenting a position statement concerning standardization of this intervention[8,11].
Different studies have assessed the impact of CR programmes in the setting of IHD[9,23,51,52]. A meta-analysis performed by Anderson et al[23] reported on significant benefits in terms of CV mortality, hospitalizations, and quality of life. Subsequently, and as to address the relevance of this intervention in a contemporary setting, the CROS-II meta-analysis (including only individuals enrolled by 1995 or later) provided further evidence on CR, as attested by reductions in mortality[9]. The benefits for patients undergoing CR in this setting have also been reported in observational real-word studies[53-55]. Importantly, the CROS-II study also reinforced the need for standardization across different programmes, as to allow further assessments[9,51]. This point should be particularly taken into consideration when analysing data from studies which do not report on benefits in terms of outcomes[51,56-58], as differences in programme design, ET compliance and intensity could (at least partially) explain some of these discrepancies[59-63]. This latter point should be further considered, and it has also been explored when addressing different training methodologies[62,63]. In this regard, albeit high-intensity interval training (HIIT) showed interesting results when compared to moderate continuous training, three large randomized controlled trials in coronary artery disease (CAD), HF with reduced and preserved ejection fractions (respectively) failed to show an advantage of HIIT in terms of the pVO2[62-64]. Importantly, exercise prescription played a pivotal role, as acknowledged by the authors, reinforcing the need for a personalized and highly integrated approach[62,63]. It should also be recalled that the number of CR sessions performed can influence results, as illustrated by data showing that performing a smaller number can lead to worse outcomes[65,66]. These concepts had previously been elegantly raised by Sandercock et al[56] by comparing the case of ET to the prescription of pharmacological therapies, where in both cases dosing issues could affect the overall results of the intervention.
Differential responses should also be further explored, as studies have shown that the functional response to CR (namely as expressed by the pVO2) can be associated with outcomes[67,68]. In this regard De Schutter et al[67], assessing data from 1171 individuals with coronary heart disease (CHD) who underwent a phase II CR programme, showed significant differences in mortality when comparing those who had improvements in pVO2 to those who did not. When assessing pVO2 as a continuous variable, a 1 mL/kg/min improvement in pVO2 was reported as being associated with a 10% reduction in mortality[67]. Recently, Carbone et al[68] also reported that among individuals with CHD undergoing CR, pVO2 at the end of the CR programme was a predictor of mortality. Notably, associations between pVO2 and CV events have also been reported in other settings, further reiterating the need for rigorous programme designs, namely in terms of exercise prescription[8,11,68,69]. Of mention, the timing of CR initiation (after an acute event) should also be taken into consideration as this can be associated not only with reduced uptake and completion but can also influence the response to ET[10,28,29,70].
Another issue which should be discussed pertains to the cost-effectiveness of CR[8,23]. Some studies have suggested the cost-effectiveness of CR among individuals with IHD, while an analysis by Hinde et al[70] also supports potential benefits in expanding overall CR coverage[71-73]. Though these data concur as to the relevance of CR, as discussed by Barradas-Pires, differences in terms of programmes and population under study should also be noted, as standardization of CR programmes (as discussed above) would allow further analysis of the best ways to optimize this intervention, while potentially streamlining patient care[71,74]. Beyond this, it should also be referred that differences in terms of overall policies (when comparing world regions) could also influence CR programmes (namely in terms of accessibility and uptake), a factor which should also be acknowledged[13,14].
While the abovementioned caveats should be kept under consideration, the wealth of data supporting the relevance of CR in individuals with IHD in terms of both morbidity and mortality reinforces its role in this group of patients. This is reflected by current guidelines by both the European Society of Cardiology and the American Heart Association/American College of Cardiology, which attribute these programmes high levels of recommendation in this setting, highlighting the paramount role of contemporary CR in the optimal management of IHD[4,6,7,75,76].
CHALLENGES TO CR
As stated above, CR programmes are endorsed as part of the standard management strategy of IHD[4,6,7,75]. Whilst this, data has shown that CR is often underutilized and that even in those who are referred for this intervention, many do not complete the pre-specified programme[8,13,14,77,78]. Notably, while the issue of CR underutilization can affect a substantial number of individuals, as illustrated by data from the ESC-EORP EUROASPIRE V study where less than half of individuals with CAD were referred for CR, this can particularly affect certain subgroups such as women and older patients[77-81].
A seminal work derived from the European Cardiac Rehabilitation Inventory Survey showed that asymmetries could affect different phases of CR, while also noting geographical differences[14]. This latter issue was also reported on a study assessing CR availability worldwide, showing important differences according to location[13]. Though outside the scope of the present report, several factors encompassing patient-related, physician-related, and system-related barriers can affect CR referral as well as completion[5,14,82-84] (Table 1). As such, and as reviewed by Chindhy et al[83], strategies directed at each of these components should be the focus of further tailoring, as to allow increased CR uptake. Strategies such as physician and patient education on the benefits of CR, automatic patient referral, flexible hours as well as optimization of expense coverage and early appointments after hospital discharge have been among some of the modalities postulated as to tackle some of these barriers[14,83,85]. Additionally, the potential utilization of alternative modalities should also be reflected upon, to mitigate some of these barriers[82,86-88]. Interestingly, and as discussed below, home-based CR (HBCR) as well as the incorporation of different technologies (such as sensors) could also be of interest, as to address some of these gaps[82,83,89,90]. As detailed in a statement concerning HBCR, this could be an option to overcome several barriers to CR such as scheduling, access, and transportation issues, as well as enrolment delays, though pitfalls such as less intensive training, monitoring and safety concerns related to higher risk patients have also been noted as some of its potential disadvantages[89,91,92]. Importantly, data has shown that this strategy can be performed safely while providing several benefits[89,91,93]. Whilst this, differences in programme designs (including patient characteristics as well as programme duration and frequency) should be considered when analysing comparisons with centre-based CR[89]. Interestingly, although older individuals have traditionally been less represented, a study has shown that a home-based programme was associated with significant functional benefits among the elderly, thus showcasing its possible relevance in this subgroup[92,94]. Notwithstanding the major advances facilitated by the growing digitalization of healthcare, adaptation of facilities as to provide the different facets of contemporary CR (including not only ET but also testing, educational sessions and other interventions) should also be reflected upon, as to maximize resource utilization[11,95].
Table 1.
Some of the challenges concerning cardiac rehabilitation uptake and completion
| Suboptimal referral rates |
| Limited access (centre availability, geographical issues, transportation, etc.) |
| Challenges concerning programme design (working hours, participant characteristics, etc.) |
| Low participation of different subsets of patients (women, elderly, patients with multiple comorbidities, etc.) |
| Language barriers |
| Socio-economic issues |
| Low motivation and/or low self-efficacy |
| Challenges in the patient/provider relationship |
| Lack of knowledge concerning cardiac rehabilitation |
One important aspect pertains to the presence of multiple comorbidities among individuals with IHD[8,96,97]. Indeed, as patients present with increasingly complex clinical contexts (such as in the elderly, as well as those with HF and polyvascular disease), tailoring of CR programmes can be particularly challenging[8,96-98]. Notably, ET can be associated with functional improvements such as walking distance in patients with peripheral artery disease (PAD), being recommended as an important part of the management of individuals with intermittent claudication[8,99]. Whilst this, studies have shown that functional benefits can differ when comparing patients with CAD with those who present with both CAD and PAD[96,98,100]. Another frontier field which is rapidly expanding relates to cardio-oncology rehabilitation[8,101]. Importantly, attending to the specificities related both to CV pathophysiology as well as to the potential impact of the oncologic disease and its associated treatments, the most adequate programme should be highly individualized and structured on a multidisciplinary setting[101-104]. Given these backgrounds, optimization of CR programmes in these frontier fields should be the focus of further research.
As mentioned above, the response to CR is an important aspect, as this has been shown in some studies to be associated with outcomes[67,68]. While some factors such as age and gender have been associated with modulation of the response to CR, several others have been postulated as having a role in explaining some of the differences in this response[17,25,67,81]. As expertly reviewed by Gevaert et al[25], the overall determinants to the complex individual response to CR should be further ascertained, as to allow improvements in its application. In this context, both clinical research as well as translational data, supplemented by the possible inclusion of insights gained from the application of novel instruments such as artificial intelligence and multi-omics technologies could improve current knowledge on the pathways involved in the response to CR in different individuals[25,105].
FUTURE PERSPECTIVE
As detailed in the current review, contemporary CR provides an ample secondary prevention framework, able to provide a comprehensive approach to the complex patient with IHD[4,6,8,10]. Nevertheless, questions related to the optimal application of CR among distinct subsets of patients (with a focus on those with different comorbidities) as well as the asymmetries in patient referral and completion still present highly important challenges.
The use of novel technologies has steadily made an impact across different fields of Medicine, including CR[25,90,105-107]. Though the interest in HBCR has been present over the years, with data showing that this could be an interesting option in different subsets of patients, the recent COVID-19 pandemic has markedly expanded the interest in novel models (including hybrid ones) of CR[89,90,108,109]. In this background, models which incorporate concepts of telehealth (namely encompassing different technologies) have been proposed as to allow continuity of care, while minimizing risk[110,111]. Of note, beyond this transitioning phase, these have been postulated as being of potential use to allow for future improvements in overall CR access[90]. Though the use of tele-rehabilitation has made great strides over the last years, as to mitigate some of the barriers associated with CR (particularly in terms of transportation, timing, and potentially cost), questions related to the relative role of hybrid models, as well as of the individuals who could benefit most from these, should be the focus of further study[90,94,109,112]. Moreover, the inclusion of digital tools such as mobile applications as well as sensors (to address not only data related to ET but also to different physiological facets including weight and diet as well as possible CVRF control) should also be a cornerstone of research[90,106,113,114]. Interestingly, some studies highlight the potential in the use of digital applications (often included in the broader concept of mHealth, as the use of wireless technologies with the aim of improving health outcomes) in CR[114]. These could improve access to CR (namely when applied in the framework of HBCR) and allow for more intensive monitoring of different parameters (such as CVRF and physical activity)[90,106,114]. Indeed, some reports have shown that telemonitoring could be of interest in IHD, namely being associated with benefits in functional capacity, whereas the integration of other modalities could allow additional options to address psychological parameters[113,115,116]. In this regard, a randomized study comparing the use of a wrist heart rate monitor with standard training showed that this could be associated with similar increases in pVO2 at twelve weeks, whereas another randomized study (the REMOTE-CR trial, assessing 162 individuals with CHD) showed that cardiac telerehabilitation could lead to comparable results in terms of pVO2[117,118]. While highly promising, questions related to the optimal application of mHealth in CR, particularly in terms of its inclusion across different moments in the CR continuum, should be the focus of additional research[110,114,118,119]. Beyond this, studies aimed at defining the most adequate platforms for a given programme (as well as their comparison to standard methodologies and subsequent validation) and further large, randomized trials would also be of importance, as to allow for an increasingly personalized approach[90,94,120-122].
Another aspect worthy of mention pertains to the functional assessment methodology. While this point has been comprehensively reviewed in a position statement by the EAPC, novel insights (as discussed above) could also add interesting data[11,42,120,121]. While exercise testing (namely cardiopulmonary exercise stress testing) has a central role, other methods have also been described as of potential interest[11,42,90,123,124]. In this regard, the use of the 6-min walk test in assessing exercise progression has been proposed, whereas another recent study (albeit in a small number of individuals) reported on the use of the 200-m fast walking test in tailoring exercise in low to moderate risk CHD patients undergoing HBCR[123,124]. The relative role of these parameters (namely in the face of data derived from digital platforms) should also be further ascertained[121,125].
Finally, the concept of programme standardization will continue to have a central place when addressing the data for CR[8,11,12]. Data from different CVD shows that there are still variances across CR programmes in ET prescription, a fact which should be considered[126,127]. As mentioned above, standardization (and potential certification) of CR programmes could be of marked importance as to allow benchmarking and process optimization, across varied settings[11,12]. In this regard, also the evolution of preventive cardiology as a highly specialized area of Cardiology, as endorsed by the recently published core curriculum in Preventive Cardiology by the EAPC, could allow for further developments in this specific setting[11,128-130].
CONCLUSION
While substantial advances have been made in the management of IHD, this remains a major cause of morbidity and mortality. Contemporary CR programmes encompass a broad range of interventions, aimed at providing a comprehensive secondary prevention approach to these challenging individuals. Though differences in programme design and application should be considered, data has shown its relevance in improving outcomes, across different contexts. Importantly, the optimal strategy in different groups of patients (such as the elderly and other traditionally less represented individuals) remains an evolving field.
As the complexity of IHD in terms of patient characteristics and different therapeutic strategies (with an increasing focus on mitigating residual risk) grows, the central role of CR as a highly tailored intervention will grow ever more relevant, in the era of precision-based personalized medicine.
Footnotes
Conflict-of-interest statement: All authors declare that there are no conflicts on interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: June 27, 2021
First decision: July 30, 2021
Article in press: November 30, 2021
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batalik L S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
Contributor Information
Eduardo M Vilela, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal. eduardomvilela@gmail.com.
Ricardo Ladeiras-Lopes, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal; Department of Surgery and Physiology, Cardiovascular Research Unit (UnIC), Faculty of Medicine, University of Porto, Porto 4200-319, Portugal.
Ana Joao, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal.
Joana Braga, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal.
Susana Torres, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal.
Sofia Viamonte, Centro de Reabilitação do Norte, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4405-565, Portugal.
José Ribeiro, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal.
Madalena Teixeira, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal.
José P Nunes, Faculty of Medicine, University of Porto, Porto 4200-319, Portugal.
Ricardo Fontes-Carvalho, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal; Department of Surgery and Physiology, Cardiovascular Research Unit (UnIC), Faculty of Medicine, University of Porto, Porto 4200-319, Portugal.
References
- 1.Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, Mossialos EA, Maggioni AP, Kazakiewicz D, May HT, De Smedt D, Flather M, Zuhlke L, Beltrame JF, Huculeci R, Tavazzi L, Hindricks G, Bax J, Casadei B, Achenbach S, Wright L, Vardas P European Society of Cardiology. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur Heart J. 2020;41:12–85. doi: 10.1093/eurheartj/ehz859. [DOI] [PubMed] [Google Scholar]
- 2.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 3.Ma LY, Chen WW, Gao RL, Liu LS, Zhu ML, Wang YJ, Wu ZS, Li HJ, Gu DF, Yang YJ, Zheng Z, Hu SS. China cardiovascular diseases report 2018: an updated summary. J Geriatr Cardiol. 2020;17:1–8. doi: 10.11909/j.issn.1671-5411.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;37:2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piepoli MF, Corrà U, Dendale P, Frederix I, Prescott E, Schmid JP, Cupples M, Deaton C, Doherty P, Giannuzzi P, Graham I, Hansen TB, Jennings C, Landmesser U, Marques-Vidal P, Vrints C, Walker D, Bueno H, Fitzsimons D, Pelliccia A. Challenges in secondary prevention after acute myocardial infarction: A call for action. Eur J Prev Cardiol. 2016;23:1994–2006. doi: 10.1177/2047487316663873. [DOI] [PubMed] [Google Scholar]
- 6.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 7.Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 8.Ambrosetti M, Abreu A, Corrà U, Davos CH, Hansen D, Frederix I, Iliou MC, Pedretti RF, Schmid JP, Vigorito C, Voller H, Wilhelm M, Piepoli MF, Bjarnason-Wehrens B, Berger T, Cohen-Solal A, Cornelissen V, Dendale P, Doehner W, Gaita D, Gevaert AB, Kemps H, Kraenkel N, Laukkanen J, Mendes M, Niebauer J, Simonenko M, Zwisler AO. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020:2047487320913379. doi: 10.1177/2047487320913379. [DOI] [PubMed] [Google Scholar]
- 9.Salzwedel A, Jensen K, Rauch B, Doherty P, Metzendorf MI, Hackbusch M, Völler H, Schmid JP, Davos CH. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: Update of the Cardiac Rehabilitation Outcome Study (CROS-II) Eur J Prev Cardiol. 2020;27:1756–1774. doi: 10.1177/2047487320905719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, Collet JP, Corrado D, Drezner JA, Halle M, Hansen D, Heidbuchel H, Myers J, Niebauer J, Papadakis M, Piepoli MF, Prescott E, Roos-Hesselink JW, Graham Stuart A, Taylor RS, Thompson PD, Tiberi M, Vanhees L, Wilhelm M ESC Scientific Document Group. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42:17–96. doi: 10.1093/eurheartj/ehaa605. [DOI] [PubMed] [Google Scholar]
- 11.Abreu A, Frederix I, Dendale P, Janssen A, Doherty P, Piepoli MF, Völler H Secondary Prevention and Rehabilitation Section of EAPC Reviewers: Marco Ambrosetti, Davos CH. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: The avenue towards EAPC accreditation programme: A position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC) Eur J Prev Cardiol. 2020:2047487320924912. doi: 10.1177/2047487320924912. [DOI] [PubMed] [Google Scholar]
- 12.Abreu A, Mendes M, Dores H, Silveira C, Fontes P, Teixeira M, Santa Clara H, Morais J. Mandatory criteria for cardiac rehabilitation programs: 2018 guidelines from the Portuguese Society of Cardiology. Rev Port Cardiol (Engl Ed) 2018;37:363–373. doi: 10.1016/j.repc.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Turk-Adawi K, Supervia M, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, Bjarnason-Wehrens B, Derman W, Abreu A, Babu AS, Santos CA, Jong SK, Cuenza L, Yeo TJ, Scantlebury D, Andersen K, Gonzalez G, Giga V, Vulic D, Vataman E, Cliff J, Kouidi E, Yagci I, Kim C, Benaim B, Estany ER, Fernandez R, Radi B, Gaita D, Simon A, Chen SY, Roxburgh B, Martin JC, Maskhulia L, Burdiat G, Salmon R, Lomelí H, Sadeghi M, Sovova E, Hautala A, Tamuleviciute-Prasciene E, Ambrosetti M, Neubeck L, Asher E, Kemps H, Eysymontt Z, Farsky S, Hayward J, Prescott E, Dawkes S, Santibanez C, Zeballos C, Pavy B, Kiessling A, Sarrafzadegan N, Baer C, Thomas R, Hu D, Grace SL. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine. 2019;13:31–45. doi: 10.1016/j.eclinm.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bjarnason-Wehrens B, McGee H, Zwisler AD, Piepoli MF, Benzer W, Schmid JP, Dendale P, Pogosova NG, Zdrenghea D, Niebauer J, Mendes M Cardiac Rehabilitation Section European Association of Cardiovascular Prevention and Rehabilitation. Cardiac rehabilitation in Europe: results from the European Cardiac Rehabilitation Inventory Survey. Eur J Cardiovasc Prev Rehabil. 2010;17:410–418. doi: 10.1097/HJR.0b013e328334f42d. [DOI] [PubMed] [Google Scholar]
- 15.Thompson MP, Yaser JM, Hou H, Syrjamaki JD, DeLucia A 3rd, Likosky DS, Keteyian SJ, Prager RL, Gurm HS, Sukul D. Determinants of Hospital Variation in Cardiac Rehabilitation Enrollment During Coronary Artery Disease Episodes of Care. Circ Cardiovasc Qual Outcomes. 2021;14:e007144. doi: 10.1161/CIRCOUTCOMES.120.007144. [DOI] [PubMed] [Google Scholar]
- 16.Witvrouwen I, Van Craenenbroeck EM, Abreu A, Moholdt T, Kränkel N. Exercise training in women with cardiovascular disease: Differential response and barriers - review and perspective. Eur J Prev Cardiol. 2019:2047487319838221. doi: 10.1177/2047487319838221. [DOI] [PubMed] [Google Scholar]
- 17.Vilela EM, Ladeiras Lopes R, Torres S, João A, Ribeiro J, Primo J, Fontes-Carvalho R, Campos L, Miranda F, Nunes JPL, Teixeira M, Braga P. Differential Impact of a Cardiac Rehabilitation Program on Functional Parameters in Elderly vs Non-Elderly Myocardial Infarction Survivors. Cardiology. 2020;145:98–105. doi: 10.1159/000504875. [DOI] [PubMed] [Google Scholar]
- 18.Prescott E, Eser P, Mikkelsen N, Holdgaard A, Marcin T, Wilhelm M, Gil CP, González-Juanatey JR, Moatemri F, Iliou MC, Schneider S, Schromm E, Zeymer U, Meindersma EP, Crocamo A, Ardissino D, Kolkman EK, Prins LF, van der Velde AE, Van't Hof AW, de Kluiver EP. Cardiac rehabilitation of elderly patients in eight rehabilitation units in western Europe: Outcome data from the EU-CaRE multi-centre observational study. Eur J Prev Cardiol. 2020;27:1716–1729. doi: 10.1177/2047487320903869. [DOI] [PubMed] [Google Scholar]
- 19.Buckley JP. The changing landscape of cardiac rehabilitation; from early mobilisation and reduced mortality to chronic multi-morbidity management. Disabil Rehabil. 2021:1–8. doi: 10.1080/09638288.2021.1921062. [DOI] [PubMed] [Google Scholar]
- 20.Fontes-Carvalho R, Vilela EM, Gonçalves-Teixeira P. The effect of exercise training in systolic and diastolic function. In: Watson RR, Zibadi S, editors. Lifestyle in heart health and disease. 1st edition. Amsterdam: Elsevier; 2018: 153–162. [Google Scholar]
- 21.Newman LB, Andrews MF, Koblish MO, Baker LA. Physical medicine and rehabilitation in acute myocardial infarction. AMA Arch Intern Med. 1952;89:552–561. doi: 10.1001/archinte.1952.00240040031004. [DOI] [PubMed] [Google Scholar]
- 22.Rojano-Castillo J, Ilarraza-Lomelí H, Zavala-Ramírez J, Cantero-Colín R, Rodríguez-Reyes A, Lerma-Espinosa R, Mancilla-Pérez M, Rius-Suárez MD, García-Saldivia MA. Seventy-five years of cardiovascular rehabilitation in Mexico. Arch Cardiol Mex. 2019;89:233–241. doi: 10.24875/ACME.M19000057. [DOI] [PubMed] [Google Scholar]
- 23.Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016:CD001800. doi: 10.1002/14651858.CD001800.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vilela EM, Ladeiras-Lopes R, Ruivo C, Torres S, Braga J, Fonseca M, Ribeiro J, Primo J, Fontes-Carvalho R, Campos L, Miranda F, Nunes JPL, Gama V, Teixeira M, Braga P. Different outcomes of a cardiac rehabilitation programme in functional parameters among myocardial infarction survivors according to ejection fraction. Neth Heart J. 2019;27:347–353. doi: 10.1007/s12471-019-1269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gevaert AB, Adams V, Bahls M, Bowen TS, Cornelissen V, Dörr M, Hansen D, Kemps HM, Leeson P, Van Craenenbroeck EM, Kränkel N. Towards a personalised approach in exercise-based cardiovascular rehabilitation: How can translational research help? Eur J Prev Cardiol. 2020;27:1369–1385. doi: 10.1177/2047487319877716. [DOI] [PubMed] [Google Scholar]
- 26.Vilela EM, Bastos JC, Rodrigues RP, Nunes JP. High-sensitivity troponin after running--a systematic review. Neth J Med. 2014;72:5–9. [PubMed] [Google Scholar]
- 27.Franklin BA, Thompson PD, Al-Zaiti SS, Albert CM, Hivert MF, Levine BD, Lobelo F, Madan K, Sharrief AZ, Eijsvogels TMH American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council. Exercise-Related Acute Cardiovascular Events and Potential Deleterious Adaptations Following Long-Term Exercise Training: Placing the Risks Into Perspective-An Update: A Scientific Statement From the American Heart Association. Circulation. 2020;141:e705–e736. doi: 10.1161/CIR.0000000000000749. [DOI] [PubMed] [Google Scholar]
- 28.Zhang YM, Lu Y, Tang Y, Yang D, Wu HF, Bian ZP, Xu JD, Gu CR, Wang LS, Chen XJ. The effects of different initiation time of exercise training on left ventricular remodeling and cardiopulmonary rehabilitation in patients with left ventricular dysfunction after myocardial infarction. Disabil Rehabil. 2016;38:268–276. doi: 10.3109/09638288.2015.1036174. [DOI] [PubMed] [Google Scholar]
- 29.Haykowsky M, Scott J, Esch B, Schopflocher D, Myers J, Paterson I, Warburton D, Jones L, Clark AM. A meta-analysis of the effects of exercise training on left ventricular remodeling following myocardial infarction: start early and go longer for greatest exercise benefits on remodeling. Trials. 2011;12:92. doi: 10.1186/1745-6215-12-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ross R, Blair SN, Arena R, Church TS, Després JP, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisløff U American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Cardiovascular and Stroke Nursing; Council on Functional Genomics and Translational Biology; Stroke Council. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation. 2016;134:e653–e699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 31.Louvaris Z, Vogiatzis I. Physiological basis of cardiopulmonary rehabilitation in patients with lung or heart disease. Breathe (Sheff) 2015;11:120–127. doi: 10.1183/20734735.021114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laoutaris ID, Piotrowicz E, Kallistratos MS, Dritsas A, Dimaki N, Miliopoulos D, Andriopoulou M, Manolis AJ, Volterrani M, Piepoli MF, Coats AJS, Adamopoulos S ARISTOS-HF trial (Aerobic, Resistance, InSpiratory Training OutcomeS in Heart Failure) Investigators. Combined aerobic/resistance/inspiratory muscle training as the 'optimum' exercise programme for patients with chronic heart failure: ARISTOS-HF randomized clinical trial. Eur J Prev Cardiol. 2020 doi: 10.1093/eurjpc/zwaa091. [DOI] [PubMed] [Google Scholar]
- 33.Bédard A, Carsin AE, Fuertes E, Accordini S, Dharmage SC, Garcia-Larsen V, Heinrich J, Janson C, Johannessen A, Leynaert B, Sánchez-Ramos JL, Peralta GP, Pin I, Squillacioti G, Weyler J, Jarvis D, Garcia-Aymerich J. Physical activity and lung function-Cause or consequence? PLoS One. 2020;15:e0237769. doi: 10.1371/journal.pone.0237769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thompson G, Davison GW, Crawford J, Hughes CM. Exercise and inflammation in coronary artery disease: A systematic review and meta-analysis of randomised trials. J Sports Sci. 2020;38:814–826. doi: 10.1080/02640414.2020.1735684. [DOI] [PubMed] [Google Scholar]
- 35.Guo Y, Chen J, Qiu H. Novel Mechanisms of Exercise-Induced Cardioprotective Factors in Myocardial Infarction. Front Physiol. 2020;11:199. doi: 10.3389/fphys.2020.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao Z, Li D, Chen Y, Li Y, Huang R, Zhu K, Chen H, Yuan Z, Zheng X, Zhao H, Pu Q, Qi X, Cai D. Early moderate exercise benefits myocardial infarction healing via improvement of inflammation and ventricular remodelling in rats. J Cell Mol Med. 2019;23:8328–8342. doi: 10.1111/jcmm.14710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aune D, Schlesinger S, Leitzmann MF, Tonstad S, Norat T, Riboli E, Vatten LJ. Physical activity and the risk of heart failure: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2021;36:367–381. doi: 10.1007/s10654-020-00693-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parry-Williams G, Sharma S. The effects of endurance exercise on the heart: panacea or poison? Nat Rev Cardiol. 2020;17:402–412. doi: 10.1038/s41569-020-0354-3. [DOI] [PubMed] [Google Scholar]
- 39.Aengevaeren VL, Mosterd A, Sharma S, Prakken NHJ, Möhlenkamp S, Thompson PD, Velthuis BK, Eijsvogels TMH. Exercise and Coronary Atherosclerosis: Observations, Explanations, Relevance, and Clinical Management. Circulation. 2020;141:1338–1350. doi: 10.1161/CIRCULATIONAHA.119.044467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vilela EM, Bettencourt-Silva R, Nunes JP, Ribeiro VG. BNP and NT-proBNP elevation after running--a systematic review. Acta Cardiol. 2015;70:501–509. doi: 10.2143/AC.70.5.3110509. [DOI] [PubMed] [Google Scholar]
- 41.Sharma S, Merghani A, Mont L. Exercise and the heart: the good, the bad, and the ugly. Eur Heart J. 2015;36:1445–1453. doi: 10.1093/eurheartj/ehv090. [DOI] [PubMed] [Google Scholar]
- 42.Hansen D, Abreu A, Ambrosetti M, Cornelissen V, Gevaert A, Kemps H, Laukkanen JA, Pedretti R, Simonenko M, Wilhelm M, Davos CH, Doehner W, Iliou MC, Kränkel N, Völler H, Piepoli M. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: why and how: a position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab007. [DOI] [PubMed] [Google Scholar]
- 43.Ruegsegger GN, Booth FW. Health Benefits of Exercise. Cold Spring Harb Perspect Med. 2018;8 doi: 10.1101/cshperspect.a029694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van Halewijn G, Deckers J, Tay HY, van Domburg R, Kotseva K, Wood D. Lessons from contemporary trials of cardiovascular prevention and rehabilitation: A systematic review and meta-analysis. Int J Cardiol. 2017;232:294–303. doi: 10.1016/j.ijcard.2016.12.125. [DOI] [PubMed] [Google Scholar]
- 45.Bozkurt B, Fonarow GC, Goldberg LR, Guglin M, Josephson RA, Forman DE, Lin G, Lindenfeld J, O'Connor C, Panjrath G, Piña IL, Shah T, Sinha SS, Wolfel E ACC’s Heart Failure and Transplant Section and Leadership Council. Cardiac Rehabilitation for Patients With Heart Failure: JACC Expert Panel. J Am Coll Cardiol. 2021;77:1454–1469. doi: 10.1016/j.jacc.2021.01.030. [DOI] [PubMed] [Google Scholar]
- 46.Pashkow FJ. Cardiac rehabilitation: not just exercise anymore. Cleve Clin J Med. 1996;63:116–123. doi: 10.3949/ccjm.63.2.116. [DOI] [PubMed] [Google Scholar]
- 47.Hu Y, Li L, Wang T, Liu Y, Zhan X, Han S, Huang L. Comparison of cardiac rehabilitation (exercise + education), exercise only, and usual care for patients with coronary artery disease: A non-randomized retrospective analysis. Pharmacol Res Perspect. 2021;9:e00711. doi: 10.1002/prp2.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cowie A, Buckley J, Doherty P, Furze G, Hayward J, Hinton S, Jones J, Speck L, Dalal H, Mills J British Association for Cardiovascular Prevention and Rehabilitation (BACPR) Standards and core components for cardiovascular disease prevention and rehabilitation. Heart. 2019;105:510–515. doi: 10.1136/heartjnl-2018-314206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, Franklin B, Sanderson B, Southard D American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Nutrition, Physical Activity, and Metabolism; American Association of Cardiovascular and Pulmonary Rehabilitation. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 50.Piepoli MF, Corrà U, Adamopoulos S, Benzer W, Bjarnason-Wehrens B, Cupples M, Dendale P, Doherty P, Gaita D, Höfer S, McGee H, Mendes M, Niebauer J, Pogosova N, Garcia-Porrero E, Rauch B, Schmid JP, Giannuzzi P. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol. 2014;21:664–681. doi: 10.1177/2047487312449597. [DOI] [PubMed] [Google Scholar]
- 51.Abell B, Zecchin R, Gallagher R. Making Sense of the Unfavourable Systematic Review of Exercise-Based Cardiac Rehabilitation in the Modern Era: How Should We Proceed? Heart Lung Circ. 2019;28:204–206. doi: 10.1016/j.hlc.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 52.Francis T, Kabboul N, Rac V, Mitsakakis N, Pechlivanoglou P, Bielecki J, Alter D, Krahn M. The Effect of Cardiac Rehabilitation on Health-Related Quality of Life in Patients With Coronary Artery Disease: A Meta-analysis. Can J Cardiol. 2019;35:352–364. doi: 10.1016/j.cjca.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 53.Eijsvogels TMH, Maessen MFH, Bakker EA, Meindersma EP, van Gorp N, Pijnenburg N, Thompson PD, Hopman MTE. Association of Cardiac Rehabilitation With All-Cause Mortality Among Patients With Cardiovascular Disease in the Netherlands. JAMA Netw Open. 2020;3:e2011686. doi: 10.1001/jamanetworkopen.2020.11686. [DOI] [PubMed] [Google Scholar]
- 54.Doimo S, Fabris E, Piepoli M, Barbati G, Antonini-Canterin F, Bernardi G, Maras P, Sinagra G. Impact of ambulatory cardiac rehabilitation on cardiovascular outcomes: a long-term follow-up study. Eur Heart J. 2019;40:678–685. doi: 10.1093/eurheartj/ehy417. [DOI] [PubMed] [Google Scholar]
- 55.Ekblom Ö, Cider Å, Hambraeus K, Bäck M, Leosdottir M, Lönn A, Börjesson M. Participation in exercise-based cardiac rehabilitation is related to reduced total mortality in both men and women: results from the SWEDEHEART registry. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab083. [DOI] [PubMed] [Google Scholar]
- 56.Sandercock GR, Cardoso F, Almodhy M, Pepera G. Cardiorespiratory fitness changes in patients receiving comprehensive outpatient cardiac rehabilitation in the UK: a multicentre study. Heart. 2013;99:785–790. doi: 10.1136/heartjnl-2012-303055. [DOI] [PubMed] [Google Scholar]
- 57.West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart. 2012;98:637–644. doi: 10.1136/heartjnl-2011-300302. [DOI] [PubMed] [Google Scholar]
- 58.Conraads VM, Denollet J, De Maeyer C, Van Craenenbroeck E, Verheyen J, Beckers P. Exercise training as an essential component of cardiac rehabilitation. Heart. 2012;98:674–5; author reply 675. doi: 10.1136/heartjnl-2012-301912. [DOI] [PubMed] [Google Scholar]
- 59.Ibeggazene S, Moore C, Tsakirides C, Swainson M, Ispoglou T, Birch K. UK cardiac rehabilitation fit for purpose? BMJ Open. 2020;10:e037980. doi: 10.1136/bmjopen-2020-037980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McGregor G, Powell R, Kimani P, Underwood M. Does contemporary exercise-based cardiac rehabilitation improve quality of life for people with coronary artery disease? BMJ Open. 2020;10:e036089. doi: 10.1136/bmjopen-2019-036089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nichols S, McGregor G, Breckon J, Ingle L. Current Insights into Exercise-based Cardiac Rehabilitation in Patients with Coronary Heart Disease and Chronic Heart Failure. Int J Sports Med. 2021;42:19–26. doi: 10.1055/a-1198-5573. [DOI] [PubMed] [Google Scholar]
- 62.Conraads VM, Pattyn N, De Maeyer C, Beckers PJ, Coeckelberghs E, Cornelissen VA, Denollet J, Frederix G, Goetschalckx K, Hoymans VY, Possemiers N, Schepers D, Shivalkar B, Voigt JU, Van Craenenbroeck EM, Vanhees L. Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. Int J Cardiol. 2015;179:203–210. doi: 10.1016/j.ijcard.2014.10.155. [DOI] [PubMed] [Google Scholar]
- 63.Ellingsen Ø, Halle M, Conraads V, Støylen A, Dalen H, Delagardelle C, Larsen AI, Hole T, Mezzani A, Van Craenenbroeck EM, Videm V, Beckers P, Christle JW, Winzer E, Mangner N, Woitek F, Höllriegel R, Pressler A, Monk-Hansen T, Snoer M, Feiereisen P, Valborgland T, Kjekshus J, Hambrecht R, Gielen S, Karlsen T, Prescott E, Linke A SMARTEX Heart Failure Study (Study of Myocardial Recovery After Exercise Training in Heart Failure) Group. High-Intensity Interval Training in Patients With Heart Failure With Reduced Ejection Fraction. Circulation. 2017;135:839–849. doi: 10.1161/CIRCULATIONAHA.116.022924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mueller S, Winzer EB, Duvinage A, Gevaert AB, Edelmann F, Haller B, Pieske-Kraigher E, Beckers P, Bobenko A, Hommel J, Van de Heyning CM, Esefeld K, von Korn P, Christle JW, Haykowsky MJ, Linke A, Wisløff U, Adams V, Pieske B, van Craenenbroeck EM, Halle M OptimEx-Clin Study Group. Effect of High-Intensity Interval Training, Moderate Continuous Training, or Guideline-Based Physical Activity Advice on Peak Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction: A Randomized Clinical Trial. JAMA. 2021;325:542–551. doi: 10.1001/jama.2020.26812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Scherrenberg M, Janssen J, Lauwers A, Schreurs I, Swinnen M, Dendale P. Is there an optimal dose of cardiac rehabilitation in coronary artery disease patients? Int J Cardiol. 2021;330:7–11. doi: 10.1016/j.ijcard.2021.01.065. [DOI] [PubMed] [Google Scholar]
- 66.Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.De Schutter A, Kachur S, Lavie CJ, Menezes A, Shum KK, Bangalore S, Arena R, Milani RV. Cardiac rehabilitation fitness changes and subsequent survival. Eur Heart J Qual Care Clin Outcomes. 2018;4:173–179. doi: 10.1093/ehjqcco/qcy018. [DOI] [PubMed] [Google Scholar]
- 68.Carbone S, Kim Y, Kachur S, Billingsley H, Kenyon J, De Schutter A, Milani RV, Lavie CJ. Peak Oxygen Consumption Achieved at the End of Cardiac Rehabilitation Predicts Long-Term Survival in Patients with Coronary Heart Disease. Eur Heart J Qual Care Clin Outcomes. 2021 doi: 10.1093/ehjqcco/qcab032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Franklin BA, Lavie CJ, Squires RW, Milani RV. Exercise-based cardiac rehabilitation and improvements in cardiorespiratory fitness: implications regarding patient benefit. Mayo Clin Proc. 2013;88:431–437. doi: 10.1016/j.mayocp.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 70.Hinde S, Harrison A, Bojke L, Doherty P. Quantifying the impact of delayed delivery of cardiac rehabilitation on patients' health. Eur J Prev Cardiol. 2020;27:1775–1781. doi: 10.1177/2047487320912625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shields GE, Wells A, Doherty P, Heagerty A, Buck D, Davies LM. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart. 2018;104:1403–1410. doi: 10.1136/heartjnl-2017-312809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Oldridge N, Taylor RS. Cost-effectiveness of exercise therapy in patients with coronary heart disease, chronic heart failure and associated risk factors: A systematic review of economic evaluations of randomized clinical trials. Eur J Prev Cardiol. 2020;27:1045–1055. doi: 10.1177/2047487319881839. [DOI] [PubMed] [Google Scholar]
- 73.Hinde S, Bojke L, Harrison A, Doherty P. Improving cardiac rehabilitation uptake: Potential health gains by socioeconomic status. Eur J Prev Cardiol. 2019;26:1816–1823. doi: 10.1177/2047487319848533. [DOI] [PubMed] [Google Scholar]
- 74.Barradas-Pires A. Cardiac rehabilitation programmes: Cost-effective and a potential instrument against health inequalities. Eur J Prev Cardiol. 2020;27:1101–1103. doi: 10.1177/2047487319887829. [DOI] [PubMed] [Google Scholar]
- 75.Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, Gale CP, Gilard M, Jobs A, Jüni P, Lambrinou E, Lewis BS, Mehilli J, Meliga E, Merkely B, Mueller C, Roffi M, Rutten FH, Sibbing D, Siontis GCM ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–1367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 76.Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ ACC/AHA Task Force Members; Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2354–2394. doi: 10.1161/CIR.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 77.Bittner V. Cardiac Rehabilitation for Women. Adv Exp Med Biol. 2018;1065:565–577. doi: 10.1007/978-3-319-77932-4_34. [DOI] [PubMed] [Google Scholar]
- 78.Clark AM, King-Shier KM, Thompson DR, Spaling MA, Duncan AS, Stone JA, Jaglal SB, Angus JE. A qualitative systematic review of influences on attendance at cardiac rehabilitation programs after referral. Am Heart J. 2012;164:835–45.e2. doi: 10.1016/j.ahj.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 79.Pirruccello JP, Traynor K, Aragam KG. "Road Map" to Improving Enrollment in Cardiac Rehabilitation: Identifying Barriers and Evaluating Alternatives. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.007468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kotseva K, De Backer G, De Bacquer D, Rydén L, Hoes A, Grobbee D, Maggioni A, Marques-Vidal P, Jennings C, Abreu A, Aguiar C, Badariene J, Bruthans J, Castro Conde A, Cifkova R, Crowley J, Davletov K, Deckers J, De Smedt D, De Sutter J, Dilic M, Dolzhenko M, Dzerve V, Erglis A, Fras Z, Gaita D, Gotcheva N, Heuschmann P, Hasan-Ali H, Jankowski P, Lalic N, Lehto S, Lovic D, Mancas S, Mellbin L, Milicic D, Mirrakhimov E, Oganov R, Pogosova N, Reiner Z, Stöerk S, Tokgözoğlu L, Tsioufis C, Vulic D, Wood D EUROASPIRE Investigators*. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26:824–835. doi: 10.1177/2047487318825350. [DOI] [PubMed] [Google Scholar]
- 81.Vilela EM, Ladeiras-Lopes R, Joao A, Braga J, Torres S, Ribeiro J, Primo J, Fontes-Carvalho R, Campos L, Miranda F, Nunes JP, Teixeira M, Braga P. Differential impact of a cardiac rehabilitation program in functional parameters according to patient gender. Am J Cardiovasc Dis. 2020;10:367–375. [PMC free article] [PubMed] [Google Scholar]
- 82.Winnige P, Vysoky R, Dosbaba F, Batalik L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World J Clin Cases. 2021;9:1761–1784. doi: 10.12998/wjcc.v9.i8.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chindhy S, Taub PR, Lavie CJ, Shen J. Current challenges in cardiac rehabilitation: strategies to overcome social factors and attendance barriers. Expert Rev Cardiovasc Ther. 2020;18:777–789. doi: 10.1080/14779072.2020.1816464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW American Heart Association Science Advisory and Coordinating Committee. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 85.Ades PA, Keteyian SJ, Wright JS, Hamm LF, Lui K, Newlin K, Shepard DS, Thomas RJ. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map From the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92:234–242. doi: 10.1016/j.mayocp.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lavie CJ, Pack QR, Levine GN. Expanding Traditional Cardiac Rehabilitation in the 21st Century. J Am Coll Cardiol. 2020;75:1562–1564. doi: 10.1016/j.jacc.2020.02.038. [DOI] [PubMed] [Google Scholar]
- 87.Salmoirago-Blotcher E, Wayne PM, Dunsiger S, Krol J, Breault C, Bock BC, Wu WC, Yeh GY. Tai Chi Is a Promising Exercise Option for Patients With Coronary Heart Disease Declining Cardiac Rehabilitation. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.006603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ma J, Zhang JW, Li H, Zhao LS, Guo AY, Chen ZH, Yuan W, Gao TM, Li YM, Li CH, Wang HW, Song B, Lu YL, Cui MZ, Wei QY, Lyu SJ, Yin HC. Safety and effectiveness of a Tai Chi-based cardiac rehabilitation programme for chronic coronary syndrom patients: study protocol for a randomised controlled trial. BMJ Open. 2020;10:e036061. doi: 10.1136/bmjopen-2019-036061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, Forman DE, Franklin BA, Keteyian SJ, Kitzman DW, Regensteiner JG, Sanderson BK, Whooley MA. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Am Coll Cardiol. 2019;74:133–153. doi: 10.1016/j.jacc.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Scherrenberg M, Wilhelm M, Hansen D, Völler H, Cornelissen V, Frederix I, Kemps H, Dendale P. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020:2047487320939671. doi: 10.1177/2047487320939671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dalal HM, Doherty P, McDonagh ST, Paul K, Taylor RS. Virtual and in-person cardiac rehabilitation. BMJ. 2021;373:n1270. doi: 10.1136/bmj.n1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schopfer DW, Whooley MA, Allsup K, Pabst M, Shen H, Tarasovsky G, Duvernoy CS, Forman DE. Effects of Home-Based Cardiac Rehabilitation on Time to Enrollment and Functional Status in Patients With Ischemic Heart Disease. J Am Heart Assoc. 2020;9:e016456. doi: 10.1161/JAHA.120.016456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ramachandran HJ, Jiang Y, Tam WWS, Yeo TJ, Wang W. Effectiveness of home-based cardiac telerehabilitation as an alternative to Phase 2 cardiac rehabilitation of coronary heart disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Snoek JA, Prescott EI, van der Velde AE, Eijsvogels TMH, Mikkelsen N, Prins LF, Bruins W, Meindersma E, González-Juanatey JR, Peña-Gil C, González-Salvado V, Moatemri F, Iliou MC, Marcin T, Eser P, Wilhelm M, Van't Hof AWJ, de Kluiver EP. Effectiveness of Home-Based Mobile Guided Cardiac Rehabilitation as Alternative Strategy for Nonparticipation in Clinic-Based Cardiac Rehabilitation Among Elderly Patients in Europe: A Randomized Clinical Trial. JAMA Cardiol. 2021;6:463–468. doi: 10.1001/jamacardio.2020.5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mazza A, Paneroni M. Gym space in the era of digital cardiovascular rehabilitation: Often overlooked but critically important. Eur J Prev Cardiol. 2020;27:2059–2062. doi: 10.1177/2047487319869576. [DOI] [PubMed] [Google Scholar]
- 96.Nguyen CH, Marzolini S, Oh P, Thomas SG. A Retrospective Comparison of Fitness and Exercise Progression in Patients With Coronary and Peripheral Artery Disease in Cardiac Rehabilitation. Can J Cardiol. 2021;37:260–268. doi: 10.1016/j.cjca.2020.04.013. [DOI] [PubMed] [Google Scholar]
- 97.Taylor RS, Singh S. Personalised rehabilitation for cardiac and pulmonary patients with multimorbidity: Time for implementation? Eur J Prev Cardiol. 2020:2047487320926058. doi: 10.1177/2047487320926058. [DOI] [PubMed] [Google Scholar]
- 98.Tam MC, Longenecker CT, Chow C, Vest M, Sukeena R, Madan Mohan SK, Carman T, Parikh SA, Josephson RA. Occult peripheral artery disease is common and limits the benefit achieved in cardiac rehabilitation. Vasc Med. 2016;21:130–136. doi: 10.1177/1358863X15625370. [DOI] [PubMed] [Google Scholar]
- 99.Aboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Röther J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I ESC Scientific Document Group. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) Eur Heart J. 2018;39:763–816. doi: 10.1093/eurheartj/ehx095. [DOI] [PubMed] [Google Scholar]
- 100.Devrome AN, Aggarwal S, McMurtry MS, Southern D, Hauer T, Lamb B, Arena R, Moore RD, Wilton SB, Stone J, Martin BJ. Cardiac rehabilitation in people with peripheral arterial disease: A higher risk population that benefits from completion. Int J Cardiol. 2019;285:108–114. doi: 10.1016/j.ijcard.2019.02.070. [DOI] [PubMed] [Google Scholar]
- 101.Gilchrist SC, Barac A, Ades PA, Alfano CM, Franklin BA, Jones LW, La Gerche A, Ligibel JA, Lopez G, Madan K, Oeffinger KC, Salamone J, Scott JM, Squires RW, Thomas RJ, Treat-Jacobson DJ, Wright JS American Heart Association Exercise, Cardiac Rehabilitation, and Secondary Prevention Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Peripheral Vascular Disease. Cardio-Oncology Rehabilitation to Manage Cardiovascular Outcomes in Cancer Patients and Survivors: A Scientific Statement From the American Heart Association. Circulation. 2019;139:e997–e1012. doi: 10.1161/CIR.0000000000000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.D'Ascenzi F, Anselmi F, Fiorentini C, Mannucci R, Bonifazi M, Mondillo S. The benefits of exercise in cancer patients and the criteria for exercise prescription in cardio-oncology. Eur J Prev Cardiol. 2019:2047487319874900. doi: 10.1177/2047487319874900. [DOI] [PubMed] [Google Scholar]
- 103.Zamorano JL, Gottfridsson C, Asteggiano R, Atar D, Badimon L, Bax JJ, Cardinale D, Cardone A, Feijen EAM, Ferdinandy P, López-Fernández T, Gale CP, Maduro JH, Moslehi J, Omland T, Plana Gomez JC, Scott J, Suter TM, Minotti G. The cancer patient and cardiology. Eur J Heart Fail. 2020;22:2290–2309. doi: 10.1002/ejhf.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Murray J, Bennett H, Bezak E, Perry R. The role of exercise in the prevention of cancer therapy-related cardiac dysfunction in breast cancer patients undergoing chemotherapy: systematic review. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab006. [DOI] [PubMed] [Google Scholar]
- 105.Tuka V, Linhart A. Personalised exercise prescription: Finding the best for our patients. Eur J Prev Cardiol. 2020;27:1366–1368. doi: 10.1177/2047487319884376. [DOI] [PubMed] [Google Scholar]
- 106.Falter M, Scherrenberg M, Dendale P. Digital Health in Cardiac Rehabilitation and Secondary Prevention: A Search for the Ideal Tool. Sensors (Basel) 2020;21 doi: 10.3390/s21010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Frederix I, Caiani EG, Dendale P, Anker S, Bax J, Böhm A, Cowie M, Crawford J, de Groot N, Dilaveris P, Hansen T, Koehler F, Krstačić G, Lambrinou E, Lancellotti P, Meier P, Neubeck L, Parati G, Piotrowicz E, Tubaro M, van der Velde E. ESC e-Cardiology Working Group Position Paper: Overcoming challenges in digital health implementation in cardiovascular medicine. Eur J Prev Cardiol. 2019;26:1166–1177. doi: 10.1177/2047487319832394. [DOI] [PubMed] [Google Scholar]
- 108.Anderson L, Sharp GA, Norton RJ, Dalal H, Dean SG, Jolly K, Cowie A, Zawada A, Taylor RS. Home-based vs centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6:CD007130. doi: 10.1002/14651858.CD007130.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ambrosetti M, Abreu A, Cornelissen V, Hansen D, Iliou MC, Kemps H, Pedretti RFE, Voller H, Wilhelm M, Piepoli MF, Beccaluva CG, Beckers P, Berger T, Davos CH, Dendale P, Doehner W, Frederix I, Gaita D, Gevaert A, Kouidi E, Kraenkel N, Laukkanen J, Maranta F, Mazza A, Mendes M, Neunhaeuserer D, Niebauer J, Pavy B, Gil CP, Rauch B, Sarzi Braga S, Simonenko M, Cohen-Solal A, Sommaruga M, Venturini E, Vigorito C. Delphi consensus recommendations on how to provide cardiovascular rehabilitation in the COVID-19 era. Eur J Prev Cardiol. 2021;28:541–557. doi: 10.1093/eurjpc/zwaa080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Van Iterson EH, Laffin LJ, Crawford M, Mc Mahan D, Cho L, Khot U. Cardiac Rehabilitation Is Essential in the COVID-19 Era: DELIVERING UNINTERRUPTED HEART CARE BASED ON THE CLEVELAND CLINIC EXPERIENCE. J Cardiopulm Rehabil Prev. 2021;41:88–92. doi: 10.1097/HCR.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yeo TJ, Wang YL, Low TT. Have a heart during the COVID-19 crisis: Making the case for cardiac rehabilitation in the face of an ongoing pandemic. Eur J Prev Cardiol. 2020;27:903–905. doi: 10.1177/2047487320915665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Janssen A, Scherrenberg M, Bonné K, Dendale P. The Jessa Hospital experience for cardiac rehabilitation. Eur Heart J. 2021;42:1451–1453. doi: 10.1093/eurheartj/ehaa439. [DOI] [PubMed] [Google Scholar]
- 113.Song Y, Ren C, Liu P, Tao L, Zhao W, Gao W. Effect of Smartphone-Based Telemonitored Exercise Rehabilitation among Patients with Coronary Heart Disease. J Cardiovasc Transl Res. 2020;13:659–667. doi: 10.1007/s12265-019-09938-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Epstein E, Patel N, Maysent K, Taub PR. Cardiac Rehab in the COVID Era and Beyond: mHealth and Other Novel Opportunities. Curr Cardiol Rep. 2021;23:42. doi: 10.1007/s11886-021-01482-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Szczepańska-Gieracha J, Jóźwik S, Cieślik B, Mazurek J, Gajda R. Immersive Virtual Reality Therapy as a Support for Cardiac Rehabilitation: A Pilot Randomized-Controlled Trial. Cyberpsychol Behav Soc Netw. 2021;24:543–549. doi: 10.1089/cyber.2020.0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dorje T, Zhao G, Tso K, Wang J, Chen Y, Tsokey L, Tan BK, Scheer A, Jacques A, Li Z, Wang R, Chow CK, Ge J, Maiorana A. Smartphone and social media-based cardiac rehabilitation and secondary prevention in China (SMART-CR/SP): a parallel-group, single-blind, randomised controlled trial. Lancet Digit Health. 2019;1:e363–e374. doi: 10.1016/S2589-7500(19)30151-7. [DOI] [PubMed] [Google Scholar]
- 117.Batalik L, Dosbaba F, Hartman M, Batalikova K, Spinar J. Benefits and effectiveness of using a wrist heart rate monitor as a telerehabilitation device in cardiac patients: A randomized controlled trial. Medicine (Baltimore) 2020;99:e19556. doi: 10.1097/MD.0000000000019556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Maddison R, Rawstorn JC, Stewart RAH, Benatar J, Whittaker R, Rolleston A, Jiang Y, Gao L, Moodie M, Warren I, Meads A, Gant N. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart. 2019;105:122–129. doi: 10.1136/heartjnl-2018-313189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Marcin T, Bengel C, Goldberg T, Peterhans J, Eser P, Wilhelm M. Patient interest in mHealth as part of cardiac rehabilitation in Switzerland. Swiss Med Wkly. 2021;151:w20510. doi: 10.4414/smw.2021.20510. [DOI] [PubMed] [Google Scholar]
- 120.Bayoumy K, Gaber M, Elshafeey A, Mhaimeed O, Dineen EH, Marvel FA, Martin SS, Muse ED, Turakhia MP, Tarakji KG, Elshazly MB. Smart wearable devices in cardiovascular care: where we are and how to move forward. Nat Rev Cardiol. 2021;18:581–599. doi: 10.1038/s41569-021-00522-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Meinhart F, Stütz T, Sareban M, Kulnik ST, Niebauer J. Mobile Technologies to Promote Physical Activity during Cardiac Rehabilitation: A Scoping Review. Sensors (Basel) 2020;21 doi: 10.3390/s21010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Falter M, Scherrenberg M, Kaihara T, Dendale P. Exercise-based cardiac rehabilitation: different angles to grasp its beauty. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab105. [DOI] [PubMed] [Google Scholar]
- 123.De Cannière H, Smeets CJP, Schoutteten M, Varon C, Morales Tellez JF, Van Hoof C, Huffel SV, Groenendaal W, Vandervoort P. Short-Term Exercise Progression of Cardiovascular Patients throughout Cardiac Rehabilitation: An Observational Study. J Clin Med. 2020;9 doi: 10.3390/jcm9103160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Batalik L, Konecny V, Dosbaba F, Vlazna D, Brat K. Cardiac Rehabilitation Based on the Walking Test and Telerehabilitation Improved Cardiorespiratory Fitness in People Diagnosed with Coronary Heart Disease during the COVID-19 Pandemic. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18052241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.De Cannière H, Corradi F, Smeets CJP, Schoutteten M, Varon C, Van Hoof C, Van Huffel S, Groenendaal W, Vandervoort P. Wearable Monitoring and Interpretable Machine Learning Can Objectively Track Progression in Patients during Cardiac Rehabilitation. Sensors (Basel) 2020;20 doi: 10.3390/s20123601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hansen D, Rovelo Ruiz G, Doherty P, Iliou MC, Vromen T, Hinton S, Frederix I, Wilhelm M, Schmid JP, Abreu A, Ambrosetti M, Garcia-Porrero E, Coninx K, Dendale P EAPC EXPERT working group. Do clinicians prescribe exercise similarly in patients with different cardiovascular diseases? Eur J Prev Cardiol. 2018;25:682–691. doi: 10.1177/2047487318760888. [DOI] [PubMed] [Google Scholar]
- 127.Vromen T, Peek N, Abu-Hanna A, Kemps HM. Practice Variations in Exercise Training Programs in Dutch Cardiac Rehabilitation Centers: Prospective, Observational Study. Phys Ther. 2019;99:266–275. doi: 10.1093/ptj/pzy140. [DOI] [PubMed] [Google Scholar]
- 128.Shapiro MD, Maron DJ, Morris PB, Kosiborod M, Sandesara PB, Virani SS, Khera A, Ballantyne CM, Baum SJ, Sperling LS, Bhatt DL, Fazio S. Preventive Cardiology as a Subspecialty of Cardiovascular Medicine: JACC Council Perspectives. J Am Coll Cardiol. 2019;74:1926–1942. doi: 10.1016/j.jacc.2019.08.1016. [DOI] [PubMed] [Google Scholar]
- 129.Wilhelm M, Abreu A, Adami PE, Ambrosetti M, Antonopoulou M, Biffi A, Cavarretta E, D'Ascenzi F, Gibson I, Grobbee DE, Iliou MC, Koskinas K, Marques-Vidal P, Nixdorff U, Papadakis M, Piepoli MF, Vassiliou V, Wood D, Dendale P, Halle M. EAPC Core Curriculum for Preventive Cardiology. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab017. [DOI] [PubMed] [Google Scholar]
- 130.Shapiro MD, Fazio S. Preventive cardiology as a dedicated clinical service: The past, the present, and the (Magnificent) future. Am J Prev Cardiol. 2020;1:100011. doi: 10.1016/j.ajpc.2020.100011. [DOI] [PMC free article] [PubMed] [Google Scholar]