Abstract
Purpose of Review
Malnutrition, cancer cachexia, and sarcopenia often co-occur in patients with advanced cancer and are associated with poorer response to chemotherapy and reduced survival. Here, we evaluate the current literature regarding the role of nutrition and these associated conditions in patients with advanced lung cancer.
Recent Findings
While rates of malnutrition are high, nutritional intervention studies have generally been limited by small sample sizes. Novel strategies such as home-based meal delivery may have promise. While no therapy is approved for cancer cachexia, ghrelin agonists and other targeted therapies have yielded promising data in clinical trials. Recent data also suggest that obesity may improve immunotherapy responsiveness.
Summary
Malnutrition and associated muscle wasting are clearly negative prognostic markers in advanced lung cancer. Patients with malnutrition should be urgently referred for dietary counseling and guidelines for nutritional support should be followed. Optimal treatment of these syndromes will likely include nutrition and anti-cachexia interventions used in combination.
Keywords: Lung Cancer, Malnutrition, Sarcopenia, Cancer cachexia, Immunotherapy, Obesity
Introduction
Patients with lung cancer are at risk for malnutrition [1], sarcopenia [2], and cancer cachexia [3]. While these conditions are often present during the early stages of disease, individuals with advanced cancer are typically at highest risk. The presence of one or more of these conditions has been associated with poor outcomes in patients with advanced cancer including reduced treatment tolerance [2], decreased therapeutic efficacy [2], reduced quality-of-life [4], higher healthcare costs [5], poor clinical trial outcomes [6], and reduced survival [7]. Unfortunately, despite some improvements in the management of these conditions over the years, malnutrition, sarcopenia, and cancer cachexia often remain under-recognized and therefore untreated [8, 9]. Thus, there is an urgent need to find better strategies to identify these poor prognostic conditions early and intervene aggressively in an effort to improve cancer outcomes.
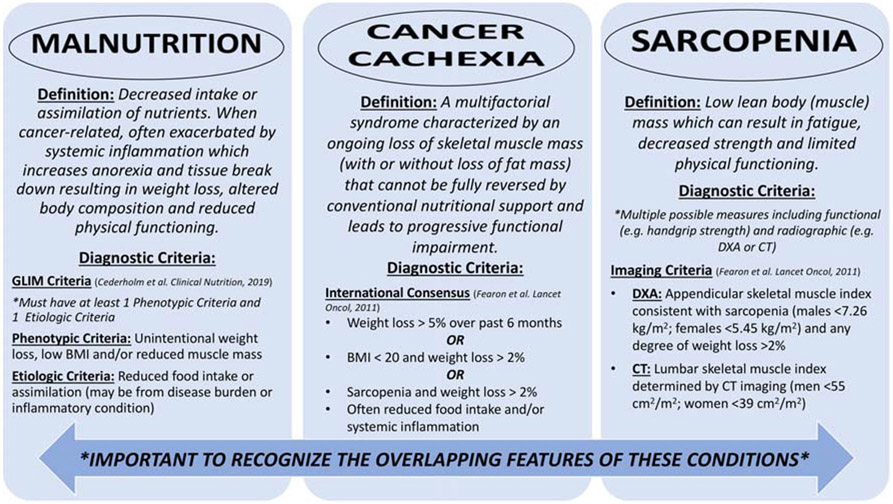
While malnutrition, sarcopenia, and cancer cachexia have overlapping features, it is important to recognize the differences between these conditions (Fig. 1). Malnutrition is commonly defined as a deficiency of energy intake which can lead to altered body composition, impaired physical and mental functioning, and poor clinical outcomes in patients with chronic diseases [10]. Unlike simple malnutrition which should be reversible by caloric repletion alone, cancer-associated malnutrition is far more complex with associated metabolic derangements (e.g., insulin resistance, lipolysis, proteolysis) which may not respond to nutritional repletion. Cancer cachexia is a multifactorial syndrome characterized by skeletal muscle loss with or without loss of adiposity [11]. A number of tumor- and host-related factors (e.g., altered cytokines and systemic inflammation, energy imbalance, adipose tissue depletion) have been implicated in the etiology of cancer cachexia [12]. Sarcopenia is strictly the loss of skeletal muscle mass, strength, and/or function [10]. While inadequate caloric intake is frequently observed in these conditions, conventional nutritional support alone may only partially reverse the weight and muscle loss seen in these conditions.
Fig. 1.
Overlapping features of malnutrition, cancer cachexia, and sarcopenia. GLIM Global Leadership Initiative on Malnutrition, BMI body mass index, DXA dual energy X-ray absorptiometry, CT computed tomography
In this review, we present updated analysis demonstrating the important role nutrition and cachexia play in cancer treatment, and discuss ongoing research efforts to better understand this interplay and eventually develop interventions to improve the outcomes of patients with advanced NSCLC.
Recent Changes in Lung Cancer Therapy
Lung cancer is the greatest cause of cancer-related death in the USA [13]. The treatment for metastatic non-small cell lung cancer (NSCLC), the most common type of lung cancer, has changed dramatically over the course of the last few years. Patients with metastatic NSCLC are now offered treatments tailored to the specific changes detected within the genes or proteins of their tumor cells. Patients may receive targeted therapy based on mutations in EGFR, ALK, and other genes, and these targeted therapies are associated with higher response rates and longer progression-free survival than chemotherapy [14, 15]. Recently, the expression of the checkpoint protein programmed death-ligand 1(PD-L1) has been shown to predict patients that are more likely to respond to treatment with pembrolizumab, an immunotherapy agent, than to standard chemotherapy [16]. In fact, nearly all patients with advanced NSCLC are currently treated with immunotherapy either alone or in combination with chemotherapy as their first treatment option [17-19]. Despite these advances, however, the median overall survival for patients with metastatic NSCLC is still less than 1 year [20], and less than half of patients see a significant decrease in their tumor burden with immunotherapy alone [16]. Multiple biomarkers have been evaluated to better predict which patients will respond to treatment with immunotherapy agents. In addition to PD-L1 expression which is an FDA-approved biomarker, other biomarkers being studied include tumor mutational burden (TMB) [21-23], mismatch-repair status (although uncommon in NSCLC) [24], the host microbiome [25], and weight loss prior to or during treatment, which has long been recognized as an indicator of poor outcome in NSCLC [26, 27].
Malnutrition in Advanced Lung Cancer
There is a high prevalence of malnutrition in patients with lung cancer with reported rates ranging from 34.5 to 69% [28-31]. Malnutrition is particularly prevalent in patients who have been hospitalized and in those with advanced or metastatic disease [30, 32, 33]. While a large proportion of patients with advanced lung cancer have overt malnutrition at the time of their first oncology visit [33], adverse effects of advanced lung cancer treatments can also alter nutritional status. For example, chemotherapy and targeted therapy induced side effects (e.g., nausea/vomiting, diarrhea, taste changes) that can impact an individual’s ability or desire to eat [34]. Malnutrition can also be exacerbated by radiation-related toxicity including mucositis and esophagitis. Immunotherapy-related adverse events such as colitis or pancreatitis may also alter nutritional status, appetite, and oral intake. The toxicity profile of combination chemotherapy-immunotherapy is just beginning to be understood, with any grade of decreased appetite observed in 28% of patients in the landmark KEYNOTE-189 study [17]. Given the strong associations between malnutrition and adverse treatment outcomes (e.g., poorer treatment tolerance, inferior survival, impaired quality-of-life), early identification is critical. Differing rates of malnutrition in the reported literature are likely due to the multiple methods used to screen for and diagnose malnutrition in patients with cancer [35]. Weight loss is available for all patients as part of standard clinical assessments and is a fundamental aspect of most malnutrition screening and assessment strategies, and pre-treatment weight loss at diagnosis is common. For example, in a study of European patients with lung cancer, median weight loss was 6.5%—with 34.5% of patients reporting a weight loss of more than 10% prior to initiation of treatment [31]. Other studies have found that up to 31% of patients had sustained weight loss of 5% or more within 90 days of initiation of radiotherapy [36, 37]. Research shows that pre-diagnosis weight loss is strongly associated with inferior survival with one study showing a 17%, 23%, and 46% increased mortality risk in patients with a pre-diagnosis weight loss of < 5 kg, 5–10 kg, or ≥ 10 kg, respectively [38]. Weight loss can be exacerbated by tumor growth as well as treatment-related complications, and studies show that post-diagnostic weight loss is associated with inferior survival, underscoring the strong prognostic impact of weight loss in this disease [26].
While the significance of weight loss is known, the influence of body mass index (BMI, kg/m2), a commonly used anthropometric measure, on advanced lung cancer outcomes is less clear [38]. Low BMI (e.g., BMI < 18.5 or BMI < 20) is commonly included in diagnostic criteria for malnutrition or cancer cachexia and is clearly associated with negative outcomes in patients with advanced malignancies [11, 39••]. In patients with lung cancer and brain metastases, those who are underweight have inferior survival [40]. While a “normal” BMI ranges from > 18.5 to < 25, recent studies have suggested that a “high-normal” or even “overweight” BMI may be advantageous in some cancer populations, perhaps due to greater lean-mass stores [41]. For example, a recent small retrospective analysis of patients with SCLC found that patients with a BMI ≥ 23 had improved survival [42]. A larger single-center study of 1935 patients with NSCLC (including those with stage III+ disease) who underwent surgical resection at MD Anderson Cancer Center generally found that a higher BMI was associated with improved outcomes [43]. After adjusting for other known prognostic markers, BMI was an independent predictor of survival with a significantly improved overall survival in patients with a BMI ≥ 30 in comparison with a BMI of 25. Population studies in older adults have also suggested a reduced mortality risk in individuals who are overweight (BMI 25–30) or in those with a BMI at the higher-end of the “normal” BMI spectrum (> 23) with all-cause increasing with BMI < 23 [44]. As lung cancer is a disease of aging as the median age of lung cancer diagnosis is 70 [45], higher age-related BMI cutoffs may be particularly relevant in this disease. One major limitation when using BMI is that it does not account for differences in muscle versus fat mass. As the condition of sarcopenic obesity (obesity in the presence of low muscle loss) gains attention as an independent predictor of poor prognosis in cancer [46•], it is likely that body composition assessments which quantify muscle mass in addition to fat mass will ultimately provide enhanced predictive and prognostic ability in advanced lung cancer in comparison with BMI or weight loss alone.
Nutritional Assessment
A number of validated nutritional screening and assessment modalities exist with a superior ability to detect malnutrition than by simply assessing weight loss or BMI alone. The Malnutrition Screening Tool (MST) is commonly used and is an effective predictor of malnutrition risk in oncology outpatients [47]. The MST incorporates two questions to determine risk: weight loss (with increasing points for higher degrees) and decreased appetite. In the MST, a score of 2 or more suggests the individual is “at risk” for malnutrition. The NUTRISCORE screening tool was also recently validated and goes beyond the MST with emphasis on the nutritional risk of the patient’s underlying malignancy and accompanying treatments [48•]. For example, an at-risk patient with lung cancer (moderate risk, additional one point) getting chemoradiation therapy (additional two points) who only has a small amount of weight or appetite loss would be captured with NUTRISCORE. Both the MST and NUTRISCORE have high degrees of sensitivity and specificity for preferred nutritional assessment methods such as the Patient Generated Subjective Global Assessment (PG-SGA) [47, 48•].
The PG-SGA builds upon screening tools, incorporating the impact of performances status, food intake, metabolic stress, and physical findings of muscle loss to provide a comprehensive assessment of nutritional status [49]. The PG-SGA also integrates the impact of nutrition-related symptoms, also known as nutrition-impact symptoms (NIS), such as nausea, diarrhea, or pain which can interfere with eating. Identification of and aggressive treatment of NIS may be particularly valuable in patients with advanced lung cancer who are undergoing systemic anti-neoplastic therapy. In an effort to build a unifying global consensus regarding the diagnostic criteria for malnutrition, the Global Leadership Initiative on Malnutrition (GLIM) criteria were recently published [39••] and provide a framework for the diagnosis of malnutrition in clinical settings. After reviewing the existing approaches to nutritional screening and assessment, the GLIM working group identified specific phenotypic criteria (weight loss, low BMI, or reduced muscle mass) and etiologic criteria (reduced food intake or inflammation) for malnutrition [39••]. Both phenotypic and etiologic criteria are required for diagnosis, and stages of severity are provided. Regardless of the strategy used, we advocate for the clinical integration of a standardized nutritional screening technique longitudinally throughout the treatment of patients with advanced lung cancer to enhance early identification of—and timely intervention for—patients at risk.
Nutritional Interventions
Multiple nutritional interventions can be offered to patients with advanced lung cancer, including dietary counseling, oral nutritional supplements (ONS), enteral feeding, and even parenteral feeding. The choice of nutritional support varies largely on patient-, disease-, and treatment-related factors. While there have been some studies conducted on the routine integration of total parenteral nutrition (TPN) in patients with advanced lung cancer, outcomes were mixed and these studies were mostly conducted in the era prior to modern chemotherapy approaches. For instance, one randomized study studying the effects of 4 weeks of TPN in patients with small cell lung cancer showed temporary improvements in total caloric intake, body weight, and arm muscle circumference; however, there were no long-term improvements in nutritional parameters [50]. A subsequent meta-analysis on routine use of TPN in cancer patients concluded that despite a trend towards improved survival, the risks (e.g., infections) were high without any clinically significant impact on improving chemotherapy toxicity [51]. With respect to enteral feeding (e.g., percutaneous endoscopic gastrostomy (PEG) tube or jejunostomy tube (J-tube) feeding), little data exists regarding routine use in patients with advanced lung cancer. Cancer specific nutrition guideline consensus from major organizations such as the European Society of Parenteral and Enteral Nutrition (ESPEN) and the American Society of Parenteral and Enteral Nutrition (ASPEN) advises against routine use of enteral or parental nutrition in cancer patients [52, 53]. However, certain circumstances may warrant consideration of enteral or parenteral feeding. For instance, if oral food intake has been decreased for a prolonged period of time (e.g., after chemoradiation-induced esophagitis), enteral feeding may be necessary. Though less common in advanced lung cancer, if a patient has lost a large portion of their intestinal tract (e.g., after small bowel obstruction requiring extensive resection), parenteral nutrition may be indicated. In these specific circumstances, clinicians must rely heavily on registered dietitians (RDs) for an accurate assessment of caloric intake and needs while balancing risks and benefits of nutritional support options as part of a multidisciplinary discussion [54].
While routine use of enteral and parenteral feeding is not recommended, routine screening for malnutrition and dietary counseling by an RD with or without use of ONS is strongly recommended in inpatients and outpatients with malnutrition and advanced cancer [52]. Some studies have specifically evaluated the impact of dietary counseling with or without ONS interventions on outcomes in patients with lung cancer (Table 1) [55-62]. Studies evaluated interventions ranging from dietary counseling alone, ONS alone to dietary counseling with ONS [55-62]. The studies are heterogeneous with respect to the clinical setting of the intervention (e.g., during chemoradiation versus chemotherapy alone), the duration of intervention (few weeks to 6 months), intensity of intervention, and trial type (randomized versus single arm). Unfortunately, most studies are also limited by a small sample size making it challenging to derive conclusions regarding efficacy. Nonetheless, certain interventions did show some improvements in weight maintenance, muscle function, or even quality-of-life. ONS containing omega-3 polyunsaturated fatty acids seemed particularly promising in preventing muscle or weight loss and should be evaluated in larger studies [59]. Preliminary data from a novel home food and snack delivery intervention strategy appears promising and should be studied in larger, randomized studies [61]. The integration of commonly used nutritional support strategies in conjunction with anti-cachexia therapies may be particularly valuable and efficacious.
Table 1.
Examples of previously completed nutritional intervention studies in lung cancer
| Study (year of publication) | a) Tumor type b) Setting c) Study design sample size |
a) Intervention b) Control c) Duration |
Key results | Main conclusions |
|---|---|---|---|---|
| Tozer [55] (2008) |
a) Stage III and IV NSCLC b) Patients receiving radiation or chemotherapy or both c) Randomized control trial (double-blind) d) Intervention (n = 32), control (n = 34) |
a) 30 g of cysteine-rich protein ONS daily b) Casein protein in same volume and presentation c) 6 months |
Significant increase in body mass and handgrip strength compared with control group No impact on survival |
Cysteine-rich protein ONS compared with casein-based formula reduced weight loss and improved muscle function Small study and little impact of interventions in patients near end-of-life |
| Van der Meji [56, 57] (2010, 2012) |
a) Stage III NSCLC b) During chemotherapy and thoracic radiation c) Randomized control trial (double-blind) d) Intervention (n = 21), control (n = 21) |
a) Protein and energy dense ONS (2 cans daily) with omega-3 polyunsaturated fatty acids (PUFA) providing 2.02 g EPA plus 0.92 g DHA daily b) Isocaloric control ONS without added PUFA c) 5 weeks during chemoradiation therapy |
No significant improvement in body weight, handgrip strength Intervention group had significantly improved QOL and social functioning, less nausea and vomiting, better physical and cognitive functioning |
ONS with added PUFA may improve QOL but not body mass or muscle function Small study and planned recruitment not achieved Plasma lipid testing suggestive of dietary EPA consumption against protocol which could have diluted effect of intervention |
| Murphy [58] (2011) |
a) Stage III or IV NSCLC b) During first-line platinum based doublet chemotherapy c) Open-label controlled study with prospective reference group d) Intervention (n = 17), control/ standard of care (n = 24) |
a) Patients instructed to take 2.2 g EPA daily in capsule or liquid form b) Standard of care (not placebo-controlled) c) At least 6 weeks (2 cycles of chemotherapy) |
Significant improvement in weight and muscle preservation | EPA reduces muscle and adipose tissue wasting and improves muscle quality in patients with advanced NSCLC getting first-line platinum doublet chemotherapy No placebo control and small study size are limitations |
| Sanchez-Lara [59] (2014) |
a) Stage III or IV NSCLC b) During first-line platinum based doublet chemotherapy c) Open-label controlled study with prospective reference groups d) Intervention fish oil group (n = 16), standard of care group (n = 24) and reference group (n = 104) |
a) Patients instructed to take 2.2 g EPA daily in capsule or liquid form b) Standard of care (not placebo-controlled) c) Duration of chemotherapy |
Intervention group were able to maintain weight in comparison with average weight loss of 2.3 kg in standard of care group Increase in ability to gain or maintain muscle mass in intervention group Patients with highest plasma EPA levels had greatest gain in muscle mass |
ONS with fish oil (EPA) improves maintenance of weight and muscle mass in patients with stage III or IV NSCLC undergoing chemotherapy First study to evaluate the effect of fish oil supplementation on CT-based sarcopenia assessments |
| Kiss [60] (2016) |
a) Stage IIA-IIIB NSCLC or SCLC b) Patients receiving chemoradiation c) Randomized control trial (non-blinded) d) Intervention (n = 11), control (n = 12) |
a) Intensive dietary counseling b) Usual care c) 7 weeks (1 week before chemoradiation thru duration of chemoradiation) |
Clinically important improvements in weight, fat-free mass, physical well-being and functional well-being, though most differences were non-significant | Showed the feasibility acceptability of dietary counseling during chemoradiation for lung cancer Limited by small sample size and attrition of 37% |
| Leedo [61] (2017) |
a) Stage II-IV NSCLC or SCLC b) Any treatment or no treatment c) Randomized control trial (non-blinded) d) Intervention (n = 21), control (n = 19) |
a) Energy and protein rich main meals and snacks delivered three times per week b) Continuation of habitual diet c) 12 weeks |
Intervention group improved Chair Stand Test compared with control Intervention had positive impact on performance score Higher energy and protein intakes were associated with improved QOL, handgrip strength, symptom burden |
Food delivery program with energy and protein rich meals and snacks can improve muscle strength and performance status Limited by small sample size |
| Tanaka [62] (2018) |
a) Inoperable (primarily stage IIIB-IV) b) Patients receiving chemotherapy c) Single arm study with retrospective cohort as comparator d) Intervention (n = 10), control (n = 38) |
a) Dietary counseling and ONS b) Retrospective comparator who received usual care c) 90 days |
Patients in intervention did not have significant weight or BMI loss during the 90 day intervention Those in intervention had a higher odds of weight gain than those in retrospective cohort |
Early nutritional intervention reduces weight loss. No significant improvements in QOL, inflammatory biomarkers were seen. Study limited by small sample size and lack of prospective control arm. |
NSCLC non-small cell lung cancer, ONS oral nutritional supplementation, N sample size, PUFA polyunsaturated fatty acid, QOL quality-of-life, EPA eicosapentanoic acid, gm gram, CT computed tomography, SCLC small cell lung cancer
Pre-Clinical and Clinical Studies Targeting Cachexia in NSCLC
As immunotherapy continues to transform the management of advanced solid and hematologic malignancies, an ongoing challenge has been identifying and utilizing appropriate pre-clinical immune-competent models [63]. Multiple murine models of cancer cachexia have been described including several models of lung cancer that exhibit wasting [64, 65]. The Lewis Lung Carcinoma (LLC) model is well characterized and has been used extensively in the pre-clinical evaluation of anti-cachectic therapy. Notably, administration of ghrelin was associated with improved cachectic outcomes in LLC-tumor-bearing mice [66]. Ghrelin is the ligand for the G protein–coupled ghrelin receptor (GRLN) [67], leads to growth hormone (GH) release, and has anabolic and anti-inflammatory properties [68].
Targeting Ghrelin in Cancer Cachexia
Based on strong pre-clinical evidence, anamorelin, an orally active ghrelin receptor agonist, was evaluated in phase 1 and 2 studies of patients with a variety of tumor types as well as in the phase 3 setting in patients with NSCLC [69•]. The phase 3 program included two phase 3, double-blinded, randomized, placebo-controlled international clinical trials (ROMANA 1 and 2) in patients with stage III or IV NSCLC. Eligibility criteria included involuntary weight loss of at least 5% within the prior 6 months or a BMI less than 30 kg/m2. Patients were stratified by cancer treatment status—starting new course of chemotherapy and/or radiation, maintenance chemotherapy, or no active treatment—geographic region, and degree of weight loss. However, patients were not stratified by stage of disease, histology of NSCLC, treatment regimen, time from diagnosis, ECOG performance score, or molecular biomarkers. The study co-primary endpoints were change in lean body mass and handgrip strength at 12 weeks. Secondary endpoints included change in bodyweight, symptoms of cachexia and fatigue, and overall survival at 1 year. A total of 484 patients were enrolled in ROMANA 1 and 495 in ROMANA 2. In both studies, patients who received anamorelin had a statistically significant increase in lean body mass but neither study demonstrated a difference in handgrip strength. Additional post hoc analyses demonstrated higher total body mass, fat mass, and appendicular lean body mass in patients who received anamorelin compared with those receiving placebo. No significant difference was observed in 1-year overall survival in patients who received anamorelin (hazard ratio 1.06; 95% confidence interval [CI] 0.89, 1.26, p = 0.47) [69•]. In both ROMANA 1 and 2, anamorelin was overall well tolerated, with a slight increased risk of hypoglycemia and poorly controlled diabetes observed in patients receiving anamorelin. In the safety extension ROMANA 3 study, which evaluated 513 of the 703 patients initially enrolled to ROMANA 1 and 2 for an additional 12 weeks (i.e., weeks 12–24), no new safety signals emerged, with most common toxicities being grade 1 and 2 edema, nausea, vomiting, and constipation [70]. Although neither study demonstrated an improvement in handgrip strength, which was a co-primary endpoint, the improvement in lean body mass and cachexia-related symptoms was felt to be promising and an ongoing phase 3 study is ongoing to evaluate administration of anamorelin over 24 weeks in patients with NSCLC, with a composite primary endpoint of body weight gain and improvement in the Anorexia Symptom Scale (NCT03743051).
Similar to anamorelin, the selective androgen receptor modulator enobosarm was evaluated as anti-cachectic therapy in advanced NSCLC patients [71]. Enobosarm’s registration trials differed from the ROMANA trials in their primary endpoint (stair climb power test) and enrollment criteria (no weight loss required) but similarly failed to successfully demonstrate efficacy [72].
Immunotherapy Antibody Clearance and Cancer Cachexia
As mentioned, the introduction of immune checkpoint inhibitors (ICI) in the first- and second-line setting for patients with advanced NSCLC has transformed clinical outcomes for these patients. However, mechanisms of primary and acquired resistance remain unknown. Notably, recent studies have demonstrated pembrolizumab and nivolumab baseline clearance (CL0) was among the strongest predictors of overall survival in multivariate analyses in patients with NSCLC and melanoma [73•, 74-76]. However, somewhat paradoxical is the absence of a relationship between drug exposure and clinical response with immune checkpoint inhibitors (ICIs) [73•, 75, 77, 78], suggesting that increased clearance of ICIs is not the key cause of poor outcomes but rather a surrogate marker of other underlying mechanisms leading to poor outcomes. Similarly, ICI antibody clearance often decreases over time in lung cancer and other diseases, and greater magnitude of decrease in clearance is associated with better outcomes [79]. Elevated protein turnover and antibody drug clearance often occur in catabolic disorders such as cachexia, and close association of high antibody CL0, shorter survival, and presence of cachectic features was noted in both NSCLC and melanoma patients treated with pembrolizumab [73•]. However, these studies have not assessed patients based on the consensus definition of cachexia [11], and the underlying mechanisms tying ICI therapy, high CL0, and poor outcomes in patients with cachectic features remain to be studied [80, 81].
Biomarkers and Future Directions
There remains a clear need to identify cachectic NSCLC patients as soon as possible yet reliable biomarkers of cachexia have yet to be identified [82]. Driven by the strong relationship between low lean body mass and poor outcomes in other cancers [83], CT-derived assessments of body composition are being explored in NSCLC patients [84]. Though not without its challenges [85], the use of diagnostic or cancer staging image information to asses cachexia in NSCLC patients has demonstrated some promise [86]. Lastly, the recent recognition of the importance of gut microbiome in impacting responsiveness to immunotherapy [25], as well as data supporting the role of the microbiome in cancer cachexia [87, 88], points to a possible novel role for the gut microbiome to impact not only the efficacy of cancer therapy but also to prevent cachexia. One promising study demonstrated that modulating the gut microbiome could improve not only cachexia but also exert anti-tumor effects in pre-clinical models of leukemia and cachexia [89].
Obesity and Immunotherapy Responsiveness
Despite the marked success of PD1/PD-L1 inhibition in the treatment of lung cancer, treatment responses vary and far-reaching efforts are underway to identify biomarkers or clinical features as tools to forecast treatment response [17, 90, 91]. Obesity leads to a state of chronic inflammation which can augment T cell presence and function. This may be characterized as T cell exhaustion associated with a progressive loss of effector function following chronic antigen exposure or inflammatory state, and has been characterized in cases of viral infection, autoimmunity, and cancer [92]. Wang et al. found there were significantly fewer tumor-infiltrating T cells and significantly increased PD-1 expression in tumors of obese patients [93]. Clinically, through an analysis of a cohort (n = 250) of patients with various cancers who received treatment with a checkpoint inhibitor, there was an improved response among patients with high BMI. Patients with BMI > 30 achieved significant improvement in progression-free survival (median, 237 days versus 141 days) and overall survival (median, 523 days versus 361 days) when compared with patients with normal BMI. Notably, there were no increases in immune-related adverse effects observed in obese patients [93]. Obesity, which is linked to an increased risk of certain cancers and tumor progression through the milieu of chronic inflammation and metabolic dysfunction, yields accelerated immune senescence or exhaustion that may yet offer vulnerability that can be harnessed for dedicated cancer treatment [92-94, 95•].
Conclusion
Malnutrition, sarcopenia, and cancer cachexia are associated with poor outcomes in advanced lung cancer. Oncology healthcare providers and organizations should include nutritional screening and assessment mechanisms to identify these conditions early and nutritional support should be provided appropriately. A number of novel biomarkers of malnutrition, sarcopenia, and cancer cachexia are being evaluated, and anti-cachexia agents are currently being evaluated in late-phase clinical trials. Additional biomarkers such as the role of the intestinal microbiome or obesity may also play a key role in predicting response to lung cancer therapies including immunotherapy. Though data from large randomized studies is lacking, research suggests that early and aggressive nutritional interventions may improve outcomes in this disease. Future studies should evaluate multimodal approaches (e.g., anti-cachexia therapies in conjunction with nutritional support) to optimize the efficacy of interventions.
Footnotes
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest Rishi Jain declares that he has no conflict of interest. Chris Coss has received compensation from Immuneering for service as a consultant; has patents pending on anti-cachexia therapeutic strategies; was a previous employee of GTx, Inc., which developed Enobosarm as an anti-cachexia therapy, but has had no financial or other relationship with GTx since 2014. Peter Whooley declares that he has no conflict of interest. Mitch Phelps declares that he has no conflict of interest. Dwight H. Owen has received research funding (paid to his institution) from Merck, Bristol-Myers Squibb, Palobiofarma, and Genentech; has received compensation from AstraZeneca for participation on an advisory board; and has received compensation from theMednet for service as a consultant.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Baracos VE. Cancer-associated malnutrition. Eur J Clin Nutr. 2018;72(9):1255–9. [DOI] [PubMed] [Google Scholar]
- 2.Bozzetti F Forcing the vicious circle: sarcopenia increases toxicity, decreases response to chemotherapy and worsens with chemotherapy. Ann Oncol. 2017;28(9):2107–18. [DOI] [PubMed] [Google Scholar]
- 3.Fearon KC, Glass DJ, Guttridge DC. Cancer cachexia: mediators, signaling, and metabolic pathways. Cell Metab. 2012;16(2):153–66. [DOI] [PubMed] [Google Scholar]
- 4.Nipp RD, Fuchs G, El-Jawahri A, et al. Sarcopenia is associated with quality of life and depression in patients with advanced cancer. Oncologist. 2018;23(1):97–104. 10.1634/theoncologist.2017-0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goates S, Du K, Braunschweig CA, Arensberg MB. Economic burden of disease-associated malnutrition at the state level. PLoS One. 2016;11(9). 10.1371/journal.pone.0161833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jain R, Handorf E, Khare V, Blau M, Chertock Y, Hall MJ. Impact of baseline nutrition and exercise status on toxicity and outcomes in phase I and II oncology clinical trial participants. Oncologist. 2020;25(2):161–69. 10.1634/theoncologist.2019-0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer. 2016;57:58–67. [DOI] [PubMed] [Google Scholar]
- 8.Walsh D, et al. Malnutrition in cancer care: time to address the elephant in the room. J Oncol Pract. 2019;15(7):357–9. [DOI] [PubMed] [Google Scholar]
- 9.Ryan AM, Power DG, Daly L, Cushen SJ, Ní Bhuachalla Ē, Prado CM. Cancer-associated malnutrition, cachexia and sarcopenia: the skeleton in the hospital closet 40 years later. Proc Nutr Soc. 2016;75(2):199–211. [DOI] [PubMed] [Google Scholar]
- 10.Cederholm T, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64. [DOI] [PubMed] [Google Scholar]
- 11.Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–95. [DOI] [PubMed] [Google Scholar]
- 12.Baracos VE, et al. Cancer-associated cachexia. Nat Rev Dis Primers. 2018;4:17105. [DOI] [PubMed] [Google Scholar]
- 13.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
- 14.Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim DW, et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377(9):829–38. [DOI] [PubMed] [Google Scholar]
- 15.Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25. [DOI] [PubMed] [Google Scholar]
- 16.Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–33. [DOI] [PubMed] [Google Scholar]
- 17.Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, de Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078–92. [DOI] [PubMed] [Google Scholar]
- 18.Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819–30. [DOI] [PubMed] [Google Scholar]
- 19.Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gümüş M, Mazières J, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med. 2018;379(21):2040–51. [DOI] [PubMed] [Google Scholar]
- 20.Abernethy AP, Arunachalam A, Burke T, McKay C, Cao X, Sorg R, et al. Real-world first-line treatment and overall survival in non-small cell lung cancer without known EGFR mutations or ALK rearrangements in US community oncology setting. PLoS One. 2017;12(6):e0178420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carbone DP, Reck M, Paz-Ares L, Creelan B, Horn L, Steins M, et al. First-line Nivolumab in stage IV or recurrent non–small-cell lung cancer. N Engl J Med. 2017;376(25):2415–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hellmann MD, Ciuleanu TE, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C, et al. Nivolumab plus Ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Mutational landscape determines sensitivity to PD-1 blockade in non–small cell lung cancer. Science. 2015;348(6230):124–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le DT, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372(26):2509–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Routy B, le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359(6371):91–7. [DOI] [PubMed] [Google Scholar]
- 26.Mytelka DS, Li L, Benoit K. Post-diagnosis weight loss as a prognostic factor in non-small cell lung cancer. J Cachexia Sarcopenia Muscle. 2018;9(1):86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sanders KJ, Hendriks LE, Troost EG, Bootsma GP, Houben RM, Schols AM, et al. Early weight loss during chemoradiotherapy has a detrimental impact on outcome in NSCLC. J Thorac Oncol. 2016;11(6):873–9. [DOI] [PubMed] [Google Scholar]
- 28.Segura A, Pardo J, Jara C, Zugazabeitia L, Carulla J, de Las Peñas R, et al. An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin Nutr. 2005;24(5):801–14. [DOI] [PubMed] [Google Scholar]
- 29.Read JA, Choy SB, Beale P, Clarke SJ. An evaluation of the prevalence of malnutrition in cancer patients attending the outpatient oncology clinic. Asia Pac J Clin Oncol. 2006;2(2):80–6. [Google Scholar]
- 30.Hebuterne X, et al. Prevalence of malnutrition and current use of nutrition support in patients with cancer. JPEN J Parenter Enteral Nutr. 2014;38(2):196–204. [DOI] [PubMed] [Google Scholar]
- 31.Bozzetti F, Mariani L, Lo Vullo S, SCRINIO Working Group, Amerio ML, Biffi R, et al. The nutritional risk in oncology: a study of 1,453 cancer outpatients. Support Care Cancer. 2012;20(8):1919–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal E, Ferguson M, Banks M, Bauer J, Capra S, Isenring E. Nutritional status and dietary intake of acute care patients: results from the Nutrition Care Day Survey 2010. Clin Nutr. 2012;31(1):41–7. [DOI] [PubMed] [Google Scholar]
- 33.Muscaritoli M, Lucia S, Farcomeni A, Lorusso V, Saracino V, Barone C, et al. Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study. Oncotarget. 2017;8(45):79884–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campagna S, et al. Prevalence, severity, and self-reported characteristics of taste alterations in patients receiving chemotherapy. Oncol Nurs Forum. 2018;45(3):342–53. [DOI] [PubMed] [Google Scholar]
- 35.Bharadwaj S, Ginoya S, Tandon P, et al. Malnutrition: laboratory markers vs nutritional assessment. Gastroenterol Rep (Oxf). 2016;4(4):272–80. 10.1093/gastro/gow013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kiss N, Isenring E, Gough K, Krishnasamy M. The prevalence of weight loss during (chemo)radiotherapy treatment for lung cancer and associated patient- and treatment-related factors. Clin Nutr. 2014;33(6):1074–80. [DOI] [PubMed] [Google Scholar]
- 37.Kiss N, et al. Dosimetric factors associated with weight loss during (chemo)radiotherapy treatment for lung cancer. Eur J Clin Nutr. 2014;68(12):1309–14. [DOI] [PubMed] [Google Scholar]
- 38.Morel H, et al. Prediagnosis weight loss, a stronger factor than BMI, to predict survival in patients with lung cancer. Lung Cancer. 2018;126:55–63. [DOI] [PubMed] [Google Scholar]
- 39.••. Cederholm T, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr. 2019;38(1):1–9 This is a recent global consensus on the assessment of malnutrition. Both phenotypic and etiologic criteria for malnutrition are reviewed.
- 40.Masel EK, et al. Decreased body mass index is associated with impaired survival in lung cancer patients with brain metastases: a retrospective analysis of 624 patients. Eur J Cancer Care (Engl). 2017;26(6). [DOI] [PubMed] [Google Scholar]
- 41.Greenlee H, et al. Association between body mass index (BMI) and cancer survival in a pooled analysis of 22 clinical trials. Cancer Epidemiol Biomark Prev. 2017;26(1):21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee CH, Lin C, Wang CY, et al. Premorbid BMI as a prognostic factor in small-cell lung cancer—a single institute experience. Oncotarget. 2018;9(37):24642–52. 10.18632/oncotarget.24935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sepesi B, Gold KA, Correa AM, Heymach JV, Vaporciyan AA, Roszik J, et al. The influence of body mass index on overall survival following surgical resection of non-small cell lung cancer. J Thorac Oncol. 2017;12(8):1280–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Winter JE, MacInnis R, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. 2014;99(4):875–90. [DOI] [PubMed] [Google Scholar]
- 45.@NCICancerStats. Cancer of the lung and bronchus - Cancer Stat Facts. 2019; Available from: https://seer.cancer.gov/statfacts/html/lungb.html.
- 46.•. Prado CM, et al. Sarcopenia and cachexia in the era of obesity: clinical and nutritional impact. Proc Nutr Soc. 2016;75(2):188–98 This article reviews the impact of sarcopenia and the entity of sarcopenic obesity on clinical outcomes.
- 47.Isenring E, Cross G, Daniels L, Kellett E, Koczwara B. Validity of the malnutrition screening tool as an effective predictor of nutritional risk in oncology outpatients receiving chemotherapy. Support Care Cancer. 2006;14(11):1152–6. [DOI] [PubMed] [Google Scholar]
- 48.•. Arribas L, et al. NUTRISCORE: a new nutritional screening tool for oncological outpatients. Nutrition. 2017;33:297–303 This article offers a nutritional screening tool that can be intergrated in clinical practice.
- 49.Bauer J, Capra S, Ferguson M. Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr. 2002;56(8):779–85. [DOI] [PubMed] [Google Scholar]
- 50.Evans WK, Makuch R, Clamon GH, Feld R, Weiner RS, Moran E, et al. Limited impact of total parenteral nutrition on nutritional status during treatment for small cell lung cancer. Cancer Res. 1985;45(7):3347–53. [PubMed] [Google Scholar]
- 51.McGeer AJ, Detsky AS, O'Rourke K. Parenteral nutrition in cancer patients undergoing chemotherapy: a meta-analysis. Nutrition. 1990;6(3):233–40. [PubMed] [Google Scholar]
- 52.Arends J, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36(5):1187–96. [DOI] [PubMed] [Google Scholar]
- 53.August DA, Huhmann MB. A.S.P.E.N. clinical guidelines: nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. JPEN J Parenter Enteral Nutr. 2009;33(5):472–500. [DOI] [PubMed] [Google Scholar]
- 54.Jain R, Dotan E. Nutrition and aging: a practicing oncologist’s perspective. Curr Oncol Rep. 2017;19(11):71. [DOI] [PubMed] [Google Scholar]
- 55.Tozer RG, Tai P, Falconer W, Ducruet T, Karabadjian A, Bounous G, et al. Cysteine-rich protein reverses weight loss in lung cancer patients receiving chemotherapy or radiotherapy. Antioxid Redox Signal. 2008;10(2):395–402. [DOI] [PubMed] [Google Scholar]
- 56.van der Meij BS, et al. Oral nutritional supplements containing (n-3) polyunsaturated fatty acids affect the nutritional status of patients with stage III non-small cell lung cancer during multimodality treatment. J Nutr. 2010;140(10):1774–80. [DOI] [PubMed] [Google Scholar]
- 57.van der Meij BS, et al. Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect quality of life and functional status in lung cancer patients during multimodality treatment: an RCT. Eur J Clin Nutr. 2012;66(3):399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murphy RA, Mourtzakis M, Chu QS, Baracos VE, Reiman T, Mazurak VC. Nutritional intervention with fish oil provides a benefit over standard of care for weight and skeletal muscle mass in patients with nonsmall cell lung cancer receiving chemotherapy. Cancer. 2011;117(8):1775–82. [DOI] [PubMed] [Google Scholar]
- 59.Sanchez-Lara K, et al. Effects of an oral nutritional supplement containing eicosapentaenoic acid on nutritional and clinical outcomes in patients with advanced non-small cell lung cancer: randomised trial. Clin Nutr. 2014;33(6):1017–23. [DOI] [PubMed] [Google Scholar]
- 60.Kiss N, Isenring E, Gough K, Wheeler G, Wirth A, Campbell BA, et al. Early and intensive dietary counseling in lung cancer patients receiving (chemo)radiotherapy-a pilot randomized controlled trial. Nutr Cancer. 2016;68(6):958–67. [DOI] [PubMed] [Google Scholar]
- 61.Leedo E, et al. The effect of a home delivery meal service of energy- and protein-rich meals on quality of life in malnourished outpatients suffering from lung cancer: a randomized controlled trial. Nutr Cancer. 2017;69(3):444–53. [DOI] [PubMed] [Google Scholar]
- 62.Tanaka N, Takeda K, Kawasaki Y, Yamane K, Teruya Y, Kodani M, et al. Early intensive nutrition intervention with dietary counseling and oral nutrition supplement prevents weight loss in patients with advanced lung cancer receiving chemotherapy: a clinical prospective study. Yonago Acta Med. 2018;61(4):204–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Taylor MA, et al. Longitudinal immune characterization of syngeneic tumor models to enable model selection for immune oncology drug discovery. J Immunother Cancer. 2019;7(1):328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ballaro R, Costelli P, Penna F. Animal models for cancer cachexia. Curr Opin Support Palliat Care. 2016;10(4):281–7. [DOI] [PubMed] [Google Scholar]
- 65.Goncalves MD, Hwang SK, Pauli C, Murphy CJ, Cheng Z, Hopkins BD, et al. Fenofibrate prevents skeletal muscle loss in mice with lung cancer. Proc Natl Acad Sci U S A. 2018;115(4):E743–e752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen JA, et al. Ghrelin prevents tumour- and cisplatin-induced muscle wasting: characterization of multiple mechanisms involved. J Cachexia Sarcopenia Muscle. 2015;6(2):132–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402(6762):656–60. [DOI] [PubMed] [Google Scholar]
- 68.Guillory B, Splenser A, Garcia J. Chapter Three - The Role of Ghrelin in Anorexia–Cachexia Syndromes. In: Litwack G, editor. Vitamins & Hormones: Academic Press; 2013. p. 61–106. [DOI] [PubMed] [Google Scholar]
- 69.•. Temel JS, et al. Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol. 2016;17(4):519–31 This is a large study evaluating the efficacy of a ghrelin agonist to treat cancer cachexia in NSCLC.
- 70.Currow D, Temel JS, Abernethy A, Milanowski J, Friend J, Fearon KC. ROMANA 3: a phase 3 safety extension study of anamorelin in advanced non-small-cell lung cancer (NSCLC) patients with cachexia. Ann Oncol. 2017;28(8):1949–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Crawford J, Prado CM, Johnston MA, Gralla RJ, Taylor RP, Hancock ML, et al. Study design and rationale for the phase 3 clinical development program of Enobosarm, a selective androgen receptor modulator, for the prevention and treatment of muscle wasting in cancer patients (POWER trials). Curr Oncol Rep. 2016;18(6):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Crawford J Clinical results in cachexia therapeutics. Curr Opin Clin Nutr Metab Care. 2016;19(3):199–204. [DOI] [PubMed] [Google Scholar]
- 73.•. Turner DC, et al. Pembrolizumab exposure-response assessments challenged by association of cancer cachexia and catabolic clearance. Clin Cancer Res. 2018;24(23):5841–9 This study evaluates the clearance of pembrolizumab in patients with weight loss and cancer cachexia.
- 74.Wang X, Feng Y, Bajaj G, Gupta M, Agrawal S, Yang A, et al. Quantitative characterization of the exposure-response relationship for cancer immunotherapy: a case study of nivolumab in patients with advanced melanoma. CPT Pharmacometrics Syst Pharmacol. 2017;6(1):40–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Feng Y, et al. Nivolumab exposure-response analyses of efficacy and safety in previously treated squamous or nonsquamous non-small cell lung cancer. Clin Cancer Res. 2017;23(18):5394–405. [DOI] [PubMed] [Google Scholar]
- 76.Bajaj G, Wang X, Agrawal S, Gupta M, Roy A, Feng Y. Model-based population pharmacokinetic analysis of nivolumab in patients with solid tumors. CPT Pharmacometrics Syst Pharmacol. 2017;6(1):58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Badawi M, Coss CC, Phelps MA. Letter to the editor: exposure-response or clearance-response relationship in immune checkpoint therapy?-a comment on ‘correlation between nivolumab exposure and treatment outcomes in non-small-cell lung cancer’ by Basak et al et al. Eur J Cancer. 2019;114:25–6. [DOI] [PubMed] [Google Scholar]
- 78.Bellesoeur A, Ollier E, Allard M, et al. Is there an exposure-response relationship for nivolumab in real-world NSCLC patients? Cancers (Basel). 2019;11(11). 10.3390/cancers11111784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li H, Yu J, Liu C, Liu J, Subramaniam S, Zhao H, et al. Time dependent pharmacokinetics of pembrolizumab in patients with solid tumor and its correlation with best overall response. J Pharmacokinet Pharmacodyn. 2017;44(5):403–14. [DOI] [PubMed] [Google Scholar]
- 80.Coss CC, Clinton SK, Phelps MA. Cachectic cancer patients: immune to checkpoint inhibitor therapy? Clin Cancer Res. 2018;24(23):5787–89. 10.1158/1078-0432.CCR-18-1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hurkmans DP, Basak EA, van Dijk T, Mercieca D, Schreurs MWJ, Wijkhuijs AJM, et al. A prospective cohort study on the pharmacokinetics of nivolumab in metastatic non-small cell lung cancer, melanoma, and renal cell cancer patients. J Immunother Cancer. 2019;7(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Loumaye A, Thissen JP. Biomarkers of cancer cachexia. Clin Biochem. 2017;50(18):1281–8. [DOI] [PubMed] [Google Scholar]
- 83.Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar L, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31(12):1539–47. [DOI] [PubMed] [Google Scholar]
- 84.Recio-Boiles A, Galeas JN, Goldwasser B, Sanchez K, Man LMW, Gentzler RD, et al. Enhancing evaluation of sarcopenia in patients with non-small cell lung cancer (NSCLC) by assessing skeletal muscle index (SMI) at the first lumbar (L1) level on routine chest computed tomography (CT). Support Care Cancer. 2018;26(7):2353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Antoun S, Rossoni C, Lanoy E. What’s next in using CT scans to better understand cachexia? Curr Opin Support Palliat Care. 2018;12(4):427–33. [DOI] [PubMed] [Google Scholar]
- 86.Nattenmuller J, et al. Prognostic impact of CT-quantified muscle and fat distribution before and after first-line-chemotherapy in lung cancer patients. PLoS One. 2017;12(1):e0169136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Potgens SA, et al. Klebsiella oxytoca expands in cancer cachexia and acts as a gut pathobiont contributing to intestinal dysfunction. Sci Rep. 2018;8(1):12321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bindels LB, Neyrinck AM, Salazar N, Taminiau B, Druart C, Muccioli GG, et al. Non digestible oligosaccharides modulate the gut microbiota to control the development of leukemia and associated cachexia in mice. PLoS One. 2015;10(6):e0131009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bindels LB, Neyrinck AM, Claus SP, le Roy CI, Grangette C, Pot B, et al. Synbiotic approach restores intestinal homeostasis and prolongs survival in leukaemic mice with cachexia. Isme J. 2016;10(6):1456–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372(21):2018–28. [DOI] [PubMed] [Google Scholar]
- 91.Mehnert JM, Monjazeb AM, Beerthuijzen JMT, Collyar D, Rubinstein L, Harris LN. The challenge for development of valuable immuno-oncology biomarkers. Clin Cancer Res. 2017;23(17):4970–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aguilar EG, Murphy WJ. Obesity induced T cell dysfunction and implications for cancer immunotherapy. Curr Opin Immunol. 2018;51:181–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang Z, et al. Paradoxical effects of obesity on T cell function during tumor progression and PD-1 checkpoint blockade. Nat Med. 2019;25(1):141–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lauby-Secretan B, et al. Body fatness and cancer–viewpoint of the IARC working group. N Engl J Med. 2016;375(8):794–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.•. Murphy WJ, Longo DL. The surprisingly positive association between obesity and cancer immunotherapy efficacy. Jama. 2019;321(13):1247–8 This study evalautes influence of obesity on immunotherapy responsiveness.