Abstract
Stressors associated with COVID-19 pandemic stay-at-home orders are associated with increased depression and anxiety and decreased physical activity. Given that physical activity and time spent outdoors in nature are associated with improved mental health, we examined the longitudinal association of these variables during the pandemic. Over 20,000 adults who participated in the U.S. Kaiser Permanente Research Bank, did not report COVID-19 symptoms, and responded to an online baseline and 3 follow-up surveys over approximately 3 months formed the cohort. Physical activity was assessed from a modified survey, time spent outdoors was assessed from one question, and anxiety and depression scores were assessed from validated instruments. Almost 60% were women, 82.8% were non-Hispanic white, and more than 93% of respondents were over the age of 50. Less in-person contact with friends and visiting crowded places was highly prevalent (>80%) initially and decreased somewhat (>70%). Participants in the lowest physical activity category (no physical activity) had the highest depression and anxiety scores compared to each successive physical activity category (p < 0.001). Spending less time outdoors was associated with higher depression and anxiety scores. This effect was greater for participants in the younger age categories compared with older age categories. The effect of less time spent outdoors on anxiety (p = 0.012) and depression (p < 0.001) scores was smaller for males than females. Results suggest that physical activity and time outdoors is associated with better mental health. People should be encouraged to continue physical activity participation during public health emergencies.
Keywords: COVID-19, Physical activity, Time outdoors, Depression, Anxiety, Older adults
1. Introduction
In March 2020, the coronavirus disease-2019 (COVID-19) pandemic wreaked havoc around the world with no known treatment, leaving public health officials to recommend reducing human interactions through stay-at-home policies and temporarily closing or altering business practices to suppress the virus's spread. Due to these and other COVID-19 related factors, the worldwide economy has deteriorated, with vast numbers of people furloughed or laid off from their work and concerned with meeting their financial obligations. These stressors, along with reduced ability to socialize with friends and family, increased symptoms of depression and anxiety in the general population, healthcare workers, and persons diagnosed with COVID-19 (Krishnamoorthy et al., 2020).
It is well-established that regular physical activity is associated with lower symptoms of depression and anxiety (2018 Physical Activity Guidelines Advisory Committee Scientific Report, 2018). Information is emerging that COVID-19 related social distancing influenced a person's ability to be physically active, which may contribute to negative mental health exacerbations. A number of cross-sectional studies noted declines in physical activity during the COVID-19 pandemic (Ammar et al., 2020; Lesser and Nienhuis, 2020; Violant-Holz et al., 2020; Maugeri et al., 2020; Wolf et al., 2021). A survey conducted among 1491 adults in Australia found almost half reported a decline in physical activity, which correlated with higher depression and anxiety symptoms (Stanton et al., 2020). Other studies across the globe have reported similar results (Violant-Holz et al., 2020; Maugeri et al., 2020; Wolf et al., 2021; Schuch et al., 2020; Duncan et al., 2020; Creese et al., 2020; Faulkner et al., 2021; Jacob et al., 2020; Haider et al., 2021). Reports are emerging in the U.S. population (Meyer et al., 2020; Callow et al., 2020; Cross et al., 2021), which has one of the highest burdens of COVID-19 cases, but are limited by cross-sectional design, small sample sizes, and an inability to examine effects by sociodemographic factors.
Time spent outdoors in nature may provide another benefit to mental health. Beyer and colleagues found that time spent outdoors was associated with lower levels of depression (Beyer et al., 2016). A Canadian study found that among inactive adults, spending more time outdoors during the COVID-19 pandemic was correlated with higher well-being (Lesser and Nienhuis, 2020) and a cross-sectional study from Austria found time spent outdoors during COVID-19 was associated with better mental health (Haider et al., 2021). The Centers for Disease Control and Prevention (CDC), promoting physical activity during the pandemic, included guidance for Americans to spend time in parks, trails, and open space to relieve stress, get fresh air, and stay active (Center for Disease Control and Prevention, 2021). Evaluating time spent in nature during the pandemic and its association with mental health symptoms using longitudinal data can provide additional evidence to support CDC recommendations.
Using survey responses from participants of the Kaiser Permanente Research Bank (KPRB), we conducted a longitudinal study of physical activity, time spent outdoors, and mental health characteristics in response to the “safer at home” orders that were imposed on U.S. residents. Over 125,000 completed a COVID-19 baseline survey and over 60,000 completed 3 follow-up surveys. For the purposes of this report and to be able to evaluate these associations among individuals without COVID-19 symptoms, we limited analyses to about 20,000 adults who completed the follow-up surveys and who also did not report COVID-19 symptoms.
2. Materials and methods
KP is a large, integrated health care system that serves approximately 12.5 million members across eight regions (Hawaii, Washington, Northwest [Oregon], Northern California, Southern California, Colorado, Mid-Atlantic States [Virginia, Maryland, District of Columbia], Georgia). Membership is generally similar to the regions' underlying insured population, although there is under-representation of people with very low and very high incomes (Koebnick et al., 2012). The KPRB is a collection of lifestyle surveys and biospecimens from over 350,000 KP members from the broader KP membership base who were invited and consented to participate in the KPRB. Prior to the COVID-19 pandemic, adult KP members were sent email invitations to consider participation in the KPRB.
Participation in the KPRB involves completing the consent form, filling out a baseline questionnaire, and providing a blood sample. The consent form gives permission to access the electronic medical record (EMR), clinically-collected specimens, future contact, as well as use of questionnaire data, DNA, and other blood components. The KPRB was approved by the institutional review board for the KP Mid-Atlantic States region, with oversight approval from all other KP regions.
In April 2020, we launched a series of COVID-19 surveys to 269,363 KPRB participants who were enrolled in a KP health plan as of that date and for whom we had current email information. Three surveys were created; all designed to be completed online in less than 10 min. The baseline survey included self-report of up to 12 COVID-19 symptoms since January 2020 and included symptoms such as fever, cough, headache, or fatigue. The survey also queried about work status, tobacco and marijuana use, and the number of people living in the household and their symptoms. Approximately every two weeks after completing the baseline survey, follow-up survey A or B was sent to the 129,385 participants who completed the baseline survey. Survey A included the same symptoms along with items related to social contacts at home and community settings, physical activity, anxiety, depression, and change in health behaviors and formed the basis of the present study. Survey B consisted of other questions not included in this analysis.
2.1. Participants
We included participants without common COVID-19 symptoms (fever, cough, shortness of breath, or loss of sense, smell, or taste during the previous 2 weeks) on the baseline or any of the survey A follow-ups. This eliminated potential confounding where physical activity might be reduced due to illness.
2.2. Independent variables
2.2.1. Physical activity
The survey included items similar to the Godin Leisure-Time Exercise Questionnaire (Godin and Shephard, 1985). Participants were asked to record the number of days and the average minutes per day of physical activity in mild, moderate, and vigorous exercise. Mild exercise was defined as walking fast enough to cause heart rate to increase somewhat. Moderate exercise was defined as sports or other physical activity, but not walking, that causes heart rate to increase somewhat. Vigorous exercise was defined as sports or other activity that caused a person to work up a sweat or heart rate to greatly increase. The number of days in each intensity category was grouped as none, 1–2 days, 3–4 days, 5–6 days, or every day. Minutes per day was categorized as 0–9 min, 10–19 min, 20–20 min, 30–59 min, or 60 min or more. The Godin Questionnaire differs from the survey used in that mild exercise is described as “minimal effort,” moderate activity as “not exhausting,” and strenuous exercise as “heart beats rapidly.” It also does not pre-categorize number of days or minutes per day of exercise.
A physical activity score was calculated. Because the instrument categorized number of days and number of minutes per day, the lowest number in each category was used for the score. The Godin Questionnaire intensity weightings of 3, 5, and 9 were used to weight mild, moderate, and vigorous exercise categories, respectively. Each intensity category was multiplied by number of days, minutes per day, and intensity weighting, with each category summed to create a total score. Possible scores ranged from 0 to 7140. Total physical activity scores were first separated into two groups: scores of 0, which indicate no physical activity, and scores greater than 0. Scores greater than 0 were further divided into quartiles for analysis.
2.2.2. Time spent outdoors in nature
A total of 10 single items about behavior, including the item time spent outdoors in nature, was queried. The question was adapted from the Environmental influences on Child Health Outcomes COVID-19 questionnaire. The original item queried “Which of the following behaviors have you changed because of the COVID-19 outbreak?” Because we planned to administer a longitudinal survey, we revised the item to: “Compared to a month ago, have you changed any of the following behaviors?” Response options were no change, I do this more often than I did a month ago, and I do this less often than I did a month ago.
2.3. Dependent variables
2.3.1. Depressive symptoms
The 2-item Patient Health Questionnaire (PHQ-2) was used to assess depressive symptoms. The 2 items query on the frequency of depressed mood and anhedonia symptoms. Response options are not at all, several days, more than half of the days, and nearly every day. Each item is scored as 0 to 3, with 3 corresponding to nearly every day. Scores from the 2 items are summed with possible scores of 0–6. The PHQ-2 is sensitive to a diagnosis of major depression determined by the Composite International Diagnostic Interview (CIDI); at a threshold of 2 the sensitivity is 0.86 and specificity is 0.78 (Arroll et al., 2010).
2.3.2. Anxiety symptoms
The 2-item Generalized Anxiety Disorder (GAD-2) assessed symptoms of anxiety. The two items are scored as 0–3 and summed for possible response options of 0–6. A systematic review found that compared with gold standard methods of diagnosing anxiety, by using a cut-off of 3, sensitivity was 0.76 and specificity 0.81 for identifying anxiety disorder (Plummer et al., 2016).
2.4. Covariates
Demographic data (age, sex, self-reported race/ethnicity) were derived from participants' EMR. Neighborhood education, determined from US Census block group in the participant's main residence, was used as an estimate of socioeconomic status. Height and weight were determined from self-report obtained from the COVID-19 survey. Body mass index (BMI; kg/m2) was calculated and values were categorized as Underweight (<18.5 kg/m2), Normal (18.5–24.9 kg/m2), Overweight (25.0–29.9 kg/m2), and Obese (≥30.0 kg/m2). Number of comorbidities, using the Charlson's comorbidity index (Charlson et al., 1987), was obtained from the EMR and coded as 0, 1, 2, 3+ comorbidities. KP region was included.
Race/ethnicity categories were collapsed into non-Hispanic white, Hispanic, Black, Asian, and Other/Unknown. Based on the distribution of the analytic cohort, age was initially categorized as less than 50 years and 50 years or older. We then divided the 50 and older age group into tertiles for analysis.
2.5. Analyses
We assessed the longitudinal associations between time spent outdoors and physical activity and continuous depression and anxiety scores by running two separate models for each outcome. Because responses were collected from each participant at multiple time points, we used linear mixed models with participants as a random effect to account for within-subject correlation. Models controlled for age, sex, race/ethnicity, Charlson's comorbidity index, BMI, neighborhood education, and KP region. To assess whether the association between the exposures and the outcomes differed by demographic factors, we tested two-way interactions between physical activity and time spent outdoors and race/ethnicity, sex, and age. Best model fit was based on the lowest Akaike information criteria (AIC). Results are presented as beta coefficients and 95% confidence intervals. For figures, we calculated predicted outcomes for each exposure of interest, setting adjustment covariates to the reference category.
Missing outcome measures at any time point were handled through maximum likelihood estimation under the assumption of missing at random. Because missing data were rare, we ran complete-case analyses where participants with missing covariate or exposure data were excluded from the model. To measure the validity of our complete-case analysis, we imputed missing values through multiple imputation using m = 5 imputations. We assessed the pooled parameter estimates after multiple imputation and noted only minor differences from the estimates from the complete-case analysis (Supplemental Table 1). All analyses were performed using R version 4.0.4, packages lme4 v1.1.26 and mice v3.13.0 (R Code Team. R, 2021; van Buuren, 2011; Bates et al., 2015).
Human Subjects: The KPRB was approved by the institutional review board for protection of human subjects for the KP Mid-Atlantic States region, with oversight approval from all other KP regions.
3. Results
A total of 20,012 participants met study inclusion criteria and comprised the analytic cohort. The average date of the first follow-up survey completion was May 3, 2020 (range April 29 – June 1), the second was June 4, 2020 (range June 2 – June 30), and the third was July 2, 2020 (range June 29 – August 16).
Almost 60% were women, 82.8% were non-Hispanic white, and more than 93% of respondents were over the age of 50 years (Table 1 ).
Table 1.
Participant characteristics of N = 20,012 respondents of the Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020.
| Characteristic | Frequency | Percent |
|---|---|---|
| Female, percent | 11,936 | 59.6 |
| Race/ethnicity | ||
| Non-Hispanic white | 16,577 | 82.8 |
| Asian | 1136 | 5.7 |
| Hispanic | 1064 | 5.3 |
| Black | 452 | 2.3 |
| Other/unknown | 783 | 3.9 |
| Age categories | ||
| Less than 50 years | 1345 | 6.7 |
| Age 50–66 years | 5919 | 29.6 |
| Age 67–73 years | 6357 | 31.8 |
| Age 74+ | 6391 | 31.9 |
| Employment status | ||
| Employed, full or part time | 6168 | 30.8 |
| Job designated as essential service | 1653 | 8.3 |
| Moved to remote work | 2625 | 13.3 |
| Retired | 13,621 | 68.1 |
| Other | 315 | 1.6 |
| Neighborhood education | ||
| 0–25% high school or higher | 67 | 0.3 |
| 26–50% high school or higher | 1332 | 6.7 |
| 51–75% high school or higher | 8489 | 42.5 |
| Over 75% high school or higher | 10,089 | 50.1 |
A total of 68.1% of respondents were retired, although 89.2% of respondents less than age 50 years reported full-time or part-time employment. Half (50.1%) lived in neighborhoods in which over 75% of residents had at least a high school education. The demographics are similar to the 60,577 respondents who were excluded because they reported a COVID-19 symptom (Supplemental Table 2).
Participants reported reducing their activities due to the safer at home guidelines (Table 2 ). In May 2020, 86.4% reported less in-person contact with friends, 83.1% reported visiting crowded places less often, and 81.6% reported visiting public places less often. The prevalence of doing less of these activities decreased: in June 79.3% reported fewer in-person contacts with friends, 78.2% reported visiting of crowded places less, and 74.4% reported visiting public places less. By July, the prevalences were even lower: 71.8%, 73.0%, and 68.3%, respectively.
Table 2.
Frequencies and percentages of isolation behaviors, physical activity score, time spent outdoors in nature, and depression and anxiety scores of respondents of the Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020. Sample sizes ranged from 18,707 to 19,9 due to missing values.
| Time 1 |
Time 2 |
Time 3 |
|
|---|---|---|---|
| May 2020 | June 2020 | July 2020 | |
| Reporting doing less in the past month due to COVID-19, n, % | |||
| In-person contact with friends | 17,289 (86.4) | 15,875 (79.4) | 14,354 (71.8) |
| In-person contact with family outside of home | 14,549 (72.7) | 12,623 (63.1) | 11,201 (56.0) |
| Visiting public places | 16,318 (81.6) | 14,880 (74.4) | 13,662 (68.3) |
| Visiting crowded places | 16,621 (83.1) | 15,633 (78.2) | 14,591 (73.0) |
| In person event in the community, including religious events | 14,304 (71.5) | 12,574 (62.9) | 11,086 (55.4) |
| Traveling in state | 14,249 (71.2) | 12,526 (62.6) | 10,815 (54.1) |
| In-person contact with co-workers (non-retired persons only n = 6380) | 4590 (71.9) | 3925 (61.5) | 3384 (53.1) |
| Physical activity category, n, % | |||
| None (0) | 2160 (10.9) | 2281 (11.6) | 2481 (12.6) |
| 1 (mean score 112, SD 71.4) | 4074 (20.6) | 4203 (21.3) | 4203 (21.4) |
| 2 (mean score 403, SD 98.2) | 4678 (23.7) | 4652 (23.6) | 4554 (23.2) |
| 3 (mean score 829, SD 177.2) | 4474 (22.7) | 4365 (22.2) | 4290 (21.8) |
| 4 (mean score 2027, SD 997.0) | 4359 (22.1) | 4198 (21.3) | 4137 (21.0) |
| Total physical activity score, mean (SD) | 754 (874.7) | 739 (881.2) | 734 (885.2) |
| Time spent outdoors in nature, n, % | |||
| No change | 10,173 (51.0) | 12,589 (63.1) | 14,167 (71.0) |
| More often than a month ago | 4143 (20.8) | 3766 (18.9) | 3277 (16.4) |
| Less often than a month ago | 5614 (28.2) | 3603 (18.1) | 2498 (12.5) |
| Depression score, mean (SD) | 0.63 (1.1) | 0.64 (1.1) | 0.58 (1.0) |
| Meets criteria for depression, n, % | 3614 (18.1) | 3761 (18.9) | 3455 (17.3) |
| Anxiety score, mean (SD) | 0.58 (1.1) | 0.59 (1.1) | 0.52 (1.0) |
| Meets criteria for anxiety, n, % | 1028 (5.2) | 1004 (5.0) | 780 (3.9) |
The total physical activity mean score decreased minimally over the follow-up periods from May to July 2020 (Table 2). The total physical activity score ranged from 754.0 ± 874.7 at time 1 to 733.7 ± 885.2 at time 3. At all three time points between 10.9% and 12.6% reported no activity.
After covariate adjustment, anxiety and depression scores were significantly higher in follow-up time 1 (May) and time 2 (June) compared with time 3 (July) (Table 3 ). Based on the PHQ-2 criterion cut-points of major depression symptoms, over time 18.1%, 18.9%, and 17.3%, respectively, met the criteria. Using the GAD-2 threshold for anxiety disorder, 5.2%, 5.0%, and 3.9% met the criteria from May to July.
Table 3.
Beta estimates and 95% confidence intervals for covariates included in the mixed effect linear regression model assessing physical activity category, time spent outdoors in nature, and depression and anxiety scores among 20,012 participants of the Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020. Models also controlled for BMI, Charlson's comorbidity index, neighborhood education, and KP region.
| Predictors | Depression score |
Anxiety score |
||
|---|---|---|---|---|
| Estimates (95% CI) | p-value | Estimates (95% CI) | p-value | |
| Intercept | 0.66 (0.61, 0.71) | <0.001 | 0.50 (0.46, 0.55) | <0.001 |
| Follow-up visit #1 vs. follow-up visit #3 | 0.02 (0.01, 0.03) | <0.001 | 0.04 (0.03, 0.06) | <0.001 |
| Follow-up visit #2 vs. follow-up visit #3 | 0.05 (0.04, 0.06) | <0.001 | 0.07 (0.05, 0.08) | <0.001 |
| Age < 50 years vs. 74–99 years | 0.43 (0.37, 0.49) | <0.001 | 0.65 (0.59, 0.71) | <0.001 |
| Age 50–66 years vs. 74–99 years | 0.16 (0.13, 0.20) | <0.001 | 0.27 (0.23, 0.30) | <0.001 |
| Age 67–73 years vs. 74–99 years | 0.09 (0.05, 0.12) | <0.001 | 0.12 (0.09, 0.16) | <0.001 |
| Asian vs. white | −0.23 (−0.29, −0.18) | <0.001 | −0.23 (−0.28, −0.17) | <0.001 |
| Black or African American vs. white | −0.21 (−0.30, −0.12) | <0.001 | −0.15 (−0.23, −0.07) | <0.001 |
| Hispanic vs. white | −0.12 (−0.18, −0.07) | <0.001 | −0.05 (−0.11, 0.00) | 0.07 |
| Other/unknown vs. white | 0.04 (−0.03, 0.11) | 0.24 | 0.02 (−0.05, 0.08) | 0.60 |
| Males vs. females | −0.21 (−0.24, −0.18) | <0.001 | −0.25 (−0.28, −0.23) | <0.001 |
| PA score 1st quartile vs. PA score 0 | −0.06 (−0.09, −0.04) | <0.001 | −0.02 (−0.05, 0.00) | 0.07 |
| PA score 2nd quartile vs. PA score 0 | −0.14 (−0.17, −0.11) | <0.001 | −0.05 (−0.08, −0.02) | <0.001 |
| PA score 3rd quartile vs. PA score 0 | −0.18 (−0.21, −0.15) | <0.001 | −0.07 (−0.10, −0.04) | <0.001 |
| PA score 4th quartile vs. PA score 0 | −0.20 (−0.23, −0.17) | <0.001 | −0.09 (−0.12, −0.06) | <0.001 |
| Time outdoors: Less often vs. no change | 0.18 (0.15, 0.22) | <0.001 | 0.11 (0.08, 0.15) | <0.001 |
| Time outdoors: More often vs. no change | 0.03 (−0.01, 0.07) | 0.17 | 0.04 (0.01, 0.08) | 0.02 |
| Time outdoors: Less often × age < 50 years | 0.10 (0.03, 0.17) | 0.01 | 0.16 (0.09, 0.24) | <0.001 |
| Time outdoors: Less often × age 50–66 years | 0.05 (0.00, 0.10) | 0.03 | 0.05 (0.00, 0.09) | 0.05 |
| Time outdoors: Less often × age 67–73 years | 0.04 (−0.01, 0.08) | 0.14 | 0.06 (0.01, 0.10) | 0.01 |
| Time outdoors: More often × age < 50 years | −0.03 (−0.10, 0.05) | 0.44 | 0.04 (−0.03, 0.11) | 0.31 |
| Time outdoors: More often × age 50–66 years | 0.01 (−0.04, 0.05) | 0.80 | 0.03 (−0.02, 0.07) | 0.28 |
| Time outdoors: More often × age 67–73 years | −0.00 (−0.05, 0.04) | 0.87 | −0.01 (−0.06, 0.04) | 0.68 |
| Time outdoors: Less often × males | −0.07 (−0.11, −0.03) | <0.001 | −0.05 (−0.08, −0.01) | 0.01 |
| Time outdoors: More often × males | 0.02(−0.02, 0.06) | 0.41 | −0.01 (−0.05, 0.03) | 0.67 |
Bold indicates the differences are statistically significant at the designated p value.
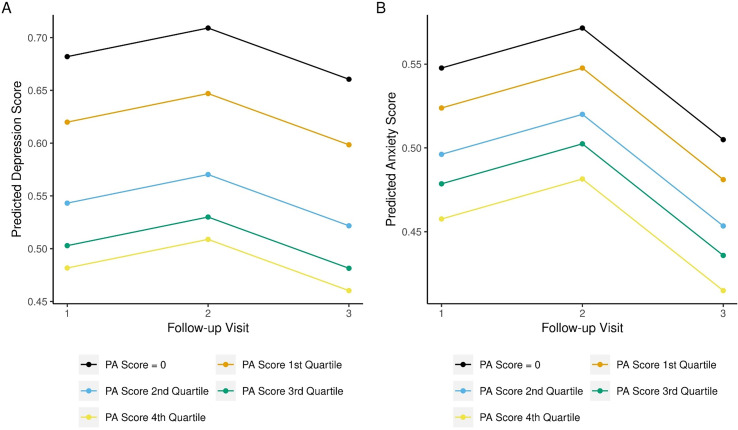
Participants in the lowest physical activity category (no reported physical activity) had the highest depression and anxiety scores compared to each successive physical activity category across follow-up, as shown in Fig. 1 . Table 3 displays the beta coefficient and its corresponding 95% confidence interval (CI). Each higher physical activity category had lower depression and anxiety scores, evidenced by the negative beta coefficient (Table 3). We did not detect any interaction between physical activity and demographic factors.
Fig. 1.
Fully adjusted model of (A) depression and (B) anxiety scores by physical activity category. All covariates in each model were set to the reference category.
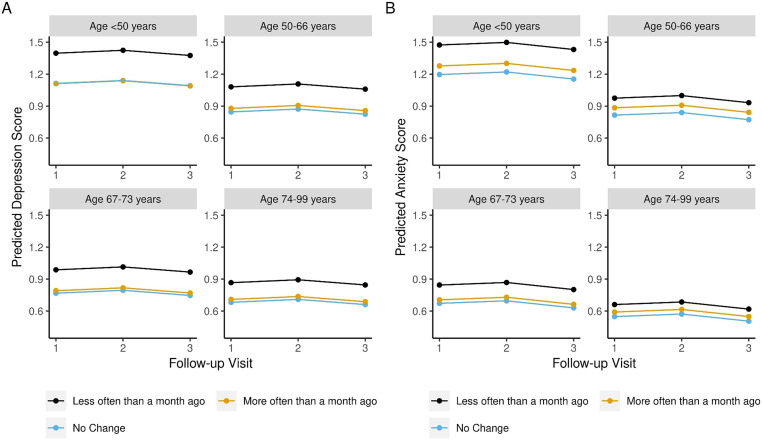
Compared with respondents reporting no change in the prior month spending time outdoors in nature, participants reporting less time spent outdoors had higher depression and anxiety scores (Table 3). We found significant interactions between time spent outdoors and age and sex (Table 3). Spending less time outdoors was associated with higher depression and anxiety scores more for those in the less than 50 years (β = 0.10, 95% CI: 0.03, 0.17; β = 0.16, 95% CI: 0.09, 0.24) and the 50–66 (β = 0.05, 95% CI: 0.00, 0.10; β = 0.10, 95% CI: 0.05, 0.09) age categories than for participants in the older age categories.
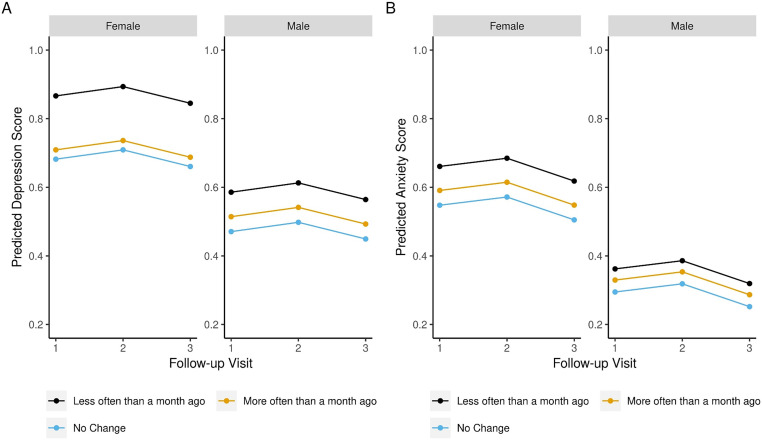
Fig. 2 displays this trend for both depression and anxiety scores. The effect of less time spent outdoors on depression (β = −0.07, 95% CI: −0.11, −0.03) and anxiety (β = −0.05, 95% CI: −0.08, −0.01) scores was smaller for males than for females (Table 3, Fig. 3 ). Participants reporting increasing their time outdoors had higher anxiety scores than respondents reporting no change in time spent outdoors in nature, and this was consistent across demographic groups.
Fig. 2.
Fully adjusted model of (A) depression and (B) anxiety scores by time spent outdoors and age categories. All covariates in each model were set to the reference category.
Fig. 3.
Fully adjusted model of (A) depression and (B) anxiety scores by time spent outdoors and sex. All covariates in each model were set to the reference category.
4. Discussion
Among this cohort reporting no COVID-19 symptoms, which consisted mostly of older, retired, white women and who mostly adhered to the “safer at home” orders during May to July 2020, anxiety and depression scores decreased over time. Scores were higher for females and the younger age categories and lower for Asian and Black people compared with white respondents. Controlling for covariates, participants reporting no physical activity had higher depression and anxiety scores than participants in the higher physical activity categories. During the COVID-19 pandemic, well-known associations among physical activity and anxiety and depression remained and were consistent over a longitudinal period of approximately 3 months.
The associations between time spent outdoors in nature and depression and anxiety scores were more complex. Less time spent outdoors was associated with higher depression and anxiety scores compared with no change. However, increasing one's time spent outdoors was also associated with higher anxiety scores. Patterns differed by age and sex, in which the trends were stronger for the younger age categories and less strong for men. We do not have baseline prevalence of time spent outdoors in nature, making these results difficult to interpret.
Our longitudinal results indicate that, even during the COVID-19 lockdown, more physical activity was associated with lower symptoms of depression and anxiety. This is consistent with cross-sectional data from the U.K. (Jacob et al., 2020) and others (Lesser and Nienhuis, 2020; Wolf et al., 2021; Faulkner et al., 2021; Haider et al., 2021; Callow et al., 2020). Rather than evaluating cross-sectional associations, we were able to test these associations in a longitudinal manner. People should be encouraged to continue physical activity participation during this and other public health emergencies to benefit their mental as well as physical health.
It is well-known that exposure to nature enhances well-being (Bowler et al., 2010). Early in the pandemic in in the spring/summer 2020 when our data collection occurred, many jurisdictions closed parks, trails, beaches, and other nature venues. If individuals were spending less time outdoors than usual either because they were adhering to the safer at home orders or the nature locations they typically visited were closed, poorer mental health may have resulted. A cross-sectional study found that respondents who reported feeling deprived to nature exposure because of the pandemic also reported less flourishing (i.e., happiness, mental and physical health, life purpose) (Tomasso et al., 2021). Even though our study had a longitudinal design, because we did not have baseline assessments of depression, anxiety, or prevalence of adults who spent time outdoors, we can only report associations. Nonetheless, for adults who enjoy time in nature and find it associated with improved mental health, it is reasonable to expect lower mental well-being if deprived of this outlet. Policies for future public health emergencies that require isolation should carefully weigh the risks of and benefits of restricting people from experiencing nature.
We found interactions between spending less time in nature and poorer mental health, in which the association was greater for the younger age groups. Tomasso and colleagues also found younger ages had worse outcomes associated with nature deprivation than older adults (Tomasso et al., 2021). Those in the younger age groups in our study were more likely to be in the workforce, which may be particularly stressful during a pandemic. The combination of spending less time in nature and working, perhaps in a home environment, may have contributed to poorer mental health for younger respondents.
Depression and anxiety scores were lower across higher age categories. It has been opined that those more vulnerable to adverse effects from contracting COVID-19, including the elderly, are at risk for adverse psychosocial outcomes (Pfefferbaum and North, 2020; Vahia et al., 2020). However, other studies have reported results similar to ours (Stanton et al., 2020; Klaiber et al., 2021; Pieh et al., 2020), including U.S. adults (Czeisler et al., 2020). Gambin et al. reported that younger age groups (18–29, 30–44) reported higher levels of depressive and generalized anxiety symptoms than older age groups (45–59, 60–85) among adults living in Poland (Gambin et al., 2021). Age distribution of our cohort skewed to the right, so we were able to detect differences in mental health scores across more granular age categories than Gambin and colleagues. Our oldest age group had the lowest anxiety and depression score, which included over 6000 adults over the age of 74 years. Lind et al. used a life story approach that highlights how older adults have greater capacity to “take the long view” and put the current pandemic into a reflection of their life history and other adversities they have faced compared with younger adults (Lind et al., 2021). There has also been speculation that this apparent resilience with regard to negative mental health outcomes may result from wisdom that is gained with aging (Vahia et al., 2020).
We found that depression and anxiety decreased over the 3-month follow-up period and was consistent for all demographic subgoups. In a German cohort over roughly the same time period (April to June 2020) as our study, Mata et al. also noted a decline in anxiety and depression (Mata et al., 2021). We do not know what may explain these results, although it is possible that respondents were adapting to the lockdown. Mata et al. hypothesized habituation to stay at home orders would result in improved mental health symptoms (Mata et al., 2021). We noted that prevalence of lockdown behaviors decreased somewhat over these months, which may have improved the respondents' mental health outlook.
Women exhibit higher levels of depression and anxiety than men (Altemus et al., 2014), and others have reported this trend continuing during the pandemic (Duncan et al., 2020; Creese et al., 2020). Among Chinese adults assessed with the GAD-2 and PHQ-2 during COVID-19, women reported higher levels of anxiety but no sex differences were noted for depression (Hou et al., 2020). Stanton et al. did not find differences in depression, anxiety, or stress between males and females among Australian adults during COVID-19 (Stanton et al., 2020). The different results across studies could relate to their being conducted across countries that were experiencing the pandemic at different periods of time and differing severity.
We are aware of only one study that examined mental health outcomes during the pandemic by different race/ethnicities. The CDC reported higher prevalence of anxiety or depressive symptoms among Hispanic survey respondents than for Black, Asian, and white respondents and lower symptoms among Asian compared with white adults (Czeisler et al., 2020). Our results indicating lower mental health scores among Asian people compared with white participants correspond to the CDC results, but, in contrast, we also found that Black adults and Hispanic adults had lower scores compared with white people. The difference in the sex and age distributions across cohorts may explain the results.
The study had limitations. KP members are insured and located in distinct regions and not generalizable to the entire US population. Participants in the KPRB are not generalizable to the underlying KP membership due to low responses to invitations to participate. Those responding to the COVID-19 surveys were a small subset of KPRB participants and were likely to be women, older adults, and live in highly educated neighborhoods than the general KP membership base and that of the US population. Thus, our results may not generalizable beyond the study cohort. We did not have pre-COVID-19 assessments of physical activity, time spent outdoors in nature, depression, or anxiety scores. The physical activity measure, while similar to the Godin Leisure Survey, was not a validated survey. Moreover, walking was categorized as a mild intensity activity and intensity may have been underestimated. The scoring of the survey resulted in a score, rather than actual or estimated energy expenditure, disallowing us to quantify physical activity. The item assessing time spent outdoors in nature was general and did not provide a definition of nature and there was no reference point for the response options. Job loss, unpaid work, and the responsibility of caring/teaching children not in school that occurred during the pandemic lockdown may have contributed to anxiety and depression. This analysis did not cover the entire period of the lockdown and behaviors may have changed with longer follow-up. However, there also were strengths. A large cohort with regional diversity was followed over 3 months during the early phase of the pandemic. The assessments of anxiety and depression are well-validated.
5. Conclusion
Higher physical activity was associated with lower anxiety and depression scores over approximately 3 months during the initial lockdown period of the COVID-19 pandemic. People should be encouraged to continue physical activity participation during this and other public health emergencies to benefit their mental and physical health. Outdoor opportunities for physical activity, including parks and other nature venues, should remain open for use during future pandemics.
The following are the supplementary data related to this article.
Beta estimates and 95% confidence intervals for covariates included in the mixed effect linear regression model in the complete case model assessing physical activity category, time spent outdoors in nature, and depression and anxiety scores among 20,012 participants of the Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020. Models also controlled for BMI, Charlson's comorbidity index, neighborhood education, and KP region.
Participant characteristics of N = 20,012 respondents completing three consecutive COVID-19 surveys and reporting no symptoms compared with N = 60,577 respondents completing three consecutive COVID-19 surveys and reporting at least one COVID-19 symptom. The Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020.
Funding
The Kaiser Permanente Research Bank provided funding for this work. No author has any possible, perceived, or real financial conflicts of interest.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank Dr. Andrea Burnett-Hartmann for leading the development of the COVID-19 surveys. We acknowledge the contribution of participants in the Kaiser Permanente Research Bank for their willingness to share their personal health information.
References
- 2018 Physical Activity Guidelines Advisory Committee Scientific Report. 2018. https://health.gov/paguidelines/second-edition/report/ (Accessed December 4, 2018)
- Altemus M., Sarvaiya N., Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammar A., Brach M., Trabelsi K., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6) doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arroll B., Goodyear-Smith F., Crengle S., et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Fam. Med. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D.M.M., Bolker B., Walker S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015;67(1):1–68. [Google Scholar]
- Beyer K.M., Szabo A., Nattinger A.B. Time spent outdoors, depressive symptoms, and variation by race and ethnicity. Am. J. Prev. Med. 2016;51(3):281–290. doi: 10.1016/j.amepre.2016.05.004. [DOI] [PubMed] [Google Scholar]
- Bowler D.E., Buyung-Ali L.M., Knight T.M., Pullin A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health. 2010;10:456. doi: 10.1186/1471-2458-10-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callow D.D., Arnold-Nedimala N.A., Jordan L.S., et al. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am. J. Geriatr. Psychiatry. 2020;28(10):1046–1057. doi: 10.1016/j.jagp.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention Visiting Parks and Recreational Facilities. 2021. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/visitors.html (Accessed April 14, 2021)
- Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Creese B., Khan Z., Henley W., et al. Loneliness, physical activity, and mental health during COVID-19: a longitudinal analysis of depression and anxiety in adults over the age of 50 between 2015 and. Int. Psychogeriatr. 2020;2020:1–10. doi: 10.1017/S1041610220004135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross T.J., Isautier J.M.J., Morris S.J., Johnson B.D., Wheatley-Guy C.M., Taylor B.J. The influence of social distancing behaviors and psychosocial factors on physical activity during the COVID-19 pandemic: cross-sectional survey study. JMIR Public Health Surveill. 2021;7(9) doi: 10.2196/31278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.E., Lane R.I., Petrosky E., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan G.E., Avery A.R., Seto E., Tsang S. Perceived change in physical activity levels and mental health during COVID-19: findings among adult twin pairs. PLoS One. 2020;15(8) doi: 10.1371/journal.pone.0237695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner J., O’Brien W.J., McGrane B., et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: a multi-country cross-sectional analysis. J. Sci. Med. Sport. 2021;24(4):320–326. doi: 10.1016/j.jsams.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambin M., Sekowski M., Wozniak-Prus M., et al. Generalized anxiety and depressive symptoms in various age groups during the COVID-19 lockdown in Poland. Specific predictors and differences in symptoms severity. Compr Psychiatry. 2021;105:152222. doi: 10.1016/j.comppsych.2020.152222. [DOI] [PubMed] [Google Scholar]
- Godin G., Shephard R.J. A simple method to assess exercise behavior in the community. CanJ ApplSport Sci. 1985;10(3):141–146. [PubMed] [Google Scholar]
- Haider S., Smith L., Markovic L., et al. Associations between physical activity, sitting time, and time spent outdoors with mental health during the First COVID-19 lock down in Austria. International Journal of Environmental Research and Public Health. 2021;18(17) doi: 10.3390/ijerph18179168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou F., Bi F., Jiao R., Luo D., Song K. Gender differences of depression and anxiety among social media users during the COVID-19 outbreak in China:a cross-sectional study. BMC Public Health. 2020;20(1):1648. doi: 10.1186/s12889-020-09738-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob L., Tully M.A., Barnett Y., et al. The relationship between physical activity and mental health in a sample of the UK public: a cross-sectional study during the implementation of COVID-19 social distancing measures. Ment. Health Phys. Act. 2020;19:100345. doi: 10.1016/j.mhpa.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaiber P., Wen J.H., DeLongis A., Sin N.L. The ups and downs of daily life during COVID-19: age differences in affect, stress, and positive events. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e30–e37. doi: 10.1093/geronb/gbaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koebnick C., Langer-Gould A.M., Gould M.K., et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. The Permanente journal. 2012;16(3):37–41. doi: 10.7812/tpp/12-031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy Y., Nagarajan R., Saya G.K., Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293:113382. doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesser I.A., Nienhuis C.P. The impact of COVID-19 on physical activity behavior and well-being of Canadians. International journal of environmental research and public health. 2020;17(11) doi: 10.3390/ijerph17113899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind M., Bluck S., McAdams D.P. More vulnerable? The life story approach highlights older people’s potential for strength during the pandemic. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e45–e48. doi: 10.1093/geronb/gbaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mata J., Wenz A., Rettig T., et al. Health behaviors and mental health during the COVID-19 pandemic: a longitudinal population-based survey in Germany. Soc. Sci. Med. 2021;287:114333. doi: 10.1016/j.socscimed.2021.114333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maugeri G., Castrogiovanni P., Battaglia G., et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 2020;6(6) doi: 10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J., McDowell C., Lansing J., et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. International journal of environmental research and public health. 2020;17(18) doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- R Code Team. R A Language and Environment for Statistical Computing. 2021. https://www.R-project.org (Accessed April 23, 2021)
- Schuch F.B., Bulzing R.A., Meyer J., et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: a cross-sectional survey in Brazil. Psychiatry Res. 2020;292:113339. doi: 10.1016/j.psychres.2020.113339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R., To QG, Khalesi S., et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. International journal of environmental research and public health. 2020;17(11) doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasso L.P., Yin J., Cedeno Laurent J.G., Chen J.T., Catalano P.J., Spengler J.D. The Relationship between Nature Deprivation and Individual Wellbeing across Urban Gradients under COVID-19. International journal of environmental research and public health. 2021;18(4) doi: 10.3390/ijerph18041511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahia I.V., Jeste D.V., Reynolds C.F. 3rd. Older adults and the mental health effects of COVID-19. Jama. 2020;324(22):2253–2254. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- van Buuren S.G.-O.K. mice: Multivariate imputation by chained equations in R. Journal of Statistical Software. 2011;45:1–67. [Google Scholar]
- Violant-Holz V., Gallego-Jimenez M.G., Gonzalez-Gonzalez C.S., et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. International journal of environmental research and public health. 2020;17(24) doi: 10.3390/ijerph17249419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf S., Seiffer B., Zeibig J.M., et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. 2021;51(8):1771–1783. doi: 10.1007/s40279-021-01468-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Beta estimates and 95% confidence intervals for covariates included in the mixed effect linear regression model in the complete case model assessing physical activity category, time spent outdoors in nature, and depression and anxiety scores among 20,012 participants of the Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020. Models also controlled for BMI, Charlson's comorbidity index, neighborhood education, and KP region.
Participant characteristics of N = 20,012 respondents completing three consecutive COVID-19 surveys and reporting no symptoms compared with N = 60,577 respondents completing three consecutive COVID-19 surveys and reporting at least one COVID-19 symptom. The Kaiser Permanente Research Bank COVID-19 survey, U.S. adults, 2020.