Abstract
Introduction
Smooth muscle tumours of uncertain malignant potential (STUMP) are mesenchymal uterine tumours with a malignant potential found somewhere between that of benign leiomyomas and leiomyosarcomas. Only three cases of STUMP pulmonary metastasis exist in the literature.
Case presentation
We report the case of a 63 year-old female patient presenting with dysphonia secondary to recurrent laryngeal nerve paralysis due to an enormous mediastinal STUMP metastasis, 14 years after having undergone a total hysterectomy with bilateral salpingo-oophorectomy. A successful left pneumonectomy was performed and the mass weighing 1570 g was histologically confirmed as a STUMP metastasis.
Discussion
Only three cases of pulmonary metastasis from STUMP have been reported in the recent literature and no robust information exists about the metastatic nature of STUMP. No cases exist in the literature of a successful pneumonectomy performed for a STUMP metastasis of such large dimensions presenting after many years from the diagnosis of the primary uterine lesion. Physicians should keep in mind that the finding of a smooth muscle tumour in the lung of a woman should promptly raise the suspicion of a metastatic uterine malignancy, even several years after diagnosis of the primary lesion.
Conclusion
Despite the size, invasiveness and late presentation of the STUMP metastasis, the surgery was successful and the patient no longer requires oxygen therapy.
Keywords: Lung, Metastasis, Leiomyoma, Leiomyosarcoma, STUMP
Highlights
-
•
Smooth muscle tumours of uncertain malignant potential (STUMP) are mesenchymal uterine tumours with malignant potential.
-
•
Pulmonary metastasis from STUMP is very rare, with only 3 cases found in the recent literature.
-
•
These tumours have a malignant potential somewhere between that of benign leiomyomas and leiomyosarcomas.
-
•
Smooth muscle tumours may metastasize several years after removal of the primary uterine lesion.
1. Introduction
Smooth muscle tumours of uncertain malignant potential (STUMP) are mesenchymal uterine tumours with a malignant potential found somewhere between that of benign leiomyomas and leiomyosarcomas [1]. Only three cases of STUMP pulmonary metastasis exist in the literature. More common yet still rare are uterine leiomyosarcoma lung metastasis, in which lung metastases usually occur within 2 years of the initial diagnosis with some studies reporting 75% of metastasis within 5 years [2]. Benign leiomyoma metastasis was first described by Steiner in 1939 and has since been a subject of controversy as these tumours are complex and difficult to classify [3], [4]. In general, very little is known about the clinicopathological details and outcomes of benign metastasizing leiomyomas, but they are thought to be clinically benign [5]. According to the World Health Organization classification, a uterine smooth muscle tumour that cannot be classified as benign or malignant should be termed smooth muscle tumour of uncertain malignant potential (STUMP) [6].
We report the case of a 63-year-old woman who presented with an enormous mass displacing the mediastinum and occupying most of the left thoracic cavity, who underwent a salvage left pneumonectomy which revealed a diagnosis of metastatic STUMP, 14 years after radical hysterectomy and salpingo-oophorectomy.
This case report was drafted and submitted according to the SCARE guidelines [7].
2. Case presentation
A 63-year-old Caucasian woman was referred to our unit for the incidental finding of a large mass of the mediastinum and left lung after being admitted to our Otorhinolaryngology ward for dysphonia secondary to recurrent laryngeal nerve paralysis. Computed tomography (CT) scan of the head and neck revealed an 18 cm × 11 cm mass of the mediastinum that appeared to infiltrate the hilum and left upper lobe of the lung. Apart from the vocal cord paralysis she had no other signs or symptoms. Her medical history included mixed anxiety-depressive disorder, phacoemulsification of the left eye 2 years prior for cataract and a radical hysterectomy and salpingo-oophorectomy for a STUMP 14 years prior. She had a smoking history of 45 pack years and continued to smoke up until the surgery. She reported no prior drug use and her family medical history was unremarkable.
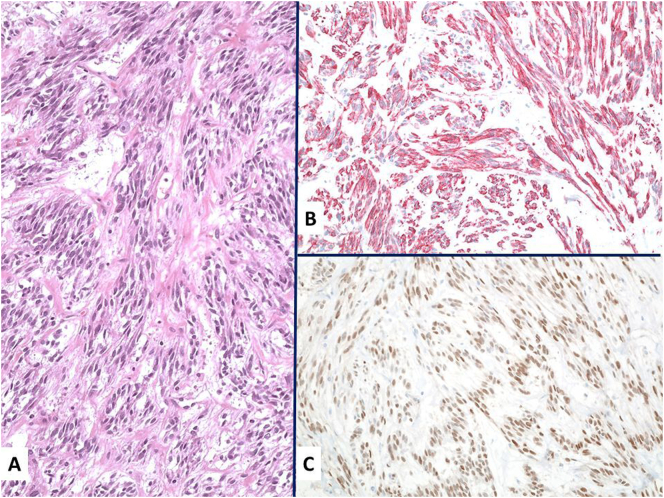
The patient underwent a total-body CT scan with contrast medium which revealed an extensive vascularized solid formation of mediastinal origin that extended to the left hemithorax and occupied the entire left upper lobe (Fig. 1). A fluorodeoxyglucose (FDG)-positron emission tomography (PET)-CT scan revealed radiotracer accumulation of the mass of the mediastinum and left upper lobe (SUVmax 6.4). Pulmonary function tests were performed and were on the limit of operability. FVC was 0.89 L (30%), FEV1 was 0.69 L (28%), DLCO 12 L (50%), DLCO/VA 2.19 L (41%). The patient then underwent a lung perfusion scintigraphy which revealed a 98% distribution of the right lung and a 2% distribution of the left lung. A CT-guided transthoracic needle biopsy was inconclusive. During the patient workup she developed acute respiratory distress syndrome (ARDS) requiring oxygen therapy and it was decided to perform a salvage pneumonectomy via a clamshell incision with standard double-lumen endobronchial intubation. The surgery was performed by a thoracic surgeon with over 25 years of experience performing major lung resections and lung transplants, in an academic hospital. The procedure was complicated by the enormous size of the mass, weighing 1570 g and measuring 19 × 16 × 5 cm in size, which also infiltrated the left main pulmonary artery (Fig. 2). Grossly, the mass revealed a whitish cut surface and a tense-elastic consistency. The center of the mass contained necrotic areas and a peripheral capsule was observed. The final histological report revealed a malignant mesenchymal neoplasm with a mitotic index of 2 mitoses × 10 HPF with a labelling index with Ki67 around 10–15%. At immunohistochemistry, the neoplastic cells expressed smooth-muscle actin, desmin and oestrogen receptors, whereas pan-cytokeratins (clone AE1/AE3), S100, CD34, STAT6, melan-A and HMB45 were entirely negative (Fig. 3). The neoplasm invaded the parietal pleura and lung parenchyma. A diagnosis of mesenchymal neoplasm with smooth muscle differentiation with malignant characteristics (in relation to size, areas of necrosis and the proliferative index) compatible with a low-grade leiomyosarcoma was made. Finally, the morphologic and immunohistochemical comparison with the previous smooth muscle neoplasm of the uterus lead to a definitive diagnosis of pulmonary metastasis of STUMP. The postoperative stay was complicated by anemia which required several packed red blood cells and plasma transfusions as well as the need for oxygen therapy for the first 10 postoperative days. The patient was discharged after 18 days and did not require oxygen therapy at discharge. At the 1, 3 and 6 month follow ups the patient was in good condition and did not require oxygen therapy. The patient was referred for an oncological evaluation where it was decided to perform a strict follow up without adjuvant therapy.
Fig. 1.
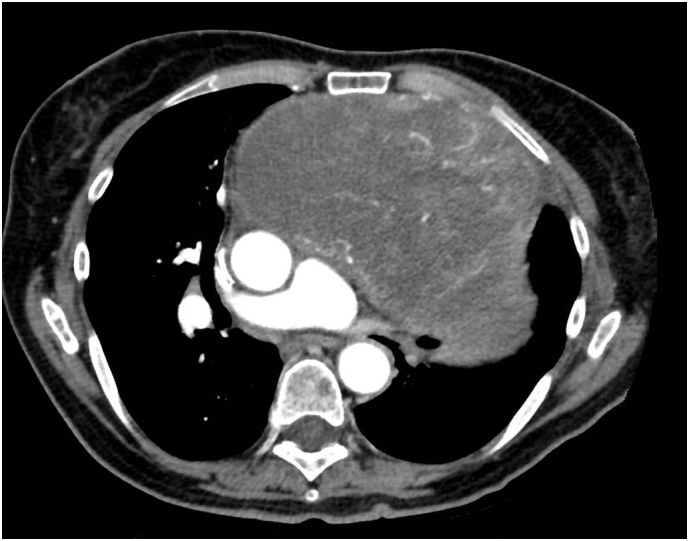
Chest-CT scan with contrast medium revealing an extensive vascularized solid formation of mediastinal origin that extended to the left hemithorax and occupied the entire left upper lobe.
Fig. 2.

The left lung with the left upper lobe completely infiltrated by the tumour. The tumour weighed 1570 g and was 19 × 16 × 5 cm in size.
Fig. 3.
At histology, the tumour consisted of a spindle cell proliferation with mild cell atypia and fibrous stroma (A, hematoxylin-eosin × 180). The tumour cells expressed smooth muscle actin (B, immunohistochemistry × 180) and oestrogen receptors (C, immunohistochemistry × 180).
3. Discussion
Pulmonary metastasis from STUMP is very rare, with only 3 cases found in the recent literature. The first case of lung metastasis from “primary uterine myoma” was described by Steiner in 1939 [3] and the term STUMP was first used in the literature by Kempson in 1973 [8]. By definition, STUMP tumours cannot be classified as completely benign or malignant neoplasms and a detailed histopathological and immunohistochemical examination should be carried out to confirm the diagnosis of this rare group of uterine tumours [1]. No robust information exists about the metastatic nature of STUMP, and we can only speculate that they spread via hematogenous dissemination as is the case with uterine leiomyosarcomas.
The correct management of patients with metastasizing leiomyoma is a complete surgical resection [9]. Unfortunately, the preoperative biopsy was non diagnostic and it was decided to perform a pneumonectomy to improve the patient's chances of survival. The enormous size of the mass and the fact that the patient only presented with vocal cord paralysis demonstrates how lung cancer can remain asymptomatic until the tumour is in a very advanced stage. To the best of our knowledge, no other cases exist in the literature of a successful pneumonectomy performed for a STUMP metastasis of such large dimensions presenting after many years from the diagnosis of the primary uterine lesion. Of the 3 cases reported in the literature, the pulmonary lesions were small and multiple in nature, while our patient presented with a mass that occupied the entire left thoracic cavity. In one case the lesions were bilateral. Surgery was performed in 2 of the cases and in the other case chemotherapy was the treatment of choice. Two of the cases presented 3 years after hysterectomy and the third case presented after 9 years [1], [4], [6].
The mass weighed 1570 g and a clamshell incision was performed in order to mobilize the lung and the mediastinal mass as well as to perform an intrapericardial isolation and ligation of the pulmonary artery. Initially, the patients pulmonary function tests were not satisfactory for a pneumonectomy, but lung perfusion scintigraphy demonstrated that the left lung had already been completely excluded by the neoplastic mass and the predicted postoperative lung function was sufficient to perform the surgery.
At histology, several tumour entities may enter in differential diagnosis, such as perivascular epithelioid cell tumour (PEComa), monophasic synovial sarcoma (MSS), solitary fibrous tumour (SFT) and spindle cell epithelial tumours (e.g., peripheral carcinoids, sarcomatoid carcinoma) [10].
PEComa shows a marked female predominance and nearly all show immunoreactivity for both smooth muscle (actin and/or desmin) and melanocytic (HMB-45 and/or melan-A) markers. MSS shows a higher and denser cellularity with frequent mitoses and atypia coupled to patchy expression of cytokeratins and negative staining with muscle markers and oestrogens. SFT is characterized by a heterogeneous spindle cell proliferation expressing CD34 and STA6, alternating hypo- and hypercellular areas with collagen-rich stroma and hemangiopericytoma-like vessels. Negative staining with pan-cytokeratins ruled out conventional pulmonary epithelial tumours [11].
Pathologists and physicians should keep in mind that the finding of a smooth muscle tumour in the lung of a woman should promptly raise the suspicion of a metastatic leiomyoma/leiomyosarcoma, even if a previous hysterectomy was performed several years before the finding of a pulmonary lesion. Thus, a meticulous past medical history and comparison of the original uterine tumour with the current lung lesion is the cornerstone in reaching a correct diagnosis. Due to the invasive nature of the surgical procedure the patient had a lengthy hospital stay, but the patient did not require oxygen therapy and returned to a normal life after surgery. At the multidisciplinary meeting, apart from a clinic-radiologic follow-up, no adjuvant therapy was proposed in light of the lack of standardized treatment in these rare cases and a radical margin-free surgery.
4. Conclusion
Pulmonary metastases from STUMP are extremely rare. Our case was also characterized by an unreported long interval of time between hysterectomy and diagnosis of the lung metastasis. Despite the gravity of the patient's situation in terms of tumour size and invasiveness, the surgery was successful and she no longer requires oxygen therapy.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
None required.
Funding
No funding used.
Guarantor
Beatrice Aramini MD PhD, Prof. Franco Stella MD PhD.
Research registration number
N/A.
CRediT authorship contribution statement
Angelo Paolo Ciarrocchi: conceptualization, writing - original draft, writing - review & editing, investigation; Beatrice Aramini: supervision, project administration, investigation; Stefano Sanna: validation, investigation; Giulio Rossi: writing - original draft, investigation; Desideria Argnani: investigation, supervision; Franco Stella: supervision, project administration, resources.
Declaration of competing interest
None to declare.
References
- 1.Kotsopoulos I.C., Barbetakis N., Asteriou C., Voutsas M.G. Uterine smooth muscle tumor of uncertain malignant potential: a rare cause of multiple pulmonary nodules. Indian J. Med. Paediatr. Oncol. 2012 Jul;33(3):176–178. doi: 10.4103/0971-5851.103148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pautier P., Genestie C., Rey A., Morice P., Roche B., Lhommé C., Haie-Meder C., Duvillard P. Analysis of clinicopathologic prognostic factors for 157 uterine sarcomas and evaluation of a grading score validated for soft tissue sarcoma. Cancer. 2000 Mar 15;88(6):1425–1431. [PubMed] [Google Scholar]
- 3.Steiner P.E. Metastasizing fibroleiomyoma of the uterus: report of a case and review of the literature. Am. J. Pathol. 1939 Jan;15(1):89–110. 7. [PMC free article] [PubMed] [Google Scholar]
- 4.Esch M., Teschner M., Braesen J.H. Pulmonary metastases of a uterine smooth muscle tumour with undefined malignancy potential. Geburtshilfe Frauenheilkd. 2014 Mar;74(3):288–292. doi: 10.1055/s-0034-1368182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng J.S., Han A., Chew S.H., Low J. A clinicopathologic study of uterine smooth muscle tumours of uncertain malignant potential (STUMP) Ann. Acad. Med. Singap. 2010 Aug;39(8):625–628. [PubMed] [Google Scholar]
- 6.Ip P.P., Cheung A.N., Clement P.B. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): a clinicopathologic analysis of 16 cases. Am. J. Surg. Pathol. 2009 Jul;33(7):992–1005. doi: 10.1097/PAS.0b013e3181a02d1c. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Kempson R.L. In: The Uterus. Norris H.J., Hertig A.T., Abell M.R., editors. Williams & Wilkins; Baltimore: 1973. Sarcomas and related neoplasms. [Google Scholar]
- 9.Won H.S., Chun H.G., Lee K. Retroperitoneal smooth muscle tumor of uncertain malignant potential after hysterectomy: a case report. J. Med. Case Rep. 2011 May;28(5):214. doi: 10.1186/1752-1947-5-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dey B., Srinivas B.H., Badhe B., Nachiappa Ganesh R., Gochhait D., Toi P.C., Jinkala S. Malignant epithelioid soft tissue tumours- a Pathologist's perspective with review of literature. Cureus. 2020;12(12) doi: 10.7759/cureus.12263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hornick J.L., Fletcher C.D. PEComa: what do we know so far? Histopathology. 2006 Jan;48(1):75–82. doi: 10.1111/j.1365-2559.2005.02316.x. [DOI] [PubMed] [Google Scholar]