Abstract
Objectives
Acute Aortic dissection (AAD) may present as out-of-hospital cardiac arrest (OHCA). However, the incidence of this presentation is not well known. Our aim was to perform a systematic review and meta-analysis of all observational studies reporting on the incidence of AAD in patients with OHCA.
Methods
We searched MEDLINE, CENTRAL, PsycInfo, Web of Science Core Collection and OpenGrey databases from inception to March-2021, for observational studies reporting on the incidence of AAD in patients with OHCA. Data was pooled using a random-effects model of proportions. The primary outcome was the incidence of AAD in OHCA patients. Secondary outcomes were the incidence of type A aortic dissections (TAAD) and type B aortic dissections (TBAD) in OHCA patients, overall mortality following AAD-OHCA and risk of death in AAD-OHCA patients compared to risk of death of non-AAD-OHCA patients.
Results
Fourteen studies were included. The pooled calculated incidence of OHCA due to AAD was 4.39% (95 %CI: 2.55; 6.8). Incidence of OHCA due to TAAD was 7.18% (95 %CI: 5.61; 8.93) and incidence of OHCA due to TBAD was 0.47% (95 %CI: 0.18; 0.85). Overall mortality following OHCA due to AAD was 100% (95 %CI: 97.62; 100). The risk of death in AAD-OHCA patients compared with non-AAD-OHCA patients was 1.10 (95 %CI: 0.94; 1.30).
Conclusion
AAD as a cause of OHCA is more frequent than previously thought. Prognosis is dire, as it is invariably lethal. These findings should lead to a higher awareness of AAD when approaching a patient with OHCA and to future studies on this matter.
Keywords: Aortic dissection, Out-of-hospital cardiac arrest, Incidence, Systematic review, Meta-analysis
1. Introduction
Acute Aortic dissection (AAD) is a serious and potentially life-threatening condition, that usually occurs without any warning signs [1]. Current literature on this topic describes mainly patients who are stable enough to progress either to surgery or to an intensive care unit (ICU) [1]. However, a significant number of patients with AAD experience out-of-hospital cardiac arrest (OHCA) and most of them do not survive the event. Up to this point, there are few studies on AAD patients presenting as OHCA, with its epidemiology and patient characteristics remaining mostly unknown [2]. Recent studies have suggested that its incidence is higher than previously reported [3], [4]..
Diagnosing AAD as a cause of OHCA poses a clinical challenge due to several reasons. Typical clinical presentation is not present in most cases, oftentimes resembling other relevant causes of OHCA [2]. Some patients who experience AAD share similar characteristics (male sex, age > 40, hypertension) with myocardial infarction (MI) patients, the leading cause of OHCA [1]. Additionally, some patients are declared dead before they arrive at the hospital, with no definitive diagnosis being made [5]. Even those who survive transport to the hospital are usually too unstable to perform a confirmatory diagnostic procedure, such as a CT-angiography [1]. For these reasons, diagnosis of AAD as a cause of OHCA is often missed [2] and its incidence is not clear [4].
Greater insight in this subject becomes increasingly important, in order to assist with clinical decision-making. While the prognosis of AAD as a cause of OHCA is currently dire [6], only the comprehensive knowledge of its incidence can lead to successful clinical pathways in the management of these patients.
The aim of this study was to perform a systematic review and meta-analysis of observational studies reporting on the incidence of AAD in patients presenting with OHCA.
2. Methods
2.1. Protocol and registration
The review followed and complied with the PRISMA [7] and MOOSE guidelines [8] and has been registered in the PROSPERO database (CRD42021228950).
2.2. Eligibility criteria
Observational studies describing the incidence of AAD in patients with OHCA were included. Any type of aortic dissection was accepted. We accepted studies based on “out-of-hospital cardiac arrest” patient samples using cross-sectional, case control, or cohort studies, studies based on administrative, and studies based on autopsy information if they provide incidence estimates of AAD at institutional, multi-institutional or national/sub-national level. There was no date, publication type or language restrictions. Papers were excluded if they reported on the same population at the same time-period (in order not to duplicate events), if specific and independent information was not given regarding aortic dissections, if the population considered was not exclusive regarding OHCA, except if we could extract the data specific to OHCA patients alone. We excluded studies who focused only on pediatric patients. If studies included both children and young adults, they were included. We excluded patients with sudden death if data on OHCA patients was not provided or autopsy reports not related to OHCA patients. If studies reported on convenience samples, they were excluded from the primary analysis and included in the sensitivity analysis to lower the risk of referral bias, for example.
2.3. Information sources and search methods
We searched MEDLINE, CENTRAL, PsycInfo, Web of Science Core Collection and OpenGrey databases from inception to March 2021. Specialists were consulted and references were cross-checked for potential additional studies.
The search strategy is detailed in the supplementary data (Supplementary data 1). The yielded search results were cross checked, and the duplicates eliminated.
2.4. Study selection, data collection process and synthesis
Two reviewers (RGM;CM) independently screened the titles and abstracts yielded by the search, with disagreements resolved through consensus or by a third reviewer (DC) serving as final arbitrator. The full reports for all references that appeared to meet the inclusion criteria or where there was any uncertainty were obtained. Three reviewers (RGM;CM;MA) independently read full text reports and determined whether these met the inclusion criteria, with disagreements being resolved through consensus or by a fourth reviewer (DC) serving as final arbitrator. Additional information was requested from study authors, when needed, to resolve questions about eligibility. Motives for exclusion were registered. References were cross-checked to look for further appropriate studies and an expert was consulted to add any relevant study not previously included.
Three reviewers (RGM;CM;MA) individually extracted study data onto a pre-piloted form and uploaded into a sheet following confirmation of agreement of the data.
The data extracted included: study publication data (authors, journal/year of publication); study design; settings; inclusion and exclusion criteria; participant demographics; number of participants; case definition of OHCA and AAD; methods of obtaining the data and outcome results.
AAD and sub-type definition were used according to the defined in each study, except for traumatic aortic dissections which were not included. We considered OHCA as defined in each study, however for the purpose of this study we only included patients with intrinsic causes of OHCA, and thus excluded patients who had an arrest due to extrinsic causes, such as trauma, drowning, drug overdose or suicide attempt [9].
The primary outcome was the incidence of patients who developed OHCA due to AAD. Incidence of AAD in OHCA patients was calculated using the number of AAD as the numerator and the total number of OHCA patients (excluding extrinsic causes) as the denominator during the study length.
The secondary outcomes were the estimates of the incidence of different types of AAD (TAAD and TBAD) in patients with OHCA, overall mortality following OHCA and difference in mortality in patients with OHCA due to AAD compared to OHCA due to other intrinsic causes. Furthermore, sensitivity analysis was performed analyzing differences among the age subset of patients (studies of children and young adults versus adult only), study designs (autopsy, registries using imaging or purely clinically driven diagnosis), geographic regions, year of publication and risk of bias (ROB).
2.5. Risk of bias
We used the tool developed by Hoy et al. [10] to assess for ROB analyzing both external and internal validity (supplementary data 2).
Two authors (RGM and CM) independently assessed every included paper. The overall ROB for each study was divided as high or low risk, with high risk being those studies in which at least two items were assessed at a high ROB, or three or more items had a rating of unclear.
“Small study effect” was assessed through Egger test in addition to visual inspection of funnel plot asymmetry. Leave-one-out meta-analysis was also performed.
2.6. Statistical analysis
Quantitative analysis was performed when appropriate using STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC) to perform meta-analysis and derive forest plots.
The results yielded by the data extraction were expressed in frequency. The incidence data was directly extracted from the paper and defined as the number of AAD as the numerator and the total number of OHCA patients (excluding extrinsic causes) as the denominator, according to the following formula:
The data was subjected to Freeman-Tukey transformation (double-arcsine transformation) to avoid negative incidence in the confidence interval(CI), limiting the CI among 0–100% [11]. A random-effects model was used to pool the data to account for the heterogeneity of the included studies such as the difference in designs [12]. Statistical heterogeneity was assessed using I2.13
Sensitivity analysis was performed regarding study designs (registries, autopsy studies, studies using CT for diagnosis), age of the patients analyzed, date of publication, geographical area (divided by continent) and according to ROB assessment.
3. Results
3.1. Included studies
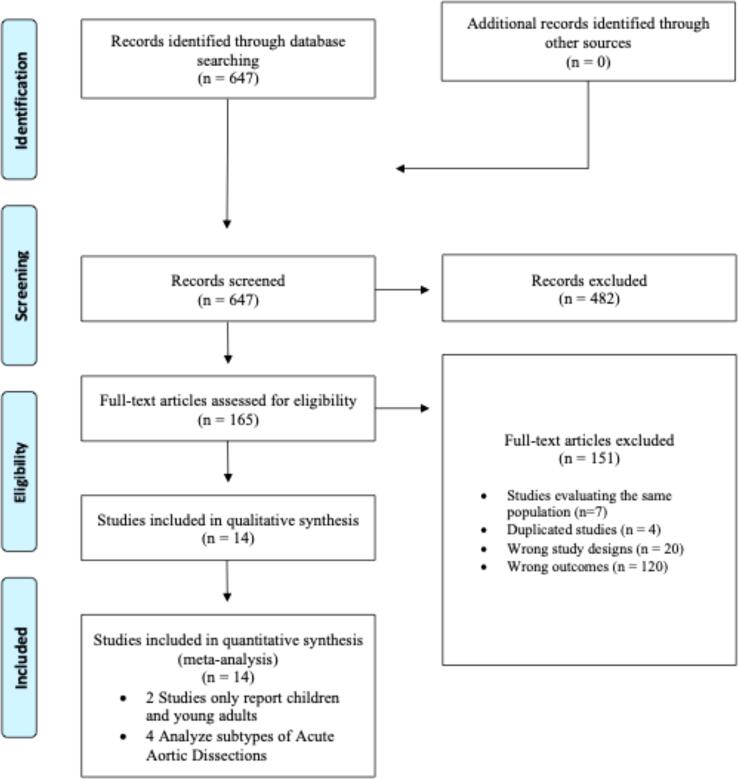
The electronic database yielded 647 articles. After title/abstract review, 165 papers were evaluated in full text. Of these, 14 [3], [4], [6], [9], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23] were included in the qualitative and quantitative synthesis (Fig. 1). Out the 14 studies, 2 studies only analyzed children and young adults [15], [21], and only 4 studies analyzed sub-types of AAD [4], [6], [16], [8]. The reasons for exclusion of the remaining 151 papers are detailed in Fig. 1.
Fig. 1.
PRISMA flow diagram.
3.2. Study characteristics and demographic data
Study details and extracted data from the paper are detailed in Table 1, Table 2, respectively. Studies reported data from 1972 to 2019, with publications ranging from 2006 to 2020. Overall, 538 OHCAs occurred due to AADs in a total of 9475 OHCA due to intrinsic causes. Nine studies reported on Asian cohorts (7 from Japan, 1 Taiwan and 1 South Korea) [6], [9], [16], [17], [18], [20], [22], [23], 2 studies reported on European cohorts (Germany and Czech Republic)[11], [13] and 3 other studies were from the American continent (2 from USA and 1 from Canada) [15], [19], [21].
Table 1.
Study characteristics.
| Author (year) | Geographic location (country/city or county) | Year(s) of inclusion | Study design and data retrieval methods | Data collecting method for AAD cases | Patients reported | Age -mean (SD) | Male sex (%) |
|---|---|---|---|---|---|---|---|
| Adler et al (2018) | Cologne, Germany | 2014–2017 | Cohort study, retrospective, single-center | Clinical analysis, angiography, CT Scan | Patients > 18 year-old) | 54,7 (15) | 82.9 |
| Allan et al (2017) | Toronto, Canada | 2009–2012 | Cohort study, population-based, retrospective, multicenter (Rescu Epistry Cardiac Arrest Database) | Hospital records and coroner investigative statement and autopsy reports | Patients aged 2–45 years old | 35 (9.3) | 70.3 |
| Pleskot et al (2006) | East Bohemia, Czech Republic | 2002–2004 | Cohort study, prospective, multi-center | Autopsy findings, clinical course and complementary examinations | Patients aged between 16 and 97 | 66 (13) | 74,1 |
| Jitsuiki et al (2017) | Izunokuni, Shizuoka, Japan | 2012–2017 | Cohort study, retrospective, single-center | CT Scan | Patients > 10 years old | NR | NR |
| Kim et al (2020) | Wonju, South Korea | 2002–2005 | Cohort study, retrospective, single-center | Transesophageal echocardiogram (convenience sample) | Patients > 20 years old | Median (IQR):71(21) | 57.8 |
| Moriwaki et al (2013) | Yokohama, Japan | 2002–2005 and 2007–2010 | Case series study, population-based, retrospective, single-center | Clinical records and perimortem CT | NR | NR | NR |
| Takeuchi et al (2020) | Kyorin, Tokyo, Japan | 1972–1998 | Cohort study, retrospective, single-center | CT-Scan | Patients > 17 years old | NR | NR |
| Tanaka et al (2016) | Sapporo, Japan | 2002–2014 | Cohort study, retrospective, single-center | CT and Perimortem CT | NR | NR | NR |
| Tseng et al (2020) | San Francisco, California, USA | 2002–2014 | Cohort study, prospective, multi-center (All consecutive San Francisco County out of hospital cardiac arrest deaths) | Autopsy | Patients aged 18–90 years old | 62.8 (14.5) | 69 |
| Yang et al (2020) | Taiwan | 2006–2019 | Cohort study, retrospective, single-center | CT Scan (first clinical evaluation after ECPR) | ECMO patients > 18 years old | 54.7 (12.2) | 90.3 |
| Meyer et al (2012) | King County, Washington, USA | 1980–2009 | Cohort study, retrospective, population-based, multi-center | Origin was determined from all available information, including emergency medical services incident reports, autopsy reports, death certificates, and hospital records when available, and a specific cause of OHCA was determined for each case | Patients aged 0–35 years old | 25.1 (10.1) | 70.6 |
| Otani et al (2017) | Osaka, Japan | 2009–2016 | Cohort study, retrospective, single-center | Clinical findings | Patients 16 years old | NR | NR |
| Yoshida et al (2016) | Kanto Region, Japan | 2012–2012 | Cohort study, retrospective, multi-center (prospectively collected data from the SOS-Kanto Registry study) | Clinical records | Patients > 17 years old | NR | NR |
| Kobayashi et al (2013) | Chiba, Japan | 2006–2011 | Cohort study, retrospective, single-center | Clinical records among patients with precise diagnosis of OHCA | Patients > 14 | NR | NR |
Legend: Study characteristics. AAD: acute aortic dissection; TBAD: type B aortic Dissection; TAAD (type A aortic dissection); CT: Computer Tomography; NR: Not Reported; USA: United States of America.
Table 2.
Aortic Dissection Patients Characteristics.
| Author (year) | Number of OHCA due to AAD | Number of OHCA due to TAAD | Number of OHCA due to TBAD | Number of OHCA | Mean age (SD) of AAD patients | Mean age (SD) of non-AAD patients | Sex (%male) of AAD patients | Sex (% male) of non-AAD patients | Survival rate (AAD/ non-AAD OHCA) |
|---|---|---|---|---|---|---|---|---|---|
| Adler et al (2018) | 1 | NR | NR | 70 | NR | NR | NR | NR | NR / NR |
| Allan et al (2017) | 13 | NR | NR | 971 | NR | NR | NR | NR | NR / NR |
| Pleskot et al (2006) | 7 | NR | NR | 560 | NR | NR | NR | NR | NR / NR |
| Jitsuiki et al (2017) | 44 | 41 | 3 | 455 | NR | NR | NR | NR | 0% / 3.9% |
| Kim et al (2020) | 10 | 5 | 5 | 45 | 75(70–75) | 69(58–81) | 50.0 | 60 | 0 / 8,6% |
| Moriwaki et al (2013) | 149 | NR | NR | 1303 | NR | NR | NR | NR | NR / NR |
| Takeuchi et al (2020) | 71 | 66 | 5 | 934 | 78 (8) | NR | 34.8 | NR | 4.2% / NR |
| Tanaka et al (2016) | 27 | 26 | 1 | 456 | 77 (13) | NR | 70 | NR | 11.1% / 34.7% |
| Tseng et al (2020) | 14 | NR | NR | 525 | NR | NR | NR | NR | NR / NR |
| Yang et al (2020) | 7 | NR | NR | 93 | NR | NR | NR | NR | NR / NR |
| Meyer et al (2012) | 2 | NR | NR | 314 | NR | NR | NR | NR | 0% / 29,5% |
| Otani et al (2017) | 118 | NR | NR | 1375 | NR | NR | NR | NR | NR / NR |
| Yoshida et al (2016) | 71 | NR | NR | 2253 | NR | NR | NR | NR | 0% / NR |
| Kobyashi et al (2013) | 4 | NR | NR | 121 | NR | NR | NR | NR | 0% /47.1% |
Legend: Study characteristics. AAD: acute aortic dissection; TBAD: type B aortic Dissection; TAAD (type A aortic dissection); CT: Computer Tomography; NR: Not Reported; USA: United States of America.
Study design and data collection method varied, ranging from review of medical records, autopsy charts, transesophageal echocardiography, emergency CT-scan, postmortem CT-scans and death certificates (Table 1).
Only 4 studies gave independent data on types of aortic dissection [4], [6], [16], [18]. One study [6] performed a comparative analysis of patients who developed OHCA due to acute aortic dissections (AAD- OHCA) with non-AAD OHCA patients and found no significant differences between both groups. Another study [16] performed a similar comparison but also included rupture of aortic aneurysms in the comparative arm alongside aortic dissections. In this study, patients with OHCA due to aortic disease tended to be female and to have a pulseless electric activity (PEA) as the initial rhythm, a higher rate of emersion to PEA during resuscitation and higher mortality.
Specific data on AAD-OHCA patients mortality was only present in 7 studies [4], [6], [9], [16], [18], [21], [23]. The majority of studies analyzed adult patients (10 studies), however, two studies analyzed both children and young adults [15], [21].
3.3. Risk of bias
Eleven studies were considered to have a high ROB (supplementary data 3). Three studies [15], [20], [21] had a high risk of selection bias due to only including children and young adults [15], [21] or due to a specific population (ECMO patients) [20].
The gold standard for diagnosis of aortic dissection is a CT-angiography, with transesophageal echocardiogram also having high sensitivity and specificity. Seeing as only 5 studies [4], [6], [16], [18], [20] used these diagnostic modalities in every patient, a high ROB regarding the accuracy of the diagnosis was present in the remainder of patients (except for the Tseng et al. study [19] which performed confirmatory autopsies in all patients). In the Kim et al. study [6], the authors report a convenience sample of OHCA patients who did not regain spontaneous circulation after prolonged CPR and underwent TEE during standard CPR in the emergency department (ED). Due to this study design, a high probability of referral bias needs to be accounted for. For this reason, this study [6] was excluded from the primary outcome analysis and included in the sensitivity analysis.
Publication bias analysis regarding small study effect was analyzed using the Egger test, which was non-significant (p = 0.66) – Supplementary data 4. Leave-one-out meta-analysis did not show a significant difference in the overall pooled result (maximum variation found was 0.49% when the Moriwaki et al. study [17] was excluded).
4. Primary outcome
4.1. Overall incidence of AAD in OHCA patients
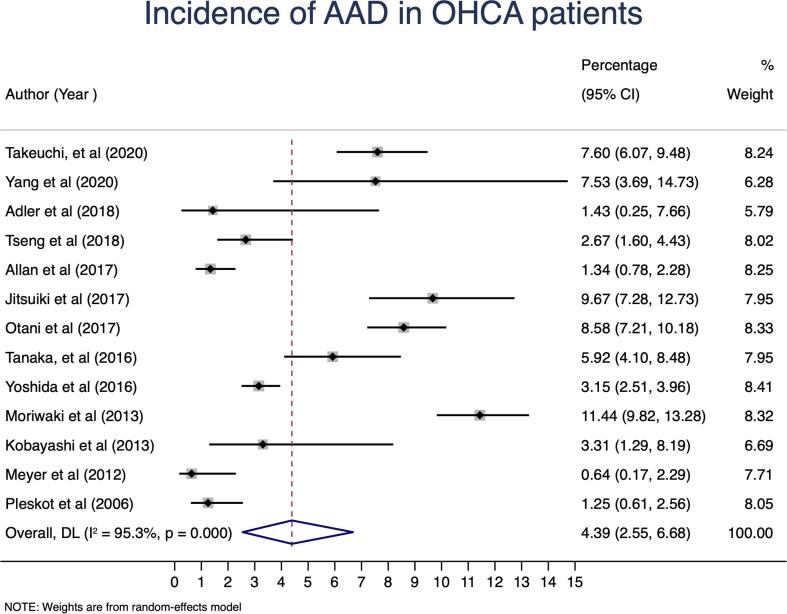
The pooled calculated incidence of OHCA due to AAD was 4.39% (95 %CI: 2.55; 6.8; I2 = 95%; 528 AAD/ 9430 intrinsic OHCA patients; 13 studies [3], [4], [9], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23])–Fig. 2.
Fig. 2.
Pooled incidence of acute aortic dissection (AAD) in patients with out-of-hospital cardiac arrest (OHCA) in observational studies. Data is expressed as the percentage of OHCA due to AAD, with respective 95% confidence interval (CI). Result: 4.39% (95% CI: 2.55; 6.8; I2 95%).
5. Secondary outcomes
5.1. Overall incidence of TAAD and TBAD in OHCA patients
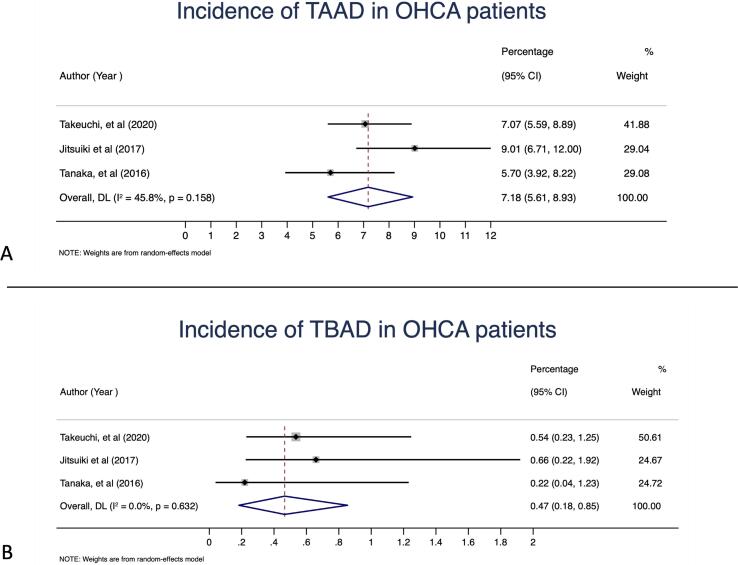
The pooled calculated incidence of OHCA due to TAAD was 7.18% (95 %CI: 5.61; 8.93; I2 = 46%; 133 TAAD/ 1845 intrinsic OHCA patients; 3 studies [4], [16], [18])–Fig. 3A. The pooled calculated incidence of OHCA due to TBAD was 0.47% (95 %CI: 0.18; 0.85; I2 = 0%; 9 TBAD/ 1845 intrinsic OHCA patients; 3 studies [4], [16], [18])–Fig. 3B.
Fig. 3.
A: Incidence of type A acute aortic dissection (TAAD) in patients with out-of-hospital cardiac arrest (OHCA). Data is expressed as the percentage of OHCA due to TAAD with respective 95% confidence interval (CI). Result: 7.18% (95% CI: 5.61; 8.93; I2 46%). B: Incidence of type B acute aortic dissection (TBAD) in patients with OHCA. Data is expressed as the percentage of OHCA due to TBAD, with respective 95% confidence interval (CI). Result: 0.47% (95% CI: 0.18; 0.85; I2 0%).
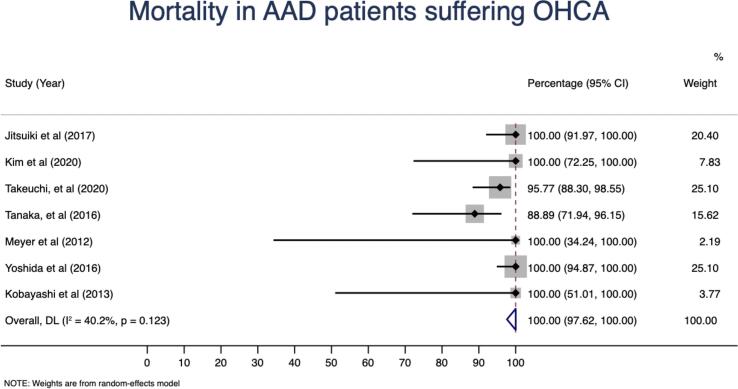
5.2. Overall mortality following AAD
Overall mortality following OHCA due to AAD was 100% (95 %CI: 97.62; 100; I2 = 40%, 7 studies [4], [6], [9], [16], [18], [21], [23])–Fig. 4.
Fig. 4.
Overall mortality following out-of-hospital cardiac arrest (OHCA) due to acute aortic dissection (AAD). Data is expressed in percentage, with respective 95% confidence interval (CI). Result: 100% (95% CI: 97.62; 100; I2 40%).
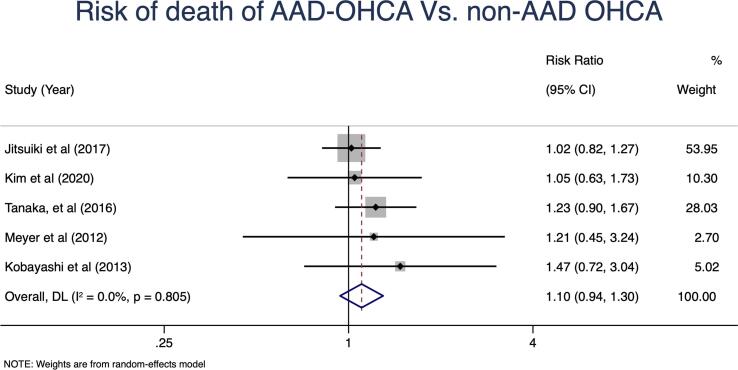
5.3. Risk of death of OHCA due to AAD vs. non-AAD OHCA
When compared to other causes of intrinsic OHCA, although there was a trend towards a higher mortality in AAD-OHCA patients, this difference was not significant–RR 1.10 (95% CI: 0.94; 1.30; I2 = 0%, p = 0.8, 5 studies [3], [4], [6], [9], [20])–Fig. 5.
Fig. 5.
Risk ratio of death in out-of-hospital cardiac arrest due to acute aortic dissection (AAD- OHCA) when compared to death in out-of-hospital cardiac arrest due to other intrinsic causes (non-AAD OHCA). Data is expressed in risk ratio, with respective 95% confidence interval (CI). Result: 1.10 (95% CI: 0.94; 1.30; I2 0%).
5.4. Sensitivity analysis (Table 3)
Table 3.
Sensitivity analysis.
| Prevalence of OHCA due to AADs | |
|---|---|
| Primary analysis | 4.39% (95 %CI: 2.55; 6.68; I2 95%) |
| Including Kim et al study | 4.91% (95 %CI: 2.95; 7.31; I2 95%) |
| Only children and young adult studies | 1.12% (95 %CI: 0.60; 1.90; I2 0%) |
| Excluding children and young adult patient studies | 5.32% (95 %CI: 3.29; 7.78; I2 94%) |
| Only studies who had anatomic imaging in all patients (CT or echocardiography) | 8.27 % (95 %CI: 5.86; 11.01; I2 81%) |
| Only autopsy studies | Only one study (Tseng et al) – 2.67% (children and young adults) |
| Only studies after 2015 | 5.58% (95 %CI: 3.41; 8.23; I2 94%) |
| Studies before 2015 | 3.28% (95 %CI: 0.03; 10.60; I2 98%) |
| Prospective studies | 1.89% (95 %CI: 0.74; 3.52; I2 64%) |
| Retrospective studies | 4.99% (95 %CI: 2.86; 7.63; I2 95%) |
| Single-center | 7.45% (95 %CI: 5.75; 9.34; I2 77%) |
| Multi-center | 1.78% (95 %CI: 0.95; 2.85; I2 79%) |
| Asia | 7.66% (95 %CI: 5.10; 10.67; I2 94%) |
| Non-Asian | 1.35% (95 %CI: 0.78; 2.04; I2 31%) |
| Non-Asian Adult Studies | 1.70% (95 %CI: 0.81; 2.86; I2 24%) |
| Excluding studies with high overall risk of bias | 7.4% (95 %CI: 2.75; 14.09; I2 96%) |
| Excluding studies with high risk of selection bias | 6.28% (95 %CI: 4.00; 9.01; I2 95%) |
| Prevalence in Patients Examined Alive with either CT or Echocardiography | 7.56% (95 %CI: 4.48; 11.31; I2 85%) |
| Prevalence in Patients Examined After Death with Autopsy or Post-Mortem CT | 5.36% (95 %CI: 2.11; 9.96; I2 91%) |
Legend: AAD: acute aortic dissection; OHCA: Out of Hospital Cardiac Arrest; ROB: Risk of Bias.
When we included the study by Kim et al. study [6], which was considered to have an unacceptably high risk of referral bias, we observed an increase in incidence (4.91% versus 4.39%). Excluding studies in which children and young adults were included [15], [21] lead also to an increase in incidence [5.80% (95 %CI: 3.75;8.47)].
If only studies in which clear imaging diagnostic modalities (CT and echocardiography) were performed in every patient [4], [6], [16], [18], [20]were analyzed, the incidence of OHCA due to AAD was also found to be higher [8.27% (95 %CI: 5.86; 11.01)].
We also analyzed studies where patients performed either a CT or echocardiography before death [4], [6], [14], [18], [20] and the incidence was found to be 7.56% (95 %CI: 4.48; 11.31; I2 85%), while in studies where the patients were diagnosed with either autopsy [19] or post-mortem CT [16], [18] had an incidence of 5.36% (95 %CI: 2.11; 9.96; I2 91%). Only one study [18 analyzed both pre and post-mortem patients with CT, and out of the 27 dissections found, 5 were found before death and 22 after.
Studies after 2015 [4], [6], [9], [14], [15], [16], [18], [19], [20], [22] also reported higher incidence rates (5.58% versus 3.28%).
In addition, Asian studies [6], [9], [16], [17], [18], [20], [22], [23] reported higher incidences when compared to other geographic areas (7.66% versus 1.70%).
When studies with a high ROB [3], [4], [6], [9], [14], [15], [18], [20], [21], [22], [23] were excluded, the incidence increased (7.40% versus 4.39%), the same occurred when studies with a high risk of selection bias [6], [14], [20], [21] were excluded (6.28% versus 4.39%).
6. Discussion
The main findings of this review were: (1) the incidence of AAD in OHCA patients was 4.39% (95 %CI: 2.55; 6.68); (2) the incidence of TAAD in OHCA patients was 7.18% (95 %CI: 5.61; 8.93), (3) the incidence of TBAD in OHCA patients was 0.47% (95 %CI: 0.18; 0.85) and (4) the overall mortality following AAD in OHCA patients was 100% (95 %CI: 97.62; 100.00).
During resuscitation, the cause of cardiac arrest is often unknown, making it difficult to make decisions regarding diagnostic procedures and treatment [6].
Our review is the first systematic review and meta-analysis on the incidence of AAD presenting as OHCA. We showed that AAD in OHCA patients is much more significant than previously thought [3], underlining the relevance of considering AAD as a differential diagnosis when approaching a patient with OHCA.
Currently, AAD diagnosis is usually confirmed with CT-angiography. Considering that this is not available in an out-of-hospital setting and that patients are usually too unstable to undergo this procedure [6], clinicians need to resort to other diagnostic procedures with significant false positive and negative rates [4]. This may lead to some AADs in OHCA patients remaining undiagnosed. Recently Kim et al. [6] has highlighted the value of TEE in this context, as it is a potential bedside imaging method that can be performed on unstable patients undergoing resuscitation maneuvers.
We found that patients presenting with OHCA due to AAD had a mortality of 100% (95% CI: 97.62; 100), which is consistent with previous reports [6]. Spontaneous circulation can only be restored in a few patients [4], [18] who may benefit from timely aortic repair, although their prognosis still remains poor [24]. This has led some authors to question the utility of resuscitation attempts in AAD-OHCA patients, due to the invariably high mortality, 100% in most studies.
Only two studies [4], [18] reported on survivors, with best survival rate of 11.1% in the Tanaka et al. study [18]. Both of these studies were performed in Japanese centers and might reflect either a higher diagnostic accuracy, since both studies used CT-Scans and found an incidence > 5% of AAD in OHCA patients, or differences in management regarding critically ill and emergent patients, with better results [25].
We found that when compared to other OHCA intrinsic causes, AAD did not confer a significant difference in mortality, although only five studies [3], [4], [6], [9], [20] were available for this analysis. This might be due to the overall bad prognosis of OHCA [16].
The difference found between the incidence of OHCA due to TAAD and OHCA due to TBAD is striking (7.18% versus 0.47%), with the former having an incidence fifteen times higher than the latter. This disparity was expected, since TAADs are associated with more serious complications, such as cardiac tamponade, stroke, and acute aortic insufficiency, that are per se causes of cardiac arrest, whereas in the case of type B dissection, OHCA usually occurs after thoracic aortic rupture, which is less frequent [2]. However, data on this subject suggests that little is known about the cardiac arrest etiologies from great vessels diseases [6].
Additionally, some studies only reported on children and young adults [15], [21]. These studies were analyzed separately in the sensitivity analysis and an incidence of AAD in OHCA patients of only 1.12% was found. This result may reflect a different subset of patients, probably suffering AAD in the context of connective tissue disorders, although this cannot be confirmed, seeing as studies did not report this etiology specifically.
There are some limitations to the present review. The difference in study designs, diagnostic methods, and definitions of both AAD and OHCA brings some clinical and statistical heterogeneity to our results. Not all patients with OHCA undertook definitive diagnostic procedures like CT, echocardiogram, or autopsy. When we included only studies that where all patients underwent CT or echocardiogram [4], [6], [16], [18], [20], the incidence increased to 8.27%. The ability to screen these patients before death is also a major limitation as some patients may not be able to perform a CT before death. In our sensitivity analysis, however, we observed that the incidence of AAD in patients submitted to CT or echocardiography before death was 7.56%, which is still a significant number of patients who may benefit from directed therapy and timely diagnosis.
The fact that the data retrieved was not age-standardized also limits our findings. The lack of data about risk factors and AAD sub-type limited our analysis on possible confounding or predictive factors. Additionally, we found a high ROB in almost every study, [3], [4], [6], [9], [14], [15], [18], [20], [21], [22], [23] which demonstrates that there is a need for more high-quality studies analyzing this daring condition.
Furthermore, we found Asian studies [6], [9], [16], [17], [18], [20], [22], [23] to have significantly higher incidence rates. This may be due to reporting issues or study designs. Future analysis on this matter would be relevant.
Considering that OHCA due to AAD is in fact a greater issue than previously considered, further studies with standardized reporting and diagnostic methods using adequate imaging methods such as CT-angiography or autopsy, are needed to better estimate the incidence of AAD.
Despite the poor prognosis, the understanding the epidemiology and management of AAD in OHCA patients across different studies and countries may lead to the development of better timely diagnostic procedures and treatments, to save, at least, some patients.
7. Conclusion
Acute aortic dissection was found to occur in 4.39% of OHCA patients. This estimate is higher than previously demonstrated. Prognosis is dire, as almost every patient dies. Type A AAD are more commonly the cause of OHCA. These findings should lead to a higher awareness of AAD when approaching a patient with OHCA. Future studies focusing on timely diagnosis and treatment strategies for AAD-OHCA are needed to improve care.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
None.
Funding: None.
Author contribution statement:
Conception and design: RM, CM, DC, AL, MS, RFF, LMP.
Analysis and interpretation: RM, DC, MA, LMP.
Data collection: RM, CM.
Writing the article: RM, CM, LMP.
Critical revision of the article: RM, DC, MA, AL, MS, RFF, LMP.
Final approval of the article: RM, CM, DC, MA, AL, MS, RFF, LMP.
Statistical analysis: RM, MA.
Obtained funding: Not applicable.
Overall responsibility: RM, LMP.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2021.100934.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Pierce L.C., Courtney D.M. Clinical characteristics of aortic aneurysm and dissection as a cause of sudden death in outpatients. Am. J. Emerg. Med. 2008;26(9):1042–1046. doi: 10.1016/j.ajem.2007.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meron G., Kürkciyan I., Sterz F., Tobler K., Losert H., Sedivy R., Laggner A.N., Domanovits H. Non-traumatic aortic dissection or rupture as cause of cardiac arrest: presentation and outcome. Resuscitation. 2004;60(2):143–150. doi: 10.1016/j.resuscitation.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Pleskot M., Babu A., Kajzr J., Kvasnicka J., Stritecky J., Cermakova E., Mestan M., Parizek P., Tauchman M., Tusl Z., Perna P. Characteristics and short-term survival of individuals with out-of-hospital cardiac arrests in the East Bohemian region. Resuscitation. 2006;68(2):209–220. doi: 10.1016/j.resuscitation.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 4.Takeuchi S., Yamaguchi Y., Soejima K., Yoshino H. Incidence and characteristics of acute aortic dissection in patients with out-of-hospital cardiopulmonary arrest evaluated by non- contrast computed tomography. Eur. Heart J. Acute Cardiovasc. Care. 2020;9:S48–S57. doi: 10.1177/2048872620923647. [DOI] [PubMed] [Google Scholar]
- 5.Nienaber C.A., Clough R.E. Management of acute aortic dissection. Lancet. 2015;385(9970):800–811. doi: 10.1016/S0140-6736(14)61005-9. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y.W., Jung W.J., Cha K.C., et al. Diagnosis of aortic dissection by transesophageal echocardiography during cardiopulmonary resuscitation. Am. J. Emerg. Med. 2021;39:92–95. doi: 10.1016/j.ajem.2020.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA Statement For Reporting Systematic Reviews And Meta-Analyses Of Studies That Evaluate Healthcare Interventions. Explanation And Elaboration. BMJ. 2009;339:2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stroup D.F., Berlin J.A., Morton S.C., et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 9.SOS-KANTO 2012 Study Group, S. Inokuchi, Y. Masui, K. Miura, et al., Investigation and treatment of pulmonary embolism as a potential etiology may be important to improve post-resuscitation prognosis in non-shockable out-of-hospital cardiopulmonary arrest: report on an analysis of the SOS-KANTO 2012 study, Acute Med. Surg., 3 (2016) 250–259. [DOI] [PMC free article] [PubMed]
- 10.Hoy D., Brooks P., Woolf A., Blyth F., March L., Bain C., Baker P., Smith E., Buchbinder R. Assessing Risk Of Bias In Prevalence Studies: Modification Of An Existing Tool And Evidence Of Interrater Agreement. J. Clin. Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Community Health. 2013;67(11):974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 12.Dersimonian R., Laird N. Meta-Analysis Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 13.Higgins J.P.T., Thompson S.G. Quantifying Heterogeneity In A Meta-Analysis. Stat. Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 14.Adler C., Paul C., Hinkelbein J., Michels G., Pfister R., Krings A., Lechleuthner A., Stangl R. Welcher Patient profitiert von einem Transport unter laufender kardiopulmonaler Reanimation?: Retrospektive Analyse von 70 Patienten mit refraktärem präklinischem HerzstillstandWhich patients benefit from transport with ongoing cardiopulmonary resuscitation?: Retrospective analysis of 70 patients with refractory preclinical cardiac arrest. Anaesthesist. 2018;67(5):343–350. doi: 10.1007/s00101-018-0441-6. [DOI] [PubMed] [Google Scholar]
- 15.Allan K.S., Morrison L.J., Pinter A., Tu J.V., Dorian P. Rescu Epistry Investigators. “Presumed cardiac” arrest in children and young adults: A misnomer? Resuscitation. 2017;117:73–79. doi: 10.1016/j.resuscitation.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Jitsuiki K., Ishikawa K., Nagasawa H., Takeuchi I., Iso T., Kondo A., Ohsaka H., Omori K., Yanagawa Y. Clinical profile of patients with cardiac arrest induced by aortic disease. Resuscitation. 2017;120:e1. doi: 10.1016/j.resuscitation.2017.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Moriwaki Y., Tahara Y., Kosuge T., Suzuki N. Etiology of out-of-hospital cardiac arrest diagnosed via detailed examinations including perimortem computed tomography. J. Emerg. Trauma Shock. 2013;6(2):87. doi: 10.4103/0974-2700.110752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tanaka Y., Sakata K., Sakurai Y., Yoshimuta T., Morishita Y., Nara S., Takahashi I., Hirokami M., Yamagishi M. Prevalence of Type A Acute Aortic Dissection in Patients With Out-Of-Hospital Cardiopulmonary Arrest. Am. J. Cardiol. 2016;117(11):1826–1830. doi: 10.1016/j.amjcard.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 19.Tseng Z.H., Olgin J.E., Vittinghoff E., Ursell P.C., Kim A.S., Sporer K., Yeh C., Colburn B., Clark N.M., Khan R., Hart A.P., Moffatt E. Prospective Countywide Surveillance and Autopsy Characterization of Sudden Cardiac Death: POST SCD Study. Circulation. 2018;137(25):2689–2700. doi: 10.1161/CIRCULATIONAHA.117.033427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang K.J., Wang C.H., Huang Y.C., Tseng L.J., Chen Y.S., Yu H.Y. Clinical experience of whole-body computed tomography as the initial evaluation tool after extracorporeal cardiopulmonary resuscitation in patients of out-of-hospital cardiac arrest. Scand. J. Trauma Resusc. Emerg. Med. 2020;28:54. doi: 10.1186/s13049-020-00746-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer L., Stubbs B., Fahrenbruch C., Maeda C., Harmon K., Eisenberg M., Drezner J. Incidence, causes, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults 0 to 35 years of age: a 30-year review. Circulation. 2012;126(11):1363–1372. doi: 10.1161/CIRCULATIONAHA.111.076810. [DOI] [PubMed] [Google Scholar]
- 22.Otani T., Sawano H., Natsukawa T., Matsuoka R., Nakashima T., Takahagi M., Hayashi Y. D-dimer predicts bleeding complication in out-of-hospital cardiac arrest resuscitated with ECMO. Am. J. Emerg. Med. 2018;36(6):1003–1008. doi: 10.1016/j.ajem.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Kobayashi N., Hata N., Shimura T., Yokoyama S., Shirakabe A., Shinada T., Tomita K., Murakami D., Takano M., Seino Y., Matsumoto H., Mashiko K., Mizuno K. Characteristics of patients with cardiac arrest caused by coronary vasospasm. Circ. J. 2013;77(3):673–678. doi: 10.1253/circj.cj-12-0846. [DOI] [PubMed] [Google Scholar]
- 24.Johansson G., Markström U., Swedenborg J. Ruptured thoracic aortic aneurysms: a study of incidence and mortality rates. J. Vasc. Surg. 1995;21(6):985–988. doi: 10.1016/s0741-5214(95)70227-x. [DOI] [PubMed] [Google Scholar]
- 25.Founding members of the Japanese Association for Hybrid Emergency Room System (JA‐HERS), The hybrid emergency room system: a novel trauma evaluation and care system created in Japan, Acute Med. Surg., 6 (2019) 247–251. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.