Abstract
Malignant optic gliomas are an uncommon pathology, with around 67 cases reported worldwide in the literature. We present the case of a 77-year-old-male with a two-month history of progressive vision loss, ultimately leading to bilateral blindness. The initial clinical suspicion was a non-inflammatory ischemic optic neuropathy. Stereotactic biopsy was performed on the optic chiasm, and the histopathological diagnosis was confirmed as Glioblastoma.
Keywords: Magnetic resonance imaging, Optic glioma, Optic nerve, Glioblastoma
Introduction
Optic gliomas represent 0.6%–1.2% of all brain tumors detected in general [1]. Most are benign and occur in the pediatric population before age 15 (85%) and are strongly associated with Type I neurofibromatosis [2,3]. Malignant optic gliomas rarely occur in adults; this entity was defined for the first time in 1973 by Hoyt et al. [4]. There have been 67 cases reported (70) in the medical literature, of which 26 [5] correspond to Glioblastoma (GBM).
Patients are usually middle-aged men presenting with progressive deterioration of vision, which leads to blindness within a few weeks. The initial diagnostic impression is often wrong due to symptoms misinterpreted as ischemic neuropathy, optic neuritis, or retinal vascular occlusion [3].
The tumor may originate in the optic chiasm, the optic tract, or the optic nerves and may occur as multifocal neoplasia. Magnetic resonance imaging (MRI) of the brain is the primary diagnostic tool. Nevertheless, the findings are nonspecific. A biopsy is needed to confirm the diagnosis. Pathologic features can be consistent with Anaplastic Astrocytoma (grade III - WHO) or GBM (grade IV- WHO) [6].
We present the case of a patient diagnosed with GBM in the optic chiasm and optic nerves. We also briefly review the clinical manifestations, neuroradiological findings, and clinical outcomes of the optical GBM cases reported in the literature to this date.
Case report
A 77-year-old-man with a two-month history of progressive bilateral vision loss, more prominent on his left eye, presented to the ophthalmologist's office. The initial presumptive diagnosis was a non-arteritic ischemic optic neuropathy, for which the patient was referred to the emergency room. The patient was assessed by a clinical neurologist, who did not find headache, mandibular claudication, or pain associated with eye movements or in the temporal area. During the physical examination, pupils were hyporeactive, and visual acuity was diminished with dyschromatopsia on the right eye and absence of light perception on the left eye. The patient had no further neurologic compromise.
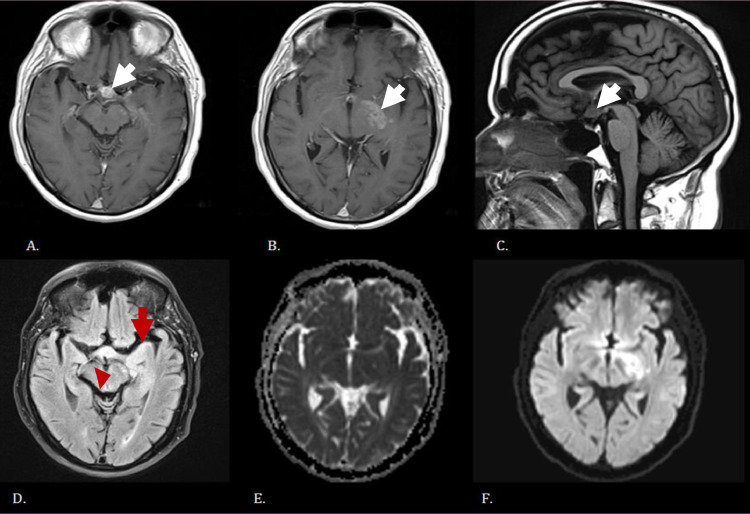
Given the clinical manifestations, a brain and orbit MRI was ordered, revealing evidence of a non-uniform enhancement in the optic chiasm and the left optic tract. Thickening and cortical enhancement were also found in the left mesial temporal lobe region and left lateral margin of the midbrain (see Fig. 1). These findings suggested an inflammatory compromise or demyelination, though it was not possible to rule out neoplastic infiltration. Under the suspicion of demyelinating disease, an analysis of oligoclonal bands was requested. The patient was treated with methylprednisolone and showed modest clinical improvement. He was discharged and sent for ambulatory studies in the Neurology Department.
Fig. 1.
(A) and (B) Axial T1 contrast-enhanced sequence with evidence of nodular thickening of the optic chiasm (white arrow on A) and left optic tract (white arrow on B) associated with enhancement of these structures. (C) Sagittal T1 sequence demonstrating evidence of nodular thickening of the optical chiasm (white arrow). (D) Axial FLAIR sequence with hyperintensity of the temporal lobe's mesial region (red arrow) and the midbrain's left lateral margin (red arrow head). (E) and (F) Axial ADC, and DWI sequences show no evidence of restriction of the previously described structures.
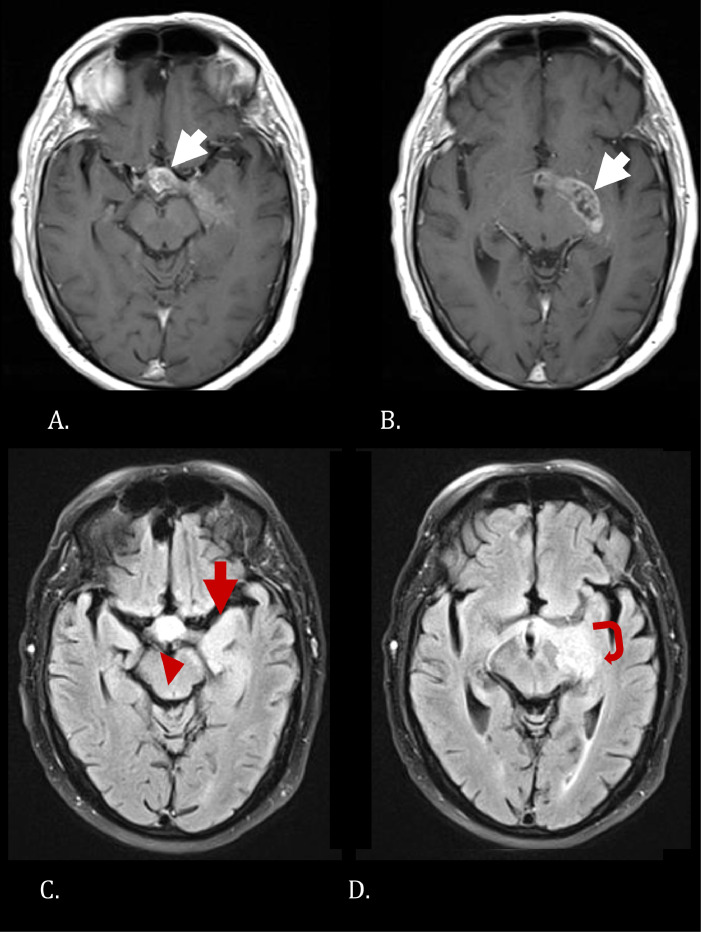
The patient returned one month later due to bilateral blindness with no additional neurologic symptoms. A new brain contrast-enhanced MRI was performed and demonstrated progressive thickening and enhancement of the same structures compared to the previous study and a heterogeneously enhancing mass in the left optic tract with similar features (see Fig. 2). Due to these new findings, the patient was referred for a stereotactic biopsy of the lesion. This procedure was made following a pallidotomy to ensure that the optic tract was reached precisely. Pathology reported a glioblastoma with a Ki67 marker of 25%.
Fig. 2.
(A) and B) Axial contrast-enhanced T1 sequence demonstrates increased thickening and heterogeneous enhancement of the chiasm (white arrow on A) and left optic tract (white arrow on B). (C) and (D) Axial FLAIR sequence shows increased hyperintensity of the mesial portion of the temporal lobe (red arrow con C), midbrain's left lateral margin (red arrowhead on C), optic chiasm and tracts (curved red arrow on D).
Due to the lesion's location, neurologic status, and clinical deterioration, surgical resection was not possible. He was offered palliative care. The patient died five months after the initial presentation.
To be granted access to clinical information and diagnostic images, the institutional ethics committee was requested to waive the case report from informed consent.
Discussion
Optic malignant gliomas are exceedingly rare. Wabbels et al. (2004) undertook a literature review and described 45 cases [7]. More recently, Traber et al. (2015) reported five patients and identified 21 additional cases published after 2004 [6]. Subsequently, Nagaichi et al. (2015) reported a new case [1]. After this report, and to our knowledge, there are at least 71 cases of optic gliomas malignancies in the medical literature, 30 corresponding to GBM (see Table 1).
Table 1.
Characteristics of the reported cases of Glioblastoma.
| Author | Age/Sex | Time to blindness | Initial diagnosis | MRI | Treatment | Time to death after dx |
|---|---|---|---|---|---|---|
| Saebo 1949 [7] | 43/F | - | Tumor of the optic nerve | - | RT and surgical resection | One year |
| Mattson 1966 [16] | 59/ F | 1 mo | Optic neuritis | - | No treatment | 4 mo |
| Hoyt et al. 1973 [4] | 55 / M | - | - | - | RT | 9–10 mo |
| Harper and Stewart-Wynne 1978 [17] | 75 / M | - | Brain tumor | - | No treatment | 3 mo |
| 79/ F | - | Brain tumor | - | No treatment | 3 mo | |
| Spoor et al. 1980 [18] | 60 / F | 2 mo | - | - | RT | 6 mo |
| Barbaro et al. 1982 [19] | 26 / M | 2 wk | Craneopharyngioma – pituitary adenoma cyst | - | RT y CT | 8 mo |
| Evens et al. 1987 [20] | 61 / F | 1 mo | - | - | RT | 9 mo |
| Albers et al. 1988 [14] | 51/ M | 2 wk | - | T2 (Hyperintense) | No treatment | 20 mo |
| Woiciechowsky et al. 1995 [21] | 76 / M | - | Malignant optic glioma | T1 + Contrast (Enhancement) | Surgical resection and RT | - |
| Pallini et al. 1996 [22] | 59 /F | - | - | - | RT | 7 mo |
| Hahn et al. 2004 [23] | 53 /M | - | Neurosarcoidosis | T1 + contrast (Enhancement) T2 (Hyperintense) | RT and CT | - |
| Hartel et al. 2006 [24] | 59 /M | <1 mo | Unknown | - | None | 8 wk |
| Dinh et al. 2007 [3] | 48 /F | 10 wk | Tumor of the optic nerve | T1 + contrast (Enhancement) | RT | 14 mo |
| Abou - Zeid et al. 2008 [25] | 56 /M | <1 mo | Metastatic brain disease | T1 + contrast (Enhancement) | RT | 3 mo |
| Brar et al. 2009 [26] | 68 / F | 2 mo | - | T1 hypointense - isointense T1 + contrast (Enhancement) T2 (Hyperintense) | - | |
| Matloob et al. 2011 [12] | 63 / F | <1 mo | Optic neuritis | T1 + contrast (Enhancement) T2 (Hyperintense) | CT | 6 mo |
| Lincoff et al. 2012 [27] | 83 / M | <1 mo | - | T1 + contrast (Enhancement) T2 (Hyperintense) | - | - |
| Ashur- Fabian et al. 2013 [15] | 64/ M | 6 mo | - | T1 + contrast (Enhancement) | RT and CT | 54 mo |
| Colpak et al. 2014 [28] | 47 / M | <1 mo | Optic neuritis or infiltrative | T1 + contrast (Enhancement) | - | 3 mo |
| Traber et al. 2015 [5] | 65 / M | 5 wk | Tumor of the optic nerve | T1 + contrast (Enhancement) T2 (Hyperintense) | RT and CT | 4.5 mo |
| 54 / M | 7 mo | Optic neuritis | T1 + contrast (Enhancement) T2 (Hyperintense) | RT and CT | 18 mo | |
| 64 / F | 6 wk | Tumor of the optic nerve | T1 + contrast (Enhancement) T2 (Hyperintense) | RT | 6 mo | |
| 75/ M | 6 wk | Optic neuritis | T1 + contrast (Enhancement) T2 (Hyperintense) | RT | 12 mo | |
| 76 / F | 4 wk | Non-artieric ischemic optic neuritis | T1 + contrast (Enhancement) T2 (Hyperintense) | RT | 7 mo | |
| Nagaishi et al. 2015 [1] | 64 / F | - | - | T1 + contrast (Enhancement) T2 (Hyperintense) | Radiosurgery and CT | 10 mo |
| Mastorakos et al. 2017 [30] | 66/M | 12 mo | Meningioma | T1 + contrast (Enhancement) | Surgical resection and CT | 16 mo |
| Lin et al. [31] | 21/M | 4 mo | Optic neuritis | T1 + contrast (Enhancement) | Srugical resection and CT | - |
| Alabiad et al. 2020 [29] | 18/F | 4 wk | Unknown | T1 + contrast (Enhancement) | Surgical resection, CT and RT | Alive (>7 y) |
| Current case | 77/ M | 3 mo | Optic neuritis | T1 + contrast (Enhancement) T2 (Hyperintense) | None | 4 mo |
Wabbels et al. (2004) revised 45 cases, and Traber et al. (2015) reported 26 cases.
Our patient presented with imaging findings and clinical characteristics like those reported in other cases of GBM, in which the median age of presentation was 61, and there was a slight predominance of male gender (11 women and 16 men). The clinical picture is characterized by rapidly progressive vision loss, either unilateral or bilateral, in conjunction with headache or periorbital pain [3]. The average time to complete vision loss in the reported cases was 5–6 weeks. Proptosis is exceptionally rare in these cases. In 1949, Saebo reported the case of a 43-year-old-woman with four months of vision loss and simultaneous proptosis of the left eye, for whom the final diagnosis was optical GBM [8].
GBM is frequently confused with another diagnosis due to the unspecific clinical picture. Non-arteritic ischemic optic neuropathy, for example, was suggested as the initial presumptive diagnosis in our case since this usually occurs in patients over their 50′s and presents as a sudden, painless loss of vision which is either unilateral or bilateral [9,10]. Another differential diagnosis is optic neuritis, which usually presents as a unilateral loss of vision; this is, however, usually found in patients younger than 50 years of age and improves with the administration of corticosteroids [11,12]. GBM can also be confused with other diagnoses such as retinal vein occlusion and temporal arteritis [3].
The tumor's site of origin determines whether the initial vision loss is unilateral or bilateral and the presence or absence of ophthalmic symptoms. Tumors originating in the optic nerve initially cause unilateral vision loss and bilateral changes in fundoscopy (disc edema and venous stasis). On the other hand, tumors in the optic chiasm present bilateral visual alterations and normal fundoscopy. The latter is more likely to infiltrate the hypothalamus and the walls of the third ventricle [3,13]. If the tumor is in the optic tract, there will be a visual field deficit contralateral to the side of the lesion.
The most common affected sites are the chiasm, and optic nerves are the hypothalamus, the temporal lobe, and the basal ganglia [7]. Symptoms of hypothalamic involvement include polyuria and polydipsia and may appear in the late course of the disease, suggesting infiltration [14].
The neuroimaging features are non-specific in the early stages of the disease, as noted by Albers et al. when they described the first case, including the results from an MRI study [15]. The reported findings were enhancement in the post-contrast T1 sequence and thickening of the nerve, chiasm, or the optic tract in the T1 weighted images. T2 hyperintensity has also been reported to affect the anterior visual pathway, initially described by Albers et al. in 1988; this last characteristic is still debatable [6]. The imaging findings reported in the medical literature are like those observed in our case, including enhancement of the optic nerve in the post-contrast T1 images and T2 hyperintensity.
There are similar imaging findings in conditions such as multiple sclerosis, peri-optic neuritis, low-grade primary optic glioma, lymphoma, leukemia, and metastasis. Infiltrative processes produce a fusiform thickening, while inflammatory processes produce a more tubular enhancement [13].
Some diseases thicken the optic nerve without affecting the sheath (optic neuritis, optic nerve ischemia). In contrast, other processes affect the sheath without any nerve swelling (meningioma, pseudotumor). The pathologies that affect both nerves and the sheath include optic glioma, peri-optic neuritis secondary to infection and granulomatous disease, leukemia, lymphoma, and metastatic disease [14]. In recent years it has been proposed that Color Doppler Flow Imaging might help the diagnosis of malignant optic gliomas.
The prognosis is poor for GMB, with an average survival time of 8–9 months of all 27 cases found in the literature. Alabiad et al. (2020) reported the case with the most extended survival (7 years, and still alive) [5].
Conclusion
Optic nerve GBM is a rare neoplasm with rapid evolution; early diagnosis is difficult due to the lack of a clear clinical presentation and characteristic imaging features. It is crucial to consider malignant optical glioma as a differential diagnosis in cases similar to that reported.
Data sharing statement
The relevant anonymized patient-level data are available via request from the authors.
Ethical approval and patient consent
The report case was reviewed and approved. Following our institutional guidelines, all protected health information was removed, and individual patient consent was not required for the analysis.
Footnotes
Acknowledgments: The author(s) received no financial support for the research, authorship, and/or publication of this article. The authors thank Dr Camila Ospina Jiménez for her initial collaboration.
Competing interests: The authors declare no conflicts of interest in the publication of this article.
References
- 1.Nagaishi M, Sugiura Y, Takano I, Tanaka Y, Suzuki K, Yokoo H, et al. Clinicopathological and molecular features of malignant optic pathway glioma in an adult. J Clin Neurosci. 2015;22(1):207–209. doi: 10.1016/j.jocn.2014.05.037. [DOI] [PubMed] [Google Scholar]
- 2.Kornreich L, Blaser S, Schwarz M, Shuper A, Vishne TH, Cohen IJ, et al. Optic pathway glioma: correlation of imaging findings with the presence of neurofibromatosis. AJNR Am J Neuroradiol. 2001;22(10):1963–1969. [PMC free article] [PubMed] [Google Scholar]
- 3.Dinh TT, Wang YY, Rosenfeld JV, Cherny M. Glioblastoma of the optic chiasm. J Clin Neurosci. 2007;14(5):502–505. doi: 10.1016/j.jocn.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Hoyt WF, Meshel LG, Lessell S, Schatz NJ. Suckling RD. Malignant optic glioma of adulthood. Brain. 1973;96(1):121–132. doi: 10.1093/brain/96.1.121. [DOI] [PubMed] [Google Scholar]
- 5.Traber GL, Pangalu A, Neumann M, Costa J, Weller M, Huna-Baron R, et al. Malignant optic glioma - the spectrum of disease in a case series. Graefes Arch Clin Exp Ophthalmol. 2015;253(7):1187–1194. doi: 10.1007/s00417-015-3045-8. [DOI] [PubMed] [Google Scholar]
- 6.Wabbels B, Demmler A, Seitz J, Woenckhaus M, Bloss HG, Lorenz B. Unilateral adult malignant optic nerve glioma. Graefes Arch Clin Exp Ophthalmol. 2004;242(9):741–748. doi: 10.1007/s00417-004-0905-z. [DOI] [PubMed] [Google Scholar]
- 7.SAEBØ J. Primary tumour of the optic nerve, glioblastoma multiforme. Br J Ophthalmol. 1949;33(11):701–708. doi: 10.1136/bjo.33.11.701. illust. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Behbehani R. Clinical approach to optic neuropathies. Clin Ophthalmol. 2007;1(3):233–246. [PMC free article] [PubMed] [Google Scholar]
- 9.Kerr NM, Chew SS, HV Danesh-Meyer. Non-arteritic anterior ischaemic optic neuropathy: a review and update. J Clin Neurosci. 2009;16(8):994–1000. doi: 10.1016/j.jocn.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Shams PN, Plant GT. Optic neuritis: a review. Int MS J. 2009;16(3):82–89. [PubMed] [Google Scholar]
- 11.Hoorbakht H, Bagherkashi F. Optic neuritis, its differential diagnosis and management. Open Ophthalmol J. 2012;6:65–72. doi: 10.2174/1874364101206010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matloob S, Fan JC, Danesh-Meyer HV. Multifocal malignant optic glioma of adulthood presenting as acute anterior optic neuropathy. J Clin Neurosci. 2011;18(7):974–977. doi: 10.1016/j.jocn.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Millar WS, Tartaglino LM, Sergott RC, Friedman DP, Flanders AE. MR of malignant optic glioma of adulthood. AJNR Am J Neuroradiol. 1995;16(8):1673–1676. [PMC free article] [PubMed] [Google Scholar]
- 14.Albers GW, Hoyt WF, Forno LS, Shratter LA. Treatment response in malignant optic glioma of adulthood. Neurology. 1988;38(7):1071–1074. doi: 10.1212/wnl.38.7.1071. [DOI] [PubMed] [Google Scholar]
- 15.Mattson RH, Peterson EW. Glioblastoma multiforme of the optic nerve. JAMA. 1966;196(9):799–800. [PubMed] [Google Scholar]
- 16.Harper CG, Stewart-Wynne EG. Malignant optic gliomas in adults. Arch Neurol. 1978;35(11):731–735. doi: 10.1001/archneur.1978.00500350035007. [DOI] [PubMed] [Google Scholar]
- 17.Spoor TC, Kennerdell JS, Martinez AJ, Zorub D. Malignant gliomas of the optic nerve pathways. Am J Ophthalmol. 1980;89(2):284–292. doi: 10.1016/0002-9394(80)90126-9. [DOI] [PubMed] [Google Scholar]
- 18.Barbaro NM, Rosenblum ML, Maitland CG, Hoyt WF, Davis RL. Malignant optic glioma presenting radiologically as a "cystic" suprasellar mass: case report and review of the literature. Neurosurgery. 1982;11(6):787–789. doi: 10.1227/00006123-198212000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Evens PA, Brihaye M, Buisseret T, Storme G, Solheid C, Brihaye J. [Malignant glioma of the chiasma in adults] Bull Soc Belge Ophtalmol. 1987;224:59–60. [PubMed] [Google Scholar]
- 20.Woiciechowsky C, Vogel S, Meyer R, Lehmann R. Magnetic resonance imaging of a glioblastoma of the optic chiasm. Case report. J Neurosurg. 1995;83(5):923–925. doi: 10.3171/jns.1995.83.5.0923. [DOI] [PubMed] [Google Scholar]
- 21.Pallini R, Lauretti L. La Marca F. Glioblastoma of the optic chiasm. J Neurosurg. 1996;84(5):898–899. doi: 10.3171/jns.1996.84.5.0898. [DOI] [PubMed] [Google Scholar]
- 22.Hahn U, Ritz R, Ernemann U. [Glioblastoma multiforme of the optic nerve] Rofo. 2004;176(11):1700–1701. doi: 10.1055/s-2004-813419. [DOI] [PubMed] [Google Scholar]
- 23.Hartel PH, Rosen C, Larzo C, Nestor S. Malignant optic nerve glioma (glioblastoma multiforme): a case report and literature review. W V Med J. 2006;102(4):29–31. [PubMed] [Google Scholar]
- 24.Abou-Zeid A, Duplessis D, Gnanalingham KK. Blindness from multiple cerebral gliomas mimicking metastatic brain disease. Br J Neurosurg. 2008;22(6):772–773. doi: 10.1080/02688690802233372. [DOI] [PubMed] [Google Scholar]
- 25.Brar R, Prasad A, Brar M. Glioblastoma of the optic pathways: an Atypical case. J Radiol Case Rep. 2009;3(9):22–28. doi: 10.3941/jrcr.v3i9.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lincoff NS, Chung C, Balos L, Corbo JC, Sharma A. Combing the globe for terrorism. J Neuroophthalmol. 2012;32(1):82–85. doi: 10.1097/WNO.0b013e31824095d1. [DOI] [PubMed] [Google Scholar]
- 27.Ashur-Fabian O, Blumenthal DT, Bakon M, Nass D, Davis PJ, Hercbergs A. Long-term response in high-grade optic glioma treated with medically induced hypothyroidism and carboplatin: a case report and review of the literature. Anticancer Drugs. 2013;24(3):315–323. doi: 10.1097/CAD.0b013e32835c7a47. [DOI] [PubMed] [Google Scholar]
- 28.Colpak AI, Isikay I, Mut M, Soylemezoglu F, Kansu T, Foroozan R. Acute visual loss: just the beginning? Surv Ophthalmol. 2014;59(5):548–552. doi: 10.1016/j.survophthal.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 29.Alabiad CR, Shah VS, Eatz TA, Sternau LL, Lam BL. Malignant optic nerve glioma in a young woman with 7 year follow up without recurrence. Am J Ophthalmol Case Rep. 2020;19 doi: 10.1016/j.ajoc.2020.100862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mastorakos P, Hays MA, Caruso JP, Chen CJ, Ding D, Taylor DG, Beatriz Lopes M, Shaffrey ME. Transtentorial dissemination of optic nerve glioblastoma: case report. J Neurosurg. 2018;128(2):406–413. doi: 10.3171/2016.10.JNS161443. [DOI] [PubMed] [Google Scholar]
- 31.Lin CY, Huang HM. Unilateral malignant optic glioma following glioblastoma multiforme in the young: a case report and literature review. BMC Ophthalmol. 2017;17(1):21. doi: 10.1186/s12886-017-0415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]