Abstract
Introduction
There has been an unprecedented spike in COVID-19–associated mucormycosis (CAM), with most patients showing rhino-orbital involvement, whereas limited data are available on COVID-19–associated pulmonary mucormycosis (CAPM). Pulmonary mucormycosis is rare and has a high mortality rate (1). COVID-19 pneumonia makes it further challenging to identify pulmonary mucormycosis at radiologic imaging. Herein, we describe the imaging findings of three confirmed cases of CAPM and supplement it with a systematic review of the literature.
Materials and Methods
In this retrospective study (approved by the institute ethics committee), we describe the imaging and clinical features of three microbiologically confirmed cases of CAPM. We performed a systematic review of the PubMed and Embase databases, using the search terms (“COVID” OR “SARS-CoV” OR “coronavirus”) AND (mucor* OR “zygomycosis”) until June 14th, 2021, to identify published cases of CAPM (diagnosed as per current recommendations) (2). We included them for analysis if individual patient and imaging data were provided.
Results
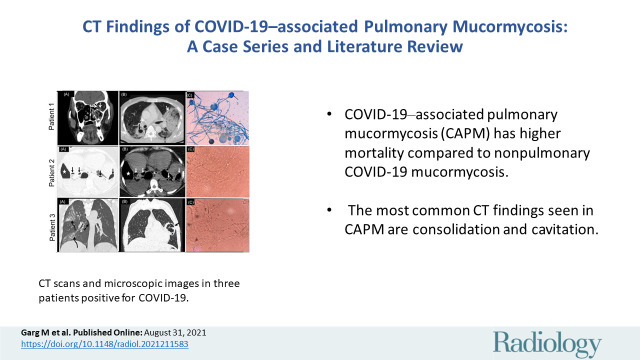
At our center, we diagnosed three cases of CAPM (Figure). Two of the three patients had no risk factor other than COVID-19. One case was of a man with diabetes with both rhino-orbital involvement and pulmonary mucormycosis. Two patients survived. We identified 180 cases of CAM in the literature during the review period and included only those 88 cases (14 CAPM and 74 nonpulmonary CAM) for which individual patient details were available (3–28). Of the 14 CAPM cases reported (three from the United States, two from the United Kingdom, three from the Netherlands, two from India, and one each from Italy, Austria, Chile, and France) (12,29–38), CT details were unavailable in one (12). After exclusions, we report the CT features of these 13 cases along with the three index cases reported by us (n = 16) (Table).
Patient 1: A 45-year-old diabetic man, positive for SARS-CoV-2, presented with loss of vision in left eye and facial swelling on the 12th day of illness. (A) Coronal CT section of paranasal sinuses and orbits shows soft tissue in the left maxillary sinus (asterisk) causing blockage of osteomeatal complex. There is fat stranding in left orbit with increased bulk of left medial and inferior rectus muscles (arrows) suggesting orbital extension. (B) Axial CT chest sections show thick-walled cavitatory lesion in right lower lobe (black arrow) and large area of consolidation in left upper lobe (white arrow). Patchy ground-glass opacities (GGOs) with septal thickening were noted in bilateral lungs (dashed black arrow) consistent with underlying COVID-19 pneumonia. (C) Lactophenol cotton blue mount (10×) of culture of endotracheal aspirate depicted long smooth-walled sporangiophores, globose sporangia (black arrows), and subglobose to ellipsoidal sporangiospores with striations suggesting it to be Rhizopus arrhizus. Patient died 25 days after the onset of illness due to massive hemoptysis.
Patient 2: A 36-year-old woman, positive for COVID-19 infection, had persistent hypoxia despite being on oxygen therapy and systemic corticosteroids. Chest CT was performed on day 24 of illness. (D,E) Axial sections of CT (lung window and corresponding mediastinal window) show multiple thin- to thick-walled cavities (black arrows in D; white arrows in E) in bilateral lungs, many of them showing air-fluid levels. Loculated right hydropneumothorax (⋆) with left pleural effusion was seen. (F) KOH wet mount preparation from endotracheal aspirate revealed aseptate, ribbon-like fungal hyphae (40×). Patient was started on amphotericin B and subsequently improved.
Patient 3: A 45-year-man with no known comorbid illness, positive for SARS-CoV-2, underwent chest CT on day 25 of illness, due to persistent fever and dyspnea. (G) Coronal section of chest CT shows patchy GGOs and consolidation with septal thickening in right lung (curved arrows) consistent with underlying COVID-19 pneumonia. Note the mild right pneumothorax (dashed arrow). (H) Coronal CT chest section performed 7 days later shows cavitatory lesion in left lung with few septae within. Pneumothorax and COVID-19 pneumonia changes have resolved. (I) Direct microscopy (KOH mount) of endotracheal aspirate (40×) shows aseptate, ribbon-like broad hyphae. Patient improved on amphotericin B treatment and was discharged.
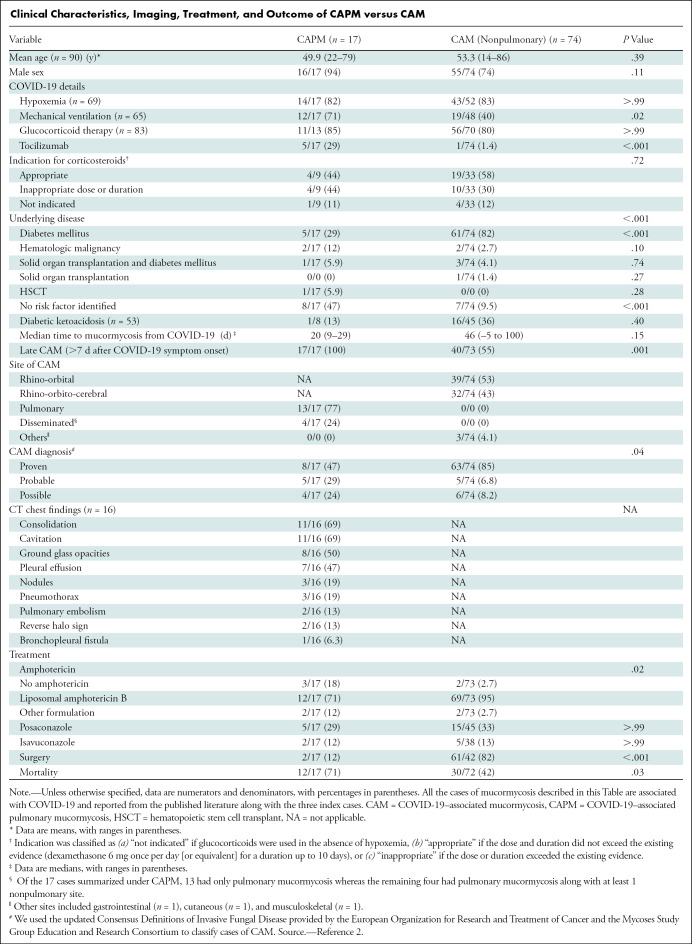
Clinical Characteristics, Imaging, Treatment, and Outcome of CAPM versus CAM
The most frequent CT findings were consolidation and cavitation seen in 11 (69%) patients. Pleural effusion was seen in seven (47%) patients, pneumothorax and nodules in three (19%) patients, and the “reverse halo” and pulmonary embolism were seen in two (13%) patients.
We compared CAPM with nonpulmonary CAM identified from our review (Table). The risk factor profile was significantly different in both groups. No risk factors other than COVID-19 and its treatment were identified in 47% of CAPM. Although diabetes mellitus was common in CAPM (29%), it was significantly less than in nonpulmonary CAM (82%). Patients with CAPM were more often undergoing mechanical ventilation than were patients with nonpulmonary CAM (71% vs 40%; P = .02). CAPM was diagnosed after a median of 20 days (range, 9–29 days) after the onset of COVID-19 symptoms. Surgery was performed only in 12% of patients with CAPM, whereas 82% of patients with nonpulmonary CAM (mostly rhino-orbital) underwent surgery. Amphotericin-B was not instituted in 18% and 3% of the CAPM and nonpulmonary CAM cases, respectively (P = .02). CAPM had higher mortality than did nonpulmonary CAM cases (71% vs 42%; P = .03). Notably, three CAPM cases were not suspected antemortem (30,34,38).
Discussion
Mucormycosis has been shown to occur in fewer than 1% of hospitalized patients with COVID-19, and pulmonary mucormycosis accounts for 9% of CAM (39,40). Although CT findings of pulmonary mucormycosis have been described previously (41,42), CAPM has not been systematically explored. In a study reporting pulmonary mucormycosis among hematologic malignancies (before the COVID-19 pandemic), consolidation (55%), and nodules (35%) were the primary initial findings, whereas central necrosis, cavity, and air crescent sign appeared later (41). We found consolidation and cavitation to be the predominant findings (69%) in our study, possibly reflecting delayed identification of cases of CAPM. The imaging findings of CAPM may overlap with COVID-19–associated pulmonary aspergillosis and cavitating bacterial pneumonias, making the differentiation difficult. Sometimes even coinfections are seen (29,31).
There were few limitations in our study. We included only confirmed cases of CAPM and it may not reflect the entire spectrum, because many patients with high suspicion remain unproven or die before reaching the hospital. Second, we did not evaluate serial CT findings. Third, many published reports did not explicitly catalog the CT findings of CAPM. We summarized the data from a small number of patients with CAPM, and larger studies are required.
In conclusion, COVID-19–associated pulmonary mucormycosis (CAPM) has higher mortality than does nonpulmonary CAPM, and the most frequent CT findings of CAPM are consolidation and cavitation.
Acknowledgments
Acknowledgments
We thank Dr MS Sandhu, MD; Dr GD Puri, MD; Dr Arunaloke Chakrabarty, MD; Dr Ashish Bhalla, MD; Dr Shivaprakash M. Rudramurthy, MD; Dr Mandeep Kang, MD; and Dr Inderpaul Sehgal, DM (PGIMER, Chandigarh, India) for their valuable opinions and input.
Footnotes
M.G. and N.P. contributed equally to this work.
Disclosures of conflicts of interest: M.G. No relevant relationships. N.P. No relevant relationships. V.M. No relevant relationships. S.F. No relevant relationships. H.K. No relevant relationships. V.S. No relevant relationships. R.A. No relevant relationships.
Referencses
- 1. Muthu V, Agarwal R, Dhooria S, et al. Has the mortality from pulmonary mucormycosis changed over time? A systematic review and meta-analysis. Clin Microbiol Infect 2021;27(4):538–549. [DOI] [PubMed] [Google Scholar]
- 2. Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis 2020;71(6):1367–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ravani SA, Agrawal GA, Leuva PA, Modi PH, Amin KD. Rise of the phoenix: Mucormycosis in COVID-19 times. Indian J Ophthalmol 2021;69(6):1563–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mekonnen ZK, Ashraf DC, Jankowski T, et al. Acute Invasive Rhino-Orbital Mucormycosis in a Patient With COVID-19-Associated Acute Respiratory Distress Syndrome. Ophthal Plast Reconstr Surg 2021;37(2):e40–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol 2021;135(5):442–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arana C, Cuevas Ramírez RE, Xipell M, et al. Mucormycosis associated with COVID-19 in two kidney transplant patients. Transpl Infect Dis 2021. 10.1111/tid.13652. Published online May 26, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maini A, Tomar G, Khanna D, Kini Y, Mehta H, Bhagyasree V. Sino-orbital mucormycosis in a COVID-19 patient: A case report. Int J Surg Case Rep 2021;82:105957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moorthy A, Gaikwad R, Krishna S, et al. SARS-CoV-2, Uncontrolled Diabetes and Corticosteroids-An Unholy Trinity in Invasive Fungal Infections of the Maxillofacial Region? A Retrospective, Multi-centric Analysis. J Maxillofac Oral Surg 2021;20(3):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ismaiel WF, Abdelazim MH, Eldsoky I, et al. The impact of COVID-19 outbreak on the incidence of acute invasive fungal rhinosinusitis. Am J Otolaryngol 2021;42(6):103080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Monte Junior ESD, Santos MELD, Ribeiro IB, et al. Rare and Fatal Gastrointestinal Mucormycosis (Zygomycosis) in a COVID-19 Patient: A Case Report. Clin Endosc 2020;53(6):746–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Waizel-Haiat S, Guerrero-Paz JA, Sanchez-Hurtado L, Calleja-Alarcon S, Romero-Gutierrez L. A Case of Fatal Rhino-Orbital Mucormycosis Associated With New Onset Diabetic Ketoacidosis and COVID-19. Cureus 2021;13(2):e13163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meshram HS, Kute VB, Chauhan S, Desai S. Mucormycosis in post-COVID-19 renal transplant patients: A lethal complication in follow-up. Transpl Infect Dis 2021. 10.1111/tid.13663. Published online June 3, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alekseyev K, Didenko L, Chaudhry B. Rhinocerebral Mucormycosis and COVID-19 Pneumonia. J Med Cases 2021;12(3):85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sen M, Lahane S, Lahane TP, Parekh R, Honavar SG. Mucor in a Viral Land: A Tale of Two Pathogens. Indian J Ophthalmol 2021;69(2):244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rao R, Shetty AP, Nagesh CP. Orbital infarction syndrome secondary to rhino-orbital mucormycosis in a case of COVID-19: Clinico-radiological features. Indian J Ophthalmol 2021;69(6):1627–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. El-Kholy NA, El-Fattah AMA, Khafagy YW. Invasive fungal sinusitis in post COVID-19 patients: a new clinical entity. Laryngoscope 2021. 10.1002/lary.29632. Published online May 19, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sai Krishna D, Raj H, Kurup P, Juneja M. Maxillofacial Infections in Covid-19 Era-Actuality or the Unforeseen: 2 Case Reports. Indian J Otolaryngol Head Neck Surg 2021;1-4:1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Revannavar SM, P S S, Samaga L, v K V. COVID-19 triggering mucormycosis in a susceptible patient: a new phenomenon in the developing world? BMJ Case Rep 2021;14(4):e241663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Veisi A, Bagheri A, Eshaghi M, Rikhtehgar MH, Rezaei Kanavi M, Farjad R. Rhino-orbital mucormycosis during steroid therapy in COVID-19 patients: A case report. Eur J Ophthalmol 2021. 10.1177/11206721211009450. Published online April 10, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pakdel F, Ahmadikia K, Salehi M, et al. Mucormycosis in patients with COVID-19: A cross-sectional descriptive multicentre study from Iran. Mycoses 2021. 10.1111/myc.13334. Published online June 7, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Khatri A, Chang KM, Berlinrut I, Wallach F. Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient - Case report and review of literature. J Mycol Med 2021;31(2):101125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Karimi-Galougahi M, Arastou S, Haseli S. Fulminant mucormycosis complicating coronavirus disease 2019 (COVID-19). Int Forum Allergy Rhinol 2021;11(6):1029–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ahmadikia K, Hashemi SJ, Khodavaisy S, et al. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: A case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses 2021;64(8):798–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am J Emerg Med 2021;42:264.e5–264.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sarkar S, Gokhale T, Choudhury SS, Deb AK. COVID-19 and orbital mucormycosis. Indian J Ophthalmol 2021;69(4):1002–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nehara HR, Puri I, Singhal V, Ih S, Bishnoi BR, Sirohi P. Rhinocerebral mucormycosis in COVID-19 patient with diabetes a deadly trio: Case series from the north-western part of India. Indian J Med Microbiol 2021;39(3):380–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dallalzadeh LO, Ozzello DJ, Liu CY, Kikkawa DO, Korn BS. Secondary infection with rhino-orbital cerebral mucormycosis associated with COVID-19. Orbit 2021;1-4:1-4. [DOI] [PubMed] [Google Scholar]
- 28. Mehta S, Pandey A. Rhino-Orbital Mucormycosis Associated With COVID-19. Cureus 2020;12(9):e10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson AK, Ghazarian Z, Cendrowski KD, Persichino JG. Pulmonary aspergillosis and mucormycosis in a patient with COVID-19. Med Mycol Case Rep 2021;32:64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zurl C, Hoenigl M, Schulz E, et al. Autopsy Proven Pulmonary Mucormycosis Due to Rhizopus microsporus in a Critically Ill COVID-19 Patient with Underlying Hematological Malignancy. J Fungi (Basel) 2021;7(2):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bellanger AP, Navellou JC, Lepiller Q, et al. Mixed mold infection with Aspergillus fumigatus and Rhizopus microsporus in a severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) patient. Infect Dis Now 2021. 10.1016/j.idnow.2021.01.010. Published online January 27, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Placik DA, Taylor WL, Wnuk NM. Bronchopleural fistula development in the setting of novel therapies for acute respiratory distress syndrome in SARS-CoV-2 pneumonia. Radiol Case Rep 2020;15(11):2378–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rabagliati R, Rodríguez N, Núñez C, Huete A, Bravo S, Garcia P. COVID-19-Associated Mold Infection in Critically Ill Patients, Chile. Emerg Infect Dis 2021;27(5):1454–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hanley B, Naresh KN, Roufosse C, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe 2020;1(6):e245–e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kanwar A, Jordan A, Olewiler S, Wehberg K, Cortes M, Jackson BR. A Fatal Case of Rhizopus azygosporus Pneumonia Following COVID-19. J Fungi (Basel) 2021;7(3):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Garg D, Muthu V, Sehgal IS, et al. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM):. Case Report and Systematic Review of Literature. Mycopathologia 2021;186(2):289–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pasero D, Sanna S, Liperi C, et al. A challenging complication following SARS-CoV-2 infection: a case of pulmonary mucormycosis. Infection 2020. 10.1007/s15010-020-01561-x. Published online December 17, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Krishna V, Morjaria J, Jalandari R, Omar F, Kaul S. Autoptic identification of disseminated mucormycosis in a young male presenting with cerebrovascular event, multi-organ dysfunction and COVID-19 infection. IDCases 2021;25:e01172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patel A, Agarwal R, Rudramurthy SM, et al. Multicenter Epidemiologic Study of Coronavirus Disease-Associated Mucormycosis, India. Emerg Infect Dis 2021;27(9):2349–2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rudramurthy SM, Hoenigl M, Meis JF, et al. ECMM/ISHAM recommendations for clinical management of COVID-19 associated mucormycosis in low- and middle-income countries. Mycoses 2021;64(9):1028–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nam BD, Kim TJ, Lee KS, Kim TS, Han J, Chung MJ. Pulmonary mucormycosis: serial morphologic changes on computed tomography correlate with clinical and pathologic findings. Eur Radiol 2018;28(2):788–795. [DOI] [PubMed] [Google Scholar]
- 42. Jamadar DA, Kazerooni EA, Daly BD, White CS, Gross BH. Pulmonary zygomycosis: CT appearance. J Comput Assist Tomogr 1995;19(5):733–738. [DOI] [PubMed] [Google Scholar]