Abstract
Background and purpose
Whether the off-hour effect has an impact on workflow and outcomes of endovascular treatment (EVT) for anterior circulation large vessel occlusion (AC-LVO) remains uncertain. This study aimed to compare the characteristics and outcomes of patients who presented or were treated during off-hour versus on-hour in a multi-center registry.
Methods
AC-LVO patients from 21 centres were categorised into the off-hour group and the on-hour group. Off-hour (weekends, holidays, and 18:00–7:59 on weekdays) and on-hour (8:00–17:59 on weekdays except for holidays) were defined according to arrival and groin-puncture time points, respectively. Subgroup comparisons between patients both arrived and treated during off-hour (true off-hour) and on-hour (true on-hour) were performed. The primary outcome was the 90-day modified Rankin Scale (mRS) score. Secondary outcomes included favourable outcome (mRS 0–2 at 90 days), EVT-related time metrics, and other clinical outcomes. Ordinary and binary logistic regression and linear regression were taken to adjust for confounding factors.
Results
Of all 698 patients enrolled, 435 (62.3%) and 456 (65.3%) patients were categorised into the off-hour arrival and off-hour puncture group, respectively. Shorter onset to door time (adjusted ß coefficient: −21.56; 95% CI −39.96 to −3.16; p=0.022) was noted in the off-hour arrival group. Ordinal and dichotomous mRS scores at 90 days were comparable between the off-hour group and the on-hour group regardless of off-hour definitions. Other time metrics and outcomes were comparable between the two groups. Of 595 patients both presented and were treated during off-hour or on-hour, 394 patients were categorised into the true off-hour group and 201 into the true on-hour group. Time metrics and clinical outcomes were similar between the true off-hour and the true on-hour group.
Conclusions
The off-hour effect was not significant regarding clinical outcomes and in-hospital workflow in AC-LVO patients receiving EVT in this Chinese multicentre registry.
Keywords: stroke, thrombectomy
Introduction
Patients presenting or getting treated outside working hours (off-hour) are prevalent in clinical practice.1–3 Patients with different diseases admitted to hospitals during off-hour are associated with higher risks of mortality than patients admitted during regular working hours (on-hour).4 The off-hour effect might be partly explained by the absence of timely attending, delayed interventions, lower hospital staffing levels and lower quality of medical resources.5–9 Theoretically, the off-hour effect might be more significant in conditions that are more sensitive to the rapid availability of specialised medical care.7
Endovascular treatment (EVT) has been established as the golden standard of treating acute ischaemic stroke with anterior circulation large vessel occlusion (AC-LVO).10 The effectiveness of EVT is time dependent,11 and fast reperfusion leads to improved functional outcomes.12 Investigations on the off-hour effect on EVT workflow and clinical outcomes are limited, and the existing results have been conflicting.1 13–18 The definition of off-hour varies in different studies.19 Some studies define the off-hour group according to arrival time,2 13–15 17 20–23 and some according to groin-puncture time.1 3 16 18 24–26 Whether the effect will change or not when grouped by different reference time point remains uncertain. Moreover, investigation on this issue in the Chinese population is scarce. Thus, we performed a retrospective study to explore the potential off-hour effect on EVT in AC-LVO patients in a multicentre registry.
Methods
Patient selection
This study was a retrospective analysis of the acute anterior circulation ischaemic stroke registry (ACTUAL). Between January 2014 and June 2016, 698 consecutive AC-LVO patients were enrolled from 21 comprehensive stroke centres in China. Detailed descriptions on this registry have been published previously.27 Patients were enrolled after fulfilling the inclusion criteria: (1) age ≥18 years; (2) were diagnosed as acute ischaemic stroke; (3) had angiographically proven (CT angiography/magnetic resonance angiography/digital subtraction angiography) AC-LVO; (4) underwent EVT. Patients treated with intra-arterial thrombolysis alone or diagnosed with a concomitant aneurysm, arteriovenous malformation or posterior circulation occlusion were excluded to maintain the homogeneity. The ACTUAL study was approved by the ethics committee of each participating centre.
Treatment protocol
Neurointerventional teams in all participating centres were capable of providing potential EVTs across the 7-day week including nights and national holidays. All enrolled patients were treated following contemporary guidelines. Patients received intravenous thrombolysis within 4.5 hours since stroke onset after excluding contradictions. Thrombectomy was performed with a stent-like retriever (Solitaire, Covidien, Irvine, California, USA) in most patients via a transfemoral approach, with other devices permitted. Rescue therapies including balloon angioplasty, stenting, intraarterial thrombolysis and intraarterial tirofiban administration were performed at the discretions of neurointerventionalists.
Definitions and group divisions
Off-hour was defined as weekends, Chinese national holidays and 18:00–7:59 on weekdays. On-hour was defined as regular working hours between 8:00 and 17:59 on weekdays except for holidays.21 Patients were categorised into the off-hour group and the on-hour group, and off-hour was defined according to arrival time (arrival mode) and groin-puncture time (puncture mode), respectively. Some patients presented during off-hour but were treated during on-hour, and some vice versa. The true off-hour group was defined when patients arrived and treated both during off-hour. Patients who arrived and got punctured both during on-hour were defined as the true on-hour group. Comparisons between the true off-hour group and the true on-hour group were performed to explore the off-hour effect thoroughly.
Data collection
Demographics, medical histories, baseline National Institutes of Health Stroke Scale (NIHSS) score, baseline Alberta Stroke Program Early CT Score (ASPECTS), time metrics, and clinical outcomes were collected. Time metrics were calculated according to medical records and automatic time stamps on images and digital subtraction angiography documents. Onset to door time (OTD) was defined as the time interval from stroke symptom onset to emergency department arrival. Door to imaging (DTI) time was defined as the time interval between patient arrival and imaging results acquired. Onset to puncture (OTP) time and door to puncture (DTP) were defined as the time interval from symptom onset to groin-puncture and patient-arrival to groin-puncture, respectively. Puncture to reperfusion (PTR) was referred to the time interval between groin-puncture and successful reperfusion. If reperfusion failed, PTR was regarded as the time interval from groin-puncture to the ending of EVT. Time from symptom onset to reperfusion (OTR) was also calculated.
Clinical outcomes
Reperfusion status was evaluated according to the modified Thrombolysis In Cerebral Infarction (mTICI) Scale, and successful reperfusion was defined as a mTICI score of 2b-3.28 Post-EVT intracranial haemorrhages (ICH) were recorded and analysed. Symptomatic ICH (sICH) and asymptomatic ICH (aICH) were evaluated according to the Heidelberg criteria.29 Collateral flow grading was estimated through the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) grading system.30 All angiographic data were sent to a core laboratory in Jinling Hospital. The size of ICH, collateral flow grading and preprocedure and postprocedure mTICI were evaluated blindly by two physicians/interventionists with advice from the third experienced physician/interventionist in case of disagreement.27 Modified Rankin Scale (mRS) scores at 90 days were followed up by the outpatient clinic or telephone. The primary outcome was 90-day mRS score. Secondary outcomes included favourable outcome (mRS 0–2 at 90 days), successful reperfusion, time metrics, sICH, aICH, mortality in hospital and mortality at 90 days.
Statistical analyses
Multiple imputations with chain equations were performed to account for missing values (glucose level: 7.02%; atrial fibrillation: 0.14%; ASPECTS: 3.72%; ASITN/SIR grade: 0.86%; DTI time: 1.29%; PTR: 1.00%; OTR: 0.86%). Categorical variables were expressed as numbers (percentages). Continuous variables were displayed as means (SD) or medians (IQR) according to the normality of data distributions. Univariate analysis was performed between the off-hour group and the on-hour group by using t-test, Mann-Whitney U test, χ2 test or Fisher exact test as appropriate.
The on-hour group was set as the reference in multivariable regressions. Ordinary logistic regression (shift analysis) was taken to analyse differences in the 90-day mRS score between the off-hour group and the on-hour group. Linear regression and binary logistic regression were taken to compare time metrics and binary clinical outcomes between the two groups, respectively.2 In different off-hour modes, time metrics were adjusted for baseline variables with statistical trends (p<0.1 on univariate analyses). Other clinical outcomes were adjusted for baseline variables with statistical trends, OTD time and other time metrics with statistical trends. A two-sided p<0.05 was considered statistically significant. Analyses were performed using the SPSS software package, V.22.0 (IBM) and R V.3.6.3 (R Core Team (2020). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Results
Overview
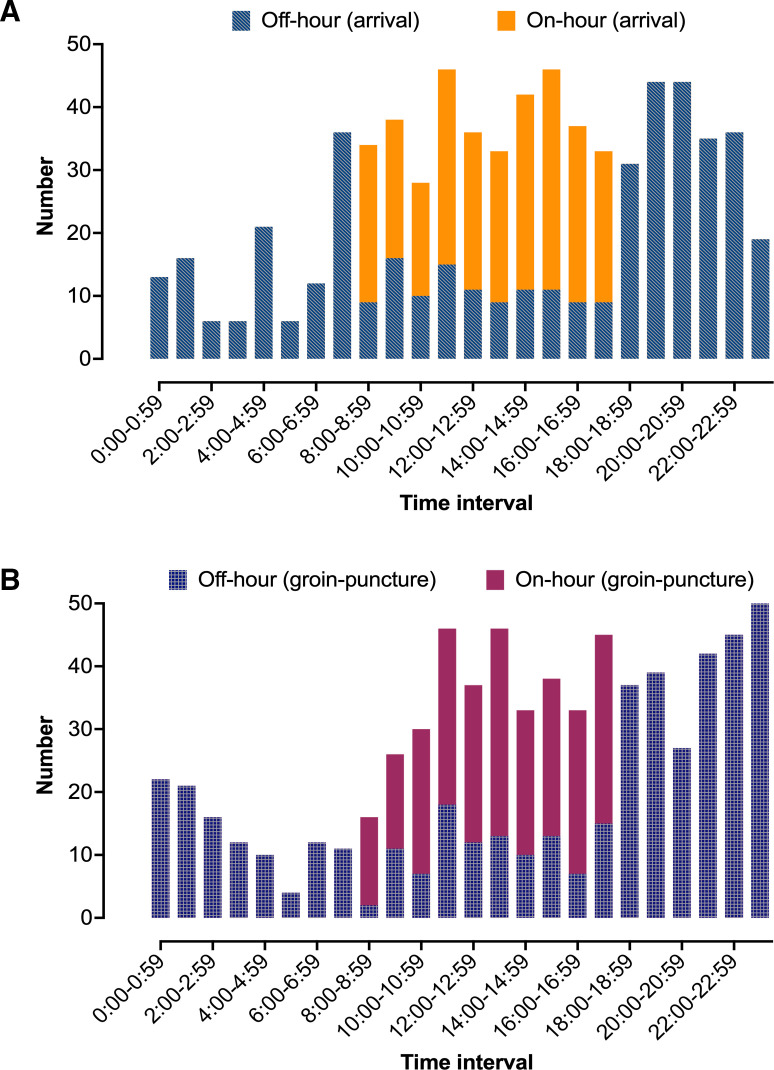
Of all 698 patients enrolled in the ACTUAL registry, the median (IQR) age was 66 (57–74) years old, and men accounted for 60.6% (423/698). The median (IQR) admission NIHSS score and ASPECTS were 16.0 (12.0–21.0) and 9.0 (8.0–10.0), respectively. Two hundred and twenty-nine (32.8%) patients received intravenous thrombolysis. The median OTD, DTI, DTP, PTR, OTP and OTR time metrics were 125.0, 23.0, 125.0, 100.0, 271.5 and 380.5 min, respectively. Four hundred and thirty-five (62.3%) patients were categorised into the off-hour group and 263 (37.7%) patients into the on-hour group in the arrival mode. Four hundred and fifty-six (65.3%) patients were categorised into the off-hour group and 242 (34.7%) patients were into the on-hour group in the puncture mode. Arrival and puncture times across all days are illustrated in figure 1. Patients who arrived or were treated in the afternoon/evening were more prevalent than those in the morning in both modes. A total of 579 (83.0%) patients reached successful reperfusion. Two hundred and eighteen (31.2%) patients were diagnosed as aICH and 108 (15.5%) as sICH. The median (IQR) mRS score at 90 days was 3 (1–6). At 90 days, 304 (43.6%) patients had favourable outcomes.
Figure 1.
Distributions of arrival and groin-puncture times across all days: (A) arrival mode; (B) puncture mode.
Baseline characteristics
Table 1 shows comparisons on the baseline characteristics and clinical outcomes between the off-hour group and the on-hour group in different modes. Male sex was much more prevalent in the off-hour arrival group (64.8% vs 53.6%, p=0.003). Admission glucose level was significantly higher in the off-hour puncture group (median: 6.8 mmol/L vs 6.4 mmol/L, p=0.024). No other statistical difference in baseline characteristics was noted between the off-hour group and the on-hour group.
Table 1.
Demographics and clinical outcomes between the off-hour group and the on-hour group
| Variable | Defined off-hour with arrival time (arrival mode) | P value | Defined off-hour with groin-puncture time (puncture mode) | P value | ||
| Off-hour n=435 | On-hour n=263 | Off-hour n=456 | On-hour n=242 | |||
| Age, year, median (IQR) | 65.0 (57.0–73.0) | 66.0 (56.0–75.0) | 0.587 | 65.0 (57.0–73.0) | 66.0 (56.0–75.0) | 0.831 |
| Male, n (%) | 282 (64.8) | 141 (53.6) | 0.003 | 285 (62.5) | 138 (57.0) | 0.159 |
| SBP, mm Hg, median (IQR) | 145.0 (130.0–160.0) | 146.0 (129.0–160.0) | 0.624 | 145.0 (130.0–160.8) | 145.0 (127.5–160.0) | 0.474 |
| DBP, mm Hg, median (IQR) | 82.0 (76.0–92.0) | 83.0 (74.0–93.0) | 0.697 | 83.0 (76.0–92.0) | 80.0 (72.0–93.0) | 0.079 |
| Glucose, mmol/L, median (IQR) | 6.8 (5.8–8.6) | 6.5 (5.5–8.6) | 0.082 | 6.8 (5.8–8.6) | 6.4 (5.5–8.4) | 0.024 |
| Medical history, n (%) | ||||||
| Atrial fibrillation | 177 (40.7) | 111 (42.2) | 0.693 | 189 (41.4) | 99 (40.9) | 0.891 |
| Hypertension | 278 (63.9) | 164 (62.4) | 0.680 | 290 (63.6) | 152 (62.8) | 0.837 |
| Diabetes | 80 (18.4) | 48 (18.3) | 0.963 | 85 (18.6) | 43 (17.8) | 0.777 |
| Current smoking, n (%) | 123 (28.3) | 61 (23.2) | 0.140 | 131 (28.7) | 53 (21.9) | 0.051 |
| ASPECTS, median (IQR) | 9.0 (8.0–10.0) | 9.0 (8.0–10.0) | 0.932 | 9.0 (8.0–10.0) | 9.0 (8.0–10.0) | 0.925 |
| Baseline NIHSS, median (IQR) | 16.0 (12.0–20.0) | 17.0 (12.0–21.0) | 0.154 | 16.0 (12.0–20.0) | 17.0 (12.0–21.0) | 0.071 |
| Intravenous thrombolysis, n (%) | 153 (35.2) | 76 (28.9) | 0.087 | 158 (34.6) | 71 (29.3) | 0.155 |
| Local anaesthesia, n (%) | 358 (82.3) | 202 (76.8) | 0.077 | 373 (81.8) | 187 (77.3) | 0.153 |
| Stroke aetiology, n (%) | 0.669 | 0.950 | ||||
| LAA | 191 (43.9) | 118 (44.9) | 202 (44.3) | 107 (44.2) | ||
| CE | 216 (49.7) | 124 (47.1) | 223 (48.9) | 117 (48.3) | ||
| Others | 28 (6.4) | 21 (8.0) | 31 (6.8) | 18 (7.4) | ||
| ICA occlusion, n (%) | 174 (40.0) | 107 (40.7) | 0.858 | 187 (41.0) | 94 (38.8) | 0.579 |
| MCA occlusion, n (%) | 257 (59.1) | 154 (58.6) | 0.891 | 264 (57.9) | 147 (60.7) | 0.467 |
| ASITN/SIR 0–1, n (%) | 221 (50.8) | 117 (44.5) | 0.106 | 226 (49.6) | 112 (46.3) | 0.409 |
| Onset to door, min, median (IQR) | 120.0 (60.0–212.0) | 140.0 (64.0–240.0) | 0.047 | 125.0 (60.0–220.0) | 127.0 (63.5–232.5) | 0.542 |
| Door to imaging, min, median (IQR) | 23.0 (12.0–33.0) | 24.0 (13.0–32.0) | 0.940 | 23.0 (12.0–34.0) | 24.0 (15.0–32.0) | 0.885 |
| Door to puncture, min, median (IQR) | 128.0 (84.0–177.0) | 125.0 (80.0–172.0) | 0.597 | 130.0 (86.3–177.0) | 120.0 (75.0–165.0) | 0.161 |
| Puncture to reperfusion, min, median (IQR) | 100.0 (72.0–145.0) | 101.0 (77.0–138.0) | 0.858 | 99.5 (70.0–140.8) | 103.0 (79.8–143.5) | 0.235 |
| Onset to puncture, min, median (IQR) | 266.0 (201.0–345.0) | 285.0 (210.0–360.0) | 0.098 | 273.5 (204.3–349.5) | 270.5 (210.0–360.0) | 0.711 |
| Onset to reperfusion, min, median (IQR) | 380.0 (299.0–470.0) | 383.0 (310.0–488.0) | 0.393 | 382.0 (299.0–470.0) | 380.5 (313.0–488.5) | 0.656 |
| Successful reperfusion, n (%) | 361 (83.0) | 218 (82.9) | 0.973 | 378 (82.9) | 201 (83.1) | 0.957 |
| Symptomatic ICH, n (%) | 69 (15.9) | 39 (14.8) | 0.715 | 74 (16.2) | 34 (14.0) | 0.449 |
| Asymptomatic ICH, n (%) | 140 (32.2) | 78 (29.7) | 0.485 | 144 (31.6) | 74 (30.6) | 0.786 |
| Mortality in hospital, n (%) | 104 (23.9) | 59 (22.4) | 0.655 | 110 (24.1) | 53 (21.9) | 0.509 |
| mRS score at 90 days, median (IQR) | 3 (1–6) | 3 (1–6) | 0.624 | 3 (1–6) | 3 (2–6) | 0.549 |
| Favourable outcome, n (%) | 190 (43.7) | 114 (43.3) | 0.932 | 200 (43.9) | 104 (43.0) | 0.823 |
| Mortality at 90 days, n (%) | 109 (25.1) | 68 (25.9) | 0.814 | 116 (25.4) | 61 (25.2) | 0.947 |
ASITN/SIR, American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology; ASPECTS, Alberta Stroke Program Early CT Score; CE, cardioembolism; DBP, diastolic blood pressure; ICA, intracranial artery; ICH, intracranial haemorrhage; LAA, large-artery atherosclerosis; MCA, middle cerebral artery; mRS, modified Rankin Scale; NIHSS, National Institute of Health Stroke Scale; SBP, systolic blood pressure.
Clinical outcomes
In univariate analysis, mRS scores at 90 days were comparable between the off-hour arrival group and the on-hour arrival group (median: 3 vs 3; p=0.624). The OTD time was significantly shorter in the off-hour arrival group (120.0 min vs 140.0 min, p=0.047). Other EVT-related time metrics and clinical outcomes including successful reperfusion, favourable outcome, sICH, aICH, mortality in hospital and mortality at 90 days were comparable between the two groups (table 1). In the puncture mode, there was no significant difference concerning all clinical outcomes between the off-hour and on-hour presentations. Figure 2 illustrates distributions of mRS scores in different modes.
Figure 2.
Distributions of modified Rankin Scale scores in the on-hour group and the off-hour group in different definitions: (A) on-hour arrival versus off-hour arrival; (B) on-hour puncture versus off-hour puncture; (c) true on-hour versus true off-hour.
In multivariable analyses, OTD was significantly shorter in the off-hour arrival group after adjusting for covariates (adjusted ß coefficient: −21.56 min; 95% CI −39.96 to −3.16 min; p=0.022). Ordinary logistic regression indicated that the 90-day mRS scores remained comparable between the two groups in arrival mode (common OR: 0.98; 95% CI 0.74 to 1.29; p=0.881) and puncture mode (common OR: 0.96; 95% CI 0.72 to 1.28; p=0.792). No significant difference was found regarding other time metrics and clinical outcomes between the off-hour group and the on-hour group in both arrival and puncture modes (table 2).
Table 2.
Analyses on the off-hour effect regarding time metrics and clinical outcomes
| Variable | Defined off-hour with arrival time (arrival mode) |
Adjusted p value | Defined off-hour with puncture time (puncture mode) |
Adjusted p value | ||
| Unadjusted ß coefficient/OR (95% CI) | Adjusted ß coefficient/OR (95% CI) * | Unadjusted ß coefficient/OR (95% CI) | Adjusted ß coefficient/OR (95% CI) † | |||
| Onset to door time | −20.91 (–39.52 to –2.30) | −21.56 (–39.96 to –3.16) | 0.022 | −3.41 (–22.43 to 15.60) | −3.20 (–22.40 to 16.00) | 0.744 |
| Door to imaging time | −0.97 (–4.86 to 2.91) | −0.82 (–4.76 to 3.12) | 0.682 | −1.51 (–5.46 to 2.44) | −1.28 (–5.27 to 2.71) | 0.529 |
| Door to puncture time | 6.06 (–7.53 to 19.65) | 6.95 (–6.70 to 20.60) | 0.318 | 4.21 (–9.63 to 18.05) | 2.26 (–11.64 to 16.16) | 0.749 |
| Puncture to reperfusion | 2.74 (–6.65 to 12.13) | 3.50 (–5.88 to 12.87) | 0.464 | −3.58 (–13.14 to 5.98) | −4.899 (–14.54 to 4.74) | 0.319 |
| Onset to puncture time | −14.85 (–35.30 to 5.60) | −14.61 (–35.12 to 5.89) | 0.162 | 0.80 (–20.06 to 21.65) | −0.94 (–21.95 to 20.07) | 0.930 |
| Onset to reperfusion time | −12.21 (–35.20 to 10.78) | −11.36 (–34.44 to 11.72) | 0.334 | −4.75 (–28.17 to 18.67) | −7.75 (–31.36 to 15.86) | 0.520 |
| Successful reperfusion | 1.01 (0.67 to 1.51) | 0.96 (0.63 to 1.46) | 0.838 | 0.99 (0.65 to 1.50) | 0.96 (0.63 to 1.47) | 0.853 |
| Symptomatic ICH | 1.08 (0.71 to 1.66) | 1.14 (0.73 to 1.76) | 0.569 | 1.18 (0.76 to 1.84) | 1.18 (0.75 to 1.85) | 0.473 |
| Asymptomatic ICH | 1.13 (0.81 to 1.57) | 1.13 (0.80 to 1.59) | 0.480 | 1.05 (0.75 to 1.47) | 1.10 (0.78 to 1.55) | 0.587 |
| Mortality in hospital | 1.09 (0.76 to 1.56) | 1.14 (0.78 to 1.67) | 0.494 | 1.13 (0.78 to 1.65) | 1.23 (0.82 to 1.86) | 0.316 |
| 90-day mRS score (shift analysis) | 0.94 (0.71 to 1.22) | 0.98 (0.74 to 1.29) | 0.881 | 0.92 (0.70 to 1.21) | 0.96 (0.72 to 1.28) | 0.792 |
| Favourable outcome | 1.01 (0.74 to 1.38) | 0.96 (0.70 to 1.33) | 0.808 | 1.04 (0.76 to 1.42) | 1.00 (0.70 to 1.42) | 0.994 |
| Mortality at 90 days | 0.96 (0.68 to 1.36) | 1.01 (0.70 to 1.46) | 0.964 | 1.01 (0.71 to 1.45) | 1.07 (0.72 to 1.59) | 0.722 |
Reference: patients who presented or get treated during the on-hour period.
*Time metrics were adjusted for gender, glucose level, intravenous thrombolysis and local anaesthesia. Other clinical outcomes were adjusted for gender, glucose level, intravenous thrombolysis, local anaesthesia, onset to door time and onset to puncture time.
†Time metrics were adjusted for diastolic blood pressure, glucose level, current smoking and baseline National Institute of Health Stroke Scale (NIHSS) score. Other clinical outcomes were adjusted for diastolic blood pressure, glucose level, current smoking, baseline NIHSS score and onset to door time.
ICH, intracranial haemorrhage; mRS, modified Rankin Scale.;
Subgroup analysis
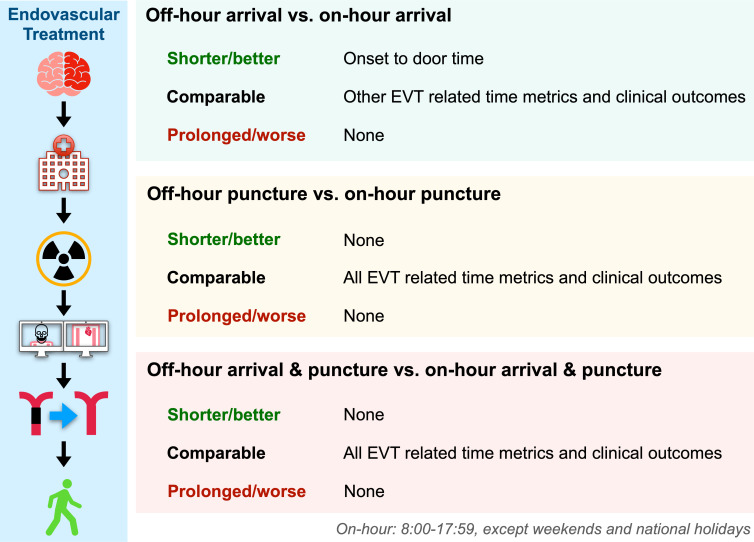
Of 595 patients who presented and were treated during the same period (both during off-hour or during on-hour), 394 patients were categorised into the true off-hour group and 201 into the true on-hour group. Baseline characteristics between the two groups were shown in online supplemental table 1. A trend towards a longer DTP time metric was witnessed in the true off-hour group (median: 125.0 min vs 116.0 min; adjusted ß coefficient: 12.17 min; 95% CI −1.20 to 25.55; p=0.074). No significant difference in other time metrics and clinical outcomes was noted between the two groups (table 3). The summary of this research is illustrated in figure 3.
Table 3.
Time metrics and clinical outcomes between the true off-hour group and the true on-hour group
| Variable | Overall n=595 | True off-hour n=394 | True on-hour n=201 | Adjusted ß coefficient/OR (95% CI)* | P value |
| Onset to door, min, median (IQR) | 131.0 (60.0–230.0) | 124.5 (60.0–218.2) | 146.0 (73.5–240.0) | −15.56 (−35.78 to 4.65) | 0.131 |
| Door to imaging, min, median (IQR) | 22.0 (12.0–32.0) | 22.0 (11.8–32.2) | 23.0 (12.0–30.5) | −0.37 (−4.30 to 3.56) | 0.855 |
| Door to puncture, min, median (IQR) | 120.0 (76.0–164.0) | 125.0 (80.0–170.2) | 116.0 (67.0–150.0) | 12.17 (−1.20 to 25.55) | 0.074 |
| Puncture to reperfusion, min, median (IQR) | 100.0 (74.0–143.0) | 100.0 (71.0–144.2) | 103.0 (78.5–140.5) | −0.57 (−10.93 to 9.79) | 0.914 |
| Onset to puncture, min, median (IQR) | 270.0 (203.0–348.0) | 265.5 (200.0–345.0) | 271.0 (210.0–359.0) | −3.39 (−24.78 to 17.99) | 0.755 |
| Onset to reperfusion, min, median (IQR) | 374.0 (300.0–470.0) | 374.5 (294.0–463.8) | 372.0 (312.0–485.5) | −5.10 (−29.14 to 18.94) | 0.677 |
| Successful reperfusion, n (%) | 494 (83.0) | 327 (83.0) | 167 (83.1) | 0.96 (0.60 to 1.54) | 0.878 |
| Symptomatic ICH, n (%) | 95 (16.0) | 65 (16.5) | 30 (14.9) | 1.20 (0.73 to 1.95) | 0.474 |
| Asymptomatic ICH, n (%) | 186 (31.3) | 126 (32.0) | 60 (29.9) | 1.13 (0.77 to 1.65) | 0.525 |
| Mortality in hospital, n (%) | 141 (23.7) | 96 (24.4) | 45 (22.4) | 1.28 (0.82 to 2.00) | 0.281 |
| 90-day mRS score, median (IQR) | 3.0 (1.0–6.0) | 3.0 (1.0–6.0) | 3.0 (2.0–6.0) | 0.97 (0.71 to 1.32) | 0.848 |
| Favourable outcome, n (%) | 252 (42.4) | 169 (42.9) | 83 (41.3) | 0.95 (0.65 to 1.40) | 0.790 |
| Mortality at 90 days, n (%) | 154 (25.9) | 101 (25.6) | 53 (26.4) | 1.09 (0.71 to 1.67) | 0.692 |
Reference: patients who presented or get treated during the on-hour period.
*Time metrics were adjusted for gender, glucose level, current smoking, baseline National Institute of Health Stroke Scale (NIHSS) score, intravenous thrombolysis, local anaesthesia. Other clinical outcomes were adjusted for gender, glucose level, current smoking, baseline NIHSS score, intravenous thrombolysis, local anaesthesia, onset to door time and door to puncture time.
ICH, intracranial haemorrhage; mRS, modified Rankin Scale.;
Figure 3.
The central illustration of this study. EVT, endovascular treatment.
svn-2021-000949supp001.pdf (101KB, pdf)
Discussions
This multicentre study demonstrated that the prehospital time metric (OTD time) was shorter in patients presented during the off-hour period. However, off-hour arrival/treatment did not influence in-hospital workflow and clinical outcomes.
Qualities of stroke care might not be consistent in different periods throughout the day. A majority of stroke patients are proved to arrive at hospitals outside working hours.3 17 18 25 Potential deleterious effects of off-hour might include longer preparation times for EVT staff, increased procedural time and staff fatigue.3 9 Thus, it is of great importance to investigate this effect on EVT workflow and outcomes, and identify the specific process on which interventions should be targeted.
Our results revealed that the 90-day mRS score and other clinical outcomes were not influenced by the arrival/groin-puncture time before and after adjusting for confounders, which was in line with previous research.1 2 17 18 Almallouhi et al demonstrate that off-hour EVT is associated with poor functional outcome, possibly owing to the significantly higher baseline NIHSS scores in the off-hour group.16 A recent study indicates that patients treated during nighttime hours achieve favourable clinical outcomes more frequently and have lower in-hospital mortality rates than those treated during daytime hours. But the relatively small sample might cause potential bias.31 Comparable clinical outcomes between the off-hour group and the on-hour group in our study might be explained by following reasons. First, EVT-related time metrics, successful reperfusion rates and ICH rates were similar between the two groups. Second, EVT has been widely recommended since the publication of several randomised clinical trials.32–36 EVT centres are expected to be fully resourced and staffed independent of working hours. Third, all centres enrolled in this study were comprehensive stroke centres. A previous study has proved that comprehensive stroke centres may ameliorate the off-hour effect in patients with stroke due to the 24/7 availability of stroke specialists.37
Interestingly, the OTD time was significantly shorter during off-hour in the arrival mode after adjusting for confounding factors, but other time metrics remained comparable between the off-hour group and the on-hour group in all three modes. We hypothesised that this phenomenon might be related to less traffic outside working hours although without relevant evidence. In previous studies, off-hour arrival/treatment is proved to be associated with longer onset to imaging time,1 22 longer door to reperfusion time13 and longer door to needle time.17 A recent meta-analysis also indicates that off-hour is associated with prevalent delays before EVT.19 But some studies indicate that pre-EVT time metrics are not influenced by the off-hour effect.14 15 Disparities in time metrics might result from the differences in EVT workflows in various stroke centres and heterogeneous definitions of off-hour. According to our experience, EVT teams tend to stay in the hospital in response to the potential emergent thrombectomy outside working hours in China, whereas neurointerventional teams at some centres from other countries are often ‘on-call’ from home for potential endovascular intervention during nights/weekends,3 16 25 which may cause procedural delays. The locations of the on-call neurointerventional team might account for disparities in time metrics and clinical outcomes to some extent. Further investigations on this issue are needed to provide more direct evidence.
The strengths of this study included multicentre design, detailed classifications and efforts in controlling confounding factors. To our knowledge, evidence on the off-hour effect in EVT for acute AC-LVO in the Chinese population is scarce. Considering the limited number of senior medical staff on the national holiday, we also categorised national holidays into the off-hour group to reduce heterogenicity. Apart from the strengths mentioned above, several weaknesses of this study were also noteworthy. First, our study was limited by its retrospective nature. Second, the ACTUAL registry could not perfectly represent contemporary EVT considering the investigation date (2014–2016). Third, data on staffing levels and quality of medical resources were absent in our study. Taking all these factors into consideration, this study still provided valuable information on this research area of uncertainty.
Conclusions
AC-LVO patients who arrived at hospitals outside working hours and underwent EVT were associated with shorter OTD time comparing with the on-hour population. But the potential hazardous off-hour effect was not evident regarding in-hospital workflow and clinical outcomes.
Acknowledgments
We sincerely thanked all efforts made by ACTUAL investigators.
Footnotes
MZ, QY and SL contributed equally.
DY and XL contributed equally.
Contributors: Study design, analysis and data interpretation: MZ, QY, SL, DY, XL. Data collection: DY, XL. Drafting and modification of the manuscript: MZ, QY, SL, DY, XZ, KH, HC, MW, QL, RL, XL. Contributed to the article and approved the submitted version: all authors.
Funding: This study was partly supported by the National Nature and Science Foundation (Grant No. 81901218, 81870946, 81530038, and 81701299).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The central ethics committee at Jinling Hospital and the ethics committee of each participating center approved this registry.
References
- 1. Almekhlafi MA, Hockley A, Desai JA, et al. Overcoming the evening/weekend effects on time delays and outcomes of endovascular stroke therapy: the Calgary stroke program experience. J Neurointerv Surg 2014;6:729–32. 10.1136/neurintsurg-2013-011000 [DOI] [PubMed] [Google Scholar]
- 2. Hinsenveld WH, de Ridder IR, van Oostenbrugge RJ, et al. Workflow intervals of endovascular acute stroke therapy during on- versus off-hours: the Mr clean registry. Stroke 2019;50:2842–50. 10.1161/STROKEAHA.119.025381 [DOI] [PubMed] [Google Scholar]
- 3. Tschoe C, Kittel C, Brown P, et al. Impact of off-hour endovascular therapy on outcomes for acute ischemic stroke: insights from StAR. J Neurointerv Surg 2020. 10.1136/neurintsurg-2020-016474. [Epub ahead of print: 08 Sep 2020]. [DOI] [PubMed] [Google Scholar]
- 4. Zhou Y, Li W, Herath C, et al. Off-Hour admission and mortality risk for 28 specific diseases: a systematic review and meta-analysis of 251 cohorts. J Am Heart Assoc 2016;5:e003102. 10.1161/JAHA.115.003102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Concha OP, Gallego B, Hillman K, et al. Do variations in hospital mortality patterns after weekend admission reflect reduced quality of care or different patient cohorts? a population-based study. BMJ Qual Saf 2014;23:215–22. 10.1136/bmjqs-2013-002218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abougergi MS, Travis AC, Saltzman JR. Impact of day of admission on mortality and other outcomes in upper Gi hemorrhage: a nationwide analysis. Gastrointest Endosc 2014;80:228–35. 10.1016/j.gie.2014.01.043 [DOI] [PubMed] [Google Scholar]
- 7. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663–8. 10.1056/NEJMsa003376 [DOI] [PubMed] [Google Scholar]
- 8. Sorita A, Ahmed A, Starr SR, et al. Off-hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta-analysis. BMJ 2014;348:f7393. 10.1136/bmj.f7393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Potts MB, Abdalla RN, Golnari P, et al. Analysis of mechanical thrombectomy for acute ischemic stroke on nights and weekends versus weekdays at comprehensive stroke centers. J Stroke Cerebrovasc Dis 2021;30:105632. 10.1016/j.jstrokecerebrovasdis.2021.105632 [DOI] [PubMed] [Google Scholar]
- 10. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart Association/American stroke association. Stroke 2019;50:e344–418. 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 11. Saver JL, Goyal M, van der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 2016;316:1279–88. 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 12. Goyal M, Jadhav AP, Bonafe A, et al. Analysis of workflow and time to treatment and the effects on outcome in endovascular treatment of acute ischemic stroke: results from the swift prime randomized controlled trial. Radiology 2016;279:888–97. 10.1148/radiol.2016160204 [DOI] [PubMed] [Google Scholar]
- 13. Mpotsaris A, Kowoll A, Weber W, et al. Endovascular stroke therapy at nighttime and on weekends-as fast and effective as during normal business hours? J Vasc Interv Neurol 2015;8:39–45. [PMC free article] [PubMed] [Google Scholar]
- 14. Nikoubashman O, Probst T, Schürmann K, et al. Weekend effect in endovascular stroke treatment: do treatment decisions, procedural times, and outcome depend on time of admission? J Neurointerv Surg 2017;9:336–9. 10.1136/neurintsurg-2015-012220 [DOI] [PubMed] [Google Scholar]
- 15. Raymond SB, Akbik F, Stapleton CJ, et al. Protocols for endovascular stroke treatment diminish the weekend effect through improvements in off-hours care. Front Neurol 2018;9:1106. 10.3389/fneur.2018.01106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Almallouhi E, Al Kasab S, Harvey JB, et al. Impact of treatment time on the long-term outcome of stroke patients treated with mechanical thrombectomy. J Stroke Cerebrovasc Dis 2019;28:185–90. 10.1016/j.jstrokecerebrovasdis.2018.09.033 [DOI] [PubMed] [Google Scholar]
- 17. Groot AE, de Bruin H, Nguyen TTM, et al. Presentation outside office hours does not negatively influence treatment times for reperfusion therapy for acute ischemic stroke. J Neurol 2021;268:133–9. 10.1007/s00415-020-10106-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kaaouana O, Bricout N, Casolla B, et al. Mechanical thrombectomy for ischaemic stroke in the anterior circulation: off-hours effect. J Neurol 2020;267:2910–6. 10.1007/s00415-020-09946-6 [DOI] [PubMed] [Google Scholar]
- 19. Zha M, Yang Q, Liu S, et al. Off-hour effect on time metrics and clinical outcomes in endovascular treatment for large vessel occlusion: a systematic review and meta-analysis. Int J Stroke 2021;0(0:17474930211012545. 10.1177/17474930211012545 [DOI] [PubMed] [Google Scholar]
- 20. Hoepner R, Weber R, Reimann G, et al. Stroke admission outside daytime working hours delays mechanical thrombectomy and worsens short-term outcome. Int J Stroke 2019;14:517–21. 10.1177/1747493018790079 [DOI] [PubMed] [Google Scholar]
- 21. Kim J-G, Choi JC, Kim DJ, et al. Effect of the number of neurointerventionalists on off-hour endovascular therapy for acute ischemic stroke within 12 hours of symptom onset. J Am Heart Assoc 2019;8:e011933. 10.1161/JAHA.119.011933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Löwhagen Hendén P, Rentzos A, Karlsson J-E, et al. Off-hour admission and impact on neurological outcome in endovascular treatment for acute ischemic stroke. Acta Anaesthesiol Scand 2019;63:208–14. 10.1111/aas.13241 [DOI] [PubMed] [Google Scholar]
- 23. Weddell J, Parr E, Knight S, et al. Mechanical thrombectomy: can it be safely delivered out of hours in the UK? BMC Neurol 2020;20:326. 10.1186/s12883-020-01909-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Flottmann F, Broocks G, Faizy TD, et al. Factors associated with failure of reperfusion in endovascular therapy for acute ischemic stroke : a multicenter analysis. Clin Neuroradiol 2021;31:197–205. 10.1007/s00062-020-00880-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wilson TA, Leslie-Mazwi T, Hirsch JA, et al. A multicenter study evaluating the frequency and time requirement of mechanical thrombectomy. J Neurointerv Surg 2018;10:235–9. 10.1136/neurintsurg-2017-013147 [DOI] [PubMed] [Google Scholar]
- 26. Dandapat S, Kasab SA, Zevallos CB, et al. In-House anesthesia and interventional radiology technologist support optimize mechanical thrombectomy workflow after hours. J Stroke Cerebrovasc Dis 2020;29:105246. 10.1016/j.jstrokecerebrovasdis.2020.105246 [DOI] [PubMed] [Google Scholar]
- 27. Zi W, Wang H, Yang D, et al. Clinical effectiveness and safety outcomes of endovascular treatment for acute anterior circulation ischemic stroke in China. Cerebrovasc Dis 2017;44:248–58. 10.1159/000478667 [DOI] [PubMed] [Google Scholar]
- 28. Yoo AJ, Simonsen CZ, Prabhakaran S, et al. Refining angiographic biomarkers of revascularization: improving outcome prediction after intra-arterial therapy. Stroke 2013;44:2509–12. 10.1161/STROKEAHA.113.001990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. von Kummer R, Broderick JP, Campbell BCV, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 2015;46:2981–6. 10.1161/STROKEAHA.115.010049 [DOI] [PubMed] [Google Scholar]
- 30. Higashida RT, Furlan AJ, Roberts H, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 2003;34:e109–37. 10.1161/01.STR.0000082721.62796.09 [DOI] [PubMed] [Google Scholar]
- 31. Benali A, Moynier M, Dargazanli C, et al. Mechanical thrombectomy in nighttime hours: is there a difference in 90-day clinical outcome for patients with ischemic stroke? AJNR Am J Neuroradiol 2021;42:530–7. 10.3174/ajnr.A6997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 33. Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–18. 10.1056/NEJMoa1414792 [DOI] [PubMed] [Google Scholar]
- 34. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30. 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 35. Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372:2296–306. 10.1056/NEJMoa1503780 [DOI] [PubMed] [Google Scholar]
- 36. Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372:2285–95. 10.1056/NEJMoa1415061 [DOI] [PubMed] [Google Scholar]
- 37. Albright KC, Savitz SI, Raman R, et al. Comprehensive stroke centers and the 'weekend effect': the SPOTRIAS experience. Cerebrovasc Dis 2012;34:424–9. 10.1159/000345077 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
svn-2021-000949supp001.pdf (101KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author on reasonable request.