Abstract
Background:
Girls have unique developmental pathways to substance use and justice system involvement, warranting gender-responsive intervention. We tested the efficacy of VOICES (a 12-session, weekly trauma-informed, gender-responsive substance use intervention) in reducing substance use and HIV/STI risk behaviors among justice- and school-referred girls.
Methods:
Participants were 113 girls (Mage = 15.7 years, SD = 1.4; 12 % White, 19 % Black, 15 % multi-racial; 42 % Latinx) with a history of substance use referred from juvenile justice (29 %) and school systems (71 %). Study assessments were completed at baseline, 3-, 6- and 9-months follow-up. Primary outcomes included substance use and HIV/STI risk behaviors; secondary outcomes included psychiatric symptoms (including posttraumatic stress) and delinquent acts. We hypothesized that girls randomized to the VOICES (n = 51) versus GirlHealth (attention control; n = 62) condition would report reduced alcohol, cannabis and other substance use, HIV/STI risk behaviors, psychiatric symptoms, and delinquent acts.
Results:
Girls randomized to VOICES reported significantly less cannabis use over 9-month follow-up relative to the control condition (time by intervention, p < .01), but there were no between group differences over time in HIV/STI risk behavior. Girls in both conditions reported fewer psychiatric symptoms and delinquent acts over time.
Conclusions:
Data support the use of a trauma-informed, gender-responsive intervention to reduce cannabis use among girls with a substance use history and legal involvement; reducing cannabis use in this population has implications for preventing future justice involvement and improving public health outcomes for girls and young women, who are at disproportionate health and legal risk relative to their male counterparts.
Keywords: Cannabis use, Justice-involved girls, School-based intervention
1. Introduction
Research demonstrates that girls have unique developmental pathways to substance use and justice system involvement. Justice-involved girls experience substantially higher rates of trauma (particularly interpersonal such as sexual abuse) and associated posttraumatic stress symptoms than boys (Modrowski et al., 2017), which is associated with girls’ increased substance use (Smith and Saldana, 2013) and more severe psychopathology [particularly internalizing disorders, such as depression (Conrad et al., 2017)]. Certain psychological constructs, such as self-esteem and self-efficacy (Guthrie and Low, 2000), gender and ethnic identity development and empowerment (De La Rosa et al., 2010) and developmental issues, gender role characteristics and coping styles (Khoury, 1998) have been found to differentiate girls from boys in relation to substance use. Girls’ complex emotional and behavioral health needs are also related to increased juvenile justice involvement (Messina and Grella, 2006). Likewise, family dysfunction and conflictual interpersonal relationships appear related to girls’ substance use, sexual and reproductive health, and delinquency (Chesney-Lind, 1997; Owen, 1998; Owen and Bloom, 1995). Taken together, these findings highlight justice-involved girl’s distinct life experiences that create unique developmental pathways into substance use and criminal involvement (Grella et al., 2005; Leban and Gibson, 2020; Messina and Grella, 2006) and warrant empirically-supported gender-responsive substance use interventions to disrupt pathways (Messina et al., 2010a, 2010b; Prendergast et al., 2011).
While Monitoring the Future survey results find that overall cannabis use did not increase in 2019, cannabis use overall remains prevalent and increases are observed for certain subpopulations (8th and 10th graders) and in daily use. Increases in daily use may, however, be related to method of use, such as increases in vaping (Schulenberg et al., 2019). Lifetime cannabis use rates among justice-involved youth (14 years old) living in the community are approximately 50 % (Tolou-Shams et al., 2020) and more than twice that reported by 12th graders in general adolescent population surveys (National Institute on Drug Abuse, 2019). Justice-involved youth report higher rates of cannabis use (48 % of community-supervised; 54 % of detained youth) than their same-age, non-justice-involved peers, and often begin using cannabis by 13 years old (Grigorenko et al., 2015; Tolou-Shams et al., 2020). Youth arrested in the past year have over 6 times higher prevalence of cannabis use disorder compared to those with no past year justice involvement (Winkelman et al., 2017). Rates of cannabis use are particularly high among female justice-involved youth in the community, with 55 % reporting lifetime use (versus 45 % of males) (Tolou-Shams et al., 2020). Cannabis use is associated with multiple negative consequences for justice-involved youth, with those who report past year use being more likely to experience school failure, use other substances, sell and be offered drugs, and engage in violent behavior (Vaughn et al., 2020). Despite these harms, justice-involved youth are unlikely to receive substance use prevention services; only 33 % of community supervision and behavioral health providers serving justice-involved youth provide such programming (Funk et al., 2020). Thus, interventions targeting adolescent cannabis use in gender-responsive ways, particularly for justice-involved girls and girls with a history of increased substance use relative to their peers, are sorely needed.
VOICES is an adolescent, group-based, gender-responsive, trauma-informed substance use intervention developed specifically for justice-involved girls (Covington et al., 2017). Adapted from an efficacious adult substance use intervention for incarcerated women (Messina et al., 2010a, 2010b), Helping Women Recover (Covington, 2008), VOICES includes content corresponding with ten principles of trauma-informed care, including emphasizing strengths and resilience and recognizing the impact of victimization on development and coping strategies (Markoff et al., 2005). Activities are based on relational and gender empowerment theories (Bloom et al., 2003; Miller, 2012). Substance use, mental health, and well-being are addressed through activities promoting learning and understanding of feelings about self and interpersonal relationships. VOICES is not designed as a trauma treatment; however, it is a trauma-informed, secondary intervention to reduce and prevent adolescent substance misuse.
1.1. Current study
The primary aim of our Project VOICES randomized controlled trial was to test the efficacy of a 12-week, 1 -h weekly group intervention in reducing substance use and HIV/STI risk behaviors with 113 justice and school system-referred girls (12–17 years) with a lifetime history of substance use. VOICES was compared to a psychoeducational group intervention (GirlHealth) that included didactic content on a range of health topics and was matched for time (12 sessions; 1 h each) and appeal to VOICES. The VOICES curriculum was not originally designed as an HIV/STI risk reduction intervention; however, the intervention’s relational and gender-responsive approach and targeted mechanisms of change (e.g., self-efficacy, empowerment, communication) have demonstrated associations with reduced HIV/STI risk, e.g., among adolescent African American girls (DiClemente et al., 2004; Hendrick and Canfield, 2017). Thus, the current study also included adolescent HIV/STI risk outcomes. Secondary outcomes of psychiatric symptoms and delinquent acts were also explored. We hypothesized girls randomized to VOICES compared to GirlHealth would report less alcohol, cannabis and other drug use and fewer HIV/STI risk behaviors, psychiatric symptoms, and delinquent acts over a 9-month follow-up.
2. Methods
2.1. Participants
School-referred and justice-involved girls and young women, ages 12–24, with lifetime history of substance use were eligible for the trial. Of the 384 girls and young women referred, 195 were eligible and of those, 132 consented to participate (see Fig. 1 for CONSORT diagram). Of the 63 who did not consent for participation, reasons included: no history of substance use, active pregnancy, uninterested in completing project screening and unable to contact. Of the 132 who consented, 16 were transition-age youth (TAY; ≥18 years at time of enrollment) and three girls (ages 12–17) were part of the original trial design which included a Standard of Care (SOC) comparison group (i.e., the trial was revised in August 2016 to include an active comparison condition; GirlHealth). TAY were excluded from the current sample and outcome analysis due to the small number enrolled and low rate of intervention completion. Likewise, the first three 12–17-year-old participants randomized to the SOC condition were excluded. Trial outcome analyses were thus conducted on a final sample of 113 school- and justice-referred girls, ages 12–17, who reported a lifetime history of alcohol, cannabis or other drug use, were living in the community (i.e., not detained or in group home), and who were randomized to either VOICES or GirlHealth. Exclusion criteria included: a) lack of English language fluency, b) impairment precluding informed assent or consent, c) active substance use requiring higher level of care, d) active psychosis or other significant psychiatric and/or cognitive impairment that might preclude ability to participate in groups. Decisions regarding substance use level of care and/or psychiatric/cognitive impairment were made by the referral sources (i.e., this exclusion criteria was relayed to them in considering whom to refer) and/or observation of or self-report by youth during study screening.
Fig. 1.
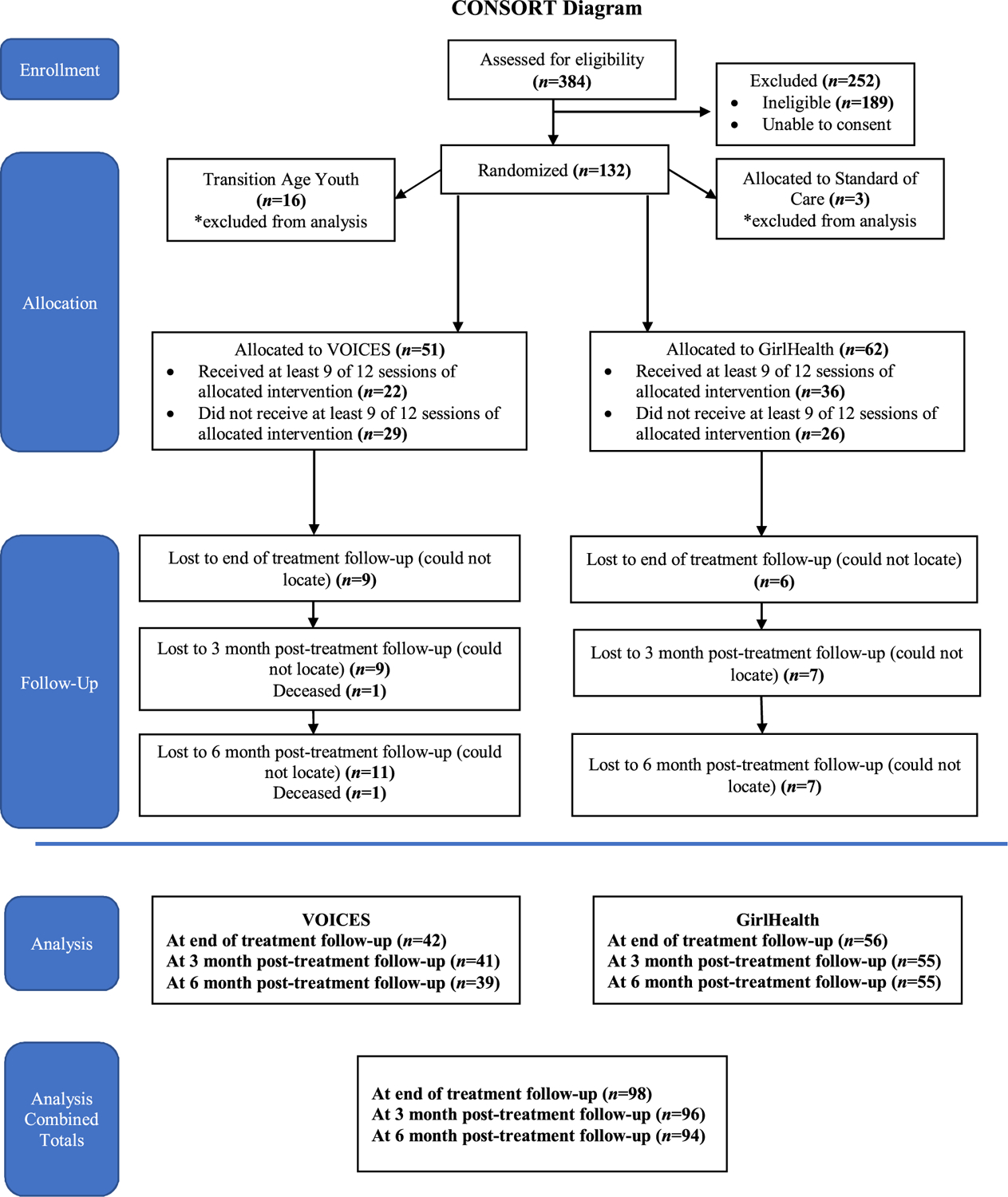
CONSORT Diagram.
2.2. Procedures
Between March 2016 and August 2019, juvenile probation, community diversion programs, and schools in two Northern California counties referred interested girls to the study for eligibility screening. All referred girls completed a computerized-assisted, anonymous study screener in a location allowing for privacy. Assent and caregiver consent were obtained for eligible girls aged 12–17 years. Enrolled girls completed baseline, 3-, 6- and 9-month follow-up assessments (≤ 2 h per assessment) using electronic questionnaires (REDCap) in English that were completed remotely or in-person with the questionnaire on a study tablet. In-person assessments were conducted by study staff in the home or another community location (e.g., library). All girls met research staff in-person to complete the urine toxicology screens.
To enhance engagement and retention, study staff: obtained a locator form with contact information for up to 5 individuals who would be familiar with the girl’s whereabouts; sent weekly appointment reminder emails, texts, personalized letters from study staff, and birthday and holiday cards from the project and reminded girls and caregivers of home or community-based visit options for assessment. The Principal Investigator’s university Institutional Review Board approved all recruitment and study procedures.
2.3. Intervention
Girls were randomized to VOICES or GirlHealth using computer-generated, block randomization; blocks were determined by county and referral source (i.e., justice versus school setting) and consisted of 5–7 girls (depending on referral stream). The trial compared a 12 session, 1 h per session version of VOICES to GirlHealth, a health promotion (didactic/psychoeducational) group condition matched for time and appeal that has been used in other substance use intervention trials with justice-involved youth (Tolou-Shams et al., 2011, 2017). Group sessions were co-led by a clinician and non-clinician (e.g., research assistant) study staff and were conducted in various community-based settings (e.g., schools, hospital). Facilitators received 2 days of training each in VOICES (by facilitator from the Center for Gender and Justice) and GirlHealth (by curriculum developer/PI), including detailed manual review, role plays, and directly observed skills practice. Facilitators received weekly supervision from a trained licensed clinician to monitor fidelity and intervention drift.
2.3.1. VOICES (active intervention)
The 12 VOICES sessions were organized into four modules (Table 2). Module A (Self) focuses on establishing group cohesion, enhancing self-efficacy and self-esteem, identifying self-attributes, understanding gender stereotypes and gender role identity, identifying positive female role models, and empowering assertiveness. Module B (Connecting with Others) centers on communication skills, family dynamics (e.g., mother-daughter relationship), acquiring positive peer support, learning about prosocial friendships, promoting healthy and safe sexual behavior and positive dating relationships, and learning signs of abusive relationships. Module C (Healthy Living) focuses on substance use and spirituality. Substance use content highlights refusal skills and understanding motivations for use, including intergenerational patterns of substance use. Module D (Journey Ahead) centers on building future orientation, goal-setting and motivational principles for behavior change. Participants received a VOICES journal that supported intervention content, and allowed for exploring and recording experiences, thoughts, and feelings throughout the intervention.
Table 2.
Intervention sessions and content.
| Session | VOICES | GirlHealth |
|---|---|---|
| 1 | Who am I? | Stress Management |
| 2 | My Life Story | Wellness |
| 3 | Breaking the Silence | Nutrition |
| 4 | The World Girls Live In | Sleep and Exercise |
| 5 | Communication | Alcohol |
| 6 | My Family & Mothers and Daughters | Nicotine |
| 7 | Dating, Sexuality, Healthy Relationships (1) | Marijuana |
| 8 | Dating, Sexuality, Healthy Relationships (2) | Other Drugs |
| 9 | Abusive Relationships | Sexual Health |
| 10 | Alcohol and Other Drugs | Internet Safety |
| 11 | Spirituality | Bullying |
| 12 | Crossroads and Packing for My Journey | Wrap-up |
2.3.2. GirlHealth (comparison condition)
As an attention-only control intervention, GirlHealth provides didactic and interactive group instruction matched for time, appeal, and format to VOICES. GirlHealth targets general health promotion (Table 2), and does not include active skills learning, practice, or content not readily accessible online or similar to standard health education classes. A version of this intervention has been used in other substance use intervention trials with justice-involved youth (Tolou-Shams et al., 2011, 2017). All sessions incorporated activities, such as games and interactive discussion, to keep youth engaged.
3. Measures (Baseline and 3, 6, 9-month follow-up)
3.1. Demographics
(self-report) included (at baseline only) age, sexual orientation, race, ethnicity, receipt of public assistance and household annual income. Adolescents’ educational, legal, systems-involvement and behavioral health treatment history was collected at each timepoint.
3.2. Primary outcomes: substance use and HIV/STI risk behaviors (all timepoints)
The Adolescent Risk Behavior Assessment (ARBA; Donenberg et al., 2001) assessed self-report of: 1) substance use [lifetime and past 90 days nicotine, alcohol, cannabis and other drug use (e.g., cocaine) and other past use descriptives (e.g., age of initiation)] and 2) sexual activity [type of sexual behavior (i.e., oral, vaginal or anal), frequency of condom use and intercourse (e.g., condom use at last sexual intercourse), age of sexual debut, number of sex partners, and substance use preceding and/or during sex].
Cannabis and alcohol use related consequences were assessed using the 24-item Brief Young Adult Alcohol Consequences Questionnaire (α = .86; Kahler et al., 2005) and the 21-item Brief Marijuana Consequences Scale (α = .83; Simons et al., 2012). Youth respond yes (1) or no (0) to statements describing typical consequences of substance use (e.g., “The quality of my work or schoolwork has suffered because of my marijuana use” for cannabis). Summed higher scores on both scales indicated greater alcohol or cannabis-related problems.
Urine toxicology screens assessed the presence of: methadone, amphetamine, opiates, oxycodone, propoxyphene, benzodiazepines, barbiturates, methamphetamines, cocaine, and cannabis. Measures of test validity (e.g., temperature, pH, oxidants) were examined at the time of toxicology screen administration.
3.3. Secondary outcomes: psychiatric symptoms and delinquency (all timepoints)
Brief Symptom Inventory (BSI; Derogatis and Melisaratos, 1983). The BSI is a 53-item measure of the extent to which youth have been bothered (0=not at all to 4=extremely) in the past week by various symptoms. Two items related to self-harm or harming others were removed, resulting in a 51-item version of the measure. The BSI has nine subscales assessing different symptom groups (i.e., somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) and a Global Severity Index (GSI; α = .95; Derogatis and Melisaratos, 1983). The GSI is calculated by summing the nine subscales and three additional items, and dividing the total number of items with the number of actual respones. Higher scores indicate greater psychological distress.
National Stressful Events Survey PTSD Short Scale (NSESSS; Kilpatrick et al., 2013). This 9-item measure assesses youth exposure to trauma and posttraumatic stress symptoms. Youth reported experiences of posttraumatic stress symptoms on a 5-point scale (1=not at all to 5=extremely). The total symptom score was used, with higher scores indicating greater symptom severity. We added an additional response option (6=I have never experienced a stressful event) to identify youth with no trauma exposure. Prorated scores were calculated when no more than two items were left unanswered (sum of items answered by the total number of items on the measure)/number of items answered, rounded to the nearest whole number).
National Youth Survey-Self-Reported Delinquency (Thornberry and Krohn, 2000). Scores from the General Delinquency subscale (range from 0 to 23) of this well-validated, 40-item self-report measure of delinquent acts (e.g., larceny, fighting, selling drugs) were used; higher scores indicate greater number of delinquent acts (in the past 120 days) endorsed (α = 0.98).1 We relied on self-report of delinquent acts as a proxy for collateral recidivism data, which we were unable to systematically collect for all participants.
3.4. Intervention fidelity
All sessions were audio-recorded; 20 % were coded and 5% were blindly double-coded by trained study clinicians. Session fidelity was measured across three domains (scale: 0=not at all to 3=fully): 1) how much of the scripted manual content was delivered for each content/activity area; 2) quality of facilitator skills; and 3), inclusion of fundamental items (e.g., adherence to session structure, absence of external interruptions); each domain was averaged to derive a percentile score.
4. Data analyses
We originally powered to the study to detect an effect size of 0.3 or greater (at ≥0.80), based on a final analytic sample of 160 girls. Power was determined using the Monte Carlo facility of Mplus, including 500 replications in a model specified as described below. Unfortunately, due to lower than anticipated number of eligible girls for recruitment in justice and school settings, we were unable to enroll the target sample size, but proceeded with the analyses as originally planned, acknowledging that we may be under-powered to detect statistically significant effects (if present).
Descriptive statistics, including means and SDs for continuous variables and frequencies for categorical variables, were computed for all variables. Generalized linear mixed models, implemented using SAS PROC GLIMMIX (SAS Institute Inc, 2013), were used to conduct repeated measures analyses of intervention effects over time. These models accommodate variously distributed dependent variables, including dichotomous, count, and continuous variables, account for correlations associated with repeated measurements, and accommodate missing data so all available data could be analyzed. Dichotomous outcomes were analyzed using a binomial distribution and a logit link function; count variables were analyzed using negative binomial regression with a log link function; normally distributed, continuous variables were analyzed with an identity link function.
All models included intervention (VOICES vs GirlHealth) as a between-subjects effect and time as a repeated, within-subjects effect. The intervention × time effect was evaluated as the primary test of differential intervention effect. Age and a dichotomous indicator of completion of 9–12 intervention sessions were included as covariates in all models.
Some outcomes were recoded or excluded from analyses following examination of the descriptive statistics. Alcohol use was too infrequent to examine change over time. Similarly, limited use of substances other than cannabis precluded longitudinal analysis of individual substances. A dichotomous indicator of any alcohol or substance use was examined. Delinquent acts measured by the NYS General Delinquency scale were infrequently observed at follow-up and a dichotomous indicator reflecting any delinquent acts was analyzed instead of the scale score. Multiple scales from the BSI were examined; results were similar and only the GSI was included in the final analyses.
5. Results
5.1. Descriptives
Participant characteristics at baseline are summarized in Table 1. Participants’ mean age was 15.70 years (SD = 1.36) with almost all in grades 9–12. Participants predominantly identified as being a racial and/or ethnic minority and as heterosexual. Approximately one-third of girls were referred from juvenile justice settings and two-thirds were referred from schools. GirlHealth and VOICES groups differed at baseline only on report of lifetime sexual intercourse; 66.7 % (34) of the VOICES group and 43.6 % (27) of the GirlHealth group reported prior sexual intercourse (x2(1) = 6.02, p = .02).
Table 1.
VOICES Trial Participant Characteristics at Baseline.
| Full Sample (N = 113) N (%) or M (SD) | GirlHealth (n = 62) N (%) or M (SD) | VOICES (n = 51) N (%) or M (SD) | |
|---|---|---|---|
| Demographics | |||
| Age (in years) | 15.70 (1.36) | 15.50 (1.35) | 15.94 (1.33) |
| Race/Ethnicity | |||
| Latinx | 47 (41.6) | 27 (43.6) | 20 (39.2) |
| Black | 21 (18.6) | 10 (16.1) | 11 (21.6) |
| Multiracial | 17 (15.0) | 11 (17.7) | 6 (11.8) |
| White | 14 (12.4) | 7 (11.3) | 7 (13.7) |
| Asian | 8 (7.1) | 5 (8.1) | 3 (5.9) |
| Middle Eastern/North | 2 (1.8) | 1 (1.6) | 1 (2.0) |
| African | |||
| Native American | 2 (1.8) | 0 (0.0) | 2 (3.9) |
| Native Hawaiian/Pacific | 2 (1.8) | 1 (1.6) | 1 (2.0) |
| Islander | |||
| Sexual Orientation | |||
| Heterosexual | 78 (69.0) | 43 (69.4) | 35 (68.6) |
| Bisexual | 33 (29.2) | 18 (29.0) | 15 (29.4) |
| Homosexual | 1 (0.9) | 0 (0.0) | 1 (2.0) |
| Other | 1 (0.9) | 1 (1.6) | 0 (0.0) |
| Ever had sexual intercourse1 | 61 (54.0) | 27 (43.6) | 34 (66.7) |
| Family receives public assistance | 34 (30.1) | 16 (25.8) | 18 (35.3) |
| Annual Household Income | |||
| $0–29,999 | 16 (14.2) | 9 (14.5) | 7 (13.7) |
| $30,000–59,999 | 12 (10.6) | 6 (9.7) | 6 (11.8) |
| $60,000–89,999 | 6 (5.3) | 5 (8.1) | 1 (2.0) |
| $90,000 and more | 8 (7.1) | 4 (6.5) | 4 (7.8) |
| Unknown / not reported | 71 (62.8) | 38 (61.3) | 23 (64.7) |
| Recruitment source | |||
| Juvenile Justice | 33 (29.2) | 21 (33.9) | 12 (23.5) |
| School | 80 (70.8) | 41 (66.1) | 39 (76.5) |
| Education/School-Related | |||
| Grade in School | |||
| 7th-8th | 4 (3.5) | 3 (4.8) | 1 (2.0) |
| 9th-10th | 52 (46.0) | 32 (51.6) | 20 (39.2) |
| 11th-12th | 55 (48.7) | 26 (41.9) | 29 (56.9) |
| GED | 1 (0.9) | 1 (1–6) | 0 (0.0) |
| In College | 1 (0.9) | 0 (0.0) | 1 (2.0) |
| Ever expelled from school | 7 (6.2) | 4 (6.5) | 3 (5.9) |
| Ever received special ed. services | 11 (9.7) | 9 (14.5) | 2 (3.9) |
| Ever had an Individualized | 23 (20.4) | 12 (19.4) | 11 (21.6) |
| Education Plan or 504 Plan | |||
| Legal and Behavioral Health History | |||
| Ever removed from home by child welfare agency2 | 6 (5.7) | 2 (3.3) | 4 (8.7) |
| # types of delinquent acts in lifetime | 2.41 (3.05) | 2.55 (3.41) | 2.25 (2.57) |
| Ever been arrested3 | |||
| # arrests (if ever arrested) | 2.73 (2.63) | 2.70 (3.02) | 2.80 (1.92) |
| Experienced traumatic event (s) | 109 (96.5) | 59 (95.2) | 50 (98.0) |
| Ever given a mental health diagnosis2 | 22 (20.8) | 15 (25.0) | 7 (15.2) |
| Ever received outpatient mental health treatment2 | 11 (10.4) | 7 (11.7) | 4 (8.7) |
| Ever taken psychiatric medications2 | 13 (12.3) | 10 (16.7) | 3 (6.5) |
| Ever hospitalized (medical or psychiatric)2 | 8 (7.6) | 5 (8.3) | 3 (6.5) |
| Type of hospital (if hospitalized) | |||
| Medical | 3 (37.5) | 2 (40.0) | 1 (33.3) |
| Psychiatric | 1 (12.5) | 1 (20.0) | 0 (0.0) |
| Both | 4 (50.0) | 2 (40.0) | 2 (66.7) |
| Ever received inpatient substance use treatment2 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ever received outpatient substance use treatment2 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
GirlHealth and VOICES differ, p<.05.
N=106.
N = 101.
5.2. Group attendance
Girls attended an average of 7 of 12 sessions (51 % attended 9–12 sessions) and there were no group differences in intervention dose.
5.3. Intervention fidelity
Group facilitators (both conditions) provided most session content (M = 91 %, range = 55–100 %), included most fundamental items (M = 91 %, range = 60–100 %), and were rated at high skill levels (M = 99 %, range = 79–100 %). There were no differences in fidelity based on VOICES or GirlHealth condition, cohort, year session was delivered, or supervisor (all t-test and ANOVA p values > 0.05); only 5 of the 66 unique sessions coded had a rating of less than 70 % (all due to content missing for school-based groups that ended because of unanticipated changes to school schedule [e.g., unannounced early dismissal]).
5.4. Follow-up retention
Fig. 1 presents retention over time; 94 % of girls completed at least one follow-up by 9 months post-baseline.
5.5. Primary outcomes
5.5.1. Substance use
Girls randomized to VOICES had significantly lower rates of cannabis use up to month 9 (6 months post-intervention) compared to those randomized to GirlHealth (Table 3 and Fig. 2). In the VOICES group, cannabis use decreased from 56.9 % at baseline to 38.5 % at month 9. In contrast, use in the GirlHealth group increased from 50.0 % at baseline to 58.2 % at month 9. The intervention × time interaction was statistically significant (F(3, 281) = 2.92, p = .03). Similar differences were observed in biologically confirmed (urine toxicology) cannabis use; cannabis was detected in 33.3 % of the VOICES group at baseline and 26.5 % at month 9, and 25.6 % of the GirlHealth group at baseline and 39 % at month 9 (intervention × time, F(3, 244) = 2.28, p = .08). Findings for any self-reported alcohol or drug use paralleled those for cannabis use (intervention × time F(3, 281) = 3.39, p = .02). Consequences of cannabis and alcohol use did not differ across the two interventions, decreasing over time in both groups (cannabis x2(3) = 22.55, p<.0001, alcohol x2(3) = 19.69, p = .0002).
Table 3.
Longitudinal Outcomes by Intervention.
| Outcome variable | GirlHealth (n = 62) N (%) or M (SD) | VOICES (n = 51) N (%) or M (SD) | Intervention × Time p-value |
|---|---|---|---|
| Cannabis use in last 3 mos | .03 | ||
| Baseline | 31 (50.0) | 29 (56.9) | |
| 3 month follow-up | 28 (50.0) | 18 (42.9) | |
| 6 month follow-up | 27 (49.1) | 18 (43.9) | |
| 9 month follow-up | 32 (58.2) | 15 (38.5) | |
| Biologically detected cannabis use | .08 | ||
| Baseline | 16 (25.8) | 16 (33.3) | |
| 3 month follow-up | 17 (33.3) | 9 (25.00 | |
| 6 month follow-up | 15 (29.4) | 13 (38.2) | |
| 9 month follow-up | 16 (34.0) | 9 (26.5) | |
| Any alcohol or drug use in last 3 mos | .02 | ||
| Baseline | 36 (58.1) | 38 (74.5) | |
| 3 month follow-up | 32 (57.1) | 29 (59.5) | |
| 6 month follow-up | 30 (43.6) | 23 (56.1) | |
| 9 month follow-up | 36 (65.5) | 21 (53.9) | |
| Sexual intercourse in last 3 mos | .94 | ||
| Baseline | 21 (33.9) | 23 (45.1) | |
| 3 month follow-up | 15 (26.8) | 14 (33.3) | |
| 6 month follow-up | 18 (32.7) | 21 (51.2) | |
| 9 month follow-up | 19 (34.6) | 16 (41.0) | |
| if had sexual intercourse: | |||
| Used condom at last intercourse | .92 | ||
| Baseline | 13 (48.2) | 15 (44.1) | |
| 3 month follow-up | 3 (20.0) | 4 (28.6) | |
| 6 month follow-up | 5 (27.8) | 5 (23.5) | |
| 9 month follow-up | 7 (36.8) | 7 (37.5) | |
| Used any birth control in last 3 mos | .89 | ||
| Baseline | 18 (29.0) | 17 (33.3) | |
| 3 month follow-up | 13 (23.2) | 12 (28.6) | |
| 6 month follow-up | 16 (29.1) | 15 (36.6) | |
| 9 month follow-up | 17 (30.9) | 13 (33.3) | |
| Substance use during sex in last 3 mos (participant) | .08 | ||
| Baseline | 10 (47.6) | 15 (65.2) | |
| 3 month follow-up | 7 (46.7) | 8 (57.1) | |
| 6 month follow-up | 12 (66.7) | 9 (42.9) | |
| 9 month follow-up | 10 (52.6) | 8 (50.0) | |
| Substance use during sex in last 3 mos (partner) | .13 | ||
| Baseline | 9 (42.9) | 8 (65.2) | |
| 3 month follow-up | 6 (40.0) | 8 (57.1) | |
| 6 month follow-up | 10 (55.6) | 9 (42.9) | |
| 9 month follow-up | 10 (52.6) | 6 (37.5) | |
| Marijuana Consequences (B-MACQ)1 | .38 | ||
| Baseline | 3.39 (4.59) | 3.62 (4.91) | |
| 3 month follow-up | 2.09 (4.03) | 1.67 (3.20) | |
| 6 month follow-up | 2.15 (4.04) | 1.56 (3.38) | |
| 9 month follow-up | 2.04 (3.32) | 1.36 (3.13) | |
| Alcohol Consequences (B-YAACQ)1 | .64 | ||
| Baseline | 2.00 (3.47) | 3.32 (4.51) | |
| 3 month follow-up | 1.20 (2.67) | 1.40 (3.81) | |
| 6 month follow-up | 1.11 (2.19) | 1.93 (4.06) | |
| 9 month follow-up | 0.93 (2.26) | 1.72 (3.90) | |
| PTSD (NSESSS)1 | .62 | ||
| Baseline | 13.26 (5.73) | 14.00 (11.13) | |
| 3 month follow-up | 11.19 (9.97) | 11.78 (9.31) | |
| 6 month follow-up | 10.19 (10.36) | 10.34 (9.90) | |
| 9 month follow-up | 8.06 (9.46) | 11.06 (10.59) | |
| Psychiatric Symptoms (BSI General Severity Index)1 | .75 | ||
| Baseline | 0.89 (0.77) | 0.93 (0.83) | |
| 3 month follow-up | 0.77 (0.87) | 0.84 (0.83) | |
| 6 month follow-up | 0.69 (0.83) | 0.81 (0.84) | |
| 9 month follow-up | 0.69 (0.95) | 0.78 (0.77) | |
| Any delinquent acts (NYS)1 | .41 | ||
| Baseline | 37 (59.7) | 36 (70.6) | |
| 3 month follow-up | 13 (23.2) | 11 (26.2) | |
| 6 month follow-up | 15 (27.3) | 9 (22.0) | |
| 9 month follow-up | 7 (12.7) | 4 (10.3) |
Decrease over time, p<.05.
Fig. 2.
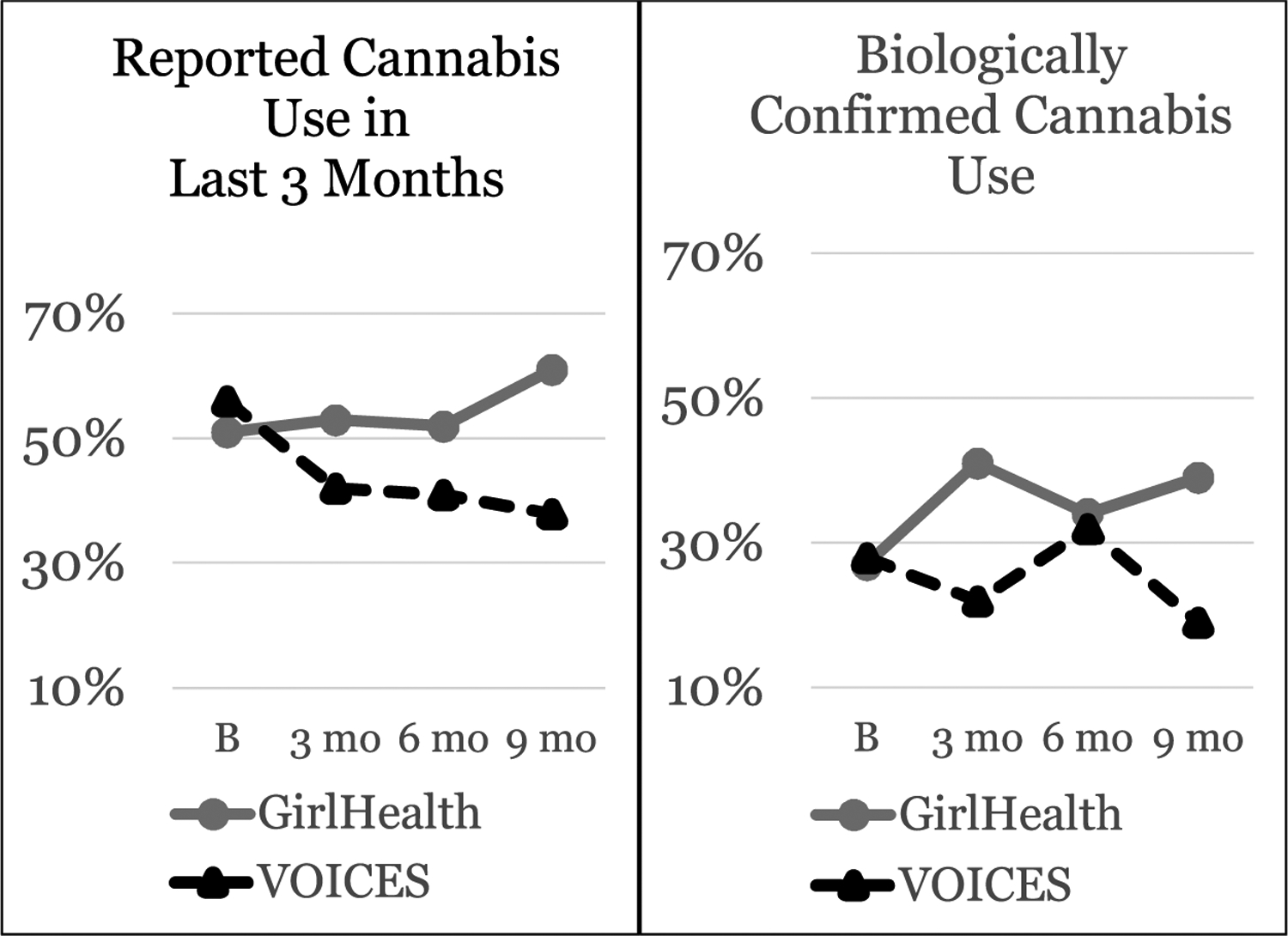
Cannabis use over time by intervention group. Intervention × time interaction p = .03 for Reported Cannabis Use in Last 3 Months, p = .08 for Biologically Confirmed Cannabis Use.
5.5.2. HIV/STI risk behaviors
No group differences nor changes over time were observed (Table 3).
5.6. Secondary outcomes
Statistically significant decreases over time in PTSD-related symptoms (F(3, 209) = 7.64, p < .0001) and general psychiatric symptoms (F (3, 266) = 3.31, p = .02) were observed in both groups (Table 3). Statistically significant decreases in reports of any delinquent act(s) were also observed in both groups (F(3, 281) = 28.08, <.0001).
6. Discussion
Our study is among the first to empirically support a trauma-informed, gender-responsive approach to reducing adolescent girls’ cannabis use. Walker et al. (2019) present RCT findings of a gender-responsive cognitive behavioral substance use prevention intervention with court-involved girls (57 % endorsed substance use at baseline) but found no intervention effects on substance use (type not reported). Family-based and/or intensive lengthy interventions (e.g., Multisystemic Therapy and Multidimensional Family Treatment; Henggeler and Schaeffer, 2016; Liddle, 2016), that include justice-involved youth have demonstrated reductions in substance use and consequences over time, but these are not gender-responsive interventions addressing the unique needs of girls already justice-involved or at increased likelihood for involvement due to early cannabis use. The current study emphasizes that the VOICES intervention was successful in reducing cannabis use among substance using adolescent girls. Monitoring the Future survey data over the past 40 years demonstrates that adolescent cannabis use is more recently driven by coping-related reasons (e.g., to cope with anger/frustration, to escape) among US high school students (Patrick et al., 2019). It is plausible that VOICES intervention content (trauma-informed and gender-responsive approaches to building coping skills through enhancing self-esteem, self--efficacy and building healthier relationships) and modality (female-only group in which girls could relate to and validate one another’s stressors) was particularly effective in improving coping with negative affect and thereby decreasing cannabis use. Future research will explore specific mechanisms of change in cannabis use for those in the VOICES intervention. Additional research should focus on enhancing the reach and accessibility of VOICES given the intervention’s initial efficacy.
Consistent with our primary hypotheses, the VOICES intervention was efficacious in reducing girls’ substance use, particularly cannabis use. Rates of cannabis use were substantially less over time for girls randomized to VOICES versus an attention control comparison for up to 6 months post-intervention. Rates of alcohol and other drug use mirrored the same reductions seen for cannabis use, but the overall substance use decreases appeared largely driven by cannabis use as it was the predominant drug of choice. Collateral urine toxicology data reflected similar patterns and group differences over time; biological specimens suggested lower levels of cannabis use than self-report, however, this is likely due to the shorter detection window than the 3-month self-report and suggests participant reports of higher use are likely valid. Both groups reported fewer substance use consequences over time, but with no between-group differences, highlighting that substance use and substance use-related consequences are not always syntonic. Girls in the VOICES condition may be accurately perceiving fewer consequences tied with lesser cannabis use; however, girls in the control condition who reported increased cannabis use over time, but fewer perceived consequences associated with use, suggests that their substance use quantity and frequency would be an important focus of future intervention.
Contrary to hypotheses, there were no intervention versus control group differences nor changes over time in adolescent HIV/STI risk behaviors. These findings are perhaps due to the notion that targeting the mechanisms of behavioral change for sexual safety is necessary but not sufficient; that is, that adolescent HIV/STI prevention interventions must also include a direct HIV/STI knowledge and skills-based component (e.g., condom use demonstration and practice; condom use negotiation role-plays) in order to increase adolescent condom use and safe sexual practices (Hosek and Pettifor, 2019; Petrova and Garcia-Retamero, 2015). GirlHealth included some HIV/STI didactic content, but intentionally not more than any standard school-based HIV prevention curriculum and neither intervention included skills-based HIV/STI prevention activities. Also contrary to hypotheses, there were no between group differences in psychiatric (including traumatic stress) symptoms and self-reported delinquent behaviors; girls in both groups improved over time. There is some literature suggesting the relational aspect of coming together with other adolescent girls and receiving social support just by regularly participating in a group could improve girls’ emotional and behavioral health symptoms, which may have been true for the VOICES participants (Calhoun et al., 2005).
Placing the current study in a larger context, access to empirically-supported substance use prevention for adolescents is severely limited; for justice-involved youth in the US, two-thirds of their serving systems (e.g., courts, probation, schools, community-based providers) don’t provide or lack access to such services (Funk et al., 2020). These statistics are alarming when research clearly supports the association between adolescent substance use and adverse public health, educational, social and legal outcomes, extending into adulthood, including for system-involved girls (Leve et al., 2013). Substance use is the most salient predictor of recidivism for justice-involved youth (Dowden and Brown, 2002; Stoolmiller and Blechman, 2005; van der Put et al., 2014), and there appear to be differences with respect to the strength of this association for justice-involved girls relative to boys (Scott and Brown, 2018). Research on ways to expand access to empirically-supported substance use interventions (e.g., through use of technology), such as VOICES, for justice-involved and underserved female populations, is a key next step (Tolou-Shams et al., 2021).
6.1. Limitations
All data with the exception of urine toxicology results were provided via adolescent self-report; substance use and psychiatric symptom rates were high and consistent with prior literature however, suggesting underreporting is not likely of concern. Ideally our study would have included collateral report of recidivism (e.g., official court records), but given two-thirds of the sample was school-referred, we relied instead on self-report of delinquent acts for the entire sample. We initially intended to enroll girls and young women ages 12–24, but due to the small number of TAY enrolled (none of whom completed the intervention) and significant baseline differences in substance use between adolescents and TAY (likely due to developmental and life-course differences), we did not include them in trial outcome analyses. Future research should aim to incorporate sufficient numbers of TAY women into such trials and/or develop and study trauma-informed, gender-responsive substance use interventions tailored to their unique development and life-course needs. This trial tested a shortened version of the original 18 session, 90 min per session VOICES intervention (Covington et al., 2017) because juvenile justice and school stakeholders in the early trial phases indicated they would not be interested in referring to a service of that length or intensity; in fact, only 51 % of youth attended more than 9 sessions. Future research with the VOICES intervention should consider testing the effectiveness and implementation of the efficacious 12-session version as well as examining efficacy of a briefer version (e.g., 9 session or less) that might result in improved attendance. Finally, given the challenges of recruitment and retention in this population, thus some of the analyses may have been under-powered to detect statistically significant effects (if present).
6.2. Conclusions
Our study contributes to the small, but growing body of literature demonstrating that trauma-informed and gender-responsive substance use interventions are efficacious among girls who use substances, including justice-involved females (Messina et al., 2010a, 2010b, 2012). Future directions include empirical study of telehealth delivery of the VOICES intervention to reach larger numbers of justice-involved girls and implementation science study approaches to understanding barriers and enablers of adoption and implementation of the VOICES intervention directly in the systems serving these youth (i.e., with community-based providers serving justice-involved girls, school wellness and/or counseling centers). Ultimately, leveraging technology to disseminate VOICES and rigorous study of other implementation approaches to increase access to empirically supported secondary substance use prevention has implications for 1) preventing further and future justice involvement and 2) improving public health outcomes for substance-using girls for whom interventions that lead to longer-term reductions in cannabis use are highly limited.
Role of funding source
This work was supported by the National Institutes of Health| National Institute on Drug Abuse [R01DA035231; Tolou-Shams, K24DA046569; Tolou-Shams,R25DA037190; Dauria; PI Beckwith].
Footnotes
Declaration of Competing Interest
Dr. Stephanie Covington is the curriculum developer of VOICES, the active intervention in this efficacy trial. She acted as study consultant on intervention delivery. No other conflict of interest declared.
The original subscale includes 24 items. Due to an error in the audio-assisted computerized assessment development, item 24, “Have you had sexual intercourse with a person who was not your serious partner when involved in a relationship?” was not administered to study participants; therefore, subscale scores range from 1–23 but still accurately indicate that greater scores represent greater number of delinquent acts.
References
- Bloom B, Owen B, Covington S, Raeder N, 2003. Gender-responsive strategies. Res. Pract. Guiding Principles Women Offenders 31–48. [Google Scholar]
- Calhoun GB, Bartolomucci CL, McLean B, 2005. Building connections. Women Ther. 28 (2), 17–29. 10.1300/J015v28n02_2. [DOI] [Google Scholar]
- Chesney-Lind M, 1997. The Female Offender: Girls, Women and Crime. Sage Publications, Thousand Oaks, CA. [Google Scholar]
- Conrad SM, Queenan R, Brown LK, Tolou-Shams M, 2017. Psychiatric symptoms, substance use, trauma, and sexual risk: a brief report of gender differences in marijuana-using juvenile offenders. J. Child Adolesc. Subst. Abuse 26 (6), 433–436. 10.1080/1067828X.2017.1322017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covington SS, 2008. Women and addiction: a trauma-informed approach. J. Psychoactive Drugs 40, 377–385. 10.1080/02791072.2008.10400665. [DOI] [PubMed] [Google Scholar]
- Covington SS, Covington K, Covington M, 2017. Voices: Participant Workbook: A Program of Self-Discovery and Empowerment for Girls. Hazelden. [Google Scholar]
- De La Rosa M, Dillon FR, Ganapati NE, Rojas P, Prado G, 2010. Latina mother-daughter dyads: Relations between attachement and sexual behavior under the influence of alcohol or drugs. Arch. Sexual Behav 39, 1305–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N, 1983. The brief symptom inventory: an introductory report. Psychol. Med 13 (3), 595–605. 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, HookIII EW, Oh MK, Crosby RA, Hertzberg VS, Gordon AB, Hardin JW, Parker S, Robillard A, 2004. Efficacy of an HIV prevention intervention for African American adolescent GirlsA randomized controlled trial. JAMA 292 (2), 171–179. 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E, 2001. Understanding AIDS-risk behavior among adolescents in psychiatric care: links to psychopathology and peer relationships. J. Am. Acad. Child Adolesc. Psychiatry 40 (6), 642–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowden C, Brown SL, 2002. The role of substance abuse factors in predicting recidivism: a meta-analysis. Psychol. Crime Law 8 (3), 243–264. 10.1080/10683160208401818. [DOI] [Google Scholar]
- Funk R, Knudsen HK, McReynolds LS, Bartkowski JP, Elkington KS, Steele EH, Sales JM, Scott CK, 2020. Substance use prevention services in juvenile justice and behavioral health: results from a national survey. Health Justice 8 (1), 1–8. 10.1186/s40352-020-00114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Stein JA, Greenwell L, 2005. Associations among childhood trauma, adolescent problem behaviors, and adverse adult outcomes in substance-abusing women offender. Psychol. Addict. Behav 19 (1), 43–53. [DOI] [PubMed] [Google Scholar]
- Grigorenko EL, Edwards L, Chapman J, 2015. Cannabis use among juvenile detainees: typology, frequency and association. CBMH 25, 54–65. 10.1002/cbm. [DOI] [PubMed] [Google Scholar]
- Guthrie BJ, Low LK, 2000. A substance use prevention framework: considering the social context for african american girls. Public Health Nurs. 17 (5), 363–373. 10.1046/j.1525-1446.2000.00363.x. [DOI] [PubMed] [Google Scholar]
- Hendrick CE, Canfield C, 2017. HIV risk-reduction prevention interventions targeting African American adolescent women. Adolesc. Res. Rev 2 (2), 131–149. 10.1007/s40894-016-0036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Schaeffer CM, 2016. Multisystemic Therapy®: clinical overview, outcomes, and implementation research. Fam. Process 55 (3), 514–528. 10.1111/famp.12232. [DOI] [PubMed] [Google Scholar]
- Hosek S, Pettifor A, 2019. HIV prevention interventions for adolescents. Curr. HIV/AIDS Rep 16 (1), 120–128. 10.1007/s11904-019-00431-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute Inc, S., 2013. SAS/STAT® 13.1 User’s Guide.
- Kahler CW, Strong DR, Read JP, 2005. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcoholism 29 (7), 1180–1189. 10.1097/01.ALC.0000171940.95813.A5. [DOI] [PubMed] [Google Scholar]
- Khoury E, 1998. A develoment perspecitive on gender differences in risk factors for substance use among adolescents. Drug Use and Ethnicity in Early Adolescence. Plenum. [Google Scholar]
- Kilpatrick DG, Resnick HS, Friedman MJ, 2013. National Stressful Events Survey PTSD Short Scale (NSESS-PTSD).
- Leban L, Gibson CL, 2020. The role of gender in the relationship between adverse childhood experiences and delinquency and substance use in adolescence. J. Crim. Justice 66, 1–11. [Google Scholar]
- Leve LD, Kerr DCR, Harold GT, 2013. Young adult outcomes associated with teen pregnancy among high-risk girls in a randomized controlled trial of multidimensional treatment foster care. J. Child Adolesc. Subst. Abuse 22 (5), 421–434. 10.1080/1067828X.2013.788886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle HA, 2016. Multidimensional family therapy: evidence base for transdiagnostic treatment outcomes, change mechanisms, and implementation in community settings. Fam. Process 55 (3), 558–576. 10.1111/famp.12243. [DOI] [PubMed] [Google Scholar]
- Markoff LS, Fallot RD, Reed BG, Elliott DE, Bjelajac P, 2005. Implementing trauma-informed alcohol and other drug and mental health services for women: lessons learned in a multisite demonstration project. Am. J. Orthopsychiatry 75 (4), 525–539. 10.1037/0002-9432.75.4.525. [DOI] [PubMed] [Google Scholar]
- Messina N, Grella C, 2006. Childhood trauma and women’s health outcomes in a California prison population. Am. J. Public Health 96 (10), 1842–1848. 10.2105/AJPH.2005.082016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N, Grella CE, Cartier J, Torres S, 2010a. A randomized experimental study of gender-responsive substance abuse treatment for women in prison. J. Subst. Abuse Treat 38 (2), 97–107. 10.1016/j.jsat.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N, Grella CE, Cartier J, Torres S, 2010b. A randomized experimental study of gender-responsive substance abuse treatment for women in prison. J. Subst. Abuse Treat 38 (2), 97–107. 10.1016/j.jsat.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N, Calhoun S, Warda U, 2012. Gender-responsive drug court treatment: a randomized controlled trial. Crim. Justice Behav 39 (12), 1539–1558. 10.1177/0093854812453913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JB, 2012. Toward a New Psychology of Women. Beacon Press. [Google Scholar]
- Modrowski CA, Bennett DC, Chaplo SD, Kerig PK, 2017. Screening for PTSD among detained adolescents: implications of the changes in the DSM–5. Psychol. Trauma 9 (1), 10–17. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse, 2019. Monitoring the Future Survey: High School and Youth Trends Drug Facts. https://www.drugabuse.gov/publications/drugfacts/monitoring-future-survey-high-school-youth-trends.
- Owen B, 1998. In the Mix: Struggle and Survival in a Women’s Prison. SUNY Press, Albany, NY. [Google Scholar]
- Owen Barbara, Bloom B, 1995. Profiling women prisoners: findings from national surveys and a California sample. Prison J. 75 (2), 165–185. 10.1177/0032855595075002003. [DOI] [Google Scholar]
- Patrick ME, Evans-Polce RJ, Kloska DD, Maggs JL, 2019. Reasons high school students use marijuana: prevalence and correlations with use across four decades. J. Stud. Alcohol Drugs 80 (1), 15–25. 10.15288/jsad.2019.80.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrova D, Garcia-Retamero R, 2015. Effective evidence-based programs for preventing sexually-transmitted infections: a meta-analysis. Curr. HIV Res 13 (5), 432–438. [DOI] [PubMed] [Google Scholar]
- Prendergast ML, Messina NP, Hall EA, Warda US, 2011. The relative effectiveness of women-only and mixed-gender treatment for substance-abusing women. J. Subst. Abuse Treat 40 (4), 336–348. 10.1016/j.jsat.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME, 2019. Monitoring the Future National Survey Results on Drug Use, 1975–2018: Volume II, College Students and Adults Ages 19–60. Institute for Social Research, The University of Michigan, Ann Arbor. [Google Scholar]
- Scott T, Brown S, 2018. Risks, strengths, gender, and recidivism among justice-involved youth: a meta-analysis. J. Consult. Clin. Psychol 86 (11), 931–945. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Merrill JE, Read JP, 2012. Dimensions and severity of marijuana consequences: development and validation of the Marijuana Consequences Questionnaire (MACQ). Addict. Behav 37 (5), 613–621. 10.1016/j.addbeh.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Saldana L, 2013. Trauma, delinquency, and substance use: co-occurring problems for adolescent girls in the juvenile justice system. J. Child Adolesc. Subst. Abuse 22 (5), 450–465. 10.1080/1067828X.2013.788895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoolmiller M, Blechman E, 2005. Substance Use Is a Robust Predictor of Adolescent Recidivism. https://journals.sagepub.com/doi/abs/10.1177/0093854804274372?casa_token=U0W4UrQPqekAAAAA%3AUf3KfseV3m_gKwhXD31VwYxqWtAokjKZXJ-qrbPySCS9U_2ak4ICY684mo8ZsWiPKpqbkf1BOAEmlg&.
- Thornberry TP, Krohn MD, 2000. The self-report method for measuring delinquency and crime. In: Duffee D (Ed.), Measurement and Analysis of Crime and Justice: Criminal Justice. U.S. Department of Justice, pp. 33–84. [Google Scholar]
- Tolou-Shams M, Houck C, Conrad SM, Tarantino N, Stein LAR, Brown LK, 2011. HIV prevention for Juvenile drug court offenders: a randomized controlled trial focusing on affect management. J. Correct. Health Care 17 (3). 10.1177/1078345811401357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolou-Shams M, Dauria E, Conrad SM, Kemp K, Johnson S, Brown LK, 2017. Outcomes of a family-based HIV prevention intervention for substance using juvenile offenders. J. Subst. Abuse Treat 77, 115–125. 10.1016/j.jsat.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolou-Shams Marina, Brown LK, Marshall BDL, Dauria E, Koinis-Mitchell D, Kemp K, Poindexter B, 2020. The behavioral health needs of first-time offending justice-involved youth: substance use, sexual risk, and mental health. J. Child Adolesc. Subst. Abuse 28 (5), 291–303. 10.1080/1067828X.2020.1774023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolou-Shams Marina, Folk JB, Marshall BDL, Dauria EF, Kemp K, Li Y, Koinis-Mitchell D, Brown LK, 2021. Predictors of cannabis use among first-time justice-involved youth: a cohort study. Drug Alcohol Depend. 225, 108754 10.1016/j.drugalcdep.2021.108754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Put CE, Creemers HE, Hoeve M, 2014. Differences between juvenile offenders with and without substance use problems in the prevalence and impact of risk and protective factors for criminal recidivism. Drug Alcohol Depend. 134, 267–274. 10.1016/j.drugalcdep.2013.10.012. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, AbiNader M, Salas-Wright CP, Holzer K, Oh S, Chang Y, 2020. Trends in cannabis use among justice-involved youth in the United States, 2002–2017. Am. J. Drug Alcohol Abuse 46 (4), 462–471. 10.1080/00952990.2020.1732398. [DOI] [PubMed] [Google Scholar]
- Walker SC, Duong M, Hayes C, Berliner L, Leve LD, Atkins DC, Herting JR, Bishop AS, Valencia E, 2019. A tailored cognitive behavioral program for juvenile justice-referred females at risk of substance use and delinquency: A pilot quasi-experimental trial. PLoS One 14 (11), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkelman TNA, Frank JW, Binswanger IA, Pinals DA, 2017. Health conditions and racial differences among justice-involved adolescents, 2009 to 2014. Acad. Pediatr 17 (7), 723–731. 10.1016/j.acap.2017.03.003. [DOI] [PubMed] [Google Scholar]


