Abstract
Background
Intravenous recombinant tissue plasminogen activator (r-tPA) and urokinase (UK) are both recommended for the treatment of acute ischaemic stroke (AIS) in China, but with few comparative outcome data being available. We aimed to compare the outcomes of these two thrombolytic agents for the treatment of patients within 4.5 hours of onset of AIS in routine clinical practice in China.
Methods
A pre-planned, prospective, nationwide, multicentre, real-world registry of consecutive patients with AIS (age ≥18 years) who received r-tPA or UK within 4.5 hours of symptom onset according to local decision-making and guideline recommendations during 2017–2019. The primary effectiveness outcome was the proportion of patients with an excellent functional outcome (defined by modified Rankin scale scores 0 to 1) at 90 days. The key safety endpoint was symptomatic intracranial haemorrhage according to standard definitions. Multivariable logistic regression was used for comparative analysis, with adjustment according to propensity scores to ensure balance in baseline characteristics.
Results
Overall, 4130 patients with AIS were registered but 320 had incomplete or missing data, leaving 3810 with available data for analysis of whom 2666 received r-tPA (median dose 0.88 (IQR 0.78–0.90) mg/kg) and 1144 received UK (1.71 (1.43–2.00)×104 international unit per kilogram). There were several significant intergroup differences in patient characteristics: r-tPA patients were more educated, had less history of stroke, lower systolic blood pressure, greater neurological impairment and shorter treatment times from symptom onset than UK patients. However, in adjusted analysis, the frequency of excellent outcome (OR 1.18, 95% CI 1.00 to 1.40, p=0.052) and symptomatic intracranial haemorrhage (OR 0.70, 95% CI 0.33 to 1.47, p=0.344) were similar between groups.
Conclusions
UK may be as effective and carry a similar safety profile as r-tPA in treating mild to moderate AIS within guidelines in China.
Registration
http://www.clinicaltrials.gov. unique identifier: NCT02854592.
Keywords: thrombolysis, stroke
Introduction
Intravenous recombinant tissue plasminogen activator (r-tPA) is the regulatory-approved, guideline-recommended standard thrombolytic treatment for patients with acute ischaemic stroke (AIS) worldwide. However, another intravenous thrombolytic agent, urokinase (UK), is also variably used for the treatment of AIS in Asian countries, and is including being regulatory approved for such use in China1 a positive result in a large national multicentre clinical trial.2 Chinese guidelines recommend UK for use within 6 hours of onset of AIS (class II, level B) as an alternative to r-tPA with its shorter (4.5 hours) therapeutic time window (class I, level B).1 3 Given that UK has a much cheaper and may have an apparent longer therapeutic time window than r-tPA, additional comparative data for these two agents could have broader relevance to clinical practice, particularly in low resource settings. We undertook a ‘real world’ national, INtravenous Thrombolysis REgistry for Chinese Ischaemic Stroke within 4.5 hours of onset (INTRECIS) registry study to compare the outcomes between intravenous r-tPA and UK within 4.5 hours of AIS.
Methods
Study design
INTRECIS was a nationwide, multicentre, prospective registry of consecutive adult patients (age ≥18 years) with CT or MRI confirmed AIS who were previously well (modified Rankin scale (mRS) scores 0 or 1) and were eligible for treatment with either intravenous r-tPA or UK within 4.5 hours of a definite time of onset of symptoms. Patients were excluded if they had a history of intracranial haemorrhage (subarachnoid, intracranial and haemorrhagic transformation of cerebral infarction); head injury or acute stroke within 3 months; known intracranial tumour, arteriovenous malformation or aneurysm; intracranial or spinal cord surgery within 3 months; gastrointestinal or urinary tract haemorrhage within the previous 21 days; low blood glucose level (<2.7 mmol/L or <50 mg/dL); use of heparin or oral anticoagulation therapy within 48 hours; use of warfarin with an international normalised ratio >1.7 or prothrombin time >15 s; severe systemic disease with poor life expectancy (<3 months); major surgery within 1 month; uncontrolled hypertension (systolic pressure ≥180 mm Hg and/or diastolic pressure ≥100 mm Hg); thrombocytopenia (platelet count <10×109/L); and involvement in a clinical trial within 3 months. After the attending clinician provided information on the evidence for the agents, their costs and rationale for the research study, all patients and/or their legally authorised surrogate decided on which thrombolytic agent to use, and provided informed consent for data collection and follow-up.
Procedures
Participating patients with AIS received different doses of r-tPA (0.6–0.9 mg/kg over 60 min) or UK (1.0–1.5×1 000 000 U/kg), according to their age and neurological severity. For example, higher dose was generally chosen for younger patients with greater neurological severity on the National Institutes of Health Stroke Scale (NIHSS), whereas lower doses were used for older patients with lower NIHSS scores. All other management, including the use of antiplatelets, statins and antihypertensive agents, were given according to guideline recommendations. Demographic, clinical (including neurological severity on the NIHSS) and functional assessment on the mRS were obtained at admission, 24 hours, and 7 and 14 days in-person, and at 90 days in-person or by telephone, post-thrombolysis.
Outcomes
The primary outcome was ‘excellent recovery’ (mRS scores 0 to 1) at 90 days. Secondary outcomes were ‘functional independence’ (mRS scores 0 to 2), recurrent stroke, all-cause mortality and early change in NIHSS scores. The primary safety endpoint was symptomatic intracerebral haemorrhage (sICH), defined as an increase of ≥4 on scores on the NIHSS caused by intracranial haemorrhage within 36 hours,4 with all clinician-reported details centrally adjudicated. All the patients with neurological worsening received CT or MRI to identify the occurrence of intracerebral haemorrhage. Other safety outcomes included any bleeding or severe adverse event.
Statistical analysis
Previous studies indicate that approximately 48% of patients with AIS have a 90-day favourable outcome (mRS 0 to 1) after r-tPA,5 but such data are more limited for UK. We estimated that 2800 patients would be required for 90% power (two tailed α 0.05) to detect a 6% absolute intergroup difference in the primary outcome (ie, 48% vs 42% in the r-tPA and UK groups, respectively). However, taking account of the greater utilisation of r-tPA over UK, and assuming 10% missing outcome data, the sample size was increased to 4000 patients, that of 2600 and 1400 for the r-tPA and UK groups, respectively.
We performed propensity score matching (PSM) between patients with guideline-recommended standard-dosage r-tPA (0.9 mg/kg) and UK (1.0–1.5×1 000 000 U). PSM was performed with the ratio of 1:1, calliper of 0.1 and a nearest-neighbour matching strategy by R software V.3.6.3. PSM was operated with control factors including age, gender, body mass index, current smoker, current drinker, hypertension, diabetes mellitus, history of stroke, coronary heart disease, atrial fibrillation, onset-to-treatment time, door-to-needle time, systolic blood pressure, NIHSS score at admission, pathological subtype of AIS according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification system, hospital classification and educational level.
Two-sample t-test or Wilcoxon rank test and χ2 test were used to assess differences in baseline variables according to continuous or categorical distribution, respectively. Propensity score analysis was used to adjust for baseline imbalances, whereby the score (predicted probability of a patient receiving r-tPA) calculated in a multivariable logistic regression model was used as a covariate in adjusted analyses. Differences between the two agents were assessed across six subgroups defined by age (<65 and ≥65 years), sex, history of stroke and baseline NIHSS score (≤5 vs >5), onset to treatment time (<180 vs 180–270 min) and systolic blood pressure (<140 vs ≥140 mm Hg). Data are reported with ORs and 95% CIs.
Generalised estimating equation (GEE) models with normal distribution and identity link function were used for analysis of continuous outcomes with repeated measurements, such as change in NIHSS scores between admission and day 1 and day 14. The GEE model included treatment, time, and interaction between treatment and time as fixed effects, baseline measurement and propensity score as covariates, and patient as a cluster effect. Sensitivity analyses of outcomes were performed by replacing propensity score with individual baseline covariates in regression models. All analyses were performed on a complete case series. Sensitivity analyses were performed by imputing missing baseline covariates using a simple imputation method based on their sample distributions (eg, imputation of a missing value for a continuous variable by a normal distribution derivation given sample mean and standard derivation). A p value <0.05 was considered statistically significant. All analyses were performed using SAS V.9.4 (SAS Institute, Cary, NC, USA).
Results
Overall, 4130 consecutive patients with AIS were enrolled in the study between 1 April 2017 and 1 July 2019, of whom 245 were excluded for various reasons and 75 lost to follow-up (online supplemental figure S1). Thus, 3810 patients (2666 and 1144 in r-tPA and UK groups, respectively) were included in the analysis set. Table 1 shows the baseline characteristics of participants, with the r-tPA group being more educated, had less history of stroke, lower systolic blood pressure, but presented with greater neurological deficit and shorter times from symptom onset to treatment, than those in the UK group. The distribution of r-tPA and UK across participating sites is shown in online supplemental figure S2.
Table 1.
Baseline characteristics
| Variable | r-tPA (N=2666) | UK (N=1144) | P value |
| Dose, mg/U per kg | 0.88 (0.78–0.90) | 1.71 (1.43–2.00)×104 | – |
| Age, years | 63.8 (11.5) | 63.5 (63.8) | 0.399 |
| Male | 1827 (68.5) | 779 (68.1) | 0.791 |
| BMI, kg/m2 | 24.1 (3.8) | 24.2 (3.4) | 0.490 |
| Educational level | 0.006 | ||
| Primary school degree or below | 762 (28.6) | 370 (32.3) | |
| Middle school degree | 1623 (60.9) | 685 (59.5) | |
| Bachelor degree or above | 281 (10.5) | 89 (7.8) | |
| Current smoker | 1006 (37.7) | 442 (38.6) | 0.599 |
| Current drinker | 607 (22.8) | 279 (24.4) | 0.278 |
| Hypertension | 1435/2599 (55.2) | 599/1097 (54.6) | 0.733 |
| Coronary heart disease | 394/2549 (15.5) | 167/1069 (15.6) | 0.900 |
| History of stroke | 532/2573 (20.7) | 263/1089 (22.6) | 0.020 |
| Diabetes mellitus | 507/2600 (19.5) | 209/1092 (19.1) | 0.800 |
| Atrial fibrillation | 254/2547 (10.0) | 93/1064 (8.7) | 0.252 |
| SBP, mm Hg | 151.2 (22.8) | 153.3 (23.7) | 0.009 |
| OTT, min | 170 (128–210) | 190 (142–234) | <0.001 |
| DNT, min | 30 (14–55) | 35 (18–61) | <0.001 |
| NIHSS score | 6.0 (3.0–10.0) | 5.0 (3.0–9.0) | 0.010 |
| TOAST classification | 0.639 | ||
| LAA | 1297 (49.4) | 538 (47.7) | |
| CE | 304 (11.6) | 124 (11.0) | |
| SAO | 814 (31.0) | 378 (33.5) | |
| ODC | 63 (2.4) | 24 (2.1) | |
| UND | 149 (5.7) | 65 (5.8) | |
| Hospital classification | 0.417 | ||
| Tertiary | 2418 (90.7) | 1047 (91.5) | |
| Secondary | 248 (9.3) | 97 (8.5) |
Data are n/N (%), mean (SD) or median (IQR).
BMI, body mass index; CE, cardioembolism; DNT, door-to-needle time; LAA, large-artery atherosclerosis; NIHSS, National Institutes of Health Stroke Scale; ODC, stroke of other determined cause; OTT, onset-to-treatment time; r-tPA, recombinant tissue plasminogen activator; SAO, small-artery occlusion; SBP, systolic blood pressure; TOAST, Trial of Org 10172 in Acute Stroke Treatment; UK, urokinase; UND, stroke of undetermined cause.
svn-2020-000640supp001.pdf (455KB, pdf)
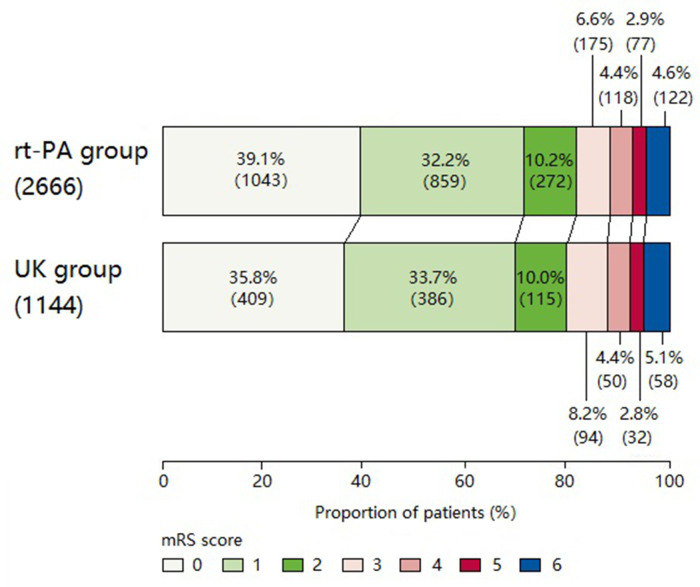
Tables 2 and 3 show that the primary endpoint of excellent recovery (mRS scores 0 to 1) at 90 days was similar between the two groups: r-tPA (71.3%) and UK (69.5%), with unadjusted OR 1.09 (95% CI 0.94 to 1.27, p=0.250) and adjusted OR 1.15 (95% CI 0.98 to 1.35, p=0.078). The distribution of the full range of mRS scores was comparable between the groups (figure 1). Table 2 also showed similarly comparable secondary clinical outcomes and safety between the two groups. The consistency of the results was confirmed in sensitivity analysis using different methods of adjustment for potential baseline confounders (table 3). Other than a borderline significant effect of age and educational level on the primary outcome, there was consistency in primary effectiveness outcome across subgroups (online supplemental figure S3).
Table 2.
Effectiveness and safety outcomes for rt-PA and UK
| Outcome | rt-PA n/N (%) | UK n/N (%) | Unadjusted OR or mean difference (95% CI) | P value | Adjusted OR or mean difference (95% CI)* | P value |
| mRS scores 0 to 1 at 90 days | 1902/2666 (71.3) | 795/1144 (69.5) | 1.09 (0.94 to 1.27) | 0.250 | 1.15 (0.98 to 1.35) | 0.078 |
| mRS scores 0 to 2 at 90 days | 2174/2666 (81.5) | 910/1144 (79.5) | 1.14 (0.96 to 1.35) | 0.150 | 1.22 (1.01 to 1.46) | 0.036 |
| mRS distribution at 90 days | 0.369 | 0.140 | ||||
| 0 | 1043/2666 (39.1) | 409/1144 (35.8) | ||||
| 1 | 859/2666 (32.2) | 386/1144 (33.7) | ||||
| 2 | 272/2666 (10.2) | 115/1144 (10.1) | ||||
| 3 | 175/2666 (6.6) | 94/1144 (8.2) | ||||
| 4 | 118/2666 (4.4) | 50/1144 (4.4) | ||||
| 5 | 77/2666 (2.9) | 32/1144 (2.8) | ||||
| 6 | 122/2666 (4.6) | 58/1144 (5.1) | ||||
| ΔNIHSS score to 24 hours† | 2.4±5.1 | 2.0±4.4 | 0.20 (−0.21 to 0.61) | 0.334 | 0.23 (−0.10 to 0.57) | 0.173 |
| ΔNIHSS score to 14 days† | 3.7±6.1 | 3.1±5.5 | 0.14 (−0.25 to 0.53) | 0.470 | 0.28 (−0.14 to 0.70) | 0.194 |
| sICH at 36 hours | 30/2666 (1.1) | 16/1144 (1.4) | 0.80 (0.44 to 1.48) | 0.479 | 0.69 (0.35 to 1.35) | 0.281 |
| Other bleeding events | 30/2666 (1.1) | 8/1144 (0.7) | 1.62 (0.74 to 3.54) | 0.230 | 1.48 (0.66 to 3.29) | 0.341 |
| Recurrent stroke at 90 days | 36/2557 (1.4) | 28/1097 (2.6) | 0.55 (0.33 to 0.90) | 0.016 | 0.57 (0.34 to 0.94) | 0.028 |
| All-cause mortality at 90 days | 122/2666 (4.6) | 58/1144 (5.1) | 0.90 (0.65 to 1.24) | 0.510 | 0.76 (0.52 to 1.12) | 0.164 |
*Propensity scores adjustment for all baseline variables in the model.
†From baseline.
mRS, modified Rankin scale; NIHSS, National Institutes of Health Stroke Scale; rt-PA, recombinant tissue plasminogen activator; sICH, symptomatic intracerebral haemorrhage; UK, urokinase.
Table 3.
Sensitivity analysis for different methods of adjustment
| Outcome | Adjusted OR or mean difference (95% CI)* | P value | Adjusted OR or mean difference (95% CI)† | P value |
| mRS scores 0 to 1 at 90 days | 1.19 (1.00 to 1.42) | 0.047 | 1.15 (0.98 to 1.35) | 0.078 |
| mRS scores 0 to 2 at 90 days | 1.27 (1.04 to 1.56) | 0.021 | 1.22 (1.01 to 1.46) | 0.036 |
| mRS distribution at 90 days | 0.060 | 0.140 | ||
| ΔNIHSS score to 24 hours‡ | 0.24 (−0.07 to 0.55) | 0.125 | 0.23 (−0.10 to 0.57) | 0.173 |
| ΔNIHSS score to 14 days‡ | 0.28 (−0.09 to 0.65) | 0.133 | 0.28 (−0.14 to 0.70) | 0.194 |
| sICH at 36 hours | 0.72 (0.36 to 1.43) | 0.349 | 0.69 (0.35 to 1.35) | 0.281 |
| Other bleeding events | 1.43 (0.64 to 3.19) | 0.384 | 1.48 (0.66 to 3.29) | 0.341 |
| Recurrent stroke at 90 days | 0.57 (0.34 to 0.95) | 0.030 | 0.57 (0.34 to 0.94) | 0.028 |
| All-cause mortality at 90 days | 0.74 (0.49 to 1.11) | 0.148 | 0.76 (0.52 to 1.12) | 0.164 |
*Adjustment with all baseline variables in the model.
†Propensity scores used to adjust all baseline variables in the model.
‡From baseline.
mRS, modified Rankin scale; NIHSS, National Institutes of Health Stroke Scale; rt-PA, recombinant tissue plasminogen activator; sICH, symptomatic intracerebral haemorrhage; UK, urokinase.
Figure 1.
Distribution of modified Rankin Scale (mRS) score.
In addition, we determined the effectiveness and safety outcomes in PSM patients with guideline-recommended standard-dosage r-tPA (0.9 mg/kg) and UK (1.0–1.5×1 000 000 U) where there were no significant differences in baseline characteristics between the two groups (online supplemental table S1). The primary endpoint of excellent recovery (mRS scores 0 to 1) was similar between the two groups: r-tPA (71.5%) and UK (69.2%), OR 1.12 (95% CI 0.90 to 1.39, p=0.316). The secondary clinical safety outcomes were also comparable between the two groups (online supplemental table S2).
We also performed dichotomised analysis by NIHSS scores 1–5 and 6–10 in patients with 0.9 mg/kg r-tPA versus 1.0–1.5×1 000 000 U UK, where again there was similar effectiveness and safety outcomes (online supplemental table S3 and S4).
Discussion
This large multicentre prospective registry study specifically designed to compare r-tPA with UK in patients with AIS has shown that they are associated with similar effectiveness and safety outcome that are relevant to ‘real world’ clinical practice in China.
As second-generation thrombolytic drug, r-tPA, a serine protease that converts the proenzyme plasminogen into the proteinase plasmin, was approved as the standard thrombolytic treatment for AIS across the world on the basis of the National Institutes of Stroke and Neurological Diseases trial, published in 1995.6 However, the first-generation thrombolytic agent UK, which acts directly to convert plasminogen to plasmin,7 has also undergone investigations in AIS,1 8–10 most as low dose administered over several days (240 000–600 000 U/day).8–10 However, a Chinese national muticentre UK trial showed that two higher doses of UK (1 000 000 or 1 500 000 U/patient) given over 30 min were similarly effective when administered within 6 hours of AIS,2 which resulted in it being approved for use (class II, level B).1 3 However, these results were criticised outside of China,11 which together with its variable supply have made UK seldom used for AIS outside of Asia. Prior to the advent of modern endovascular clot retrieval, intra-arterial UK was a popular treatment of large vessel occlusive AIS on the basis of several positive small trials,12–16 and despite the potential of a higher bleeding risk due to its low fibrin specificity.7 Our study is the first indirect comparison of r-tPA and UK, where the possibly similar effectiveness and safety to r-tPA, but much lower price, makes UK an attractive option in low resource settings. The lower rate of sICH and higher rate of excellent recovery found in our study is comparable with an early study.4 17 The lower rate of sICH in our study compared with ECASS II and ECASS III study could possibly be due to the inclusion of patients with predominantly mild neurological deficits, ethnic differences in risk and where some patients were given lower doses of the agents in practice. A meta-analysis has shown that the risk of sICH according to SITS-MOST ranged from 1.5% for AIS with NIHSS scores of 0–4 and ≥22, respectively,18 while a retrospective study showed the risk of sICH was 1.8%.19 The multinational Enhanced Control of Hypertension ANd Thrombolysis strokE Study (ENCHANTED) clinical trial showed that sICH occurred in 1.0% of the participants in low-dose compared with in 2.1% standard-dose rtPA groups.20
The strengths of our study include the large sample size, minimum selection bias from the consecutive recruitment of patients into a prospective registry and the systematic data collection of variables within routine practice. As shown in ENCHANTED,21 there was no clear non-inferiority of low (0.6 mg/kg) compared with standard (0.9 mg/kg) doses of intravenous r-tPA on functional outcomes for thrombolysed patients with AIS with mild–moderate severity (NIHSS scores 5–6). Our study showed that a high dose of UK is associated with comparable clinical outcomes with the use of variable doses of r-tPA, and without any increase in sICH: a suitable weight-adjusted dose of UK is 250 000×104 U/kg.
However, we recognise several limitations, most importantly being the lack of randomisation that precluded an ability to fully adjust for measured and unmeasured confounders. Another is the conduct limited to China, where differences in the body mass, comorbid factors and patterns of cerebrovascular disease in patients with AIS compared with other populations may raise concerns over the generalisability of our results. There may also be concerns over potential variability in the potency of UK across sites in relation to it being sourced from different manufacturers. However, all these issues may also strengthen the relevance of the findings to current practice. In addition, we have not collected the premorbid mRS in the current study, although all enrolled patients were previously well (mRS score 0 or 1). Finally, despite the adoption of standardised protocol, the open design could have introduced various assessment, reporting and indication biases.
Conclusions
In summary, our prospective national registry study suggests that UK may be as safe and effective as r-tPA in treating mild to moderate acute ischaemic stroke within 4.5 hours, on the basis of equivalent outcomes. These results provide additional support for guidelines recommending UK as a suitable cost-effective alternative to r-tPA for AIS in China. Further multinational, multicentre, randomised controlled comparative-effectiveness studies of these and other lytic agents may now be warranted.
Footnotes
Contributors: XW, XL and HC: conception and design; YX, RL, QY, YZ, FW, BS, RW, SC, LW, LS and BP: collection and assembly of data; XH, YC and DW: data analysis and interpretation; XW, XL, CSA, HC: manuscript writing.
Funding: This study was funded by National Key R&D Program of China (2017YFC1308200) and Stroke Prevention and Treatment Project of the National Health Commission - Research and Popularization of Appropriate Intervention Technology for the Stroke High Risk Group in China (GN-2016R0008).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was centrally approved by General Hospital of the Northern Theatre Command (the former General Hospital of Shenyang Military Region), China.
References
- 1. Neurology branch of Chinese Medical Association . Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol [Chinese] 2018;51:666–82. [Google Scholar]
- 2. Cooperating Group for National 95’s Project. Intravenous thrombolysis with urokinase for acute cerebral infarctions. Chin J Neurol [Chinese] 2002;35:210–3. [Google Scholar]
- 3. Dong Q, Dong Y, Liu L, et al. The Chinese Stroke Association scientific statement: intravenous thrombolysis in acute ischaemic stroke. Stroke Vasc Neurol 2017;2:147–59. 10.1136/svn-2017-000074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hacke W, Kaste M, Fieschi C, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 1998;352:1245–51. 10.1016/s0140-6736(98)08020-9 [DOI] [PubMed] [Google Scholar]
- 5. Xu Y, Hackett ML, Chalmers J, et al. Frequency, determinants, and effects of early seizures after thrombolysis for acute ischemic stroke: the ENCHANTED trial. Neurol Clin Pract 2017;7:324–32. 10.1212/CPJ.0000000000000384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group . Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581–8. 10.1056/NEJM199512143332401 [DOI] [PubMed] [Google Scholar]
- 7. Murray V, Norrving B, Sandercock PAG, et al. The molecular basis of thrombolysis and its clinical application in stroke. J Intern Med 2010;267:191–208. 10.1111/j.1365-2796.2009.02205.x [DOI] [PubMed] [Google Scholar]
- 8. Abe T, Kazama M, Naito I, et al. Clinical evaluation for efficacy of tissue cultured urokinase (TCUK) on cerebral thrombosis by means of multi-centre double blind study. Blood & Vessel 1981;12:321–41. 10.2491/jjsth1970.12.321 [DOI] [Google Scholar]
- 9. Atarashi J, Ohtomo E, Araki G. Clinical utility of urokinase in the treatment of acute stage cerebral thrombosis: multi-center double blind study in comparison with placebo. Clin Eval 1985;13:659–709. [Google Scholar]
- 10. Ohtomo E, Araki G, Itoh E. Clinical efficacy of urokinase in the treatment of cerebral thrombosis: multi-centre double-blind study in comparison with placebo. Clin Eval 1985;15:711–31. [Google Scholar]
- 11. Wardlaw JM, Murray V, Berge E. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 2014;2014:CD000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Macleod MR, Davis SM, Mitchell PJ, et al. Results of a multicentre, randomised controlled trial of intra-arterial urokinase in the treatment of acute posterior circulation ischaemic stroke. Cerebrovasc Dis 2005;20:12–17. 10.1159/000086121 [DOI] [PubMed] [Google Scholar]
- 13. Ogawa A, Mori E, Minematsu K, et al. Randomized trial of intraarterial infusion of urokinase within 6 hours of middle cerebral artery stroke: the Middle Cerebral Artery Embolism Local Fibrinolytic Intervention Trial (MELT) Japan. Stroke 2007;38:2633–9. 10.1161/STROKEAHA.107.488551 [DOI] [PubMed] [Google Scholar]
- 14. Brekenfeld C, Remonda L, Nedeltchev K, et al. Symptomatic intracranial haemorrhage after intra-arterial thrombolysis in acute ischaemic stroke: assessment of 294 patients treated with urokinase. J Neurol Neurosurg Psychiatry 2007;78:280–5. 10.1136/jnnp.2005.078840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. van Houwelingen RC, Luijckx G-J, Mazuri A, et al. Safety and outcome of intra-arterial treatment for basilar artery occlusion. JAMA Neurol 2016;73:1225–30. 10.1001/jamaneurol.2016.1408 [DOI] [PubMed] [Google Scholar]
- 16. Kaesmacher J, Bellwald S, Dobrocky T, et al. Safety and efficacy of intra-arterial urokinase after failed, unsuccessful, or incomplete mechanical thrombectomy in anterior circulation large-vessel occlusion stroke. JAMA Neurol 2020;77:318–26. 10.1001/jamaneurol.2019.4192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317–29. 10.1056/NEJMoa0804656 [DOI] [PubMed] [Google Scholar]
- 18. Whiteley WN, Emberson J, Lees KR, et al. Risk of intracerebral haemorrhage with alteplase after acute ischaemic stroke: a secondary analysis of an individual patient data meta-analysis. Lancet Neurol 2016;15:925–33. 10.1016/S1474-4422(16)30076-X [DOI] [PubMed] [Google Scholar]
- 19. Romano JG, Smith EE, Liang L, et al. Outcomes in mild acute ischemic stroke treated with intravenous thrombolysis: a retrospective analysis of the Get With the Guidelines-Stroke registry. JAMA Neurol 2015;72:423–31. 10.1001/jamaneurol.2014.4354 [DOI] [PubMed] [Google Scholar]
- 20. Anderson CS, Robinson T, Lindley RI, et al. Low-dose versus standard-dose intravenous alteplase in acute ischemic stroke. N Engl J Med 2016;374:2313–23. 10.1056/NEJMoa1515510 [DOI] [PubMed] [Google Scholar]
- 21. Wang X, Robinson TG, Lee T-H, et al. Low-dose vs standard-dose alteplase for patients with acute ischemic stroke: secondary analysis of the ENCHANTED randomized clinical trial. JAMA Neurol 2017;74:1328–35. 10.1001/jamaneurol.2017.2286 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
svn-2020-000640supp001.pdf (455KB, pdf)
Data Availability Statement
Data are available on reasonable request.