Abstract
Background:
Patient care aides, who provide basic care to patients in a variety of healthcare settings, have been observed to have higher prevalences of adverse health metrics than the general U.S. workforce. However, few studies have examined how healthcare access and health behaviors and outcomes among patient care aides differ by work setting (home health, nursing home, and hospital).
Methods:
Data from the 2013–2016 Behavioral Risk Factor Surveillance System (BRFSS) were used to assess prevalences of healthcare access, health-related behaviors, and health outcomes among patient care aides in different work settings, and among nurses (licensed vocational/practical and registered). Adjusted prevalence ratios were used to compare prevalences for healthcare workers to those for non-healthcare clerical workers.
Results:
Overall, patient care aides are a low-wage workforce with high prevalences of multiple adverse health metrics and low prevalences of positive health behaviors compared to clerical workers. Results differed by work setting. Home health aides had the lowest income levels and most adverse results for multiple metrics; nursing home aides had better healthcare access and somewhat better health outcomes. Most metrics were best (though still quite poor) for hospital aides, who showed few significant differences from clerical workers.
Conclusions:
These results show the need to focus resources on the patient care aide workforce, particularly those in home health. While some needs of nursing home aides, such as improving influenza vaccination coverage and reducing the prevalence of arthritis-related conditions, would benefit from standardized workplace interventions, alternate, workplace-specific approaches are needed for home health aides.
INTRODUCTION
Workers in healthcare support occupations, a diverse group ranging from orderlies to pharmacy aides (U.S. Census occupation codes 3600–3650), have been found to have significantly higher prevalences of several adverse health outcomes than other workers. Healthcare support workers have been observed to have higher prevalences than most other occupational groups for short sleep,1 and current asthma,2,3 and obesity (male workers only).4 However, health behaviors and outcomes are not uniform across this workforce. For example, in a study of short sleep, nursing, psychiatric and home health aides had the highest adjusted prevalence, at 43%.1 Adverse health metrics in the healthcare workforce can negatively impact not only the health of these workers but also patient safety and health. 5 Design of effective interventions to decrease the prevalence of adverse health metrics among healthcare support workers (and consequences to patients) requires understanding health disparities among specific workforces within the larger healthcare support group.
The U.S. Census occupation grouping “Nursing, psychiatric, and home health aides” comprises a large, low-wage segment of the healthcare support workforce. These workers, who are employed primarily in nursing homes, private homes, and hospitals, perform a variety of hands-on patient care activities, ranging from bathing to checking vital signs. The nomenclature, training, and activities for these workers vary by state, work setting and even workplace; henceforth, for this research, they will be referred to collectively as “patient care aides.”
In 2017, an estimated 2,393,040 workers were employed as patient care aides;6 the number of patient care aides was projected to increase by 24% in the period 2016–2026, with jobs for home health aides expected to rise most sharply, by 47%, during this time period.7 In 2017, the median wage for this workforce was $12.31 per hour.6 Wages affect healthcare access both directly and through healthcare insurance coverage.8,9
Past surveys, including the 2007 National Home Health Aide Survey10 and the 2004 National Nursing Assistant Survey11 provided assessments of patient care aides in specific settings and identified a number of exposure hazards, as well as elevated prevalence of adverse outcomes, including violence, injuries, and musculoskeletal disorders (MSDs), among specific subsets of workers.12–15 However, few studies have comprehensively examined how health metrics for patient care aides differ by work setting. Identifying the prevalence of specific adverse metrics by work setting can inform decisions about prioritizing potential improvements; moreover, the work setting can influence both the extent of health-related problems and the feasibility of potential solutions.
The Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System (BRFSS) data present an opportunity to estimate prevalences for a range of health-related metrics among patient care aides by setting. While assessment of chronic health outcomes among healthcare support workers are often limited to those that are most often connected to work, such as MSDs and, to some extent, asthma, BRFSS covers multiple chronic conditions, as well as metrics for healthcare access and health-related behaviors.
The current analysis of 2013–2016 BRFSS data examined prevalences of multiple health metrics among patient care aides in the home health, nursing home, and hospital settings, as well as among licensed vocational nurses/licensed practical nurses (LVNs/LPNs) and registered nurses (RNs). A subset of non-healthcare clerical and secretarial workers were the comparison group. The purpose of this investigation was to identify setting-specific differences in health metrics within the patient care aide workforce, in order to facilitate targeted workplace-specific interventions for the groups at highest risk.
METHODS
The BRFSS is a national survey administered by state health departments via landline and cellular phones to the U.S. non-institutionalized adult population (18 years or older).16 Persons in the U.S. non-institutional adult population (18 years or older) are selected to complete the survey using random digit dialing techniques on both landlines and cell phones. From 2013–2016, the BRFSS response rate across states ranged from 30.7% to 65.0%, with response rates for cell phone responders increasing comparing 2013 to 2016 from 37.8% to 46.4% and those for landlines decreasing slightly from 49.6% to 47.7%. Response rates overall and by state can be found at https://www.cdc.gov/brfss/data_documentation/index.htm.
The BRFSS includes a core survey, as well as optional modules that states can choose to include. Since 2013, the survey has included a module sponsored by the National Institute for Occupational Safety and Health (NIOSH) to elicit the industry and occupation of respondents who are employed for wages, out of work for less than one year, or self-employed. Different states have administered the industry and occupation module during 2013–2016, with 14 states participating all four years and 25 states for at least one of the four years.17 Industry and occupation, respectively, were elicited by open-ended questions: “What kind of work do you do?” followed by “What kind of business or industry do you work in?” Data used for the analyses were from all states that used the industry and occupation (I/O) module for at least one year during 2013–2016. In addition, Washington and Wyoming collected industry and occupation information using state-added questions in 2013.18,19 In Washington in 2013, the state-added questions were asked in the opposite order from that used in the BRFSS module. Responses to the 2013 questions added by Washington and Wyoming were used as well. State participation in the BRFSS I/O module by year is presented in Online Appendix A.
BRFSS respondents who reported that they were currently employed (employed for wages or self-employed at any time in the past 12 months) comprised the study population. In total, 429,344 study respondents from the BRFSS survey years 2013–2016 indicated they were employed or self-employed in responses to either the I/O module or the state-added questions at the time they were surveyed. Of these respondents, 61,012 (14.2%) were excluded because industry or occupation was missing or could not be coded; because they were active military; or because of conflicting employment status information. Responses were autocoded by the NIOSH Industry and Occupation Computerized Coding System or by human coders using computer-assisted coding to the 2002 U.S. Census Bureau industry and occupation codes.20
Census industry and occupation groups and the associated codes that were the focus of these analyses are shown in Figure 1. The patient care aide workforce comprises nursing, psychiatric, and home health aides. Patient care aides were identified by selecting nursing, psychiatric, and home health aides (Census occupation code 3600) and subdividing them into the following settings by Census industry code: 1) nursing homes; 2) home health; and 3) hospitals. Although patient care aides are also found in the outpatient setting, the Census code for this industry also includes workers for whom industry could not be identified, and results would be difficult to interpret. Another occupational group, personal and home care aides (Census occupation code 4610), has some overlap in coverage and function with patient care aides, particularly in the home health setting. However, many personal care aides are employed outside healthcare, and they may or may not perform medical support functions as part of their job duties. Therefore, personal care aides were not included in the primary analyses, although health outcomes including this group were assessed in an alternate analysis. Thus, for this study, the patient care aide workforce of primary interest is found in three industries: nursing homes, home health, and hospitals. These subsets of patient care aides, differentiated by work industry/setting, are referred to herein as “nursing aides”, “home health aides”, and “hospital aides” respectively.
Figure 1:
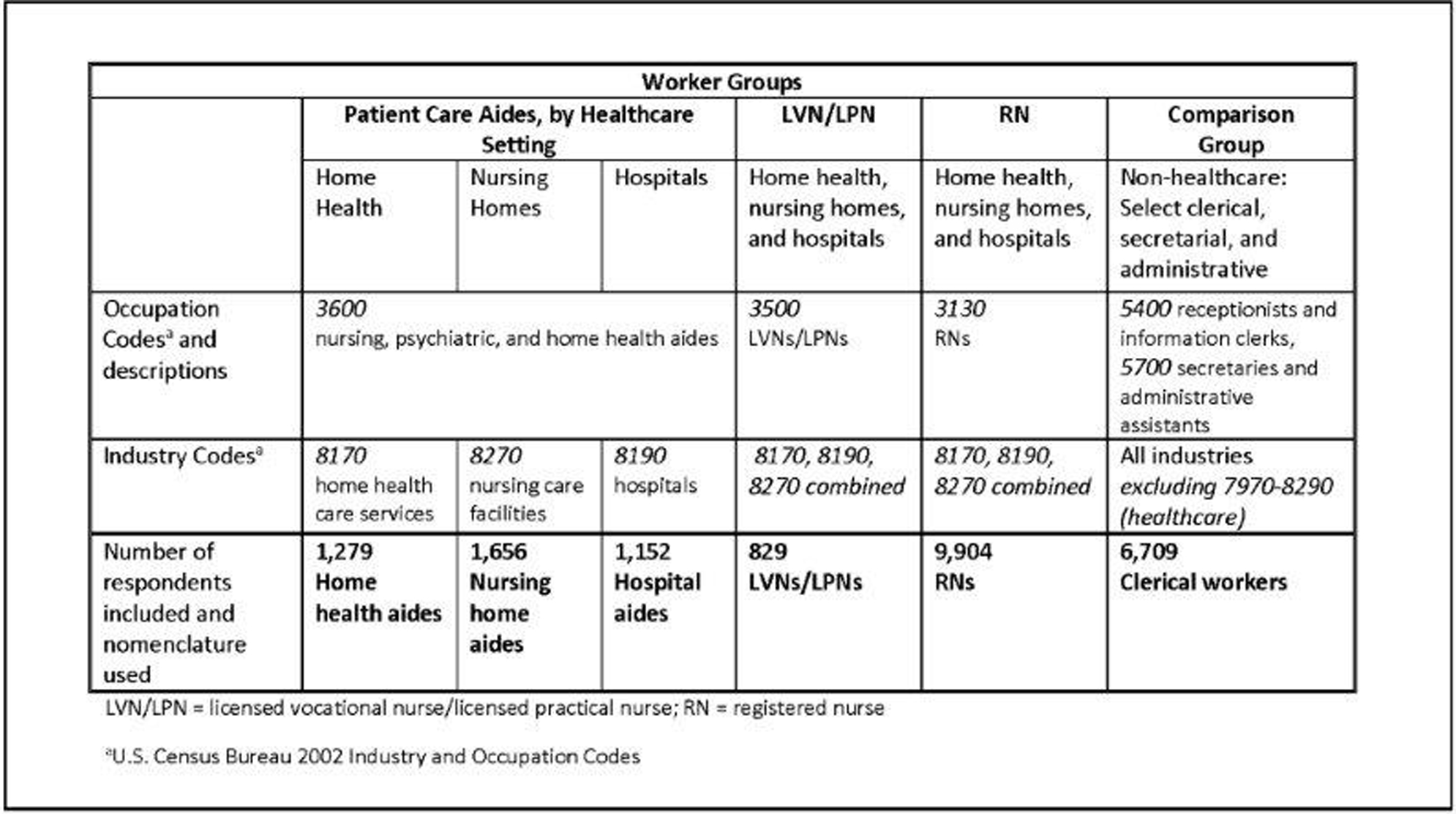
Worker Groups of Primary Interest, as Defined by 2002, U.S. Census Industry and Occupation Codes
Also included in the analyses are two groups of nurses from the three industries of interest: licensed vocational nurses/licensed practical nurses (LVNs/LPNs) and registered nurses (RNs). These groups were included because they represent potential career endpoints for patient care aides. The two groups of nurses were treated separately but not further divided by industry/work setting for the analyses.
Workers from “all other occupations” are often used as a comparison group with survey data. However, we wanted to select a workforce 1) generally free from workplace chemical and physical hazards found in some segments of the general and healthcare workforces and 2) with relatively similar demographic characteristics to the patient care aide workforce. We selected a subset of clerical, secretarial, and administrative workers (henceforth referred to as “clerical”) from outside the healthcare industry as the comparison group for patient care aides and nurses. This comparison group includes receptionists, information clerks, secretaries, and administrative assistants who worked in industries other than healthcare. In the 2013–2016 BRFSS data, these workers comprise a workforce similar to patient care aides in terms of some demographic metrics (education in particular and also age and sex), although they were more likely to be white. The household income distribution for patient care aides skews quite low compared to other workforces, including the clerical group comparison group, whose income distribution is more similar to those of the U.S. workforce as a whole.
We calculated distributions of demographic characteristics (weighted according to state distributions and then aggregated) for each group of healthcare workers and for the clerical comparison group. Health-related metrics of interest spanned three areas: healthcare access (healthcare coverage, access to health practitioners, cholesterol screening, and influenza vaccination); health-related behaviors [smoking status, binge drinking (defined as 5 or more drinks for men or 4 or more drinks for women on an occasion during the past 30 days), obesity (defined as having a Body Mass Index (BMI) of ≥30 kg/m2 based on self-reported height and weight), physical exercise, and inadequate sleep (<7 hours average sleep per 24 hour period)]; and self-reported health outcomes [self-rated general, physical and mental health; physician diagnosed high blood pressure (excluding during pregnancy), high cholesterol, depression, chronic obstructive pulmonary disease, arthritis (a range of outcomes from fibromyalgia to rheumatoid arthritis), cancer (other than skin cancer), diabetes (excluding gestational and pre/borderline diabetes), current asthma, and ever asthma].
The 2014 BRFSS data permit calculation of a simplified percentage of the Federal Poverty Level (FPL) for each responding household that reported an annual household income range for 2013, the number of adults in the household, and the number of children in the household. The BRFSS question used to assess household income is categorical (respondents select from a set of income ranges), so the midpoint of each BRFSS income range was used by BRFSS to estimate FPL and, for the top-end income level, ≥ $75,000, the weighted mean of income from census data.
We conducted all analyses using SAS version 9.4 (SAS Institute Inc., Cary, NC) and SAS-callable SUDAAN version 11.0 (RTI International, Research Triangle Park, NC) to perform analyses accounting for the complex survey design and incorporating respondent sampling weight in BRFSS. We used the SURVEYFREQ procedure to estimate population counts and weighted, but unadjusted, prevalence rates (PRs) for all variables. To examine differences in healthcare access, health behaviors, and health outcomes by workgroup, we used the RLOGISTIC procedure to perform logistic regression and estimate adjusted prevalence ratios (aPRs) and their 95% confidence intervals (CIs) comparing healthcare workers to clerical workers. We considered CIs for aPRs that do not span the null to be statistically significant.
For primary analyses, we adjusted the regression models for age in years (18–29, 30–34, 35–39,40–44, 45–49, 50–54, 55–59, 60–64, 65 or older); sex; race/ethnicity combined (classified as white non-Hispanic, black non-Hispanic, other non-Hispanic, Hispanic) and marital status (collapsed to married vs. all other due to small numbers in many categories). All percentages are weighted, unadjusted prevalences.
Because we were interested in health metrics among this group of low-wage healthcare workers specifically, because low wages are widespread across the patient care aide workforce, and because household income has complex relations with choice of occupation, healthcare access, health-related behaviors and health outcomes that cannot be adequately addressed in the context of a cross-sectional study, we did not adjust for household income in the primary analyses. However, we performed alternate analyses with income in the model; the findings are discussed in the results section and presented in full in Online Appendix B for the interested reader.
RESULTS
Demographics
Of the 368,332 BRFSS respondents who were currently working, had codable I/O, and were not active military (data not shown), the 21,529 who were in the healthcare occupations of interest or in the comparison group (non-healthcare industry clerical workers) were the focus of the analyses. The work setting distribution of the 4,087 patient care aides was as follows: 31.3% home health (n=1,279), 40.5% nursing homes (n=1,656), and 28.2% hospitals (n=1,152). Other healthcare workers of interest comprised LVN/LPNs (829) and RNs (9,904). The comparison group comprised 6,709 non-healthcare industry clerical workers.
Patient care aides were largely female (88%, data not shown). Hospitals had the highest percentage (30%) of male patient care aides (Table 1). While at least 60% of LVNs/LPNs, RNs, and clerical workers identified as non-Hispanic whites, at least 55% of patient care aides in each setting identified as Hispanic, non-Hispanic non-white, or non-Hispanic multiracial.
Table 1.
Demographics of low-wage patient care aides, LVNs/LPNs, and comparison groups, 2013–2016 Behavior Risk Factor Surveillance System (BRFSS)a
| Patient Care Aides by Setting | Nurses | Comparison Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home Health | Nursing Home | Hospital | LVN/LPN | RN | Non-healthcare Clerical | ||||||||
| Characteristic | Category | Sample Size |
Weighted % |
Sample Size |
Weighted % |
Sample Size |
Weighted % |
Sample Size |
Weighted % |
Sample Size |
Weighted % |
Sample Size |
Weighted % |
| Total Respondents Weighted N |
1,279 (262,484) |
1,656 (309,130) |
1,152 (289,753) |
829 (152,116) |
9,904 (1,688,324) |
6,709 (1,169,850) |
|||||||
| Sex | Male | 105 | 8.1 | 127 | 9.3 | 224 | 30.4 | 56 | 10.9 | 876 | 12.9 | 272 | 8.6 |
| Female | 1,174 | 91.9 | 1,529 | 90.7 | 928 | 69.6 | 773 | 89.1 | 9,027 | 87.1 | 6,437 | 91.4 | |
| Race/ethnicity | White, non-Hispanic |
762 | 45.4 | 1,011 | 45.2 | 677 | 48.7 | 632 | 60.7 | 8,155 | 66.8 | 5,612 | 71.6 |
| Black, non-Hispanic |
254 | 34.6 | 383 | 34.1 | 264 | 29.8 | 136 | 27.7 | 818 | 13.0 | 359 | 9.2 | |
| Other, non-Hispanic |
91 | 6.3 | 103 | 9.2 | 90 | 8.8 | 26 | 3.4 | 454 | 14.8 | 285 | 10.0 | |
| Hispanic | 144 | 13.7 | 140 | 11.6 | 101 | 12.7 | 26 | 8.2 | 374 | 5.48 | 390 | 9.2 | |
| Age (years) | 18–29 | 156 | 20.5 | 400 | 33.1 | 253 | 27.6 | 90 | 22.0 | 951 | 13.7 | 549 | 19.4 |
| 30–34 | 98 | 12.8 | 175 | 14.2 | 137 | 13.2 | 67 | 10.5 | 894 | 12.0 | 321 | 7.3 | |
| 35–39 | 91 | 8.0 | 146 | 9.3 | 123 | 9.7 | 73 | 11.4 | 963 | 10.4 | 400 | 6.3 | |
| 40–44 | 111 | 8.7 | 137 | 8.5 | 100 | 15.7 | 85 | 11.1 | 1,029 | 13.8 | 484 | 8.8 | |
| 45–49 | 126 | 7.9 | 152 | 7.6 | 113 | 9.6 | 82 | 10.6 | 1,056 | 9.6 | 752 | 10.7 | |
| 50–54 | 187 | 15.1 | 177 | 10.4 | 139 | 12.3 | 95 | 9.4 | 1,368 | 14.4 | 1,025 | 15.7 | |
| 55–59 | 203 | 12.0 | 191 | 7.4 | 126 | 5.7 | 127 | 8.9 | 1,531 | 13.9 | 1,131 | 14.7 | |
| 60–64 | 140 | 8.1 | 138 | 6.2 | 91 | 3.7 | 118 | 11.4 | 1,253 | 8.0 | 966 | 9.4 | |
| 65 or older | 158 | 6.8 | 123 | 3.3 | 57 | 2.5 | 86 | 4.8 | 753 | 4.2 | 1,000 | 7.8 | |
| Marital status | Married | 503 | 35.9 | 608 | 37.5 | 521 | 47.1 | 414 | 43.0 | 6,386 | 65.1 | 4,115 | 55.8 |
| Non-marriedb | 767 | 64.1 | 1044 | 62.5 | 625 | 52.9 | 411 | 57.0 | 3,451 | 39.4 | 2565 | 44.2 | |
| Education, highest level completed | High school graduate or less | 617 | 54.9 | 849 | 55.0 | 400 | 33.1 | 79 | 1.3 | 339 | 4.49 | 2,085 | 30.9 |
| Some college or technical school | 470 | 37.3 | 628 | 36.4 | 512 | 51.1 | 616 | 75.7 | 2,956 | 32.4 | 2,841 | 43.6 | |
| College graduate or more | 189 | 7.8 | 175 | 8.7 | 239 | 15.8 | 134 | 11.9 | 6,603 | 63.1 | 1,778 | 25.5 | |
| <$10,000 | 68 | 6.7 | 34 | 2.8 | 17 | 0.7 | <5 | NRc | 19 | 1.2 | 53 | 1.4 | |
| $10–<15,000 | 122 | 11.4 | 83 | 4.8 | 35 | 3.9 | <5 | NRc | 20 | 0.2 | 92 | 1.8 | |
| Household income from all sources | $15–<20,000 | 220 | 25.1 | 203 | 13.0 | 86 | 8.0 | 20 | 1.6 | 76 | 1.3 | 208 | 3.3 |
| $20–<25,000 | 207 | 16.7 | 336 | 23.5 | 168 | 24.6 | 42 | 5.2 | 140 | 1.3 | 350 | 5.4 | |
| $25–<35,000 | 195 | 16.1 | 347 | 19.1 | 232 | 19.0 | 96 | 17.3 | 324 | 2.9 | 700 | 10.5 | |
| $35–<50,000 | 142 | 9.6 | 207 | 15.8 | 189 | 12.7 | 232 | 29.3 | 913 | 9.6 | 1,153 | 17.8 | |
| $50–<75,000 | 95 | 6.4 | 144 | 10.8 | 135 | 16.1 | 190 | 21.4 | 2,056 | 18.0 | 1,377 | 19.1 | |
| ≥ $75,000 | 89 | 8.0 | 95 | 10.1 | 181 | 15.1 | 160 | 23.6 | 5,565 | 65.3 | 2,005 | 40.7 | |
| Housing status | Owns home | 665 | 40.7 | 827 | 51.4 | 644 | 53.7 | 596 | 65.20 | 8,326 | 85.63 | 5,344 | 76.53 |
| Rents or other arrangement | 609 | 59.3 | 809 | 48.6 | 499 | 46.3 | 226 | 34.80 | 1,506 | 14.37 | 1,309 | 23.47 | |
LVN = licensed vocational nurse, LPN = licensed practical nurse, RN = registered nurse, NR = not reported
State-by-state participation in BRFSS by year is charted in Online Appendix A. General BRFSS documentation can be found at https://www.cdc.gov/brfss/datadocumentation/index.htm
Divorced, widowed, separated, never married, unmarried couple
Not reported because number of respondents is <5.
Education differed by industry and occupation. More than 95% of RNs had completed at least some college or technical school, compared to 88% of LVNs/LPNs, 69% of clerical workers, 67% of hospital care aides, and 45% of both home health and nursing home aides. Almost 20% of home health aides had not completed high school (data not shown). Workers in the home health setting were also most likely to report being self-employed (16%); this compares to less than 5% of all other groups (data not shown).
Home care aides were most likely (43%) to report household incomes under $20,000 per year. This compares with 22% of nursing home aides, 13% of hospital aides, 6% of clerical workers, and less than 3% each of LVNs/LPNs and RNs. Using 2014 BRFSS data (results not shown), home health aides were also most likely to be below 100% of the simplified 2013 Federal Poverty Level (30%) or in the 100-<400% category (58%). Over 50% of nursing home aides, hospital aides, and LVNs/LPNs were in the 100-<400% category. In contrast, 73% of RNs had household incomes at or above 400% FPL. Home ownership levels were consistent with these findings, lowest among home health aides (41%); slightly over half of nursing home and hospital aides owned their home, and home ownership was substantially higher among LVNs/LPNs (69%) and RNs (86%).
Healthcare Access
Healthcare access was not evenly distributed among patient care aides employed in different settings (Table 2). For the four-year period (2013–2016), 21% of home health aides and 17% of nursing home aides lacked health insurance. These prevalences are much higher than those observed among LVNs/LPNS (8%), hospital aides (7%), and RNs (3%) and the comparison group of clerical workers (6%).
Table 2.
Prevalence estimates and adjusted prevalence ratios (aPRs) for healthcare access metrics: comparison of patient care aides, LVN/LPNs, and RNs to non-healthcare clerical workers, 2013–2016 Behavioral Risk Factor Surveillance System (BRFSS)b
| Patient Care Aides by Setting | Nurses | Comparison Group | ||||
|---|---|---|---|---|---|---|
| Healthcare access metric | Home Health Prevalencec (%) aPR (95% CI) |
Nursing Home Prevalence (%) aPR (95% CI) |
Hospital Prevalence (%) aPR (95% CI) |
LVN/LPN Prevalence (%) aPR (95% CI) |
RN Prevalence (%) aPR (95% CI) |
Non-healthcare Clerical Prevalence (%) Adjusted Prevalence (95% CI) |
|
| ||||||
| Lacks health care coverage (health insurance, prepaid plan, or government plan) | 20.7 2.53 (1.84–3.48) |
16.9 1.85 (1.33–2.56) |
6.8 0.80 (0.52–1.23) |
8.2 1.07 (0.62–1.87) |
3.3 0.59 (0.41–0.85) |
6.1 8.9 (7.0–11.2) |
| Does not have at least one personal doctor or health care provider | 19.3 1.40 (1.05–1.86) |
20.4 1.26 (0.94–1.68) |
15.3 0.93 (0.65–1.35) |
11.3 0.92 (0.57–1.48) |
9.0 0.83 (0.62–1.12) |
11.6 17.9 (14.3–22.2) |
| Did not visit doctor in past year for routine checkup | 26.2 1.01 (0.83–1.24) |
22.7 0.84 (0.69–1.04) |
20.7 0.68 (0.51–0.90) |
26.6 1.01 (0.76–1.35) |
20.6 0.80 (0.67–0.96) |
26.2 32.7 (28.4–37.3) |
| Needed to see doctor in last 12 months but could not because of cost | 29.3 2.33 (1.75–3.09) |
21.1 1.59 (1.20–2.09) |
16.2 1.28 (0.89–1.84) |
19.3 1.60 (1.04–2.47) |
7.2 0.70 (0.54–0.89) |
10.5 10.7 (9.0–12.7) |
| Did not visit dentist in past yeard | 40.6 1.73 (1.23–2.43) |
40.1 1.52 (1.13–2.05) |
23.4 0.95 (0.63–1.42) |
36.8 1.57 (1.07–2.32) |
17.6 0.91 (0.68–1.24) |
19.7 24.1 (18.8–30.3) |
| Never had blood cholesterol checkede | 22.8 1.32 (0.93–1.88) |
29.5 1.48 (1.10–1.99) |
18.6 0.88 (0.59–1.31) |
12.8f 0.91 (0.46–1.79) |
6.5 0.54 (0.38–0.76) |
13.5 18.7 (14.9–23.1) |
| Did not have flu vaccine last 12 months | 59.8 0.84 (0.75–0.95) |
45.6 0.62 (0.55–0.70) |
34.3 0.46 (0.38–0.56) |
41.8 0.61 (0.50–0.75) |
30.2 0.49 (0.43–0.56) |
67.0 72.3 (69.5–75.0) |
PR = prevalence ratio, CI = confidence interval, LVN = licensed vocational nurse, LPN = licensed practical nurse, RN = registered nurse
Adjusted for: age (18–29, 30–34, 35–39,40–44, 45–49, 50–54, 55–59, 60–64, >=65); sex; race/ethnicity combined (classified as white non-Hispanic, black non-Hispanic, other non-Hispanic, Hispanic) and marital status (married vs. all other)
State-by-state participation in BRFSS by year is charted in Online Appendix A. General BRFSS documentation can be found at https://www.cdc.gov/brfss/datadocumentation/index.htm
Weighted, unadjusted prevalence
In 2014 and 2016 surveys only.
In 2013 and 2015 surveys only.
Estimate has a relative standard error >30%–<=50% and should be interpreted with caution.
Between 20–27% of each patient care aide group, nurses, and clerical workers had not seen a health practitioner for a checkup during the past year, with no apparent pattern by health insurance status. Home health and nursing home aides, as well as LVNs/LPNs, were significantly less likely than clerical workers to have had a dental visit in the previous 12 months. Nursing home (29%) and home health (23%) aides were more likely than clerical workers (14%) to have never had their blood cholesterol checked; the adjusted prevalence ratio compared to clerical workers was statistically significant only for nursing home aides.
Two-thirds of clerical workers had not received an influenza vaccine in the previous 12 months; compared to this group, each group of health care workers was more likely to have been vaccinated during this time period. However, nearly 60% of home health aides had not received an influenza vaccine in the past 12 months; the prevalences were 46% for nursing home aides, and 42% for LVNs/LPNs. Influenza vaccination coverage was better for hospital aides, but 34% lacked an influenza vaccine, as did 30% of RNs.
Health Behaviors
Current smoking prevalence was highest among home health and nursing home aides, at nearly one in four workers in these groups. aPRs for current smoking were significantly elevated for these subgroups and for LVNs/LPNS, compared to clerical workers (Table 3). The prevalence of current and former smoking combined was highest for home health aides, at 46%. Binge drinking prevalence was lower among home health and nursing home aides than among clerical workers, with the deficit statistically significant for nursing homes aides. The aPR comparing LVNs/LPNs to clerical workers had a statistically nonsignificant elevation, with nearly one in five LVNs/LPNs reporting binge drinking.
Table 3.
Prevalence estimates and adjusteda prevalence ratios (aPRs) for health behaviors: comparison of patient care aides, LVNs/LPNs, and RNs to non-healthcare clerical workers, 2013–2016 Behavioral Risk Factor Surveillance Systemb
| Patient Care Aides by Setting | Nurses | Comparison Group | ||||
|---|---|---|---|---|---|---|
| Health Behavior, status, or outcome | Home Health Prevalencec (%) aPR (95% CI) | Nursing Home Prevalence (%) aPR (95% CI) |
Hospital Prevalence (%) aPR (95% CI) |
LVN/LPN Prevalence (%) yaPR (95% CI) | RN Prevalence (%) aPR (95% CI) |
Non-healthcare Clerical Prevalence (%) Adjusted Prevalence (95% CI) |
|
| ||||||
| Smoker – current | 24.3 1.95 (1.54–2.46) |
23.2 1.80 (1.43–2.26) |
15.6 1.14 (0.86–1.50) |
18.9 1.48 (1.02–2.16) |
9.2 0.83 (0.68–1.02) |
11.4 13.3 (11.3–15.5) |
| Smoker – former | 21.3 1.16 (0.90–1.48) |
15.4 0.92 (0.68–1.24) |
18.2 1.06 (0.83–1.37) |
17.3 0.89 (0.69–1.15) |
19.0 0.88 (0.76–1.03) |
22.6 23.7 (21.2–26.4) |
| Binge drinking (during the past 30 days had 5 or more drinks for men or 4 or more drinks for women on an occasion) | 11.7 0.84 (0.58–1.21) |
10.7 0.67 (0.51–0.87) |
15.4 0.80 (0.56–1.14) |
21.3 1.34 (0.86–2.07) |
14.5 0.98 (0.79–1.20) |
15.1 20.4 (17.3–23.9) |
| Did not participate in any physical activities or exercise during past month | 30.8 1.30 (1.04–1.64) |
27.4 1.25 (1.02–1.54) |
25.3 1.19 (0.92–1.54) |
20.8 0.97 (0.68–1.40) |
17.3 0.93 (0.73–1.18) |
20.9 20.9 (18.4–23.7) |
| Obese (body mass index >= 30)d | 42.1 1.30 (1.09–1.56) |
37.7 1.24 (1.04–1.46) |
35.0 1.12 (0.89–1.42) |
45.6 1.47 (1.18–1.83) |
26.0 0.89 (0.73–1.07) |
29.2 30.8 (27.7–34.1) |
| Short sleep (less than 7 hours per 24 hour period)e | 44.9 1.30 (1.05–1.61) |
48.4 1.39 (1.15–1.69) |
50.9 1.49 (1.19–1.87) |
46.1 1.38 (1.08–1.77) |
44.5 1.43 (1.22–1.67) |
30.1 31.7 (27.7–36.0) |
PR = prevalence ratio, CI = confidence interval, LVN = licensed vocational nurse, LPN = licensed practical nurse, RN = registered nurse
Adjusted for: age (18–29, 30–34, 35–39,40–44, 45–49, 50–54, 55–59, 60–64, >=65); sex; race/ethnicity combined (classified as white non-Hispanic, black non-Hispanic, other non-Hispanic, Hispanic) and marital status (collapsed to married vs. all other)
State-by-state participation in BRFSS by year is charted in Online Appendix A. General BRFSS documentation can be found at https://www.cdc.gov/brfss/datadocumentation/index.htm
Weighted, unadjusted prevalence
Computed from self-reported height and weight.
In 2013, 2014, and 2016 surveys only
At least 25% of each patient care aide group reported that they had not participated in any physical activities or exercise in the past month; the same was true of 21% of clerical workers. Among the home health aides and LVNs/LPNs, the prevalence of obesity was greater than 40%, and more than one in three patient care aides working in nursing homes and hospitals were obese. Every healthcare group had a significantly increased prevalence for short sleep (<7 hours per 24-hour period) compared to clerical workers; the prevalence of short sleep was above 40% for every group and was highest for patient care aides in hospitals.
Health Outcomes
Home health and nursing home aides had worse self-reported health (rating general health as fair or poor) than other healthcare workers and clerical workers (Table 4). These aides also were most likely to report that their physical health and mental health was not good for at least 14 of the previous 30 days; the aPRs compared to clerical workers were statistically significant for overall health and physical health.
Table 4.
Prevalence estimates and adjusteda prevalence ratios (aPRs) of health status and outcomes: comparison of patient care aides, LVNs/LPNs, and RNs to non-healthcare clerical workers, 2013–2016 Behavioral Risk Factor Surveillance System (BRFSS)b
| Patient Care Aides by Setting | Nurses | Comparison Group | ||||
|---|---|---|---|---|---|---|
| Health status or outcome | Home Health Prevalencec (%) aPR (95% CI) |
Nursing Home Prevalence (%) aPR (95% CI) |
Hospital Prevalence (%) aPR (95% CI) |
LVN/LPN Prevalence (%) aPR(95% CI) |
RN Prevalence (%) aPR (95% CI) |
Non-healthcare Clerical Prevalence (%) Adjusted Prevalence (95% CI) |
|
| ||||||
| Rates general health as fair or poor | 18.2 2.10 (1.58–2.80) |
16.3 2.18 (1.61–2.97) |
10.4 1.41 (0.96–2.06) |
7.5 1.02 (0.61–1.73) |
6.8 1.16 (0.65–2.06) |
6.9 7.2 (6.0–8.7) |
| Physical health was not good at least 14 of the last 30 days | 12.5 1.97 (1.32–2.95) |
9.2 1.62 (1.12–2.34) |
6.4 1.14 (0.70–1.87) |
5.9 0.98 (0.59–1.63) |
4.0 0.69 (0.49–0.98) |
6.2 5.6 (4.5–7.0) |
| Mental health was not good at least 14 of the last 30 days | 14.6 1.46 (0.94–2.27) |
13.8 1.35 (0.92–1.98) |
9.7 1.05 (0.71–1.54) |
10.3 1.05 (0.57–1.92) |
7.1 0.81 (0.62–1.05) |
9.1 8.1 (6.5–10.0) |
| Has a health professional ever told you that you had (% of affirmative responses): | ||||||
| Depression? | 22.4 1.48 (1.16–1.88) |
19.5 1.19 (0.93–1.54) |
15.7 1.10 (0.82–1.46) |
23.8 1.46 (1.08–1.96) |
15.0 0.94 (0.80–1.10) |
17.0 12.9 (11.4–14.6) |
| High blood pressure (excluding during pregnancy only)?d | 36.1 1.42 (1.15–1.76) |
23.2 1.02 (0.72–1.42) |
17.0 0.82 (0.61–1.12) |
21.1 0.87 (0.58–1.30) |
23.1 0.94 (0.80–1.10) |
25.9 25.8 (22.8–29.2) |
| High cholesterol? d | 39.9 1.28 (1.05–1.56) |
30.9 1.03 (0.72–1.47) |
25.0 0.88 (0.66–1.17) |
26.0 0.93 (0.69–1.27) |
31.5 1.05 (0.91–1.22) |
32.0 32.9 (29.5–36.5) |
| Diabetes (excludes gestational diabetes, and prediabetes/borderline diabetes)? | 7.6 1.11 (0.79–1.56) |
7.4 1.50 (1.00–2.24) |
8.7 1.66 (1.03–2.69) |
6.4 1.15 (0.78–1.70) |
7.1 1.13 (0.62–2.07) |
6.0 6.2 (5.1–7.4) |
| Arthritis? e | 25.9 1.37 (1.11–1.70) |
20.7 1.37 (1.08–1.74) |
18.8 1.37 (1.07–1.76) |
23.2 1.24 (0.91–1.68) |
16.0 0.82 (0.70–0.97) |
21.8 16.5 (14.7–18.4) |
| Cancer (other than skin cancer)? | 5.4 1.24 (0.79–1.94) |
6.3f 1.72 (0.82–3.59) |
2.8 0.99 (0.59–1.65) |
3.8 0.79 (0.44–1.42) |
4.1 0.83 (0.61–1.14) |
6.0 3.7 (3.0–4.5) |
| Chronic obstructive pulmonary disease (including emphysema or chronic bronchitis)? | 5.9 1.47 (0.91–2.36) |
4.0 1.06 (0.68–1.63) |
3.2 0.82 (0.46–1.48) |
3.9 0.97 (0.53–1.78) |
2.2 0.64 (0.44–0.92) |
3.9 3.1 (2.4–4.1) |
| Asthma? | 21.6 1.54 (1.08–2.21) |
14.4 1.03 (0.77–1.37) |
15.3 1.12 (0.80–1.58) |
16.6 1.23 (0.73–2.08) |
12.5 1.00 (0.80–1.24) |
12.8 11.3 (9.6–13.4) |
| Do you still have asthma? | 16.9 1.79 (1.13–2.84) |
9.1 1.02 (0.73–1.41) |
9.7 1.11 (0.74–1.65) |
12.9f 1.47 (0.76–2.84) |
8.2 1.00 (0.79–1.27) |
8.5 6.5 (5.4–7.9) |
PR = prevalence ratio, CI = confidence interval, LVN = licensed vocational nurse, LPN = licensed practical nurse, RN = registered nurse
Adjusted for: age (18–29, 30–34, 35–39,40–44, 45–49, 50–54, 55–59, 60–64, >=65); sex; race/ethnicity combined (classified as white non-Hispanic, black non-Hispanic, other non-Hispanic, Hispanic) and marital status (collapsed to married vs. all other).
State-by-state participation in BRFSS by year is charted in Online Appendix A. General BRFSS documentation can be found at https://www.cdc.gov/brfss/datadocumentation/index.htm
Weighted, unadjusted prevalence
In 2013 and 2015 surveys only
(Ever told) you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia? (Arthritis diagnoses include: rheumatism, polymyalgia rheumatica; osteoarthritis (not osteoporosis); tendonitis, bursitis, bunion, tennis elbow; carpal tunnel syndrome, tarsal tunnel syndrome; joint infection, etc.)
Estimate has a relative standard error >30%-<=50% and should be interpreted with caution.
Home health aides had the highest prevalences for multiple adverse health outcomes: high blood pressure, high cholesterol, arthritis, asthma (current or ever), and COPD. More than one in three home health aides had been diagnosed with high blood pressure; the same was true for high cholesterol. One in four of these workers reported a diagnosis of arthritis. Cancer (other than skin cancer), COPD, and diabetes were the only provider-diagnosed health outcomes for which aPRs were not significantly elevated in home health aides compared to clerical workers.
Depression was significantly elevated among home health aides and LVNs/LPNs compared to clerical workers, affecting more than 20% of workers in the home health and LVN/LPN groups. Diagnosis with arthritis and related conditions was statistically higher among all patient care aide groups and LVNs/LPNs than in clerical workers; for all patient care aide groups, the elevations were statistically significant. Nursing home aides were most likely to report having been diagnosed with some form of cancer (excluding skin cancer), though the elevation was not statistically significant compared to clerical workers. The prevalence of diabetes was highest among hospital aides, with an elevation of borderline statistical significance compared to clerical workers; aside from arthritis, no other health outcome had a significantly elevated aPR.
Alternate Analyses
a. Patient care aides combined with personal care aides
Within all three patient care aide groups, but particularly in the home health setting, personal care aides may fill the same positions as patient care aides. An alternate analysis including personal care aides had little effect on point estimates for the health-related metrics presented here, although the addition of so many respondents (997 personal care aides added to 1279 patient care aides) to the home health group led to an increased number of statistically significant aPRs (data not shown).
b. Healthcare coverage, health-related behaviors, and health outcomes adjusted for household income
An alternate analysis included household income in the regression models. Income was missing for different percentages of the healthcare subgroups: home health aides (11.0%); nursing home aides (12.5%); hospital aides (9.5%); LVNs/LPNs (9.1%); RNs (8.1%); and the clerical comparison group (11.5%).
Including income in the aPR models affected multiple metrics. Many adverse health metrics observed in the main models were attenuated among patient care aides, and a number of these lost statistical significance (results in online Appendix B Tables 2–4). All health professions continued to have significantly elevated aPRs for short sleep compared to clerical workers.
For home health aides, no health coverage, inability to see a doctor because of cost, current and former smoking status, poor general health, high blood pressure, arthritis, and ever and current asthma remained significantly elevated compared to the clerical worker group after adjustment for income. However, the aPRs had lower elevations that were no longer significant for several other outcomes: no personal physician, no dental visit in past 12 months, no exercise, obesity, poor physical health, and depression.
Nursing home aides still had significantly elevated aPRs for current smoking and poor general and physical health, but the aPRs for a number of metrics were attenuated and no longer statistically significant: lacking healthcare coverage, not seeing doctor due to cost, not visiting the dentist, never having blood cholesterol checked, no exercise, obesity, arthritis, and diabetes (the last had borderline statistical significance in the models without income).
Hospital aides, who had few significant elevations before adjustment for income, had small increases or decreases in aPRs for most metrics; however, the elevations for arthritis and diabetes were not statistically significant. LVNs/LPNs still had elevated aPRs for being unable to see a doctor due to cost and for not having a dental visit in the past year. For LVNs/LPNs, modest increases in the aPRs were observed for most health outcomes, but statistical significance did not change for any item in any domain. In contrast, among RNs, previously observed deficits for a number of metrics were attenuated and no longer statistically significant: no health plan; no checkup in the past year; unable to see doctor due to cost; poor physical health; and COPD.
DISCUSSION
The patient care aide segment of the healthcare support workforce had a constellation of adverse health-related metrics in these analyses of the 2013–2016 BRFSS data: suboptimal prevalences of healthcare access, preventive care, and positive health behaviors, as well as elevated prevalences of multiple adverse health conditions. Among patient care aides, multiple health-related metrics differed markedly by work setting.
Home health aides had the most strongly adverse results for multiple health-related metrics, including less access to healthcare, low prevalences of physical exercise, and high prevalences of poor self-rated health, smoking, high blood pressure, high cholesterol, asthma, COPD, and arthritis and related conditions. Nursing home aides had better healthcare access than those working in home health and reported somewhat better health outcomes. Of the three patient care aide groups, hospital aides had the most positive results for almost all health metrics, although prevalences for many metrics highlight the need for improvement in this group as well.
The study has some positive results. Binge drinking prevalence was lower for nursing home and home health aides than for clerical workers, and the difference was statistically significant for nursing home aides. Of the patient care aide groups, hospital aides were most likely to have health insurance coverage (although healthcare cost remained an access barrier for some of these workers) and prevalences of several health conditions (high blood pressure, high cholesterol, cancer) were lower for hospital aides than for clerical workers (though the deficits were not statistically significant). Hospital aides had the highest prevalence of short sleep of all the healthcare workers, but only had a significantly elevated prevalence compared to clerical workers for arthritis and related conditions and for diabetes.
Findings on income and healthcare access for nursing home and home health aides in this study generally align with results from earlier surveys of these groups. The National Nursing Assistant Survey was a supplement of the 2004 National Nursing Homes Study that focused on Certified Nurse Assistants working in nursing homes.11 The study reported that nearly one-third of respondents were receiving at least one public benefit (food assistance, housing assistance, Medicare or Medicaid), that 26% of respondents did not have paid sick leave, and that while nearly 90% had health insurance available from an employer, 16% were not participating in employer-sponsored insurance; 42% of non-participants cited being unable to afford the insurance premium as the reason for not participating. An analysis of data from the National Home Health Aide Study found that 19% of this group had household incomes below 100% of the FPL, while an additional 35% had incomes between 100 and 199% of FPL.21 Beginning in 2015, home health workers were covered by the Fair Labor Standard Act’s minimum wage and overtime protections. However, the federal minimum wage, at $7.25 per hour (or annual income of $15,080 for 2,080 hours worked), equated to just under 130% of the FPL for 2014 ($11,670) for a single worker with no children and was slightly below the poverty level ($15,730) for a single worker with a child.22 In the current analysis, 16% of the home health workforce reported being self-employed; this group was probably less likely to have access to employer-sponsored insurance available, although some could have access to employer coverage through family members.
Certification as an LVN/LPN has been described as a career progression path for Certified Nurse Aides.23 In 2017, the median wage was $21.65/hour for LPNs/LVNs, who have additional licensing requirements but also participate in direct patient care.6 In the current analyses, LVNs/LPNs fared better on some health outcomes than patient care aides. However, this group still had the highest prevalences of binge drinking, depression, and obesity of all groups examined and, despite relatively high levels of healthcare access, were least likely to have visited a dentist in the past year. The LVN/LPN workforce was not divided by work setting in this study due to small numbers, but 36% of LVNs/LPNs in the study were from hospitals, 8% in nursing homes, and 34% worked in home health, with the remainder in outpatient or other settings, so results for this group reflect a range of working conditions. Nurse aides have cited cost and competing demands as barriers to pursuing certification as LVNs/LPNs.24 The adverse health outcomes seen among LVNs/LPNs in the current study suggest that despite somewhat higher socioeconomic status, this workforce is also in need of interventions to address these adverse health metrics. Further study of a larger group of LVNs/LPNs separated by work setting is warranted to better understand the needs of this workforce.
The second year of the study period (2014) coincided with the start of healthcare coverage under the Affordable Care Act. The expansion of Medicaid (which in many cases expanded eligibility to workers with household incomes up to 138% of the FPL) in select states may have impacted patient care aides, many of whom have incomes too high for Medicaid (particularly without expansions) but too low to purchase employer-sponsored insurance while still meeting other critical financial needs. As states participating in BRFSS changed over this period and adoption of the Medicaid expansion varied by state, the impact of changes in the healthcare coverage system on health metrics among this low-wage workforce could not be evaluated in these analyses. Some research has shown improved healthcare access and some health metrics following implementation of the ACA, particularly in states that expanded Medicaid.8,9,25–27 However, the results of other studies highlight residual inequities in access to care due to structural issues ranging from reluctance of some providers to accept Medicaid patients and inability to afford coinsurance, particularly among the working poor, to lack of transportation, childcare, and employer-provided time off for preventive care visits.28–30 The results of alternate analyses adjusting for income in the current study suggest that increased wages among the patient care workforce could ameliorate the high prevalence of some adverse health metrics observed among these groups, but that other types of intervention would be needed to address residual differences in outcomes, particularly those stemming from work activities, rather than work arrangements, such as arthritis. However, given the actual pay level of this workforce, efforts to both increase compensation and address the full range of adversities across health metrics identified in the primary analyses are needed.
One health metric, influenza vaccination, can be used to illustrate both how prevalence rates for patient care aides vary by setting and why a workplace-specific approach is needed to improve outcomes. All groups of patient care aides, as well as LVNs/LPNs and RNs, had influenza vaccination rates well below the Healthy People 2020 goal of 90% yearly influenza vaccination for healthcare workers.31 While all healthcare worker groups were significantly more likely to report being vaccinated than non-healthcare clerical workers, this result primarily reflects the very low vaccination rates (under one-third) in the latter group. Recent data from an internet panel survey of healthcare personnel32 found that vaccination coverage was lower among assistants and aides (69.1%) than among other healthcare groups, with weighted vaccination prevalence for assistants and aides varying by setting: 91.1% in hospitals, 74.4% in outpatient settings, 66.9% in long-term care (home health was not included). In the current study, home health aides had the lowest and hospital aides the highest vaccination rates among patient care aides, respectively. Increasing vaccination rates would offer greater protection to both direct-care workers and their clients, who are often high risk both from influenza and its sequelae, such as pneumonia (and, if recent research is confirmed, myocardial infarction33).
Considering potential interventions to improve influenza vaccination prevalence highlights setting-specific issues within the patient care aide workforce. In the internet panel survey, 72.5% of healthcare respondents said they were vaccinated at work; 11.5% in a pharmacy, drugstore, or other store; and 10.9% in a physician’s office.32 The authors found that vaccination requirements were associated with a high coverage rate, and that personnel with the option of workplace vaccination were more likely to be covered than those without this option, even when vaccination was not required. The authors discuss the benefits of offering workplace vaccinations not only in hospitals (where they are often already in place), but also in nursing homes, given the potential benefit to the patient population. The efficacy of vaccine requirements in hospitals has been confirmed by other research.31 The relatively high levels of coverage among hospital personnel may reflect adoption by hospitals of recommendations to mandate or strongly encourage vaccination among their workers, as well as the relative ease of offering on-site vaccination in this setting. Findings of low vaccination rates in nursing home aides in the current study suggest the need for wider adoption of workplace vaccination in this setting.
The best mechanism for increasing vaccination is unclear for home health care workers, a workforce with higher levels of self-employment (often involving multiple clients) and with employed workers not necessarily visiting the employing agency on a regular basis. Previous researcher that modelled costs of employee-sponsored influenza vaccination, whether at the worksite or through paid-time-off to obtain vaccination off-site, found the costs to be limited (even with provision of financial reward for compliance).34 That research did not account for the additional benefits of reduced transmission to patients. Home health agencies might be less likely to realize immediate financial benefits of workplace vaccination than employers who grant paid sick leave, have more static workforce requirements, and who are subject to closer tracking of, and perhaps financial penalties for, adverse patient outcomes. The discrepancies in influenza vaccination rates in the patient care aide workforce by setting likely also reflect other differences observed in this study (poor access to healthcare, including lack of insurance, cost as a barrier to physician visits, lack of a primary practitioner, and lack of regular checkups).
Similar differences by work setting apply to potential interventions to address adverse outcomes such as joint pain (and related problems) included in the arthritis outcome: the availability of assistive devices and workplace design efforts might be most difficult to address in the home health setting, where workplaces change frequently and employer resources, as well as penalties for noncompliance, are likely more limited. In 2010, NIOSH released a series of “Fast Facts” tip sheets for home health workers, one of which provides information on preventing MSDs, but acknowledges that the home setting is not likely to have assistive devices for patient lifting.15 Medicare Part B may cover patient lifts if prescribed by a doctor,35 but training in the safe use of these devices is required15,36 and may be more difficult to address in the home health context, where workers often move among multiple homes. In a recent study of home health aides, nearly 40% reported having no access to equipment to assist with moving clients.14 New research in this area has focused on evaluating, for example, portable, relatively affordable solutions for patient transfer. 37 However, more research in this area, including mechanisms for disseminating information to the highly-dispersed home health workforce, is needed.
BRFSS has both strengths and limitations. Strengths of the study include the use of standardized weighting methodology across states and years, as well as the large sample size. This large participant pool facilitates assessment of health metrics of specific workforces, such as these analyses of the patient care aide workforce. However, the industry and occupation module is optionally administered by the states, with different states participating each year, and the survey excludes active military employees, so the findings are not nationally representative. Moreover, the current analyses did not address state, regional, or yearly variations. Industry and occupation, health behaviors, and health outcomes are all self-reported and potentially misclassified. Some respondents did not answer all questions. The demographic question most commonly left blank concerned income, which was missing for 8.1–12.5% of each healthcare group. In addition, results for less common health outcomes such as cardiovascular disease, skin cancer, and kidney disease could not be reported because the prevalence estimates were too unstable, and the issue of comorbidities was not addressed.
BRFSS does not ask about the work-relatedness of health outcomes. Within healthcare, multiple characteristics not measured in BRFSS, such worksite exposures, can lead to between-group differences in prevalence of specific health outcomes. For example, in the current analyses, home health care was the only group with statistically significant elevated prevalences of asthma diagnoses (both ever and current). These workers likely experience more uncontrolled exposures both in the workplace (clients’ homes) and in their own homes (nearly 60% of the group were renters). In a study of home health workers, 33% reported exposure to cockroach allergens, 21.3% to animal hair, 19.3% to excessive dust, 16.5% to irritating chemicals (e.g. bleach, cleaning agents) and 10.0% to mold or dampness.12 In a recent study of home health workers, 30% reported exposure to bleach and 10% to second-hand smoke in the workplace.14 Although these on-the-job exposures to asthmagens are self-reported, they highlight the prevalence of a range of exposures in this work setting.
In addition, the broad definitions for some health outcomes included in the BRFSS survey, particularly arthritis, hinder interpretation of some findings. However, the results for arthritis in this study, are consistent with those of other studies noting high levels of musculoskeletal disorders and injuries (which could be reported as arthritis in BRFSS) in healthcare in general and higher levels among healthcare support workers,38 with studies in various settings finding that patient care aides had the highest risk for MSDs.33,39
As the design of BRFSS is cross-sectional, the causal direction of observed associations cannot be assessed. Whether, for example, home health aides have the highest prevalence of smoking because more smokers enter the occupation or whether something about the work setting leads workers to begin smoking or hinders smoking cessation cannot be discerned from these data. However, some differences, such as the high prevalence of being uninsured in this group, probably reflect work structure, as home health aides have the highest prevalence of self-employment and the lowest compensation rates among patient care aides. Both work structure and work activities likely contribute to the adverse health metrics observed across the patient care workforce in these analyses.
CONCLUSION
This analysis assessed how a variety of health metrics differ by work setting within the patient care aide workforce. This approach facilitates understanding of the distribution of health-related problems and provides a clearer picture of what resources are most needed by workers in different settings. The observation of high prevalences of current smoking, obesity, and several adverse health outcomes in all subgroups of patient care workers suggest the need to focus resources across this workforce. However, the need for intervention is strongest for home health aides, many of whom have limited economic resources and who have the highest prevalences of numerous adverse health metrics. The more positive findings for hospital aides, as well as findings from other research, suggest the merits of addressing some of these problems, such as low influenza vaccination rates, at the worksite, particularly for nursing home aides. Unfortunately, problems in the home health workforce are more difficult to approach in this way, due to dispersed worksites, high annual turnover rates of 60–75%,40 and somewhat higher rates of self-employment. Further research focusing on patient care aides, and particularly home health aides, is needed to determine how best to address the needs of this particularly vulnerable segment of the healthcare workforce.
Supplementary Material
Acknowledgements:
We wish to thank Marie Haring Sweeney, Chief of Surveillance Branch, Division of Field Studies and Engineering, National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, for her helpful review of the manuscript and to acknowledge the following branch staff for their work related to coding of industry and occupation: Pam Schumacher, Susan Burton, Matthew Hirst, Jenny Huddleston, Jeff Purdin, and Surprese Watts. We are also grateful for the efforts of the BRFSS state coordinators from the 30 states providing occupational data.
Funding:
The authors report that there was no funding source for the work that resulted in the article or the preparation of the article.
Footnotes
Disclosure (Authors): The authors declare no conflicts of interest.
Disclaimer: The findings and conclusions presented in this article are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health/Centers for Disease Control and Prevention.
Institution at which the work was performed: NIOSH
Institution and Ethics approval and informed consent:
The BRFSS survey data are collected, with informed consent, by CDC under OMB approval 0920–1061, expiration date 03/31/2021. The analytic work herein was performed at NIOSH and was determined by the NIOSH IRB to be exempt research involving human subjects (NIOSH protocol 2988).
References
- 1.Shockey TM, Wheaton AG. Short Sleep Duration by Occupation Group - 29 States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2017;66(8):207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mazurek JM, Syamlal G. Prevalence of Asthma, Asthma Attacks, and Emergency Department Visits for Asthma Among Working Adults - National Health Interview Survey, 2011–2016. MMWR Morb Mortal Wkly Rep. 2018;67(13):377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dodd KE, Mazurek JM. Asthma Among Employed Adults, by Industry and Occupation - 21 States, 2013. MMWR Morb Mortal Wkly Rep. 2016;65(47):1325–1331. [DOI] [PubMed] [Google Scholar]
- 4.Birdsey J, Sussell AL. Prevalence of Obesity, No Leisure-Time Physical Activity, and Short Sleep Duration Among Occupational Groups in 29 States. J Occup Environ Med. 2017;59(12):1221–1228. [DOI] [PubMed] [Google Scholar]
- 5.Loeppke R, Boldrighini J, Bowe J, et al. Interaction of Health Care Worker Health and Safety and Patient Health and Safety in the US Health Care System: Recommendations From the 2016 Summit. J Occup Environ Med. 2017;59(8):803–813. [DOI] [PubMed] [Google Scholar]
- 6.BLS. May 2017 National Occupational Employment and Wage Estimates United States. In: Bureau of Labor Statistics; 2017. [Google Scholar]
- 7.Martiniano R, Chorost S, Moore J. Health care employment projections 2014–2024: an analysis of Bureau of Labor Statistics Projections by Setting and by Occupations. . Rensselaer, NY: Center for Health Workforce Studies, School of Public Health, SUNY Albany;2016. [Google Scholar]
- 8.Okoro CA, Zhao G, Fox JB, Eke PI, Greenlund KJ, Town M. Surveillance for Health Care Access and Health Services Use, Adults Aged 18–64 Years - Behavioral Risk Factor Surveillance System, United States, 2014. MMWR Surveill Summ. 2017;66(7):1–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in Self-reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act. JAMA. 2015;314(4):366–374. [DOI] [PubMed] [Google Scholar]
- 10.Bercovitz A, Moss A, Sengupta M, Park-Lee EY, Jones A, Harris-Kojetin LD. An overview of home health aides: United States, 2007. Natl Health Stat Report. 2011(34):1–31. [PubMed] [Google Scholar]
- 11.Squillace MR, Remsburg RE, Harris-Kojetin LD, Bercovitz A, Rosenoff E, Han B. The National Nursing Assistant Survey: improving the evidence base for policy initiatives to strengthen the certified nursing assistant workforce. Gerontologist. 2009;49(2):185–197. [DOI] [PubMed] [Google Scholar]
- 12.Gershon RRM, Pogorzelska M, Qureshi KA, et al. Home Health Care Patients and Safety Hazards in the Home: Preliminary Findings. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 1: Assessment). Rockville (MD)2008. [Google Scholar]
- 13.Hittle B, Agbonifo N, Suarez R, Davis KG, Ballard T. Complexity of occupational exposures for home health-care workers: nurses vs. home health aides. J Nurs Manag. 2016;24(8):1071–1079. [DOI] [PubMed] [Google Scholar]
- 14.Quinn MM, Markkanen PK, Galligan CJ, et al. Occupational health of home care aides: results of the safe home care survey. Occup Environ Med. 2016;73(4):237–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NIOSH. NIOSH hazard review: occupational hazards in home healthcare. Home Healthc Nurse. 2010;28(4):211. [DOI] [PubMed] [Google Scholar]
- 16.CDC . About BRFSS. https://www.cdc.gov/brfss/about/index.htm. Accessed 01/22/2019.
- 17.CDC . Behavioral Risk Factor Surveillance Sytem. Annual Survey Data. https://www.cdc.gov/brfss/annual_data/annual_data.htm. Accessed 02/22/2019. [Google Scholar]
- 18.Washington State Department of Health. Data Source: Washington State Department of Health, Center for Health Statistics, Behavioral Risk Factor Surveillance System, supported in part by Centers for Diseaes Control and Prevention, Cooperatiave Agreement, U58/SO000047–1 though 3 (2011–013). In.
- 19.Wyoming Department of Health. Data Source: Wyoming Department of Health, Public Health Division, Behavioral Risk Factor Surveillance System, supported in part by Centers for Disease Control and Prevention, Cooperative Agreement, U58/SO000015–1 though 3 (2011–013). In.
- 20.NIOSH. Industry and Occupation Coding: About the NIOSH Industry & Occupation Computerized Coding System (NIOCCS). https://www.cdc.gov/niosh/topics/coding/overview.html. Accessed 12/13/2018.
- 21.Stone R, Wilhelm J, Bishop CE, Bryant NS, Hermer L, Squillace MR. Predictors of Intent to Leave the Job Among Home Health Workers: Analysis of the National Home Health Aide Survey. Gerontologist. 2017;57(5):890–899. [DOI] [PubMed] [Google Scholar]
- 22.ASPE. 2014. Poverty Guidelines. https://aspe.hhs.gov/2014-poverty-guidelines. Accessed 04/15/2019.
- 23.Alaska Colleagues in Caring. Alaska Recertification Survey for Certified Nurses Aides (CNAs), 2002. Anochorage, Alaska: University of Alaska Anchorage;2003. [Google Scholar]
- 24.Colorado Health Institute. 2006 Colorado Certified Nurse Aide Workforce Survey Findings. Denver, Co: Colorado Health Institute;2009. [Google Scholar]
- 25.McKenna RM, Langellier BA, Alcala HE, Roby DH, Grande DT, Ortega AN. The Affordable Care Act Attenuates Financial Strain According to Poverty Level. Inquiry. 2018;55:46958018790164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA Intern Med. 2016;176(10):1501–1509. [DOI] [PubMed] [Google Scholar]
- 27.Farietta TP, Lu B, Tumin R. Ohio’s Medicaid Expansion and Unmet Health Needs Among Low-Income Women of Reproductive Age. Matern Child Health J. 2018;22(12):1771–1779. [DOI] [PubMed] [Google Scholar]
- 28.Kino S, Kawachi I. The impact of ACA Medicaid expansion on socioeconomic inequality in health care services utilization. PLoS One. 2018;13(12):e0209935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gaffney A, McCormick D. The Affordable Care Act: implications for health-care equity. Lancet. 2017;389(10077):1442–1452. [DOI] [PubMed] [Google Scholar]
- 30.Himmelstein KEW, Venkataramani AS. Economic Vulnerability Among US Female Health Care Workers: Potential Impact of a $15-per-Hour Minimum Wage. Am J Public Health. 2019;109(2):198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Vaccine Advisory Committee. Strategies to achieve the healthy people 2020 annual influenza vaccine coverage goal for health-care personnel: recommendations from the national vaccine advisory committee. Public Health Rep. 2013;128(1):7–25. [PMC free article] [PubMed] [Google Scholar]
- 32.Black CL, Yue X, Mps, et al. Influenza Vaccination Coverage Among Health Care Personnel - United States, 2016–17 Influenza Season. MMWR Morb Mortal Wkly Rep. 2017;66(38):1009–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kwong JC, Schwartz KL, Campitelli MA. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N Engl J Med. 2018;378(26):2540–2541. [DOI] [PubMed] [Google Scholar]
- 34.Lee BY, Bailey RR, Wiringa AE, et al. Economics of employer-sponsored workplace vaccination to prevent pandemic and seasonal influenza. Vaccine. 2010;28(37):5952–5959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Center for Medicare and Medicaid Services. Does Medicare cover patient lifts? https://www.medicare.gov/coverage/patient-lifts. Accessed 02/14/2019.
- 36.D’Arcy LP, Sasai Y, Stearns SC. Do assistive devices, training, and workload affect injury incidence? Prevention efforts by nursing homes and back injuries among nursing assistants. J Adv Nurs. 2012;68(4):836–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun C, Buchholz B, Quinn M, Punnett L, Galligan C, Gore R. Ergonomic evaluation of slide boards used by home care aides to assist client transfers. Ergonomics. 2018;61(7):913–922. [DOI] [PubMed] [Google Scholar]
- 38.McCaughey D, McGhan G, Kim J, Brannon D, Leroy H, Jablonski R. Workforce implications of injury among home health workers: evidence from the National Home Health Aide Survey. Gerontologist. 2012;52(4):493–505. [DOI] [PubMed] [Google Scholar]
- 39.Pompeii LA, Lipscomb HJ, Schoenfisch AL, Dement JM. Musculoskeletal injuries resulting from patient handling tasks among hospital workers. Am J Ind Med. 2009;52(7):571–578. [DOI] [PubMed] [Google Scholar]
- 40.National Research Council. The Future of Home Health Care: Workshop Summary. Washington, D.C.: The National Academies Press;2015. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


