Summary
Upper limb burn treatment represents a major medical and surgical challenge. Enzymatic escharolysis is a rather new technique to treat thermal burns in an easy and rapid way, as an alternative to the standard of care. The aim of the study was to investigate and describe the efficacy of treatment of upper limb burns with NexoBrid® in a non-burn referral center. All patients suffering from upper limb burns and admitted within 36 hours to the Hand and Microsurgery Unit of the ASST Sette Laghi from December 2016 to June 2018 were enrolled in the study. A retrospective analysis was performed, evaluating time to wound healing, time of hospitalization, and scar aesthetic appearance with patient and observer scar assessment scale (POSAS) and disabilities of the arm, shoulder and hand score (DASH). A total of 18 patients with burns involving the upper limb from December 2016 to June 2018 were treated. The mean TBSA% involved was 3%; 4 out of 18 patients suffered circumferential burns. The mean POSAS score was 14; the mean DASH score at 6-month follow up was 21, while it reduced to 11 at the last follow up visit. Enzymatic escharolysis is a novel, rapid and selective treatment option that allows early physiotherapy with overall satisfying functional results. We believe that enzymatic escharolysis should be considered, in most cases, as the standard of care in the treatment of upper limb burn wounds in non-burn referral centers.
Keywords: burn wound, hand surgery, upper limb, compartment syndrome, enzymatic debridement, escharotomy
Abstract
Le traitement des brûlures du membre supérieur (MS) est un défi médico- chirurgical majeur. Le débridement enzymatique est une technique relativement récente, facile et rapide, représentant une alternative au traitement classique. Le but de cette étude est d’évaluer l’utilisation du Nexobrid® dans le traitement, hors CTB, des brûlures du MS. Les 18 patients souffrant de brûlure du MS, hospitalisés entre décembre 2016 et juin 2018 dans le service de microchirurgie et de chirurgie de la main du Groupement Hospitalier de Territoire Sette Laghi dans les 36 h suivant l’accident ont été étudiés selon une étude rétrospective évaluant le délai de cicatrisation, la durée d’hospitalisation, l’aspect esthétique de la cicatrice (échelle POSAS), la fonction du MS (échelle DASH). La surface atteinte moyenne était de 3%, 4 patients avaient une atteinte circulaire. Le POSAS moyen était de 14, le DASH moyen à 6 mois de 21, s’abaissant à 11 à la dernière consultation de suivi. Le débridement enzymatique permet une rééducation plus précoce, avec des résultats fonctionnels satisfaisants. Nous pensons que cette technique est à privilégier dans le traitement hors CTB des brûlures du MS.
Introduction
Burns are common traumatic injuries caused by heat, cold or chemicals that can lead to superficial to full thickness skin and soft tissue damage. Although in most studies there is evidence of a reduction in incidence and mortality associated with burns, these injuries represent the fourth most frequent cause of trauma worldwide1 and are still cause of morbidity and mortality, prolonged hospitalization, disability and retracting scars that affect the quality of a patient’s life. Burn injuries of the hands have a specific place in the field of burn care, being very common, involving 30% to 90% of all burnt patients,2-4 especially in the pediatric age. Since hand function is based on its extreme mobility, which involves structures coming from arm and forearm, it is important to keep the flexibility and elasticity of this region, preventing retraction, dysfunction and disfigurement consequent to the burn-related scar. In recent decades, several studies3-5 focused on the investigation of an effective debridement technique capable of removing all necrotic tissue while preserving the vital dermis, in order to improve the patient’s outcome and the quality of the sub-sequential scar.
Indeed, when a full thickness burn scar is present, it is mandatory to radically remove the burn eschar with the purpose of preventing eschar-related complication and debride the non-viable tissue. Ideally, debridement should also be effective in preventing and resolving burn-induced compartment syndrome (BICS).
Currently, the standard of care (SOC) consists in an early tangential excision and skin grafting,6-7 which is rapid and effective but can lead to important blood loss,8-9 pain,10 and often poor aesthetic and functional outcome.11 Furthermore, it is a non-selective process that removes also potentially vital tissues, that, in the upper limb, can make the difference between a functional or non-functional arm and requires, in most cases, general anesthesia in the operating theatre.
Enzymatic debridement is an innovative and promising system which uses proteolytic enzymes or chemical agents to remove the burn eschar.12 This procedure has some advantages: blood loss is reduced, vital dermis is preserved (keeping the regenerative potential intact), and it is less traumatic and painful compared to a purely surgical procedure.13-16 However, among the drawbacks it is well known that it is a very slow process, it is less effective than surgical excision, and is related with a higher rate of severe infections.17
Only in the last few years has a new bromelain-derived topical treatment been developed, approved in late 2012. NexoBrid (MediWound, Yavne, Israel)is a pharmaceutical product that uses proteolytic enzymes enriched in bromelain (a derivative from the stem of the pineapple plant) as an escharolitic agent, that allows for a rapid and selective debridement of the burn eschar with, in some cases, a potential reduction in healing time and better long-term results.11-12,16 The aim of the present study was to investigate and describe the efficacy of treatment of upper limb burns with NexoBrid® in a non-burn referral center.
Materials and methods
All patients suffering from upper limbs burns and admitted to the Hand and Microsurgery Unit of the ASST Sette Laghi within 36 hours from December 2016 to June 2018 were enrolled in the study. Patients suffering from burns to the upper extremities and elsewhere were included in the study, but for the study purpose only the upper limb outcomes were evaluated. The exclusion criteria were represented by a proven allergy to bromelain. No other exclusions were present since major burns do not arrive at our hospital. A retrospective analysis was performed, evaluating time to wound healing, time of hospitalization and scar aesthetic appearance with the patient and observer scar assessment scale (POSAS) and disabilities of the arm, shoulder and hand score (DASH).
Treatment protocol
At admission, the burnt area was assessed, recording the burn characteristics and etiology, the total body surface area (TBSA) and patient demographics. The burnt area was then washed with sterile saline to remove necrotic superficial tissues. Meanwhile, Nexobrid powder was prepared for the application. The product was spread on the burnt region, preventively delimited by petroleum-based gel, to delimitate the affected area and to limit the dispersion of the product during the procedure. Occlusive dressing remained in place for four hours on top of the area. After this time, the dressing was removed, and all necrotic tissues were taken away by scratching them with a sterile wooden tongue depressor. The treatment proceeded applying a wet-todry dressing, which was changed every two hours, until the wound bed was clean (Fig. 1).
This process was repeated approximately twice per week until epithelialization occurred, or a surgical coverage was planned.
Fig. 1. A) Case of a 75-year-old woman with a circumferential deep dermal and subdermal burn on the forearm; B) Notice the appearance of the region after the first dressing change and after product application and C) the result after wet to dry dressing removal after 12 hours; D) The result after 58 days.

Anesthetic protocols and settings of treatment
Patients were treated in different settings depending on age, comorbidities, extension and location of the injury. According to the setting where the patient was treated, different anesthetic protocols were used: a soft sedation with Midazolam or another benzodiazepine, with 5mg intramuscular injection of morphine for pain control, was applied in the outpatient setting on the burns affecting the hand only 30 minutes before the application and removal of the product. Patients with a more extensive TBSA% of the upper limb proximal to the hand required a controlled anesthetic procedure in the Recovery Room with brachial plexus anesthesia.
For patients with extensive burns (where not only the upper limb was involved or depending on age and comorbidities), a general anesthesia or deep sedation was performed in theatre.
Vital parameters of all patients were monitored during the anesthetic procedure and product application.
General burns vital support and monitoring were performed.18 Pain assessment was measured with the visual analogue scale (VAS) both before and after the debridement until the patient was discharged.
At 6 months after injury we administered the POSAS and DASH questionnaire to the patients in order to evaluate range of motion related to daily routine, and the DASH questionnaire at the last follow-up visit.
Results
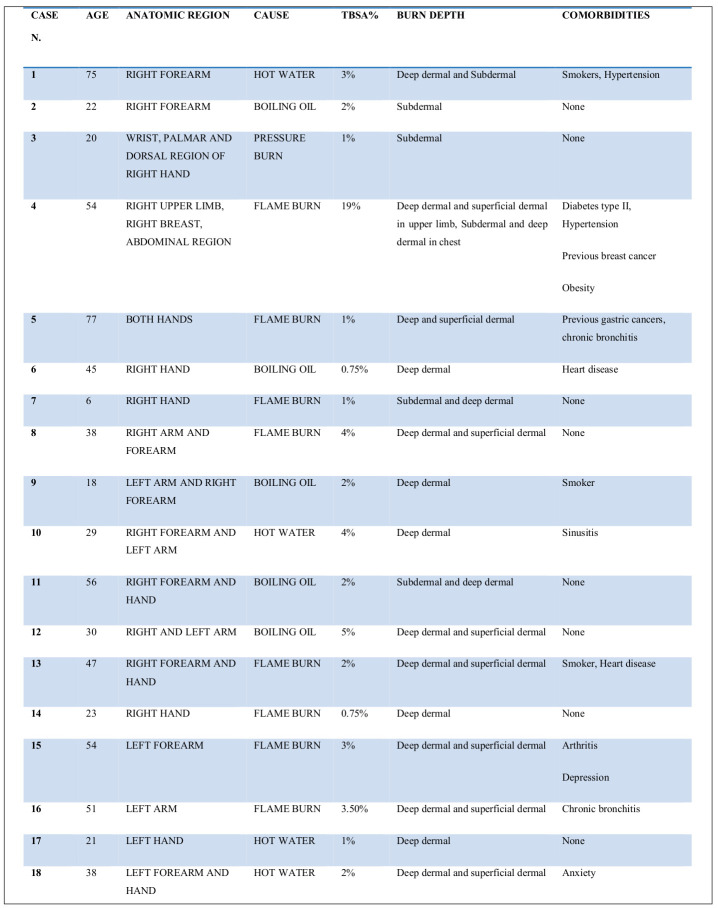
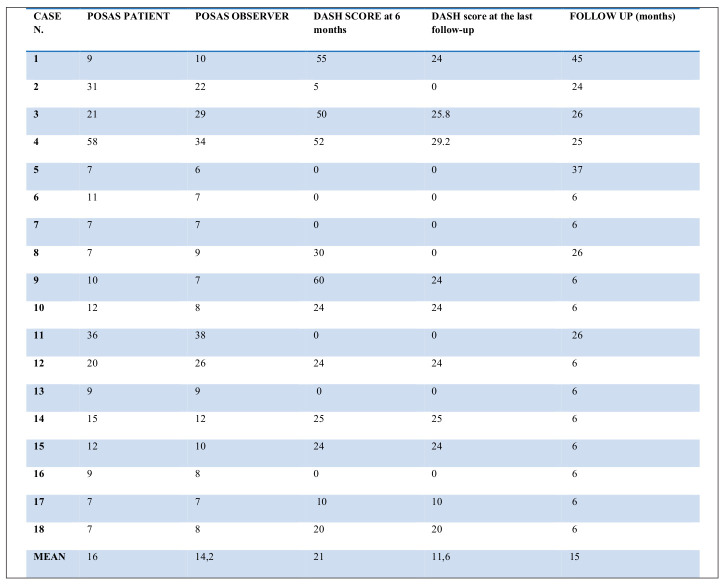
upper limb from December 2016 to June 2018 were enrolled. The mean TBSA% involved was 3% (range 1-19%) and therefore the burns were to be classified as minor/moderate burn injuries that did not require a Burn Center referral. The patients did not present relevant comorbidities and were overall in good health. Mean age was 39 years (range 18-77 years), 10 were male and 8 female. At admission and after product application, intra-compartment pressure was measured with a slit catheter (Table I).
Table I. Patient demographics and burn characteristics.
The vast majority of the burns were caused by domestic accidents and were thermal injuries (hot liquid in 9 cases, 5 by direct flame damage and 4 by fuel backfire) while only 1 burn occurred at work (pressure burn) (Table I). Six patients presented burns involving the hand alone, while the others involved the forearm as well (7), the forearm alone (3) (Fig. 1), one the forearm and the arm, one the arm alone, and in one case the entire upper limb and part of the abdominal region (Table I).
A mean of 19.88 days was necessary to reach a complete closure of the wound defects (range 8-65 days). Only 3 cases required skin graft coverage.19 Physiotherapy started immediately after wet to dry medication removal, under analgesic control for the first days. The hospitalization time varied from a minimum of 1 day to a maximum of 4 days, with an average of 2.16 days. Three out of 18 patients underwent refinement surgeries, such as a secondary debridement or bandage change in plexus anesthesia in one-day surgery, and were regularly discharged before evening.
Only four patients needed to be treated in the operating theater; most of them (14 out of 18) were treated in an outpatient room (Fig. 2), and 4 in the theatre. The average follow-up was 15 months (6-45 months). At 6-month follow up the DASH questionnaire was administered to all patients: six patients obtained a score of 0 on the DASH scale (Table II). Physiotherapy was started as soon as possible, generally within 2 days (range 2-31days) from the procedures (Fig. 3).
Table II. POSAS and DASH scale results.
Fig. 2. 21-year-old patient with burn from hot water. A) The appearance before enzymatic escarolysis and B) with a surgical glove, working as an occlusive bandage containing the product.

Fig. 3. A) The same patient immediately after the treatment and B) after a few weeks. The hand healed perfectly without any additional treatment.

In four cases the patients suffered from circumferential burn, which needed a more careful monitoring of intra-compartment pressure (Table III).
Table III. Diagram of intra compartmental pressure variation (before and after enzymatic debridement) in circumferential cases.
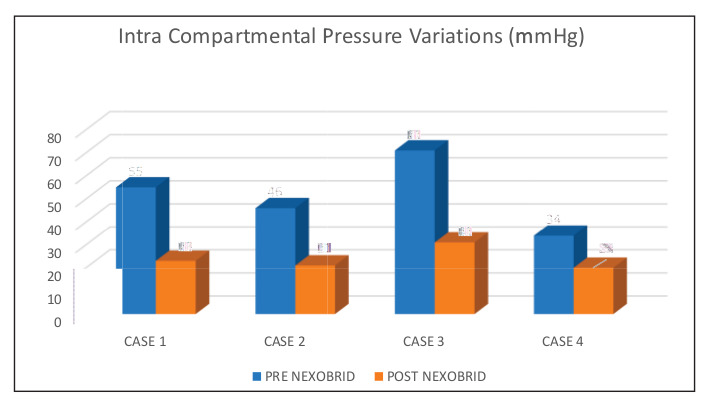
The first circumferential burn case was a 75-yearold woman with a 3% TBSA burn involving the forearm, caused by hot water. The patient presented deep dermal and full thickness injured areas. When Nexobrid was applied at admission, 36 hours after trauma, intra-compartment pressure resulted 55 mmHg. After 4 hours of application, pressure decreased to 23 mmHg.
The second case was a 22-year-old man who suffered from a work accident that caused a circumferential full thickness hand burn with a subtotal necrosis of the palmar region of the right hand. The wound was treated 6 hours after the trauma. Intra-compartment-pressure corresponded to 71 mmHg. Hence, we decided to combine escharolitic debridement with an open carpal tunnel decompression and the pressure lowered to 31 mmHg. Considering the severity of the lesion, the patient was investigated with indocyanine green to evaluate vascularization both before and after treatment.
The third patient presented a hot liquid burn, implicating 2% TBSA and involving the forearm, and the vast majority of the burns were full thickness. Escharolysis was performed 24 hours after the trauma and the pressure recorded decreased from the 46-mmHg initial value to 21 mmHg.
The last patient was a 54-year-old woman suffering from class 3 obesity that had previously undergone an axillary dissection after a lumpectomy for breast cancer. At the emergency department arrival, she presented a 20% TBSA burn, caused by fuel backfire, involving almost the totality of her right upper limb. The burn was classified as deep dermal and Nexobrid was applied also to prevent a possible burn-induced compartment syndrome (BICS) onset. Pressure decreased from 34 mmHg to 20 mmHg after the drug application.
No minor or major complications (haematoma/sieroma/major infection/adverse reaction to Nexobrid application) were recorded. One of the patients developed a scar contraction of the palm, probably due to secondary intention healing. After complete healing, the scar contraction impaired his everyday life and a suprafascial super-thin antero lateral thigh free flap, with standard post-operative care,20,21 was performed to release the scar contracture and restore function (Figs. 4,5,6).
Fig. 4. A) 18-year-old patient with burn due to a work accident with a flam; B) The hand appeared to be seriously compromised after enzymatic debridement; C) The third-degree burns area was treated with the dermal substitute.

Fig. 5. The same patient as in Fig. 4. At one-year follow-up, despite the initial good appearance, a severe scar contraction occurred resulting in a limitation of hand movement. A) upper and B) frontal view showing the scar contracture.

Fig. 6. A) The scar was removed, and the image gives an idea of the cutaneous defect; B) The final treatment was a thin suprafascial anterolateral thigh free flap; C) The final appearance after 12 months of follow-up.

In all cases we applied the POSAS scale22 in order to assess vascularity, pigmentation, thickness, relief, pliability and the surface area of the skin, with a mean score of 14 (range 6-38) (Table II).
Discussion
Tangential eschar removal followed by skin graft represents the standard of care (SOC) in burn treatment.5 On the other hand, this procedure is not selective and can lead to important blood loss and pain and the need for more complex reconstructive options.23 In the last few years, the surgical trend aimed to comprehend the least invasive procedures for the patient. Also, in burn treatment a minimally invasive procedure is generally desirable. Escharolitic debridement with a bromelainderived product allows to selectively digest non-viable tissues, limiting the blood loss common in SOC. This has also been demonstrated through bioptic investigations of partial thickness burn wounds, before and after enzymatic escharolysis. The dermis showed some “homogenization” characteristics, looking very similar to the scaffold of dermal matrices currently in use on the market.14 Moreover, sparing the vital dermis, it gives a spontaneous regenerative skin potential to create a greater number of newly formed epithelial cells that lead to wound healing in a shorter period.24
Furthermore, studies showed a potential benefit for enzymatic debridement in the treatment of severely burned hands and forearms specifically, reporting their clinical experience treated in a referral Burn Center.17
One of the essential features of enzymatic escharolysis compared to standard tangential escharectomy debridement is the possibility of an early and selective removal of the necrotic tissue. Hence, the diagnosis of burn depth by direct visual inspection is faster and wound healing and rehabilitation related treatment can both start promptly. An early and precise diagnosis of burn depth allows us to optimize the sub-sequential steps of burn wound management (e.g. further debridements, skin grafts). The peculiar way of applying the product and the smaller number of patients needing a skin graft makes a complete range of movements possible after the wet-to-dry dressing removal (average of 8 days from the trauma in our series).
The characteristic selectivity of Nexobrid® debridement allows a clean dermal bed where inflammation is minimized, and the risk of abundant granulation is controlled.
For all these reasons, complete restoration of fully healed tissue can be achieved in a short time (19.8 days), allowing for a prompt start to physiotherapy, which is of capital importance for the full recovery of movements in the upper limb.17 Also, hypertrophic scars occur more rarely if physiotherapy is started early.25
In our experience, the choice of bromelain-based escharolysis can be considered convenient once we take into account the total time of hospitalization (average time 2.16 days), operating theater use for escharolysis (only in 4 out of 18 cases) and the number of necessary secondary surgeries such as skin grafts (which was indicated only in full thickness defects in 3 out of 18 cases and always performed in day surgery).
Furthermore, in selected patients the products could be applied at the bedside or in an outpatient room, with minimal anesthesiology assistance (Figs. 2-3).
These considerations are particularly important in a small department of plastic and/or hand surgery, not designated as a burn center, where the use of enzymatic debridement for burn treatment allows a faster, easier and customized management and allocation of the patient.
One of the strengths of this study, at the current state of the literature, lies in having collected the highest number of cases of patients (18) with burns of the upper limb treated with Nexobrid. In addition, we consider the average follow-up days (401 days) to be sufficient to evaluate the final maturation of the scar and the complete rehabilitation protocol. A late scar contraction occurs even after an enzymatic procedure, and this required complete scar release and a free flap reconstruction. One of the main limits of the study is represented by the relatively small cohort of patients, which was not sufficient for a statistical analysis. Moreover, we use bromelain for treatment of burns and scalds. We are not sure how many of these could be healed appropriately even without the enzymatic treatment. Therefore, a comparative prospective study should be performed for more appropriate data. However, we think that a bromelain-derived product could be an adequate tool for the treatment of burns in non-burn referral centers. It not only performed the escharolysis but helped a non-expert burns surgeon to perform a correct diagnosis. Further studies are needed in order to perform a comparison between the use of Nexobrid vs. standard of care in upper limb burns to evaluate final morphological appearance and final function. This study represents a starting point and a point of reflection about the best treatment to be used on delicate areas, where the restoration of function is of paramount importance. It needs always to be taken into account that bromelain enzymatic treatment is not a final and a complete alternative to SOC. If conservative treatment fails in the first 3 weeks, a second surgical treatment is recommended.
In our experience, enzymatic debridement is a valuable tool in the treatment of burn wounds. The simplicity of its application, its selectivity and effectiveness in digesting only non-viable tissue and the possibility of an early treatment and diagnosis of burn depth make an optimal management of the burn wounds possible, even in delicate situations such as in the thermal injury of the upper limb, where also a moderate scar contracture may lead to a severe impairment of function.
Moreover, it has been shown that prompt enzymatic escharolysis can prevent, solve and vicariate the treatment of compartment syndrome, lowering intra-compartment pressure. Our experience should not be referred in the case of severe and deep circumferential burns, when escharotomy must be performed as soon as possible and the indication is clear. It does suggest, however, that in the case of moderate burns we can prevent unnecessary cuts.
Based on these findings, we consider the contribution provided by our experience to be important, as it adds important information to the understanding, management and treatment of this type of burns through the use of less invasive therapies, freer of complications. It is our opinion, indeed, that enzymatic debridement represents a valid or, in selected cases, even superior alternative to the current standard of care in the management of upper limb burn wounds.
Acknowledgments
Institutional review approval.This study was designed and registered within the internal database held in the Microsurgery and Hand Surgery unit, ASST “Sette Laghi”, University of Insubria, Varese, Italy
Ethical standards.All patients filled an informed valid consent prior to the treatment. This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000. The study was registered within the internal database of audits held in the Microsurgery and Hand Surgery unit, ASST “Sette Laghi”, University of Insubria, Varese, Italy and the Hospital institution accepted the publication of the data obtained and previously presented in the clinical audit section. The paper is an observational longitudinal study, it follows the STROBE checklist for cohort studies.
Acknowledgements.A special thanks to Marta Pedroni for her contribution to collecting data.
References
- 1.Smolle C, Cambiaso-Daniel J, Forbes AA, Wurzer P. Recent trends in burn epidemiology worldwide: a systematic review. Burns. 2017;43(2):249–257. doi: 10.1016/j.burns.2016.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krieger Y, Rubin G, Schulz A, Rosenberg N. Bromelainbased enzymatic debridement and minimal invasive modality (mim) care of deeply burned hands. Ann Burns Fire Disasters. 2017;30(3):198–204. [PMC free article] [PubMed] [Google Scholar]
- 3.Atiyeh BS, Gunn SW, Hayek SN. State of the art in burn treatment. World J Surg. 2005;29(2):131–148. doi: 10.1007/s00268-004-1082-2. [DOI] [PubMed] [Google Scholar]
- 4.Klasen HJ. A review on the nonoperative removal of necrotic tissue from burn wounds. Burns. 2000;26(3):207–222. doi: 10.1016/s0305-4179(99)00117-5. [DOI] [PubMed] [Google Scholar]
- 5.Choi M, Panthaki ZJ. Tangential excision of burn wounds. J Craniofac Surg. 2008;19(4):1056–1060. doi: 10.1097/SCS.0b013e318175f4f9. [DOI] [PubMed] [Google Scholar]
- 6.Prasanna M, Singh K, Kumar P. Early tangential excision and skin grafting as a routine method of burn wound management: an experience from a developing country. Burns. 1994;20(5):446–450. doi: 10.1016/0305-4179(94)90040-x. [DOI] [PubMed] [Google Scholar]
- 7.Pidcoke HF, Isbell CL, Herzig MC. Acute blood loss during burn and soft tissue excisions: an observational study of blood product resuscitation practices and focused review. J Trauma Acute Care Surg. 2015;78(6 Suppl 1):S39–S47. doi: 10.1097/TA.0000000000000627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo G, Fan H, Sun W. Blood loss during extensive escharectomy nd auto-microskin grafting in adult male major burn patients. Burns. 2011;37(5):790–793. doi: 10.1016/j.burns.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Singer AJ, Beto L, Singer DD, Williams J. Association between burn characteristics and pain severity. Am J Emerg Med. 2015;33(9):1229–1231. doi: 10.1016/j.ajem.2015.05.043. [DOI] [PubMed] [Google Scholar]
- 10.Van Zuijlen PP, Kreis RW, Vloemans AF, Groenevelt F, Mackie DP. The prognostic factors regarding long-term functional outcome of full-thickness hand burns. Burns. 1999;25:709–714. doi: 10.1016/s0305-4179(99)00067-4. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg L, Lapid O, Bogdanov-Berezovsky A. Safety and efficacy of a proteolytic enzyme for enzymatic burn debridement: a preliminary report. Burns. 2004;30(8):843–850. doi: 10.1016/j.burns.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg L, Krieger Y, Bogdanov-Berezovski A, Silberstein E. A novel rapid and selective enzymatic debridement agent for burn wound management: a multi-center RCT. Burns. 2014;40(3):466–474. doi: 10.1016/j.burns.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 13.Rosenberg L, Shoham Y, Krieger Y. Minimally invasive burn care: a review of seven clinical studies of rapid and selective debridement using a bromelain-based debriding enzyme (Nexobrid). Ann Burns Fire Disasters. 2015;28(4):264–274. [PMC free article] [PubMed] [Google Scholar]
- 14.Di Lonardo A, Nardini V, De Rosa M. Enzymatic escharolysis with Nexobrid® on partial thickness burn wound: pre- and post-debridement histological assessment. Ann Burns Fire Disasters. 2018;31(1):23–27. [PMC free article] [PubMed] [Google Scholar]
- 15.Cherubino M, Pellegatta I, Sallam D, Pulerà E, Valdatta L. Enzymatic debridement after mobile phone explosion: a case report. Ann Burns Fire Disasters. 2016;29(4):273–275. [PMC free article] [PubMed] [Google Scholar]
- 16.Hummel RP, Kautz PD, MacMillan BG, Altemeier WA. The continuing problem of sepsis-following enzymatic debridement ofburns. J Trauma. 1974;14(7):572–579. doi: 10.1097/00005373-197407000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Hirche C, Citterio A, Hoeksema H. Eschar removal by bromelain based enxymatic debridement (NexoBrid) in burns: a European consensus. Burns. 2017;43(8):1640–1653. doi: 10.1016/j.burns.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 18.Cordts T, Horter J, Vogelpohl J, Kremer T. Enzymatic debridement for the treatment of severly burned upper extremities – early single center experiences. BMC Dermatology. 2016;16:8–8. doi: 10.1186/s12895-016-0045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stocco C, Berton F, Papa G, Bussani R, Arnež ZM. Vicryl hypersensitivity test with histological response. Dermatitis. 2016;27(3):145–146. doi: 10.1097/DER.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 20.Arnež ZM, Ramella V, Papa G, Novati FC. Is the LICOX PtO2 system reliable for monitoring of free flaps? Comparison between two cohorts of patients. Microsurgery. 2019;39(5):423–427. doi: 10.1002/micr.30396. [DOI] [PubMed] [Google Scholar]
- 21.Stocco C, Papa G, Ramella V, Arnež ZM. Early detection of vascular obstruction in microvascular flaps using a thermographic camera. J Reconstr Microsurg. 2019;35(7):e5–e5. doi: 10.1055/s-0040-1702172. [DOI] [PubMed] [Google Scholar]
- 22.Vercelli S, Ferriero G, Bravini E. Cross-cultural adaptation, reproducibility and validation of the Italian version of the Patient and Observer Scar Assessment Scale (POSAS). Int Wound J. 2017;14(6):1262–1268. doi: 10.1111/iwj.12795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davis SC, Mertz PM, Bilevich DE, Cazzaniga AL, Eaglstein WH. Early debridement of second-degree burn wounds enhances the rate of epithelization - an animal model to evaluate burn wound therapies. J Burn Care Rehabil. 1996;17(6 Pt 1):558–561. doi: 10.1097/00004630-199611000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Maberou Houngbedji G, Alagnide E, Niama D, Dagba BS, Kpadonou TG. Effectiveness of early physiotherapy on cutaneous and musculoskeletal impairments in burn. Ann Phys Rehabil Med. 2016;59S:e141–e141. [Google Scholar]
- 25.Karimi H, Mobayen M, Alijanpour A. Management of hypertrophic burn scar: a comparison between the efficacy of exercise-physiotherapy and pressure garment-silicone on hypertrophic scar. Asian J Sports Med. 2013;4(1):70–75. doi: 10.5812/asjsm.34536. [DOI] [PMC free article] [PubMed] [Google Scholar]