Summary
Our aim is to characterize chronic wound response to autologous adipose-derived stem cell (ADSC) sheet transplantation. A pilot descriptive longitudinal study was conducted at the Wound Healing Center of the Vietnam National Burn Hospital from July 1, 2019 to August 30, 2020. Thirty patients with 38 chronic wounds were enrolled in the study and were grafted with autologous ADSC sheets on the wound bed. Wound edges, wound bed, wound size and structure using H&E staining, ultrastructure changes by transmission electron microscope at the time of transplantation and at the first, second and third week of follow-up were observed. Results indicated that after ADSC sheet transplantation, the structure and ultrastructure of chronic wounds had improved. The extracellular matrix (ECM), neo-vascular, fibroblast and collagen fibers proliferated and arranged side by side at the dermis layer. Fibroblast proliferated and increased secretion of collagen. Keratinocytes proliferated and immigrated in the epidermis layer. After three weeks of autologous ADSC sheet transplantation, epithelial cells covered 90% of the wound surface. Neo-vascular, fibroblast and collagen proliferation increased weekly. The image of lymphocyte infiltration in connective tissues decreased. Wound size reduced significantly compared to before the experiment, wound beds were cleaner and filled with granulation tissue. Re-epithelialization appeared at the wound edge and throughout the wound. Wound measurements were statistically significant at the second and third weeks after starting treatment (week 2: 12.8±11.56 cm2 [range: 1-47.42 cm2], p<0.05; week 3: 7.44 ± 5.68 cm2 [range: 0.45- 20.10 cm2], p<0.001), indicating autologous ADSC treatment enhanced healing of chronic wounds. In conclusion, ADSCs have a beneficial effect on cutaneous regeneration and chronic wound healing.
Keywords: adipose-derived stem cells, chronic wounds, structure, ultrastructure
Abstract
Cet étude a pour but de caractériser la réponse des plaies chroniques à la greffe de feuillets de CSA. Nous avons réalisé une étude pilote longitudinale descriptive auprès de 30 patients porteurs de 38 plaies chroniques hospitalisés dans le service de vulnérologie de l’hôpital brûlologique national du Vietnam entre le 1er juillet 2019 et le 30 août 2020, greffés par des feuillets de CSA autologues. La plaies a été évaluée cliniquement, optiquement après coloration hématoxyline- éosine et sous microscope électronique à transmission au moment de la greffe et à 1, 2 et 3 semaines. Ces examens objectivent une amélioration de la plaie. On constate une prolifération de la matrice extra- cellulaire, un développement de la néo- vascularisation, une prolifération fibroblastique avec sécrétion de fibres collagènes qui s’arrangent parallèlement dans le derme, progressant de semaine en semaine, alors que l’infiltration lymphocytaire. On observe une prolifération de kératinocytes, qui migrent vers l’épiderme. À 3 semaines, les cellules épithéliales couvraient 90% de la surface de la plaie, à partir des bords comme du fond de la plaie dont la surface diminuait de manière significative. Les berges étaient plus propres et colonisées par du tissu de granulation. La variation de surface étaient significatives dès la 2ème semaine (12,8 +/- 11,56 cm² ; de 1 à 47,42). À la 3ème semaine, elle était de 7,44 +/- 5,68 cm² (0,45 à 20,1) ; p< 0,05. Nous concluons que la greffe de feuillets de CSA promeut la cicatrisation des plaies chroniques.
Introduction
Chronic wounds are breaks in the skin of greater than six weeks or with frequent recurrence. The most common etiologies of chronic wounds include venous leg ulcers, pressure ulcers, diabetic neuropathic foot ulcers, and leg ulcers of arterial insufficiency.1 From the etiologic classification alone, comorbid conditions are identified that have a significant impact on patient morbidity and mortality related to wounds.1 Chronic wounds present major challenges for the clinician and wound care specialist by consuming a great deal of healthcare resources.2 Despite the development of new therapeutic methods, the treatment of chronic wounds remains unsatisfactory, and more effective treatment strategies are needed.2 Adipose-derived stem cells (ADSCs) isolated from liposuction or lipectomy specimens are mesenchymal and multipotential stem cells.3 ADSCs are easier to isolate and are relatively abundant, which may make them better stem cell sources for wound repair and regeneration.3 Studies demonstrate that ADSCs are involved in the wound healing process by secretion of growth factors and cytokines to promote skin repair and regeneration, and differentiate into other lineages and cell types.4,5,6,7,8 However, the mechanism of how ADSCs promote skin regeneration is unclear.8 Most published trials on the effectiveness of ADSCs in skin regeneration are in vivo or in vitro studies. Few clinical trials have been conducted. 9,10,11,12
In Vietnam, there is only one wound healing center located at the Vietnam National Burn Hospital in the capital city of Hanoi. Every year, on average our center treats approximately 1,000 in-patients with acute and chronic wounds. The goal of the study is to evaluate the effects of autologous ADSC sheet transplantation by measuring clinical signs, structure and ultrastructure changes of chronic wounds.
Methods
A pilot descriptive longitudinal case series study was conducted at the Wound Healing Center of Vietnam National Burn Hospital from July 1, 2019 to August 30, 2020 after Institutional Ethics Committee approval.
Ethics statement
This study was executed in accordance with the recommendations and approved by the Scientific Council of Vietnam Ministry of Health (decision number 338/QD-BYT of January 22, 2014) and the Ethics Committee of the National Institute of Burns (permit was signed on August 20, 2013).
Subjects
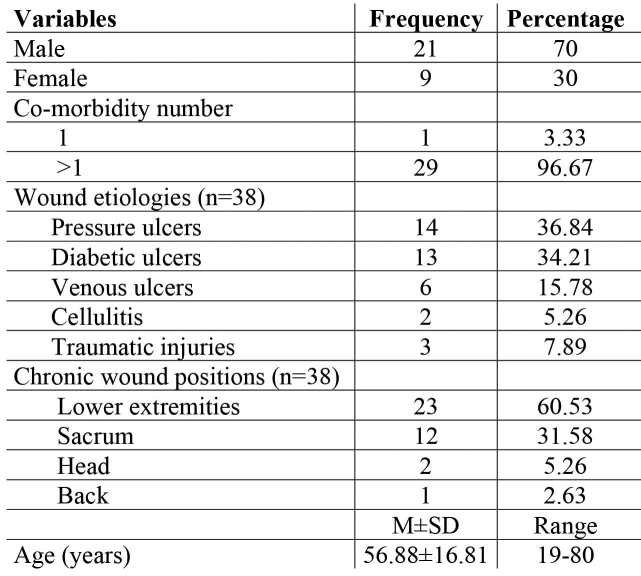
The study included 30 patients with a mean age of 56.88±16.81 years (range: 19-80 years). Most patients in this group were men (male to female ratio was 2:3). Twenty-nine (96.67%) patients had more than 1 comorbidity. These 30 patients had 38 wounds which demonstrated wound etiologies such as pressure ulcers (36.84%), diabetic ulcers (34.21%), venous ulcers (15.78%), cellulitis (5.26%), traumatic injuries (7.89%) and wound positions such as lower extremities (60.53%), sacrum (31.58%), head (5.26%) and back (2.63%) (Table I).
Table I. Socio-demographic variables and clinical characteristics of chronic wounds.
Procedure
On admission, all patients were evaluated for comorbid conditions, and chronic wound beds were managed by the multidisciplinary wound care team. Based on examination results, these teams planned activities aimed at improving comorbidities and optimizing wound bed preparation for cell therapy.
Isolation and culture of ADSCs in vitro
ADSCs were isolated from adipose tissue by ADSC extraction kit® which is manufactured by Geneworld Co., Ltd (ISO 13485, 16128 management system). This kit has been approved by the Ministry of Health to circulate in Vietnam (permit number: 87/2016/BYT-TBCT). Samples of human subcutaneous adipose tissue weighing 3-5grams were acquired from the patient’s hypogastric or groin area by the surgical ablation of adipose tissue. The adipose tissue was digested with 0.075% collagenase type I in phosphate-buffered saline under gentle agitation for 30 minutes at 37°C and centrifuged at 800×g for 10 minutes to obtain the stromal cell fraction. The pellets were resuspended, passed through a 100-mm mesh filter, and cultured at 37°C in 5% CO2 in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum, 100 mg/ml streptomycin, and 100 UI/ml penicillin. The culture medium was replaced every 3 days. The primary cells were cultured until 80% confluence and were defined as passage 1. In this study, ADSCs were used at passage 5. ADSCs at passage 5 were seeded onto a polycarbonate membrane of transwell with a density of 5x104 cells per cm2. The average time spent in isolation and culture of ADSCs in vitro was 12.63±3.78 days (range: 8-17 days).
Chronic wound management and autologous ADSC sheet transplantation
While waiting for isolation and culture of ADSCs, wound beds were prepared in all patients following the TIME framework13 by the wound care team. We only performed autologous ADSC sheet transplantation on wound beds of patients in a stable clinical condition. The wound beds themselves had no signs of necrosis or infection. In addition, bacterial culture result was negative or, if positive, with a median bacterial count in wound site before grafting of less than 105 cfu/cm2.
The autologous ADSC sheets were grafted on the wound surface every 2-5 days until wounds were closed by re-epithelialization and/or operation.
We assessed the wound edge and wound bed changes at the time of transplantation and at the first, second and third week of studied progress. This assessment was supported by photography. Wound size was calculated at every visit by the Image Pro Plus 4.5 software.
The wound biopsy was done before transplantation and at the first, second and third week to establish a baseline and follow progress through H&E staining and transmission electron microscope (TEM).
Statistical analysis
The results before and after the experiment were recorded and compared using Stata 11.0 software. The Wilcoxon test was used for comparative studies. The value of p ≤0.05 was considered statistically significant.
Results
Autologous ADSC transplantation could enhance wound healing of chronic wound
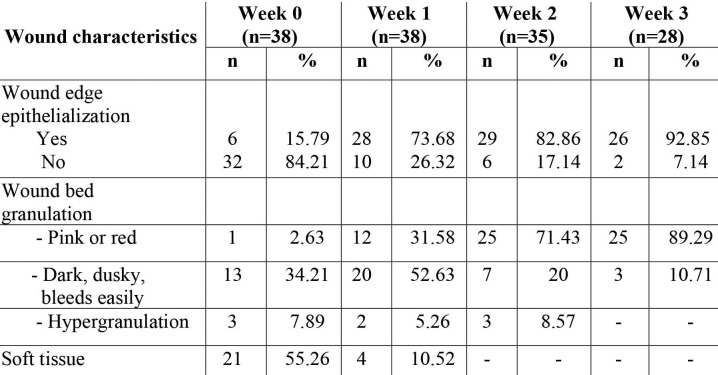
Among 38 wounds, before autologous ADSC sheet transplantation (week 0), 32 (84.21%) wounds had no epithelial signs along the wound edges, 21 (55.26%) showed absence of granulation tissue in the wound bed, 17 (44.73%) showed unhealthy granulation tissue that manifested as dark and dusky and bled easily (13 wounds - 34.21%). Only one wound had red granulation tissue and 3 (7.89%) wounds demonstrated hypergranulation tissue (Table II). After autologous ADSC sheet transplantation (weeks 1, 2 and 3), the wounds were markedly improved as the treatment progressed. The proportion of wounds with epithelialization at the wound edge and healthy granulation tissue increased significantly compared to before autologous ADSC sheet transplantation (82.86% of wounds at week 2 and 92.85% at week 3 had epithelialization, 71.43% of wounds at week 2 and 89.29% at week 3 had healthy granulation tissue). Three wounds (after 2 weeks) and 10 wounds (after 3 weeks) were closed by epithelialization alone or with skin grafts or skin flaps (Table II).
Table II. Wound characteristics before and after autologous ADSC sheet transplantation.
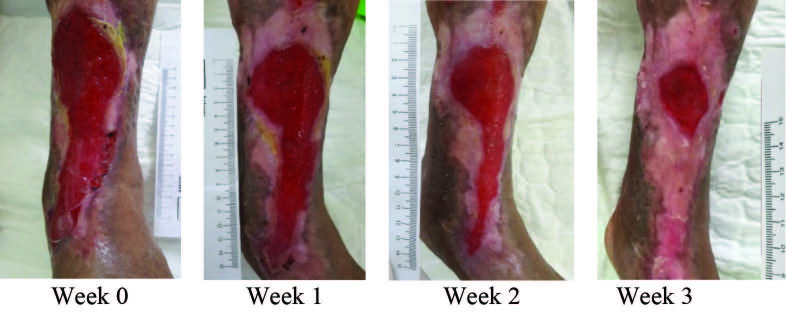
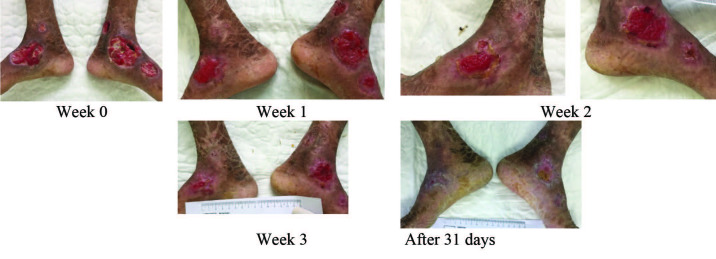
Autologous transplantation of ADSC sheets was used to treat chronic wounds with areas ranging between 23.72±19.85 cm2 (range: 3.01-81.38 cm2). The wound measurements were recorded weekly. The results before and after the experiment were compared by the Wilcoxon test. Our quantitative data were significantly different at the second and third weeks after starting treatment (week 2: 12.8±11.56 cm2 [range: 1-47.42 cm2], p<0.05; week 3: 7.44±5.68 cm2 [range: 0.45-20.10 cm2], p<0.001) (Fig. 1), indicating the autologous ADSC treatment enhanced the healing of chronic wounds.
Fig. 1. Chronic wound was treated by autologous ADSC sheets: representative images of venous ulcer are shown at week 0,1,2 and 3.
Structure and ultrastructure of chronic wound after autologous ADSC sheet transplantation
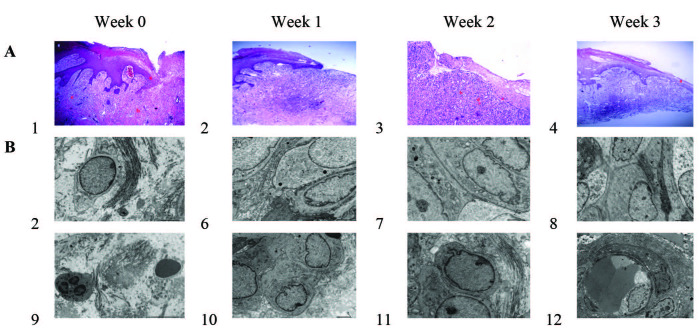
In the 30 patients, 38 chronic wounds were biopsied for H&E staining and TEM. Before autologousADSC transplant, chronic wound structure was characterized by hyperproliferative epidermis. In addition, presence of hyperkeratosis (a thick cornified layer) and parakeratosis were additional hallmarks portraying epidermal keratinocytes of chronic wound. The capillary and fibroblast density were low. In the epidermis and dermis layer, the principal leukocytes were polymorphonuclear leukocytes and macrophages (Fig. II A1). In ultrastructure imaging, tissue was swollen. Collagen fibers were deranged and not bound (interact). There were many polymorphonuclear leukocytes and lymphocytes in ECM (Fig. II B5 and B9).
At week one post autologous ADSC sheet transplantation, wound beds were cleaner and had filled with granulation tissue. Re-epithelialization appeared at the wound edge. The neo-vascular, fibroblast and collagen fibers proliferated and arranged side by side at the dermis layer. There were many active rough endoplasmic reticulum in the fibroblast. Fibroblast increased pro-collagen production and collagen secretion (collagen fibers were arranged in compact, parallel and beside fibroblast) (Fig. II A2, B6 and B10).
At week two post autologous ADSC sheet transplantation, keratinocytes proliferated and immigrated to the epidermis layer. However, this epidermis layer was still thin (which only had stratum basale layer, stratum spinosum layer and partial stratum granulosum layer). Connective tissue was densely infiltrated with lymphocytes. Images of neo-vascular, fibroblast and collagen proliferation were very clear in the dermis layer (Fig. II A3). In the ultrastructure image, the epithelial cells of the stratum basale layer were close to each other, without intercellular space (Fig. II B7). In ECM, fibroblast proliferated strongly and increased secretion of collagen (Fig. II B11).
At week three post autologous ADSC sheet transplantation, epithelial cells covered most of the wound surface. Structure of the epidermis layer gradually returned to the epidermis structure of healthy skin. Neo-vascular, fibroblast and collagen proliferated at an increased rate compared to the previous weeks. Fewer lymphocytes infiltrated in the connective tissues (Fig. II A4). In ultrastructure imaging, fibroblasts replaced myofibroblast (Fig. II B8). ECM significantly improved as seen with neo-vascular (which has thin wall and large endothelial cells) (Fig. II B12).
Fig. 2. Histology of chronic wound before and after autologous ADSC sheet transplantation: (A) Chronic wound histological images (original magnification x100, H&E stain); (B) Chronic wound ultrastructure images (TEM). (A1, B5 and B6) The structure and ultrastructure before the autologous ADSC sheet transplantation. (A2, B6 and B10), (A3, B7 and B11), (A4, B8 and B12) are the structures and ultrastructure of chronic wound after 1 week, 2 weeks and 3 weeks from autologous ADSC transplantation.
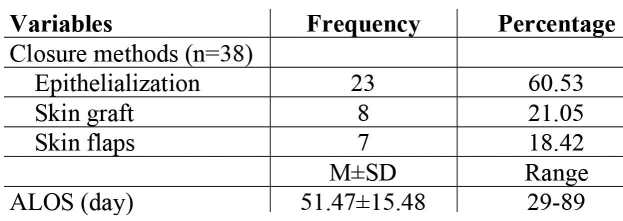
The treatment result and side effects of autologous ADSC sheet transplantation
After autologous ADSC sheet transplantation, among 38 wounds, 23 (60.53%) wounds were closed by epithelialization alone (Fig. III), 15 (39.47%) wounds were closed by skin grafts or skin flaps. The average length of stay in hospital (ALOS) was 51.47±15.48 days (range: 29-89 days) (Table III). 32 (84.21%) wounds had no side effects, and 3 (7.89%) wounds had infection and hypergranulation.
Fig. 3. After autologous ADSC sheet transplantation: wound in lower extremities of the patient with ichthyosis was closed by epithelialization.
Table III. Closure methods and average length of stay in hospital.
Discussion
While not all wounds in this pilot study closed primarily through ADSC, it appeared all wounds demonstrated improved ECM. Chronic wounds lack an ECM that promotes wound healing.2,14 Several therapies exist to promote chronic wound healing, however the lack of a healthy ECM limits wound healing. For instance, negative pressure wound therapy (NPWT) promotes wound healing by improving oxygenation, cellular proliferation, granulation and reducing bacterial load and inhibitory cytokines.15 Another therapy option is low temperature plasma (LTP) following surgical debridement.16,17 LTP is considered fine-tuning the debridement after removing nonvisible necrotic tissue with LTP.16 Platelet rich plasma (PRP) is another method demonstrated in a meta-analysis that promotes the healing process in chronic ulcers.17 PRP is rich in growth factors such as PDGF, transforming growth factor-β, platelet factor 4, epidermal growth factor, epithelial cell growth factor which causes cellular proliferation, angiogenesis, reduced inflammation and epithelialization to stimulate wound healing.16,17,18
Studies have demonstrated that ADSCs are involved in the wound healing process by secretion of growth factors and cytokines to promote skin repair and regeneration while differentiating into other lineages and cell types.5,6,7,8
In this study, among the 30 patients who were included, 29 (96.67%) patients had more than one comorbidity. Before hospitalization at our center, their chronic wounds failed to respond to presently available treatment plans that include dressings or skin graft. When these patients were admitted to our center, they were evaluated by our multidisciplinary teams to manage comorbidities, then grafted with autologous ADSC sheets on the wound bed.
Epithelialization is an essential component of wound healing. Epithelialization occurs by an orderly series of events whereby keratinocytes migrate, proliferate and differentiate to restore the covering function of skin.19 Granulation tissue is new connective tissue and microscopic neovascularization that form on the surfaces of a wound during the healing process. The healthy granulation tissue will create a favorable condition for epithelialization, skin grafting, or local flap surgeries at the wound site.20 In this study, before autologous ADSC sheet transplantation, almost all wounds had unhealthy granulation which was expressed as dusky, necrotic tissue (13 wounds - 34.21%). Only one of the wounds had healthy, red granulation tissue, while three (7.89%) had signs of hypergranulation (Table II). One week following ADSC, the proportion of wounds with unhealthy granulation tissue decreased, replaced by healthy granulation tissue. We also observed that after one week, epithelialization appeared at the edge of the wounds (73.68% of wounds). The proportion of the wounds with epithelialization rose at week two (82.86% of wounds) and by week three, 92.85% of wounds showed improved epithelialization.
Addressing wound size, after autologous ADSC transplantation wound dimensions decreased significantly compared to before transplantation. In a study about the effect of secretory factors of ADSCs on human keratinocytes, Kyoung Mi Moon and coworkers showed that ADSCs contained various growth factors, making it an attractive raw material for healing.20 Advanced ADSC protein extract contained growth factor/cytokines such as HGF, FGF-1, G-CSF, GM-CSF, IL-6, VEGF and TGF-β3. More keratinocyte wound healing and migration was shown in the experimental group.5 In another study, Won-Serk Kim and colleagues directly compared ADSC treatment with collagen gel solution without any transplantation, verifying that ADSCs in collagen gel solution are effective in wound healing in vivo.21 To confirm the practical role of ADSCs, Kim and colleagues went on to say that treatment of collagen gel solution and that of ADSCs in the collagen gel solution is valid.21 ADSC treatment significantly accelerated wound healing after 7 days with faster healing in the ADSC-treated group than in the control group. Closure was almost achieved within 14 days.21
Structure and ultrastructure of chronic wound after autologous ADSC sheet transplantation
In preparation for autologous ADSC sheet transplantation, while waiting for ADSC culture and to seed them onto a polycarbonate membrane of transwell with a density of 5x104 cells per cm2, besides the treatment of the patients’ comorbidities, we managed chronic wounds by dressing changes with antimicrobial agents (BETAplast Silver, Aquacel Ag) and debridement. Our aim was to prepare a clean receiving bed that was without signs of inflammation. We waited for bacterial culture results to be negative or positive with the median bacterial count in wound site before grating less than 105 cfu/cm2. However, before autologous ADSC sheet transplantation, we still saw evidence of chronicity of wounds in terms of structure and ultrastructure as determined by the presence of hyperkeratosis (a thick cornified layer) and parakeratosis. In addition, capillary and fibroblast density were very low. In the epidermis and dermis layer, the principal leukocytes were polymorphonuclear leukocytes and macrophages. Collagen fibers were degraded and not bound (interact). There were many polymorphonuclear leukocytes and lymphocytes in the ECM.
The effects of ADSCs on wound healing and skin regeneration has been proven by in vivo and in vitro studies. Seung Ho and co-authors found that the proliferation of HaCaT cells and fibroblasts was increased by ADSCs in the viability assay.4 ADSCs promoted in vitro wound healing of HaCaT cells and increased the contraction of the fibroblast-populated collagen lattice. Transcription-polymerase chain reaction showed that the transcription of the type I procollagen α1 chain gene in fibroblasts was upregulated by conditioned medium of ADSCs (ADSCs-CM). ADSCs promoted human dermal fibroblast (HDF) proliferation, not only by cell-to-cell direct contact, which was confirmed by co-culture experiment, but also by paracrine activation through secretory factors, resolved by transwell co-culture and culturing with conditioned medium of ADSCs. ADSCs enhanced the secretion of type I collagen in HDFs by regulating the mRNA levels of ECM proteins: upregulation of collagen type I, III and fibronectin and down-regulation of MMP-1.19 Moreover, ADSCs-CM showed a stimulatory effect on migration of HDFs in vitrowound healing models.19As an in vivo comparison study, the impact of human ADSC sheet transplantation onto mice full-thickness excision wound, Cerqueira and co-investigators found that ADSCs promoted neo-tissue vascularization at days 14 and 21.22
In this study, we observed improved wound healing rates and structure of the wound as seen in in vitro and in vivo studies.18,19,20,21,22 The neo-vascular, fibroblast and collagen fiber proliferation and arranging side-byside at the dermis layer improves wound healing.18,19,21,22 Fibroblast increased pro-collagen production and collagen secretion (collagen fibers were arranged in compact, parallel and beside fibroblast) at day seven. Neo-vascular, fibroblast and collagen proliferation were very clear in the dermis layer. The epithelial cells of the stratum basale layer were close to each other, without intercellular space. In the ECM, fibroblast proliferated strongly and increased their secretion of collagen at days 14, which resulted in almost complete re-epithelialization of the wound by week 3.
Currently, a number of investigators have used ADSCs in wound healing studies.7,8 Some studies demonstrated transdifferentiation of ADSCs into keratinocyte-like cells7 and epithelial and endothelial lineages,7 others reported improved wound healing parameters including increasedwound closure rate (reepithelialization), increased healthy granulation tissue, and improved wound vascularity and perfusion. 23,24,25,26,27 However, the mechanism of how ADSCs promote skin regeneration is unclear.5 Our study is a descriptive longitudinal case series study limited by the absence of a control group. Nevertheless, we feel that the longitudinal nature of our study adds significance to the attractiveness of autologous ADSC sheet transplantation as a supportive therapy. These observations are preliminary, and therefore not conclusive, as they require further studies allowing comparisons with a control group and evaluation of changes of ADSCs after transplantation on the wound bed.
Conclusion
This study demonstrates statistically significant improved wound healing rates related to the effects of ADSCs in cutaneous regeneration. ADSC sheet transplantation promotes the wound healing process through cell proliferation and improved structure of ECM in the chronic wound site.
Acknowledgments
Conflict of interest.The authors declare no conflict of interest.
Acknowledgements.We are grateful to all staff of the National Burn Hospital, Hanoi, and the Histology Department for helping us to collect data.
References
- 1.Markova A, Eliot NM. skin disease assessment: ulcer and wound care. Dermatol Clin. 2012;30(1)):107–111. doi: 10.1016/j.det.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care. 2015;4(8):560–582. doi: 10.1089/wound.2015.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zuk PA, Zhu P, Ashjian P, De Ugarte DA, Huang JI. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13:4279–4295. doi: 10.1091/mbc.E02-02-0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seung Ho Lee , Sang Yun Jin , Jin Seok Song Paracrine effects of adipose-derived stem cells on keratinocytes and dermal fibroblasts. Ann Dermatol. 2012;24(2):136–143. doi: 10.5021/ad.2012.24.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kyoung Mi Moon , Ye-Hyoung Park , Jea Seol Lee The effect of secretory factors of adipose-derived stem cells on human keratinocytes. Int J Mol Sci. 2012;13:1239–1257. doi: 10.3390/ijms13011239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mazini L, Rochette L, Admou B. Hopes and limits of adipose-derived stem cells (ADSCs) and mesenchymal stem cells (MSCs) in wound healing. Int J Mol Sci. 2020;21(4):1–19. doi: 10.3390/ijms21041306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chavez-Munoz C, Nguyen KT, Xu W. Trans-differentiation of adipose-derived stem cells into keratinocyte-like cells: engineering a stratified epidermis. PLoS ONE. 2013;8(2):e80587–e80587. doi: 10.1371/journal.pone.0080587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nie C, Yang D, Xu J, Si Z. Locally administered adiposederived stem cells accelerate wound healing through differentiation and vasculogenesis. Cell Transplant. 2001;20(2):205–216. doi: 10.3727/096368910X520065. [DOI] [PubMed] [Google Scholar]
- 9.Marino G, Moraci M, Armenia E. Therapy with autologous adipose-derived regenerative cells for the care of chronic ulcer of lower limbs in patients with peripheral arterial disease. J Surg Res. 2013;185(1):36–44. doi: 10.1016/j.jss.2013.05.024. [DOI] [PubMed] [Google Scholar]
- 10.Han S-K, Kim H-R, Kim W-K. The treatment of diabetic foot ulcers with uncultured, processed lipoaspirate cells: a pilot study. Wound Repair Regen. 2010;18(4)X:342–348. doi: 10.1111/j.1524-475X.2010.00593.x. [DOI] [PubMed] [Google Scholar]
- 11.Chopinaud M, Labbé D, Creveuil C. Autologous adipose tissue graft to treat hypertensive leg ulcer: a pilot study. Dermatology. 2017 doi: 10.1159/000478009. 10.1159/000478009. [DOI] [PubMed] [Google Scholar]
- 12.Holm JS, Toyserkani NM, Sorensen JA. Adipose-derived stem cells for treatment of chronic ulcers: current status. Stem Cell Res Ther. 2018;9:142–142. doi: 10.1186/s13287-018-0887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schultz G, Sibbald G, Falanga V. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen. 2003;11:1–28. doi: 10.1046/j.1524-475x.11.s2.1.x. [DOI] [PubMed] [Google Scholar]
- 14.Pai DR, Madan SS. Techniques in chronic wound management: review of the literature and recent concepts. J Nov Physiother. 2013;3(2) 134.doi:10.4172/2165-7025.1000134. [Google Scholar]
- 15.Plikaitis CM, Molnar JA. Subatmospheric pressure wound therapy and the vacuum-assisted closure device: basic science and current clinical successes. Expert Rev Med Devices. 2006;3:175–184. doi: 10.1586/17434440.3.2.175. [DOI] [PubMed] [Google Scholar]
- 16.Kramer A, Hübner NO, Weltmann WD, Lademann J. Polypragmasia in the therapy of infected wounds-conclusions drawn from the perspectives of low temperature plasma technology for plasma wound therapy. GMS Krankenhhyg Interdiszip. 2008;3:13–13. [PMC free article] [PubMed] [Google Scholar]
- 17.Villela DL, Santos VL. Evidence on the use of platelet-rich plasma for diabetic ulcer: a systematic review. Growth Factors. 2010;28:111–116. doi: 10.3109/08977190903468185. [DOI] [PubMed] [Google Scholar]
- 18.Lacci KM, Dardik A. Platelet-rich plasma: support for its use in wound healing. Yale J Biol Med. 2010;83:1–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Pastar I, Stojadinovic O, Yin NC. Epithelialization in wound healing: a comprehensive review. Adv Wound Care. 2014;3(7):445–464. doi: 10.1089/wound.2013.0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Oliveira Gonzalez AC, Fortuna Costa T, de Araújo Andrade Z. Wound healing - a literature review. An Bras Dermatol. 2016;91(5):614–620. doi: 10.1590/abd1806-4841.20164741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Won Serk Kim , Byung Soon Park , Jong Hyuk Sung Wound healing effect of adipose-derived stem cells: a critical role of secretory factors on human dermal fibroblasts. J Dermatol Sci. 2007;48:15–24. doi: 10.1016/j.jdermsci.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 22.Cerqueira MT, Pirraco RP, Santos TC. Human adipose stem cells cell sheet constructs impact epidermal morphogenesis in full-thickness excisional wounds. Biomacromolecules. 2013;14(11):3997–4008. doi: 10.1021/bm4011062. [DOI] [PubMed] [Google Scholar]
- 23.Manning CN, Martel C, Sakiyama SE-E. Adipose-derived mesenchymal stromal cells modulate tendon fibroblast responses to macrophage-induced inflammation in vitro. Stem Cell Research Therapy. 2015;6(74):59–64. doi: 10.1186/s13287-015-0059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nakagami H, Maeda K, Morishita R. Novel autologous cell therapy in ischemic limb disease through growth factor secretion by cultured adipose tissue-derived stromal cells. Arterioscler Thromb Vasc Bio. 2005;25:2542–2547. doi: 10.1161/01.ATV.0000190701.92007.6d. [DOI] [PubMed] [Google Scholar]
- 25.Alexaki VI, Simantiraki D, Panayiotopoulou M. Adipose tissue-derived mesenchymal cells support skin re-epithelialization through secretion of KGF-1 and PDGF-BB: comparison with dermal fibroblasts. Cell Transplantation. 2012;21:2441–2454. doi: 10.3727/096368912X637064. [DOI] [PubMed] [Google Scholar]
- 26.Mendez JJ, Ghaedi M, Sivarapatna A. Mesenchymal stromal cells form vascular tubes when placed in fibrin sealant and accelerate wound healing in vivo. Biomaterials. 2015;40:61–71. doi: 10.1016/j.biomaterials.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McLaughlin MM, Marra KG. The use of adipose-derived stem cells as sheets for wound healing. Organogenesis. 2013;9(2):79–81. doi: 10.4161/org.24946. [DOI] [PMC free article] [PubMed] [Google Scholar]