Abstract
Background:
Religiosity and/or spirituality (R/S) of physicians have been reported to inform behavior regarding religiosity and spirituality in clinical practice (R/S-B). Our aim was to study this association.
Methods:
Building upon a large international data pool of physician values we performed network and systematic literature searches using Google Scholar, Web of Science, Embase, Medline, and PsycInfo. Measures for R/S and R/S-B were selected for comparability with existing research. We performed a two-stage IPDMA using R/S coefficients from sample-wise multiple regression analyses as summary measures. We controlled for age, gender, and medical specialty. An additional sub-analysis compared psychiatrists to non-psychiatrists.
Results:
We found 11 eligible surveys from 8 countries (n = 3159). We found a positive association between R/S and R/S-B with an overall R/S coefficient of 0.65 (0.48–0.83). All samples revealed a positive association between R/S and R/S-B. Only 2 out of the 11 samples differed from the overall confidence interval. Psychiatrists had a higher degree of R/S-B, but associations with R/S did not differ compared to non-psychiatrists.
Conclusions:
We confirmed a significant association between R/S and R/S-B in this study. Despite large cultural differences between samples, coefficients remained almost constant when controlling for confounders, indicating a cultural independent effect of R/S on R/S-B, which to our knowledge has not been documented before.
Such interaction can constitute both facilitators and barriers for high quality health care and should be considered in all aspects of patient and relationship-centered medicine.
Keywords: meta-analysis, physicians, religion, religiosity, spirituality
1. Introduction
Physicians’ attitudes and self-reported behavior regarding religiosity and spirituality in clinical practice (R/S-B) have been reported to be informed by physicians’ own religious and/or spiritual characteristics (R/S).[1] Physicians who describe themselves as religious or spiritual have been linked with a higher likelihood of discussing and attending to patients’ R/S issues,[1,2,3,4,5,6,7,8] to pray with patients,[1] and less often referring patients to mental health facilities than their non-religious peers.[9] Also, cooperation with clergy and/or pastoral professionals are reported more often by religious physicians.[10]
Statements like these have been tone-setting throughout this research field during the last 2 decades. Still, findings stem primarily from an American survey from 2005[11] and several additional observational studies. Most commonly the association between R/S and R/S-B has been analyzed using single variable measures for R/S-B (i.e., self-reported tendency to inquire about patients’ R/S), and while measurements for R/S have sometimes been based on a single variable[8,12,13] others have used a composite scale.[1,4,5,14,15] Findings have been mixed. While some report a positive association,[1,4,5,7,8,14] others have not been able to confirm this relationship,[3,12,13] and some have reported mixed results.[15] Most studies known to us report findings based on analyses that do not control for known confounders like age, gender and medical specialty.[3,5,7,8,12,14] In summary, the designs and robustness of previous analyses seem largely varied and deficient as a basis for drawing valid and comparable conclusions.
Only a few studies have attempted international comparison of findings,[6,16] and the association between R/S and R/S-B has never been explored in a systematic meta-analysis. The international comparisons that exist have pointed toward large cross-cultural differences in both physicians’ religiosity and their attitudes and behavior towards R/S. Also, besides age and gender, medical specialty has been found to influence behavior,[3] and mainly psychiatrists have been pointed out as being less religious, but possibly more spiritual, than their colleagues from other medical specialties.[9,17] Due to the many heterogeneous studies and findings over the last 2 decades, there is a need for an international overview using standardized measurements in a weighted comparison.
In this study our aim was to investigate the association between physicians’ religious characteristics (R/S) and their self-reported behavior regarding R/S in clinical practice (R/S-B) using raw data from a large international data pool of physician values. Using comparable outcome measures of associations, we were able to compare the degree of association between the samples.
2. Methods and materials
2.1. Data source
We used the NERSH Data Pool v3.0 as data source.[18,19] Members of the international Network for Research in Spirituality and Health (NERSH) have shared ideas and data since 2003. The original questionnaire used was the Religion and Spirituality in Medicine: Physicians’ Perspectives (RSMPP) by Curlin, which was used in a nation-wide survey of American physicians in 2005.[11] Later, members of NERSH created a new questionnaire based on the RSMPP called the “NERSH Questionnaire.” By 2015 the network had performed a total of 12 surveys in nine different countries. These surveys became the founding datasets of the first version of the NERSH Data Pool (N = 5353).[20,21]
The data pool has been updated twice since 2015 using 3different strategies: Network, citation, and literature searches. Network searches were performed continuously in an unformal way using primarily e-mail correspondences between NERSH collaborators with a focus on available raw datasets based on either the RSMPP or the NERSH Questionnaire regardless if published or unpublished. Citation and literature searches were performed in 2016 and 2020 looking for articles based on either the RSMPP or the NERSH Questionnaire (See Table S1, Supplemental Digital Content in Supplemental Content for search details including search strings).
In 2016 we added 3 more samples from known NERSH collaborators: A sample of Brazilian resident physicians by Lucchetti (N = 171), a South Korean sample of psychiatric staff members by Lee et al (N = 281)[22,23] and a sample of Swiss physicians used in the thesis by Münger (N = 79).[24] In addition, we performed a citations search in Web of Science, and systematic literature searches (Medline, Embase, PsycInfo, Web of Science and Google Scholar).[25] Searches were performed by the first and last author, looking for RSMPP or NERSH surveys that were not already known within our network.[20] The citation search yielded 316 and 1572 items, respectively, and identified 2 samples not previously known to us: Tomasso et al (N = 146)[26] and Al-Yousefi (N = 225).[13] Both research groups were invited to join the collaboration, and both agreed. The systematic literature search using the search strings did not find any samples not already found using the network or citation searches. In total, 5 new samples were added to the data pool in 2016 and was released as NERSH Data Pool 2.0 comprising a total of 17 samples.
In 2020 we renewed the searches, applying the same strategy and search strings.[18] In total 6 new surveys were eligible to import into the NERSH Data Pool. Two from the network search and 4 from the citation search in Web of Science. The systematic literature search using the search strings did not find any samples not already found using the network or citation searches. From within the NERSH collaboration Lee et al were able to share with us a sample of German hospital chaplains (N = 138),[27] and Hefti et al had used the questionnaire to query family practitioners from the region of Bale and Aarau in Switzerland (N = 105).[28] The citation search found 4 eligible surveys. Cordero et al had collected 2 samples of Spanish and Portuguese nursing students,[29,30] (N = 75 and N = 158 respectively), and from Brazil by Menegatti-Chequini et al we identified 2 samples of psychiatrists: the first based on a survey among members of the Brazilian Psychiatry Association (ABP) (N = 508), and also a sample from a psychiatric department in São Paulo (N = 84). All researchers were contacted and invited to share their data, and all agreed to join the NERSH collaboration.
Signed data sharing agreements were collected from all contributors to the data pool. Raw data were sent to the first author in charge of data management and data curation in the NERSH Data Pool. Where interpretation of data was unclear, the original authors/researchers were contacted, and issues were resolved in collaboration. Each study included in the NERSH Data Pool was approved by the local research ethics committee if applicable.
We expected the published articles found in the systematic searches to report very distinct outcome measures. Also, because our goal was to find and recruit only raw datasets, regardless of individual local study goals, it did not make sense to quality grade the found articles.
Some local researchers used only a part of the original questionnaire, and others added further questions to their survey. Samples were acquired by traditional self-administered questionnaires except for the 2012 Brazilian physician study where face-to-face interviews were used.
The third version of the NERSH Data Pool used in this meta-analysis comprised a total of 7323 health professionals of which 4872 were physicians. The data pool has been described in detail in another publication,[18] and its codebook is available for download through the Open Science Framework.[19]
2.2. Meta-analysis design
Based on the original data described above we performed IPDMA. This design carries several advantages over traditional meta-analysis on aggregated data, allowing us to enforce strict inclusion/exclusion criteria, a uniform handling of missing values and also, we were able to include previously unpublished data.[31]
We performed 2 meta-analyses: a) Our primary analysis using all eligible surveys without grouping, and b) a separate analysis of the same samples but grouped into 2 groups: Psychiatrists and Non-psychiatrists. Both meta-analyses were performed as two-stage analyses using a random-effects inverse-variance model with DerSimonian-Laird estimate of tau. The dependent variables used were survey-wise multiple regression coefficients of physician R/S with physician R/S-B. We included age, gender, and medical specialty as potential confounders in both analyses. For the Congo sample (N = 112) we did not have information about medical specialty and could only control for age and gender.
All statistics were made with Stata 16.[32]
2.3. Physician R/S
A measure for physician R/S was constructed based on the 3 variables selected by Curlin et al in 2006.[1] This construct was chosen for its comparability to earlier research, and as a brief and pragmatic measure that includes both a “doing” and “being” aspect of intrinsic religiosity:[33] ”I try hard to carry my religious beliefs over into all my other dealings in life” (RS1) and “My whole approach to life is based on my religion” (RS2), respectively, as well as a measure of the identification as a spiritual person: “To what extent do you consider yourself a spiritual person” (RS3). RS1 and RS2 are the same items used as 2 out of 3 items in the intrinsic religiosity sub-scale of the DUREL index.[34]
RS3 was set as mandatory as it was the only measure of spirituality. If RS1 or RS2 was missing a value was imputed as the average of the other 2 variables. Sum scores were calculated as RS1+RS2+RS3 = R/S score. Internal consistency was evaluated using Cronbach's alpha. Characteristics including details of imputation are presented in Table 2.
Table 2.
Characteristics of measurements used.
| Measure | Item scoring∗ | Imputed, N | Sum score | N∗∗ | Mean (SD) | Min-max | Cronbachs α | |
| Religiosity/Spirituality (R/S) | ||||||||
| RS1 | ”I try hard to carry my religious beliefs over into all my other dealings in life” | 1–4 | 91† | Calculated as sum of individual scores. Total score ranging from 3 to 12 | 3159 | 7.02 (2.49) | 3–12 | 0.82‡ |
| RS2 | “My whole approach to life is based on my religion” | 1–4 | 27† | |||||
| RS3 | “To what extent do you consider yourself a spiritual person” | 1–4 | Not imputed | |||||
| Self-reported behavior regarding R/S in clinical practice (R/S-B) | ||||||||
| B1 | “I do inquire about R/S (yes/no)” | 0 – 1 | 79§ | Calculated as sum of individual scores. Total score ranging from 0 to 17 | 3,159 | 7.54 (3.13) | 0-17 | 0.61‡ |
| B2 | “I share my own R/S ideas and experiences” | 0–4 | 3† | |||||
| B3 | “I encourage patients’ R/S beliefs and practices” | 0–4 | 689† | |||||
| B4 | “I try to change the subject when R/S comes up” | 0–4 (reversed) | 10† | |||||
| B5 | “I pray with patients” | 0–4 | 3† | |||||
2.4. Physician R/S-B
For comparability with the original research by Curlin and to define a meaningful construct of self-reported behavior regarding R/S in clinical practice (R/S-B) we chose to construct a measure based on the 5 behavior variables reported by Curlin in 2006.[1] This construct covers different aspects of physician behavior including collection of information about patient R/S: “I do inquire about R/S (yes/no)” (B1), willingness to share personal R/S ideas and experiences with patients actively: “I share my own R/S ideas and experiences” (B2), physician use of patients’ R/S as a resource in treatment: “I encourage patients’ R/S beliefs and practices” (B3), avoidant behavior of the physician when confronted with R/S in the clinical setting: “I try to change the subject when R/S comes up” (B4), and whether the physician engages in active prayer with patients: “I pray with patients” (B5).
We required at least 4 out of the 5 question answered for the observation to be included in the meta-analysis. If B1 was missing we imputed a new value as either 0, 0.5 or 1 depending on the mean score of the available values B2-B5. If B2, B3, B4, or B5 was missing we set the value to the mean value of the remaining items.
The score of the BS4-item was reversed, and the total R/S-B score was calculated B1+B2+B3+B4 (reversed)+B5 = R/S-B. Internal consistency was evaluated using Cronbach's alpha. Characteristics including details of imputation are presented in Table 2.
2.5. Exclusion criteria
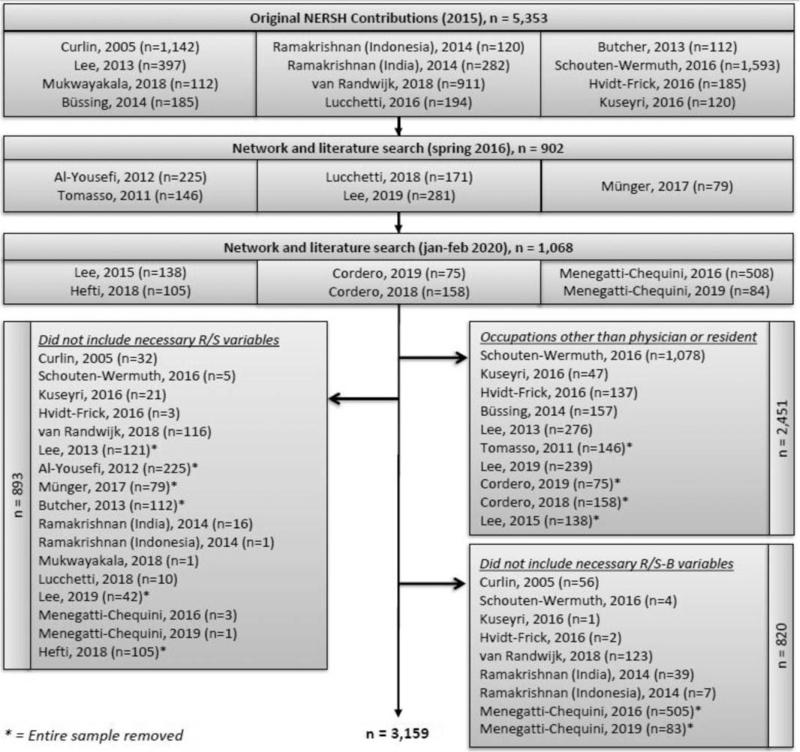
Gender identification and an age requirement of at least 18 years were enforced when building the data pool. For this study, we excluded further all non-physician participants (N = 2451). For the R/S-measure RS3 was set as mandatory, while we allowed either RS1 or RS2 to be omitted. This excluded 893 physicians. In addition, we required at least 4 out of the 5 R/S-B-measures, removing another 820 physicians. The full inclusion/exclusion diagram is presented in Figure 1.
Figure 1.
Inclusion and exclusion criteria.
3. Results
The latest systematic citation and literature searches in 2020 found 763 and 4,929 hits, respectively. Together with the network searches the original Data Pool comprised 7323 health professionals at the time of analysis.
After exclusion criteria were enforced a total of 3159 physicians from 11 samples remained for the meta-analysis. Eight countries were represented. Five studies were European, 2 were Brazilian, 2 were Asian, one was African, and one was American. The exclusion criteria seemed to favor samples from the earlier versions of the data pool. This was unintentional. Adjusting the criteria during or after analysis would compromise good research practice and was thus not an option.
Observations were sampled between 2002 (American sample by Curlin) and 2018 (Brazilian sample by Lucchetti). Age differed significantly between the samples, with the American and Danish physicians being eldest with a mean age of 48.8 and 48.5, respectively. The physicians from the samples by Ramakrishnan (Indonesia), 2014, and Lucchetti (Brazil), 2018, were the youngest with mean ages of 29.1 and 28.4. The gender composition of the samples differed as well. In total 42% of the included physicians were female. See Table 1 for the characteristics of the included physicians. (Table 1).
Table 1.
Characteristics of the physicians in the study (N = 3,159).
| Age | Gender (%) | Medical specialty (%) | ||||||||||||
| Author/study∗ | Country | Sample year | Mean | SD | Female | Male | Medical specialty | General practitio-ner | Gyn/Obs | Surgical | Para-clinial | Pediatric | Psych-iatry | Other |
| Curlin, 2005 | USA | 2002 | 48.8 | 8.4 | 280 (27) | 774 (73) | 291 (28) | 294 (28) | 77 (7) | 109 (10) | 17 (2) | 141 (13) | 94 (9) | 31 (3) |
| Schouten-Wermuth, 2016† | Germany | 2014 | 37.9 | 8.9 | 334 (66) | 172 (34) | – | – | 506 (100) | – | – | – | – | – |
| Kuseyri, 2016† | Germany | 2016 | 34.8 | 8.3 | 27 (53) | 24 (47) | 17 (34) | – | 2 (4) | 12 (24) | – | 4 (8) | 3 (6) | 12 (24) |
| Hvidt-Frick, 2016 | Germany | 2014 | 38.3 | 10.2 | 16 (37) | 27 (63) | 28 (65) | – | 9 (21) | – | – | – | – | 6 (14) |
| Büssing, 2014‡ | Austria | 2014 | 41.6 | 10.5 | 12 (43) | 16 (57) | 16 (59) | – | – | 4 (15) | – | – | – | 7 (26) |
| van Randwijk, 2018 | Denmark | 2012 | 48.5 | 12.2 | 284 (42) | 388 (58) | 111 (24) | 159 (35) | 21 (5) | 99 (22) | 11 (2) | 14 (3) | 36 (8) | 8 (2) |
| Ramakrishnan, 2014 | India | 2012 | 31.9 | 10.5 | 127 (56) | 100 (44) | 14 (8) | 43 (24) | 11 (6) | 5 (3) | 38 (21) | 10 (6) | 38 (21) | 20 (11) |
| Ramakrishnan, 2014 | Indonesia | 2010 | 29.1 | 3.6 | 60 (54) | 52 (46) | 8 (9) | 21 (22) | 7 (7) | 24 (26) | 14 (15) | 2 (2) | 1 (1) | 17 (18) |
| Mukwayakala, 2018† | Congo | 2012 | 35.1 | 8.0 | 28 (25) | 83 (75) | n/a | |||||||
| Lucchetti, 2016 | Brazil | 2012 | 37.7 | 11.1 | 49 (25) | 145 (75) | 146 (75) | – | 10 (5) | 26 (13) | – | 12 (6) | – | – |
| Lucchetti 2018‡ | Brazil | 2018 | 28.4 | 3.3 | 99 (61) | 62 (39) | 40 (25) | – | 19 (12) | 10 (6) | – | 17 (11) | 10 (6) | 65 (40) |
| Total | 1,316 (42) | 1,843 (58) | 671 | 517 | 662 | 289 | 80 | 200 | 182 | 166 | ||||
The constructed measures were evaluated for internal consistency with Cronbach's alpha. The R/S scale had an alpha value of 0.82, and the R/S-B scale 0.61 (Table 2), which were found acceptable for this study. The mean R/S-score in the combined dataset was 7.02 (SD = 2.49), and the mean R/S-B was 7.54 (SD = 3.13). (See Table S2, Supplemental Digital Content in Supplemental Content, for sample-wise unweighted mean-scores).
3.1. Association between R/S and R/S-B
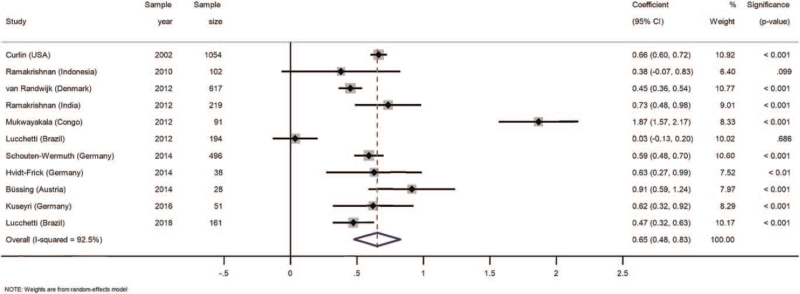
The overall coefficient for R/S (95% confidence interval) was 0.65 (0.48–0.83). All samples revealed a positive association and only 2 out of the 11 samples were outside the overall confidence interval. The Indonesian sample by Ramakrishnan (n = 102) and the Brazilian sample from Lucchetti, 2012 (n = 194) were not able to confirm a significant influence of R/S on R/S-B as their confidence intervals overlapped zero and P values were above .05. A significant and positive association was found for the remaining nine samples, P < .001 (Fig. 2). The between-study variance was high (Overall I 2 = 92.5%), explaining most of the total variance. (See Table S3, Supplemental Digital Content in Supplemental Content for sample-wise and unweighted results of the multiple regression analyses, including coefficients, confidence intervals, and significance levels of covariates).
Figure 2.
Forest plot of associations between physician religiosity/spirituality (R/S) and their self-reported behavior regarding R/S in clinical practice (R/S-B). Weights are from random effects model.
3.2. Psychiatrists versus non-psychiatrists
In a separate analysis of the psychiatrists included in the study we did not find any difference in overall R/S scores (95% confidence interval), 7.0 (6.92–7.10) for non-psychiatrists (N = 2977) compared to 7.2 (6.83–7.52) for psychiatrists (N = 182), but we found that overall self-reported behavior regarding R/S in clinical practice (R/S-B) was significantly different between the 2 groups. R/S-B for non-psychiatrists were 7.5 (7.38–7.61) compared to 8.3 (7.93–8.71) for the psychiatrists (see Table S4, Supplemental Digital Content, Supplemental Content, for detailed statistics of the 2 groups).
To analyze the association between R/S and R/S-B for the 2 groups we performed a separate meta-analysis using the same settings as the main meta-analysis in the study (random-effects model). For non-psychiatrists we found an overall coefficient of 0.55 (0.41–0.69), I 2 = 87.0%, and for the psychiatrists an overall coefficient for R/S of 0.49 (0.23–0.75), I 2 = 60.6%. The group coefficients were not statistically different. (See Figure S1, Supplemental Digital Content in Supplemental Content for the forest plot, including sample sizes and R/S coefficient significance levels.
4. Discussion
We found a significant association between R/S and R/S-B in the included samples. Coefficients were alike for all surveys except 2 samples from Brazil and Congo which we will discuss below. Psychiatrists reported a higher degree of R/S-B than their non-psychiatrist colleagues. Still the effects of R/S on R/S-B were equal for both groups. In neither meta-analysis performed did we find reason to suspect R/S to influence R/S-B differently across the included samples and cultures.
In the discussion below, we want to address 2 reasonable questions about the study design, and second to comment on our findings in relation to existing research.
4.1. Cross-cultural perspective
First, we need to answer whether it is feasible to compare physicians across cultures using a common R/S measure, and also whether it conceptually makes sense to do cross-cultural comparisons of physicians’ R/S and R/S-B at all when both have clear cultural underpinnings.
Albeit several instruments exist,[34,35,36,37] there is no consensus on how to measure R/S in research. Some have argued against finding a common R/S-measure, and instead favored a focus on better validity of local measurements within the local cultural context. Due to the multi-dimensional nature of religiosity and spirituality developing a uni-dimensional scale with both high internal and external validity has not been fruitful, and some have argued instead to focus on single-variable measures or reporting sub-scales like intrinsic religiosity.[34] While we agree with these thoughts and strategies to some degree, we must point out that scales adapted for local studies inhibit later meta-analyses, and thus limits international and cross-cultural research. Therefore, we must choose between uniform comparable measures with lower validity that enables meta-analyses, or a lot of separate developed measures with high internal validity, but with very limited external validity and difficult to include in meta-analyses. We cannot have both.
We therefore suggest that both strategies be applied in our research field, and that researchers learn to toggle between them when interpreting the literature aware of their strengths and limitations.
In this study we chose to perform the meta-analysis using IPDMA and utilized this study design's advantages over traditional meta-analyses, one of them being the possibility to enforce equal outcome measures for all studies. Enforcing less strict criteria on the validation of the measurements in exchange for better comparability, we had the possibility to enforce equal account for confounding influencers like age, gender, and medical specialty across all samples, which most other studies in this field have not been able to do.
Still, we were not able to control for influence from local culture other than that exerted by the medical specialty of which the physicians belong. Difference in cultural background is not solely an international challenge, but a phenomenon that may just as well be present in a sample of physicians from a single university hospital in a country with a diverse ethnic and religious landscape like the USA or most European countries.
As countries keep facing similar diseases and problems in health care it follows that they should prioritize international perspectives into the development of national healthcare strategies. Not least with the Covid-19 pandemic we saw just how quickly a local virus outbreak became the highest healthcare priority in every corner of the world. Illnesses that contain spiritual or existential dimensions are ubiquitous, underlining the need for healthcare professionals that understand and can work with these dimensions of illnesses.[38]
We also see how the world is becoming increasingly connected. Medical knowledge, education and even health care workers are crossing borders every day, sharing thoughts and experiences on how to perform optimal health care. This continual exchange of information (and culture) impacts first individual healthcare professionals, and second, the global medical community as a whole into something less disparate, and with greater and comparable overlaps in our views on health care. We thus believe it important to continually investigate the similarities and differences between physicians worldwide, accepting that culture contributes to the variation in the sample.
4.2. Association between R/S and R/S-B
This study utilized raw data from all samples found in the systematic searches, which allowed us to measure sample-wise associations using multiple regression while controlling for known confounders. Coefficients were weighted in the analysis and presented in the Forest plot (Fig. 2). Enforcing equal calculation of outcome measures of each included sample enabled us to limit variations in all comparisons. Still, the included samples were collected from different parts of the world, and hence it is only expected that the groups have distinct characteristics. Most likely one of the primary influencers here were local, regional, or national culture. Still, no other study has performed cross-cultural comparisons while controlling for as many other possible confounders as we did in this study, and we believe that we have raised the level of evidence behind the postulate that religious physicians more often than their non-religious colleagues engage in discussions with their patients about R/S-issues, including attention to the R/S needs of their patients.
We were not surprised to find a positive association between R/S and R/S-B looking solely on the American sample because we designed our outcome measures based on the variables selected by the original American study.[1] This is, however, the first time this association is documented using combined measures for both R/S and R/S-B in an American sample. Re-testing this hypothesis using another statistical design lifts the level of evidence and reassures us in the now widely held belief that many physicians may be influenced by personal belief and value systems in clinical practice.
Due to our exclusion criteria, 2 new Brazilian samples by Menegatti-Chequini et al were excluded from the analysis as they did not include the necessary R/S-B variables. Local analysis of their pilot sample did not find a significant correlation between physicians’ frequency of inquiry about patients’ religious/spiritual issues and the physicians’ religiosity or spiritualty in an uncontrolled comparison of 2 single-variables measures.[12] Later the same research group performed a more detailed latent profile analysis using a more complex measure of R/S on 592 psychiatrists controlling for covariates, showing that less religious psychiatrists less frequently asked about R/S-issues of their patients.[4] Their findings highlight the importance of robust statistical analysis that controls for confounders. Menegatti-Chequini et al also suggest that duration of psychiatric practice and level of academic education negatively correlated with being in the group of highly religious psychiatrists. Unfortunately, our raw material available in the present study did not allow us to include these parameters as covariates.
Influences by covariates were also reported in a Muslim sample of 225 physicians by Al-Yousefi et al The analysis controlled for covariates, and did not find physician R/S a significant factor for inquiring patients about R/S, but rather that higher age, male gender and intrinsic religiosity were positively associated with odds of physicians sharing their own R/S experiences.[13] Also, a German study by Voltmer et al reports that especially for female physicians, religiosity and spirituality were positively associated with addressing R/S issues with patients.[8]
Two Danish studies by Randwijk et al used a validated 4-item scale of “Religiosity of Health Professionals” that reported a positive association but did not control for a potential influence of age, gender, or medical specialty.[5,7] We included these data in our analysis and confirmed the earlier published findings even when covariates were taken into account.
4.3. Psychiatrists versus non-psychiatrists
We performed a sub-analysis stratifying the physicians into a group of psychiatrists and a control group of physicians of other medical specialties. We could not detect a difference in R/S between the groups using our combined R/S-measure (See Table S4, Supplemental Digital Content). Earlier studies identified a so-called “religiosity gap” between physicians and their patients, a gap that was larger in psychiatrists than in other specialties;[39] our study did not substantiate this difference, on the contrary. Due to our research design we were not able to delineate potential differences between the more distinct religious and spiritual dimensions in this measure, why we are not able to discard the hypothesis that psychiatrists are less religious but more spiritual.
Looking at the self-reported behavior of the psychiatrist we found a significant difference compared to other medical specialties using our combined R/S-B measure in which psychiatrists scored higher. This difference may be explained by how psychiatrists work in a field where patients often face existential crises involving private sacred entities that are either violated, threatened, or even lost. We use the term “sacred entities” here in the sense described by Pargament as private core experiences covering transcendence, boundlessness and ultimacy.[40] This premise in psychiatry may cultivate psychiatrists’ ability to meet, diagnose and treat these patients within a framework of understanding that facilitates the expression of R/S-values central to the patients’ suffering.
In the comparative analysis we did not find any significant difference between the association between R/S and R/S-B between the 2 groups. Based on these data we have no reason to suspect that any influence of personal values, whether religious or spiritual, exert a more significant or less influence on the psychiatrists than equal values would affect physicians from other medical specialties.
4.4. Cultural independent influence of R/S on R/S-B?
In each multiple regression analysis, we measured how much a single point increase in R/S-score changed the R/S-B score on average for that study. Following the hypothesis that religion and spirituality are very distinct concepts we could not discard the possibility that an increase in R/S-score would impact R/S-B at very different rates for separate samples and cultures. However, we found that the correlation coefficients for nine out of the eleven samples did not differ. We saw no significant positive correlation for the sample from Brazil, which may be explained by the fact that answers were collected using face-to-face interviews possibly limited extreme answers due to fear of stigmatization. The sample from Congo differed significantly from all other samples with an almost 2-point increase in R/S-B value for each increase in R/S (1.87, 95% CI 1.57–2.17). However, this finding may be biased because we lacked information about the medical specialty of the physicians from Congo and were thus not able to include this variable in the local regression analysis. Furthermore, the samples from Congo and Indonesia were the only samples not to include any physicians without a religious affiliation. We thus cannot reject the possibility that coefficients of these 2 samples are outliers due to their different designs, and for the Congo sample also sampling.
We believe we are the first research group to present plausible statistical evidence that the influence of R/S on R/S-B appears to be uniform across cultures.
4.5. Limitations
Any comparison of local survey results must be done with caution due to the significant between-samples heterogeneity. The heterogeneity was lower in the analysis grouped by medical specialty. Further stratification in future studies may make comparisons more feasible.
Even though the questionnaires were adapted to local cultural context, respondents’ understanding of religiosity and spirituality may still vary between studies to a degree not accounted for by the questionnaires. This may have added to the heterogeneity.
We have not been able to control for cohort effects because none of the samples have performed a follow-up survey.
The dataset from Lucchetti, 2016, of Brazilian physicians[6] was based on interviews rather than self-administered questionnaires, which may have led respondents to give less-extreme answers in fear of stigmatization. Contrary, face-to-face interviews may limit acquiescence bias where responders tire out in written questionnaires and give the same answer to multiple subsequent questions.
The outcome measures used in this study were chosen from available datasets, and to ensure comparability with earlier research, mainly the tone-setting work by Curlin. The measures showed promising initial reliability and we found them suitable for our purpose. Should they be used henceforth in new surveys we highly recommend evaluating them prior hand using best practice guidelines like COSMIN[41] and statistical testing using factor analysis.
We may have missed relevant potential confounders not available to us on our data material. Duration of working experience and level of academic degree are worth considering for future studies.
4.6. Perspectives
Our study points to substantial interaction of personal values and clinical practice across cultural settings, whether highly secular or more religiously inclined cultures. Such interaction can constitute both barriers and facilitators for high quality health care. As examples of barriers physician subjective values can
-
1.
breach with values and preferences of patients with different values,
-
2.
can become a trojan horse for hidden missionary ambitions and
-
3.
can breach with ideals of neutrality in healthcare.
As examples of facilitators subjective values can
-
1.
enhance sensitivity, understanding and empathy with the patients with R/S or other value-based challenges or resources,
-
2.
can strengthen the personal motivation of the physician, and
-
3.
can help an organization reflect the values that found its practice.
5. Conclusion
This study confirmed a positive association between physicians’ own religious and/or spiritual characteristics and their self-reported behavior regarding religiosity and spirituality in clinical practice. Although R/S-B was more prevalent among psychiatrists we did not find differences in R/S and R/S-B association compared to non-psychiatrists.
We suspect that cultural differences contributed to the large heterogeneity of the samples. Still, association coefficients remained almost constant when controlling for confounders, indicating a cultural independent effect of R/S on R/S-B, which to our knowledge, has not been documented before.
Reflexivity on the interplay between subjective values and clinical practice is of high relevance for high quality health care and should be considered in all aspects of patient and relationship centered medicine. Transparency seems to us the most viable approach to avoiding barriers and enhance facilitators of subjective values of physicians, an approach to which the present study seeks to contribute.
While local culture may explain why some physicians seem more prepared to handle R/S-issues in clinical practice than others, we believe these skills can be taught and practiced across cultures.
We recommend future research to include the development and evaluation of R/S programs for physicians, and that a future meta-analysis of the association between R/S and R/S-B be performed as the NERSH Data Pool grows.
Acknowledgments
The authors wish to thank Farr A. Curlin for his work within this field of research and not least for the development of the RSMPP, upon which the NERSH data pool rests. Also, Curlin contributed with the American dataset included in the data pool. Several NERSH collaborators have contributed to the NERSH data pool with local samples, for which we are very grateful: Christian Balslev van Randwijk, Can Kuseyri, Tryphon Mukwayakala, Wyatt Butcher.
We also thank statistician Sonja Wehberg who reviewed the meta-analyses performed by the authors.
Author contributions
Conceptualization: Alex Kappel Kørup, Niels Christian Hvidt.
Data curation: Alex Kappel Kørup, Rocío de Diego-Cordero, Maria Cecilia Menegatti-Chequini.
Formal analysis: Alex Kappel Kørup.
Funding acquisition: Alex Kappel Kørup, Giancarlo Lucchetti.
Investigation: Giancarlo Lucchetti, Parameshwaran Ramakrishnan, Klaus Baumann, Eunmi Lee, Eckhard Frick, Arndt Büssing, Nada A Alyousefi, Azimatul Karimah, Esther Schouten, Inga Wermuth, René Hefti, Niels Christian Hvidt.
Methodology: Alex Kappel Kørup.
Project administration: Alex Kappel Kørup, Niels Christian Hvidt.
Resources: Jens Søndergaard.
Supervision: Jens Søndergaard, Niels Christian Hvidt.
Visualization: Alex Kappel Kørup.
Writing – original draft: Alex Kappel Kørup.
Writing – review & editing: Jens Søndergaard, Giancarlo Lucchetti, Parameshwaran Ramakrishnan, Klaus Baumann, Eunmi Lee, Eckhard Frick, Arndt Büssing, Nada A Alyousefi, Azimatul Karimah, Esther Schouten, Inga Wermuth, René Hefti, Rocío de Diego-Cordero, Maria Cecilia Menegatti-Chequini, Niels Christian Hvidt.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: IPDMA = individual participant data meta-analysis, NERSH = network for research in spirituality and health, R/S = religiosity and/or spirituality, R/S-B = self-reported behavior regarding R/S in clinical practice, RSMPP = religion and spirituality in medicine: physicians’ perspectives (questionnaire).
How to cite this article: Kørup AK, Søndergaard J, Lucchetti G, Ramakrishnan P, Baumann K, Lee E, Frick E, Büssing A, Alyousefi NA, Karimah A, Schouten E, Wermuth I, Hefti R, de Diego-Cordero R, Menegatti-Chequini MC, Hvidt NC. Physicians’ religious/spiritual characteristics and their behavior regarding religiosity and spirituality in clinical practice: a meta-analysis of individual participant data. Medicine. 2021;100:52(e27750).
Ethics approval and consent to participate: Within the research field of “Religiosity and Health” it is only natural for readers to question potential influences of religious values of the researchers conducting the research. All authors of this study are committed to transparency and to obtaining the highest scientific standards. Nowhere in this article is one belief system, personal value or virtue set above another, and we have no intention, nor right, to argue in favor of any. Some of the authors are atheists. Others are devoted to own religious or spiritual belief systems, and several are affiliated with organized religious organizations.
Alex Kørup: Scholarship from University of Southern Denmark, and research grant from Psychiatric Research Foundation of Southern Denmark (Psykiatriens forskningsfond, Region of Southern Denmark).
Giancarlo Lucchetti: Grantee of Research Productivity Scholarship – Level 1D (Medicine) - Brazilian National Council for Scientific and Technological Development (CNPq), Brazil
Alex Kappel Kørup wrote the article as first author. Study conception and design. Statistical analysis. Data manager of the NERSH Data Pool.
Jens Søndergaard, hosting the NERSH Data Pool, research oversight; Study design and critical manuscript revision;
Giancarlo Lucchetti conceived, designed and performed the 2 Brazilian surveys. Data collection. Critical manuscript revision;
Parameshwaran Ramakrishnan conceived, designed and performed Indian survey. Data collection. Critical manuscript revision;
Klaus Baumann conceived, designed and performed the German survey in Freiburg: Data collection. Co-founder of the NERSH-Network; Critical manuscript revision;
Eunmi Lee conceived, designed and performed the survey German sample in Freiburg. Data collection. Critical manuscript revision;
Eckhard Frick, co-founder of the NERSH-Network, conceived, designed and performed a local German survey. Data collection. Critical manuscript revision;
Arndt Büssing, co-founder of the NERSH-Network. Critical manuscript revision. Performed reliability analyses in the first evaluation round;
Nada A. AlYousefi conceived, designed, and performed the Saudi Arabian survey. Data collection. Critical manuscript revision;
Azimatul Karimah conceived, designed and performed Indonesian survey. Data collection. Critical manuscript revision;
Esther Schouten, Data collection of the German perinatal sample. Critical manuscript revision;
Inga Wermuth, Study conception and design of the German perinatal sample; Data collection; Critical manuscript revision;
Rene Hefti, Study conception and design of the Swiss sample; Data collection; Critical manuscript revision;
Niels Christian Hvidt, project conception. Co-founder and coordinator of the NERSH-Network. Data collection of Danish sample. Critical manuscript revision;
The authors have no conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Supplemental digital content is available for this article.
First publication of local sample if any. If un-published the name of the head researcher and sample year was used.
Thesis.
Not published locally, sampling year used for identification.
Higher scores indicating higher degree of the construct measured.
Complete cases only.
Imputed as mean of remaining items.
Imputation did not alter α coefficient.
Mean of remaining item scores was converted to either 0, 0.5, or 1.
References
- [1].Curlin FA, Chin MH, Sellergren SA, Roach CJ, Lantos JD. The association of physicians’ religious characteristics with their attitudes and self-reported behaviors regarding religion and spirituality in the clinical encounter. Med Care 2006;44:446–53. [DOI] [PubMed] [Google Scholar]
- [2].Palmer Kelly E, Paredes AZ, Hyer M, Tsilimigras DI, Pawlik TM. The beliefs of cancer care providers regarding the role of religion and spirituality within the clinical encounter. Supportive Care Cancer 2021;29:909–15. [DOI] [PubMed] [Google Scholar]
- [3].Vasconcelos APSL, Lucchetti ALG, Cavalcanti APR, et al. Religiosity and spirituality of resident physicians and implications for clinical practice—the SBRAMER multicenter study. J General Internal Med 2020;35:3613–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Menegatti-Chequini MC, Loch AA, Leão FC, Peres MFP, Vallada H. Patterns of religiosity and spirituality of psychiatrists in Brazil and the implications for clinical practice: a latent profile analysis. BMC Psychiatry 2020;20:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Van Randwijk CB, Opsahl T, Assing Hvidt E, et al. Similarities and differences between Danish and American physicians’ religious characteristics and clinical communication: two cross-sectional surveys. Religions 2021;12:116. [Google Scholar]
- [6].Lucchetti G, Ramakrishnan P, Karimah A, et al. Spirituality, religiosity, and health: a comparison of physicians’ attitudes in Brazil, India, and Indonesia. Int J Behav Med 2016;23:63–70. [DOI] [PubMed] [Google Scholar]
- [7].van Randwijk CB, Opsahl T, Hvidt EA, et al. Characteristics of religious and spiritual beliefs of Danish Physicians: and likelihood of addressing religious and spiritual issues with patients. J Religion Health 2019;58:333–42. [DOI] [PubMed] [Google Scholar]
- [8].Voltmer E, Bussing A, Koenig HG, Al Zaben F. Religiosity/spirituality of German doctors in private practice and likelihood of addressing R/S issues with patients. J Relig Health 2014;53:1741–52. [DOI] [PubMed] [Google Scholar]
- [9].Curlin FA, Odell SV, Lawrence RE, et al. The relationship between psychiatry and religion among U.S. physicians. Psychiatr Serv 2007;58:1193–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Daaleman TP, Frey B. Prevalence and patterns of physician referral to clergy and pastoral care providers. Arch Fam Med 1998;7:548. [DOI] [PubMed] [Google Scholar]
- [11].Curlin FA, Lantos JD, Roach CJ, Sellergren SA, Chin MH. Religious characteristics of U.S. physicians: a national survey. J Gen Intern Med 2005;20:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Menegatti-Chequini MC, Maraldi EdO, Peres MF, Leao FC, Vallada H. How psychiatrists think about religious and spiritual beliefs in clinical practice: findings from a university hospital in Sao Paulo, Brazil. Braz J Psychiatry 2019;41:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Al-Yousefi NA. Observations of muslim physicians regarding the influence of religion on health and their clinical approach. J Relig Health 2012;51:269–80. [DOI] [PubMed] [Google Scholar]
- [14].Lee E, Baumann K. German psychiatrists’ observation and interpretation of religiosity/spirituality. Evid Based Complement Alternat Med 2013;2013:08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lee E, Zahn A, Baumann K. Religion in psychiatry and psychotherapy?” a pilot study: the meaning of religiosity/spirituality from staff's perspective in psychiatry and psychotherapy. Religions 2011;2:525–35. [Google Scholar]
- [16].Korup AK, Sondergaard J, Lucchetti G, et al. Religious values of physicians affect their clinical practice: a meta-analysis of individual participant data from 7 countries. Medicine (Baltimore) 2019;98:e17265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Curlin FA, Lawrence RE, Odell S, et al. Religion, spirituality, and medicine: psychiatrists’ and other physicians’ differing observations, interpretations, and clinical approaches. Am J Psychiatry 2007;164:1825–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kørup A, Søndergaard J, Alyousefi NA, et al. Health professionals’ attitudes toward religiosity and spirituality: a NERSH Data Pool based on 23 surveys from six continents. F1000Research 2021;10:446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kørup AK. NERSH Data Pool 3.0 Codebook. Open Science Framework (osr.io)2021. 10.17605/OSF.IO/J79PT. [DOI] [Google Scholar]
- [20].Hvidt NC, Kørup AK, Curlin FA, et al. The NERSH international collaboration on values, spirituality and religion in medicine: development of questionnaire, description of data pool, and overview of pool publications. Religions 2016;7:107. [Google Scholar]
- [21].Kørup AK, Nielsen CT, Søndergaard J, et al. The international NERSH data pool—a methodological description of a data pool of religious and spiritual values of health professionals from six continents. Religions 2017;8:24. [Google Scholar]
- [22].Lee E, Baumann K. Religiosity and spirituality: is it an appropriate issue in psychiatry and psychotherapy? —comparative studies of Germany and South Korea. Open J Soc Sci 2019;7:300–10. [Google Scholar]
- [23].Lee E, Baumann K. How Korean psychiatric staff deal with religious and spiritual issues of patients: what is professional? Religions 2019;10:544. [Google Scholar]
- [24].Münger R. Religious Characteristics of Family Physicians and their Perception of Religious and Spiritual Issues in the Doctor-Patient Relationship. 2017;Bern, Germany: Medical Faculty, University of Berne, 24. [Google Scholar]
- [25].Kørup AK, Søndergaard J, Alyousefi NA, et al. The international NERSH data pool of health professionals’ attitudes toward religiosity and spirituality in 12 countries. J Relig Health 2020;60:596–619. [DOI] [PubMed] [Google Scholar]
- [26].Tomasso CD, Beltrame IL, Lucchetti G. Knowledge and attitudes of nursing professors and students concerning the interface between spirituality, religiosity and health. Rev Lat Am Enfermagem 2011;19:1205–13. [DOI] [PubMed] [Google Scholar]
- [27].Lee E, Zahn A, Baumann K. How do psychiatric staffs approach religiosity/spirituality in clinical practice? Differing perceptions among psychiatric staff members and clinical chaplains. Religions 2015;6:930–47. [Google Scholar]
- [28].Hefti R, Wartenweiler T, Merz O. Der einfluss von religiosität und spiritualität auf die haltung von schweizer Ärzten gegenüber ethisch umstrittenen medizinischen Fragen. Praxis 2018;107:373–8. [DOI] [PubMed] [Google Scholar]
- [29].de Diego Cordero R, Lucchetti G, Fernández-Vazquez A, Badanta-Romero B. Opinions, knowledge and attitudes concerning “spirituality, religiosity and health” among health graduates in a Spanish University. J Relig Health 2019;58:1592–604. [DOI] [PubMed] [Google Scholar]
- [30].Cordero RDD, Romero BB, De Matos FA, et al. Opinions and attitudes on the relationship between spirituality, religiosity and health: A comparison between nursing students from Brazil and Portugal. J Clin Nurs 2018;27:2804–13. [DOI] [PubMed] [Google Scholar]
- [31].Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ 2010;340. [DOI] [PubMed] [Google Scholar]
- [32].StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. Stata (RRID:SCR_012763) [computer program]. [Google Scholar]
- [33].la Cour P, Hvidt NC. Research on meaning-making and health in secular society: secular, spiritual and religious existential orientations. Soc Sci Med 2010;71:1292–9. [DOI] [PubMed] [Google Scholar]
- [34].Koenig HG, Büssing A. The Duke University Religion Index (DUREL): a five-item measure for use in epidemological studies. Religions 2010;1:78–85. [Google Scholar]
- [35].Monod S, Brennan M, Rochat E, Martin E, Rochat S, Büla CJ. Instruments measuring spirituality in clinical research: a systematic review. J Gen Intern Med 2011;26:1345–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Huber S, Huber OW. The centrality of religiosity scale (CRS). Religions 2012;3:710–24. [Google Scholar]
- [37].Pargament K, Feuille M, Burdzy D. The brief RCOPE: current psychometric status of a short measure of religious coping. Religions 2011;2:51–76. [Google Scholar]
- [38].Hvidt NC, Nielsen KT, Kørup AK, et al. What is spiritual care? Professional perspectives on the concept of spiritual care identified through group concept mapping. BMJ Open 2020;10:e042142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Cook CCH. The faith of the psychiatrist. Mental Health, Religion Culture 2011;14:09–17. [Google Scholar]
- [40].Pargament KI. Spiritually Integrated Psychotherapy: Understanding and Addressing the Sacred. 2011;New York, NY: Guilford Press, 39. [Google Scholar]
- [41].Prinsen CAC, Mokkink LB, Bouter LM, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Quality of Life Research 2018;27:1147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.