Abstract
Rationale:
Plastic endobiliary stents, after endoscopic retrograde cholangiopancreatography, can get spontaneously dislocated from the common bile duct and migrate intothe distal bowel. Most migrated biliary stents are removed with the passing of stool. However, migrated biliary stents can cause bowel perforation, albeit rarely, and surgical intervention may be required. Recently, we observed a colonic diverticular perforation caused by a migrated biliary stent, and we have reported this case with a review of the literature.
Patients concerns:
A 74-year-old man presented with severe right lower quadrant pain after biliary stent insertion 1month ago.
Diagnoses:
Abdominal computed tomography revealed perforation of the proximal ascending colon by the migrated biliary stent, combined with localized peritonitis.
Interventions:
Emergency diagnostic laparoscopic examination revealed penetration of the proximal ascending colon by the plastic biliary stent, and right hemicolectomy was performed.
Outcomes:
On pathological examination, colonic diverticular perforation by the biliary stent was confirmed. The patient was discharged without any additional complications.
Lessons:
Endoscopic retrograde cholangiopancreatography endoscopists must always be cautious of the possibility of stent migration in patients with biliary stents in situ. In cases of biliary stent dislocation from the common bile duct in asymptomatic patients, follow-up with serial, plain abdominal radiographs, and physical examination is needed until confirmation of spontaneous passage through stool. In symptomatic cases suggesting peritonitis, abdominal computed tomography scan confirmation is needed, and early intervention should be considered.
Keywords: biliary stent, bowel perforation, endoscopic retrograde, endoscopic retrograde cholangiopancreatography
1. Introduction
Endoscopic biliary stents have been widely used for internal biliary drainage during endoscopic retrograde cholangiopancreatography (ERCP). Dislocation and migration of the endobiliary stent from the common bile duct (CBD) occasionally occurs.[1,2] Dislocated biliary stents usually migrate to the distal bowel owing to peristalsis, and spontaneously pass out with feces, not requiring additional intervention so long as it does not cause symptoms.[3] However, distal bowel perforation by migrated biliary stent occurs rarely, and it may require surgical intervention.[3,4,5,6,7] Herein, we report a case of colonic diverticular perforation caused by a migrated biliary stent, which is a very rare, late complication of ERCP, with a comprehensive review of previously reported cases.
2. Case report
A 74-year-old man presented with abdominal pain. He had a medical history of ERCP and laparoscopic cholecystectomy due to cholangitis with CBD stones and cholecystitis with gallbladder stones about 1 year ago. Biliary colic, associated with fever and chills, was observed. Physical examination revealed the presence of tenderness (and the absence of rebound tenderness) in the right upper quadrant area. Icteric sclera was also observed. Laboratory findings revealed white blood cell counts of 10,730/mm3, hemoglobin levels of 15.3 g/dL, total bilirubin levels of 3.0 mg/dL, aspartate aminotransferase levels of 346 IU/L, alanine aminotransferase levels of 85 IU/L, alkaline phosphatase levels of 156 IU/L, and gamma-glutamyl transferase levels of 1010 IU/L. Abdominal computed tomography (CT) revealed multiple CBD stones with bile duct dilation. ERCP was performed to remove the CBD stones, followed by endoscopic retrograde biliary drainage with a 10 Fr x 7 cm straight-type plastic stent inserted into the CBD to control acute suppurative cholangitis (Fig. 1). The patient was discharged without early complications. One month later, he presented with severe right lower quadrant (RLQ) pain. Physical examination revealed tenderness in the RLQ area with rebound tenderness. Laboratory findings revealed white blood cell counts of 8700/mm3, hemoglobin levels of 14.5 g/dL, total bilirubin levels of 1.1 mg/dL, aspartate aminotransferase levels of 19 IU/L, alanine aminotransferase levels of 11 IU/L, alkaline phosphatase levels of 53 IU/L, gamma-glutamyl transferase levels of 99 IU/L, and C-reactive protein levels of 12.5 mg/dL. On plain abdominal radiography, the migrated biliary stent was found in the distal bowel (located in the RLQ area) (Fig. 2). Abdominal CT revealed perforation of the proximal ascending colon by the migrated biliary stent, combined with localized peritonitis. However, there was no evidence of ascites, pneumoperitoneum, or peritonitis (Fig. 3). Emergency diagnostic laparoscopic examination revealed penetration of the proximal ascending colon by the plastic biliary stent, and right hemicolectomy was performed. On pathological examination, colonic diverticular perforation by the biliary stent was confirmed (Fig. 4). The patient was discharged without any additional complications. The patient has provided informed consent for publication of the case. The study was approved by the Institutional Review Board of the Inje University Seoul Paik Hospital (IRB No. PAIK 2021-06-012-001).
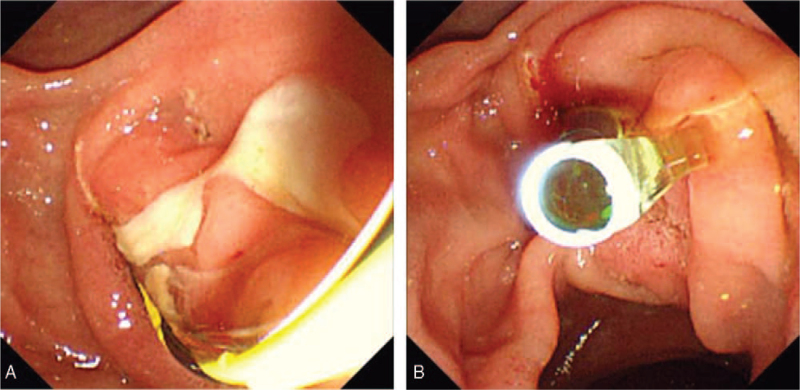
Figure 1.
(A) Large amount of pus drained through the papilla. (B) After removal of the common bile duct (CBD) stone, a straight type plastic biliary stent inserted into the CBD to control acute suppurative cholangitis.
Figure 2.
On abdominal radiography, the migrated endobiliary stent (arrow) is noted in the right lower quadrant area.
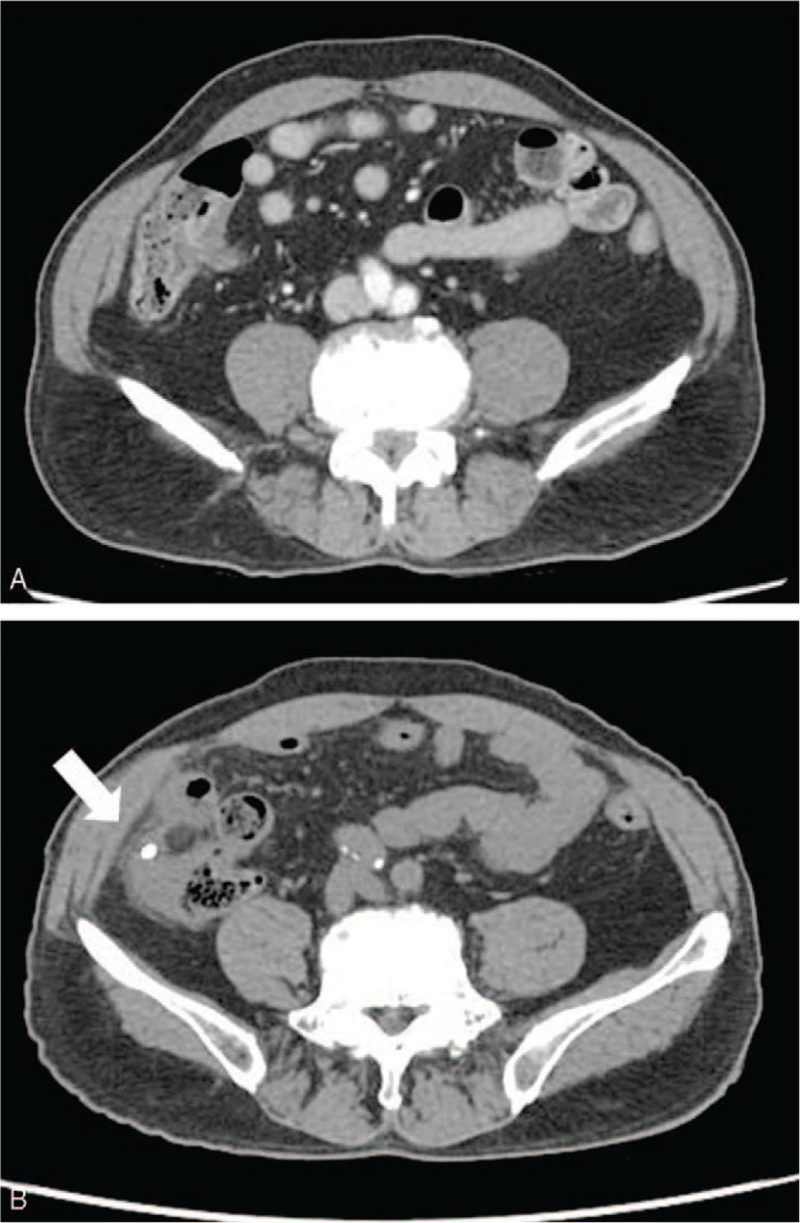
Figure 3.
Abdominal computed tomography (CT) shows perforation of the proximal ascending colon with localized peritonitis by a migrated biliary stent.
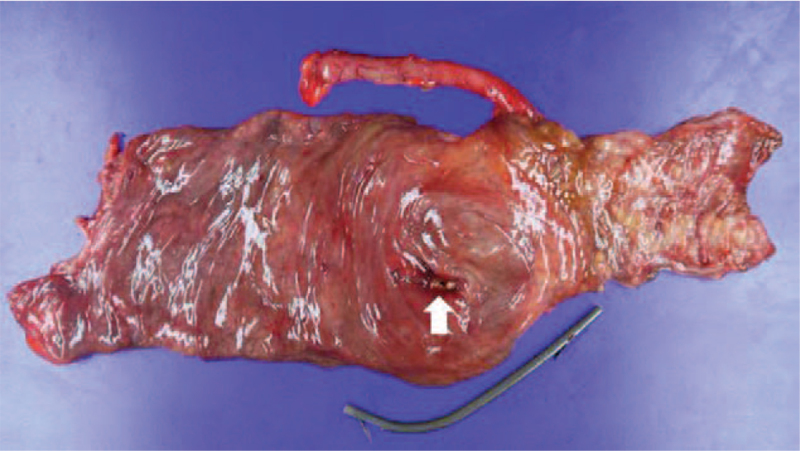
Figure 4.
Pathological examination confirms diverticular perforation (arrow) in the proximal ascending colon associated with the endobiliary stent.
3. Discussion
Biliary stent migration can occur in 5% to 10% of patients with endoscopic biliary stenting.[1] The risk factor for biliary stent migration from the CBD to the distal bowel has not yet been established. In a retrospective cohort study, biliary plastic stent migration occurred more frequently in benign biliary strictures than in malignant biliary strictures.[2] Distal migration was associated with long stents, and proximal and postcholecystectomy strictures, whereas proximal migration was associated with short stents, and distal and non-postcholecystectomy strictures.
Migrated plastic biliary stents in the large intestine, which have passed through the narrow diameter of the small intestine, rarely cause symptoms. Colon perforations due to migrated plastic biliary stents are very rare. The sigmoid colon was the most commonly involved segment.[5] Bowel perforation by a dislocated endobiliary stent was associated with structural bowel abnormalities or variations, such as postoperative bowel adhesion, diverticulosis, hernia, or stricture.[3]
The detailed clinical features of the colon perforation cases by distal migrated biliary stents are summarized in Table 1. A total of 30 cases of colon perforation, including the current case, were identified. Most cases were associated with colonic diverticulum (20 out of 30 cases), and the most commonly involved colonic segment was the sigmoid colon (25 sigmoid colon, 1 cecum, 1 ascending colon, 1 splenic flexure, 1 rectum, 1 appendix). A total of 22 cases required surgical treatment, and 8 patients recovered by medical treatment without surgery.
Table 1.
Clinical features of colon perforation by migrated plastic biliary stent.
| Study | Age/sex | Risk factor | Indication for ERCP | Type of biliary stent | Time to migration | Location of perforation | Treatment |
| D’Costa 1994[8] | M/73 | N/A | CBD cancer | N/A | N/A | Sigmoid | Surgery |
| Baty 1996[9] | F/86 | Diverticulosis | Pancreas head cancer with CBD invasion | N/A | N/A | Sigmoid | Sigmoidectomy |
| Schaafsma 1996[10] | F/77 | Diverticulosis | Acute cholangitis with CBD stone | Straight | 6 mo | Sigmoid | Surgery |
| Lenzo 1998[11] | F/82 | Diverticulosis | Acute cholangitis with CBD stone | Straight 10 Fr x 7.5 cm | 4 wks | Sigmoid | Surgical primary closure |
| Størkson 2000[12] | M/86 | N/A | Acute cholangitis with CBD stone | Straight 7 Fr x 5 cm | 2 yrs | Sigmoid | Surgical primary closure |
| Figueiras 2001[13] | M/47 | N/A | Chronic pancreatitis with distal biliary stricture | Straight 10 Fr x 10 cm | 3 mo | Splenic flexure | Removal through colocutaneous fistula |
| Klein 2001[14] | F/70 | Diverticulosis | CBD stone | Straight 7 Fr x 5 cm | 3 yrs | Sigmoid | Surgery |
| Elliott 2003[15] | F/80 | N/A | Acute cholangitis with CBD stone | Straight 10 Fr x 10 cm | 4 mo | Sigmoid | Hartmann procedure |
| Diller 2003[16] | F/58 | Diverticulosis | Post-LT bile duct stricture | Straight 7 Fr x 10 cm | 1 mo | Sigmoid | Sigmoidectomy |
| Welhelm 2003[3] | F/85 | Diverticulosis | CBD stone | Straight | N/A | Sigmoid | Sigmoidectomy |
| Anderson 2007[17] | F/80 | Diverticulosis | CBD stone | Straight | 5 mo | Sigmoid | Endoscopic removal |
| Namdar 2007[7] | F/65 | N/A | Post-cholecystectomy bile leakage | Straight 12 Fr x 10 cm | 3 mo | Rectum | Rectal resection |
| Bagul 2010[18] | F/79 | Diverticulosis | Post-cholecystectomy bile duct stricture | Double pigtail 10 Fr x 9 cm | 1 mo | Sigmoid | Endoscopic removal |
| Jafferbhoy 2011[19] | F/82 | Diverticulosis | Post-cholecystectomy bile leakage | Straight 7 Fr x 7 cm | 3 mo | Sigmoid | Endoscopic removal and clip closure |
| Lankisch 2011[20] | F/65 | N/A | Pancreas head cancer with CBD invasion | Straight 10 Fr x 10 cm | 2 wks | Sigmoid | Surgery |
| Malgras 2011[21] | 73 y/o | Diverticulosis | Pancreas head cancer with CBD invasion | Straight 10 Fr x 5 cm | 15 d | Sigmoid | Hartmann procedure |
| Wagemakers 2011[22] | F/76 | Diverticulosis | CBD stone | N/A | 1 mo | Sigmoid | Sigmoidectomy |
| Alcaide 2012[23] | M/73 | Diverticulosis | CBD stone with benign biliary stricture | Straight 10 Fr x 12 cm | 15 d | Sigmoid | Endoscopic removal and clip closure |
| Jones 2013[24] | M/66 | N/A | Post-op CBD stricture | Straight | 3 mo | Cecum | Endoscopic removal |
| Mady 2015[25] | M∗ | Diverticulosis | Pancreas head cancer with CBD invasion | N/A | 4 wks | Sigmoid | Hartmann procedure |
| Virgilio 2015[5] | Case 1, F∗ Case 2, F∗ | DiverticulosisDiverticulosis | CBD stoneCBD stone | N/AStraight 12 Fr x 12 cm | N/AN/A | SigmoidSigmoid | Hartmann procedureEndoscopic removal |
| Chittleborough 2016[26] | M/73 | Diverticulosis | Acute cholangitis with CBD stone | Straight 10 Fr x 5 cm | 3 mo | Sigmoid | Hartmann procedure |
| Chou 2017[27] | F/85 | N/A | CBD stone | N/A | N/A | Sigmoid | Endoscopic removal and clip closure |
| Siaperas 2017[28] | F/75 | Diverticulosis | Post-op CBD stricture | Straight | 1 mo | Sigmoid | Hartmann procedure with colostomy |
| Riccardi 2019[29] | F/79 | Diverticulosis | CBD stone | Straight 10 Fr x 10 cm, Double pigtail 7 Fr | 4 wks | Sigmoid | Hartmann procedure with colostomy |
| Marcos 2020[6] | F/65 | Diverticulosis | CBD stone | Straight 10 Fr x 5 cm | 1 yr | Sigmoid | Surgical primary closure |
| Pengermä 2021[30] | F/66 | N/A | Chronic pancreatitis with distal biliary stricture | Straight, 10 Fr x 5 cm | 4 d | Appendix | Appendectomy |
| Tao 2021[31] | M/54 | N/A | Acute cholangitis with CBD stone, biliary pancreatitis | Straight | 3 mo | Sigmoid | Sigmoidectomy+colostomy |
| Current case | M/74 | Diverticulosis | Acute suppurative cholangitis with CBD stone | Straight, 10 Fr x 7 cm | 1 mo | Proximal ascending | Rt. hemicolectomy |
In conclusion, we report a case of perforation of the proximal ascending colon caused by a migrated biliary stent. ERCP endoscopists must always be cautious of the possibility of stent migration in patients with biliary stents in situ. In cases of biliary stent dislocation from the CBD in asymptomatic patients, follow-up with serial, plain abdominal radiographs and physical examination is needed until confirmation of spontaneous passage through stool. In symptomatic cases suggesting peritonitis, abdominal CT scan confirmation is needed, and early intervention should be considered.
Author contributions
Conceptualization: Tae Young Park.
Data curation: Tae Young Park, Sung Woo Hong, Hyoung-Chul Oh.
Methodology: Sung Woo Hong, Hyoung-Chul Oh.
Supervision: Sung Woo Hong, Jae Hyuk Do.
Validation: Hyoung-Chul Oh.
Writing – original draft: Tae Young Park.
Writing – review & editing: Tae Young Park, Jae Hyuk Do.
Footnotes
Abbreviations: CBD = common bile duct, CT = computed tomography, ERCP = endoscopic retrograde cholangiopancreatography, RLQ = right lower quadrant.
How to cite this article: Park TY, Hong SW, Oh HC, Do JH. Colonic diverticular perforation by a migrated biliary stent: a case report with literature review. Medicine. 2021;100:52(e28392).
This research was supported by the Chung-Ang University Research Grants in 2021 (Tae Young Park).
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
CBD = common bile duct, ERCP = endoscopic retrograde cholangiopancreatography, F = female, LT = liver transplantation, M = male, N/A = not available.
Age, not available.
References
- [1].Johanson JF, Schmalz MJ, Geenen JE. Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest Endosc 1992;38:341–6. [DOI] [PubMed] [Google Scholar]
- [2].Arhan M, Odemiş B, Parlak E, et al. Migration of biliary plastic stents: experience of a tertiary center. Surg Endosc 2009;23:769–75. [DOI] [PubMed] [Google Scholar]
- [3].Wilhelm A, Langer C, Zoeller G, et al. Complex colovesicular fistula: a severe complication caused by biliary stent migration. Gastrointest Endosc 2003;57:124–6. [DOI] [PubMed] [Google Scholar]
- [4].Yaprak M, Mesci A, Colak T, et al. Biliary stent migration with duodenal perforation. Eurasian J Med 2008;40:154–6. [PMC free article] [PubMed] [Google Scholar]
- [5].Virgilio E, Pascarella G, Scandavini CM, et al. Colonic perforations caused by migrated plastic biliary stents. Korean J Radiol 2015;16:444–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Marcos P, Capelão G, Atalaia-Martins C, et al. Sigmoid perforation by a migrated plastic biliary stent. GE - Port J Gastroenterol 2020;27:215–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Namdar T, Raffel A-M, Topp S-A, et al. Complications and treatment of migrated biliary endoprostheses: a review of the literature. World J Gastroenterol 2007;13:5397–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].D’Costa H, Toy E, Dennis MJ, et al. Case report: intestinal perforation--an unusual complication of endoscopic biliary stenting. Br J Radiol 1994;67:1270–1. [DOI] [PubMed] [Google Scholar]
- [9].Baty V, Denis B, Bigard MA, et al. Sigmoid diverticular perforation relating to the migration of a polyethylene endoprosthesis. Endoscopy 1996;28:781. [DOI] [PubMed] [Google Scholar]
- [10].Schaafsma RJ, Spoelstra P, Pakan J, et al. Sigmoid perforation: a rare complication of a migrated biliary endoprosthesis. Endoscopy 1996;28:469–70. [DOI] [PubMed] [Google Scholar]
- [11].Lenzo NP, Garas G. Biliary stent migration with colonic diverticular perforation. Gastrointest Endosc 1998;47:543–4. [DOI] [PubMed] [Google Scholar]
- [12].Størkson RH, Edwin B, Reiertsen O, et al. Gut perforation caused by biliary endoprosthesis. Endoscopy 2000;32:87–9. [DOI] [PubMed] [Google Scholar]
- [13].Figueiras RG, Echart MO, Figueiras AG, et al. Colocutaneous fistula relating to the migration of a biliary stent. Eur J Gastroenterol Hepatol 2001;13:1251–3. [DOI] [PubMed] [Google Scholar]
- [14].Klein U, Weiss F, Wittkugel O. Migration of a biliary Tannenbaum stent with perforation of sigmoid diverticulum. ROFO 2001;173:1057. [DOI] [PubMed] [Google Scholar]
- [15].Elliott M, Boland S. Sigmoid colon perforation following a migrated biliary stent. ANZ J Surg 2003;73:669–70. [DOI] [PubMed] [Google Scholar]
- [16].Diller R, Senninger N, Kautz G, et al. Stent migration necessitating surgical intervention. Surg Endosc 2003;17:1803–7. [DOI] [PubMed] [Google Scholar]
- [17].Anderson EM, Phillips-Hughes J, Chapman R. Sigmoid colonic perforation and pelvic abscess complicating biliary stent migration. Abdom Imaging 2007;32:317–9. [DOI] [PubMed] [Google Scholar]
- [18].Bagul A, Pollard C, Dennison AR. A review of problems following insertion of biliary stents illustrated by an unusual complication. Ann R Coll Surg Engl 2010;92:W27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jafferbhoy SF, Scriven P, Bannister J, et al. Endoscopic management of migrated biliary stent causing sigmoid perforation. BMJ Case Rep 2011;2011: doi: 10.1136/bcr.04.2011.4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Lankisch TO, Alten TA, Lehner F, et al. Biliary stent migration with colonic perforation: a very rare complication and the lesson that should be learned from it. Gastrointest Endosc 2011;74:924–5. discussion 925. [DOI] [PubMed] [Google Scholar]
- [21].Malgras B, Pierret C, Tourtier JP, et al. Double sigmoid colon perforation due to migration of a biliary stent. J Visc Surg 2011;148:e397–9. [DOI] [PubMed] [Google Scholar]
- [22].Wagemakers S, Ibelings M. Colovesicular fistula after migration of a biliary stent. Ned Tijdschr Geneeskd 2011;155:A3615. [PubMed] [Google Scholar]
- [23].Alcaide N, Lorenzo-Pelayo S, Herranz-Bachiller MT, et al. Sigmoid perforation caused by a migrated biliary stent and closed with clips. Endoscopy 2012;44: (Suppl 2 UCTN): E274. [DOI] [PubMed] [Google Scholar]
- [24].Jones M, George B, Jameson J, et al. Biliary stent migration causing perforation of the caecum and chronic abdominal pain. BMJ Case Rep 2013;2013:01–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Mady RF, Niaz OS, Assal MM. Migrated biliary stent causing perforation of sigmoid colon and pelvic abscess. BMJ Case Rep 2015;2015:01–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chittleborough TJ, Mgaieth S, Kirkby B, et al. Remove the migrated stent: sigmoid colon perforation from migrated biliary stent. ANZ J Surg 2016;86:947–8. [DOI] [PubMed] [Google Scholar]
- [27].Chou ND, Burbridge RA, Jowell PS. Colonic perforation secondary to retained biliary stent. Am J Gastroenterol 2017;112:13. [DOI] [PubMed] [Google Scholar]
- [28].Siaperas P, Ioannidis A, Skarpas A, et al. A rare cause for Hartmann's procedure due to biliary stent migration: a case report. Int J Surg Case Rep 2017;31:83–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Riccardi M, Deters K, Jabbar F. Sigmoid diverticulitis and perforation secondary to biliary stent migration. Case Rep Surg 2019;2019:2549170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pengermä P, Katunin J, Turunen A, et al. Appendiceal perforation due to biliary stent migration in a neutropenic patient with lung cancer receiving chemotherapy: a case report. Mol Clin Oncol 2021;15:136–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Tao Y, Long J. Sigmoid colon perforation caused by migrated plastic biliary stents: a case report. Int J Colorectal Dis 2021;36:199–201. [DOI] [PubMed] [Google Scholar]