Abstract
Purpose
In this study, we aimed to evaluate the clinical validity of the modified tunneling technique using minimal soft tissue harvesting and volume-stable collagen matrix in the anterior mandible.
Methods
In total, 27 anterior mandibular teeth and palatal donor sites in 17 patients with ≥1 mm of gingival recession (GR) were analyzed before and after root coverage. For the recipient sites, vertical vestibular incisions were made in the interdental area and a subperiosteal tunnel was created with an elevator. After both sides of the marginal gingiva were tied to one another, a prepared connective tissue graft and volume-stable collagen matrix were inserted through the vestibular vertical incision and were fixed with resorbable suture material. The root coverage results of the recipient site were measured at baseline (T0), 3 weeks (T3), 12 weeks (T12), and the latest visit (Tl). For palatal donor sites, a free gingival graft from a pre-decided area avoiding the main trunk of the greater palatine artery was harvested using a prefabricated surgical template at a depth of 2 mm after de-epithelization using a rotating bur. In each patient, the clinical and volumetric changes at the donor sites between T0 and T3 were measured.
Results
During an average follow-up of 14.5 months, teeth with denuded root lengths of 1–3 mm (n=12), 3–6 mm (n=11), and >6 mm (n=2) achieved root coverage of 97.01%±7.65%, 86.70%±5.66%, and 82.53%±1.39%, respectively. Miller classification I (n=12), II (n=10), and III (n=3) teeth showed mean coverage rates of 97.01%±7.65%, 86.91%±5.90%, and 83.19%±1.62%, respectively. At the donor sites, an average defect depth of 1.41 mm (70.5%) recovered in 3 weeks, and the wounds were epithelized completely in all cases.
Conclusions
The modified tunneling technique in this study is a promising treatment modality for overcoming GR in the anterior mandible.
Keywords: Gingival recession, Connective tissue, Gingivoplasty
Graphical Abstract
INTRODUCTION
The coronally advanced flap (CAF) with a subepithelial connective tissue graft (SCTG) is considered a gold-standard procedure because of its high success rate, harmonious color matching with the surrounding tissue, and phenotypical thickening [1,2,3]. However, in the mandible, the thin anterior gingiva makes it difficult to perform partial-thickness flap operations [4,5], and the shallow vestibular depth or frenulum often acts as an opposing force for the CAF, which compromises the results of the CAF procedure by exposing the graft and increasing the risk of graft necrosis [6,7].
To compensate for the disadvantages of the CAF procedure in root coverage, various methods and modifications of the pedicle flap have been devised to minimize coronal movement of the mucogingival junction and operative complications without releasing incisions; examples include the lateral repositioned flap [8], double papilla flap [9,10], and tunneling technique [11,12]. The tunneling technique is a procedure without coronal displacement of the mucogingival junction, as described by Raetzke [11]. With the tunneling technique [12,13], minimal damage to the blood supply and diminished risk of scar tissue formation was possible without a releasing incision or papilla dissection [14]. Furthermore, a double-papilla repositioned flap could be used when the interdental papillae on both sides of the exposed root surface were intact without any destruction. Minimal damage of the underlying periosteum on the adjacent papillae and reduction of the tension on the recipient site could be a major advantage of using the double-papilla repositioned flap, without increasing the shallowness of the vestibule or displacing the mucogingival junction [9,10].
At the donor site, various techniques are used to obtain the SCTG from the palate, including the trap-door, de-epithelization with laser or rotary/hand instruments, and single-incision techniques [11,15,16]. The single-incision technique was introduced as the least invasive of these techniques because it ensures healing by primary intention and reduces pain/discomfort [16,17]. However, sloughing of the overlaying flap [18], reduced visibility, and decreased predictability of graft size are disadvantages of the single-incision technique [19]. At the same time, the greater palatine artery limits the size of the palatal donor area, reducing the visible denuded area and graft tissue area ratio, which is a significant factor associated with optimal root coverage results [20].
This study aimed to evaluate the clinical validity of the modified tunnel technique using minimal soft tissue harvesting and volume-stable collagen matrix in the anterior mandible.
MATERIALS AND METHODS
Study population
This retrospective study included patients who visited the Department of Periodontology of Seoul National University Dental Hospital from August 2018 to August 2019 to receive root coverage treatment of anterior mandibular teeth. In total, 27 anterior mandibular teeth in 17 healthy patients aged 21–39 years (mean age: 29.65 years) with gingival recession (GR) of ≥1 mm and a periodontal probing depth of ≤3 mm with Miller class I–III recession were included in the recipient site study. Patients with active periodontal disease or an ambiguous cementoenamel junction, dental caries, restorations, and systemic disease were excluded, as were those taking any medication that could potentially affect periodontal wound healing. Table 1 presents the distribution of the recipient site study population and the details of the target teeth. This retrospective study was exempted from Institutional Review Board (IRB) approval by the Seoul National University Dental Hospital Research Ethics Committee (IRB254/04-20).
Table 1. Study population and results of root coverage using the modified tunneling technique at T12 and Tl.
| Patient# | Age | Sex | Tooth | Miller class | Denuded root length T0 (mm) | Root coverage T12 (mm) | Root coverage Tl (mm) | Follow-up period at Tl (mon) |
|---|---|---|---|---|---|---|---|---|
| 1 | 24 | Female | #41 | II | 3.35 | 2.43 (72.56) | 2.90 (86.57) | 10 |
| 2 | 39 | Female | #41a) | I | 3.08 | 1.91 (61.98) | 2.17 (70.45) | 16 |
| #31 | I | 1.52 | 1.52 (100.0) | 1.52 (100.0) | ||||
| #32 | I | 0.93 | 0.93 (100.0) | 0.93 (100.0) | ||||
| 3 | 23 | Male | #31 | II | 4.92 | 4.08 (82.84) | 4.08 (82.93) | 13 |
| #32 | I | 2.22 | 1.94 (87.35) | 1.62 (72.97) | ||||
| #41 | I | 2.83 | 2.49 (88.05) | 2.83 (100.0) | ||||
| #42 | I | 1.41 | 1.41 (100.0) | 1.41 (100.0) | ||||
| 4 | 31 | Female | #31 | I | 2.49 | 2.49 (100.0) | 2.49 (100.0) | 12 |
| 5 | 29 | Male | #31a) | I | 3.36 | 1.67 (49.63) | 1.75 (52.14) | 10 |
| 6 | 38 | Female | #31 | II | 4.5 | 3.68 (81.70) | 3.81 (84.67) | 17 |
| #41 | I | 1.59 | 1.59 (100.0) | 1.59 (100.0) | ||||
| 7 | 31 | Female | #31 | II | 4.41 | 3.57 (80.96) | 3.46 (78.46) | 15 |
| 8 | 25 | Female | #31 | I | 2.82 | 2.42 (85.73) | 2.57 (91.13) | 16 |
| 9 | 26 | Female | #31 | I | 2.41 | 2.41 (100.0) | 2.41 (100.0) | 21 |
| #41 | I | 1.73 | 1.73 (100.0) | 1.73 (100.0) | ||||
| 10 | 33 | Female | #31 | II | 6.47 | 5.43 (83.94) | 5.43 (83.94) | 10 |
| 11 | 36 | Female | #31 | III | 3.69 | 2.92 (79.17) | 2.99 (81.03) | 19 |
| 12 | 24 | Male | #41 | II | 7.37 | 5.98 (81.12) | 5.98 (81.12) | 8 |
| 13 | 30 | Female | #31 | II | 3.9 | 3.49 (89.51) | 3.55 (91.03) | 8 |
| #32 | I | 1.8 | 1.80 (100.0) | 1.80 (100.0) | ||||
| #41 | I | 2.37 | 2.37 (100.0) | 2.37 (100.0) | ||||
| 14 | 31 | Female | #31 | III | 4.58 | 3.16 (68.85) | 3.89 (84.93) | 20 |
| #41 | III | 3.48 | 2.62 (75.23) | 2.91 (83.62) | ||||
| 15 | 32 | Female | #31 | II | 5.59 | 5.59 (100.0) | 5.11 (91.41) | 18 |
| 16 | 21 | Female | #31 | II | 4.27 | 3.48 (81.53) | 3.80 (88.99) | 22 |
| 17 | 31 | Female | #31 | II | 4.34 | 4.34 (100.0) | 4.34 (100.0) | 12 |
| Mean | 29.65 | 3.39±1.55 | 2.87±1.30 (87.04±13.31) | 2.94±1.27 (89.09±11.67) | 14.5 |
Data are shown as mean±standard deviation or number (%).
a)Tooth with non-caries cervical lesion.
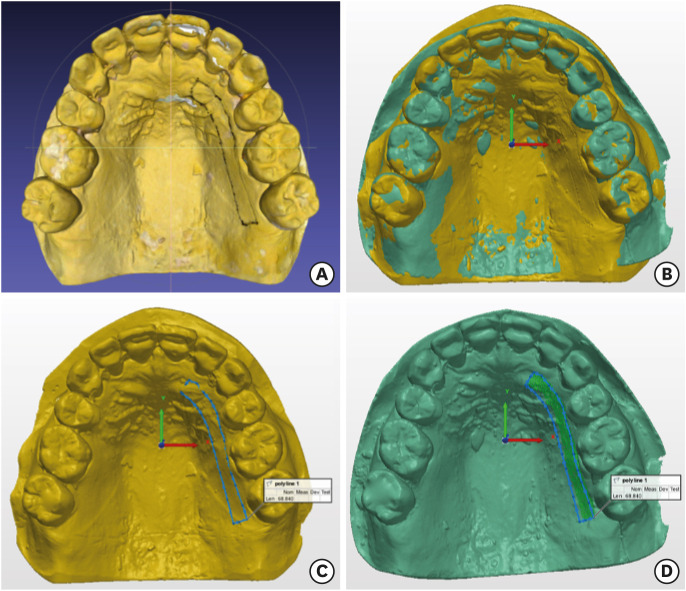
Study design
For each patient, clinical photographs and impressions for the mandible and maxilla using hydrocolloid material (Alginate GC Aroma Fine Plus, GC Co., Tokyo, Japan) were taken at baseline (T0), 3 weeks (T3), 12 weeks (T12), and the latest visit (Tl). The denuded root length was defined as the distance from the cementoenamel junction to the marginal gingiva and was derived from clinical photographs at T0, T12, and Tl using the proportional ratio between the denuded root length and the incisal edge of tooth #31, which was measured with digital calipers (Mitutoyo Co., Kanagawa, Japan) on the T0 casts. For the palatal donor sites, the volumetric change at the donor sites from the T0 to T3 casts was measured using an optical scanner (Medit, Seoul, Korea) and computer-aided design software (Dental CAD, EGS, Bologna, Italy). The region of interest (ROI) was set along the border of established donor area on the casts (Figure 1A). Three-dimensional images of the T0 and T3 casts obtained with optical scanning were superimposed using 3D measurement software (Polyworks, Innovmetric, Quebec, Canada) (Figure 1B). A polyline drawn along the ROI at T0 was projected to an arbitrary average surface vector, and volumes from the projected polyline to the scanned surface at T0 and T3 were calculated (Figure 1C). The volumetric change was divided by the area of the projection and quantified as the displacement between the surfaces (Figure 1D). The present manuscript follows the STROBE statement for improving the quality of reports of cross-sectional studies (http://www.strobe-statement.org/).
Figure 1. Demonstration of the 3-dimensional volumetric analysis of the donor site before and 3 weeks after surgery. (A) The ROI was set along the border of the established donor area on the casts. (B) Three-dimensional images of T0 and T3 casts obtained by optical scanning were superimposed. (C) A polyline was drawn along the ROI of T0. (D) To derive the volumetric change, the volume from the projected polyline to the scanned surface of the T3 cast was calculated.
ROI: region of interest.
Statistical analysis of the recipient and donor sites
The root coverage results of the recipient site (between T0, T12, and Tl) and donor site (between T0 and T3) were analyzed using the paired t-test in SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
Presurgical procedure
All the patients were instructed to maintain proper oral hygiene. Scaling and root planing were performed 1 month before the day scheduled for surgery, and patients with a plaque index <20% underwent the root coverage procedure.
Surgical procedures
Recipient site preparation
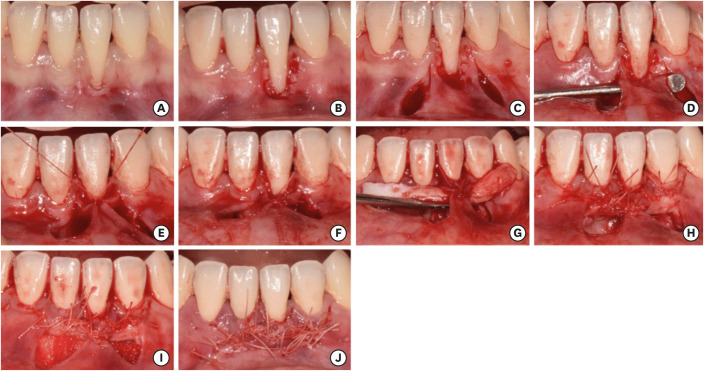
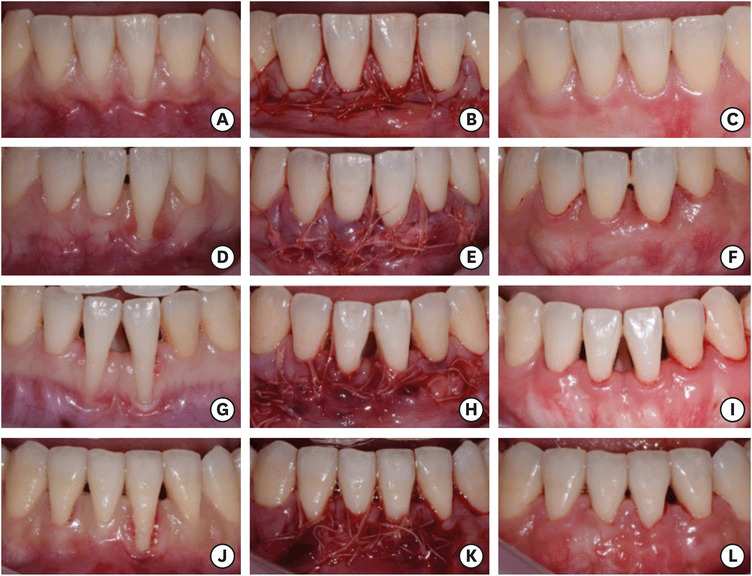
After the surgical field was anesthetized using 2% lidocaine and 1:100,000 epinephrine (Huons, Seongnam, Korea), thorough debridement of teeth, flattening of the root eminence, and de-epithelization of the gingival margin were performed (Figure 2B). Vertical vestibular incisions were made through the periosteum in the interdental area beyond the teeth that required root coverage, from the vestibular depth apically to beneath the papillae that remained intact (Figure 2C). A subperiosteal tunnel was created with a specifically designed elevator (CM9, Osung, Gimpo, Korea) exposing the facial bone (Figure 2D). The tunnel was extended to just below the papilla coronally and beyond the mucogingival junction apically so that the marginal gingiva of the teeth to be treated was mobilized and allowed coronal repositioning with low tension.
Figure 2. Clinical photographs of the modified tunneling technique procedure. (A) Preoperative appearance. (B) De-epithelization of the marginal gingiva. (C) Vestibular vertical incision. (D) Tunneling procedure. (E, F) Suturing of the papilla pedicle flap. (G) Application of the SCTG. (H) Fixation of the SCTG with 5-0 resorbable suture material. (I) Application of the auxiliary collagen matrix. (J) Suturing of the vestibular incision.
SCTG: subepithelial connective tissue graft.
The mobilized mesial and distal sides of the marginal gingiva were tied to one another (Figure 2E and F). The prepared connective tissue graft was inserted through the vestibular vertical incision and placed on the coronal part of the tunnel (Figure 2G), stabilized using interrupted sutures with 5-0 irradiated polyglactin 910 (Vicryl Rapide, Ethicon, Cincinnati, OH, USA) along the vertical incisions (Figure 2H). Volume-stable collagen matrix (Collagen Graft, GENOSS, Suwon, Korea) was inserted through the vestibular incision and placed apical part of the tunnel beneath the connective tissue graft (Figure 2I). The vertical vestibular incisions were sutured with 5-0 irradiated polyglactin 910 suture material (Ethilon, Ethicon) (Figure 2J).
Donor site preparation
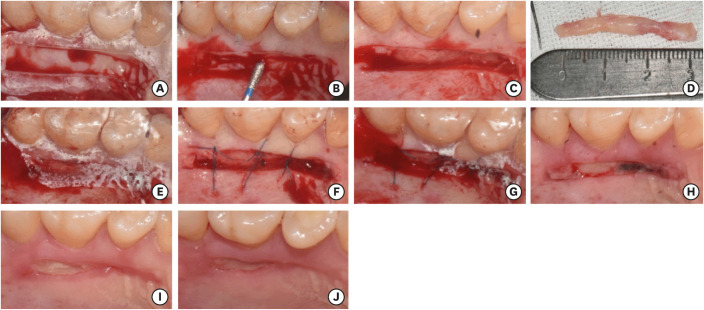
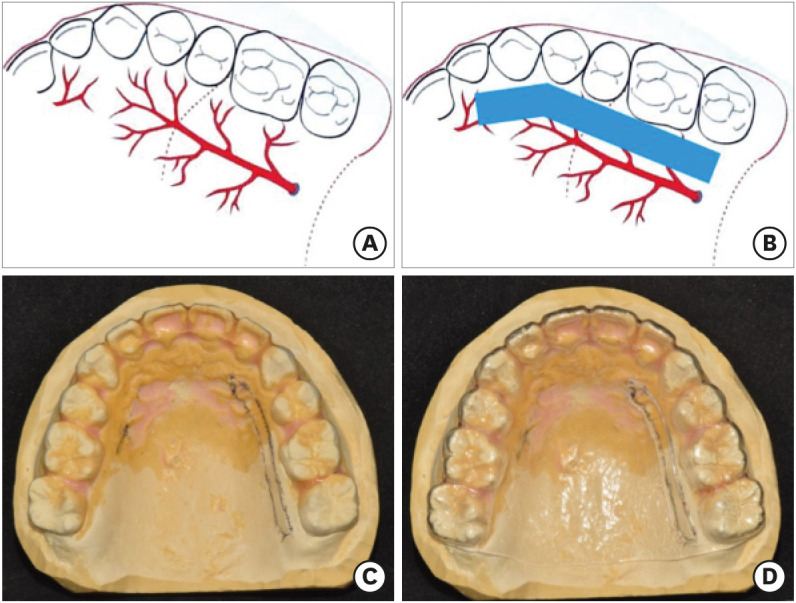
Before entering the surgical phase, the required width and length of connective tissue graft were calculated with a periodontal probe in the T0 casts, and the appropriate palatal donor site area was decided via intraoral palpation of the palate to avoid the main trunk of the greater palatine artery, as depicted in Figure 3A and B. Once the harvest area was established and marked on the T0 casts (Figure 3C), the protecting device and surgical template were fabricated using a vacuum former (Biostar, SCHEU, Iserlohn, Germany) (Figure 3D).
Figure 3. (A) Location of the greater palatine artery. (B) Harvest area, established to avoid the main trunk of the greater palatine artery. Establishment of the donor site on the T0 cast (C) and surgical template (D).
The surgical field was anesthetized with 2% lidocaine and 1:100,000 epinephrine (Huons). Applying a prefabricated surgical template, an incision was made using a #15c blade at a depth of 2 mm along the marked area on the surgical template (Figure 4A). De-epithelization was performed with a diamond point (EX-21, Mani, Tochigi, Japan) (Figure 4B), and a de-epithelized SCTG was obtained (Figure 4C). While adipose tissue was being trimmed from the graft, a prefabricated protecting device was applied to the patient for hemostasis (Figure 4D and E). Simple interrupted suturing was performed at the end of surgery after confirming hemostasis in the donor area (Figure 4F).
Figure 4. Clinical photographs of the harvest of the free gingival graft at the palatal donor site. (A) The palatal donor site area was reproduced in the oral cavity using a surgical template. (B) De-epithelization was accomplished with a rotating diamond point bur. (C) The free gingival graft was harvested with a 2-mm-deep incision. (D) Adipose tissue was trimmed. (E) A prefabricated hemostatic device was applied until work on the recipient site was finished. (F) Simple interrupted sutures were used to close the incision. (G) The prefabricated hemostatic device was left in place until the 1-week recall check. (H) Appearance 1 week after surgery. (I) Appearance 2 weeks after surgery. (J) Appearance 3 weeks after surgery.
Postsurgical procedures
Antibiotics (amoxicillin [500 mg] orally 3 times daily), analgesics (aceclofenac [250 mg] orally 2 times daily), and 0.1% chlorhexidine gluconate (rinse twice a day) were prescribed, and patients were instructed not to exert external forces on the surgical area with actions such as pulling their lips or toothbrushing for 3 weeks. At 21 days postoperatively, the sutures were removed, and no adverse events were noted.
RESULTS
Root coverage results of the recipient site
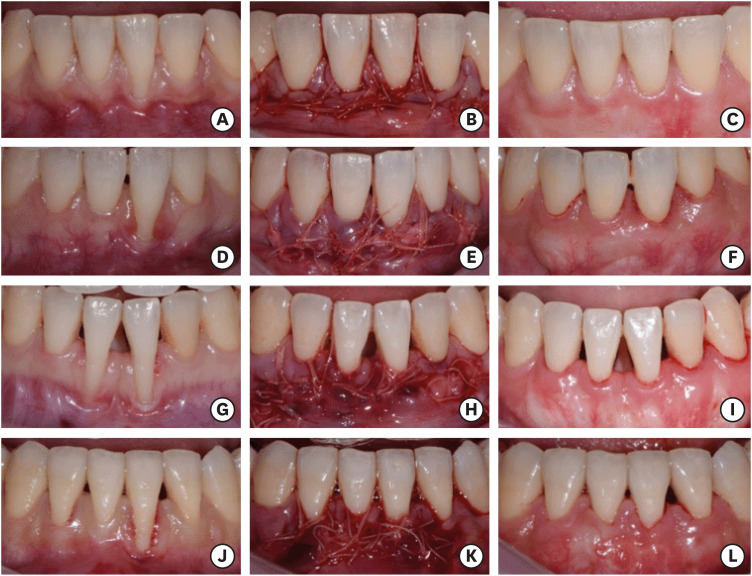
Of the 27 survey target teeth, 2 teeth were classified as having non-caries cervical lesions (NCCLs), and 12, 10, and 3 teeth were classified as having Miller class I, II, and III recession, respectively. The average follow-up period at the latest visit (Tl) was 14.5 months (Table 1). The average length of the denuded root was 3.39±1.55 mm at T0. The average root coverage was 2.87±1.30 mm (87.61%±13.31%) at T12, and 2.94±1.27 mm (89.09%±11.67%) at Tl (Table 1).
On average, the 12 teeth with a denuded root length of 1–3 mm had 97.01%±7.65% root coverage, the 11 teeth with a denuded root length of 3–6 mm had 86.70%±5.66% root coverage, and the 2 teeth with a denuded root length of >6 mm had 82.53%±1.39% root coverage (Table 2). In the 12 teeth with Miller class I recession, 97.01%±7.65% root coverage was achieved, while the 10 teeth with Miller class II recession showed 86.69%±5.90% root coverage and the 3 teeth with Miller class III recession demonstrated 83.19%±1.62% root coverage (Table 3). Ten of the 12 teeth (83.33%) with Miller class I recession and 1 of the 10 teeth (10%) with Miller class II recession showed complete root coverage. Teeth with a 1- to 3-mm denuded root length showed a significantly higher root coverage rate (P<0.05) than did those with a 3- to 6-mm denuded root length, and teeth with Miller class I recession also showed significantly more root coverage than did those with Miller class II recession. The teeth with NCCLs (n=2) showed 61.27%±9.13% root coverage at Tl. Figure 5 demonstrates representative clinical cases.
Table 2. Results of root coverage accomplished with the modified tunneling technique according to denuded root length.
| Denuded root length | 1–3 mm (n=12) | 3–6 mm (n=11) | 6–7 mm (n=2) |
|---|---|---|---|
| Denuded root length at T0 (mm) | 2.01±0.57 | 4.27±0.62 | 6.92±0.45 |
| Root coverage at Tl (mm) | 1.94±0.55 | 3.71±0.63 | 5.71±0.28 |
| Root coverage rate at Tl (%) | 97.01±7.65 | 86.70±5.66a) | 82.53±1.39 |
| Complete root coverage at Tl (%) | 83.33% (10 out of 12) | 18.18% (2 out of 11) | - |
Teeth with non-caries cervical lesions (n=2) were excluded. All data are provided as mean±standard deviation.
a)Statistically significant difference compared to the 1- to 3-mm group (P<0.05) using the independent t-test.
Table 3. Results of root coverage accomplished with the modified tunneling technique according to the Miller classification (I–III).
| Miller classification | I (n=12) | II (n=10) | III (n=3) |
|---|---|---|---|
| Denuded root length at T0 (mm) | 2.18±0.68 | 4.91±1.16 | 3.92±0.48 |
| Root coverage at Tl (mm) | 2.93±0.55 | 4.25±0.92 | 3.26±0.44 |
| Root coverage rate at Tl (%) | 97.01±7.65 | 86.91±5.90a) | 83.19±1.62 |
| Complete root coverage at Tl (%) | 83.33% (10 out of 12) | 10% (1 out of 10) | - |
Teeth with non-caries cervical lesions (n=2) were excluded. All data are provided as mean±standard deviation.
a)Statistically significant difference compared to the Miller classification I group (P<0.05) using the independent t-test.
Figure 5. Representative clinical cases. (A-C) Patient #4 with Miller class I recession of tooth #31. (D-F) Patient #17 with Miller class II recession of tooth #31. (G-I) Patient #14 with multiple Miller class III recession of teeth #31 and #41. (J-L) Patient #11 with Miller class III of tooth #31. (A, D, G, J) Pre-operative appearance. (B, E, H, K) Appearance immediately after surgery. (C, F, I, L) Appearance at Tl.
Creeping attachment was observed in 14 teeth at Tl among 17 teeth that showed incomplete root coverage at T12, and 1 of those teeth achieved complete root coverage by creeping attachment at Tl. The mean creeping attachment of the 14 teeth was 0.21±0.20 mm (5.78%±5.19%).
Volumetric analysis of early healing of donor site
No severe complications at donor sites were noted 1 week after surgery. The mean surface area was 135.79±22.61 mm2, and the mean dimensional change between T0 and T3 was 0.59±0.40 mm in depth, which was statistically significant (P<0.001). This result indicates that approximately 1.41 mm (70.5%) of the donor site volume defect recovered in 3 weeks on average, as the harvesting incision was performed at a depth of 2 mm. Clinically, almost complete epithelization of the wound was noticed in all patients at T3 (Figure 4H-J).
DISCUSSION
CAF with SCTG has been reported to achieve mean root coverage values of 64.5% to 97.3% and complete root coverage of 10%–66% in teeth with Miller class I or II recession (at least 2-mm root recession) [2,21,22,23,24,25,26]. Regarding the tunneling technique with subperiosteal incision, teeth with a denuded root length of 1–3 mm showed 95% mean coverage and those with a denuded root length of 4–6 mm demonstrated 73% mean root coverage [27]. However, few studies have reported the success rate of CAF or the tunneling (envelope) technique with the SCTG procedure in the anterior mandible, especially in teeth with a denuded root length of >3 mm. The tunneling technique is a procedure without coronal displacement of the mucogingival junction, as described by Raetzke [11], but for teeth with a denuded root length above 3 mm, the graft is exposed in the tunneling technique, although exposure of the graft up to 2.8 mm does not hinder the result of root coverage [28,29]. Because of the thin anterior gingiva and shallow vestibule in the anterior mandible, the vestibular incision sub-periosteal tunnel access technique described by Zadeh [30] also has difficulties in coronally repositioning the overlying flap in teeth with a denuded root length above 3 mm. However, the double-papilla pedicle flap for the treatment of denuded tooth roots in the anterior mandible was reported to show better clinical outcomes than the CAF procedure [31].
In a study where the free gingival graft, trap-door, and single-incision techniques were compared in terms of early healing of the palatal donor area, the single-incision group showed complete epithelization in 50% of patients within 2 weeks and in all patients within 3 weeks. In contrast, the free gingival graft group showed complete epithelization in 50% of the patients at 3 weeks and in all patients at 4 weeks, and patients exhibited postoperative discomfort at 1 week postoperatively [19]. In this study, modifications were applied to the graft harvesting procedure in the palatal donor area, such as minimizing the graft size using an auxiliary volume-stable collagen matrix and a well-designed harvesting area that avoided the greater palatine artery. In this study, an average of 1.41 mm (70.5%) of the donor site volume defect recovered, and complete epithelization was noted in all patients at 3 weeks, representing a healing rate that was 1 week faster than that reported for the conventional free gingival graft procedure and similar to that reported for the single-incision technique.
To minimize the graft size, an auxiliary volume-stable collagen matrix was used. The collagen matrix placed beneath the SCTG and apical portion of the denuded root reduced the required size of the graft. Although the collagen matrix appears to be less effective for root coverage than SCTG [32,33,34], it reduces the required size of the graft and plays the roles of biotype modification and gingival thickness improvement, helping to prevent relapse of GR and improving long-term results [35,36,37].
For successful periodontal plastic surgery, patients' subjective discomfort, gingival thickness (to prevent relapse of GR), and multifaceted esthetic criteria [38], such as gingival health, harmonious gingival color, and morphological features that include surface texture and gingival contour should be considered. In a further study of the modified tunneling technique described herein, these aspects need to be evaluated over the long term.
In conclusion, the modified tunneling technique in this study is a promising treatment modality for overcoming GR in the anterior mandible.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI15C1535).
- Conceptualization: Sungtae Kim.
- Formal analysis: Yoonsub Lee.
- Investigation: Yoonsub Lee, Methodology.
- Project administration: Sungtae Kim, Dajung Lee.
- Resources: Sungtae Kim, Dajung Lee.
- Software: Yoonsub Lee, Dajung Lee.
- Writing - original draft: Sungtae Kim, Yoonsub Lee.
- Writing - review & editing: Sungtae Kim, Young Ku, In-Chul Rhyu.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of Miller Class I and II recession-type defects? J Dent. 2008;36:659–671. doi: 10.1016/j.jdent.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 2.da Silva RC, Joly JC, de Lima AFM, Tatakis DN. Root coverage using the coronally positioned flap with or without a subepithelial connective tissue graft. J Periodontol. 2004;75:413–419. doi: 10.1902/jop.2004.75.3.413. [DOI] [PubMed] [Google Scholar]
- 3.Harris RJ. A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J Periodontol. 2004;75:734–743. doi: 10.1902/jop.2004.75.5.734. [DOI] [PubMed] [Google Scholar]
- 4.Goaslind GD, Robertson PB, Mahan CJ, Morrison WW, Olson JV. Thickness of facial gingiva. J Periodontol. 1977;48:768–771. doi: 10.1902/jop.1977.48.12.768. [DOI] [PubMed] [Google Scholar]
- 5.Eger T, Müller HP, Heinecke A. Ultrasonic determination of gingival thickness. Subject variation and influence of tooth type and clinical features. J Clin Periodontol. 1996;23:839–845. doi: 10.1111/j.1600-051x.1996.tb00621.x. [DOI] [PubMed] [Google Scholar]
- 6.Stimmelmayr M, Allen EP, Gernet W, Edelhoff D, Beuer F, Schlee M, et al. Treatment of gingival recession in the anterior mandible using the tunnel technique and a combination epithelialized-subepithelial connective tissue graft-a case series. Int J Periodontics Restorative Dent. 2011;31:165–173. [PubMed] [Google Scholar]
- 7.Pini Prato G, Pagliaro U, Baldi C, Nieri M, Saletta D, Cairo F, et al. Coronally advanced flap procedure for root coverage. Flap with tension versus flap without tension: a randomized controlled clinical study. J Periodontol. 2000;71:188–201. doi: 10.1902/jop.2000.71.2.188. [DOI] [PubMed] [Google Scholar]
- 8.Grupe HE, Warren RF., Jr Repair of gingival defects by a sliding flap operation. J Periodontol. 1956;27:92–95. [Google Scholar]
- 9.Cohen DW, Ross SE. The double papillae repositioned flap in periodontal therapy. J Periodontol. 1968;39:65–70. doi: 10.1902/jop.1968.39.2.65. [DOI] [PubMed] [Google Scholar]
- 10.Blanes RJ, Allen EP. The bilateral pedicle flap-tunnel technique: a new approach to cover connective tissue grafts. Int J Periodontics Restorative Dent. 1999;19:471–479. [PubMed] [Google Scholar]
- 11.Raetzke PB. Covering localized areas of root exposure employing the “envelope” technique. J Periodontol. 1985;56:397–402. doi: 10.1902/jop.1985.56.7.397. [DOI] [PubMed] [Google Scholar]
- 12.Rebele SF, Zuhr O, Schneider D, Jung RE, Hürzeler MB. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part II. Volumetric studies on healing dynamics and gingival dimensions. J Clin Periodontol. 2014;41:593–603. doi: 10.1111/jcpe.12254. [DOI] [PubMed] [Google Scholar]
- 13.Zuhr O, Rebele SF, Schneider D, Jung RE, Hürzeler MB. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part I. Clinical and patient-centred outcomes. J Clin Periodontol. 2014;41:582–592. doi: 10.1111/jcpe.12178. [DOI] [PubMed] [Google Scholar]
- 14.Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M. Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: a comparative controlled randomized clinical trial. J Periodontol. 2009;80:1083–1094. doi: 10.1902/jop.2009.090041. [DOI] [PubMed] [Google Scholar]
- 15.Edel A. Clinical evaluation of free connective tissue grafts used to increase the width of keratinised gingiva. J Clin Periodontol. 1974;1:185–196. doi: 10.1111/j.1600-051x.1974.tb01257.x. [DOI] [PubMed] [Google Scholar]
- 16.Hürzeler MB, Weng D. A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent. 1999;19:279–287. [PubMed] [Google Scholar]
- 17.Lorenzana ER, Allen EP. The single-incision palatal harvest technique: a strategy for esthetics and patient comfort. Int J Periodontics Restorative Dent. 2000;20:297–305. [PubMed] [Google Scholar]
- 18.Farnoush A. Techniques for the protection and coverage of the donor sites in free soft tissue grafts. J Periodontol. 1978;49:403–405. doi: 10.1902/jop.1978.49.8.403. [DOI] [PubMed] [Google Scholar]
- 19.Del Pizzo M, Modica F, Bethaz N, Priotto P, Romagnoli R. The connective tissue graft: a comparative clinical evaluation of wound healing at the palatal donor site. A preliminary study. J Clin Periodontol. 2002;29:848–854. doi: 10.1034/j.1600-051x.2002.290910.x. [DOI] [PubMed] [Google Scholar]
- 20.Yotnuengnit P, Promsudthi A, Teparat T, Laohapand P, Yuwaprecha W. Relative connective tissue graft size affects root coverage treatment outcome in the envelope procedure. J Periodontol. 2004;75:886–892. doi: 10.1902/jop.2004.75.6.886. [DOI] [PubMed] [Google Scholar]
- 21.Borghetti A, Glise JM, Monnet-Corti V, Dejou J. Comparative clinical study of a bioabsorbable membrane and subepithelial connective tissue graft in the treatment of human gingival recession. J Periodontol. 1999;70:123–130. doi: 10.1902/jop.1999.70.2.123. [DOI] [PubMed] [Google Scholar]
- 22.Cheung WS, Griffin TJ. A comparative study of root coverage with connective tissue and platelet concentrate grafts: 8-month results. J Periodontol. 2004;75:1678–1687. doi: 10.1902/jop.2004.75.12.1678. [DOI] [PubMed] [Google Scholar]
- 23.McGuire MK, Nunn M. Evaluation of human recession defects treated with coronally advanced flaps and either enamel matrix derivative or connective tissue. Part 1: comparison of clinical parameters. J Periodontol. 2003;74:1110–1125. doi: 10.1902/jop.2003.74.8.1110. [DOI] [PubMed] [Google Scholar]
- 24.Paolantonio M, Dolci M, Esposito P, D'Archivio D, Lisanti L, Di Luccio A, et al. Subpedicle acellular dermal matrix graft and autogenous connective tissue graft in the treatment of gingival recessions: a comparative 1-year clinical study. J Periodontol. 2002;73:1299–1307. doi: 10.1902/jop.2002.73.11.1299. [DOI] [PubMed] [Google Scholar]
- 25.Wang HL, Bunyaratavej P, Labadie M, Shyr Y, MacNeil RL. Comparison of 2 clinical techniques for treatment of gingival recession. J Periodontol. 2001;72:1301–1311. doi: 10.1902/jop.2001.72.10.1301. [DOI] [PubMed] [Google Scholar]
- 26.Zucchelli G, Amore C, Sforza NM, Montebugnoli L, De Sanctis M. Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J Clin Periodontol. 2003;30:862–870. doi: 10.1034/j.1600-051x.2003.00397.x. [DOI] [PubMed] [Google Scholar]
- 27.Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994;14:216–227. [PubMed] [Google Scholar]
- 28.Moisa DH, Connolly JA, Cheng B, Lalla E. Impact of connective tissue graft thickness on surgical outcomes: a pilot randomized clinical trial. J Periodontol. 2019;90:966–972. doi: 10.1002/JPER.18-0741. [DOI] [PubMed] [Google Scholar]
- 29.Cordioli G, Mortarino C, Chierico A, Grusovin MG, Majzoub Z. Comparison of 2 techniques of subepithelial connective tissue graft in the treatment of gingival recessions. J Periodontol. 2001;72:1470–1476. doi: 10.1902/jop.2001.72.11.1470. [DOI] [PubMed] [Google Scholar]
- 30.Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31:653–660. [PubMed] [Google Scholar]
- 31.Harris RJ, Miller LH, Harris CR, Miller RJ. A comparison of three techniques to obtain root coverage on mandibular incisors. J Periodontol. 2005;76:1758–1767. doi: 10.1902/jop.2005.76.10.1758. [DOI] [PubMed] [Google Scholar]
- 32.Schmitt CM, Matta RE, Moest T, Humann J, Gammel L, Neukam FW, et al. Soft tissue volume alterations after connective tissue grafting at teeth: the subepithelial autologous connective tissue graft versus a porcine collagen matrix - a pre-clinical volumetric analysis. J Clin Periodontol. 2016;43:609–617. doi: 10.1111/jcpe.12547. [DOI] [PubMed] [Google Scholar]
- 33.Zeltner M, Jung RE, Hämmerle CH, Hüsler J, Thoma DS. Randomized controlled clinical study comparing a volume-stable collagen matrix to autogenous connective tissue grafts for soft tissue augmentation at implant sites: linear volumetric soft tissue changes up to 3 months. J Clin Periodontol. 2017;44:446–453. doi: 10.1111/jcpe.12697. [DOI] [PubMed] [Google Scholar]
- 34.Tonetti MS, Cortellini P, Pellegrini G, Nieri M, Bonaccini D, Allegri M, et al. Xenogenic collagen matrix or autologous connective tissue graft as adjunct to coronally advanced flaps for coverage of multiple adjacent gingival recession: Randomized trial assessing non-inferiority in root coverage and superiority in oral health-related quality of life. J Clin Periodontol. 2018;45:78–88. doi: 10.1111/jcpe.12834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Song YW, Kim S, Waller T, Cha JK, Cho SW, Jung UW, et al. Soft tissue substitutes to increase gingival thickness: histologic and volumetric analyses in dogs. J Clin Periodontol. 2019;46:96–104. doi: 10.1111/jcpe.13034. [DOI] [PubMed] [Google Scholar]
- 36.Woodyard JG, Greenwell H, Hill M, Drisko C, Iasella JM, Scheetz J. The clinical effect of acellular dermal matrix on gingival thickness and root coverage compared to coronally positioned flap alone. J Periodontol. 2004;75:44–56. doi: 10.1902/jop.2004.75.1.44. [DOI] [PubMed] [Google Scholar]
- 37.Wennström JL, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2-year prospective clinical study. J Clin Periodontol. 1996;23:770–777. doi: 10.1111/j.1600-051x.1996.tb00608.x. [DOI] [PubMed] [Google Scholar]
- 38.Zuhr O, Hürzeler M, Hürzeler B, Rebele S, Wandrey SON. Plastic-esthetic periodontal and implant surgery: a microsurgical approach. London: Quintessence; 2012. [Google Scholar]