Abstract
Background
Indigo naturalis (IN) is an herbal medicine that has been used for ulcerative colitis with an unclear mechanism of action. Indigo and indirubin, its main constituents, are ligands of the aryl hydrocarbon receptor (AhR). We assessed the safety, efficacy, and colon AhR activity of IN given orally to patients with treatment-refractory ulcerative colitis. The role of AhR in IN benefit was further evaluated with an AhR antagonist in a murine colitis model.
Methods
This open-label, dose-escalation study sequentially treated 11 patients with ulcerative colitis with either IN 500 mg/day or 1.5 g/day for 8 weeks, followed by a 4-week non-treatment period. The primary efficacy endpoint was clinical response at week 8, assessed by total Mayo score. Secondary endpoints included clinical remission, Ulcerative Colitis Endoscopic Index of Severity, quality of life, and colon AhR activity measured by cytochrome P450 1A1 (CYP1A1) RNA expression.
Results
Ten of 11 (91%) patients, including 8/9 (89%) with moderate-to-severe disease, achieved a clinical response. Among these 10 patients, all had failed treatment with 5-aminosalicylic acid, 8 patients with a tumour necrosis factor (TNF)-alpha inhibitor, and 6 patients with TNF-alpha inhibitor and vedolizumab. Five patients were corticosteroid dependent. Clinical response was observed in all five patients who had been recommended for colectomy. Three patients achieved clinical remission. All patients experienced improved endoscopic severity and quality of life. Four weeks after treatment completion, six patients had worsened partial Mayo scores. Four patients progressed to colectomy after study completion. Colon CYP1A1 RNA expression increased 12 557-fold at week 8 among six patients evaluated. No patient discontinued IN due to an adverse event. Concomitant administration of 3-methoxy-4-nitroflavone, an AhR antagonist, in a murine colitis model abrogated the benefit of IN.
Conclusion
IN is a potentially effective therapy for patients with treatment-refractory ulcerative colitis. This benefit is likely through AhR activation.
Trial registration number
Keywords: ulcerative colitis, clinical trials, inflammatory bowel disease
Summary box.
What is already known about this subject?
Ulcerative colitis (UC) is a chronic disease of unknown aetiology characterised by inflammation of the mucosal layer of the colon. Active disease results in a burden across most indices of quality of life. Uncontrolled disease is associated with acute complications such as pain, severe bleeding, toxic megacolon, and perforation, and chronic complications such as strictures, dysplasia, and colorectal cancer.
Current treatments have suboptimal rates of both clinical remission and response.
Indigo naturalis (IN) is an herbal medicine with a long history of use in traditional Chinese medicine. Small studies have shown benefits of IN in patients with UC.
The mechanism of the purported benefit is unknown but may be activation of the aryl hydrocarbon receptor (AhR) based on the main IN constituents (indigo and indirubin), which are ligands of AhR.
What are the new findings?
IN resulted in a clinical response in 10/11 patients treated for 8 weeks in this open-label dose-escalation pilot study of patients with UC refractory to prior treatment. Three patients achieved clinical remission. All patients experienced improved endoscopic severity and quality of life. Following treatment cessation, six patients worsened and four patients progressed to colectomy.
A 12 557-fold increase in colon AhR activity measured by cytochrome P450 1A1 RNA expression occurred at week 8 compared with baseline in the six patients evaluated. In a dextran sodium sulfate-induced murine colitis model, IN attenuated disease activity compared with vehicle control, and this benefit was abrogated when combined with an AhR antagonist.
How might it impact on clinical practice in the foreseeable future?
There is an unmet need for treatment options for patients with UC refractory to current therapies, including for those recommended for colectomy. Our preliminary data suggest a potential benefit of IN for this patient population and demonstrate that the primary mechanism of this benefit is through AhR activation.
Introduction
Ulcerative colitis (UC) is an idiopathic chronic inflammatory disease of the colon. Typical symptoms are abdominal pain, bloody diarrhoea, and cramping rectal pain. Symptoms of UC are often disruptive to the ability to work, and those with active disease experience a debilitating burden across most indices of quality of life.1 Uncontrolled disease can be associated with acute complications such as toxic megacolon and perforation, and chronic complications such as strictures, dysplasia, and colorectal cancer.1 2 The personal and economic burden of UC is reflected by high hospitalisation rates, emergency department visits, and decreased work productivity.1–3 Treatment of UC is suboptimal. More than half of patients with UC fail to respond to first-line 5-aminosalicylic acid (5-ASA) drugs and require escalation of therapy.4 Although biologics are currently the most effective therapeutics, few patients sustain long-term remission.5 Current UC treatments are also associated with risk of infection, malignancy, and pulmonary embolism. Ultimately, 14% of patients require a colectomy.6 There is a significant unmet need for more effective UC treatments.
Indigo naturalis (IN), also referred to as Qing-Dai, has a long history of use in traditional Chinese medicine.7 8 IN is an extract derived from stems and leaves of several plant species including Baphicacanthus cusia (Nees) Bremek of the Acanthacaea family, with indigo and indirubin considered its main organic ingredients.9 Benefits of IN for UC have been reported in several controlled, open-label, and retrospective studies, primarily in Japanese populations.10–16
A purported mechanism of action of IN in UC is activation of the aryl hydrocarbon receptor (AhR). Two main organic constituents, indigo and indirubin, are AhR agonists9 17 produced by gut microbiota.18 Activation of AhR is believed to lead to production of interleukin-22, which has been associated with enhanced epithelial barrier function, induction of metabolising enzymes, alteration of gut microbiota, downregulation of proinflammatory mediators, dampening of the immune response, and promotion of mucosal healing.19 20 Patients with inflammatory bowel disease have decreased AhR activity in gut microbiota.21 In a dextran sodium sulfate (DSS)-induced murine model of colitis, IN and indigo ameliorated colitis severity22–26 and this effect was absent in AhR-deficient mice.22
We conducted a phase 1b open-label study to evaluate the safety and efficacy of 8 weeks of treatment with oral IN followed by a 4-week non-treatment period in 11 patients with treatment-refractory UC, including patients recommended for colectomy who are typically excluded from UC clinical trials. AhR activity was measured by cytochrome P450 1A1 (CYP1A1) activation in colonic biopsy specimens collected after 8 weeks of IN treatment in selected patients. We also evaluated the effect of IN and concomitant administration of an AhR antagonist on disease activity in a murine colitis model.
Methods and analysis
Study design and selection of patients
The study is registered at ClinicalTrials.gov. Written informed consent (and assent, when appropriate) was obtained from all patients. Eligible patients were aged ≥13 and ≤75 years who were refractory or intolerant to 5-ASA. All patients had a biopsy-confirmed diagnosis of mild, moderate, or severe UC at screening, defined as a Mayo score of 3–12. Patients ≤17 years old were required to have active disease and be refractory or intolerant to 5-ASA, corticosteroids, small-molecule immunomodulators, and biologics or corticosteroid-dependent. Paediatric patients were required to have a body weight ≥45 kg to receive IN 1.5 g/day.
Additional entry criteria included Physician’s Global Assessment Mayo subscore ≥1 and endoscopic evidence of active mucosal disease as assessed by flexible sigmoidoscopy with Mayo endoscopic subscore ≥1. Exclusion criteria included patients with Crohn’s disease or indeterminate colitis; a change in therapy within 2 weeks before the baseline visit; use of immunomodulators; use of tobacco; diagnosis of diabetes, heart failure, unstable angina, liver or kidney disease; liver function test values greater than 1.5 times upper limit of normal; presence of Clostridium difficile, Salmonella, Shigella, Yersinia, Campylobacter, or enteropathogenic Escherichia coli in stool; and positive test for hepatitis C or hepatitis B.
During the study, patients were allowed to remain on stable UC-specific background therapy to include 5-ASA, glucocorticoids, or biologics if no change in dosing occurred, except for tapering of glucocorticoids if clinically warranted. Patients with clinical worsening requiring new UC-specific therapies or changes in dosing of background therapy, except glucocorticoid tapering, were to be discontinued from the study.
An independent data monitoring committee comprised four members who reviewed study progress and patient safety.
Randomisation, treatment administration, and dose
Patients were sequentially enrolled into one of two cohorts to receive treatment for 8 weeks followed by a 4-week non-treatment period. Cohort 1 comprised the first four patients (adults), who received 250 mg oral IN two times per day, and Cohort 2 comprised seven patients (five adults and two adolescents) who subsequently received 750 mg IN two times per day.
Patients were administered a gelatin capsule formulation of IN. The plant extract (drug substance) was processed by Fujian Xianyou Qingfeng Herbs Cooperative (Fujian Province, China) under Chinese Pharmacopoeia standards and Good Manufacturing Practice. Magnesium stearate and microcrystalline cellulose were added as excipients. The drug substance was characterised before encapsulation by high-performance liquid chromatography-ultraviolet (HPLC-UV), quantitative nuclear magnetic resonance, and inductively coupled plasma mass spectrometry to ensure purity. The drug product was tested for stability, microbial counts, and indigo (7.2%) and indirubin (0.44%) by HPLC-UV before release.
Patients were instructed to take IN capsules in the morning and evening after meals. The two IN doses (0.5 g and 1.5 g daily) were chosen because they were within a range used for varying conditions by thousands of patients in China,27 in UC clinical studies in Japan,10–16 within the lower range of recommended doses (1–3 g/d) in the Pharmacopoeia of the People’s Republic of China28 and Chinese Materia Medica,29 and within the range (0.5–2 g/d) of the largest randomised, double-blind, placebo-controlled study that reported beneficial use of IN for 8 weeks in patients with UC.10
Efficacy assessments
Disease activity in patients was evaluated based on total and partial Mayo scores obtained at baseline or screening and study weeks 2, 4, 6, 8, 10, and 12. The total Mayo scoring system for UC disease activity ranges from 0 to 12 points and is the sum of four subscores (stool frequency, rectal bleeding, endoscopic findings, and Physician’s Global Assessment), each graded from 0 to 3 with higher scores indicating more severe disease.30 A partial Mayo score is the total Mayo score without endoscopy. Flexible sigmoidoscopy for Mayo endoscopic subscore and Ulcerative Colitis Endoscopic Index of Severity (UCEIS) scores was performed at screening and week 8. The UCEIS ranges from 0 to 8 points and consists of the following descriptors calculated as a simple sum: vascular pattern (scored 0–2); bleeding (scored 0–3); and erosions and ulcers (scored 0–3).31 Faecal calprotectin,32 a biomarker for intestinal inflammation, was evaluated at baseline and weeks 4, 8, and 12. Serum C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) levels were evaluated at baseline and week 8. The Short Inflammatory Bowel Disease Questionnaire (SIBDQ) was evaluated at each visit to measure for disease-specific quality of life in patients with inflammatory bowel disease and ranges from 10 to 70, with higher scores indicating better quality of life.33 A daily patient diary was also collected to determine drug compliance and symptom severity, including number of bowel movements, presence of blood in stool, and general sense of well-being.
The primary efficacy endpoint was the proportion of patients with clinical response at week 8. Clinical response for patients with a total Mayo score at baseline ≥5 was defined as a decrease in the Mayo score from baseline of 30% or more and 3 or more points, with an accompanying decrease in the rectal bleeding subscore of at least 1 point or an absolute rectal bleeding subscore of 0 or 1.30 For patients with a total Mayo score at baseline of 3 or 4, clinical response was defined as a decrease from baseline in the Mayo score of at least 2 points and no individual subscore greater than 1. Secondary endpoints were proportion of patients with clinical remission at week 8 (Mayo score <3, with no individual subscore >1), change from baseline to week 8 in partial Mayo subscore (excluding endoscopic evaluation), change from baseline to week 8 for UCEIS score, change from baseline to week 8 in quality of life measured by SIBDQ, and change from baseline to week 8 in serum CRP, ESR, and faecal calprotectin levels.
CYP1A1 is expressed in the colon at low levels but is rapidly produced in response to AhR activation and is widely used to assess AhR activity.34 AhR activity was measured in colon biopsy samples in six patients at screening and week 8 and one patient who discontinued drug early where activity was measured at week 6. Messenger RNA was extracted from one to two biopsies per patient, and reverse transcriptase quantitative PCR was performed in quadruplicate to measure mean change from baseline in CYP1A1 expression normalised by 18S.
Safety assessments
Safety evaluations consisted of physical examination, vital signs, and laboratory evaluations at screening or baseline, day 1 (first drug administration), and weeks 2, 4, 8, and 12. Electrocardiograms were obtained at screening and week 2. Adverse events were collected throughout the 12-week study period.
DSS-induced murine colitis model
This experiment was conducted under the approval of the Institutional Animal Care and Use Committee of WuXi AppTec (Shanghai, China). All surgery was performed under sodium pentobarbital anaesthesia. Eight to 10-week-old C57BL/6J female mice were treated with oral 3% DSS (MP Biomedicals, Irvine, California, USA) in water for 7 days and subsequently changed to normal drinking water for 2 days. Mice (n=8/group) were concurrently treated two times per day for 9 days by oral gavage in four groups with IN (600 mg/kg/day) or vehicle, with or without concomitant AhR antagonist 3-methoxy-4-nitroflavone (MNF).35 MNF was delivered via intraperitoneal injection of 20 µM in 200 µl phosphate-buffered saline two times per day before oral gavage. Body weight and Disease Activity Index (DAI) scores (defined in table 1) were evaluated daily by a blinded scorer. Mice were euthanised on day 9, 4–8 hours after the final dose.
Table 1.
Disease Activity Index (DAI) scoring system for dextran sodium sulfate-induced murine colitis model. The DAI score (maximum 12) is the sum of the three subscores
| Subscore | Stool consistency | Bleeding | Weight loss |
| 0 | Normal | Occult blood negative | <1% |
| 1 | Soft but still formed | Occult blood weak positive | 1%–5% |
| 2 | Very soft | Occult blood positive | 5%–10% |
| 3 | Diarrhoea | Bleeding | 10%–20% |
| 4 | Severe diarrhoea | Heavy bleeding | >20% |
Statistical analysis
Safety and efficacy were assessed on an intent-to-treat basis for all patients who received IN. Data were summarised using descriptive statistics for continuous variables and frequency and percentages for categorical variables. Adverse events were classified by system organ class and preferred term using Medical Dictionary for Regulatory Activities (MedDRA V.22). All p values were two-sided. Tests of significance were performed for categorical endpoints using Fisher’s exact test and continuous endpoints using a t-test.
Results
Of 15 patients who signed informed consent, 4 failed in screening (laboratory values out of range, normal colonoscopy, two did not meet Mayo score criterion) and 11 were treated in this open-label, dose-escalation study conducted at Stanford University (Stanford Hospital and Clinics and Stanford Lucile Packard Children’s Hospital, Stanford, California, USA) between 15 June 2016 and 26 April 2017. Treatment was given for 8 weeks followed by a 4-week non-treatment period. During the study, study drug was noted to be out of specifications from high microbial load during routine quality control testing. As a result, the final two patients discontinued IN early, at week 2 (Patient 10) and week 6 (Patient 11). These patients received all week eight assessments at time of study drug discontinuation and completed the 4-week non-treatment follow-up period.
Baseline and demographic characteristics
Patient demographics, disease characteristics, and patient histories are listed in table 2. Of 11 patients, 2 were adolescents (ages 14 and 15) and 9 were adults (ages 19–68 years). Most (9/11) patients had moderate or severe disease at baseline. All patients were refractory or intolerant to 5-ASA. Nine patients were refractory to tumour necrosis factor (TNF) inhibitors, six patients were refractory to both TNF inhibitors and vedolizumab used separately or in combination, and five patients were corticosteroid dependent. Five patients had been advised to undergo colectomy before seeking enrolment in the trial. At baseline, stool frequency, stool consistency, rectal bleeding, faecal calprotectin, and endoscopic findings were consistent with active UC.
Table 2.
Patient demographics, baseline disease characteristics, and key efficacy outcomes. Mean (SD) are shown for both cohorts and summed total except calprotectin, which is shown as median values
| Patients | Demographics | Baseline disease characteristics | Concomitant medications | Disease history | Key efficacy outcomes | |||||||||||||||
| Patients | Cohort | Dose (g/day) | Age | Race/ethnicity | Gender | Disease severity* | Extent of disease | Total Mayo score | Calprotectin (µg/g) | Short Inflammatory Bowel Disease Questionnaire score | 5-ASA (%) | Glucocorticoids (%) | Anti-TNF (%) | Vedolizumab (%) | Failed anti-TNF (%) | Failed anti-TNF +vedolizumab (%) | Steroid dependent (%) | Colectomy recommended (%) | Clinical response (%) | Clinical remission (%) |
| 1 | 1 | 0.5 | 58 | WN | F | Mild | Left colon | 4 | N/A | 14 | X | X | ||||||||
| 2 | 1 | 0.5 | 48 | WN | M | Moderate | Left colon | 10 | 384 | 36 | X | X | X | X | X | X | X | |||
| 3 | 1 | 0.5 | 19 | WN | M | Mild | Pancolitis | 3 | 307 | 32 | X | X | X | X | X | X | X | X | ||
| 4 | 1 | 0.5 | 60 | WN | F | Moderate | Pancolitis | 9 | >1000 | 60 | X | X | ||||||||
| 5 | 2 | 1.5 | 68 | WN | F | Moderate | Rectum and sigmoid colon | 8 | 513 | 45 | X | X | X | |||||||
| 6 | 2 | 1.5 | 31 | WN | M | Moderate | Left colon | 10 | 728 | 28 | X | X | X | X | X | |||||
| 7 | 2 | 1.5 | 19 | WN | F | Moderate | Pancolitis | 9 | >1000 | 36 | X | X | X | X | X | X | ||||
| 8 | 2 | 1.5 | 38 | WN | M | Severe | Left colon | 12 | 414 | 25 | X | X | X | X | X | |||||
| 9 | 2 | 1.5 | 19 | WN | M | Moderate | Left colon | 9 | 478 | 42 | X | X | X | X | X | X | X | |||
| 10 | 2 | 1.5 | 14 | WH | M | Moderate | Left colon | 6 | 444 | 54 | X | X | X | X | ||||||
| 11 | 2 | 1.5 | 15 | WH | F | Moderate | Left colon | 8 | N/A | 24 | X | X | X | X | X | X | X | |||
| Cohort 1 | 46 (16) | 6.5 (3.0) | 384 | 36 (16) | 0 | 50 | 0 | 50 | 75 | 50 | 50 | 50 | 100 | 50 | ||||||
| Cohort 2 | 29 (17) | 8.9 (1.7) | 496 | 36 (10) | 29 | 86 | 29 | 57 | 86 | 57 | 43 | 43 | 86 | 14 | ||||||
| Total | 35 (19) | 8.0 (2.6) | 478 | 36 (13) | 18 | 73 | 18 | 55 | 82 | 55 | 45 | 45 | 91 | 27 | ||||||
*Disease severity (Mayo score): mild (3–5), moderate (6–10), severe (11–12); WH, white, Hispanic or Latino; WN, white, not Hispanic or Latino.
5-ASA, 5-aminosalicylic acid; TNF, tumour necrosis factor.
Efficacy
Table 2 summarises key efficacy outcomes. Ten of 11 (91%) patients, including both patients who discontinued IN early (weeks 2 and 6), achieved a clinical response. Among these 10 patients, all had failed treatment to 5-ASA, 8 to TNF-alpha inhibitor, 6 to TNF-both alpha inhibitor and vedolizumab used separately or in combination, and 4 were corticosteroid dependent. Clinical response was also observed in all five patients who had a colectomy recommended before study entry.
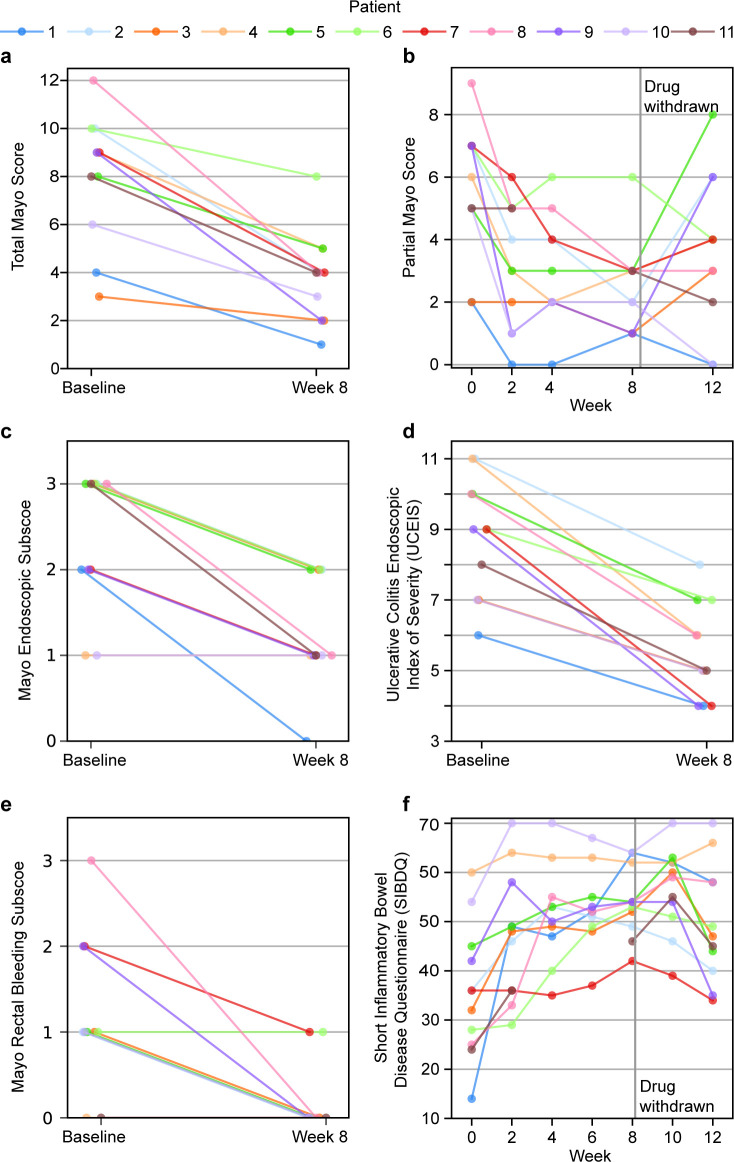
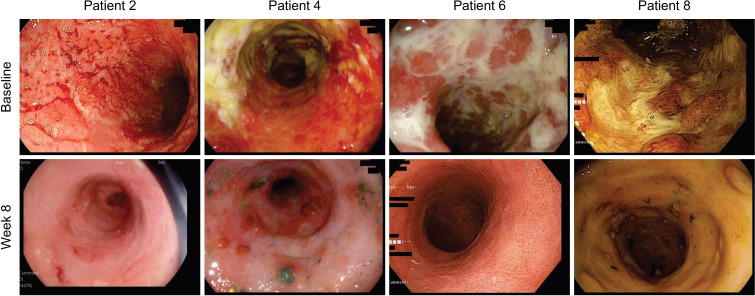
Figure 1A, B show total and partial Mayo scores for each patient. The total Mayo score decreased in all patients (mean (SD), 8.0 (2.7) to 3.8 (1.9), p<0.0001). Clinical remission was achieved in three patients. All patients experienced improvement on endoscopy after 8 weeks of treatment, with a change from baseline in mean Mayo endoscopic subscore of 2.3 to 1.3 (p<0.0001) (figure 1C) and mean UCEIS score of 8.8 to 5.5 (p<0.0001) (figure 1D). Figure 2 shows representative colon endoscopy images before and after IN treatment for four patients. Of eight patients with a Mayo rectal bleeding subscore ≥1 at baseline, seven had a subscore of 0 at week 8 (figure 1E). All patients experienced improved quality of life as measured by the SIBDQ with a change from baseline in mean (SD) SIBDQ scores from 36.0 to 54.0 (p=0.001) (figure 1F). All eight patients receiving varying doses of concomitant glucocorticoids at baseline, including five who were steroid dependent, tapered their doses by week 8 with two patients not requiring any glucocorticoids at completion of IN treatment.
Figure 1.
Individual patient efficacy outcomes. (A) Total Mayo score at baseline and week 8. (B) Partial Mayo score at weeks 0, 2, 4, 6, and 12. (C) Ulcerative Colitis Endoscopic Index of Severity (UCEIS) score at baseline and week 8. (D) Short Inflammatory Bowel Disease Questionnaire (SIBDQ) scores for all visits.
Figure 2.
Representative endoscopic images at baseline and week 8 for four patients.
Four weeks after treatment completion, 6/11 (54%) patients had worsened partial Mayo scores and 8/11 (73%) patients had worsened SIBDQ scores compared with week 8. We are aware of at least four patients who have progressed to colectomy since study discontinuation.
Safety
Table 3 summarises all adverse events. All four patients receiving IN 0.5 g/day and 5/7 (71.4%) patients receiving IN 1.5 g/day reported at least one adverse event. The most commonly reported adverse event was abdominal pain, reported by 3/4 (75%) patients receiving IN 0.5 g/day and 1/7 (14.3%) patients receiving IN 1.5 g/day. These events of abdominal pain were mild in intensity, transient, and judged to be unrelated to study drug by the investigator.
Table 3.
Incidence of adverse events
| MedDRA preferred term | (n=11) |
| Patients reporting ≥1 adverse event | 9 (82%) |
| Patients reporting ≥1 serious adverse event | 1 (9%) |
| Abdominal pain | 4 (36%) |
| Headache | 3 (27%) |
| Flatulence | 2 (18%) |
| Orthostatic hypotension | 1 (9%) |
| Anorexia | 1 (9%) |
| Sepsis | 1 (9%) |
| Pharyngitis streptococcal | 1 (9%) |
| Faeces discoloured | 1 (9%) |
| Hypotension | 1 (9%) |
| Faeces hard | 1 (9%) |
| Diarrhoea | 1 (9%) |
| Ear pain | 1 (9%) |
| Chills | 1 (9%) |
| Fatigue | 1 (9%) |
| Acne | 1 (9%) |
| Pruritus | 1 (9%) |
| Eye haemorrhage | 1 (9%) |
| Rash | 1 (9%) |
| Frequent bowel movements | 1 (9%) |
| Polyuria | 1 (9%) |
One patient had two serious adverse events during the treatment period, orthostatic hypotension and sepsis, which resolved. These two events were unrelated to IN in the judgement of the investigator. No patient discontinued IN due to an adverse event. There were no clinically significant observations or trends of IN on laboratory assessments, ECG, vital signs, or physical examination findings during the study.
Biomarkers
Faecal calprotectin levels were measured for all visits for six patients (figure 3). Data are missing for five patients due to an inability to collect fresh stool samples and premature completion of the study for two patients. For the six patients with complete data, median calprotectin at baseline was 495.5 µg/g with one patient exceeding the upper reported quantifiable limit (>1000 µg/g). The median calprotectin value at week 8 was reduced to 73.5 µg/g with one patient below the lower limit of quantitation (<15.6 µg/g). All six patients had a clinically meaningful reduction in calprotectin levels (range of reduction, 294–907 µg/g) from baseline to week 8. Neither CRP nor ESR showed marked elevations at baseline.
Figure 3.
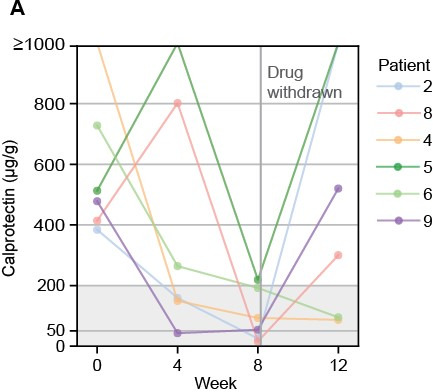
Calprotectin levels at weeks 0, 4, 8, and 12 for six patients. Normal levels are ≤50 µg/g, 200 µg/g is commonly considered positive for inflammatory bowel disease, and the upper quantifiable limit was 1000 µg/g.
AhR activation in human colon biopsies after IN treatment
Figure 4 shows an increase (12 557-fold) in mean expression of CYP1A1 between baseline and week 8 in colon tissue from six evaluated patients. One other patient (Number 10) stopped study treatment at week 6 and had a biopsy collected one day after stopping IN. This patient did not show an increase in CYP1A1 expression, consistent with AhR ligands indigo and indirubin being rapidly metabolised by CYP1A1.36
Figure 4.
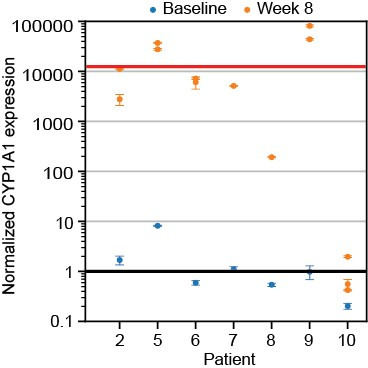
CYP1A1 expression in one to two colon tissues each from seven patients, measured by quantitative real-time PCR. The black line indicates average normalised baseline expression and the red line marks the average normalised increase (12 557-fold). Error bars represent propagated errors from CYP1A1 (n=4) and 18S (n=4) levels measured simultaneously for sample normalisation. CYP1A1, cytochrome P450 1A1.
Small molecule AhR antagonist abrogates activity of IN in DSS murine colitis model
Mice with DSS-induced colitis treated with IN (600 mg/kg) had significant improvements in DAI (mean±SEM, 4.5±1.2 vs 11±0.49, p<0.001) and body weight (17.4 g±0.7 vs 14.8 g±0.5, p=0.01) at day 9 compared with vehicle control. Administration of MNF (8 nmol/day), an AhR antagonist, abrogated the benefit of IN. Mice treated with IN and MNF had significantly worse DAI scores (9.4±1.2, p<0.01) and body weights (15.7 g±0.3, p<0.01) at day 9 compared with mice treated with IN alone. Mice treated with IN and MNF did not significantly differ compared with mice treated with MNF alone in DAI (10.5±0.9, p=0.3) or body weight (14.9 g±0.6, p=0.19) at day 9 (figure 5).
Figure 5.
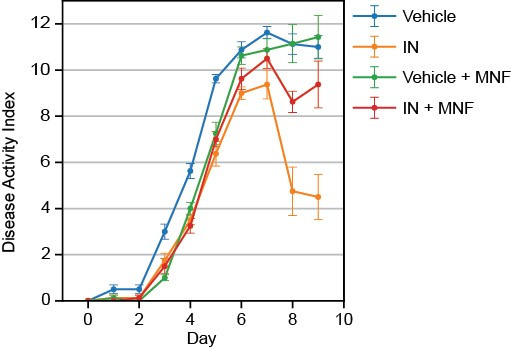
Disease Activity Index for mice with dextran sodium sulfate-induced colitis treated with vehicle or indigo naturalis (IN) through 9 days, with or without the aryl hydrocarbon receptor antagonist 3-methoxy-4-nitroflavone (MNF). Error bars represent SEM (n=8). The scoring method is outlined in table 3. Maximum score is 12.
Discussion
This open-label pilot study evaluated the safety and efficacy of 8 weeks of oral IN use in 11 patients with treatment-refractory UC. All patients showed marked endoscopic and clinical improvement from baseline to week 8 that is not expected with the natural history of treatment-refractory UC.1 Of note, a clinical response was observed at 2 weeks and 6 weeks in two patients who discontinued treatment early due to study drug being out of specification, suggesting that benefit may occur shortly after initiation of IN.12 Following discontinuation of treatment, six patients had worsening of partial Mayo scores, eight patients had worsened SIBDQ scores, and four patients progressed to colectomy.
Placebo effects are prominent in controlled trials of UC therapies.37 These effects are lower in patients with more severe baseline disease activity and prior exposure to TNF antagonists and vedolizumab.37 Our study population was refractory or intolerant to multiple agents at study entry and five patients had been recommended for colectomy, which is typically an exclusion criterion that precludes patients from entering UC clinical drug trials.1–4 The open-label nature and small sample size of our study preclude comparisons with results from large, controlled trials of approved UC drugs. Our findings, however, are consistent with prior studies demonstrating that IN improves UC, including a multicentre, randomised, controlled trial of patients with similar baseline disease severity but a less extensive history of intolerance or failure with prior treatments.10 11
The primary mechanism of action of IN in UC is believed to occur via activation of AhR. The two main organic constituents in IN, indigo and indirubin, are potent AhR agonists. AhR activation may be effective in UC by regulating the immune response and promoting mucosal healing in the intestinal microenvironment,17 18 through influences on immune cells, intestinal epithelial cells, endothelial cells, and the enteric nervous system.38 To assess the role of AhR as the main biological target of IN, we showed that 8 weeks of treatment with oral IN resulted in a~12 000-fold increase in mean RNA expression of CYP1A1, a gene directly regulated by activated AhR, in human colon biopsy samples. In a DSS-induced murine colitis model, simultaneous use of the AhR antagonist MNF abrogated the benefits of IN on disease activity.
While our pilot study showed a favourable safety profile, oral IN has been associated with a range of adverse effects, mostly outside the setting of clinical trials.39 Pulmonary arterial hypertension (PAH), which can be life-threatening, is the most serious of these complications. The incidence of PAH related to IN is unknown, with two published cases reporting development of PAH in patients with UC after IN use of 6 and 20 months, with eventual reversal of PAH with IN discontinuation.40 41 Activation of AhR has been suggested as a possible mechanism in the pathobiology of IN-induced PAH.42–44 As a natural product, the composition of IN varies widely among sources,45 making batch-to-batch consistency difficult to control. To mitigate these risks, a single molecule AhR agonist that achieves the same therapeutic effect as IN could improve quality control. Moreover, delivery of a locally acting AhR agonist in a colon-targeted delayed-release dosage form could potentially improve the safety profile by minimising systemic exposure, aberrant AhR stimulation,38 and rare but serious events such as PAH.
In conclusion, we expand on the findings of Naganuma et al that IN resulted in benefit in Japanese patients with treatment-refractory UC.10 11 Our study demonstrated benefit of IN in a Western population with a more extensive history of intolerance or failure with prior UC treatments. In addition, the study also clarifies the role of AhR activation as the primary mechanism of this benefit, consistent with the attenuation of colitis through other AhR activators in multiple animal models.46–57 Limitations of this study are its open-label nature and small sample size. Further investigation with a well-controlled study and an adequate number of patients to evaluate the use of a colon-targeted AhR agonist in patients with treatment-refractory UC is warranted.
Acknowledgments
The authors thank all study patients and their families. We acknowledge the members of the data monitoring committee and thank SPARK at Stanford advisors, including Daria Mochly-Rosen, Robert Lum, Steve Schow, and Carol Karp, for their scientific, regulatory, and manufacturing guidance. David Goodkin provided helpful advice and critical review.
Footnotes
Contributors: BL was the sponsor–investigator of the clinical study conducted under an investigator-initiated Investigational New Drug application. JPS and JOLA designed the clinical study and preclinical experiments, monitored study data collection, and analysed the data. KVG and LRF designed the clinical study and analysed the data. ES oversaw and conducted study procedures and specimen collection. MGD designed preclinical experiments and analysed data. BL and KTP were study investigators and contributed to data collection and interpretation. JPS and LRF wrote the first draft of the manuscript and all authors participated in the review. BL is guarantor of the work.
Funding: The clinical study and experiments were supported by SPARK at Stanford, Weston Havens Foundation, and Azora Therapeutics.
Competing interests: JPS and MGD are employed by and have equity in Azora Therapeutics and are co-inventors on a patent for compositions comprising indigo and/or an indigo derivative. JOLA has equity in Azora Therapeutics and is a co-inventor on a patent for compositions comprising indigo and/or an indigo derivative. LRF has stock in Azora Therapeutics related to advisory activities. BL is currently employed at the University of California, Los Angeles and has stock in Azora Therapeutics related to advisory activities. KTP declares no competing interest during the study, is an employee of Genentech, and shareholder of the Roche Group.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. De-identified patient data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the Stanford University Institutional Review Board and conducted in compliance with Good Clinical Practice guidelines, Declaration of Helsinki, and regulatory requirements.
References
- 1.Kobayashi T, Siegmund B, Le Berre C, et al. Ulcerative colitis. Nat Rev Dis Primers 2020;6:74. 10.1038/s41572-020-0205-x [DOI] [PubMed] [Google Scholar]
- 2.Fumery M, Singh S, Dulai PS, et al. Natural history of adult ulcerative colitis in population-based cohorts: a systematic review. Clin Gastroenterol Hepatol 2018;16:343–56. 10.1016/j.cgh.2017.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park KT, Ehrlich OG, Allen JI, et al. The Cost of Inflammatory Bowel Disease: An Initiative From the Crohn's & Colitis Foundation. Inflamm Bowel Dis 2020;26:1–10. 10.1093/ibd/izz104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ford AC, Khan KJ, Achkar J-P, et al. Efficacy of oral vs. topical, or combined oral and topical 5-aminosalicylates, in ulcerative colitis: systematic review and meta-analysis. Am J Gastroenterol 2012;107:167–76. 10.1038/ajg.2011.410 [DOI] [PubMed] [Google Scholar]
- 5.Sandborn WJ, Su C, Sands BE, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med 2017;376:1723–36. 10.1056/NEJMoa1606910 [DOI] [PubMed] [Google Scholar]
- 6.Parian A, Limketkai B, Koh J, et al. Appendectomy does not decrease the risk of future colectomy in UC: results from a large cohort and meta-analysis. Gut 2017;66:1390–7. 10.1136/gutjnl-2016-311550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naganuma M. Treatment with indigo naturalis for inflammatory bowel disease and other immune diseases. Immunol Med 2019;42:16–21. 10.1080/25785826.2019.1599158 [DOI] [PubMed] [Google Scholar]
- 8.Sugimoto S, Naganuma M, Kanai T. Indole compounds may be promising medicines for ulcerative colitis. J Gastroenterol 2016;51:853–61. 10.1007/s00535-016-1220-2 [DOI] [PubMed] [Google Scholar]
- 9.Plitzko I, Mohn T, Sedlacek N, et al. Composition of indigo naturalis. Planta Med 2009;75:860–3. 10.1055/s-0029-1185447 [DOI] [PubMed] [Google Scholar]
- 10.Naganuma M, Sugimoto S, Mitsuyama K, et al. Efficacy of indigo naturalis in a multicenter randomized controlled trial of patients with ulcerative colitis. Gastroenterology 2018;154:935–47. 10.1053/j.gastro.2017.11.024 [DOI] [PubMed] [Google Scholar]
- 11.Naganuma M, Sugimoto S, Fukuda T, et al. Indigo naturalis is effective even in treatment-refractory patients with ulcerative colitis: a post hoc analysis from the indigo study. J Gastroenterol 2020;55:169–80. 10.1007/s00535-019-01625-2 [DOI] [PubMed] [Google Scholar]
- 12.Uchiyama K, Takami S, Suzuki H, et al. Efficacy and safety of short-term therapy with indigo naturalis for ulcerative colitis: an investigator-initiated multicenter double-blind clinical trial. PLoS One 2020;15:e0241337. 10.1371/journal.pone.0241337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugimoto S, Naganuma M, Kiyohara H, et al. Clinical efficacy and safety of oral qing-dai in patients with ulcerative colitis: a single-center open-label prospective study. Digestion 2016;93:193–201. 10.1159/000444217 [DOI] [PubMed] [Google Scholar]
- 14.Urushikubo J, Yanai S, Nakamura S, et al. Efficacy of indigo naturalis therapy for ulcerative colitis: a case series. Intern Med 2019;58:2299–304. 10.2169/internalmedicine.2446-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suzuki H, Kaneko T, Mizokami Y, et al. Therapeutic efficacy of the Qing DAI in patients with intractable ulcerative colitis. World J Gastroenterol 2013;19:2718–22. 10.3748/wjg.v19.i17.2718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsuno Y, Hirano A, Torisu T, et al. Short-Term and long-term outcomes of indigo naturalis treatment for inflammatory bowel disease. J Gastroenterol Hepatol 2020;35:412–7. 10.1111/jgh.14823 [DOI] [PubMed] [Google Scholar]
- 17.Hubbard TD, Murray IA, Perdew GH. Indole and tryptophan metabolism: endogenous and dietary routes to Ah receptor activation. Drug Metab Dispos 2015;43:1522–35. 10.1124/dmd.115.064246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott SA, Fu J, Chang PV. Microbial tryptophan metabolites regulate gut barrier function via the aryl hydrocarbon receptor. Proc Natl Acad Sci U S A 2020;117:19376–87. 10.1073/pnas.2000047117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zelante T, Iannitti RG, Cunha C, et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity 2013;39:372–85. 10.1016/j.immuni.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 20.Mizoguchi A, Yano A, Himuro H, et al. Clinical importance of IL-22 cascade in IBD. J Gastroenterol 2018;53:465–74. 10.1007/s00535-017-1401-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lamas B, Richard ML, Leducq V, et al. Card9 impacts colitis by altering gut microbiota metabolism of tryptophan into aryl hydrocarbon receptor ligands. Nat Med 2016;22:598–605. 10.1038/nm.4102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawai S, Iijima H, Shinzaki S, et al. Indigo Naturalis ameliorates murine dextran sodium sulfate-induced colitis via aryl hydrocarbon receptor activation. J Gastroenterol 2017;52:904–19. 10.1007/s00535-016-1292-z [DOI] [PubMed] [Google Scholar]
- 23.Wang Y, Liu L, Guo Y, et al. Effects of indigo naturalis on colonic mucosal injuries and inflammation in rats with dextran sodium sulphate-induced ulcerative colitis. Exp Ther Med 2017;14:1327–36. 10.3892/etm.2017.4701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liang Y-N, Yu J-G, Zhang D-B, et al. Indigo naturalis ameliorates dextran sulfate sodium-induced colitis in mice by modulating the intestinal microbiota community. Molecules 2019;24:4086. 10.3390/molecules24224086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun Z, Li J, Dai Y, et al. Indigo naturalis alleviates dextran sulfate sodium-induced colitis in rats via altering gut microbiota. Front Microbiol 2020;11:731. 10.3389/fmicb.2020.00731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozawa K, Mori D, Hatanaka A, et al. Comparison of the anti-colitis activities of Qing Dai/Indigo Naturalis constituents in mice. J Pharmacol Sci 2020;142:148–56. 10.1016/j.jphs.2020.01.003 [DOI] [PubMed] [Google Scholar]
- 27.Qi-Yue Y, Ting Z, Ya-Nan H, et al. From natural dye to herbal medicine: a systematic review of chemical constituents, pharmacological effects and clinical applications of indigo naturalis. Chin Med 2020;15:127. 10.1186/s13020-020-00406-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.State Pharmacopoeia Commission of the PRC . Pharmacopoeia of the People’s Republic of China 2015. 10th ed. (English Edition). Beijing, China: People’s Medical Publishing Home, 2015. [Google Scholar]
- 29.Zhu Y-P. Chinese Materia MEDICA: chemistry, pharmacology and applications. 1st edn. Boca Raton, FL: CRC Press, 1998. [Google Scholar]
- 30.D'Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology 2007;132:763–86. 10.1053/j.gastro.2006.12.038 [DOI] [PubMed] [Google Scholar]
- 31.Travis SPL, Schnell D, Krzeski P, et al. Developing an instrument to assess the endoscopic severity of ulcerative colitis: the ulcerative colitis endoscopic index of severity (UCEIS). Gut 2012;61:535–42. 10.1136/gutjnl-2011-300486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.D'Amico F, Bonovas S, Danese S, et al. Review article: faecal calprotectin and histologic remission in ulcerative colitis. Aliment Pharmacol Ther 2020;51:689–98. 10.1111/apt.15662 [DOI] [PubMed] [Google Scholar]
- 33.Irvine EJ, Zhou Q, Thompson AK. The short inflammatory bowel disease questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn's relapse prevention trial. Am J Gastroenterol 1996;91:1571–8. [PubMed] [Google Scholar]
- 34.Whitlock JP. Induction of cytochrome P4501A1. Annu Rev Pharmacol Toxicol 1999;39:103–25. 10.1146/annurev.pharmtox.39.1.103 [DOI] [PubMed] [Google Scholar]
- 35.Lu YF, Santostefano M, Cunningham BD, et al. Identification of 3'-methoxy-4'-nitroflavone as a pure aryl hydrocarbon (Ah) receptor antagonist and evidence for more than one form of the nuclear Ah receptor in MCF-7 human breast cancer cells. Arch Biochem Biophys 1995;316:470–7. 10.1006/abbi.1995.1062 [DOI] [PubMed] [Google Scholar]
- 36.Sinz M, Kim S, Ferguson F. Evaluating and predicting human cytochrome P450 enzyme induction. In: Gad SC, ed. Pharmaceutical sciences encyclopedia: drug discovery, development, and manufacturing. New York, NY: John Wiley & Sons, 2010: 1–31. [Google Scholar]
- 37.Enck P, Klosterhalfen S. The placebo and nocebo responses in clinical trials in inflammatory bowel diseases. Front Pharmacol 2021;12:641436. 10.3389/fphar.2021.641436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stockinger B, Shah K, Wincent E. Ahr in the intestinal microenvironment: Safeguarding barrier function. Nat Rev Gastroenterol Hepatol 2021;18:559–70. 10.1038/s41575-021-00430-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Naganuma M, Sugimoto S, Suzuki H, et al. Adverse events in patients with ulcerative colitis treated with indigo naturalis: a Japanese nationwide survey. J Gastroenterol 2019;54:891–6. 10.1007/s00535-019-01591-9 [DOI] [PubMed] [Google Scholar]
- 40.Misumi K, Ogo T, Ueda J, et al. Development of pulmonary arterial hypertension in a patient treated with Qing-Dai (Chinese herbal medicine). Intern Med 2019;58:395–9. 10.2169/internalmedicine.1523-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nishio M, Hirooka K, Doi Y. Pulmonary Arterial Hypertension Associated With the Chinese Herb Indigo Naturalis for Ulcerative Colitis: It May Be Reversible. Gastroenterology 2018;155:577–8. 10.1053/j.gastro.2018.04.038 [DOI] [PubMed] [Google Scholar]
- 42.Dean A, Gregorc T, Docherty CK, et al. Role of the aryl hydrocarbon receptor in Sugen 5416-induced experimental pulmonary hypertension. Am J Respir Cell Mol Biol 2018;58:320–30. 10.1165/rcmb.2017-0260OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hiraide T, Teratani T, Uemura S, et al. Pulmonary arterial hypertension caused by AhR signal activation protecting against colitis. Am J Respir Crit Care Med 2021;203:385–8. 10.1164/rccm.202009-3385LE [DOI] [PubMed] [Google Scholar]
- 44.Masaki T, Okazawa M, Asano R, et al. Aryl hydrocarbon receptor is essential for the pathogenesis of pulmonary arterial hypertension. Proc Natl Acad Sci U S A 2021;118:e2023899118. 10.1073/pnas.2023899118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun Q, Leng J, Tang L, et al. A comprehensive review of the chemistry, pharmacokinetics, pharmacology, clinical applications, adverse events, and quality control of indigo Naturalis. Front Pharmacol 2021;12:664022. 10.3389/fphar.2021.664022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chu Y, Zhu Y, Zhang Y, et al. Tetrandrine attenuates intestinal epithelial barrier defects caused by colitis through promoting the expression of occludin via the AhR-miR-429 pathway. Faseb J 2021;35:e21502. 10.1096/fj.202002086RR [DOI] [PubMed] [Google Scholar]
- 47.Jing W, Dong S, Luo X, et al. Berberine improves colitis by triggering AhR activation by microbial tryptophan catabolites. Pharmacol Res 2021;164:105358. 10.1016/j.phrs.2020.105358 [DOI] [PubMed] [Google Scholar]
- 48.Scott SA, Fu J, Chang PV. Microbial tryptophan metabolites regulate gut barrier function via the aryl hydrocarbon receptor. Proc Natl Acad Sci U S A 2020;117:19376–87. 10.1073/pnas.2000047117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robles RJ, Mukherjee S, Vuerich M, et al. Modulation of CD39 and exogenous APT102 correct immune dysfunction in experimental colitis and Crohn's disease. J Crohns Colitis 2020;14:818–30. 10.1093/ecco-jcc/jjz182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marafini I, Di Fusco D, Dinallo V, et al. NPD-0414-2 and NPD-0414-24, two chemical entities designed as aryl hydrocarbon receptor (AhR) ligands, inhibit gut inflammatory signals. Front Pharmacol 2019;10:380. 10.3389/fphar.2019.00380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aoki R, Aoki-Yoshida A, Suzuki C, et al. Indole-3-Pyruvic acid, an aryl hydrocarbon receptor activator, suppresses experimental colitis in mice. J Immunol 2018;201:3683–93. 10.4049/jimmunol.1701734 [DOI] [PubMed] [Google Scholar]
- 52.Lv Q, Shi C, Qiao S, et al. Alpinetin exerts anti-colitis efficacy by activating AhR, regulating miR-302/DNMT-1/CREB signals, and therefore promoting Treg differentiation. Cell Death Dis 2018;9:890. 10.1038/s41419-018-0814-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Iyer SS, Gensollen T, Gandhi A, et al. Dietary and microbial oxazoles induce intestinal inflammation by modulating aryl hydrocarbon receptor responses. Cell 2018;173:1123–34. 10.1016/j.cell.2018.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma Y, Wang Q, Yu K, et al. 6-Formylindolo(3,2-b)carbazole induced aryl hydrocarbon receptor activation prevents intestinal barrier dysfunction through regulation of claudin-2 expression. Chem Biol Interact 2018;288:83–90. 10.1016/j.cbi.2018.04.020 [DOI] [PubMed] [Google Scholar]
- 55.Abron JD, Singh NP, Mishra MK, et al. An endogenous aryl hydrocarbon receptor ligand, ITE, induces regulatory T cells and ameliorates experimental colitis. Am J Physiol Gastrointest Liver Physiol 2018;315:G220–30. 10.1152/ajpgi.00413.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goettel JA, Gandhi R, Kenison JE, et al. Ahr activation is protective against colitis driven by T cells in humanized mice. Cell Rep 2016;17:1318–29. 10.1016/j.celrep.2016.09.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ji T, Xu C, Sun L, et al. Aryl hydrocarbon receptor activation down-regulates IL-7 and reduces inflammation in a mouse model of DSS-induced colitis. Dig Dis Sci 2015;60:1958–66. 10.1007/s10620-015-3632-x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. De-identified patient data that support the findings of this study are available from the corresponding author upon reasonable request.