Abstract
Introduction
Idiopathic pulmonary fibrosis (IPF) and non-IPF, progressive fibrotic interstitial lung diseases (PF-ILD), are associated with a progressive loss of lung function and a poor prognosis. Treatment with antifibrotic agents can slow, but not halt, disease progression, and treatment discontinuation because of adverse events is common. Fibrotic diseases such as these can be mediated by lysophosphatidic acid (LPA), which signals via six LPA receptors (LPA1–6). Signalling via LPA1 appears to be fundamental in the pathogenesis of fibrotic diseases. BMS-986278, a second-generation LPA1 antagonist, is currently in phase 2 development as a therapy for IPF and PF-ILD.
Methods and analysis
This phase 2, randomised, double-blind, placebo-controlled, parallel-group, international trial will include adults with IPF or PF-ILD. The trial will consist of a 42-day screening period, a 26-week placebo-controlled treatment period, an optional 26-week active-treatment extension period, and a 28-day post-treatment follow-up. Patients in both the IPF (n=240) and PF-ILD (n=120) cohorts will be randomised 1:1:1 to receive 30 mg or 60 mg BMS-986278, or placebo, administered orally two times per day for 26 weeks in the placebo-controlled treatment period. The primary endpoint is rate of change in per cent predicted forced vital capacity from baseline to week 26 in the IPF cohort.
Ethics and dissemination
This study will be conducted in accordance with Good Clinical Practice guidelines, Declaration of Helsinki principles, and local ethical and legal requirements. Results will be reported in a peer-reviewed publication.
Trial registration number
Keywords: interstitial fibrosis
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive condition associated with a decline in lung function, worsening dyspnoea and impaired quality of life.1 IPF belongs to a group of lung disorders called interstitial lung diseases (ILDs) and is characterised by the pathological and radiographic pattern known as usual interstitial pneumonia (UIP).2 IPF is a diagnosis of exclusion, as it refers to patients with the UIP pattern of lung injury without any identifiable cause. Although advances in the last decade have improved understanding of disease mechanisms, IPF prognosis remains poor with a 5-year mortality rate between 60% and 80%.3 Pirfenidone and nintedanib are two antifibrotic agents that can delay but not halt the progressive decline in lung function. Additionally, patients may experience adverse events (AEs) leading to treatment discontinuation, such as gastrointestinal and skin-related events with pirfenidone,4 5 or diarrhoea with nintedanib,6 highlighting the need for effective and well-tolerated treatment options.
Patients with other forms of chronic fibrotic ILDs can develop a progressive phenotype characterised by worsening respiratory symptoms, declining lung function, progressive fibrosis on imaging and early mortality.7 8 In the INBUILD trial, patients with non-IPF, progressive fibrotic ILD (PF-ILD) treated with nintedanib had a lower annual rate of decline in forced vital capacity (FVC) over the 52-week study period than those who received placebo.9 In two separate studies, one in patients with PF-ILD10 and another in patients with unclassifiable ILD that was progressive and fibrotic in nature,11 patients treated with pirfenidone experienced slower disease progression compared with those who received placebo. These data suggest that a broader population of patients with non-IPF, PF-ILD may also benefit from these antifibrotic treatment options.
The pathogenesis of fibrotic lung disease is characterised by an aberrant wound-healing response.12 Lysophosphatidic acid (LPA) is a lysophospholipid with diverse activity, including mediation of wound healing and tissue fibrosis.13 LPA exerts its physiological effects by binding to and activating a family of six G protein–coupled receptors, LPA1-6.14 LPA signalling via LPA1 impedes epithelial regeneration, increases fibroblast recruitment and promotes fibroblast resistance to apoptosis.15 Specifically, LPA1 has been implicated in the development of lung, skin, kidney, liver and peritoneal fibrosis, suggesting that this pathway is of fundamental importance in the pathogenesis of fibrotic diseases associated with tissue injury.16 LPA1 is the most highly expressed LPA receptor by lung fibroblasts in preclinical bleomycin models,16–18 and increased LPA levels have been seen in bronchoalveolar lavage fluid16 and within exhaled breath condensates19 from patients with IPF. These data suggest that LPA1 antagonism may be a valuable therapeutic strategy for patients with progressive forms of pulmonary fibrosis.20
In a phase 2 trial (NCT01766817), BMS-986020, a first-generation LPA1 antagonist, administered orally (per os (PO)) at 600 mg two times per day versus placebo for 26 weeks significantly slowed FVC decline; however, during the study there was an increased incidence of patients with hepatic enzyme and/or total bilirubin elevations, and the trial was subsequently terminated following three patients proceeding to cholecystectomy.21 Subsequent non-clinical investigations have indicated that the hepatobiliary toxicity was an unexpected effect specific to BMS-986020 and is unlikely to be associated with second-generation, structurally distinct LPA1 antagonists.22
BMS-986278 is a second-generation LPA1 antagonist in development for the treatment of patients with IPF or PF-ILD. Results from in vitro studies show that, unlike BMS-986020, BMS-986278 does not inhibit liver efflux transporters, particularly bile salt export protein (BSEP) and multidrug resistance 3 (MDR3), and no evidence of direct hepatobiliary toxicity has been seen through in vivo evaluations or phase 1 studies.22 23 Given that LPA1 antagonism was shown to be effective in patients with IPF, this phase 2 study will evaluate BMS-986278 in patients with IPF or PF-ILD.
Methods and analysis
Study design and interventions
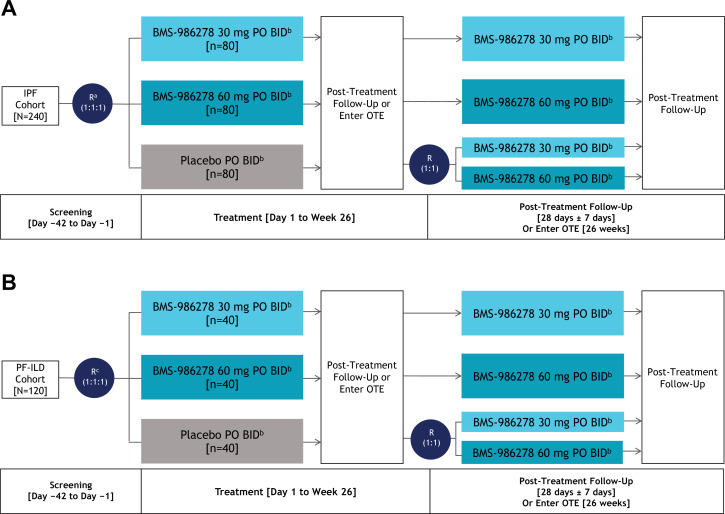
NCT04308681 is a phase 2, randomised, double-blind, placebo-controlled, international clinical study investigating the efficacy, safety, and tolerability of BMS-986278 in patients with either IPF or PF-ILD in parallel arms. The trial will consist of a 42-day screening period; a placebo-controlled, 26-week treatment period; an optional active-treatment extension (OTE) period for an additional 26 weeks; and a post-treatment follow-up for 28 days (figure 1). A schedule of key study activities is shown in online supplemental table 1. Patients will be randomised at a ratio of 1:1:1 to receive 30 mg or 60 mg BMS-986278, or placebo, administered PO two times per day for 26 weeks in the placebo-controlled treatment phase. In the OTE, patients receiving active treatment will continue to receive their assigned dosage of BMS-986278, and patients receiving placebo will be randomised to receive 30 mg or 60 mg BMS-986278.
Figure 1.
Study Design: (A) IPF and (B) PF-ILD Cohorts. aRandomisation will be stratified (1) by country (Japan vs rest of world); and (2) according to concomitant use of approved IPF therapy (pirfenidone vs nintedanib vs none). bPatients receiving 30 mg or 60 mg BMS-986278 two times per day or placebo two times per day in the main study or OTE who meet low BP criteria may have their dosage reduced to 10 mg BMS-986278 two times per day (or matching placebo for 10 mg two times per day in main study). cRandomisation will be stratified by (1) UIP pattern (typical or probable UIP vs inconsistent with UIP) of lung injury on either centrally read HRCT, surgical lung biopsy, or cryobiopsy; and (2) according to background therapy (immunosuppression (azathioprine, mycophenolate mofetil, mycophenolic acid and/or tacrolimus) vs antifibrotic agents (pirfenidone or nintedanib) vs none). BID, two times per day; BP, blood pressure; HRCT, high-resolution CT; IPF, idiopathic pulmonary fibrosis; OTE, optional active-treatment extension; PF-ILD, progressive fibrotic interstitial lung disease; PO, per os (by mouth); R, randomisation; UIP, usual interstitial pneumonia.
bmjresp-2021-001026supp001.pdf (92KB, pdf)
In the IPF cohort, approximately 240 patients with IPF will be randomised. Randomisation will be stratified (1) by country (Japan vs rest of world) and (2) according to concomitant use of approved IPF therapy (pirfenidone vs nintedanib vs none). The rationale for stratifying by country was to ensure that the Japanese patient population, which was expected to constitute a small proportion of all study patients, would be evenly randomised across arms. In the PF-ILD cohort, approximately 120 patients with PF-ILD will be randomised. Randomisation will be stratified by (1) UIP pattern (UIP or probable UIP vs indeterminate for UIP or alternative diagnosis) of lung injury on centrally read chest high-resolution CT (HRCT), and/or surgical lung biopsy or cryobiopsy if available; and (2) according to background therapy (immunosuppressive therapies alone (ie, azathioprine, mycophenolate mofetil, mycophenolic acid and/or tacrolimus) vs antifibrotic agents (ie, pirfenidone or nintedanib) vs none).
Patient population
Patient eligibility criteria are shown in box 1 for all patients and by criteria specific to either the IPF or PF-ILD cohort. In summary, adult patients with per cent predicted FVC (ppFVC) ≥40%, a forced expiratory volume in 1 s (FEV1)/FVC ≥0.7 and per cent predicted diffusing capacity of carbon monoxide in a single breath (ppDlco SB) ≥25% are eligible to participate. The IPF cohort includes patients with a diagnosis of IPF within the past 7 years and centrally read chest HRCT obtained at screening consistent with UIP or probable UIP; if the chest HRCT interpretation is indeterminate for UIP or suggests an alternative diagnosis, a surgical lung biopsy must show histopathology consistent with UIP for a patient to be enrolled in the IPF cohort.
Box 1. Patient eligibility criteria.
Inclusion criteria
All patients
ppFVC ≥40%, FEV1/FVC ≥0.7 and ppDlco SB ≥25%.
If receiving antifibrotic agents pirfenidone or nintedanib, patients must be receiving a stable dosage for ≥3 months prior to screening and during the screening period; if not receiving pirfenidone or nintedanib, patients must be naive to both drugs or not have received either 4 weeks prior to day 1.
If receiving immunosuppressive therapy (ie, mycophenolate mofetil, mycophenolic acid, azathioprine and/or tacrolimus), dosage must be stable 6 months prior to screening; these immunosuppressive medications cannot be initiated during the main study.
IPF cohort-specific inclusion criteria
Age≥40 years.
Diagnosed with IPF within 7 years of screening (including screening period).
Centrally read chest HRCT obtained at screening and is consistent with UIP or probable UIP, or lung biopsy consistent with UIP.
PF-ILD cohort-specific inclusion criteria
Age≥21 years.
-
Evidence of progressive ILD within 24 months before screening, which includes:
A decline in relative ppFVC of ≥10%, or
A decline in the relative ppFVC of ≥5% to <10% along with an increased extent of fibrosis, or
Symptoms associated with progression of ILD along with an increased extent of fibrosis.
Centrally read chest HRCT obtained at screening demonstrating evidence of >10% parenchymal fibrosis within the whole lung.
Exclusion criteria
All patients
Women who are breast feeding or of childbearing potential.
Medical conditions
Clinically significant non-parenchymal lung disease (eg, asthma, chronic obstructive pulmonary disease, cavitary or pleural diseases) at screening.
Known significant PAH, defined as previous clinical or echocardiographic evidence of significant right heart failure, history of right heart catheterisation showing a cardiac index <2 L/min/m2, or PAH requiring combination of PAH-specific therapies or any PAH parenteral therapy.
Emphysema ≥50% on HRCT assessed by a central reader, or the extent of emphysema is greater than the extent of fibrosis according to reported results from the most recent HRCT.
Acute IPF/ILD exacerbation within 6 weeks before or during screening.
Clinically significant respiratory tract infection (eg, active tuberculosis, infectious pneumonia) within 4 weeks prior to or during screening.
Significant cardiac disease or uncontrolled atrial or ventricular cardiac arrhythmias.
Known presence of significant left ventricular dysfunction.
Two-year history of alcohol or drug addiction.
Positive screening test for illegal drug use (except marijuana).
Cigarette smoking (including e-cigarettes) within 3 months before screening.
Patients who have: (1) current malignancy or (2) a previous malignancy up to 5 years prior to screening, except for those with a documented history of cured non-metastatic squamous cell skin carcinoma, basal cell skin carcinoma or cervical carcinoma in situ.
History of stroke or transient ischaemic attack within 6 months prior to screening.
History of lung reduction surgery or transplant, or is awaiting lung transplant, or plans to undergo lung reduction surgery or transplant during the study.
Positive for hepatitis C, hepatitis B, HIV-1 or HIV-2 antibodies.
Inability to tolerate oral medication or venepuncture and/or tolerate venous access.
Any other sound medical, psychiatric and/or social reason as determined by the investigator.
Prior therapy
Use of systemic corticosteroids equivalent to prednisone >15 mg/day within 2 weeks of day 1.
Use of cyclophosphamide, cyclosporine, methotrexate and/or leflunomide within 4 weeks of day 1.
Use of rituximab or other specific B–cell depleting therapies within 6 months of day 1.
Initiation or change in dosing of mycophenolate mofetil, mycophenolic acid, azathioprine and/or tacrolimus within 6 months of screening; immunosuppressive medications cannot be initiated during the main study.
Initiation or change in dosing of disease-modifying antirheumatic drugs, including but not limited to hydroxychloroquine, sulfasalazine, anti-TNF alpha antagonists, interleukin antagonists, abatacept, tofacitinib and/or baricitinib within 6 months of screening.
Use of potent inhibitors of OATPs, defined as inhibitors expected to increase exposures of OATP substrates by more than 2× within 4 weeks days of day 1.
Use of potent inhibitors or inducers of cytochrome P450 within 4 weeks of day 1.
Long-acting phosphodiesterase five inhibitors.
Simultaneous use of pirfenidone and nintedanib at screening.
Physical and laboratory tests
Seated SBP of <100 mm Hg or seated DBP of <60 mm Hg at screening or prior to day 1.
Patients with orthostatic intolerance, orthostatic hypotension (confirmed by retest within 15 min) or orthostatic tachycardia (confirmed by retest within 15 min) at screening or prior to day 1.
Uncontrolled hypertension, defined as SBP >160 mm Hg or DBP >100 mm Hg at screening or prior to the first dose of study treatment; BP may be rechecked no more than two times as clinically indicated.
ALT or AST ≥2× the ULN at screening.
Estimated glomerular filtration rate <30 mL/min at screening.
ECG prior to study treatment administration: QT ≥500 ms or QTcF ≥450 ms.
Baseline total bilirubin >1.5× ULN unless the patient has Gilbert’s syndrome; patients with Gilbert’s syndrome must have total bilirubin between ≥1.5× ULN and ≤5× ULN, with direct bilirubin at or below the ULN and no clinical or laboratory evidence of haemolysis.
History of allergy to BMS-986278 or related compounds.
IPF cohort-specific exclusion criteria
ILD associated with other known causes.
Diagnosis of sarcoidosis or any systemic autoimmune disease (including but not limited to scleroderma, polymyositis/dermatomyositis, systemic lupus erythematosus and rheumatoid arthritis).
PF-ILD cohort-specific exclusion criteria
A diagnosis of IPF with a UIP pattern.
Diagnosis of sarcoidosis or any systemic autoimmune disease (also known as ‘connective tissue disease’) other than rheumatoid arthritis (including but not limited to scleroderma, polymyositis/dermatomyositis, systemic lupus erythematosus and systemic vasculitis).
ALT, alanine aminotransferase; AST, aspartate aminotransferase; DBP, diastolic blood pressure; Dlco, diffusing capacity of carbon monoxide; ECG, electrocardiogram; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; HRCT, high-resolution CT; ILD, interstitial lung disease; IPF, idiopathic pulmonary fibrosis; OATP, organic anion transport polypeptide; PAH, pulmonary arterial hypertension; PF-ILD, progressive fibrotic interstitial lung disease; pp, percent predicted; SB, single breath; SBP, systolic blood pressure; TNF, tumour necrosis factor; UIP, usual interstitial pneumonia; ULN, upper limit of normal.
The PF-ILD cohort includes patients with a centrally read chest HRCT obtained at screening that demonstrates evidence of >10% parenchymal fibrosis and extent of emphysema less than the extent of fibrosis within the whole lung, and features of progression within the past 24 months as defined by any of these three parameters: (1) a decline in the relative ppFVC of ≥10%; (2) a decline in the relative ppFVC of ≥5% to <10% along with an increased extent of fibrosis on pre-screening chest HRCT compared with prior imaging or (3) symptoms associated with progression of ILD along with an increased extent of fibrosis on prescreening HRCT. Patients in both cohorts will be allowed to remain on a stable dosage of background therapy with either pirfenidone or nintedanib, and/or a stable dosage of immunosuppressive therapy (ie, azathioprine, mycophenolate mofetil, mycophenolic acid and/or tacrolimus). If on pirfenidone or nintedanib, patients must have been receiving a stable dosage for at least 3 months prior to screening. Similarly, immunosuppressants are permitted if the dosage has been stable for ≥6 months prior to screening.
Blood pressure monitoring
In a phase 1 single-ascending and multiple-ascending dose study (NCT03429933), placebo and BMS-986278 were associated with reversible and generally asymptomatic blood pressure (BP) reductions; BMS-986278, given as a single dose up to 150 mg and multiple dosages up to 125 mg two times per day, was well tolerated and no meaningful changes in heart rate (HR) were observed, nor were ECG abnormalities observed.23 Patients in the current study will be monitored for BP changes, as well as orthostatic signs and symptoms. Those patients meeting low BP criteria may have their dosage reduced to 10 mg BMS-986278 two times per day or matching placebo in the main study; if these patients choose to continue in the OTE, they will receive 10 mg BMS-986278 two times per day. In the OTE, patients receiving 30 mg or 60 mg BMS-986278 two times per day who meet low BP criteria may have their dosage reduced to 10 mg BMS-986278 two times per day.
Endpoints
The primary endpoint is the rate of change in ppFVC from baseline to week 26 in the IPF cohort. Key secondary and exploratory endpoints include the rate of change from baseline to week 26 in ppFVC (PF-ILD cohort only), and change from baseline in Dlco, 6 min walk test (6-MWT), Quantitative Lung Fibrosis (QLF) score24–26 measured using thoracic HRCT, patient-reported outcomes and exploratory blood-based biomarkers, as well as pharmacokinetics (PK), time to acute exacerbation and safety parameters in both the IPF and PF-ILD cohorts. Data from both cohorts will be analysed separately. All endpoints are shown in box 2.
Box 2. Study endpoints.
Primary endpoint
Rate of change in ppFVC (%) from baseline to week 26 in the IPF cohort.
Secondary endpoints
Efficacy
Rate of change in ppFVC (%) in the PF-ILD cohort from baseline to week 26.
-
Change in the following parameters from baseline to week 26.
FVC (mL) or ppFVC (%).
Dlco SB (mL/min/mm Hg) or ppDlco SB (%) (corrected for haemoglobin).
6-MWD.
Proportion of patients with ≥10% absolute decline in ppFVC (%) at weeks 4, 8, 12, 16 and 26.
Time to first ≥10% absolute decline in ppFVC (%).
-
Proportion of patients with acute exacerbations of lung fibrosis, defined as an acute, clinically significant, respiratory deterioration characterised by evidence of new widespread alveolar abnormality, as deemed by the investigator, for the following:
Acute worsening or development of dyspnoea (<1-month duration).
Imaging with new bilateral ground-glass opacity and/or consolidation superimposed on a background pattern of lung fibrosis.
Respiratory deterioration not fully explained by cardiac failure or fluid overload.
Safety
AEs.
SAEs.
Treatment-emergent deaths.
Clinical laboratory findings.
Vital signs, including BP and orthostatic hypotension assessments.
PK
BMS-986278: Cmax, Tmax and AUC(0-8 h) on day 1 and week 4 and Ctrough on week 4 and week 12 of intensive PK substudy.
Key exploratory endpoints
Efficacy
Change in the QLF score24–26 as measured by thoracic HRCT from baseline to week 26.
Composite endpoint of time to first all-cause hospitalisation or overall survival.
-
Pulmonary fibrosis progression-free survival, defined as:
≥10% decline in ppFVC relative to baseline, or
≥50 m decline in 6-MWD relative to baseline, or
Lung transplantation, or
Death.
Clinical outcomes assessments
-
Change from baseline to week 12 and week 26 in the following:
HRQoL as measured by the L-PF and SGRQ.
Dyspnoea as measured by the UCSD SOBQ.
Cough severity as measured using a VAS.
6-MWD.
Biomarkers
-
Change from baseline to week 4, week 12 and week 26 in blood-based biomarkers:
Lung fibrosis: TIMP-1, osteopontin, periostin, decorin, tenascin C.
Lung injury: MMP-7, SP-D, CA125, CA19-9.
Inflammation: CXCL13, CCL18, YKL-40, EN-RAGE, eotaxin, adiponectin.
Tissue collagen turnover and extracellular matrix: C3M, C6M, PRO-C3, PRO-C6, C4M, PRO-C4.
Blood cell gene expression and phenotyping.
Presence or absence of single nucleotide variants in genes associated with lung fibrosis.
Presence or absence of single nucleotide polymorphism variants in ADME genes such as those encoding OATPs, CYP2C8 and breast cancer resistance protein.
PK
Plasma concentrations of nintedanib and pirfenidone in patients who receive nintedanib or pirfenidone alone and coadministered with BMS-986278.
Key exploratory endpoints: optional active-treatment extension
Efficacy
-
Rate of change in the following parameters from week 26 in the main study to week 26 in the OTE, and from baseline in the main study to week 26 in the OTE.
FVC (mL) or ppFVC (%).
Dlco SB (mL/min/mm Hg) or ppDlco SB (%) (corrected for haemoglobin).
-
Changes in the following:
QLF score24–26 as measured by thoracic HRCT.
HRQoL as measured by the L-PF.
6-MWD.
Safety
AEs.
SAEs.
Treatment-emergent deaths.
Clinical laboratory findings.
Vital signs, including BP and orthostatic hypotension assessments.
Biomarkers
Blood-based biomarkers of lung fibrosis, injury and inflammation, including gene expression profiles.
PK
BMS-986278: Cmax, Tmax and AUC(0–8 h).
Plasma concentrations of pirfenidone and nintedanib coadministered with BMS-986278.
Intensive PK substudy
An intensive PK substudy will be conducted in approximately 10 patients in each treatment arm in the IPF and PF-ILD cohorts. The intensive PK substudy involves serial PK samples, ECGs, and BP and HR measurements. Additional PK samples will be collected predose on day 1, week 4 and week 12 and will be used to analyse pirfenidone or nintedanib concentrations in patients who receive these medications.
Positron emission tomography substudy
18F-BMS-986327 is an analogue of BMS-986278 that was developed as a novel positron emission tomography (PET) imaging agent.27 Patients in the IPF cohort at selected sites will receive 18F-BMS-986327 in each dose group to quantify target engagement of BMS-986278 and evaluate LPA1 distribution in the lungs.
Statistical analyses
The full analysis set (FAS), which includes all randomised patients who receive at least one dose of study treatment, will be the primary efficacy analysis population. The primary endpoint, the rate of change in ppFVC in patients with IPF, will be estimated from measurements taken over 26 weeks of treatment. This analysis will use a random coefficient linear mixed model using the FAS. The model will include time, treatment, their interactions and randomisation stratification factors specific to each cohort. No adjustment for multiple comparisons will be applied. Continuous secondary endpoints will be analysed using mixed model for repeated measures. Cochran-Mantel-Haenszel tests will be used to compare dichotomous endpoints between 30 mg and 60 mg BMS-986278 versus placebo. The Kaplan-Meier product limit method will be used to estimate the survival curves for time-to-event endpoints. Treatment comparisons between each BMS-986278 group and placebo will be performed using the log-rank test analysed by baseline stratification factors.
Analyses of safety data will be based on the safety set, which is defined as all patients who take at least one dose of study treatment. Treatment-emergent AEs, study drug–related AEs, serious AEs, physical examination findings, vital signs, clinical laboratory test results and ECG results will be summarised using descriptive statistics for continuous variables and frequency distributions for categorical variables.
The PK population is defined as all randomised patients who receive at least one dose of BMS-986278 and have any quantifiable concentration data. BMS-986278, pirfenidone and nintedanib concentration data will be summarised by visit and timepoint, as applicable, using descriptive statistics. Concentration data from both sparse and intensive PK samples will be used to further characterise the PK of BMS-986278 using population PK analysis, and to estimate model-based PK parameters.
Sample size assumptions and rationale
A sample size of 80 patients with IPF per arm was selected based on the following statistical and clinical feasibility considerations: (1) size of published early-phase trials in IPF; (2) precision to estimate the differences between the 30 mg and 60 mg two times per day doses versus placebo on ppFVC; (3) a 2.5% difference in ppFVC (favouring active treatment) would be clinically meaningful and that the SD would be 6.5%; (4) 80% of patients randomised will complete the 26-week treatment period; (5) PK and tolerability data will be key factors in the selection of a dose for further evaluation.
Given its investigative nature, no statistical considerations were utilised to determine the sample size for the PF-ILD cohort. These patients will be analysed separately and may further support the findings within the IPF cohort.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Ethics and dissemination
This study will be conducted in accordance with the principles derived from international guidelines including the Declaration of Helsinki and Council for International Organizations of Medical Sciences, Good Clinical Practice, International Council for Harmonisation, ethical principles underlying European Union Directive 2001/20/EC, US CFR, Title 21, Part 50 (21CFR50), and applicable local requirements.
All patients will provide written informed consent. Study results will be monitored by an independent Data Monitoring Committee (DMC). The DMC will review data and will make recommendations to Bristol Myers Squibb, the study sponsor, on whether the study should be allowed to continue, be modified or terminated. Final efficacy and safety results will be reported in a peer-reviewed publication.
Discussion
This is the first reported phase 2 study to enrol patients into parallel IPF or PF-ILD cohorts. The inclusion of the PF-ILD cohort reflects an important group of patients with a clinically significant disease burden who have traditionally been excluded from clinical trials that focused on IPF. This trial also permits patients to receive stable dosages of antifibrotic and/or immunosuppressive therapies, which may give insight into the role of combination therapy in patients with IPF or PF-ILD. By enroling patients with different subtypes of progressive lung fibrosis, there is an opportunity to better understand the drivers that may lead to an improved therapeutic response across different populations.
This trial also has broad inclusion criteria for the IPF cohort, which may enable recruitment of patients with more severe and progressive disease. For example, to be eligible for this trial, patients must have a diagnosis of IPF within the past 7 years and have a predicted FVC of ≥40%. In contrast, the INPULSIS studies6 required a diagnosis within the past 5 years and a predicted FVC of ≥50%, and the ASCEND study4 required a diagnosis within 4 years and a predicted FVC of 50%–90%. Furthermore, a predicted Dlco of ≥25% is permitted in this trial, whereas patients with predicted Dlco ranges of 30%–79% and 30%–90% were included in the INPULSIS and ASCEND studies, respectively.4 6 The broad eligibility criteria of the IPF cohort and inclusion of the parallel PF-ILD cohort have the potential to enrol patients who are representative of a real-world population.
This phase 2 trial is the first evaluation of a second-generation LPA1 antagonist, BMS-986278, in patients with IPF or PF-ILD. In a phase 2 trial with a first-generation LPA1 antagonist, BMS-986020, treatment with 600 mg two times per day significantly slowed the rate of FVC decline over 26 weeks compared with placebo.21 In post hoc analyses, treatment with BMS-986020 led to significant improvements in QLF (defined as a ≥2% reduction in QLF score) on HRCT28 and significant reductions in biomarkers of extracellular matrix turnover29 from baseline to week 26 relative to placebo. Although the trial was terminated because of unexpected hepatobiliary effects associated with BMS-986020 treatment,21 22 retrospective, non-clinical investigations show that these compound-specific effects associated with BMS-986020 are not expected with the second-generation BMS-986278 compound.22 For example, in contrast to BMS-986020, BMS-986278 has not been shown to inhibit liver efflux transporters, particularly BSEP and MDR3, which function to maintain normal bile acid flow and are required for the formation of protective biliary phospholipids.22 Additionally, no evidence of direct hepatobiliary toxicity has been seen through in vivo evaluations or phase 1 studies.22 23 Coupled with previous efficacy observed with LPA1 antagonism in IPF and an anticipated improved hepatobiliary safety profile, BMS-986278 shows promise for the treatment of progressive forms of pulmonary fibrosis.
The standard measures of clinical efficacy include change from baseline in FVC, Dlco and 6-MWT in both patient cohorts. Additional measures of efficacy include quality-of-life instruments, such as the Living with Pulmonary Fibrosis Questionnaire, St. George’s Respiratory Questionnaire and University of California San Diego Shortness of Breath Questionnaire, which serve to capture patient perceptions and symptom burden over the course of their treatment. Changes in QLF score from centrally analysed chest HRCT at week 26 and during the OTE will be compared with the chest HRCT performed at screening. A PET substudy will non-invasively quantify LPA1 expression in the lungs of patients with IPF and quantify target engagement of BMS-986278. This study will also have an intensive PK and a comprehensive blood biomarker strategy to evaluate changes in patients with IPF or PF-ILD following treatment with BMS-986278. These biomarker analyses will support drug mechanism of action, primary and secondary endpoints, and dose–response evaluation, as well as explore response prediction.
Conclusions
BMS-986278 is a second-generation LPA1 antagonist in clinical development that will be evaluated in a phase two study in patients with IPF or PF-ILD. Previous phase 2 trials have focused on patients with IPF, whereas this trial will also include a separate cohort of patients with PF-ILD, with both cohorts of patients being able to receive background therapy to reflect a real-world patient population. Furthermore, this trial will provide additional clinical data regarding the utility of LPA1 antagonism as a therapeutic strategy in progressive forms of pulmonary fibrosis, thereby potentially addressing the need for an effective, safe and well-tolerated treatment option in patients with IPF or PF-ILD.
Acknowledgments
The authors would like to acknowledge the Australian Centre of Research Excellence for Pulmonary Fibrosis. Bristol Myers Squibb partners in contributing to this work include LPA1 Discovery Working Group; Fibrosis Development Team; Pharmaceutical Candidate Optimization; Drug Safety Evaluation; Discovery Lead Evaluation; Bioanalytical Sciences; Veterinary Sciences; Discovery Biology; Discovery Chemistry. Medical writing support was provided by Apurva Davé, PhD, of Medical Expressions (Chicago, IL) and funded by Bristol Myers Squibb.
Footnotes
Contributors: All authors were involved in the design of the clinical study. All authors reviewed and revised drafts of the manuscript and approved the final draft. AF is responsible for the overall content of this manuscript.
Funding: This work was supported by Bristol Myers Squibb.
Competing interests: TJC has served on advisory boards for Boehringer Ingelheim, Hoffman-LaRoche, Bristol Myers Squibb, Ad-Alta, Promedior and Prometic Life Sciences. Her institution has received grants or research fees from Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Galápagos and Hoffman-La Roche, outside the submitted work. LL has served on advisory boards for United Therapeutics, Bristol Myers Squibb, AstraZeneca, Galápagos, Genentech and DevPro Biopharma; and has received research funding from Biogen, Celgene, Novartis, Bellerophon Therapeutics, Galecto, Bristol Myers Squibb, Respivant Sciences, Galápagos, Boehringer Ingelheim, Roche and Pliant Therapeutics; and has provided disease-state education for Genentech, Boehringer Ingelheim, United Therapeutics and Veracyte. JJS receives honoraria from Genentech for giving unbranded, disease-state talks on IPF; he also receives grant support from Genentech and Boehringer Ingelheim. He is a paid consultant for Boehringer Ingelheim and an unpaid consultant for Bristol Myers Squibb. TMM has received personal fees from AstraZeneca, Bayer, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Galápagos, GlaxoSmithKline, Indalo Therapeutics, Pliant Therapeutics, Roche, and UCB, outside the submitted work. His institution received grants or research fees from AstraZeneca, GlaxoSmithKline and UCB outside the submitted work. JGG is the founder of MedQIA, LLC. SMP has consulted or served on advisory boards for Boehringer Ingelheim, Bristol Myers Squibb and Altavant; and has received research funding to Duke from Boehringer Ingelheim, Bristol Myers Squibb and AstraZeneca. TS has served on advisory boards for Bristol Myers Squibb and has received an honorarium and research funding from Boehringer Ingelheim. TO has served on advisory boards for Bristol Myers Squibb and has received personal fees from Boehringer Ingelheim, Shionogi, Astellas Pharma and Toray industries. AM is a consultant for Bristol Myers Squibb. XZ, GST, BE, HX, HW, RAS, EDC and AF are all employees of Bristol Myers Squibb.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med 2018;378:1811–23. 10.1056/NEJMra1705751 [DOI] [PubMed] [Google Scholar]
- 2.Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 2018;198:e44–68. 10.1164/rccm.201807-1255ST [DOI] [PubMed] [Google Scholar]
- 3.ATS and ERS Joint Statement . Idiopathic pulmonary fibrosis: diagnosis and treatment. Am J Respir Crit Care Med 2000;161:646–64. 10.1164/ajrccm.161.2.ats3-00 [DOI] [PubMed] [Google Scholar]
- 4.King TE, Bradford WZ, Castro-Bernardini S, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014;370:2083–92. 10.1056/NEJMoa1402582 [DOI] [PubMed] [Google Scholar]
- 5.Noble PW, Albera C, Bradford WZ, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet 2011;377:1760–9. 10.1016/S0140-6736(11)60405-4 [DOI] [PubMed] [Google Scholar]
- 6.Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014;370:2071–82. 10.1056/NEJMoa1402584 [DOI] [PubMed] [Google Scholar]
- 7.Cottin V, Hirani NA, Hotchkin DL, et al. Presentation, diagnosis and clinical course of the spectrum of progressive-fibrosing interstitial lung diseases. Eur Respir Rev 2018;27. 10.1183/16000617.0076-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wijsenbeek M, Kreuter M, Olson A, et al. Progressive fibrosing interstitial lung diseases: current practice in diagnosis and management. Curr Med Res Opin 2019;35:2015–24. 10.1080/03007995.2019.1647040 [DOI] [PubMed] [Google Scholar]
- 9.Flaherty KR, Wells AU, Cottin V, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med 2019;381:1718–27. 10.1056/NEJMoa1908681 [DOI] [PubMed] [Google Scholar]
- 10.Behr J, Prasse A, Kreuter M, et al. Pirfenidone in patients with progressive fibrotic interstitial lung diseases other than idiopathic pulmonary fibrosis (RELIEF): a double-blind, randomised, placebo-controlled, phase 2b trial. Lancet Respir Med 2021;9:476–86. 10.1016/S2213-2600(20)30554-3 [DOI] [PubMed] [Google Scholar]
- 11.Maher TM, Corte TJ, Fischer A, et al. Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med 2020;8:147–57. 10.1016/S2213-2600(19)30341-8 [DOI] [PubMed] [Google Scholar]
- 12.Richeldi L, Collard HR, Jones MG. Idiopathic pulmonary fibrosis. Lancet 2017;389:1941–52. 10.1016/S0140-6736(17)30866-8 [DOI] [PubMed] [Google Scholar]
- 13.Rivera R, Chun J. Biological effects of lysophospholipids. Rev Physiol Biochem Pharmacol 2008;160:25–46. 10.1007/112_0507 [DOI] [PubMed] [Google Scholar]
- 14.Chun J, Hla T, Lynch KR, et al. International Union of basic and clinical pharmacology. LXXVIII. lysophospholipid receptor nomenclature. Pharmacol Rev 2010;62:579–87. 10.1124/pr.110.003111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shea BS, Tager AM. Role of the lysophospholipid mediators lysophosphatidic acid and sphingosine 1-phosphate in lung fibrosis. Proc Am Thorac Soc 2012;9:102–10. 10.1513/pats.201201-005AW [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tager AM, LaCamera P, Shea BS, et al. The lysophosphatidic acid receptor LPA1 links pulmonary fibrosis to lung injury by mediating fibroblast recruitment and vascular leak. Nat Med 2008;14:45–54. 10.1038/nm1685 [DOI] [PubMed] [Google Scholar]
- 17.Funke M, Zhao Z, Xu Y, et al. The lysophosphatidic acid receptor LPA1 promotes epithelial cell apoptosis after lung injury. Am J Respir Cell Mol Biol 2012;46:355–64. 10.1165/rcmb.2010-0155OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Swaney JS, Chapman C, Correa LD, et al. A novel, orally active LPA(1) receptor antagonist inhibits lung fibrosis in the mouse bleomycin model. Br J Pharmacol 2010;160:1699–713. 10.1111/j.1476-5381.2010.00828.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montesi SB, Mathai SK, Brenner LN, et al. Docosatetraenoyl LPA is elevated in exhaled breath condensate in idiopathic pulmonary fibrosis. BMC Pulm Med 2014;14:5. 10.1186/1471-2466-14-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rancoule C, Pradère J-P, Gonzalez J, et al. Lysophosphatidic acid-1-receptor targeting agents for fibrosis. Expert Opin Investig Drugs 2011;20:657–67. 10.1517/13543784.2011.566864 [DOI] [PubMed] [Google Scholar]
- 21.Palmer SM, Snyder L, Todd JL, et al. Randomized, double-blind, placebo-controlled, phase 2 trial of BMS-986020, a lysophosphatidic acid receptor antagonist for the treatment of idiopathic pulmonary fibrosis. Chest 2018;154:1061–9. 10.1016/j.chest.2018.08.1058 [DOI] [PubMed] [Google Scholar]
- 22.Gill MW, Lakshmi S, Cheng PTW. BMS-986278, an LPA1 receptor antagonist for idiopathic pulmonary fibrosis: preclinical assessments of potential hepatobiliary toxicity. Am J Respir Crit Care Med 2019;199:A5882. [Google Scholar]
- 23.Tirucherai GS, Yu D, Revankar R. BMS-986278, A lysophosphatidic acid 1 (LPA1) receptor antagonist, in healthy participants: a single/multiple ascending dose (SAD/MAD) and Japanese MAD (JMAD) phase 1 study. Am J Respir Crit Care Med 2020;201:A1492. [Google Scholar]
- 24.Kim HG, Tashkin DP, Clements PJ, et al. A computer-aided diagnosis system for quantitative scoring of extent of lung fibrosis in scleroderma patients. Clin Exp Rheumatol 2010;28:S26–35. [PMC free article] [PubMed] [Google Scholar]
- 25.Kim HJ, Brown MS, Chong D, et al. Comparison of the quantitative CT imaging biomarkers of idiopathic pulmonary fibrosis at baseline and early change with an interval of 7 months. Acad Radiol 2015;22:70–80. 10.1016/j.acra.2014.08.004 [DOI] [PubMed] [Google Scholar]
- 26.Wu X, Kim GH, Salisbury ML, et al. Computed tomographic biomarkers in idiopathic pulmonary fibrosis. The future of quantitative analysis. Am J Respir Crit Care Med 2019;199:12–21. 10.1164/rccm.201803-0444PP [DOI] [PubMed] [Google Scholar]
- 27.Smith R, Kim J, Donnelly D. BMS-986327 as a novel PET imaging agent for assessment of LPA1 receptors in IPF. Eur Respir J 2019;54:PA1399. [Google Scholar]
- 28.GHJ K, Goldin JG, Hayes W. The value of imaging and clinical outcomes in a phase II clinical trial of a lysophosphatidic acid receptor antagonist in idiopathic pulmonary fibrosis. Ther Adv Respir Dis 2021;15:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luo Y, Decato B, Palmer S. Evaluation of collagen neo-epitope biomarkers in a phase 2 trial of BMS-986020, a lysophosphatidic acid receptor antagonist, for the treatment of idiopathic pulmonary fibrosis [abstract]. Am J Respir Crit Care Med 2020;201:A2751. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2021-001026supp001.pdf (92KB, pdf)