Abstract
Introduction and importance
Soft tissue chondroma is a rare benign tumor with a predilection for hands and feet. The incidence is only about 1.5% of all benign tumors and this neoplasm is rarely seen in the paediatric population. In this paper we report the case of a 14-year-old boy treated for a soft tissue chondroma located next to the left foot second metatarsal.
Case presentation
A 14-year-old boy presented with a slowly growing plantar swelling of the left foot. The mass was solid, mobile, measuring 4 cm and located in soft tissues opposite of the left foot second metatarsal. Magnetic resonance imaging was performed and revealed a mass measuring 37 ∗ 27 mm with regular seams, on iso-signal T1 and hyposignal T2 without any skeletal connection. A marginal excision of the mass was performed and the postoperative time was uneventful.
Clinical discussion
The clinical presentation of soft tissue chondroma is generally not specific which makes the diagnosis mostly challenging. Magnetic resonance imaging is the most performed paraclinical examination that allows a better analysis of the lesion. A surgical excision of the tumor is the treatment of choice.
Conclusion
Soft tissue as a primary site of chondroma is a rarely reported localisation and this neoplasm should be kept in mind as a possible diagnosis face to any plantar mass in childhood.
Keywords: Soft tissue, Chondroma, Surgery, Child, Case report, SCARE
Highlights
-
•
Soft tissue chondroma of the plantar foot is rarely seen in the paediatric population.
-
•
They must be suspected in children with principally a painless palpable mass of soft tissues that evolves slowly.
-
•
Surgical resection of the tumor represents the basis of treatment.
-
•
A regular clinical follow-up is recommanded to detect any possible reccurrence of the neoplasm.
1. Introduction
Chondroma is a common benign cartilaginous tumor arising from the bone [1]. Soft tissue chondromas (STC) are described as extremely rare benign solitary cartilaginous masses that occurs in soft tissues without any connection to the bone [2]. Mainly reported in adulthood especially between the fourth and the sixth decades, this tumor remains rarely encountered in children [3], [4]. In this case report, we discuss the findings of a STC in a 14-year-old boy successfully treated in our primary academic center. The clinical and radiological follow up after 20 months did not show any sign of reccurence. This case report has been reported in line with the SCARE Criteria [5].
2. Case presentation
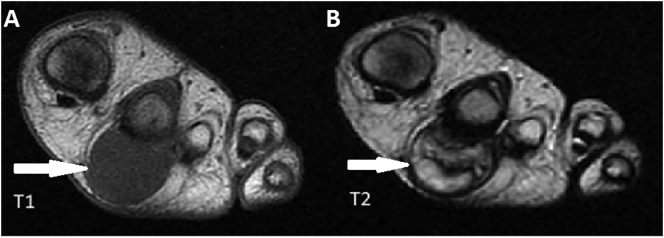
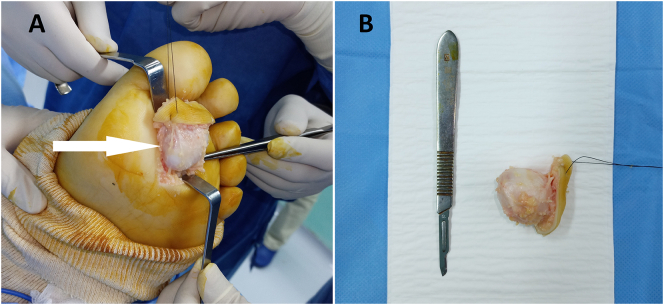
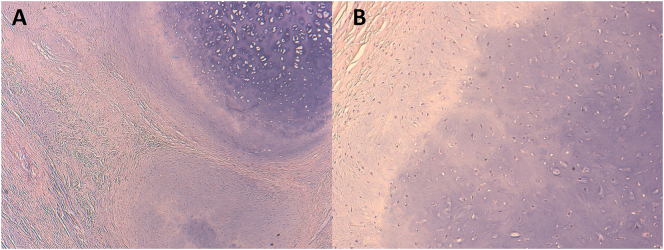
A 14-year-old boy was referred by his family physician to our department of Paediatric Surgery for a left foot plantar slowly enlarging swelling that appeared two years before and becoming painful when walking and standing for prolonged periods. The patient had no particular genetic predisposition to any family disease, no drug history nor any past surgery. The clinical examination found a patient in a good general condition with a plantar solid mobile mass, measuring 4 cm and located in soft tissues next to the second metatarsal of the left foot (Fig. 1). X-rays were normal without any calcifications or bone erosions. An ultrasond was performed and showed a very well limited mass measuring 33 ∗ 26 mm in intimate contact with the second toe flexor tendon. Importantly, a Magnetic Resonance Imaging (MRI) was performed and showed a mass measuring 37 ∗ 27 mm with regular seams, on iso-signal T1, hyposignal T2 and without any bone connection (Fig. 2). No diagnostic challenges in this case could be reported. In front of the benign nature of these radiological findings, the whole mass was excised under general anesthesia (Fig. 3). The surgical intervention was leaded by a senior paediatric surgeon with the aid of an assistant surgeon and two resident doctors. No hemmoragic or infective complication occurred during the immediate postoperative period. The macroscopic histological examination of the resected tumor found a well circumscribed mass, of nodular form, solid consistency, whitish at the cut, and measuring 4 ∗ 3 cm in size. On microscopy, the tumor was well delimitated by a peripheric fibrous capsule, and composed of lobules of mature hyaline cartilage, containing bland cytologically chondrocytes, nested in lacunar spaces or floating in a flocculent myxoid matrix. No mitosis nor abnormal mitotic figures were seen (Fig. 4). The diagnosis of a STC was made basing on the histological appearance. After twenty months of follow-up, the patient was asymptomatic without any evidence of recurrence. Additionally, no particular incidents in terms of adherence and tolerance were detected. To sum up, the evolution of the disease in our patient, its medical management, and follow-up are summerized in the timeline of Table 1.
Fig. 1.
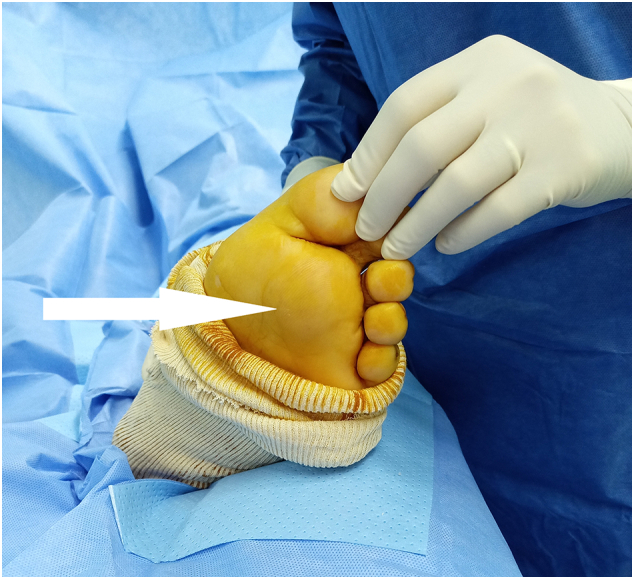
Image showing a plantar swelling measuring 4 cm and located in soft tissues opposite of the second metatarsal of the left foot (white arrow).
Fig. 2.
Transverse MRI views showing a soft tissue mass measuring 37 ∗ 27 mm with regular seams on iso-signal T1 (A) and hyposignal T2 (B) (white arrows).
Fig. 3.
A. Peroperative (white arrow) and B. postoperative images of the resected tumor showing a solid white plantar soft tissue mass made of cartilage.
Fig. 4.
A. The tumor is composed of lobules of well-formed hyaline cartilage separated by fibrous septa and delimitated by a peripheric fibrous capsule. B. Bland chondrocytes disposed within an abundant hyaline matrix that also displays myxoid areas at the periphery of the lobules.
Table 1.
A timeline showing the evolution of the disease in our patient, its medical management and following up.
| During 2 years before the consultation | Medical consultation | Postsurgical management | After 20 months of follow-up |
|---|---|---|---|
|
|
|
|
3. Discussion
Chondromas are benign neoplasms made of mature hyaline cartilage [6]. Extra-skeletal localisation is extremely rare and only about 200 cases have been reported in the literature and mostly occurred in extremities soft tissues [6], [7], [8]. Historically, the first reported clinical description of a STC in the literature was in 1883 by Baumuller B [9]. Notably, STC etiology still not very clearly described. It was suggested that stretching or repeated compression can cause a metaplasia of surrounding soft tissues in response to the chronic inflammation which may play a role in the development of this tumor [10].
Clinical manifestations of the STC are non-specific in most of patients, and physical examination can be normal or may objectify a solid and painful mobile swelling with edema, limitation of motion and erythema [11].
Radiologically, ossifications within the matrix of the tumor and remodeling of adjacent bones are detected less frequently [12], [13], [14]. In our case, foot x-ray was without bone abnormalities. Computed Tomography (CT), when performed, shows an isodense soft tissue mass without any connection to the underlying bone and calcifications detected in radiographs may be better demonstrated with CT [12]. In the present case, no CT examination was prescribed. Importantly, MRI is the most prescribed paraclinical examination given that it allows a better analysis of the lesion. It shows a well-limited and lobulated mass with low- to intermediate signal intensity on T1 and high signal intensity on T2 images [15]. The MRI findings in our patient demonstrated a uniform intermediate signal intensity which is similar to muscles on T1, and a high signal intensity on T2. The high signal on MRI is explained by elevated water concentration of the cartilage [1].
Grossly, STC are well circumscribed, usually of small size (<2 cm), with pale blue or white cut surface and with possible areas of calcifications [16]. Histologically, the tumoral proliferation is made of well circumscribed lobules of mature hyaline and myxoïd cartilage, separated by fibrous septa. The cartilage is hypercellular, containing cytologically bland chondrocytes, often arranged in clusters residing within lacunar spaces and disposed within an abundant well-formed hyaline matrix, which may also display myxoid areas. The nuclei are small, or slightly enlarged, of round form, sometimes cleaved, with dense chromatin. Mitotic activity is generally limited, and abnormal mitotic figures are absent [17].
Surgical excision of the neoplasm represents the basis of treatment [18]. The recurrence rate of the tumor is reported to reach 15–20% of cases; hence the interest of a close and prolonged clinical follow-up allowing the early detection of any recurrence [13], [18]. Recurrent tumors must be re-excised [2], [18]. In our case, the patient was totally and immediately asymptomatic after the surgical resection and without any evidence of recurrence 20 months postoperatively. During his last visit and follow-up, a complete remission was noted in our patient and his family was satisfied with our management strategy.
4. Conclusion
Skeletal chondromas are tumors commonly seen in children and adults. However, the soft tissues as a primary site of this tumor is extremely rare and should be kept in mind as a differential diagnosis in case of slowly enlarging soft tissue swelling especially in the hand and the foot.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
None.
Ethical approval
Not required.
Consent of patient
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors' contribution
L.B collected patient's data and conducted the literature review. L.B and K.E wrote the manuscript. A.H and A.B developed the histological section. S.N developed the radiological section. M.B reviewed and supervised the case report writing. All authors approved the final version of this paper.
Research registration
Not applicable.
Guarantor
Mohamed Belahcen and Larbi Benradi.
Declaration of competing interest
The authors have no conflict of interest to declare.
References
- 1.Hondar Wu H.T., Chen W., Lee O., Chang C.Y. Imaging and pathological correlation of soft-tissue chondroma: a serial five-case study and literature review. Clin. Imaging. 2006;30(1):32–36. doi: 10.1016/j.clinimag.2005.01.027. Jan-Feb. [DOI] [PubMed] [Google Scholar]
- 2.Papagelopoulos P.J., Savvidou O.D., Mavrogenis A.F., Chloros G.D., Papaparaskeva K.T., Soucacos P.N. Extraskeletal chondroma of the foot. Joint Bone Spine. 2007 May;74(3):285–288. doi: 10.1016/j.jbspin.2006.06.014. Epub 2007 Feb 27. [DOI] [PubMed] [Google Scholar]
- 3.Azouz E.M., Kozlowski K., Masel J. Soft-tissue tumors of the hand and wrist of children. Can. Assoc. Radiol. J. 1989 Oct;40(5):251–255. [PubMed] [Google Scholar]
- 4.Kamysz J.W., Zawin J.K., Gonzalez-Crussi F. Soft tissue chondroma of the neck: a case report and review of the literature. Pediatr. Radiol. 1996;26(2):145–147. doi: 10.1007/BF01372095. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Bahnassy M., Abdul-Khalik H. Soft tissue chondroma: a case report and literature review. Oman Med J. 2009;24(4):296–299. doi: 10.5001/omj.2009.60. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rapini R.P., Bolognia J.L., Jorizzo J.L. 2007. Dermatology: 2-Volume Set. St. Louis, Mosby. [Google Scholar]
- 8.Rajalakshmi V., Jayaraman, Anand V., Ramprasad N. Extraskeletal chondroma of the foot-a case report. J Clin Diagn Res. 2014;8(3):134–135. doi: 10.7860/JCDR/2014/7270.4135. Mar. Epub 2014 Mar 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baumuller B. Ein fall von ossificerendien enchondrom der weichen shaldelecken. Zentralbl. Chir. 1883;10:665–688. [Google Scholar]
- 10.Hao X., Yim J., Qi C., Mirkin G. Soft-tissue chondroma in the right hallux: a case report. J. Am. Podiatr. Med. Assoc. 2019;109(6):451–454. doi: 10.7547/18-047. Nov. [DOI] [PubMed] [Google Scholar]
- 11.Lewis M.M., Marshall J.L., Mirra J.M. Synovial chondromatosis of the thumb. A case report and review of the literature. J Bone Joint Surg Am. 1974;56(1):180–183. Jan. [PubMed] [Google Scholar]
- 12.Kransdorf M.J., Meis J.M. From the archives of the AFIP. Extraskeletal osseous and cartilaginous tumors of the extremities. Radiographics. 1993 Jul;13(4):853–884. doi: 10.1148/radiographics.13.4.8356273. [DOI] [PubMed] [Google Scholar]
- 13.Chung E.B., Enzinger F.M. Chondroma of soft parts. Cancer. 1978;41(4):1414–1424. doi: 10.1002/1097-0142(197804)41:4<1414::aid-cncr2820410429>3.0.co;2-o. Apr. [DOI] [PubMed] [Google Scholar]
- 14.Zlatkin M.B., Lander P.H., Begin L.R., Hadjipavlou A. Soft-tissue chondromas. AJR Am J Roentgenol. 1985;144(6):1263–1267. doi: 10.2214/ajr.144.6.1263. Jun. [DOI] [PubMed] [Google Scholar]
- 15.Woertler K., Blasius S., Brinkschmidt C., Hillmann A., Link T.M., Heindel W. Periosteal chondroma: MR characteristics. J Comput Assist Tomogr. 2001;25(3):425–430. doi: 10.1097/00004728-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Horvai A.E., Link T.M. Elsevier Health Sciences; 2012. Bone and soft tissue pathology. [Google Scholar]
- 17.Yamamoto H. WHO Classification of Tumours Editorial Board. Fibroblastic/myofibroblastic Tumors. WHO Classification of Tumors of Soft Tissue and Bone. 5th edition. International Agency for Research on Cancer; Lyon, France: 2020. pp. 109–112. [Google Scholar]
- 18.Weiss S.W. In: Enzinger and Weiss’s soft tissue tumors. Goldblum J.R., editor. Mosby-Elsevier; 2008. pp. 303–324. [Google Scholar]