Abstract
Snakebite envenoming is a public health concern in many countries affected by humanitarian crises. Its magnitude was recognized internationally but associations between snakebite peaks and humanitarian crises were never clearly established or analysed. This scoping review searched any available evidence of this hypothesized association between snakebite types of crises, through PubMed/Medline by two researchers. The search also included hand searching, and reports from humanitarian organizations working in this area.
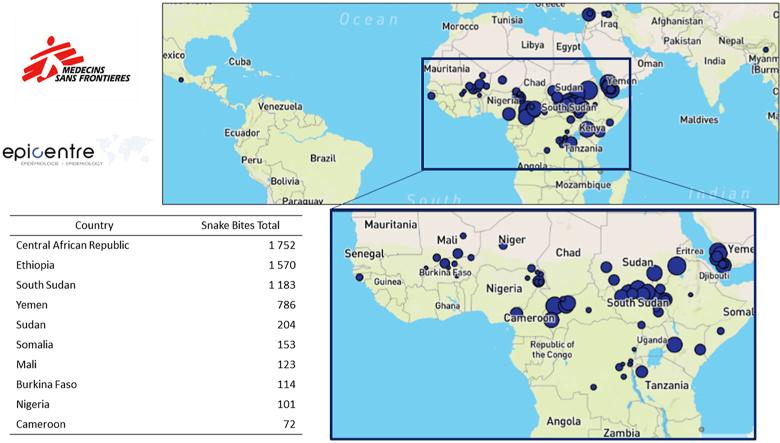
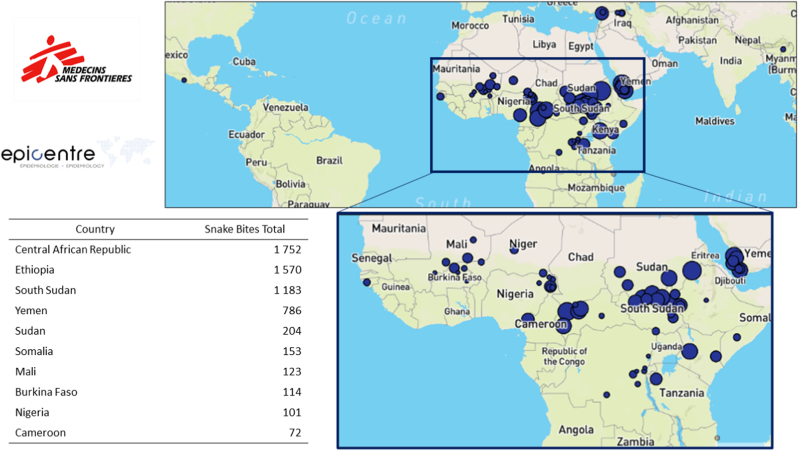
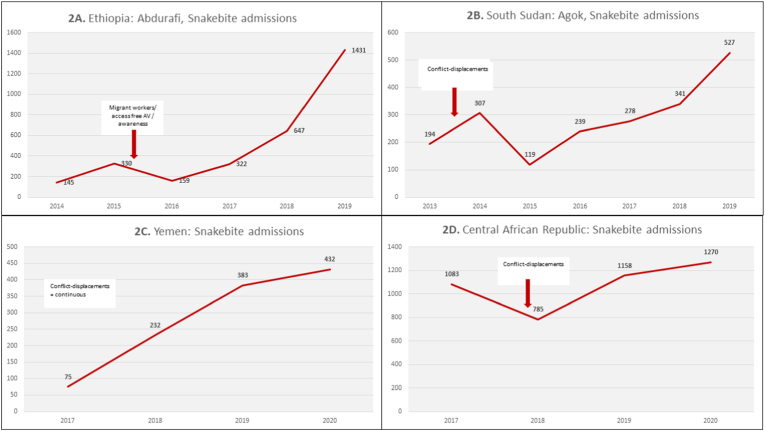
The scoping review yielded 41 results. None described a robust epidemiological link or evidence of causality. There is an evidence gap regarding our research question. Several publications however point or hint towards the occurrence of snakebite outbreaks during conflict, displacement, floods, and migration of impoverished agricultural workers. Non-systematic screening yielded another 11 publications (52 in total). We found Médecins Sans Frontières routine reports showing that 6469 patients were admitted in 2019 throughout its projects in 17 countries. The impact of snakebite was the highest in four countries particularly affected by humanitarian crises, South Sudan, Ethiopia, Central African Republic, and Yemen, with some hospitals receiving more than 1000 annual admissions. Time correlations with conflict and events are shown in Figures. We found no published epidemiological data formally showing any associations between humanitarian crises and snakebite incidence. However, the search publications showing peaks during crises, and monitoring curves in four countries point towards an increased risk during humanitarian crises.
We call for urgent population-based studies and surveillance. Stakeholders should consider upgrading snakebite care and antivenom supply during humanitarian crises in snakebite-endemic countries.
Keywords: Snakebite envenoming, Disaster, Conflict, Displaced, Refugees, Migrants
Graphical abstract
Highlights
-
•
Snakebite envenoming ‘peaks’ are described during humanitarian disasters and population displacements.
-
•
This scoping review highlights the severe paucity of data and the magnitude of snakebite in humanitarian crises.
-
•
The 52 publications reviewed suggest a link, but no robust causality was found.
-
•
Routine hospital data from Médecins Sans Frontières showed snakebite 6469 admissions in 17 countries last year.
-
•
Trends in South Sudan, Ethiopia, Centrafrique, and Yemen suggest an influence of humanitarian crises on snakebite admissions.
1. Introduction
Snakebite envenoming (SBE) is a public health concern and an individual emergency in many tropical and subtropical countries affected by humanitarian crises. Its magnitude was recognized internationally when the World Health Organization (WHO) added SBE to its list of Neglected Tropical Diseases (NTDs) in 2017, and launched its strategic roadmap in 2019 (Williams et al., 2019; Minghui et al., 2019). Each year, two million of the 4.5–5.4 million global snakebite victims develop clinical envenoming, an estimated 400,000 become disabled, and 81,000–138,000 die (World_Health_Organization, 2021). Three distinct regions carry most of this global burden: South Asia (1.2–2 million cases, 50–100 thousand deaths), Sub-Saharan Africa (435–580 thousand cases, 20–30 thousand deaths) and South America (137–150 thousand cases, 3–5 thousand deaths) (Gutierrez et al., 2017). Ministries of health and international organizations have often been alarmed by peaks of snakebite injuries occurring just after man-made or natural disasters. The risk of SBE in humanitarian settings was highlighted by the WHO, the Kofi Annan Foundation, Médecins Sans Frontières and partners, in a joint meeting before Snakebite Envenoming was finally included as a priority NTD (O/KofiAnnanFoundation., 2016).
Our hypothesis was that snakebite ‘peaks’ could be a consequence of humanitarian crises. Therefore, we believed that descriptions of snake-bite risks should appear in peer-reviewed publications or reports from countries affected by conflict, internal displacement, refugee crises, as well as floods, and possibly other disasters. These crises disrupt access to care, but they also increase the likelihood of exposure to snakes and their bites. During natural disasters, snakes may be forced to find shelter outside their natural habitat. As displaced people suffer from precarious living conditions and often lack appropriate footwear, they may be more frequently exposed, particularly nocturnally or when fleeing through the bush or fields, where they are more likely to encounter snakes. We will try to support this hypothesis through this literature search.
Our aim is to describe any available evidence on SBE in humanitarian crises, or during migration, through a scoping review of available published evidence. Our second aim is to present non-peer reviewed publications or reports from Ministries of Health and medical organizations intervening in humanitarian crises, such as the WHO, UNICEF, and Médecins Sans Frontières (MSF) also known as Doctors without Borders, which could support this hypothesis.
2. Methods
Two methods were used to answer the main research questions searching evidence on SBE in humanitarian crises and migration, such as associations, causality, and epidemiological links. Scoping review was preferred over systematic review, as the main objective was to assess the volume of evidence (or lack thereof) and any publications addressing this ‘emerging’ topic, rather than to compare clinical outcomes from studies, which is the main purpose of systematic reviews. Moreover, scoping reviews allow a broader type of inclusion criteria. We conducted a rapid scoping review (Tricco et al., 2015) according to PRISMA-ScR guidance. The hypothesis of our review was that there would be very little evidence on SBE epidemiological trends during or immediately after these crises, and therefore that a causality between humanitarian crises and risk of snakebite accidents or SBE would be difficult to infer. The largest medical literature databases: PubMed and MEDLINE were searched between March and June 2021. Inclusion criteria included participants of all ages, all genders/sex, and from all contexts defined by Mistry et al. in ‘Conflict and Health’ as humanitarian crises: man-made disasters, including armed conflict, forced displacement, and refugee crises; natural disasters, such as floods, earthquakes, droughts, and major disease outbreaks (Mistry et al., 2021). No exclusion criteria were applied.
We used the following seven query boxes: “snakebite envenoming” OR “envenomation” OR “snakebite” OR “snake bite”; 1. AND “humanitarian crises”; 2. AND “conflict” OR “war”; 3. AND “displaced” OR “internally displaced”; 4. AND “refugees”; 5. AND “migration” OR “migrant”; 7. AND “developing countries”; 8. AND “disaster” OR “flood” OR “earthquake); . We applied [Title/Abstract] and [MeSH] term searches to all possible synonyms and similar concepts. Available data was appraised following the PRISMA approach.
All databases were searched without any data limiters. Search results were classified and filtered, and duplicates were removed, using Endnotes X9™. Two individual reviewers (GA and JP) independently screened titles and abstracts of studies against the inclusion criteria and performed the inclusion process separately for the PubMed/MEDLINE searches. Google Scholar and hand searches were done by one author. Ethical clearance was not necessary for routine aggregated, non-individual data. We extended this search using Google Scholar, snowballing, and hand searches of non-peer reviewed and media articles. We included publications suggested by experts.
In parallel we obtained data from the District Health Information Software 2 (DHIS2) routine monitoring tool installed in most MSF projects. MSF data was analysed at Epicentre, MSF's epidemiology partner, and it was displayed on a map locating all snakebite victims in MSF humanitarian interventions areas in Africa, America, and Asia. We analysed location and number of snakebites per project and country. Finally, we present more detailed data from four countries facing conflicts and high rates of migration or displacement.
3. Results
3.1. Literature scoping review results
The scoping review yielded 41 results. None described a robust epidemiological link or evidence of causality. There is an evidence gap regarding our research question. However, these publications describe (non-statistically), point, or hint towards an increased incidence of snakebite accidents during conflict, displacement, floods, and migration. Non-systematic screening yielded another 11 publications (52 in total).
3.1.1. Humanitarian crises, conflicts and war
There was no publication addressing directly and completely the research question of snakebite in humanitarian crises. Query boxes yielded three results, but none linking humanitarian crises and snakebite risk. One expressed the importance of access to antivenom in humanitarian crises in Sub-Saharan Africa (Brown and Landon, 2010). Query boxes on snakebite in conflict and war yielded 114 results, of which the vast majority did not address the question. One case report of a snakebite in South Africa (Firth et al., 2016) highlighted the challenges of mortality due to remoteness in humanitarian settings. Another paper highlighted the burden of snakebite and complex access to antivenom in countries affected by conflicts in Sub Saharan Africa (Brown, 2012). Finally, one study on snakebite and scorpion envenoming among military personnel of several nations in the Middle East, found an increased likelihood of being bitten in Afghanistan, attributed by the authorities to “unimproved” precarious sanitation facilities. This study describes frequent snakebites as a probable consequence of certain basic toileting facilities (trench and burn toilets) (Shiau et al., 2007).
3.1.2. Developing countries and snakebite severity
The query box on developing countries yielded more results. Multiple publications suggest that living in LMIC and in remote areas are linked with the risk of SBE and its severity (Snake bite: time to stop, 2010; Chippaux, 2011; Cruz et al., 2009; Gutiérrez et al., 2014; Hernandez et al., 2019; Iliyasu et al., 2015; McGain et al., 2004; McNamee, 2001; Simpson and Norris, 2009; Warrell, 1993). The effect of distance is specifically analysed in North-Eastern Nigeria, an area affected chronically by humanitarian crises, from internal conflict, displacement, outbreaks and malnutrition (Iliyasu et al., 2015). Snowballing using keyword “Nigeria” showed multiple publications (Iliyasu et al., 2015; Igawe et al., 2020; Nduagubam et al., 2020; Habib et al., 2001, 2015, 2021; Michael et al., 2018; Muhammed et al., 2017; Habib, 2003, 2013; Karaye et al., 2012; Habib and Abubakar, 2011; Abubakar et al., 2010; Molesworth et al., 2003; Idoko and Ikwueke, 1984; Onuaguluchi, 1960), describing specific impacts of poverty, agricultural activities, and insecurity due to conflicts in Nigeria, on time to consultation, severity and amputation, all related to human activities and poverty. One of them (Habib et al., 2001) describes specific impacts of conflict and displacement on snakebite incidence and supports the hypothesis that “Abandonment of homes for two years due to communal clashes has been thought to have allowed snake populations to grow.”
Queries on conflict-affected countries areas yielded more specific findings. In a large Middle-Eastern snakebite review, Yemen was recognized among affected countries (Amr et al., 2020). However it is not clear if the incidence of snakebite was as high before the war due to lack of comparable data. These 26 articles in LMICs show or suggest the difficult or delayed access to treatment and antivenom, and the probable link with an increased level of surgical complications, long-lasting disabilities, and death.
3.1.3. Displaced, refugees, and migrants
This search yielded two relevant publications. One describes four snakebite victims (Tameru, 2006) who arrived in an Ethiopian refugee camp: all were severe cases, one died, probably due to the long journey with a late access to treatment. The second paper describes the “frequent” occurrence of foot wounds due to snakebites among refugees (Luyckx et al., 2008). Hand searches yielded two relevant papers on refugees. First, a Lancet paper on vulnerable refugees in camps near the Afghan border in Pakistan, which describes the frequent danger of snakebite, especially while walking at night (Rashid and Adnan, 2009). Another paper describes this same danger for refugees in Kakuma, Kenya (Bolon et al., 2020). Participants mentioned the “fight against malaria and snakebites” as main priorities in Kakuma.
3.1.4. Humanitarian crises due to natural disasters
Queries on disasters, floods, and earthquakes, yielded 45 results, but only five were relevant to our specific research (Alcantara et al., 2018; da Silva Souza et al., 2018): two studies in Brazil, one study in Ecuador (Tauzer et al., 2019) and one study in India (Monteiro et al., 2012) confirming the vulnerability of farmers during the rainy season and monsoon, but these do not address a specific human disaster or humanitarian crisis, and do not show data or magnitude of effect. One study in Thailand mentions the increased incidence of snakebite in children during floods (Laohawiriyakamol et al., 2011). In Brazil a time-series study analyzing rainfall and humidity levels over years concluded that increased humidity (rather than rainfall) is related to increased snakebite yearly admissions (Ferreira et al., 2020).
The search for grey and unpublished literature through specialists yielded one publication on snakebite risks associated with flooding (Ochoa et al., 2020). Ochoa et al.‘s “review shows that flooding seems to dramatically increase the exposure of people and snakes to each other”. Finally other experts pointed towards a review on “Snake envenomation in Bangladesh”, which shows that snakebite was one of the leading causes of death in the 2004 and 2007 flooding events, and that snakebite admissions were increased during earthquakes in Chittagong (Ghose and Faiz, 2015).
3.2. Results from humanitarian organizations and specialists
The manual search and snowballing search of available “grey” literature included congress, poster, and website reports addressing the same questions. Facing interruption of production of a major polyvalent antivenom, and preexisting scarcity, key stakeholders from academia and humanitarian organizations joined to call for action to reduce neglect in affected countries as reported in Nature (Schiermeier, 2015). Several examples have emerged since this statement. Médecins Sans Frontières’ have recognized probable contributing factors in four of their large projects: Internal displacement due to armed conflict, in South Sudan, (Said et al., 2020), Central African Republic (CAR), and Yemen, and economic migration by impoverished agricultural workers observed in Ethiopia (Steegemans et al., 2021; F/DoctorsWithoutBorders, 2019).
3.2.1. Ethiopia
An Ethiopian study describes haemotoxic viper bites becoming more frequent with recent sesame agriculture expansion in north-western Ethiopia, attracting many young male migrant workers from impoverished areas (Mekonnen et al., 2016). Another study described four SBE victims, three severe and lethal, who arrived during the hottest months in a refugee camp in eastern Ethiopia (Tameru, 2006). A systematic review shows that inadequate footwear (Tomczyk et al., 2014) was strongly associated with many NTDs including snakebite, but strong statistical associations were found only for classic bacterial (Buruli ulcer) and parasitic (hookworms, strongyloidiasis) NTDs, and no data was available for snakebite. Displaced people frequently lack access to protective footwear, and as such are more exposed in sandals and flip-flops, but this remains a hypothesis only.
3.2.2. South Sudan
One study specifically showed the magnitude of snakebite admissions in an MSF project in Agok, South Sudan (Said et al., 2020). This is a war-affected area where displaced populations have sought refuge near an MSF hospital for the past ten years. Snakebite admissions have increased from 200 to more than 500 per year. The year of the worst conflict and displacement, after December 2013, saw an abrupt snakebite peak (up to 90 patients per month) due to the sudden surge in violence forcing displaced people to settle in a flooded marshland. Unprotected dwellings (tents) and inadequate footwear were the most frequently reported risk factors in arriving SBE victims.
3.2.3. Central African Republic and Cameroon
Two systematic reviews with MSF coauthors (Taieb et al., 2018; Alirol et al., 2015) showed the difficulty of access to antivenom and poor outcomes in countries of interventions such as Central African Republic and Cameroon. They highlight problems such as insufficient international support to antivenom supply, high prices of antivenoms, dangerous traditional practices, poor quality standards, and geographic inappropriateness of certain antivenoms (i.e. antivenoms for Indian species used in Africa), as well as a concern about centralization of stocks.
3.2.4. Non-peer reviewed publications and media findings
Our search was completed by non-peer reviewed publications suggested by key-informants or found outside the systematic search. Firstly, we included a large peer-reviewed study published in Toxicon-X recently that expressed the views of experts and key-informants about the impact of the global COVID-19 pandemic and crisis on the burden of snakebite (van Oirschot et al., 2021).
The informants highlighted that snakebite affects primarily the poorest communities. A health provider from India and two community members, one from Bangladesh, the other from Kenya, “thought rural migration could have increased the risk of snakebites, with people moving back to rural villages from the cities during (COVID-19) epidemic waves”. Snakebite risk was reportedly increased during the Covid-19 lockdowns (also a humanitarian crisis), due to a closure of schools and workplaces, resulting in increased exposure of children left to play outdoors. Media also report such risk in quarantine facilities infested by snakes in four different publications (Azad, 2020; Deuba, 2020; Shahi and Gahatraj, 2021; TimesNow. Uttarakhand: Mi, 2021), a tragic indirect consequence of this crisis.
Regarding natural disasters and snakebite, other informants surveyed in the study, Van Oirschot et al. reported that they had seen an increase in snakebite cases but did not directly relate this to COVID-19 (van Oirschot et al., 2021). Instead they associated it to” increased rainfall or flood” (Bangladesh, Malaysia, Nepal, Brazil). Despite the absence of statistical evidence, the authors highlight the perceived risk of snakebite by informants in their 22 countries (which are often affected by humanitarian crises).
Another media report showed that “after 2,000 km trek home from Bengaluru, migrant dies of snakebite” (Petlee, 2021). Regarding snakebite and humanitarian crisis in Africa, the National Geographic showed one more example of a snakebite envenoming occurring in Mbandaka, D.R.Congo, in an isolated area, affected by the Ebola humanitarian crisis, other epidemics, and chronic access issues (Nicolon, 2020). In areas affected by humanitarian crises (conflicts, epidemics, natural disasters), timely access to antivenom seems even more complex due to the disruption of supply, of logistic chains, and of health priorities (Potet et al., 2021), whereas the risk could be increased in these situations.
3.3. Routine data monitoring from humanitarian organizations
Médecins Sans Frontières’ (MSF) routine report shows that 6469 patients were admitted for SBE in 2019 in its hospitals throughout 17 countries. The impact of snakebite was the highest in four countries particularly affected by humanitarian crises, South Sudan, Ethiopia, Central African Republic, and Yemen with hospitals receiving more than 1000 annual admissions each. Cases were reported in 17 humanitarian settings from Africa (11 countries), the Middle East (Yemen, Syria, Iraq), Asia (Burma and Bangladesh), and America (Mexico).
The relative proportion of hospital admissions is shown in Fig. 1. MSF's hospitals in four countries, Central African Republic (CAR), Ethiopia, South Sudan, and Yemen reported more than 1000 annual snakebite admissions per country. Higher numbers seem to coincide with the timing of the humanitarian crisis in South Sudan. However, the results simply coded as “snakebite = yes/no” results do not allow further analyses yet (on demographics, outcomes, etc).
Fig. 1.
Distribution of snakebites (N = 6469 patients) per MSF intervention sites in 2019 based on DHIS-2 monitoring data.
Data from routine monitoring tools in MSF projects in South Sudan, Ethiopia, Yemen and CAR are shown in Fig. 2. These curves show increase in admissions from 2014 to 2019 in the four countries. We hypothesize that the first factor driving the surge in admissions was the humanitarian crisis occurring. Later, the further increase in admission is probably due awareness of access to free hospitalization including antivenom and surgical care. This has increased the trust and the coverage of these hospitals in their catchment area.
Fig. 2.
Snakebite admission curves from MSF largest snakebite projects in Ethiopia South Sudan, Yemen, and Central African Republic with timing of crises.
3.3.1. Ethiopia
In Ethiopia snakebite admissions are the highest among all MSF projects, at 1752 admissions in 2019, most being moderate and about 22% haemotoxic. Recent MSF data from a rural hospital in north-western Ethiopia (Steegemans et al., 2021), serving impoverished migrant agricultural labourers, working and sleeping unprotected in the open fields, show a dramatic increase in admissions from 145 in 2014 to 1431 in 2019. (Fig. 2 A). This also resulted in earlier health seeking (even for mild snakebites), and a reduction of the proportion of patients with severe envenomation requiring antivenom treatment from 35% in 2015 to 22% in 2019. In parallel, overall case fatality rate remained below 2%, and below 0.5% when appropriate antivenoms were available. In 2018–2019 there were 27 snakebite referrals from Abdurafi to a tertiary hospital; 16 for surgical amputation, 9 for severe coagulopathy, and 2 for compartment syndrome. 2 referred patients died due to intracranial haemorrhage.
3.3.2. South Sudan
South Sudan was among the most affected countries with 1183 admissions in 2019 in MSF hospital projects, half of them being in Agok (Abyei Administrative Area). In Agok, the MSF-supported hospital saw a rapid increase in snakebite admissions between 2013 and 2019, from 194 to 527 victims annually in a single hospital (Said et al., 2020) (Fig. 2 B). Out of 527 cases in 2019, 47% were severe and required antivenom. As mentioned in the article (Said et al., 2020), in Agok hospital snakebite injuries were “the fifth leading cause of surgical intervention among all performed surgical interventions. In 2019, 66 procedures among the total 527 snakebite patients represented 9.4% of all surgical interventions.” In the recent monitoring, out of 901 snakebite patients admitted, 448 presented severe syndromes requiring antivenom, 11 were discharged with disabling sequelae, and one died. The case fatality rate also dropped from 3% to 1%. Deaths were due to envenoming by haemotoxic and cytotoxic vipers (Echis pyramidum and Bitis arietans) and some neurotoxic cobras or mambas (Naja haje or Dendroaspis polylepis). Interactions between snakes and humans seem to be increased due to snake-prone habitats, tents, non-protective footwear, and flooding of the Nile.
3.3.3. Central African Republic
A systematic review of African antivenoms suggests that case fatality may be very elevated, up to 10–20%, when standard antivenoms' supply/production are interrupted, and replaced by inappropriate harmful products (Alirol et al., 2015). The venom of E. ocellatus may induce systemic haemorrhage, coagulopathy, and shock, as well as extensive local tissue damage. In the absence of treatment, the case fatality rate is 10%–20%. Médecins Sans Frontières (MSF) treats many E.ocellatus bites in its projects in sub-Saharan Africa, notably in Paoua in Central African Republic (CAR), where E. ocellatus envenoming is frequent. Mortality was clearly improved by the use several free, effective, and specific antivenoms and access to free care as described by Alirol et al. (2010). In Central African Republic, admissions with haemotoxic envenoming have been remarkably high in Paoua, an MSF project in the North West of the country. An unpublished survey by MSF-Epicentre also indicated that snakebite was among the top five causes of mortality in the community, suggesting that a large proportion of SBE victims did not reach Paoua's hospital facilities and therefore couldn't access effective antivenoms (Salou and Roederer, 2017). The number of admissions decreased temporarily in 2018, after 70,000 people were forced to flee the inner city of Paoua, due to an extension of the armed conflict. Our hypothesis is that fewer snakebite victims in the neighbouring villages in the region are now able to reach the hospital in Paoua because of insecurity. The displaced started to return home in June 2019, and the number of snakebite admissions increased again in 2019 and 2020.
3.3.4. Yemen
Finally, in Yemen, snakebite admissions are continuously increasing at MSF's hospital. From 75 in 2017, they have increased to 432. Probable contributing factors are the habitat of displaced victims living in tents, increasing influx of victims due to absence of treatment in disrupted hospitals, and awareness of free care and antivenom at MSF facilities.
4. Discussion
This scoping review and report analysis highlights both the severe paucity of data, and the magnitude of snakebite in humanitarian crises in Africa and the Middle East. The “data crisis” was recently highlighted by Genevieve et al. (2018). Most peer and non-peer reviewed publications and media reports from the scoping review hint at, but cannot clearly demonstrate, any definite association or causality, between humanitarian crises and snakebite peaks, in the absence of published epidemiological surveys, or detailed snakebite information in conflict or disaster zones. This lack of evidence, and reliance on more anecdotal reports, is due to the generalized absence of snakebite surveillance indicators in standard country surveillance systems. In addition, as care is often not available, patients will not present, so it will not be reported. Victims could die of snakebite envenoming and remain completely hidden during such crises. This calls for strengthening of routine surveillance, and detailed observational studies of routine data, which could be easy to implement.
Most data from conflict zones were obtained through MSF routine hospital data collection and associated surveillance tool, DHIS2. This same tool is also used by WHO for other NTDs, but it's only emerging as a global surveillance tool for Snakebite envenoming, in accordance with WHO's 2019 strategy on coordinated response and WHO's roadmap on SBE(Williams et al., 2019). Rapid displacement of populations fleeing with few personal items, with inadequate footwear, and experiencing precarious living conditions (tents, traditional housing, or simply living/hiding in the bush or forest) were factors most commonly reported in snakebite peaks seen during crises, but there is no formally measurable association or means to analyse causality.
The high burden of snakebite in Central African Republic, Ethiopia, South Sudan, and Yemen, seems to coincide with the disastrous humanitarian situation in three of these countries (CAR, South Sudan, and Yemen) and with the impoverished workers migration in Ethiopia. Similar conditions are found in Northern Nigeria and several other areas of the world affected by humanitarian crises and migration described in this review on four continents (Africa, Asia, America, Oceania). Additional non-systematic searches yielded two publications, media reports, and key informant interviews, which allowed to highlight a high perceived risk of snakebite in 22 tropical and subtropical countries often affected by humanitarian crises.
Our findings suggest that humanitarian crises, conflict, and displacement, can easily trigger snakebite peaks, in most tropical and subtropical areas. National authorities and international organizations should therefore plan for this and constitute stocks of antivenom and ancillary treatments for snakebite envenoming. The WHO should specifically address this NTD in conflict-settings and countries most vulnerable to environmental and humanitarian crises.
Increases in admissions were also related to awareness of availability of “free-of-charge and good quality” antivenom for these vulnerable populations. Such data from Ethiopia, South Sudan, CAR and Yemen are encouraging in the sense that any access-coverage increases may subsequently improve quality of care and result in mortality-morbidity reduction.
Therefore, government authorities, health ministries, and international organizations should be encouraged to conduct routine surveillance and notification of snakebite cases. These actors should also provide free (or affordable) clinical care and antivenom for snakebite victims in humanitarian crises and migration in endemic areas, as well as support prevention programs (shoes, shelter, bednets).
5. Conclusion
Facing both the severe paucity of data, and the magnitude of snakebite in humanitarian crises, we highlight the “data crisis”, which could be solved with simple surveillance and notification tools, such as DHIS-2. Despite an absence of robust epidemiological associations between these crises and snakebite incidence, the MSF examples and scoping review publications point towards an increased risk and call for urgent population-based studies. Stakeholders should consider the need for snakebite care and antivenom supply in all humanitarian, migration, and environmental crises. We recommend improving surveillance for snakebite injuries, particularly during conflicts and migration crises, such as those occurring in South Sudan, Central African Republic, Yemen, and Ethiopia.
Funding
None required.
Role of the funding source
None.
Supplementary material
1. Covering letter.
2. PRISMA-ScR checklist.
Handling Editor: Ray Norton
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.toxcx.2021.100089.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abubakar S.B., Habib A.G., Mathew J. Amputation and disability following snakebite in Nigeria. Trop. Doct. 2010;40(2):114–116. doi: 10.1258/td.2009.090266. Epub 2010/03/23. PubMed PMID: 20305111. [DOI] [PubMed] [Google Scholar]
- Alcantara J.A., Bernarde P.S., Sachett J., da Silva A.M., Valente S.F., Peixoto H.M., et al. Stepping into a dangerous quagmire: macroecological determinants of Bothrops envenomings, Brazilian Amazon. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0208532. Epub 2018/12/07. PubMed PMID: 30521617; PubMed Central PMCID: PMCPMC6283637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alirol E., Sharma S.K., Bawaskar H.S., Kuch U., Chappuis F. Snake bite in South Asia: a review. PLoS Neglected Trop. Dis. 2010;4(1):e603. doi: 10.1371/journal.pntd.0000603. Epub 2010/02/04. PubMed PMID: 20126271; PubMed Central PMCID: PMCPMC2811174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alirol E., Lechevalier P., Zamatto F., Chappuis F., Alcoba G., Potet J. Antivenoms for snakebite envenoming: what is in the research pipeline? PLoS Neglected Trop. Dis. 2015;9(9) doi: 10.1371/journal.pntd.0003896. Epub 2015/09/12. PubMed PMID: 26355744; PubMed Central PMCID: PMCPMC4565558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amr Z.S., Abu Baker M.A., Warrell D.A. Terrestrial venomous snakes and snakebites in the Arab countries of the Middle East. Toxicon. 2020;177:1–15. doi: 10.1016/j.toxicon.2020.01.012. Epub 2020/02/01. PubMed PMID: 32001320. [DOI] [PubMed] [Google Scholar]
- Azad S. 2020. The ‘Wild’ Quarantine Centres of Uttarakhand.https://timesofindia.indiatimes.com/city/dehradun/wild-quarantine-centres-of-uttarakhand-how-those-quarantined-in-hills-are-living-under-the-threat-of-leopards-snakes-wild-boars/articleshow/76112585.cms [3 Dec 2021]. Available from: [Google Scholar]
- Bolon I., Mason J., O'Keeffe P., Haeberli P., Adan H.A., Karenzi J.M., et al. One Health education in Kakuma refugee camp (Kenya): from a MOOC to projects on real world challenges. One Health. 2020;10:100158. doi: 10.1016/j.onehlt.2020.100158. Epub 2020/08/28. PubMed PMID: 32844109; PubMed Central PMCID: PMCPMC7439830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown N.I. Consequences of neglect: analysis of the sub-Saharan African snake antivenom market and the global context. PLoS Neglected Trop. Dis. 2012;6(6) doi: 10.1371/journal.pntd.0001670. Epub 2012/06/09. PubMed PMID: 22679521; PubMed Central PMCID: PMCPMC3367979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown N., Landon J. Antivenom: the most cost-effective treatment in the world? Toxicon. 2010;55(7):1405–1407. doi: 10.1016/j.toxicon.2010.02.012. Epub 2010/02/23. PubMed PMID: 20171241. [DOI] [PubMed] [Google Scholar]
- Chippaux J.P. Estimate of the burden of snakebites in sub-Saharan Africa: a meta-analytic approach. Toxicon. 2011;57(4):586–599. doi: 10.1016/j.toxicon.2010.12.022. Epub 2011/01/13. PubMed PMID: 21223975. [DOI] [PubMed] [Google Scholar]
- Cruz L.S., Vargas R., Lopes A.A. Snakebite envenomation and death in the developing world. Ethn. Dis. 2009;19(1 Suppl. 1) S1-42-6. Epub 2009/06/02. PubMed PMID: 19484874. [PubMed] [Google Scholar]
- da Silva Souza A., de Almeida Goncalves Sachett J., Alcantara J.A., Freire M., Alecrim M., Lacerda M., et al. Snakebites as cause of deaths in the western Brazilian amazon: why and who dies? Deaths from snakebites in the amazon. Toxicon. 2018;145:15–24. doi: 10.1016/j.toxicon.2018.02.041. Epub 2018/03/01. PubMed PMID: 29490236. [DOI] [PubMed] [Google Scholar]
- Deuba T. 2020. Youth Dies of Snake-Bite while Staying in Quarantine.https://thehimalayantimes.com/nepal/youth-dies-of-snake-bite-while-staying-in-quarantine [3 Dec 2021]. Available from: [Google Scholar]
- MSF/Doctors Without Borders “The first ten minutes are critical”: treating snakebite in Ethiopia 2019. https://www.msf.org/first-ten-minutes-are-critical-treating-snakebite-ethiopia Available from:
- Ferreira A., Reis V.P.D., Boeno C.N., Evangelista J.R., Santana H.M., Serrath S.N., et al. Increase in the risk of snakebites incidence due to changes in humidity levels: a time series study in four municipalities of the state of Rondônia. Rev. Soc. Bras. Med. Trop. 2020;53 doi: 10.1590/0037-8682-0377-2019. Epub 2020/03/05. PubMed PMID: 32130323; PubMed Central PMCID: PMCPMC7094047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth G.B., Street M., Ramguthy Y., Doedens L. Mortality following snake bite envenomation by Bitis arietans in an HIV positive child: a case report. Medicine (Baltim.) 2016;95(27) doi: 10.1097/MD.0000000000004001. Epub 2016/07/12. PubMed PMID: 27399076; PubMed Central PMCID: PMCPMC5058805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genevieve L.D., Ray N., Chappuis F., Alcoba G., Mondardini M.R., Bolon I., et al. Participatory approaches and open data on venomous snakes: a neglected opportunity in the global snakebite crisis? PLoS Neglected Trop. Dis. 2018;12(3) doi: 10.1371/journal.pntd.0006162. Epub 2018/03/09. PubMed PMID: 29518075; PubMed Central PMCID: PMCPMC5843214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghose A., Faiz A. Snake envenomation in Bangladesh. Clinical Toxinology in Aisa Pacific and Africa. 2015:233–249. [Google Scholar]
- Gutiérrez J.M., Burnouf T., Harrison R.A., Calvete J.J., Kuch U., Warrell D.A., et al. A multicomponent strategy to improve the availability of antivenom for treating snakebite envenoming. Bull. World Health Organ. 2014;92(7):526–532. doi: 10.2471/blt.13.132431. Epub 2014/08/12. PubMed PMID: 25110378; PubMed Central PMCID: PMCPMC4121869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutierrez J.M., Calvete J.J., Habib A.G., Harrison R.A., Williams D.J., Warrell D.A. Snakebite envenoming. Nat. Rev. Dis. Prim. 2017;3:17063. doi: 10.1038/nrdp.2017.63. Epub 2017/09/15. PubMed PMID: 28905944. [DOI] [PubMed] [Google Scholar]
- Habib A.G. Tetanus complicating snakebite in northern Nigeria: clinical presentation and public health implications. Acta Trop. 2003;85(1):87–91. doi: 10.1016/s0001-706x(02)00234-6. Epub 2002/12/31. PubMed PMID: 12505187. [DOI] [PubMed] [Google Scholar]
- Habib A.G. Public health aspects of snakebite care in West Africa: perspectives from Nigeria. J. Venom. Anim. Toxins Incl. Trop. Dis. 2013;19(1):27. doi: 10.1186/1678-9199-19-27. Epub 2013/10/19. PubMed PMID: 24134780; PubMed Central PMCID: PMCPMC3831819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habib A.G., Abubakar S.B. Factors affecting snakebite mortality in north-eastern Nigeria. Int. Health. 2011;3(1):50–55. doi: 10.1016/j.inhe.2010.08.001. Epub 2011/03/01. PubMed PMID: 24038050. [DOI] [PubMed] [Google Scholar]
- Habib A.G., Gebi U.I., Onyemelukwe G.C. Snake bite in Nigeria. Afr. J. Med. Med. Sci. 2001;30(3):171–178. Epub 2003/09/27. PubMed PMID: 14510123. [PubMed] [Google Scholar]
- Habib A.G., Lamorde M., Dalhat M.M., Habib Z.G., Kuznik A. Cost-effectiveness of antivenoms for snakebite envenoming in Nigeria. PLoS Neglected Trop. Dis. 2015;9(1) doi: 10.1371/journal.pntd.0003381. Epub 2015/01/09. PubMed PMID: 25569252; PubMed Central PMCID: PMCPMC4287484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habib Z.G., Salihu A.S., Hamza M., Yakasai A.M., Iliyasu G., Yola I.M., et al. Posttraumatic stress disorder and psycho-social impairment following snakebite in Northeastern Nigeria. Int. J. Psychiatr. Med. 2021;56(2):97–115. doi: 10.1177/0091217420913400. Epub 2020/03/29. PubMed PMID: 32216497. [DOI] [PubMed] [Google Scholar]
- Hernandez M.C., Traynor M., Bruce J.L., Bekker W., Laing G.L., Aho J.M., et al. Surgical considerations for pediatric snake bites in low- and middle-income countries. World J. Surg. 2019;43(7):1636–1643. doi: 10.1007/s00268-019-04953-9. Epub 2019/02/21. PubMed PMID: 30783764. [DOI] [PubMed] [Google Scholar]
- Idoko A., Ikwueke K. Snakebite in the tropics: experience in Makurdi, Nigeria. Trop. Geogr. Med. 1984;36(2):175–180. Epub 1984/06/01. PubMed PMID: 6332397. [PubMed] [Google Scholar]
- Igawe P.B., Muhammad J.O., Nwokoro U.U., Abubakar J.D., Isah S.I., Aketemo U., et al. Snakebite outbreak and associated risk factors in donga, taraba state, Nigeria, June, 2016. Pan Afr. Med. J. 2020;37:82. doi: 10.11604/pamj.2020.37.82.17288. Epub 2020/11/28. PubMed PMID: 33244345; PubMed Central PMCID: PMCPMC7680248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliyasu G., Tiamiyu A.B., Daiyab F.M., Tambuwal S.H., Habib Z.G., Habib A.G. Effect of distance and delay in access to care on outcome of snakebite in rural north-eastern Nigeria. Rural Rem. Health. 2015;15(4):3496. Epub 2015/11/22. PubMed PMID: 26590373. [PubMed] [Google Scholar]
- Karaye K.M., Mijinyawa M.S., Yakasai A.M., Kwaghe V., Joseph G.A., Iliyasu G., et al. Cardiac and hemodynamic features following snakebite in Nigeria. Int. J. Cardiol. 2012;156(3):326–328. doi: 10.1016/j.ijcard.2012.01.098. Epub 2012/02/23. PubMed PMID: 22353439. [DOI] [PubMed] [Google Scholar]
- Laohawiriyakamol S., Sangkhathat S., Chiengkriwate P., Patrapinyokul S. Surgery in management of snake envenomation in children. World J Pediatr. 2011;7(4):361–364. doi: 10.1007/s12519-011-0282-8. Epub 2011/08/31. PubMed PMID: 21877258. [DOI] [PubMed] [Google Scholar]
- Luyckx G., Vanhoenacker F.M., Parizel P.M. Exotic pathology of the hand and foot. A pictorial review. Jbr-btr. 2008;91(4):160–165. Epub 2008/09/27. PubMed PMID: 18817091. [PubMed] [Google Scholar]
- McGain F., Limbo A., Williams D.J., Didei G., Winkel K.D. Snakebite mortality at port moresby general hospital, Papua New Guinea, 1992-2001. Med. J. Aust. 2004;181(11–12):687–691. doi: 10.5694/j.1326-5377.2004.tb06525.x. Epub 2004/12/14. PubMed PMID: 15588214. [DOI] [PubMed] [Google Scholar]
- McNamee D. Tackling venomous snake bites worldwide. Lancet. 2001;357(9269):1680. doi: 10.1016/s0140-6736(00)04868-6. Epub 2001/06/27. PubMed PMID: 11425384. [DOI] [PubMed] [Google Scholar]
- Mekonnen D., Mitiku T., Tamir Y., Azazh A. Snake bite: case series of patients presented to gondar university hospital, north west Ethiopia. Ethiop. Med. J. 2016;54(2):83–86. Epub 2016/08/02. PubMed PMID: 27476228. [PubMed] [Google Scholar]
- Michael G.C., Grema B.A., Aliyu I., Alhaji M.A., Lawal T.O., Ibrahim H., et al. Knowledge of venomous snakes, snakebite first aid, treatment, and prevention among clinicians in northern Nigeria: a cross-sectional multicentre study. Trans. R. Soc. Trop. Med. Hyg. 2018;112(2):47–56. doi: 10.1093/trstmh/try028. Epub 2018/04/05. PubMed PMID: 29617989. [DOI] [PubMed] [Google Scholar]
- Minghui R., Malecela M.N., Cooke E., Abela-Ridder B. WHO's Snakebite Envenoming Strategy for prevention and control. Lancet Global Health. 2019;7(7):e837–e838. doi: 10.1016/S2214-109X(19)30225-6. Epub 2019/05/28. PubMed PMID: 31129124. [DOI] [PubMed] [Google Scholar]
- Mistry A.S., Kohrt B.A., Beecroft B., Anand N., Nuwayhid I. Introduction to collection: confronting the challenges of health research in humanitarian crises. Conflict Health. 2021;15(1):38. doi: 10.1186/s13031-021-00371-8. Epub 2021/05/16. PubMed PMID: 33990200; PubMed Central PMCID: PMCPMC8120248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molesworth A.M., Harrison R., Theakston R.D., Lalloo D.G. Geographic Information System mapping of snakebite incidence in northern Ghana and Nigeria using environmental indicators: a preliminary study. Trans. R. Soc. Trop. Med. Hyg. 2003;97(2):188–192. doi: 10.1016/s0035-9203(03)90115-5. Epub 2003/10/31. PubMed PMID: 14584375. [DOI] [PubMed] [Google Scholar]
- Monteiro F.N., Kanchan T., Bhagavath P., Kumar G.P., Menezes R.G., Yoganarasimha K. Clinico-epidemiological features of viper bite envenomation: a study from Manipal, South India. Singap. Med. J. 2012;53(3):203–207. Epub 2012/03/22. PubMed PMID: 22434296. [PubMed] [Google Scholar]
- Muhammed A., Dalhat M.M., Joseph B.O., Ahmed A., Nguku P., Poggensee G., et al. Predictors of depression among patients receiving treatment for snakebite in general hospital, kaltungo, gombe state, Nigeria: august 2015. Int. J. Ment. Health Syst. 2017;11:26. doi: 10.1186/s13033-017-0132-8. Epub 2017/04/18. PubMed PMID: 28413440; PubMed Central PMCID: PMCPMC5390352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nduagubam O.C., Chime O.H., Ndu I.K., Bisi-Onyemaechi A., Eke C.B., Amadi O.F., et al. Snakebite in children in Nigeria: a comparison of the first aid treatment measures with the world health organization's guidelines for management of snakebite in Africa. Ann. Afr. Med. 2020;19(3):182–187. doi: 10.4103/aam.aam_38_19. Epub 2020/08/22. PubMed PMID: 32820730; PubMed Central PMCID: PMCPMC7694701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolon T. 2020. Snakebites Kill Tens of Thousands of Africans a Year. [Google Scholar]
- WHO & Kofi Annan Foundation. Snakebites in Africa: Challenges and Solutions. WHO; 2016. https://www.who.int/publications/i/item/kaf-snakebites-africa-challenges-solutions Geneva, Switzerland, 13th December, 2016. [Google Scholar]
- Ochoa C., Bolon I., Durso A.M., Ruiz de Castañeda R., Alcoba G., Babo Martins S., et al. Assessing the increase of snakebite incidence in relationship to flooding events. J. Environ. Public Health. 2020;2020:6135149. doi: 10.1155/2020/6135149. [DOI] [Google Scholar]
- Onuaguluchi G.O. Clinical observations on snakebite in Wukari, Nigeria. Trans. R. Soc. Trop. Med. Hyg. 1960;54:265–269. doi: 10.1016/0035-9203(60)90073-0. Epub 1960/05/01. PubMed PMID: 14428895. [DOI] [PubMed] [Google Scholar]
- Petlee P. 3 Dec 2021. After 2,000km Trek Home from Bengaluru, Migrant Dies of Snakebite 2020.https://timesofindia.indiatimes.com/city/bengaluru/after-2000km-trek-home-from-bengaluru-migrant-dies-of-snakebite/articleshow/76146359.cms#:∼:text=BENGALURU%3A%20He%20walked%20a%20gruelling%202%2C000km%20for%2012,to%20wash%20up%20after%20the%20dusty%20journey%20home Available from: [Google Scholar]
- Potet J., Beran D., Ray N., Alcoba G., Habib A.G., Iliyasu G., et al. Access to antivenoms in the developing world: a multidisciplinary analysis. Toxicon X. 2021;12:100086. doi: 10.1016/j.toxcx.2021.100086. Epub 2021/11/18. PubMed PMID: 34786555; PubMed Central PMCID: PMCPMC8578041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashid A., Adnan M.N. Pakistan's refugees face uncertain future. Lancet. 2009;374(9683):13–14. doi: 10.1016/s0140-6736(09)61218-6. Epub 2009/07/09. PubMed PMID: 19585683. [DOI] [PubMed] [Google Scholar]
- Said M., Valdespino E., Baba S.P., Lako R., Malm A., Gonzalez A., et al. Perspectives from MSF snakebite programme implementation in Agok, Abyei region, South Sudan. South Sudan Med. J. 2020;13(4):146–152. [Google Scholar]
- Salou H., Roederer T. Epicentre; 2017. Enquête de mortalité rétrospective et de couverture vaccinale dans la sous-préfecture de Paoua (République Centrafricaine) [Google Scholar]
- Schiermeier Q. Africa braced for snakebite crisis. Nature. 2015;525(7569):299. doi: 10.1038/525299a. Epub 2015/09/19. PubMed PMID: 26381961. [DOI] [PubMed] [Google Scholar]
- Shahi M., Gahatraj R. 3 Dec 2021. Individuals at Quarantine Facilities in Banke Living with Fear of Snakes 2020.https://kathmandupost.com/province-no-5/2020/06/19/individuals-at-quarantine-facilities-in-banke-living-with-fear-of-snakes Available from: [Google Scholar]
- Shiau D.T., Sanders J.W., Putnam S.D., Buff A., Beasley W., Tribble D.R., et al. Self-reported incidence of snake, spider, and scorpion encounters among deployed U.S. military in Iraq and Afghanistan. Mil. Med. 2007;172(10):1099–1102. doi: 10.7205/milmed.172.10.1099. Epub 2007/11/08. PubMed PMID: 17985774. [DOI] [PubMed] [Google Scholar]
- Simpson I.D., Norris R.L. The global snakebite crisis--a public health issue misunderstood, not neglected. Wilderness Environ. Med. 2009;20(1):43–56. doi: 10.1580/08-weme-con-263.1. Epub 2009/04/15. PubMed PMID: 19364169. [DOI] [PubMed] [Google Scholar]
- Snake bite: time to stop the neglect. Lancet. 2010;375(9708):2. doi: 10.1016/s0140-6736(09)62168-1. Epub 2010/01/30. PubMed PMID: 20109839. [DOI] [PubMed] [Google Scholar]
- Steegemans I.M., Sisay K., Nshimiyimana E., Gebrewold G., Piening T., Tessema E.M., et al. 2021. Outcomes and Effectiveness of Antivenom Treatments in Snakebite Patients in North-West Ethiopia: Retrospective Cohort. [Google Scholar]
- Taieb F., Dub T., Madec Y., Tondeur L., Chippaux J.P., Lebreton M., et al. Knowledge, attitude and practices of snakebite management amongst health workers in Cameroon: need for continuous training and capacity building. PLoS Neglected Trop. Dis. 2018;12(10) doi: 10.1371/journal.pntd.0006716. Epub 2018/10/26. PubMed PMID: 30359385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tameru K. Snake bite envenomation at Aysha refugee camp health center. Ethiop. Med. J. 2006;44(1):75–79. Epub 2007/04/24. PubMed PMID: 17447366. [PubMed] [Google Scholar]
- Tauzer E., Borbor-Cordova M.J., Mendoza J., De La Cuadra T., Cunalata J., Stewart-Ibarra A.M. A participatory community case study of periurban coastal flood vulnerability in southern Ecuador. PLoS One. 2019;14(10) doi: 10.1371/journal.pone.0224171. Epub 2019/10/28. PubMed PMID: 31652292; PubMed Central PMCID: PMCPMC6814235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TimesNow. Uttarakhand . 3 Dec 2021. Minor Girl Dies of Snake Bite at a Quarantine Centre in Nainital 2020.https://timesofindia.indiatimes.com/videos/news/uttarakhand-minor-girl-dies-of-snake-bite-at-a-quarantine-centre-in-nainital/videoshow/76032289.cms Available from: [Google Scholar]
- Tomczyk S., Deribe K., Brooker S.J., Clark H., Rafique K., Knopp S., et al. Association between footwear use and neglected tropical diseases: a systematic review and meta-analysis. PLoS Neglected Trop. Dis. 2014;8(11):e3285. doi: 10.1371/journal.pntd.0003285. Epub 2014/11/14. PubMed PMID: 25393620; PubMed Central PMCID: PMCPMC4230915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., Antony J., Zarin W., Strifler L., Ghassemi M., Ivory J., et al. A scoping review of rapid review methods. BMC Med. 2015;13:224. doi: 10.1186/s12916-015-0465-6. Epub 2015/09/18. PubMed PMID: 26377409; PubMed Central PMCID: PMCPMC4574114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oirschot J., Ooms G.I., Waldmann B., Kadam P. Snakebite incidents, prevention and care during COVID-19: global key-informant experiences. Toxicon X. 2021;9:10–100075. doi: 10.1016/j.toxcx.2021.100075. Epub 2021/08/14. PubMed PMID: 34386765; PubMed Central PMCID: PMCPMC8342778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warrell D.A. Venomous bites and stings in the tropical world. Med. J. Aust. 1993;159(11–12):773–779. doi: 10.5694/j.1326-5377.1993.tb141345.x. Epub 1993/12/06. PubMed PMID: 8264466. [DOI] [PubMed] [Google Scholar]
- Williams D.J., Faiz M.A., Abela-Ridder B., Ainsworth S., Bulfone T.C., Nickerson A.D., et al. Strategy for a globally coordinated response to a priority neglected tropical disease: snakebite envenoming. PLoS Neglected Trop. Dis. 2019;13(2) doi: 10.1371/journal.pntd.0007059. Epub 2019/02/23. PubMed PMID: 30789906; PubMed Central PMCID: PMCPMC6383867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World_Health_Organization . 2021. Snakebite Envenoming Factsheet.https://www.who.int/news-room/fact-sheets/detail/snakebite-envenoming [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.