Abstract
Objectives
A high functioning healthcare workforce is a key priority during the COVID-19 pandemic. We sought to determine how work and mental health for healthcare workers changed during the COVID-19 pandemic in a universal healthcare system, stratified by gender factors.
Design
A mixed-methods study was employed. Phase 1 was an anonymous, internet-based survey (7 May–15 July 2020). Phase 2 was semistructured interviews offered to all respondents upon survey completion to describe how experiences may have differed by gender identity, roles and relations.
Setting
National universal healthcare system (Canada).
Participants
2058 Canadian healthcare worker survey respondents (87% women, 11% men, 1% transgender or Two-Spirit), including 783 health professionals, 673 allied health professionals, 557 health support staff. Of the 63 unique healthcare worker types reported, registered nurses (11.5%), physicians (9.9%) and pharmacists (4.5%) were most common. Forty-six healthcare workers were interviewed.
Main outcome measures
Reported pandemic-induced changes to occupational leadership roles and responsibilities, household and caregiving responsibilities, and anxiety levels by gender identity.
Results
Men (19.8%) were more likely to hold pandemic leadership roles compared with women (13.4%). Women (57.5%) were more likely to report increased domestic responsibilities than men (45%). Women and those with dependents under the age of 10 years reported the greatest levels of anxiety during the pandemic. Interviews with healthcare workers further revealed a perceived imbalance in leadership opportunities based on gender identity, a lack of workplace supports disproportionately affecting women and an increase in domestic responsibilities influenced by gender roles.
Conclusions
The COVID-19 pandemic response has important gendered effects on the healthcare workforce. Healthcare workers are central to effective pandemic control, highlighting an urgent need for a gender-transformative pandemic response strategy.
Keywords: mental health, qualitative research, COVID-19, organisation of health services, health services administration & management
Strengths and limitations of this study.
National mixed-methods study that captures a diverse cross-section of healthcare workers in a universal healthcare system.
Only captures perceptions of healthcare workforce during a specific period of time (eg, during the first wave of the COVID-19 pandemic).
Healthcare workers who were too burdened by work demands due to the COVID-19 pandemic may not have been captured in the survey or interview population.
Participants may have been motivated to participate as a result of a previous positive or negative experience related to the COVID-19 pandemic.
Canada is a high-income country with universal healthcare, and the perceptions described by healthcare workers in the study may not be reflective of those of the global healthcare workforce.
Introduction
Sex, gender and COVID-19
The effects of the COVID-19 pandemic differ by sex and gender. Sex refers to the biological attributes of a person, while gender refers to the socially constructed roles, behaviours, expressions and identities of girls, women, boys, men, and gender-diverse people.1 2 Globally, men are at greater risk of critical illness and death due to SARS-CoV-2,3 while women have disproportionately experienced indirect effects of the pandemic, including increased rates of domestic violence, financial insecurity and delayed access to reproductive services.4 5 The gender effects of the pandemic have highlighted the need for greater oversight and scrutiny of direct and indirect consequences of the virus.6
Gender in the healthcare workforce
Maintaining a high-functioning healthcare workforce is a key priority during the COVID-19 pandemic7; understanding the impacts of the pandemic on the healthcare workforce, an essential resource, is of critical importance.8 Previous work has shown gender factors, including gender identity (ie, woman, man, gender-diverse and non-binary), gender roles (ie, norms and behaviours typically associated with gender), gender relations (ie, interactions based on gender) and institutionalised gender (ie, distribution of power, resources and opportunities among genders), influence healthcare workforce readiness for viral outbreaks in other settings.9 However, these gender variables, which are central to the well-being and effectiveness of the healthcare workforce, have not been evaluated or considered in planning COVID-19 containment measures.10
Gender-transformative approaches are required in healthcare to promote equity and equalisation of power and opportunity.11 Recognising that pandemics have the potential to worsen inequity through gendered effects,12 assessing healthcare workers’ perceptions of the COVID-19 pandemic response, stratified by gender factors, is necessary to inform a gender-transformative emergency response.
Methods
The primary objective of this study was to describe healthcare workers’ COVID-19 pandemic experiences and to determine if experiences differed by gender identity and roles, using different strategies of data generation to answer different elements of the main research question. Phase 1—survey: study participation was voluntary and informed consent was obtained electronically at survey initiation. Phase 2—participant interviews: survey participants who consented to a follow-up interview at the end of the survey were contacted via telephone by study investigators up to three times, with a single message and call-back number left if the call went to voicemail. If participants were willing to take part in a semistructured telephone discussion with the study researcher at the time of the call, they provided verbal consent prior to the interview. Gender-sensitive reporting was informed by the Sex and Gender Equity in Research guidelines.13
Phase 1: electronic, cross-sectional survey of the healthcare workforce
Survey development
The survey (online supplemental appendix A) was developed with the aim of describing changes in work roles during the COVID-19 pandemic by healthcare worker gender identity and roles. Survey questions (item generation and reduction) were developed through a combination of literature review and input from 15 interdisciplinary healthcare workers (dietitian, environmental services worker, hospital spiritual care provider, independent practice physician, nurse, occupational therapist, physical therapist, resident physician, social worker, unit clerk). An assessment of face validity, clarity, length and completeness of the survey was performed through semistructured interviews (pretesting) by 10 healthcare workers.
bmjopen-2021-056434supp001.pdf (264.9KB, pdf)
Survey administration
The sampling frame for the survey was the Canadian national healthcare workforce. The survey was available in English, French, simplified and traditional Chinese, Italian and Punjabi. Survey administration was conducted using a snowball sampling technique14 through established Libin Cardiovascular Institute social media outlets (eg, Twitter, Facebook) in addition to email distribution through Canadian national and provincial healthcare societies and unions. The survey (online supplemental appendix A) was disseminated on 7 May 2020 and remained open until 15 July 2020 after the initial email contact, with reminder emails sent up to three times, each at least 2 weeks apart.15 16 Those completing the survey were asked to indicate if they consented to participate in a follow-up telephone interview.
Survey data
Information was collected on participant demographics (age range, sex assigned at birth, gender identity), type of healthcare worker, duration of practice/occupation, pandemic-induced changes to occupational leadership roles and responsibilities, household and caregiving responsibilities, stressors and anxiety levels. Specifically, gender identity was determined by the question ‘What gender do you most identify with on a daily basis?’ (woman, man, transgender woman, transgender man, Two-Spirit, non-binary, gender non-conforming, I prefer to self-describe as (free text), I prefer not to answer). Pre-pandemic and pandemic leadership roles were determined by the questions ‘How would you describe your USUAL work-related leadership role?’ (academic leadership role, healthcare leadership role, academic and healthcare leadership roles, no leadership role) and ‘Have you been asked to take on a new leadership role during the COVID-19 pandemic?’ (yes, no, not sure). Gender roles were determined by the questions ‘Has the COVID-19 pandemic changed the number of hours you spend on childcare activities and/or at home education of children?’; ‘Has the COVID-19 pandemic changed the number of hours you spend on personal caregiving activities for adult dependents?’; ‘Has the COVID-19 pandemic changed the number of hours you spend on household (cooking, cleaning, grocery shopping, etc) activities?’ The responses were categorised by frequency (severely decreased, somewhat decreased, no effect, somewhat increased and severely increased). Where relevant, questions also included an optional comment section for free-text responses. Anxiety levels before and during the pandemic were assessed using the short-form of the State Trait Anxiety Inventory for Adults, reported as a valid and reliable instrument for anxiety assessment.17 18
Data analysis
Healthcare worker types were collapsed into three groups (health professionals, allied health professional and healthcare support staff).19 Characteristics and responses from each healthcare worker group were grouped by self-identified gender identity. Responses were compared across gender identities and healthcare worker type. Data were analysed using descriptive statistics and Pearson Χ2 tests. Further comparisons were made using ordinal logistic and logistic regressions between groups. We used generalised estimating equations to analyse State Trait Anxiety scores across respondents comparing scores before and during the pandemic. We derived a minimum sample size estimate of 400 to allow for point estimates of binary responses to have a 95% CI of ±5%. To ensure sufficient sample size for stratified (eg, gender identity) and regression analyses, we targeted 1000 respondents. To protect the anonymity of respondents, cell sizes with fewer than five respondents were combined into one group.20
Phase 2: interviews of healthcare workers
Interview guide development
Interview guides were developed with the aim of providing a more comprehensive account of healthcare worker experiences during the COVID-19 pandemic and to describe how experiences may have differed by gender identity and roles (online supplemental appendix B). Interview guide development was informed by a review of the existing evidence of healthcare workforce sex and gender considerations in pandemic planning and response, and by the above-described survey. Overarching topics and questions related to healthcare worker experiences, perceptions, behaviours and implications of gender in the COVID-19 pandemic response.
bmjopen-2021-056434supp002.pdf (63.4KB, pdf)
Data collection and analysis
Interviews were conducted by two women researchers (BSM, PH). One researcher conducted interviews with administrators, allied health professionals, environmental services workers and physicians (BSM), and the other researcher conducted interviews with licensed practical nurses and registered nurses (PH). At the time of interviews, BSM had MSc-level training and PH had PhD-level training. Both interviewers were trained in qualitative research methods and had experience conducting interviews. Interviews were conducted via telephone, recorded using an audio recorder and transcribed verbatim. Interviewers conducted interviews from their homes, given work from home mandates during COVID-19. All transcripts had identifying factors removed. Data were analysed using Microsoft Word. Content analysis was used to analyse transcripts as it provides a qualitative analytical method that is well suited to analyse multifaceted, complex and sensitive subjects.21
Two researchers (BSM, PH) developed initial codes of their respective interview transcriptions. Ten per cent of coding was completed in duplicate (BSM, PH). Two researchers (BSM, PH) discussed all codes and generated subthemes and themes through discussion. Higher order subthemes and themes were also discussed with members of research team to confirm final coding (BSM, PH, JH-L and SBA). A saturation of themes or the point at which no new themes arose from the data was obtained within each of the healthcare worker categories. We applied the Consolidated Criteria for Reporting Qualitative Research Checklist22 for reporting our research (online supplemental appendix C).
bmjopen-2021-056434supp003.pdf (145.1KB, pdf)
Role of the funding source
The funding sources had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Patient and public involvement
There was no patient or public involvement in this study.
Results: phase 1
Demographics
There were 2058 Canadian respondents, of which 1789 (86.9%) identified as cisgender women, 218 (10.6%) identified as cisgender men, 17 (0.8%) identified as transgender or Two-Spirit (T2S) (combined as one group to ensure respondent confidentiality). Thirty-four respondents did not disclose their gender. Table 1 summarises respondent demographics. In total, 63 different healthcare worker types were represented in the respondents, the most common types of healthcare worker respondents were registered nurses (11.5%), physicians (9.9%) and pharmacists (4.5%). After grouping healthcare worker types, there were 783 health professionals (87.4% women, 11.9% men, 0.8% T2S), 673 allied health professionals (89.9% women, 9.2% men, 0.9% T2S) and 557 health support staff (88.2% women, 11.0% men, 0.9% T2S). Forty-five respondents did not indicate their healthcare worker type.
Table 1.
Baseline characteristics of all respondents
| All | Health professionals (n=783) |
Allied health professionals (n=673) |
Healthcare support staff (n=557) |
|||||||
| Gender identity | Gender identity | Gender identity | ||||||||
| % women | % men | % T2S | % women | % men | % T2S | % women | % men | % T2S | ||
| Age category (%) | ||||||||||
| 25–30 | 14.92 | 14.47 | 13.98 | 0.00 | 21.32 | 17.74 | 16.67 | 8.76 | 6.56 | 60.00 |
| 31–35 | 15.06 | 19.15 | 20.43 | 16.67 | 14.05 | 8.06 | 16.67 | 11.81 | 13.11 | 20.00 |
| 36–40 | 14.97 | 16.96 | 10.75 | 33.33 | 15.70 | 19.35 | 33.33 | 11.61 | 14.75 | 0.00 |
| 41–45 | 11.76 | 10.09 | 9.68 | 0.00 | 13.06 | 12.9 | 0.00 | 12.63 | 16.39 | 0.00 |
| 46–50 | 11.22 | 11.4 | 9.68 | 0.00 | 9.09 | 12.9 | 16.67 | 13.65 | 8.20 | 20.00 |
| 51–55 | 11.52 | 10.38 | 11.83 | 0.00 | 11.4 | 17.74 | 0.00 | 13.03 | 13.11 | 0.00 |
| 56–60 | 8.89 | 8.77 | 6.45 | 16.67 | 5.95 | 3.23 | 0.00 | 13.85 | 9.84 | 0.00 |
| 61–65 | 5.15 | 4.39 | 10.75 | 16.67 | 2.81 | 1.61 | 0.00 | 7.94 | 11.48 | 0.00 |
| 66–70 | 1.26 | 1.17 | 3.23 | 0.00 | 0.50 | 1.61 | 0.00 | 1.63 | 3.28 | 0.00 |
| <25 years | 3.60 | 2.34 | 0.00 | 0.00 | 5.62 | 4.84 | 0.00 | 3.87 | 3.28 | 0.00 |
| >70 years | 0.39 | 0.29 | 3.23 | 16.67 | 0.00 | 0.00 | 16.67 | 0.20 | 0.00 | 0.00 |
| Practice setting location | 0.00 | 0.58 | 0.00 | 0.00 | 0.50 | 0.00 | 0.00 | 1.02 | 0.00 | 0.00 |
| Years of practice (%) | ||||||||||
| 1–5 | 36.20 | 30.26 | 25.30 | 50.00 | 41.09 | 31.15 | 33.33 | 44.20 | 37.10 | 60.00 |
| 6–10 | 14.14 | 24.51 | 19.28 | 0.00 | 23.27 | 31.15 | 50.00 | 24.85 | 29.03 | 40.00 |
| 11–15 | 7.92 | 15.13 | 7.23 | 0.00 | 14.03 | 6.56 | 16.67 | 15.27 | 19.35 | 0.00 |
| 16–20 | 24.15 | 9.68 | 8.43 | 0.00 | 7.59 | 11.48 | 0.00 | 6.92 | 4.84 | 0.00 |
| >20 | 15.65 | 20.42 | 39.76 | 50.00 | 14.03 | 19.67 | 0.00 | 8.76 | 9.68 | 0.00 |
| Ethnicity/race (%) | ||||||||||
| Black/African/Caribbean | 0.87 | 0.18 | 0.00 | 0.00 | 1.06 | 5.08 | 16.67 | 1.30 | 1.72 | 0.00 |
| East Asian/South Asian/ Southeast Asian | 5.54 | 3.6 | 14.29 | 40.00 | 7.92 | 16.95 | 0.00 | 4.13 | 12.07 | 25.00 |
| Indigenous/Métis | 2.24 | 1.98 | 1.43 | 0.00 | 1.06 | 1.69 | 0.00 | 5.43 | 1.72 | 0.00 |
| Latina/Latino/Latinx | 0.63 | 0.72 | 0.00 | 0.00 | 0.70 | 0.00 | 0.00 | 1.09 | 0.00 | 0.00 |
| Middle Eastern | 0.39 | 0.36 | 1.43 | 0.00 | 0.35 | 1.69 | 0.00 | 0.43 | 0.00 | 0.00 |
| White/Caucasian | 74.44 | 90.09 | 78.57 | 20.00 | 82.75 | 69.49 | 66.67 | 85.22 | 77.59 | 50.00 |
| Prefer not to answer | 4.37 | 3.06 | 0.00 | 40.00 | 6.16 | 0.00 | 16.67 | 2.39 | 0.00 | 25.00 |
| Practice setting location | ||||||||||
| Rural | 11.76 | 42.69 | 25.93 | 0.00 | 27.45 | 43.75 | 0.00 | 56.31 | 28.57 | 0.00 |
| Rural and urban | 5.34 | 11.92 | 18.52 | 0.00 | 22.55 | 31.25 | 0.00 | 17.48 | 42.86 | 0.00 |
| Suburban | 1.17 | 3.46 | 14.81 | 0.00 | 3.43 | 6.25 | 0.00 | 2.91 | 0.00 | 0.00 |
| Suburban and urban | 2.19 | 5.00 | 18.52 | 33.33 | 9.31 | 0.00 | 100 | 3.88 | 14.29 | 0.00 |
| Urban | 10.16 | 36.92 | 22.22 | 66.67 | 37.25 | 18.75 | 0.00 | 19.42 | 14.29 | 100.00 |
T2S, Transgender/Two-Spirit.
Gender identity, gender relations, and pandemic leadership roles and responsibilities
Impact of pandemic on gender relations
To assess the influence of gender on leadership roles both pre-pandemic and during the pandemic, we considered how leadership roles were distributed across healthcare worker groups, stratified by gender identity (table 2). Pre-pandemic, 32.9% of women, 47.3% of men and 37.5% of T2S respondents reported holding a leadership role. During the pandemic, 13.4% of women, 19.8% of men and 12.5% of T2S reported taking on a new leadership role. No level of involvement in pandemic decision-making was reported by 79.4% of women, 72.5% of men, and 76.5% of T2S respondents.
Table 2.
COVID-19 effects of healthcare work responsibilities
| Health professionals | Allied health professionals | Healthcare support staff | |||||||
| Gender identity | Gender identity | Gender identity | |||||||
| % women | % men | % T2S | % women | % men | % T2S | % women | % men | T2S | |
| Time spent on clinical services | |||||||||
| Severely increased | 12.82 | 6.59 | 16.67 | 7.52 | 3.39 | 20.00 | 14.96 | 9.80 | 0.00 |
| Somewhat increased | 30.23 | 20.88 | 33.33 | 19.58 | 28.81 | 0.00 | 23.19 | 25.49 | 25.00 |
| No effect | 21.98 | 26.37 | 16.67 | 26.05 | 35.59 | 60.00 | 39.90 | 41.18 | 25.00 |
| Somewhat decreased | 21.68 | 28.57 | 16.67 | 20.10 | 16.95 | 0.00 | 11.72 | 11.76 | 25.00 |
| Severely decreased | 8.85 | 15.38 | 0.00 | 20.63 | 11.86 | 0.00 | 7.48 | 5.88 | 25.00 |
| Pre-existing leadership role | |||||||||
| Yes (any leadership role) | 46.21 | 52.75 | 66.67 | 27.66 | 53.33 | 0.00 | 20.63 | 55.36 | 40.00 |
| Pandemic leadership role | |||||||||
| Yes | 20.36 | 21.11 | 0.00 | 8.89 | 15.00 | 20.00 | 9.21 | 22.81 | 20.00 |
T2S, Transgender/Two-Spirit.
Impact of pandemic on gender roles
Over half of women respondents (53.5%) reported that childcare responsibilities increased (31.9% severely increased and 21.6% somewhat increased). Comparatively, 32.8% of men (14.9% severely increased and 17.9% somewhat increased) and 33.3% of T2S respondents (33.3% somewhat increased) reported that childcare responsibilities increased (figure 1). Overall, 21.9% of women reported severely (4.3%) or somewhat increased (17.6%) dependent adult responsibilities, compared with 15.0% of men (3.3% severe, 11.7% somewhat). The majority of women (57.5%) reported severely (12.6%) or somewhat increased (44.9%) household responsibilities, compared with 45% of men (6.6% severe, 38.4% somewhat) and 21.4% of T2S respondents (21.4% somewhat). When asked whether the workplace had adapted to home responsibilities, the most frequent response among all participants was ‘not at all’ (58.4% in women; 46.8% in men; 85.7% in T2S).
Figure 1.
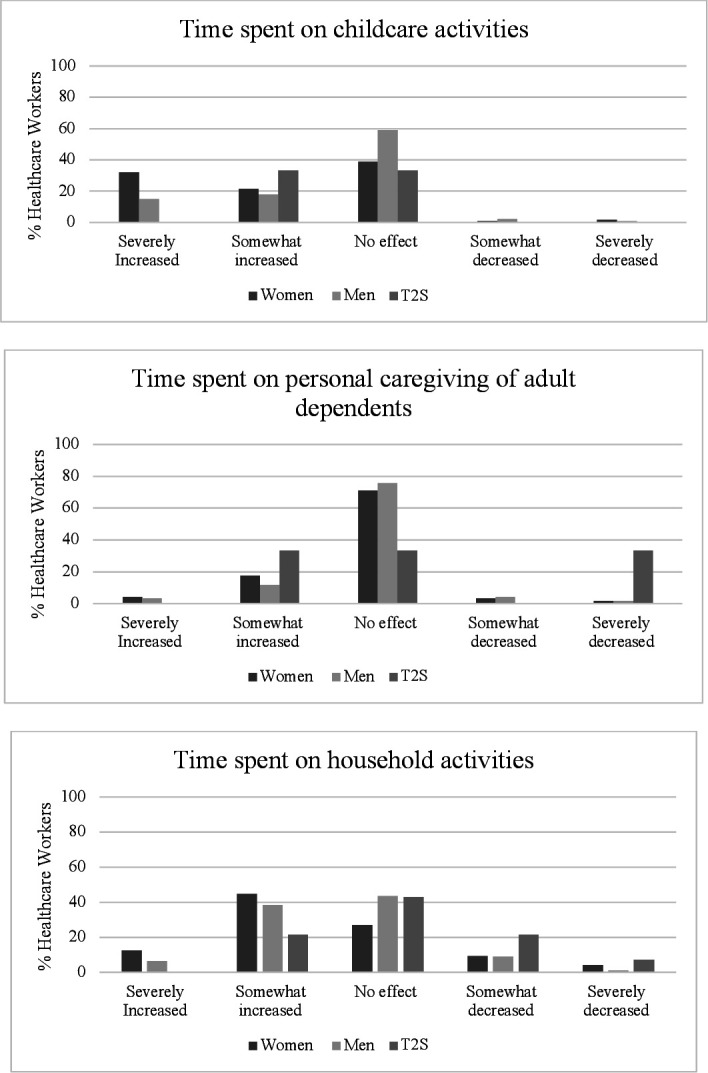
Healthcare workers’ response to levels of domestic responsibility during COVID-19. T2S, transgender or Two-Spirit.
Impact of pandemic on stress levels by gender identity
Responses to each of the six State Trait Anxiety Inventory questions were analysed by gender identity (online supplemental appendix A; Q22; Q23). Reported pre-pandemic stress levels did not differ between women and men; given the low number of T2S respondents, these results are not reported. All respondents were more likely to respond as ‘more anxious’ to each of the six questions on the State Trait Anxiety Inventory during the pandemic versus before the pandemic (p<0.01), and women responded to each of the six questions on the State Trait Anxiety Inventory as ‘significantly more anxious’ more often compared with men (p<0.01). Total scores on the State Trait Anxiety Inventory also indicated both women and men were more anxious during the pandemic versus before the pandemic (p=0.01), importantly, total scores for women indicated they were significantly more anxious during the pandemic than men (p=0.01). While there were no significant differences across healthcare worker types and State Trait Anxiety scores, either pre-pandemic or during the pandemic, those with dependents under the age of 10 years answered each of the six questions as significantly more anxious than those without a dependent under the age of 10 years (p<0.05).
Results: phase 2
Participants
One hundred and ninety-nine participants consented to be contacted, although three did not provide contact information. Ninety-nine participants were contacted. Interviews were conducted with 46 participants, including 26 health professionals (22 women, 4 men), 13 allied health professionals (12 women, 1 man) and 7 healthcare support staff (4 women, 3 men), after which time saturation of themes was reached. Ages ranged from 26 to 66 years. Ten health professionals identified as being in a leadership role, two allied health professionals identified as being in a leadership role and no healthcare support staff reported being in a leadership role. Interview time ranged from 10 to 45 min.
Content analysis of interviews revealed three major themes related to the impact of gender identity, gender roles, and gender relations on leadership roles and stress levels. We provide quotes to illustrate each theme in tables 3–5.
Table 3.
Theme 1 quotations
| Participant ID | Quote |
| HP3, W, NL | ‘And so overall, I think it results in some inequity for women’s health services. Because you have a [Surgery] department that does not understand women’s health or the duality of obstetrics and gynecology, which is very masculine and male dominated department, trying to make decisions for us when we had previously been autonomous. We are our own department. Separate from Medicine and separate from Surgery and so now we are getting more of a paternalistic leadership from the Department of Surgery which has not previously been our, like, our boss.’ |
| HP1, W, NL | ‘…a predominant amount of men submitting papers with very minimal women represented. And I think within research we already have massive gender inequities… Amplified.’ |
| HP4, W, NL | ‘I am not sure if this is a product of COVID or not but I did notice and it might have just been a coincidence, but I did notice an increase of certain male clients that have been known to be a little bit, have a derogatory attitude towards women, I did notice an increase in those behaviours during COVID.’ |
| HP4, W, NL | ‘So, one of my clients who was maybe a little bit more secretive about his attitude towards women and maybe it, just not so overtly misogynistic prior to COVID. You know, during COVID was very dissatisfied with the, the level of care that I was providing, I guess… [he] assumed that a male co-worker who is, actually, like, below me. He assumed that this male co-worker was actually my manager and so, called him assuming that he was my manager and saying that he did not want to work with me anymore and wanted to be assigned a male case manager. And made a lot of derogatory remarks towards me and my practice…’ |
HP, health professional; NL, non-leadership role; W, woman.
Table 4.
Theme 2 quotes
| Participant ID | Quote |
| HP2, W, NL | ‘And, yes we get these mass emails from, like, you know, through our [organisation email] and things that say we are behind you and we support you but it does not really amount to very much…Like, I would love to see an email saying; listen, we know that we are asking you to open up again but we also know that all the summer camps have been cancelled and that a lot of you do not have childcare and we know this. So just returning to normal is not normal. Like, how am I supposed to go to work and work five days a week when I have got three kids at home who are not in school and who are not going to be in camps?’ |
| HP2, W, NL | ‘And as a female physician with small kids, I do not feel like that got supported much at all.’ |
| HP1, W, NL | ‘But there is not really much support provided. Right? Like, other than, like, you take your kid to some random daycare… Like, that might not be perceived to be the best option for certain kids, in certain places, in certain schooling. And some people’s kids have significant learning issues, which is of course again, falling back on the parents to challenge, to deal with…’ |
HP, health professional; NL, non-leadership role; W, woman.
Table 5.
Theme 3 quotes
| Participant ID | Quote |
| HP5, T2S, L | ‘And again, I think because I am in a gendered, a fairly gendered faculty, the disproportionate effect of moving schools home and also delaying funding opportunities and changing funding opportunities and the constantly, again, shifting landscape of what was going on meant that a lot of mothers or women in the sort of sandwich generation where they are caring for seniors as well as children and having to work from home in what is now a very crowded home environment. Ya, I, you would say that it has very disproportionately affected my feminine colleagues.’ |
| HP2, W, NL | ’I think what really struck me is how many women were differentially affected by this whole system by COVID compared to men. In that, like, there were a lot of dual physician families in our department. Inevitably it was the mother who ended being the one having to do a lot of the homeschooling, the meal preparations, the co-ordinating and still working from home. And I think that there was a lot of women feeling really, really overwhelmed in our department. Because again, some of them have small children and if daycares were closed, or closed or, like, childcare was closed. And I think, that yet there are so many of the leadership roles in our department were also women.’ |
| HP1, W, NL | ‘Given that kids were at home because school was cancelled, I observed a lot of my colleagues with children who I believe identify as female, take over, again, roles that people might typically say are “female”. So they started doing, of course, their kids schooling and trying to organize home stuff while still working full time as an essential service. Is not an easy feat.’ |
| HP1, W, NL | ‘I have two elderly parents who we did not want going out, so I had to do all the things that they would normally do for themselves outside of the home… those roles that we take on as female providers. I think just tends to will sort of amplify inequity because I am spending a lot of time doing that so that that means when I am not at work, I am doing those things vs trying to catch up on the research things.’ |
| AHP1, W, NL | ‘…the homeschooling falling mainly on the working mothers and not working fathers. So, in the home, everyone is at home theoretically working from home but most of the childcare and home-schooling was being done by women and not the men. Which was very stressful for the parents that I was connecting to. Which again, mostly mothers that I connect to about treatment for their children. It is much more rare for fathers to be involved in it.’ |
AHP, allied health professional; HP, health professional; L, leadership role; NL, non-leadership role; T2S, transgender or Two-Spirit; W, woman.
Impact of gender identity, gender role and gender relations on leadership role
Theme 1: gendered division in workplace roles, responsibilities and patient relations
Health professionals reported that gender identity and gender relations influenced transitions in leadership during COVID-19, specifying inequities in representation of women. Participants also reported inequities in how women were perceived by patients.
Impact of gender identity, gender role and gender relations on stress levels
Theme 2: lack of workplace supports to address personal stress placed on healthcare workers during COVID-19
Women health professionals felt they were not provided with organisational supports to address their own health needs, which may have been intensified working in direct patient care during a pandemic. Organisational support was also perceived as superficial or lacking when considering supports given to healthcare workers also caring for children during the pandemic.
Theme 3: gender roles influenced an increase in domestic responsibilities
Health professionals and allied health professionals reported that women in the healthcare workforce had a disproportionate increase in caregiving roles and responsibilities as a consequence of the COVID-19 pandemic which was not a factor taken into account by organisational support structures.
Discussion
This mixed-methods study combined a cross-sectional survey and qualitative interviews to describe healthcare workers’ perceptions of the COVID-19 pandemic response, stratified by gender identity and roles. Men respondents reported being more likely to hold pandemic leadership roles. Women reported being more likely to spend increased time caring for children and on household responsibilities during the pandemic compared with men and T2S respondents. Healthcare workers who identified as women and who had dependents under the age of 10 years reported the greatest levels of anxiety during the pandemic. Interviews with healthcare workers further revealed a perceived imbalance in leadership opportunities based on gender identity, a lack of workplace supports which disproportionately affected women and an increase in domestic responsibilities influenced by gender roles.
The World Health Organization declared the novel coronavirus (COVID-19) outbreak a global pandemic on 11 March 2020,23 resulting in emergency response efforts including daycare and school24 closures, shifting responsibility for their provision and other care duties to households. Care roles have been disproportionately assumed by women during the COVID-19 pandemic.25 Women form 70% of the world’s healthcare workforce,26 27 however only a minority serve in leadership positions.28 During COVID-19, women in healthcare experienced increased likelihood of depression, anxiety, stress and insomnia compared with men colleagues.29 As described by Regenold and Vindrola-Padros,30 the feminised burden of care during COVID-19, coupled with conflicting societal expectations of workers and mothers, highlight the urgent need for gender-transformative approaches to support healthcare workers.
Studies examining healthcare workers’ perceptions of ethical and workforce issues in previous pandemic planning have suggested that being a woman, having childcare responsibilities or personal obligations, part-time status and a support staff role were important negative factors in willingness to work,31–33 and during the COVID-19 outbreak women frontline healthcare workers reported greater mental health burden.34 The Ebola and Zika virus health emergencies have highlighted the staggering cost of omitting a gender analysis into preparedness and response efforts.35 Despite evidence from previous pandemics, there is still increased need to approach the management of the COVID-19 pandemic from a gendered lens.31 Though gender identities, roles and relations affect healthcare worker experiences across multiple levels of the health system,9 the majority of global health organisations have ill-defined descriptions of gender, do not address gender in their programmatic policies and lack strategies to guide gender-responsive programming.36
Globally, women hold only 25% of healthcare leadership roles.37 The results of our survey suggest the gender imbalance in healthcare leadership has been perpetuated during the COVID-19 pandemic, with men respondents more likely to report holding a pandemic-specific leadership role. Furthermore, women were more likely to report an increase in time spent on childcare and household responsibilities because of the pandemic compared with men, which may have had a disproportionate impact on leadership opportunities.
Reported anxiety levels were significantly higher in women and respondents with a dependent under the age of 10 years. Qualitative themes identified during interviews align with survey results; women reported increased domestic responsibilities and a lack of workplace support to address personal stress. Increased levels of anxiety may contribute to poor quality of sleep, further diminishing mental health and well-being in women during the COVID-19 pandemic.38 Thus, the gender-based mental health burden faced by healthcare workers39 must be given the same focus as other impacts of pandemic to ensure the continued well-being of the healthcare workforce.
Reports of increased psychological stress and unpaid work among women during COVID-19 are not limited to healthcare workers.12 Women have spent increased time managing extra household work during the pandemic, which has contributed to poor mental health outcomes.40 Additional research employing content analysis to analyse online discussions published on Twitter during the pandemic found decreased joy and increased sadness, fear and disgust among healthcare workers.41 While this research did not stratify by gender factors, conclusions were similar to our work and called for increased mental health support for healthcare workers.
A variety of factors contribute to increased stress, burnout and depression among women healthcare workers during the COVID-19 pandemic, including lack of support and recognition from peers, supervisors and hospital leadership.42 These findings align with our interview findings; specifically, the lack of workplace supports to address gender discrimination from patients and stress caused by increased domestic responsibilities (eg, childcare and household responsibilities). Organisational support has been found to efficiently reduce healthcare worker burnout and may be given in the form of emotional and family-related support to address the increased burden faced by healthcare workers during the COVID-19 pandemic.43
This study has limitations. First, women healthcare workers were over-represented in our study population, though it is important to note that women form the majority of the healthcare workforce.37 Next, the majority of respondents self-identified as white, which limits the extrapolation of results to non-white healthcare workers who have been disproportionately impacted by the COVID-19 pandemic.44 Few respondents identified as a gender minority, which constrained our ability to describe perceptions of the COVID-19 pandemic response for this group of healthcare workers. The limitations of our interviews include sampling bias, in that those who chose to participate may have had more extreme experiences to discuss. Finally, Canada is a high-income country with universal healthcare, and the perceptions described by healthcare workers in the study may not be reflective of those of the global healthcare workforce. However, to the best of our knowledge, this is the first mixed-methods study examining the perceptions of the impact of the COVID-19 pandemic on the healthcare workforce stratified by gender, and the results reported highlight important areas of focus that could improve current and future pandemic responses.
Conclusion
This study suggests important gendered effects in the COVID-19 pandemic response on the healthcare workforce, highlighting the critical importance of incorporation of gender into societal emergency response efforts. Healthcare workers are central to effective pandemic control. Recognising the extent to which a pandemic effort affects healthcare workers differently based on gender is a fundamental step for creating effective and equitable policies and interventions. A gender-transformative strategy is urgently needed to optimise care for people with or at risk of COVID-19 in Canada and worldwide.
Acknowledgments
We gratefully acknowledge Alexa Desjarlais, Jaswinder Mangat, Thérèse Therrien, Jane Liang, David Vickers and Patrick Feng for their contributions, as well as our study participants and healthcare workers everywhere.
Footnotes
Twitter: @ShannonRuzycki, @SofiaAhmedMD
Contributors: BSM and SBA initiated the collaborative project, designed data collection tools, monitored data collection for the whole trial, wrote the statistical analysis plan, cleaned and analysed the data, and drafted and revised the paper. SBA is the guarantor. JH-L and PH designed data collection tools, monitored data collection for the whole trial, analysed the data and revised the draft paper. SMD, KF, IDG, KN, CN, JPL, LP, HP, VR, DR, SMR, RS and HTS designed data collection tools, interpreted the data and revised the draft paper.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by the University of Calgary Conjoint Health Research Ethics Board (ethics ID no. REB20-0584). Participants gave informed consent to participate in the study before taking part.
References
- 1. Government of Canada Canadian Institutes of Health Research . Definitions of sex and gender, 2021. Available: https://cihr-irsc.gc.ca/e/47830.html
- 2. Manandhar M, Hawkes S, Buse K, et al. Gender, health and the 2030 agenda for sustainable development. Bull World Health Organ 2018;96:644–53. 10.2471/BLT.18.211607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jin J-M, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health 2020;8:152. 10.3389/fpubh.2020.00152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wenham C, Smith J, Davies SE, et al. Women are most affected by pandemics - lessons from past outbreaks. Nature 2020;583:194–8. 10.1038/d41586-020-02006-z [DOI] [PubMed] [Google Scholar]
- 5. Wenham C, Smith J, Morgan R, et al. COVID-19: the gendered impacts of the outbreak. Lancet 2020;395:846–8. 10.1016/S0140-6736(20)30526-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smith J. Overcoming the ‘tyranny of the urgent’: integrating gender into disease outbreak preparedness and response. Gender & Development 2019;27:355–69. 10.1080/13552074.2019.1615288 [DOI] [Google Scholar]
- 7. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020;395:1225–8. 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cahan EM, Levine LB, Chin WW. The Human Touch - Addressing Health Care's Workforce Problem amid the Pandemic. N Engl J Med 2020;383:e102. 10.1056/NEJMp2020962 [DOI] [PubMed] [Google Scholar]
- 9. Steege R, Taegtmeyer M, McCollum R, et al. How do gender relations affect the working lives of close to community health service providers? empirical research, a review and conceptual framework. Soc Sci Med 2018;209:1–13. 10.1016/j.socscimed.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 10. van Daalen KR, Bajnoczki C, Chowdhury M, et al. Symptoms of a broken system: the gender gaps in COVID-19 decision-making. BMJ Glob Health 2020;5:e003549. 10.1136/bmjgh-2020-003549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tannenbaum C, Greaves L, Graham ID. Why sex and gender matter in implementation research. BMC Med Res Methodol 2016;16:145. 10.1186/s12874-016-0247-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Azcona G, Bhatt A, Encarnacion J. From insights to action: gender equality in the wake of COVID-19: un women headquarters, 2021. Available: https://www.unwomen.org/sites/default/files/Headquarters/Attachments/Sections/Library/Publications/2020/Gender-equality-in-the-wake-of-COVID-19-en.pdf2021
- 13. Heidari S, Babor TF, De Castro P, et al. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev 2016;1:2. 10.1186/s41073-016-0007-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aday LA, Cornelius LJ. Designing and conducting health surveys: a comprehensive guide. John Wiley & Sons, 2006. [Google Scholar]
- 15. Schleyer TK, Forrest JL. Methods for the design and administration of web-based surveys. J Am Med Inform Assoc 2000;7:416–25. 10.1136/jamia.2000.0070416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fischbacher C, Chappel D, Edwards R, et al. Health surveys via the Internet: quick and dirty or rapid and robust? J R Soc Med 2000;93:356–9. 10.1177/014107680009300705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tluczek A, Henriques JB, Brown RL. Support for the reliability and validity of a six-item state anxiety scale derived from the State-Trait anxiety inventory. J Nurs Meas 2009;17:19–28. 10.1891/1061-3749.17.1.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kassam A, Ellaway R. Acknowledging a holistic framework for learner wellness: the human capabilities approach. Acad Med 2020;95:9–10. 10.1097/ACM.0000000000003026 [DOI] [PubMed] [Google Scholar]
- 19. WHO . Classifying health workers: mapping occupations to the International standard classification: international labour organization, International standard classification of occupations: ISCO-08, 2020. Available: https://www.who.int/hrh/statistics/Health_workers_classification.pdf
- 20. Statistics Canada quality guidelines. Available: https://www150.statcan.gc.ca/n1/pub/12-539-x/steps-etapes/4058325-eng.htm2021
- 21. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci 2013;15:398–405. 10.1111/nhs.12048 [DOI] [PubMed] [Google Scholar]
- 22. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 23. WHO . Listings of WHO’s response to COVID-19, 2021. Available: https://www.who.int/news/item/29-06-2020-covidtimeline2021
- 24. UNESCO . 1.37 billion students now home as COVID-19 school closures expand, Ministers scale up multimedia approaches to ensure learning continuity, 2020. Available: https://en.unesco.org/news/137-billion-students-now-home-covid-19-school-closures-expand-ministers-scale-multimedia2021
- 25. Nesbitt-Ahmed Z, Subrahmanian R. Caring in the time of COVID-19: gender, unpaid care work and social protection, 2020. Available: https://blogs.unicef.org/evidence-for-action/caring-in-the-time-of-covid-19-gender-unpaid-care-work-and-social-protection/2021
- 26. Boniol M, McIsaac M, Xu L. Gender equity in the health workforce: analysis of 104 countries. Working paper 1. Geneva: World Health Organization, 2019. [Google Scholar]
- 27. HRH Global Resource Centre . Resource spotlight: gender and health workforce statistics. Available: https://www.hrhresourcecenter.org/gender_stats.html2021
- 28. Miyamoto I. COVID-19 Healthcare Workers: 70% Are Women. Daniel K. Inouye Asia-Pacific Center for Security Studies, 2020. Available: https://apcss.org/wp-content/uploads/2020/05/Security-nexus-COVID-19-Healthcare-Workers-miyamoto.pdf2021
- 29. Liu S, Yang L, Zhang C, et al. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J Psychiatr Res 2021;137:393–400. 10.1016/j.jpsychires.2021.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Regenold N, Vindrola-Padros C. Gender Matters: A Gender Analysis of Healthcare Workers’ Experiences during the First COVID-19 Pandemic Peak in England. Soc Sci 2021;10:43. 10.3390/socsci10020043 [DOI] [Google Scholar]
- 31. Cowden J, Crane L, Lezotte D, et al. Pre-pandemic planning survey of healthcare workers at a tertiary care children's Hospital: ethical and workforce issues. Influenza Other Respir Viruses 2010;4:213–22. 10.1111/j.1750-2659.2010.00145.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: an integrative review. Prehosp Disaster Med 2012;27:551–66. 10.1017/S1049023X12001331 [DOI] [PubMed] [Google Scholar]
- 33. Aoyagi Y, Beck CR, Dingwall R, et al. Healthcare workers' willingness to work during an influenza pandemic: a systematic review and meta-analysis. Influenza Other Respir Viruses 2015;9:120–30. 10.1111/irv.12310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3:e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Davies SE, Bennett B. A gendered human rights analysis of Ebola and Zika: locating gender in global health emergencies. Int Aff 2016;92:1041–60. 10.1111/1468-2346.12704 [DOI] [Google Scholar]
- 36. Bustreo F, Ponchia AG, Rocco C, et al. Strengthening the transformative potential of gender mainstreaming in global health. EClinicalMedicine 2021;34:100858. 10.1016/j.eclinm.2021.100858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. World Health Organization . Delivered by women, led by men: a gender and equity analysis of the global health and social workforce, 2019. Available: https://apps.who.int/iris/handle/10665/311322
- 38. Guadagni V, Umilta' A, Iaria G. Sleep quality, empathy, and mood during the isolation period of the COVID-19 pandemic in the Canadian population: females and women suffered the most. Front Glob Womens Health 2020;1:585938. 10.3389/fgwh.2020.585938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. López-Atanes M, Pijoán-Zubizarreta JI, González-Briceño JP, et al. Gender-Based analysis of the psychological impact of the COVID-19 pandemic on healthcare workers in Spain. Front Psychiatry 2021;12:692215. 10.3389/fpsyt.2021.692215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Xue B, McMunn A. Gender differences in unpaid care work and psychological distress in the UK Covid-19 lockdown. PLoS One 2021;16:e0247959. 10.1371/journal.pone.0247959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Elyashar A, Plochotnikov I, Cohen I-C, et al. The state of mind of health care professionals in light of the COVID-19 pandemic: text analysis study of Twitter discourses. J Med Internet Res 2021;23:e30217. 10.2196/30217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sriharan A, Ratnapalan S, Tricco AC, et al. Occupational stress, burnout, and depression in women in healthcare during COVID-19 pandemic: rapid scoping review. Front Glob Womens Health 2020;1:596690. 10.3389/fgwh.2020.596690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Morgantini LA, Naha U, Wang H, et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. PLoS One 2020;15:e0238217. 10.1371/journal.pone.0238217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rimmer A. Covid-19: two thirds of healthcare workers who have died were from ethnic minorities. BMJ 2020;369:m1621. 10.1136/bmj.m1621 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056434supp001.pdf (264.9KB, pdf)
bmjopen-2021-056434supp002.pdf (63.4KB, pdf)
bmjopen-2021-056434supp003.pdf (145.1KB, pdf)
Data Availability Statement
Data are available upon reasonable request.


