Abstract
Parrot beak tear is a white-white meniscal injury that often occurs in isolated injuries. Partial meniscectomy for parrot beak tears is often recommended, owing to the avascular zone; however, partial meniscectomy, especially with the lateral meniscus, has a high failure rate for return to sports, leading to residual meniscus extrusion and lateral compartment osteoarthritis. Thus, we have developed a repair technique to preserve the parrot beak tear of the avascular zone. This is a modification of the inside-out repair with additional reduction sutures. We recommend this procedure as a technique for repairing avascular parrot beak tears of the lateral meniscus.
Technique Video
We demonstrate a technique for a parrot beak tear of the lateral meniscus of the avascular zone, in which we present the modification of the inside-out repair with additional reduction sutures and bone marrow-derived fibrin clot, based on “ABCs” theory of meniscal repair: anatomic reduction, biologic augmentation, and circumferential compression across the tear site.
This case involved the right knee of a 21-year-old professional soccer player who had a parrot beak tear of the lateral meniscus.
From the anterolateral portal view, a parrot-beak tear was observed in the lateral meniscus in the figure-four position.
This tear started from the anterior to the posterior portion of the white-white zone of the lateral meniscus. The residual meniscus had a horizontal tear.
After meniscal instability was confirmed by a probe, an arthroscopic rasp was used to freshen the sites of the tears in the meniscus and to promote healing through the anteromedial portal.
Reduction sutures were then placed on the body of the parrot beak tear using a Scorpion suture passer through the anterolateral portal viewing from anteromedial portal.
A NanoPass was inserted into the joint below the anterior horn of lateral meniscus and the reduction suture was retrieved through the capsule in the far anterolateral portal without damaging the articular cartilage of the tibial plateau viewing from anteromedial portal.
We confirm the reduction suture work for this parrot beak tear viewing from anteromedial and anterolateral portal.
The 11-G bone marrow harvest needle was used to harvest 10
mL of bone marrow aspirate from the lateral side of the intercondylar notch of the right knee through the anteromedial portal viewing from the anterolateral portal, which is positioned in the deep flexion position without a tourniquet.
Dual meniscal repair needles loaded with 2-0 braided polyester sutures with clots are inserted into the injured site through a cannula positioned in the anteromedial portal viewing from the anterolateral portal. The suture needles are retrieved under direct visualization through a previously prepared lateral incision. After inserting the clot, needles loaded with 2-0 sutures alone are penetrated through the unstable portion of the meniscus through the anteromedial portal viewing from the anterolateral portal.
Stitches were placed at 3-mm intervals.
The repaired meniscus covers the articular surface of lateral compartment viewing from the anterolateral portal.
Introduction
The meniscus is vital for load-bearing and force distribution in the knee. This is particularly important in the lateral compartment owing to the convexity of the lateral tibial plateau. The lateral meniscus is responsible for ∼70% of the load transmission across the joint. Parrot beak tear is a tear that frequently arises following a traumatic event and is often irreparable, since it involves the avascular zone of the meniscus.1 Parrot beak tears result in mechanically unstable flaps and are associated with mechanical symptoms. Since the meniscus in the avascular zone has limited healing capacity, this pattern of tear requires resection, the so-called partial meniscectomy, to prevent tear propagation since the flap is caught within the joint during flexion. Partial meniscectomy has been the gold standard for surgical treatment of meniscal tears for many years; it is safe with a low rate of complications and reoperation.2 However, meniscectomy affects the knee biomechanics,3 lowers the rate of return to play,4 and with time could lead to osteoarthritis.5 Although it was once believed that meniscal tears in the avascular zone, including parrot beak tears, did not possess the capacity to heal, repair of tears in the avascular zone could be clinically beneficial for young patients.
We present a technique of reduction suture, additional bone marrow-derived fibrin clot, and inside-out repair to reapproximate the lateral meniscus for parrot beak tears, based on “ABCs” theory of meniscal repair: anatomic reduction, biologic augmentation, and circumferential compression across the tear site.6
Surgical Technique
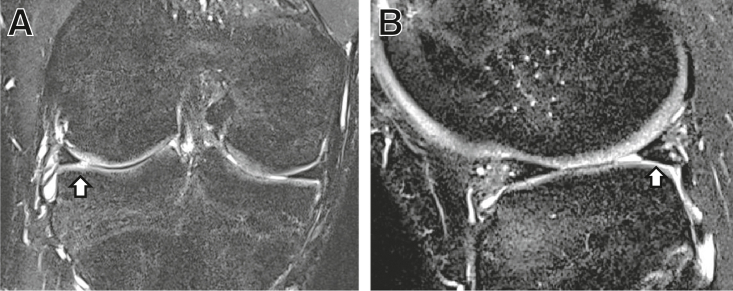
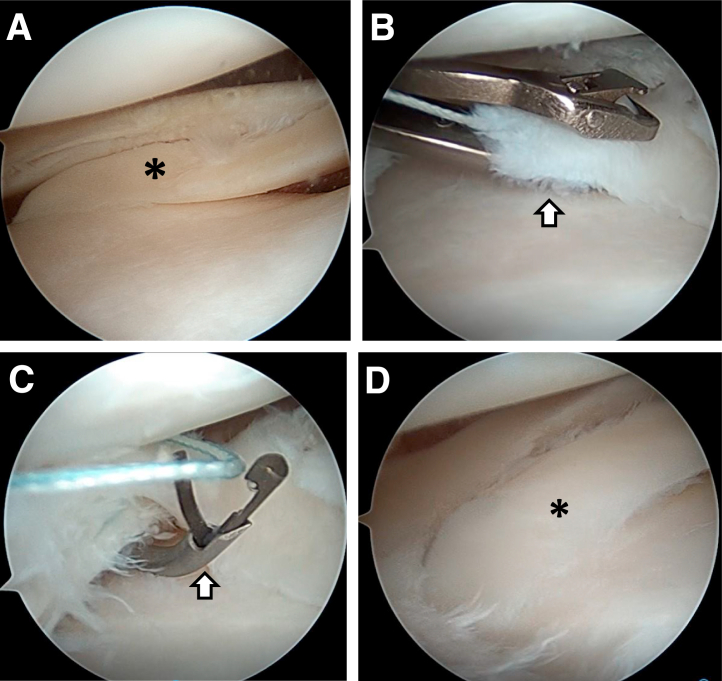
This technique is indicated for parrot beak tear of the lateral meniscus, which presents a blunted meniscus on the coronal image (Fig 1A) and inferiorly displaced meniscal fragment with a downward-curved “comma” appearance on the sagittal image (Fig 1B) on the magnetic resonance image (MRI).7 With the patient in a supine position, a nonsterile tourniquet was applied to the upper thigh of the operated leg. Arthroscopic evaluation was performed using anteromedial and anterolateral portals (Fig 2A, Video 1). The knee was placed in a figure-of-4 position to open the lateral compartment. An arthroscopic rasp was used to freshen the sites of tears in the meniscus, thus promoting healing. Reduction sutures with 2-0 FiberWire (Arthrex, Naples, FL) were subsequently placed on the body of the parrot beak tear using a Scorpion suture passer (Arthrex) through the anterolateral portal (Fig 2B, Video 1). The anteromedial portal was used for visualization. The number of reduction sutures required is based on the tear morphology and the degree of retraction. A NanoPass (Stryker, Kalamazoo, MI) was inserted into the joint below the meniscus, and the reduction suture was retrieved through the capsule in the distant anterolateral portal without damaging the articular cartilage of the tibial plateau (Fig 2C, Video 1). Reduction of the parrot beak tear was observed on pulling the reduction sutures (Fig 2D, Video 1).
Fig 1.
Coronal (A) and sagittal (B) magnetic resonance imaging of parrot beak tear of the lateral meniscus of the right knee. (A) Coronal T2-weighted magnetic resonance image showing a blunted meniscus of mid body (white arrow). (B) Sagittal T2-weighted magnetic resonance image showing an inferiorly displaced meniscal fragment with a downward-curved “comma” appearance (white arrow).
Fig 2.
Setting of reduction suture and reduction of parrot beak tear of the right knee in the figure-four position. (A) parrot beak tear (black asterisk) is observed in the lateral meniscus from the lateral portal view of the right knee. (B) Reduction sutures with 2-0 FiberWire are placed to the body of parrot beak tear using a Scorpion suture passer (white arrow) through the anterolateral portal from anteromedial portal view. (C) NanoPass (white arrow) is inserted into the joint below the anterior horn of lateral meniscus though the capsule in the far anterolateral portal without damaging the articular cartilage of the tibial plateau from anteromedial portal view. (D) Parrot beak tear is reduced to anatomical position (black asterisk) after pulling the reduction suture from the anterolateral portal view.
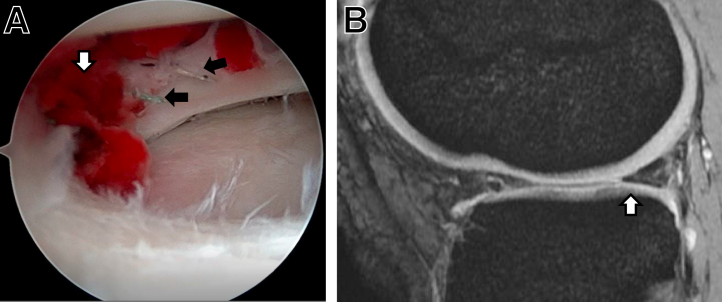
To prepare the bone marrow aspirate (BMA)-derived fibrin clot, an 11-G Bone Marrow Harvest Needle (Argon Medical Device, TX) was used to harvest 10 mL of BMA from the lateral side of the intercondylar notch of the knee joint (Video 1), which was positioned in the flexion position without a tourniquet (Fig 3, A and B). BMA was placed in a sterile glass container dish and slowly stirred with a glass rod. Clots began to develop in the dish within 5–10 min and were separated from the post-clot serum. The fibrin clot was picked up from the dish and carefully placed on gauze. After the clot was cut into several pieces with a size of 4 mm, a 2-0 braided polyester suture (Stryker, Kalamazoo, MI) was stitched to each end of the clot for subsequent intraarticular introduction (Fig 3C). The skin incision was parallel to and just posterior to the lateral collateral ligament with the knee in 90° flexion for a standard inside-out meniscal repair. The fascia was exposed and cut immediately posterior to the lateral collateral ligament. A retractor (Stryker, Kalamazoo, MI) was inserted into the interval between the lateral posterior capsule and the gastrocnemius to protect the neurovascular structures behind the knee. Once the retractor was in place, the meniscal repair was performed through the anteromedial portal in the figure-of-four-leg lock position. Following the dual meniscal repair, needles loaded with 2-0 braided polyester sutures with clots were inserted into the injured site (Fig 3D, Video 1), needles loaded with 2-0 sutures alone were penetrated through the unstable portion of the meniscus through a cannula (Stryker, Kalamazoo, MI) positioned in the anteromedial portal. The suture needles were retrieved under direct visualization through the previously prepared lateral incision. The sutures were tied over the capsule after every four sutures were passed. The technique was performed with stitches placed at intervals of at least 3 mm using 2-0 nonabsorbable sutures (Fig 4A, Video 1). The reduction suture was tied at the capsule after finishing the repair using the inside-out technique. After repairing the parrot beak tear, the stability of the meniscus was confirmed by probing.
Fig 3.
Aspiration, preparation, and placing of bone marrow-derived fibrin clot. (A) 11-G Bone marrow harvest needle (white arrow) is used to harvest 10 mL of bone marrow aspirate (BMA) from the lateral side of the intercondylar notch of the knee joint through the anteromedial portal of the right knee, which is positioned in the deep flexion position without a tourniquet. (B) Arthroscopic view of harvesting the BMA with 11-G bone marrow harvest needle (white arrow) from the lateral side of the intercondylar notch of the knee viewing from the anterolateral portal of the right knee (C) after clot is cut into several pieces, a 2-0 braided polyester suture is stitched to each end of the clot (white arrow) for subsequent intraarticular introduction. (D) The dual meniscal repair needles loaded with 2-0 braided polyester sutures with clot are inserted in the injured site (white arrow) through the anteromedial portal viewing from the anterolateral portal of the right knee.
Fig 4.
Arthroscopic findings following meniscal repair (A) and postoperative magnetic resonance imaging (B). (A) Stitches placed at least 3-mm intervals (black arrows) are performed using 2-0 nonabsorbable sutures from the anterolateral view of the right knee. White arrow: bone marrow-derived fibrin clot. (B) Postoperative sagittal magnetic resonance imaging reveals the diminishing of the comma sign, which indicates that the dislocated parrot beak tear is reduced to the anatomical position (white arrow) of the lateral meniscus of right knee.
In the present study, the patients were immobilized for 1 week using a brace, limited to a knee range of motion of 0° to 90° for 3 weeks, and then allowed protected weight-bearing for 8 weeks. They were permitted to jog and return to previous sports at 4 and 8 months, respectively following the surgery. Postoperative MRI revealed a diminishing of the comma sign, indicating the reduction of the dislocated parrot beak tear into anatomical position (Fig 4B); therefore, this method can restore the normal meniscal morphology of parrot beak tears.
Discussion
Parrot beak flap tears are oblique tears of the meniscus thought to originate as a central radial tear and propagate longitudinally toward the periphery, generating a partially detached unstable fragment that can subsequently displace into the meniscal recess.7 The coined “meniscal comma sign” represents the MRI finding of an inferiorly displaced vertical flap tear, also known as a parrot beak tear, of the meniscus into the meniscotibial recess. Conversely, this unstable flap and the parrot beak tears are more likely to respond well to surgical treatment with arthroscopic partial meniscectomy due to their distinct preoperative mechanical symptoms. However, the changes in joint motion and meniscal forces observed following even small partial lateral meniscectomies may predispose the knees to further injury.3 For athletes, lateral meniscectomy has a higher incidence of adverse events in the early recovery period, including pain/swelling and the need for further arthroscopy.4 The amount of resection is directly related to the degree of radiographic osteoarthritis.5 Biologic augmentation strategies, including bone marrow stimulation, the use of fibrin clots, and platelet-rich plasma injections for the avascular zone, attempt to promote chemotaxis, cellular proliferation, and/or matrix production at the site of meniscal repair to help overcome healing limitations.6 Krych et al.6 described the importance of the “ABCs” of meniscal repair: anatomic reduction, biologic augmentation, and circumferential compression across the tear site in order to maximize healing potential. This technique for parrot beak tear is characterized by techniques based on the “ABCs” of meniscal repair, reduction suture, additional bone marrow-derived fibrin clot, and inside-out repair to reapproximate the meniscus (Table 1). BMA is a strategy developed and used for tissue regeneration. Similar to peripheral blood-derived fibrin clots, BMA clots are easily prepared from BMA and had significantly higher levels of cytokines compared to peripheral blood-derived clots from the intercondylar notch of the knee joint, and the rates of clinical failure following meniscal repair with a BMA clot for isolated avascular meniscal injury were 10%.8 Thus, BMA clots obtained from the knee may be a superior adjuvant in promoting healing of the meniscal tissue compared to peripheral blood clots. Inside-out repair is a gold standard and cost-effective technique that allows anatomical reduction of the torn meniscus. The strong fixation results in a low clinical failure rate with equivalent healing on MRI compared to all-inside repair. Disadvantages of the inside-out technique include suture passage through the posterior capsule, resulting in possible neurovascular injury and postoperative knee stiffness. However, for parrot beak tears, the inside-out technique with a thin needle is considered a superior method compared to all-inside techniques since the parrot beak portion is very thin and weak for repair with all-inside techniques (Table 2). This is a preliminary report, and further follow-up assessing the clinical and radiologic outcomes is necessary to investigate the long-term effects of this technique.
Table 1.
Advantages and Limitations of the Procedure
| Advantages | Limitations |
|---|---|
| Standard meniscal repair skills needed | Possibility of reinjury following meniscal stabilization owing to the avascular zone |
| Preserves and stabilizes the parrot beak tear of avascular zone | Possible neurovascular injury, postoperative knee stiffness with inside-out technique |
| Provides reduction suture to maintain the anatomical position of parrot beak tear | Common complications of the arthroscopic meniscal repair include infection and deep vein thrombosis. |
| Growth factors are derived from the bone marrow derived fibrin clot, which promote cellular infiltration and healing. | Special instrumentation required |
| Clot preparation and delivery technique are simple. | Challenging technique |
| Additional tissue harvesting is not needed. |
Table 2.
Pearls and Pitfalls of the Procedure
| Pearls | Pitfalls |
|---|---|
| Careful evaluation of the meniscal volume should be performed to penetrate the reduction suture. | Improper suture management, resulting in suture entanglement and difficult suture tying |
| Enough tension to reduce the parrot beak with reduction suture | Inadequate fibrin clot introduction into the tear |
| Rapid and strong aspiration of bone marrow is needed owing to easy coagulation. | Inadequate suture knot tension resulting in gapped repair |
| Tourniquet is not necessary during aspiration. | Strong aspiration is needed for enough amount of bone marrow aspirate. |
| Immediate exogenous fibrin clot development to be performed on the back table | Sometimes slow aspiration causes bone marrow to become coagulated and no longer can be aspirated. |
| The blood is stirred in the sterile glass container dish within 10 min. | There are individual differences in the amount of the fibrin clot. |
| Inside-out technique is the easiest for placement of the fibrin clot. | Inadequate chondral clearance for suture passing may result in iatrogenic chondral injury. |
| During meniscal repair with inside-out technique, reduction suture should always be tensioned to maintain the anatomical position. | Careful retraction should be performed to protect the neurovascular structures behind the knee during inside-out technique. |
| Reduction suture is tied at the capsule following finishing repair with inside-out technique. | Inside-out technique is performed with a thin needle, so not all inside-out technique devices are recommended, since the parrot beak portion is considered thin and weak. |
| Placement of more sutures is required for increased stability. |
Acknowledgment
We thank Editage (www.editage.com) for the English language editing.
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
We demonstrate a technique for a parrot beak tear of the lateral meniscus of the avascular zone, in which we present the modification of the inside-out repair with additional reduction sutures and bone marrow-derived fibrin clot, based on “ABCs” theory of meniscal repair: anatomic reduction, biologic augmentation, and circumferential compression across the tear site.
This case involved the right knee of a 21-year-old professional soccer player who had a parrot beak tear of the lateral meniscus.
From the anterolateral portal view, a parrot-beak tear was observed in the lateral meniscus in the figure-four position.
This tear started from the anterior to the posterior portion of the white-white zone of the lateral meniscus. The residual meniscus had a horizontal tear.
After meniscal instability was confirmed by a probe, an arthroscopic rasp was used to freshen the sites of the tears in the meniscus and to promote healing through the anteromedial portal.
Reduction sutures were then placed on the body of the parrot beak tear using a Scorpion suture passer through the anterolateral portal viewing from anteromedial portal.
A NanoPass was inserted into the joint below the anterior horn of lateral meniscus and the reduction suture was retrieved through the capsule in the far anterolateral portal without damaging the articular cartilage of the tibial plateau viewing from anteromedial portal.
We confirm the reduction suture work for this parrot beak tear viewing from anteromedial and anterolateral portal.
The 11-G bone marrow harvest needle was used to harvest 10
mL of bone marrow aspirate from the lateral side of the intercondylar notch of the right knee through the anteromedial portal viewing from the anterolateral portal, which is positioned in the deep flexion position without a tourniquet.
Dual meniscal repair needles loaded with 2-0 braided polyester sutures with clots are inserted into the injured site through a cannula positioned in the anteromedial portal viewing from the anterolateral portal. The suture needles are retrieved under direct visualization through a previously prepared lateral incision. After inserting the clot, needles loaded with 2-0 sutures alone are penetrated through the unstable portion of the meniscus through the anteromedial portal viewing from the anterolateral portal.
Stitches were placed at 3-mm intervals.
The repaired meniscus covers the articular surface of lateral compartment viewing from the anterolateral portal.
References
- 1.Salem H.S., Carter A.H., Shi W.J., et al. The meniscal comma sign: Characterization and treatment of a displaced fragment in the meniscotibial recess. Orthopedics. 2018;41:e442–e444. doi: 10.3928/01477447-20180501-01. [DOI] [PubMed] [Google Scholar]
- 2.Smoak J.B., Matthews J.R., Vinod A.V., Kluczynski M.A., Bisson L.J. An up-to-date review of the meniscus literature: A systematic summary of systematic reviews and meta-analyses. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120950306. :2325967120950306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Novaretti J.V., Lian J., Patel N.K., et al. Partial lateral meniscectomy affects knee stability even in anterior cruciate ligament-intact knees. J Bone Joint Surg Am. 2020;102:567–573. doi: 10.2106/JBJS.19.00712. [DOI] [PubMed] [Google Scholar]
- 4.Nawabi D.H., Cro S., Hamid I.P., Williams A. Return to play after lateral meniscectomy compared with medial meniscectomy in elite professional soccer players. Am J Sports Med. 2014;42:2193–2198. doi: 10.1177/0363546514540271. [DOI] [PubMed] [Google Scholar]
- 5.Chahla J., Cinque M.E., Godin J.A., et al. Meniscectomy and resultant articular cartilage lesions of the knee among prospective National Football League players: An imaging and performance analysis. Am J Sports Med. 2018;46:200–207. doi: 10.1177/0363546517737991. [DOI] [PubMed] [Google Scholar]
- 6.Woodmass J.M., LaPrade R.F., Sgaglione N.A., Nakamura N., Krych A.J. Meniscal repair: Reconsidering indications, techniques, and biologic augmentation. J Bone Joint Surg Am. 2017;99:1222–1231. doi: 10.2106/JBJS.17.00297. [DOI] [PubMed] [Google Scholar]
- 7.Bassett A.J., Hadley C.J., Tjoumakaris F., Freedman K.B. The meniscal grammar signs: Comma and apostrophe signs for characterization of a displaced fragment in the meniscal recess. Arthrosc Tech. 2019;8:e727–e732. doi: 10.1016/j.eats.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashimoto Y, Nishino K, Orita K, et al. Biochemical characteristics and clinical result of bone marrow-derived fibrin clot for repair of isolated meniscal injury in the avascular zone. Arthroscopy In press. doi: 10.1016/j.arthro.2021.05.026. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We demonstrate a technique for a parrot beak tear of the lateral meniscus of the avascular zone, in which we present the modification of the inside-out repair with additional reduction sutures and bone marrow-derived fibrin clot, based on “ABCs” theory of meniscal repair: anatomic reduction, biologic augmentation, and circumferential compression across the tear site.
This case involved the right knee of a 21-year-old professional soccer player who had a parrot beak tear of the lateral meniscus.
From the anterolateral portal view, a parrot-beak tear was observed in the lateral meniscus in the figure-four position.
This tear started from the anterior to the posterior portion of the white-white zone of the lateral meniscus. The residual meniscus had a horizontal tear.
After meniscal instability was confirmed by a probe, an arthroscopic rasp was used to freshen the sites of the tears in the meniscus and to promote healing through the anteromedial portal.
Reduction sutures were then placed on the body of the parrot beak tear using a Scorpion suture passer through the anterolateral portal viewing from anteromedial portal.
A NanoPass was inserted into the joint below the anterior horn of lateral meniscus and the reduction suture was retrieved through the capsule in the far anterolateral portal without damaging the articular cartilage of the tibial plateau viewing from anteromedial portal.
We confirm the reduction suture work for this parrot beak tear viewing from anteromedial and anterolateral portal.
The 11-G bone marrow harvest needle was used to harvest 10
mL of bone marrow aspirate from the lateral side of the intercondylar notch of the right knee through the anteromedial portal viewing from the anterolateral portal, which is positioned in the deep flexion position without a tourniquet.
Dual meniscal repair needles loaded with 2-0 braided polyester sutures with clots are inserted into the injured site through a cannula positioned in the anteromedial portal viewing from the anterolateral portal. The suture needles are retrieved under direct visualization through a previously prepared lateral incision. After inserting the clot, needles loaded with 2-0 sutures alone are penetrated through the unstable portion of the meniscus through the anteromedial portal viewing from the anterolateral portal.
Stitches were placed at 3-mm intervals.
The repaired meniscus covers the articular surface of lateral compartment viewing from the anterolateral portal.
We demonstrate a technique for a parrot beak tear of the lateral meniscus of the avascular zone, in which we present the modification of the inside-out repair with additional reduction sutures and bone marrow-derived fibrin clot, based on “ABCs” theory of meniscal repair: anatomic reduction, biologic augmentation, and circumferential compression across the tear site.
This case involved the right knee of a 21-year-old professional soccer player who had a parrot beak tear of the lateral meniscus.
From the anterolateral portal view, a parrot-beak tear was observed in the lateral meniscus in the figure-four position.
This tear started from the anterior to the posterior portion of the white-white zone of the lateral meniscus. The residual meniscus had a horizontal tear.
After meniscal instability was confirmed by a probe, an arthroscopic rasp was used to freshen the sites of the tears in the meniscus and to promote healing through the anteromedial portal.
Reduction sutures were then placed on the body of the parrot beak tear using a Scorpion suture passer through the anterolateral portal viewing from anteromedial portal.
A NanoPass was inserted into the joint below the anterior horn of lateral meniscus and the reduction suture was retrieved through the capsule in the far anterolateral portal without damaging the articular cartilage of the tibial plateau viewing from anteromedial portal.
We confirm the reduction suture work for this parrot beak tear viewing from anteromedial and anterolateral portal.
The 11-G bone marrow harvest needle was used to harvest 10
mL of bone marrow aspirate from the lateral side of the intercondylar notch of the right knee through the anteromedial portal viewing from the anterolateral portal, which is positioned in the deep flexion position without a tourniquet.
Dual meniscal repair needles loaded with 2-0 braided polyester sutures with clots are inserted into the injured site through a cannula positioned in the anteromedial portal viewing from the anterolateral portal. The suture needles are retrieved under direct visualization through a previously prepared lateral incision. After inserting the clot, needles loaded with 2-0 sutures alone are penetrated through the unstable portion of the meniscus through the anteromedial portal viewing from the anterolateral portal.
Stitches were placed at 3-mm intervals.
The repaired meniscus covers the articular surface of lateral compartment viewing from the anterolateral portal.