Several preclinical and clinical studies have demonstrated a key role of the CCL5/CCR5 axis in cancer, providing the rationale for clinical trials with the CCR5 antagonist maraviroc.1 Indeed, maraviroc, approved by the Food and Drug Administration as an antiretroviral for the treatment of human immunodeficiency virus infections, has been repurposed as a potential therapeutic option for cancer treatment since it was demonstrated to inhibit tumor growth, metastasis formation, and the creation of a tumor-promoting microenvironment (TME).2,3 In breast cancer, CCR5+ tumor cells are characterized by increased levels of DNA repair genes and maraviroc enhanced both the cell killing and the DNA damage mediated by the DNA-damaging agent doxorubicin.4
Tumor cells from classical Hodgkin lymphoma (cHL) (the Hodgkin and Reed-Sternberg cells, HRS) secrete CCL5,5 and express a functional CCR5 receptor,6 and patients with high CCL5 levels have a poor prognosis.5 CCR5 is activated in both autocrine6 and paracrine5 manners by CCR5-ligands secreted by HRS cells, monocytes and cHL-mesenchymal stromal cells (MSC). Maraviroc decreases HRS cell growth in vitro and in tumor xenografts, synergizes with doxorubicin and brentuximab vedotin and decreases the self aggregation of HRS cells, monocytes and MSC in three-dimensional (3D) heterospheroids, used as an in vitro model to study the TME.5
Trabectedin covalently binds DNA, blocking transcription and interfering with DNA repair, and modifies the TME by selectively reducing tumor-associated macrophages.7 Its anticancer activities have been demonstrated in solid tumors and in preclinical models of hematologic malignancies.8 In cHL, trabectedin induces a potent in vitro antitumor activity, decreases cytokine levels and viability of heterospheroids formed by HRS cells and MSC, and inhibits tumor xenograft growth, monocyte infiltration and angiogenesis.9
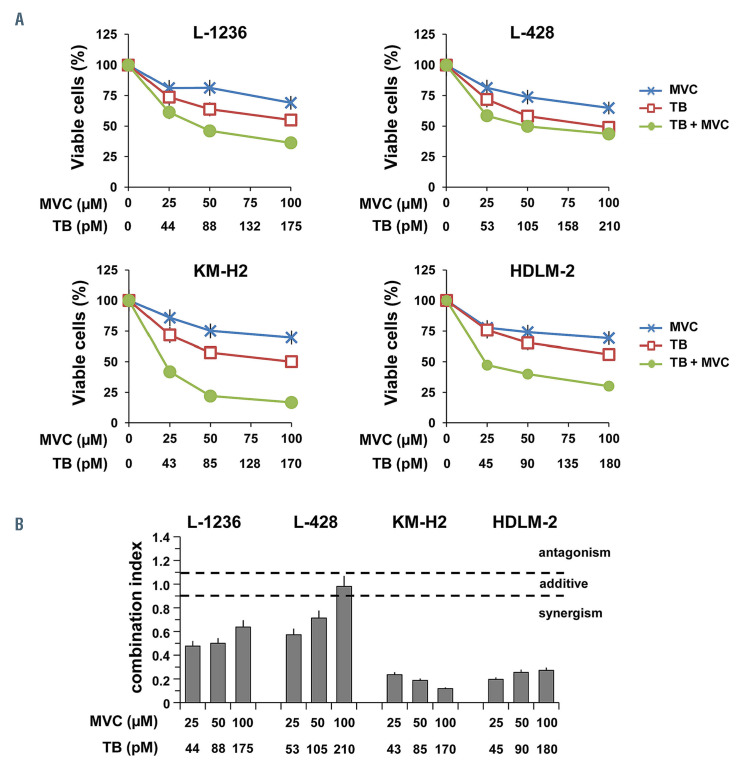
Figure 1.
Maraviroc synergized with trabectedin in Hodgkin and Reed-Sternberg cells. L-1236, L-428, KM-H2 and HDLM-2 cells (2.0x105 cells/mL), were exposed to increasing concentrations of maraviroc, trabectedin and their combination. (A) After 72 h cell viability was evaluated by trypan blue dye exclusion. Results (percentage of control) are mean and standard deviation of three independent experiments each run in triplicate. (B) Synergy was determined using Calcusyn software. Values of bar charts are mean combination index values and standard deviation of three experiments each run in triplicate. MVC: maraviroc; TB: trabectedin.
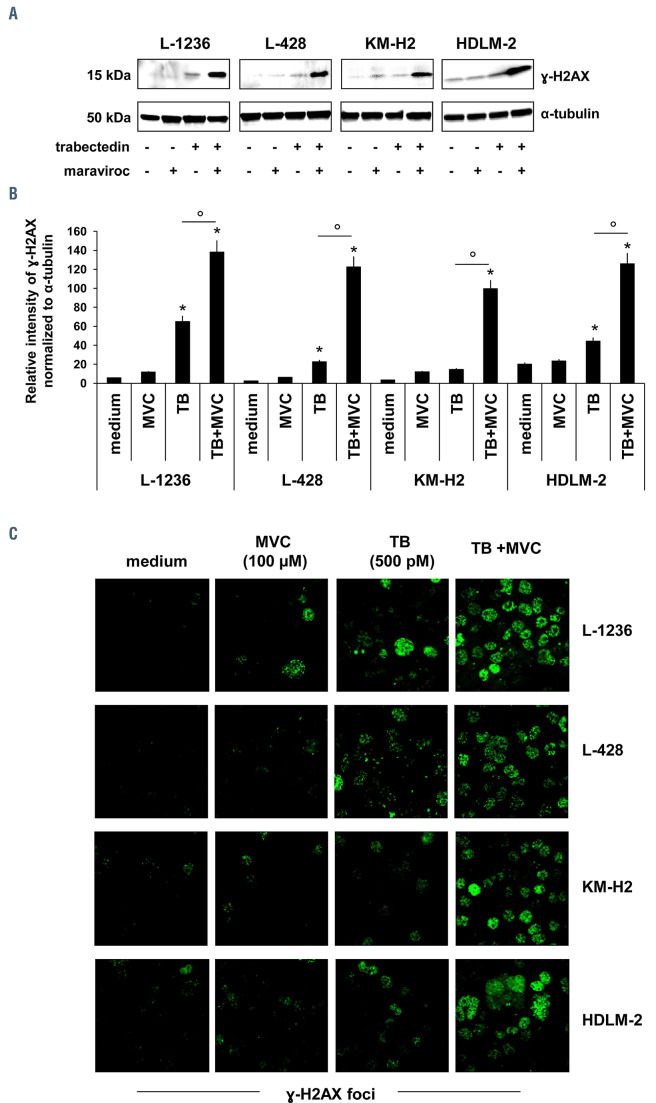
Figure 2.
Maraviroc enhanced DNA damage induced by trabectedin. Hodgkin and Reed-Sternberg (HRS) cells were treated with maraviroc (100 mM), trabectedin (500 pM) and their combination for 24 h. (A) Western blot for g-H2AX and a-tubulin protein expression in cHL cell lines. Membrane strips were incubated with mouse anti-phospho-histone H2A.X (Ser139) (clone JBW301) (Millipore) and mouse anti-a-tubulin antibody clone B-5-1-2 (Sigma Aldrich) and revealed with donkey anti-mouse IgG (H+L chain) A90-137P (Bethyl Laboratories). Images were acquired using a ChemiDoc XRS system (Bio-Rad). Data are representative of four experiments. (B) Bar charts showing densitometric analysis of g-H2AX expression normalized to a-tubulin as a loading control. Protein quantification was performed using ImageJ software. Values are means and standard deviation of four experiments. *P<0.05, treatments vs. control, One-way analysis of variance followed by the Dunnett test. °P<0.05, trabectedin vs. trabectedin and maraviroc in combination, Student t-test. (C) Immunofluorescence images (confocal microscopy) of g-H2AX foci after drug treatment. HRS cells adherent to coverslips, were fixed, permeabilized and incubated with anti-phospho-histone H2A.X (Ser139) (clone JBW301) (Millipore), followed by Alexa Fluor-488 anti-mouse secondary antibody (Thermo Scientific). Images were acquired with a Leica TCS SP8 Confocal system (Leica Microsystems Heidelberg, Mannheim, Germany), using Leica Confocal Software (LCS). MVC: maraviroc; TB: trabectedin.
Considering that HRS cells express a functional CCR5 receptor and maraviroc synergizes with doxorubicin and affects TME interactions,5 our hypothesis is that this CCR5 antagonist, by promoting DNA damage and disrupting the cross-talk between tumor cells and MSC in 3D heterospheroids could potentiate the cytotoxic effects of trabectedin.
Here we found that maraviroc in combination with trabectedin exerted synergistic effects, enhanced DNA double- strand breaks, and cooperated to decrease the viability of 3D tumor-stroma-heterospheroids.
In this study we used a panel of four authenticated cHL-derived cell lines L-1236, L-428, KM-H2, and HDLM-2 (obtained from the DSMZ, Germany), and cHLMSC obtained from frozen lymph nodes and generated as previously described.5 The effects of drug combinations were evaluated using the Chou-Talalay method, calculating the combination index (CI) with CalcuSyn software (Biosoft, Ferguson, MO, USA).5 CI values <0.9 indicate synergy, the lower the value the stronger the synergism.5,9 Phosphorylation of the H2AX histone (g-H2AX) and g-H2AX-foci formation were used to study the lethal double-strand DNA lesions.10 The combination of maraviroc (Sigma-Aldrich) with trabectedin (PharmaMar) was also tested in 3D heterospheroids. Heterospheroids were generated by co-culturing HRS cells and cHL-MSC (1.0 x 104/mL of each cell type) in RPMI-1640 medium containing 2% fetal calf serum, using plates coated with 20 mg/mL poly-HEMA (Sigma) to prevent cell adhesion.5 Statistical analysis was carried out using GraphPad Prism version 6.0 software (GraphPad, La Jolla, CA, USA). A Student t-test was used to compare two groups and one-way analysis of variance, followed by the Dunnett test, to compare each of a number of treatments with a single control. A P-value <0.05 was considered statistically significant.
First, we performed drug-combination studies with maraviroc and trabectedin using CCR5+ cHL-derived cell lines (L-1236, L-428, KM-H2, HDLM-2). Maraviroc reduced the CCR5-CCL5 mediated autocrine growth6 of HRS cells in a dose-dependent manner (Figure 1A), without an apparent correlation with CCR5 expression (Online Supplementary Figure S1A, B) or levels of secreted CCL5 (Online Supplementary Figure S1C). The combination of maraviroc with trabectedin resulted in a strong synergism (i.e., an interaction between two or more drugs that determines a greater effect than the sum of the individual effects of each drug) in KM-H2 (CI <0.3) and in HDLM-2 cells (CI <0.3), and a moderate synergism in L-1236 cells (CI ranging from 0.47 to 0.63) (Figure 1B). In L-428 cells, we observed synergy only at low drug concentrations (CI ranging from 0.57 to 0.98) (Figure 1B). Genetic lesions in members of the NF-kB and JAK/STAT pathways or TP53 alterations could be a possible explanation for the lower synergistic effects in L-428 cells.11
We then evaluated DNA fragmentation in HRS cells treated with maraviroc alone, trabectedin alone, or their combination. Phosphorylation of the histone H2AX (g-H2AX) is one of the early events associated with the detection and processing of DNA double-strand breaks10 and the formation of g-H2AX-foci, arising when the cell identifies DNA lesions. For this purpose, we analyzed g-H2AX induction and g-H2AX-foci formation after a brief period of incubating cells with the various drugs. Western blot assay showed that treatment of HRS cells with maraviroc alone did not induce or only slightly induced DNA fragmentation. On the other hand, trabectedin induced g-H2AX, an effect that was greatly enhanced by the combination with maraviroc (Figure 2A, B). To further validate that maraviroc in combination with trabectedin enhanced DNA damage, we evaluated the formation of nuclear g-H2AX foci by confocal microscopy.10 Consistently with the findings of the western blot assay (Figure 2A, B), after treatment with maraviroc only rare g-H2AX foci were detected, whereas the combination with maraviroc enhanced the formation of g-H2AX-foci by trabectedin (Figure 2C), confirming that the CCR5-antagonist in combination with trabectedin further promoted DNA fragmentation (Figure 2).
The strong cytotoxic effects of the drug combination with respect to the limited activity of single treatments were confirmed by phase contrast photographs and by annexin-V/7-aminoactinomycin D staining (Online Supplementary Figure S2).
Although maraviroc alone induced a very modest or no DNA fragmentation in HRS cells, unlike in breast cancer cells,4 we cannot exclude a possible role of CCR5 in enhancing DNA repair also in cHL. Alternatively, maraviroc could increase the concentration of trabectedin in HRS cells by competing for the drug transporter P-glycoprotein, a substrate for both drugs.12
In cHL, a few HRS cells are surrounded by a protective and immunosuppressive TME, capable of decreasing drug activity and counteracting the immune control of tumor growth.13 Heterospheroids represent a 3D model in which different cell types are cultured under nonadherent conditions. This in vitro model, developed to mimic the cross-talk of HRS cells with the TME, was recently used to study the antitumor activity of trabectedin alone,9 and of maraviroc in combination with doxorubicin.5
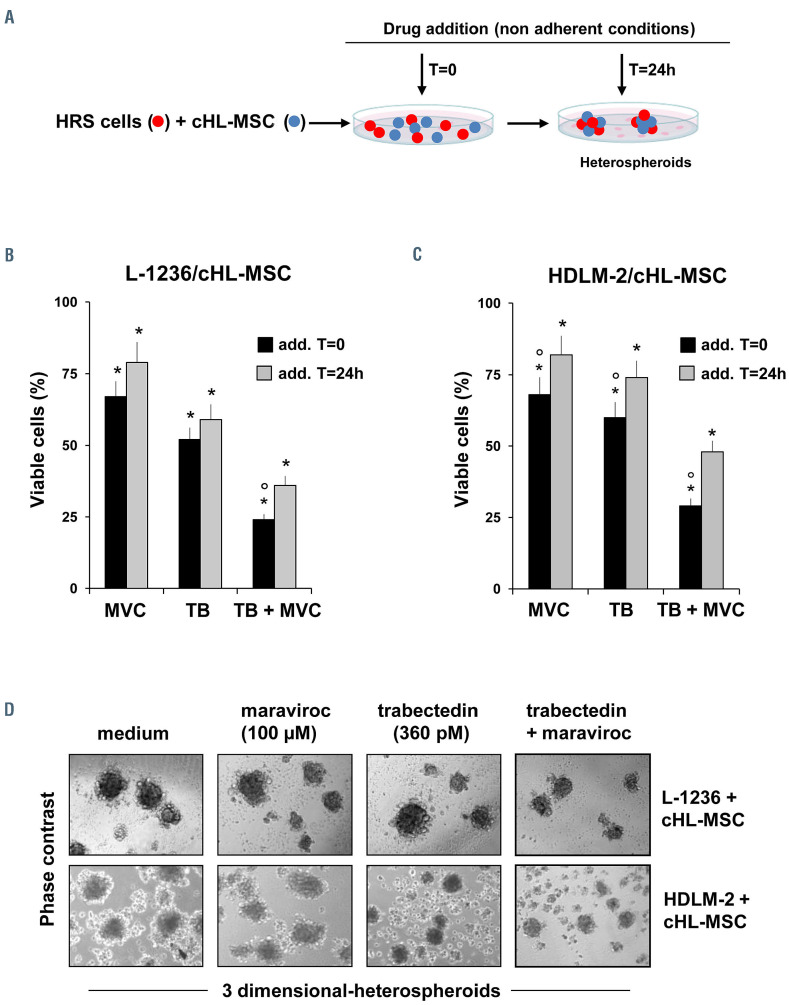
cHL-MSC can exert protective effects against anticancer drugs by their direct contact with tumor cells13,14 or by secreting tumor-promoting molecules, including CCL5.5 Since maraviroc reduces the self-assembly of HRS cells with cHL-MSC,5 it could cooperate with trabectedin not only by enhancing DNA damage in CCR5+ cells but also by counteracting the protective effects of the crosstalk between HRS and cHL-MSC. We evaluated the efficacy of the maraviroc-trabectedin combination in formed heterospheroids (direct contact). We cultured HRS cells (L-1236 or HDLM-2 cells) with cHL-MSC under nonadherent conditions. After 24 h (the time necessary to obtain cell aggregation as heterospheroids), we added maraviroc and different concentrations of trabectedin9 (Online Supplementary Figure S3). After 3 days (Online Supplementary Figure S3A, B) and 6 days (Online Supplementary Figure S3C, D) of treatment, we evaluated drug effects. Both maraviroc and trabectedin decreased heterospheroid cell viability in a dose-dependent manner and their combination further increased cytotoxicity. These effects were more evident after 6 days of treatment in HDLM-2 and in particular in L-1236 cells (Online Supplementary Figure S3).
Figure 3.
Maraviroc cooperated with trabectedin to decrease cell viability in three-dimensional heterospheroids formed by Hodgkin and Reed-Sternberg cells and classical Hodgkin lymphoma mesenchymal stromal cells. (A) Schedule of treatment of Hodgkin and Reed-Sternberg (HRS) cells and classical Hodgkin lymphoma mesenchymal stromal cells (cHL-MSC). (B) L-1236, or (C) HDLM-2 cells were cultured in non-adherent conditions with cHL-MSC (1.0 x 104/mL of each cell type) in 24-well plates and treated with trabectedin (360 pM) alone, maraviroc (100 mM) alone or in combination. Drugs were added immediately (add. T= 0) and after heterospheroid formation (add. T=24h). After 6 days, cell viability was evaluated using the PrestoBlue Cell Viability Reagent (Invitrogen). Values are mean and standard deviation of three experiments. °P<0.05 for T=0 vs. T=24h, Student t-test. *P<0.05 treatments vs. medium, One-way analysis of variance followed by the Dunnett test. (D) Representative phase contrast micrographs of heterospheroids cultured with trabectedin, maraviroc and their combination (T=0). MVC, maraviroc; TB, trabectedin. add., added.
To demonstrate that the direct contact with cHL-MSC can protect against the effects exerted by maraviroc, trabectedin and their combination, HRS cells and cHL-MSC were cultured under non-adherent conditions and drugs were added before (at T=0) and after (at T=24h) their spontaneous aggregation in heterospheroids (see Figure 3A). After 6 days cell viability of heterospheroids formed by L-1236/cHL-MSC (Figure 3B) and by HDLM-2/cHLMSC (Figure 3C) was evaluated. Both maraviroc and trabectedin alone reduced cell viability of heterospheroids (Figure 3B, C) and their combination was significantly more efficacious than single treatments. Cytotoxicity was more evident when drugs were added before cell aggregation (heterospheroid formation, T=0) (black histograms), suggesting a protective role of HL-MSC and cooperation between the two cell types, including the increased secretion and expression of pro-survival factors. 13 Representative phase contrast photographs demonstrating the increased cytotoxic activity of the combination trabectedin-maraviroc in heterospheroids are shown in Figure 3D.
Taken together our results suggest that maraviroc can enhance trabectedin activity by reducing the tumor-promoting effects of the direct contact of HRS cells with cHL-MSC13 and by inhibiting autocrine and paracrine effects induced by CCL5 secreted by HRS cells6 and tumor-educated cHL-MSC.5
In conclusion, maraviroc synergized with trabectedin, enhanced trabectedin-induced DNA double-strand breaks and decreased the protective effects of cHL-MSC in heterospheroids.
Therefore, this study offers an additional preclinical rationale for the use of maraviroc as a new therapeutic option to affect tumor microenvironmental interactions, to enhance the cytotoxic activity of DNA-damaging agents and, by decreasing their doses, to reduce adverse side effects.5 These findings provide insights for future research to investigate the possibility of potentiating the antitumoral activity of DNA-damaging agents, including gamma radiation, currently used for the treatment of cHL.15
Supplementary Material
Acknowledgments
The authors thank Dr. Alfonso Colombatti for his help with reviewing the manuscript.
Funding Statement
Funding: this work was supported in part by grant IG 15844 from the Italian Association for Cancer Research (to DA) and by the Italian Ministry of Health (Ricerca Corrente).
References
- 1.Aldinucci D, Borghese C, Casagrande N. The CCL5/CCR5 axis in cancer progression. Cancers (Basel). 2020;12(7):1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miao M, De Clercq E, Li G. Clinical significance of chemokine receptor antagonists. Expert Opin Drug Metab Toxicol. 2020;16(1):11-30. [DOI] [PubMed] [Google Scholar]
- 3.Jiao X, Nawab O, Patel T, et al. Recent advances targeting CCR5 for cancer and its role in immuno-oncology. Cancer Res. 2019; 79(19): 4801-4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiao X, Velasco-Velázquez MA, Wang M, et al. CCR5 governs DNA damage repair and breast cancer stem cell expansion. Cancer Res. 2018;78(7):1657-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casagrande N, Borghese C, Visser L, Mongiat M, Colombatti A, Aldinucci D. CCR5 antagonism by maraviroc inhibits Hodgkin lymphoma microenvironment interactions and xenograft growth. Haematologica. 2019;104(3):564-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aldinucci D, Lorenzon D, Cattaruzza L, et al. Expression of CCR5 receptors on Reed-Sternberg cells and Hodgkin lymphoma cell lines: involvement of CCL5/Rantes in tumor cell growth and microenvironmental interactions. Int J Cancer. 2008;122(4):769-776. [DOI] [PubMed] [Google Scholar]
- 7.D’Incalci M, Badri N, Galmarini CM, Allavena P. Trabectedin, a drug acting on both cancer cells and the tumour microenvironment. Br J Cancer. 2014;111(4):646-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jimenez PC, Wilke DV, Branco PC, et al. Enriching cancer pharmacology with drugs of marine origin. Br J Pharmacol. 2020;177(1):3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casagrande N, Borghese C, Favero A, Vicenzetto C, Aldinucci D. Trabectedin overcomes doxorubicin-resistance, counteracts tumorimmunosuppressive reprogramming of monocytes and decreases xenograft growth in Hodgkin lymphoma. Cancer Lett. 2021;500:182-193. [DOI] [PubMed] [Google Scholar]
- 10.Ruprecht N, Hungerbühler MN, Böhm IB, Heverhagen JT. Improved identification of DNA double strand breaks: γ-H2AX-epitope visualization by confocal microscopy and 3D reconstructed images. Radiat Environ Biophys. 2019;58(2):295-302. [DOI] [PubMed] [Google Scholar]
- 11.Cuceu C, Hempel WM, Sabatier L, Bosq J, Carde P, M’kacher R. Chromosomal Instability in Hodgkin lymphoma: an in-depth review and perspectives. Cancers (Basel). 2018;10(4):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tupova L, Ceckova M, Ambrus C, et al. Interactions between maraviroc and the ABCB1, ABCG2, and ABCC2 transporters: an important role in transplacental pharmacokinetics. Drug Metab Dispos. 2019;47(9):954-960. [DOI] [PubMed] [Google Scholar]
- 13.Aldinucci D, Celegato M, Casagrande N. Microenvironmental interactions in classical Hodgkin lymphoma and their role in promoting tumor growth, immune escape and drug resistance. Cancer Lett. 2016;380(1):243-252. [DOI] [PubMed] [Google Scholar]
- 14.Bankov K, Döring C, Ustaszewski A, et al. Fibroblasts in nodular sclerosing classical Hodgkin lymphoma are defined by a specific phenotype and protect tumor cells from brentuximab-vedotin induced injury. Cancers (Basel). 2019;11(11):1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Connors JM, Cozen W, Steidl C, et al. Hodgkin lymphoma. Nat Rev Dis Primers. 2020;6(1):61. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.