Abstract
Knee osteoarthritis is the most common orthopaedic disorder, and surgical treatments are always inevitable. Among the various surgical options, arthroscopic treatment is not favorable because strong evidence supporting its application is scarce. However, we consider that the unsatisfactory clinical results of arthroscopic surgery occur because the pain-relieving mechanism of joint replacement is not realized in the too simple and not well-designed arthroscopic procedures. Thus, we use a set of arthroscopic procedures to realize the pain-relieving mechanism of joint replacement, which we call “arthroscopic arthroplasty.” The most important parts of this technique are denervation of the subchondral bone and comprehensive synovectomy. Our clinical results indicate that we can obtain even better functional improvement with this technique than that with joint replacement. We consider that the introduction of this technique will arouse interest in the development of arthroscopic surgical procedures for knee osteoarthritis.
Technique Video
Arthroscopic arthroplasty for knee osteoarthritis in left knee. The medial and infrapatellar plicas are removed. The medial and lateral compartments are examined. The injured or degenerated meniscus is addressed through meniscectomy or trimming. Femoral notch impingement is addressed through removal of the third tibial eminence, as well as debridement and femoral notch–plasty. The osteophytes on the medial wall of the femoral notch are removed to enlarge the passage to the posteromedial compartment. The posteromedial and posterolateral portals are established. The arthroscope is placed into the posterior compartments through the posteromedial portal. The posterior septum is removed through the posterolateral portal. The posterior compartments are debrided. The periosteum on the posterior side of the medial femoral condyle is removed, and the posteromedial capsule attachment is released. Femoral notch posterior outlet–plasty is performed. The periosteum on the posterior side of the lateral femoral condyle is removed, and the posterolateral capsule attachment is released. The suprapatellar pouch is debrided. The anterior, lateral, and medial sides of the distal femur are denuded through synovectomy and periosteum removal.
Knee osteoarthritis (OA) can cause joint pain, stiffness, and limited movement. Surgery is the last resort in its comprehensive treatment, in which minimally invasive arthroscopic surgery was once reported to be effective.1, 2, 3 However, clinical studies have shown that arthroscopic joint debridement is not more effective than placebo surgery or conservative treatment.4,5 On the basis of these studies, recent reviews have found no advantage of arthroscopic surgery over conservative treatment.6, 7, 8 Therefore, many researchers limit the indications of arthroscopic treatment of knee OA to the presence of mechanical symptoms,9, 10, 11, 12, 13 although the main clinical symptoms of knee OA are not mechanical. Currently, although arthroscopy for knee OA is still being performed for various reasons,14,15 the practice seems to lack academic support.
The specific arthroscopic techniques used to treat knee OA vary widely in the literature, ranging from simple joint irrigation to complex chondroplasty, with most of the reported techniques involving arthroscopic joint debridement. Since 2000, we have adopted a special arthroscopic technique to treat knee OA, which is called “arthroscopic arthroplasty,” with the expectation to realize the pain-relieving mechanism of joint replacement through arthroscopic procedures. It is generally believed that the pain sources are the subchondral bone, synovial membrane, joint capsule ligament, patellofemoral joint, femoral notch, tendon insertions, and muscles,16, 17, 18 with synovium-derived pain and subchondral osteogenic pain as the main sources. Thus, corresponding procedures are designed to address these pain sources (Table 1) to realize the pain-relieving mechanism of joint replacement with arthroscopic arthroplasty. The described technique can be used alone or combined with other arthroscopic procedures or deformity-correcting osteotomy for all 3 categories of knee OA (Table 2). The indication of this technique is knee OA with severe pain symptoms (visual analog scale score > 6), obvious impediment to daily life, and failure of conservative treatment, especially in patients aged 70 years or younger.
Table 1.
Pain-Relieving Mechanisms of Joint Replacement Versus Arthroscopic Arthroplasty
| Origin or Cause of Pain in Knee OA | Pain-Relieving Mechanism of Joint Replacement | Pain-Relieving Mechanism of Arthroscopic Arthroplasty | Differences in Results |
|---|---|---|---|
| Subchondral bone | Removal of disordered subchondral bone layer | Denervation of disordered subchondral bone layer | Arthroscopic subchondral denervation of proximal tibial is less complete than joint replacement |
| Relieving overloading through alignment correction | Relieving overloading through combined osteotomy | Equal | |
| Synovium | Removal of inflammatory or hyperplastic synovium | Removal of inflammatory or hyperplastic synovium | Arthroscopic removal of synovium is more complete, especially in posterior compartments of knee |
| Ligament | Removal of irritating osteophyte | Osteophyte removal | Equal |
| Patellofemoral joint | Patella-plasty Patella denervation |
Patella-plasty Patella denervation Lateral retinacular release |
Lateral retinacular release is emphasized in arthroscopic arthroplasty but always overlooked in joint replacement |
| Femoral notch | Notch-plasty | Notch-plasty | Equal |
| Tendon insertion | Postoperative exercises | Postoperative exercises | Equal |
| Muscles | Postoperative exercises | Postoperative exercises | Equal |
Table 2.
Categories of Knee Osteoarthritis and Related Procedures
| Category of Knee OA | Abnormal Lower-Limb Alignment (>5° of Varus or Valgus) | Mechanical Symptoms | Possibility of Arthroscopic Arthroplasty | Combined Operation |
|---|---|---|---|---|
| Type I | Absent | Absent | Yes | — |
| Type II | Absent | Present | Yes | Related arthroscopic procedures to relieve mechanical symptoms |
| Type III | Present | Present | Yes | Osteotomy to correct alignment |
Surgical Procedures
Because most patients undergoing arthroscopic arthroplasty have both medial tibiofemoral and patellofemoral arthritis and have mild flexion contracture, arthroscopic management for these types of patients is described subsequently as the standard procedure of arthroscopic arthroplasty (Table 3).
Table 3.
Step-by-Step Procedures of Arthroscopic Arthroplasty for Knee Osteoarthritis
|
Debridement of Medial and Lateral Compartments of Knee
The high anteromedial and high anterolateral portals are established (Video 1). The medial and infrapatellar plicas are removed with a shaver (ConMed Linvatec, New York, NY). The medial and lateral compartments are examined. The injured or degenerated meniscus is first addressed through meniscectomy or trimming. All unstable cartilage tissue is removed.
Release of Medial Collateral Ligament
The tension of the medial collateral ligament (MCL) is examined through the varus stress near the knee extension position. If the medial joint space is less than 5 mm, the MCL contracture is defined. A 1-cm incision is made over the MCL at a level corresponding to the body of the medial meniscus. The MCL is released through multiple stabs (acupuncture release) with a sharp-pointed knife through this incision until the medial joint space can be opened.
Femoral Notch–plasty
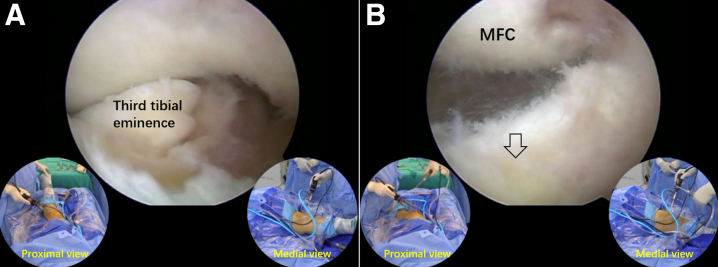
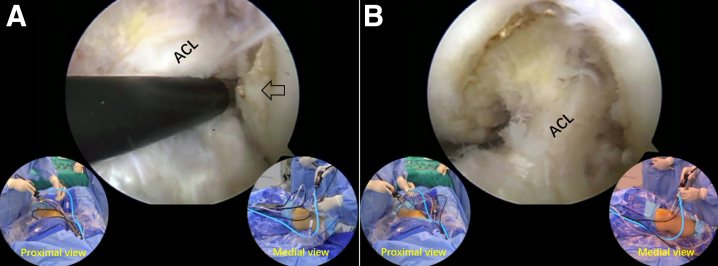
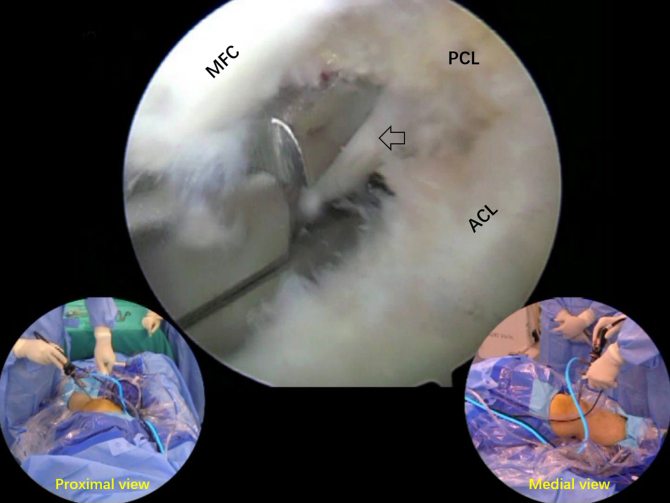
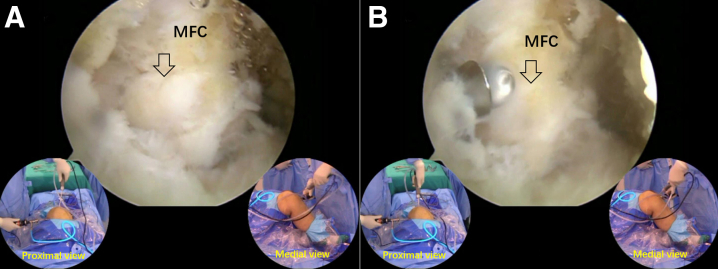
The femoral notch is examined to determine whether there is any impingement between the femoral notch and the anterior cruciate ligament, the femoral notch and the tibial eminences, and the anterior opening of the femoral notch and the third tibial eminence (Fig 1). Femoral notch–plasty and removal of the third tibial eminence are performed to eliminate any bony impingement with a burr (ConMed Linvatec) (Fig 2). The thickened synovium on the surface of the posterior cruciate ligament is removed to eliminate soft-tissue impingement between the anterior and posterior cruciate ligaments. The osteophytes on the medial wall of the femoral notch are removed to enlarge the passage between the posterior cruciate ligament and the medial wall of the femoral notch to the posteromedial compartment for subsequent procedures (Fig 3).
Fig 1.
Arthroscopic view of left knee through anterolateral portal. The third tibial eminence impinges (arrow) on the roof of the femoral notch in knee extension (A) and is removed (B). (MFC, medial femoral condyle.)
Fig 2.
Arthroscopic view of left knee through anterolateral portal. An osteophyte (arrow) impinging on the anterior cruciate ligament (ACL) is defined (A), and femoral notch–plasty is performed (B).
Fig 3.
Arthroscopic view of left knee through anterolateral portal. An osteophyte at the medial wall of the femoral notch (arrow) is removed. (ACL, anterior cruciate ligament; MFC, medial femoral condyle; PCL, posterior cruciate ligament.)
Debridement in Posterior Compartments
The arthroscope is placed through the anterolateral portal and the femoral notch into the posteromedial compartment. A posteromedial portal is established. The arthroscope is placed into the posteromedial compartment, pressed against the center of the posterior septum, and placed into the posterolateral compartment. The posterolateral portal is created.
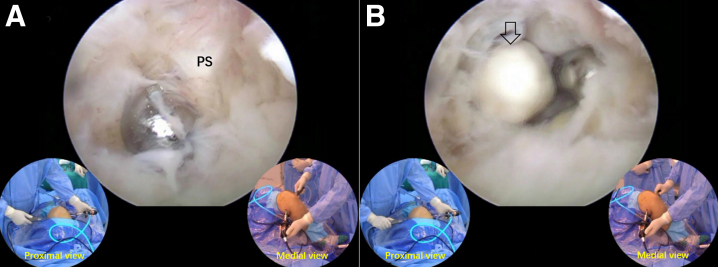
An arthroscopic shaver is placed through the posterolateral portal to the posterior septum after retrieval of the arthroscope to the posteromedial compartment. The posterior septum is then removed to connect the posterior compartments (Fig 4). The posterior compartments are debrided.
Fig 4.
Arthroscopic view of posteromedial compartment of left knee through posteromedial portal. A shaver is placed into the posterior septum (PS) (A) to remove the PS (B). The arrow indicates a free body in the PS.
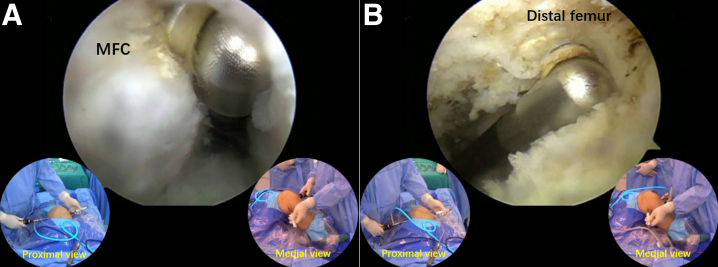
Posterior Femoral Condyle–plasty and Denervation
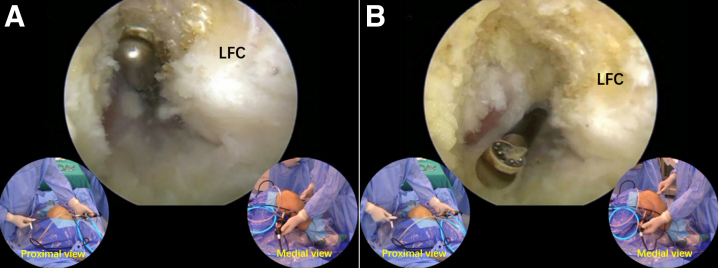
Through the posteromedial and posterolateral portals, the osteophytes on the posterior side of the femoral condyles are removed. If the osteophyte at the posterior opening of the femoral notch impinges on the posterior cruciate ligament, femoral notch posterior opening–plasty is performed (Fig 5). The synovium and periosteum between the attachment site of the capsule and the cartilage margin are removed with a radiofrequency probe (ArthroCare; Smith & Nephew, Andover, MA) to realize denervation of the posterior femoral condyles (Figs 6A and 7A).
Fig 5.
Arthroscopic view of posterior compartments of left knee through posterolateral portal. An osteophyte (arrow) at the posterior outlet of the femoral notch that impinges on the posterior cruciate ligament is defined (A) and removed (arrow) with instruments placed through the anteromedial portal (B). (MFC, medial femoral condyle.)
Fig 6.
Arthroscopic view of posteromedial compartment of left knee through posterolateral portal. The periosteum between the posterior cartilage edge and the capsule attachment of the medial femoral condyle (MFC) is removed (A) to realize denervation, and the capsule is released from the femur to address flexion contracture (B).
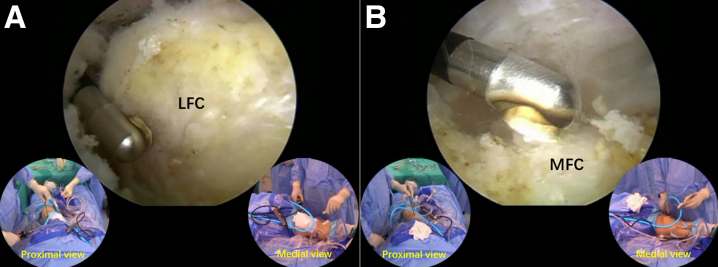
Fig 7.
Arthroscopic view of posterolateral compartment of left knee through posterolateral portal. The periosteum between the posterior cartilage edge and the capsule attachment of the lateral femoral condyle (LFC) is removed (A) to realize denervation, and the capsule is released from the femur to address flexion contracture (B).
Release of Posterior Capsule and Muscles
Extension of the knee is attempted. If full extension of the knee still cannot be reached, posterior contracture is defined. The posterior capsule is first released from the femur. The tendinous portion of the gastrocnemius muscle is released close to the posterior femoral cortex until its posterior muscular portion is visible (Figs 6B and 7B).
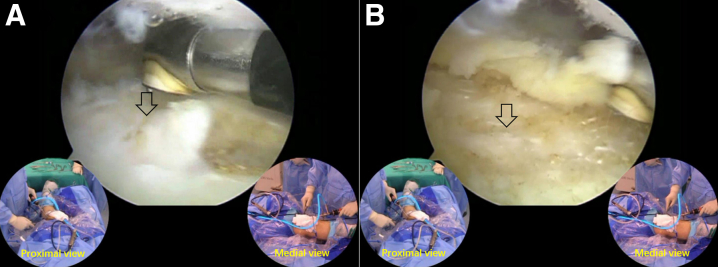
Distal Femur Denervation From Anterior, Medial, and Lateral Sides
With full knee extension, the arthroscope is inserted into the anterior compartment of the knee. A supralateral patellar portal is established. The osteophytes along the medial and lateral edges of the femoral condyles, as well as those at the proximal edge of the femoral trochlea, are removed. The soft tissue on the anterior side of the distal femur or the bottom of the suprapatellar pouch (Fig 8), the medial side of the medial femoral condyle (Fig 9A), and the lateral side of the lateral femoral condyle (Fig 9B) is removed to realize denervation of the distal femoral condyle.
Fig 8.
Arthroscopic view of suprapatellar pouch of left knee through anterolateral portal. The periosteum (arrow) at the bottom of the suprapatellar pouch is removed (A) to denude the anterior side of the distal femur (arrow) to realize denervation of the cartilage at a more distal site (B).
Fig 9.
(A) Arthroscopic view of lateral gutter of left knee through supralateral patellar portal. Removal of periosteum on lateral side of lateral femoral condyle (LFC). (B) Arthroscopic view of medial gutter of left knee through supralateral patellar portal. Removal of periosteum on medial side of medial femoral condyle (MFC).
Denervation on Anterior Side of Proximal Tibia
With the knee in an extension position, the arthroscope is placed through the supralateral patellar portal. Part of the infrapatellar pad is removed to expose and remove the soft tissue on the anterior side of the proximal tibia to realized denervation of the proximal tibia.
Denervation of Anteromedial Side of Tibia
The arthroscope is placed through the anterolateral portal, and the periosteum on the anteromedial side of the proximal tibia, with the MCL, pes anserinus, and tibial tubercle as boundaries, is removed with a radiofrequency probe.
Patella-plasty and Denervation
The osteophytes on the upper and lower poles of the patella, as well as the hyperplastic lateral edge of the patella, are removed through the anterolateral portal and the supralateral patellar portal. The synovium around the patella is removed to realize partial patellar denervation. Lateral retinacular release is performed in case of its contracture.
Discussion
The standard arthroscopic arthroplasty technique includes 11 types of surgical procedures: (1) subchondral bone denervation by adjacent periosteum removal (with the consideration that the subchondral bone is innervated mainly through the nearby periosteum instead of through the medullary canal); (2) synovectomy; (3) resection of the hyperplastic infrapatellar fat pad; (4) osteophyte removal at the proximal tibia, distal femur, and patella; (5) cancellous bone surface devitalization; (6) femoral notch–plasty; (7) resection of the hyperplastic lateral surface of the patella; (8) release of the lateral retinaculum of the patella; (9) MCL release; (10) release of the posterior capsule and gastrocnemius muscle; and (11) trimming of the articular cartilage and meniscus. This technique is quite different from the reported arthroscopic operations for knee OA to realize the pain-relieving mechanism through arthroscopic procedures.
From the technical level, arthroscopic arthroplasty of the knee is the highest level in the field of knee arthroscopy, requiring all arthroscopic portals and involving operating in various compartments of the knee, among which the posterior compartments of the knee are the most difficult in which to operate. The key to ensure the effectiveness of the operation is to complete each step as planned. Therefore, arthroscopic arthroplasty is not suitable for beginners. This procedure should be performed only after mastery of the comprehensive arthroscopic techniques, especially those related to the posterior compartment of the knee and the patellofemoral joint.
Arthroscopic arthroplasty is a “big deal” that upends patients’ understanding of arthroscopic surgery, which they expect to have a mild surgical reaction. The largest problem with this procedure is that there is relatively severe edema for the first 2 to 3 weeks after surgery, and some patients may have significant swelling around the knee. The most effective measure to eliminate edema and swelling is active activity training. The patient should be informed preoperatively about the possible situation after the operation to obtain his or her understanding and cooperation.
The pearls and pitfalls of the described technique are listed in Table 4, and the advantages and disadvantages are presented in Table 5. We have performed this procedure in over 1400 patients and observed its effectiveness. The mean operating time is less than 90 minutes.
Table 4.
Pearls and Pitfalls of Arthroscopic Arthroplasty for Knee Osteoarthritis
|
CT, computed tomography; MCL, medial collateral ligament; MRI, magnetic resonance imaging.
Table 5.
Advantages and Disadvantages of Arthroscopic Arthroplasty for Knee Osteoarthritis
| Advantages |
| The pain-relieving mechanisms of joint replacement can be realized through arthroscopic arthroplasty to avoid the placement of an artificial joint. |
| The stability and soft-tissue balance of the knee are maintained. |
| Synovitis can be better relieved through an arthroscopic procedure. |
| Disadvantages |
| Arthroscopic arthroplasty is time-consuming and technically challenging. |
| Relatively severe and prolonged postoperative edema occurs quite often. |
Footnotes
The author reports no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic arthroplasty for knee osteoarthritis in left knee. The medial and infrapatellar plicas are removed. The medial and lateral compartments are examined. The injured or degenerated meniscus is addressed through meniscectomy or trimming. Femoral notch impingement is addressed through removal of the third tibial eminence, as well as debridement and femoral notch–plasty. The osteophytes on the medial wall of the femoral notch are removed to enlarge the passage to the posteromedial compartment. The posteromedial and posterolateral portals are established. The arthroscope is placed into the posterior compartments through the posteromedial portal. The posterior septum is removed through the posterolateral portal. The posterior compartments are debrided. The periosteum on the posterior side of the medial femoral condyle is removed, and the posteromedial capsule attachment is released. Femoral notch posterior outlet–plasty is performed. The periosteum on the posterior side of the lateral femoral condyle is removed, and the posterolateral capsule attachment is released. The suprapatellar pouch is debrided. The anterior, lateral, and medial sides of the distal femur are denuded through synovectomy and periosteum removal.
References
- 1.Fond J., Rodin D., Ahmad S., et al. Arthroscopic debridement for the treatment of osteoarthritis of the knee: 2- and 5-year results. Arthroscopy. 2002;18:829–834. doi: 10.1053/jars.2002.36225. [DOI] [PubMed] [Google Scholar]
- 2.Hubbard M.J. Articular debridement versus washout for degeneration of the medial femoral condyle. A five-year study. J Bone Joint Surg Br. 1996;78:217–219. [PubMed] [Google Scholar]
- 3.Merchan E.C., Galindo E. Arthroscope-guided surgery versus nonoperative treatment for limited degenerative osteoarthritis of the femorotibial joint in patients over 50 years of age: A prospective comparative study. Arthroscopy. 1993;9:663–667. doi: 10.1016/s0749-8063(05)80503-1. [DOI] [PubMed] [Google Scholar]
- 4.Moseley J.B., O’Malley K., Petersen N.J., et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 5.Kirkley A., Birmingham T.B., Litchfield R.B., et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097–1107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 6.Khan M., Khanna V., Adili A., Ayeni O.R., Bedi A., Bhandari M. Knee osteoarthritis: When arthroscopy can help. Pol Arch Intern Med. 2018;128:121–125. doi: 10.20452/pamw.4186. [DOI] [PubMed] [Google Scholar]
- 7.Brignardello-Petersen R., Guyatt G.H., Buchbinder R., et al. Knee arthroscopy versus conservative management in patients with degenerative knee disease: A systematic review. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-016114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Navarro R.A., Adams A.L., Lin C.C., et al. Does knee arthroscopy for treatment of meniscal damage with osteoarthritis delay knee replacement compared to physical therapy alone? Clin Orthop Surg. 2020;12:304–311. doi: 10.4055/cios19114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aaron R.K., Skolnick A.H., Reinert S.E., et al. Arthroscopic débridement for osteoarthritis of the knee. J Bone Joint Surg Am. 2006;88:936–943. doi: 10.2106/JBJS.D.02671. [DOI] [PubMed] [Google Scholar]
- 10.Howell S.M. The role of arthroscopy in treating osteoarthritis of the knee in the older patient. Orthopedics. 2010;33:652. doi: 10.3928/01477447-20100722-34. [DOI] [PubMed] [Google Scholar]
- 11.Kelly M.A. Role of arthroscopic debridement in the arthritic knee. J Arthroplasty. 2006;21(suppl 1):9–10. doi: 10.1016/j.arth.2006.02.086. [DOI] [PubMed] [Google Scholar]
- 12.Stuart M.J., Lubowitz J.H. What, if any, are the indications for arthroscopic debridement of the osteoarthritic knee? Arthroscopy. 2006;22:238–239. doi: 10.1016/j.arthro.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Buldu M.T., Marsh J.L., Arbuthnot J. Mechanical symptoms of osteoarthritis in the knee and arthroscopy. J Knee Surg. 2016;29:396–402. doi: 10.1055/s-0035-1564592. [DOI] [PubMed] [Google Scholar]
- 14.Adelani M.A., Harris A.H., Bowe T.R., Giori N.J. Arthroscopy for knee osteoarthritis has not decreased after a clinical trial. Clin Orthop Relat Res. 2016;474:489–494. doi: 10.1007/s11999-015-4514-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barlow T., Plant C.E. Why we still perform arthroscopy in knee osteoarthritis: A multi-methods study. BMC Musculoskelet Disord. 2015;16:85. doi: 10.1186/s12891-015-0537-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mach D.B., Rogers S.D., Sabino M.C., et al. Origins of skeletal pain: Sensory and sympathetic innervation of the mouse femur. Neuroscience. 2002;113:155–166. doi: 10.1016/s0306-4522(02)00165-3. [DOI] [PubMed] [Google Scholar]
- 17.Niv D., Gofeld M., Devor M. Causes of pain in degenerative bone and joint disease: A lesson from vertebroplasty. Pain. 2003;105:387–392. doi: 10.1016/S0304-3959(03)00277-X. [DOI] [PubMed] [Google Scholar]
- 18.Witt K.L., Viarthroscopeky J.A. The anatomy of osteoarthritic joint pain. Clin Anat. 2014;27:451–454. doi: 10.1002/ca.22120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic arthroplasty for knee osteoarthritis in left knee. The medial and infrapatellar plicas are removed. The medial and lateral compartments are examined. The injured or degenerated meniscus is addressed through meniscectomy or trimming. Femoral notch impingement is addressed through removal of the third tibial eminence, as well as debridement and femoral notch–plasty. The osteophytes on the medial wall of the femoral notch are removed to enlarge the passage to the posteromedial compartment. The posteromedial and posterolateral portals are established. The arthroscope is placed into the posterior compartments through the posteromedial portal. The posterior septum is removed through the posterolateral portal. The posterior compartments are debrided. The periosteum on the posterior side of the medial femoral condyle is removed, and the posteromedial capsule attachment is released. Femoral notch posterior outlet–plasty is performed. The periosteum on the posterior side of the lateral femoral condyle is removed, and the posterolateral capsule attachment is released. The suprapatellar pouch is debrided. The anterior, lateral, and medial sides of the distal femur are denuded through synovectomy and periosteum removal.
Arthroscopic arthroplasty for knee osteoarthritis in left knee. The medial and infrapatellar plicas are removed. The medial and lateral compartments are examined. The injured or degenerated meniscus is addressed through meniscectomy or trimming. Femoral notch impingement is addressed through removal of the third tibial eminence, as well as debridement and femoral notch–plasty. The osteophytes on the medial wall of the femoral notch are removed to enlarge the passage to the posteromedial compartment. The posteromedial and posterolateral portals are established. The arthroscope is placed into the posterior compartments through the posteromedial portal. The posterior septum is removed through the posterolateral portal. The posterior compartments are debrided. The periosteum on the posterior side of the medial femoral condyle is removed, and the posteromedial capsule attachment is released. Femoral notch posterior outlet–plasty is performed. The periosteum on the posterior side of the lateral femoral condyle is removed, and the posterolateral capsule attachment is released. The suprapatellar pouch is debrided. The anterior, lateral, and medial sides of the distal femur are denuded through synovectomy and periosteum removal.