Abstract
Anterior cruciate ligament reconstruction (ACLR) is one of the most common orthopedic procedures performed each year. The majority of patients undergoing these reconstructions will experience long-term stability and symptomatic relief; however, some will require a revision ACLR procedure. In general, revision ACLRs are more challenging than primary ACLRs due to several diagnostic and technical considerations. A revision ACLR can be performed with either a one-stage or two-stage procedure, which is based on the presence or absence of malpositioned tunnels, bone loss, and tunnel expansion. Recently, the introduction of preshaped allograft bone dowels as a bone grafting option has gained popularity. They provide immediate structural stability and avoid donor site morbidity associated with autografts. The purpose of this article is to outline a bone-grafting tunnel technique with cannulated allograft bone dowels soaked in bone marrow aspirate concentrate (BMAC) used in the first stage of a staged revision ACLR procedure.
Technique Video
This video demonstrates the bone-grafting technique for a staged revision anterior cruciate ligament reconstruction using cannulated allograft bone dowels soaked in bone marrow aspirate concentrate.
Introduction
Anterior cruciate ligament (ACL) reconstruction is one of the most common orthopedic procedures performed each year.1 It is reported that 200,000 ACL tears occur annually in the United States with an estimated 140,000 of those undergoing ACL reconstruction (ACLR).2, 3, 4, 5 The majority of patients undergoing these reconstructions will experience long-term stability and symptomatic relief; however, approximately 1.8% to 10.4% of them will require a revision ACLR procedure.6 In general, revision ACLRs are more challenging than primary ACLRs due to several diagnostic and technical considerations; however, there is no standard revision procedure to date.
A revision ACLR can be performed with either a one-stage or two-stage procedure. This decision is based on the presence or absence of malpositioned tunnels, bone loss, and tunnel expansion.7,8 A two-stage procedure requiring an initial bone grafting stage is indicated when the original tunnels have enlarged due to the fact that achieving rigid fixation of the new graft at these dimensions is a challenge.7 Another reason to consider a two-staged procedure is when the revision tunnels are likely to converge with the previous tunnels.3
There are several options for bone grafting the originals tunnels in a staged revision ACLR, including allograft bone matrix, struts, and iliac crest autograft.5,9, 10, 11 For instance, a study using allograft bone matrix reported significant advantages with minimal risk for complications in a two-stage revision ACLR.9 A more recent additional option, bone dowels, are preshaped allograft biologics that come readily available in different diameters and lengths.12 They provide immediate structural stability and avoid donor site morbidity associated with autografts.13 The purpose of this article is to outline a bone-grafting tunnel technique with cannulated allograft bone dowels soaked in bone marrow aspirate concentrate (BMAC) used in the first stage of a staged revision ACLR procedure.
Technique
Preoperative Evaluation and Surgical Decision-Making
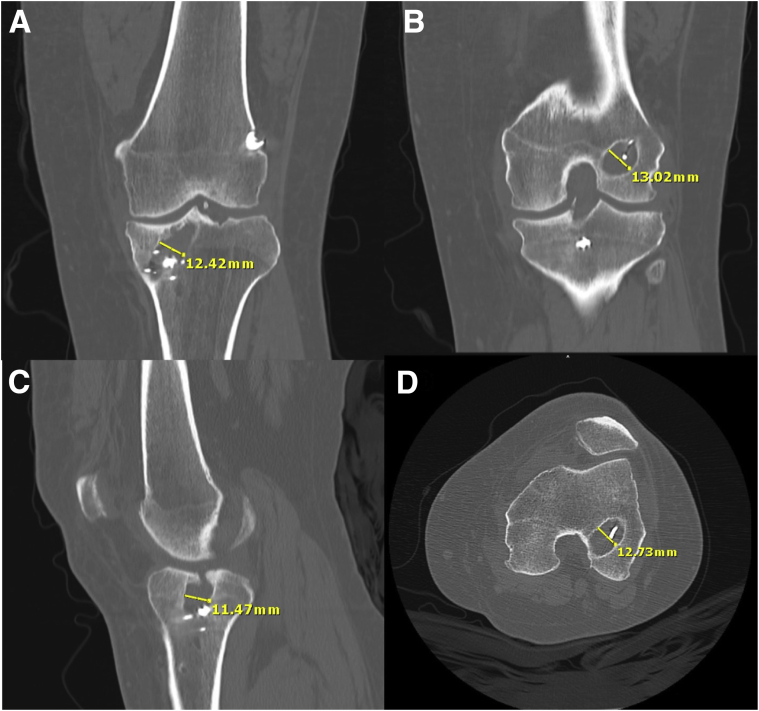
Initially, plain anterior-posterior, lateral, and merchant view radiographs are obtained to establish the position of the ACL tunnels, determining whether they are either anatomic, nonanatomic, or widened. Radiographs are also helpful to investigate the presence, location, and type of fixation hardware that may interfere with the revision procedure. If there is any concern that the diameter of the current tunnels is too large or the position of the tunnels may overlap with the position of the new tunnels, computed tomography (CT) scans should be obtained. CT scans in the axial, coronal, and sagittal planes is crucial to accurately determine the diameter of the tunnels and their three-dimensional positioning (Fig 1). In the case of anatomic tunnel placement, the tunnels can be easily reused once the previous hardware is removed. When the tunnels are nonanatomic but are positioned in such a way as to not interfere with new tunnel placement, they can be usually ignored. However, a two-stage revision procedure should be considered if the nonanatomic tunnels might interfere with revised tunnels or if significant tunnel widening greater than 12 mm in diameter is present. In this instance, an initial bone-grafting procedure may be necessary to ensure secure fixation of the new graft.
Fig 1.
Preoperative computed tomography (CT) examination of a left knee in a patient who previously underwent anterior cruciate ligament reconstruction using a nonanatomical transtibial technique. The coronal (A and B), sagittal (C), and axial (D) CT scans of the left knee demonstrate widening of the femoral and tibial tunnels.
Patient Positioning and Anesthesia:
The patient is brought into the operating room and placed in a supine position. General anesthesia is induced after an adductor canal block of the ipsilateral extremity. A thorough bilateral knee examination is performed to assess preoperative range of motion and heel height, along with anterior drawer, posterior drawer, Lachman, pivot shift, and varus/valgus stress. A padded tourniquet is placed on the operative leg and placed into a leg holder (MizuhoOSI, Union City, CA). The ability for the leg to maintain a 120° knee flexion should be confirmed. The contralateral leg is then placed in a padded abduction stirrup (Birkova Products, Gothenburg, NE). The operative leg is then placed into a pneumatic limb positioner (Spider2; Smith & Nephew, Andover, MA). Two grams of cefazolin is administered prior to incision.
Surgical Technique
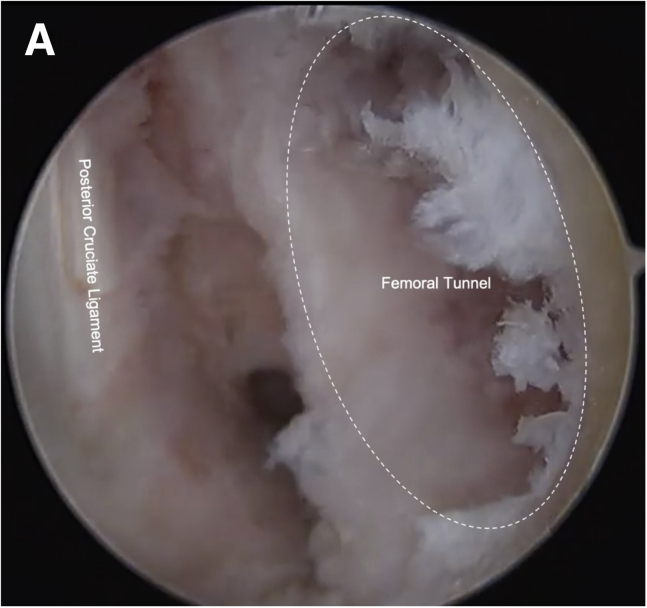
The surgical technique is demonstrated in Video 1. A routine diagnostic arthroscopy is first performed through standard anterolateral and anteromedial portals. The anteromedial arthroscopic portal should provide adequate visualization of the initial ACL femoral and tibial reconstruction tunnels (Fig 2). Next, a thorough assessment of the knee joint is performed, in addition to appropriate treatment of meniscal pathology, chondral defects, and loose bodies.
Fig 2.
Arthroscopic view of the intercondylar notch area through the anterolateral portal visualizing the expanded femoral tunnel through the lateral femoral condyle of the left knee (A).
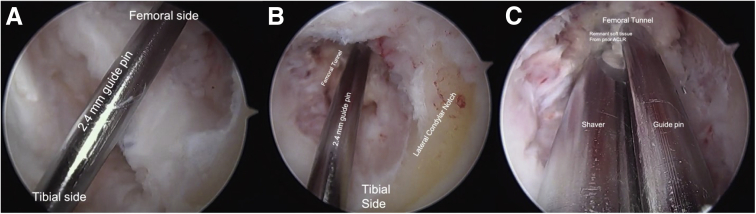
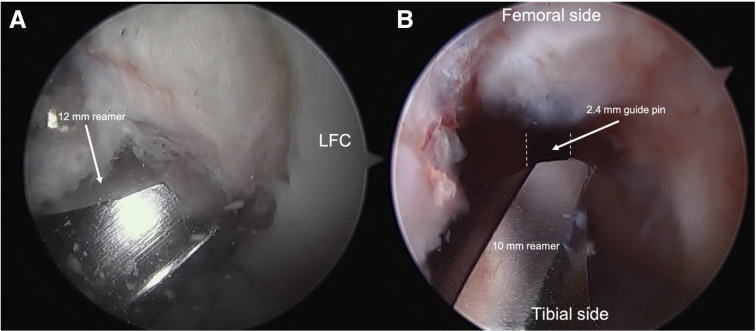
Attention is then turned to the tibia. An incision is made over the tunnel on the anteromedial tibia using the previous scar if possible. Blunt dissection is carried out to reach the previous hardware. The hardware is removed using an extraction set, which should include a staple driver to remove staples and an appropriately sized screwdriver to remove washers and screws. Oftentimes, the removal of bony growth over the screw heads, staples, or washers is necessary. The existing tunnel is identified using a 2.4-mm guide pin (Bone Dowel Revision Kit, Arthrex, Naples, FL) (Fig 3). Advancing the guide pin with your hand is recommended over a wire driver to ensure you follow the trajectory of the primary tunnel. A 12-mm reamer is then advanced over the 2.4-mm guide pin matching the length of the planned dowel and used to over-ream the tibial tunnel (Cannulated Reamer, Arthrex, Naples, FL) (Fig 4).
Fig 3.
Arthroscopic view from the anterolateral portal of the 2.4-mm guide pin traversing through the left knee joint space (A). Advancing the pin with your hand is recommended over a wire driver to ensure you follow the trajectory of the primary tunnels. Arthroscopic view from the anteromedial portal of the 2.4-mm guide pin entering the femoral tunnel in the lateral femoral condyle (B). Arthroscopic view from the anteromedial portal of a shaver clearing remnant anterior cruciate ligament graft tissue from the femoral tunnel (C).
Fig 4.
Reaming the tibial and femoral tunnels in a left knee. Arthroscopic view through the anterolateral portal visualizing the 12-mm reamer as it exits the tibial tunnel proximal opening into the joint (A). Arthroscopy view through the anteromedial portal visualizing the 10-mm reamer, as it approaches the distal opening to the femoral tunnel within the knee joint (B).
Now, attention is turned to the femoral tunnel. If the primary ACLR was performed via a transtibial technique, it may be possible to reach the high-located femoral tunnel through the tibial tunnel, avoiding the need for an additional accessory anteromedial portal. In such a case, using a transtibial approach through the tibial tunnel that was just reamed, again place the 2.4-mm guide pin through the femoral tunnel. It may be helpful to use a wire driver to drive the guide pin through the femur and out the skin. With the knee in 90° of flexion, a 10-mm reamer (Cannulated Reamer; Arthrex, Naples, FL) is placed over the guide pin matching the length of the planned dowel and over-reams the femoral tunnel. Alternatively, if the femoral tunnel cannot be reached via a transtibial technique, the femoral tunnel preparation and bone dowel placement can be completed in a similar fashion using a far medial portal with the knee in 120° of flexion. A curette and shaver are used to remove the sclerotic walls of both tunnels and any remaining soft tissue until clean, bleeding bone is observed. If fragments of hardware, such as bioabsorbable screws, are suspected within the tunnel, the 30° arthroscope can be inserted through the tibial tunnel to identify its position. A small, curved curette (V. Mueller) or a curved surgical rasper (Tunnel/Notchplasty Rasp; Arthrex, Naples, FL) may be used to remove any hardware remnants.
Approximately 60-100 mL of bone marrow aspirate (BMA) is harvested from the anterior superior iliac crest using the Angel Bone Marrow Harvest kit (Arthrex, Naples, FL). The BMA sample is introduced into a centrifuge (Arthrex Angel cPRP & Bone Marrow Processing System; Arthrex, Naples, FL) and spun for an estimated 20 minutes. The 5-cc collection syringe is emptied into a sterile specimen jar, where the allograft bone dowels (FlexiGRAFT Cannulated Revision Dowels; Arthrex, Naples, FL) used for the tibial and femoral tunnel are placed into to allow saturation of the dowels with the obtained BMAC (Fig 5).
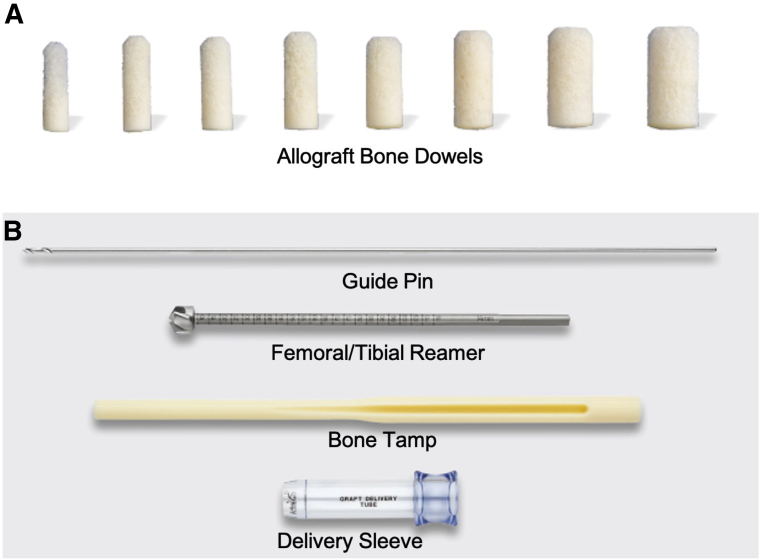
Fig 5.
Arthrex cannulated allograft bone dowels with tapered end; readily-available in different sizes to correspond with size of defect (A). Corresponding instrumentation used to insert the bone dowel, including 2.4-mm guide pin, femoral/tibial reamer, bone tamp, and delivery sleeve (B).
Next, arthroscopic fluid is evacuated from the joint. While maintaining 90° of knee flexion, the 2.4-mm guide pin is first passed through the femoral tunnel via a transtibial approach. Secondly, a delivery sleeve is advanced over the guide pin (Bone Dowel Revision Kit, Arthrex, Naples, FL), followed by a 10-mm cannulated bone dowel (tapered side first) (FlexiGRAFT Cannulated Revision Dowels, Arthrex, Naples, FL) that should be inserted into the delivery sleeve. The cannulated bone tamp is inserted (Bone Dowel Revision Kit, Arthrex, Naples, FL) over the guide pin until it sits flush with the dowel. A mallet is used to gently impact the tamp until the dowel sits slightly proud of the tunnel (Fig 6). Then, with the same technique described above using the guide pin, delivery sleeve, and bone tamp, the tibial tunnel is packed with a 12-mm bone dowel (FlexiGRAFT Cannulated Revision Dowels; Arthrex, Naples, FL) (Fig 7). A 4.5-mm bone cutter (Full Radius BONECUTTER Shaver Blade; Smith & Nephew Dyonics, Andover, MA) is used to contour the edges of the dowels to the native wall (Fig 8). Once complete, minced allograft tissue is soaked in the remaining BMAC and packed into the distal part of the tibial tunnel (Fig 9). The subcutaneous tissue, skin, and portal incisions are closed in a layered fashion. A sterile dressing is applied over the incision. Plain radiographs are obtained on postoperative day 1 for future comparison of follow-up radiographs (Fig 10). Pearls and pitfalls, as well as the advantages and limitations of this surgical technique are summarized in Table 1 and Table 2, respectively.
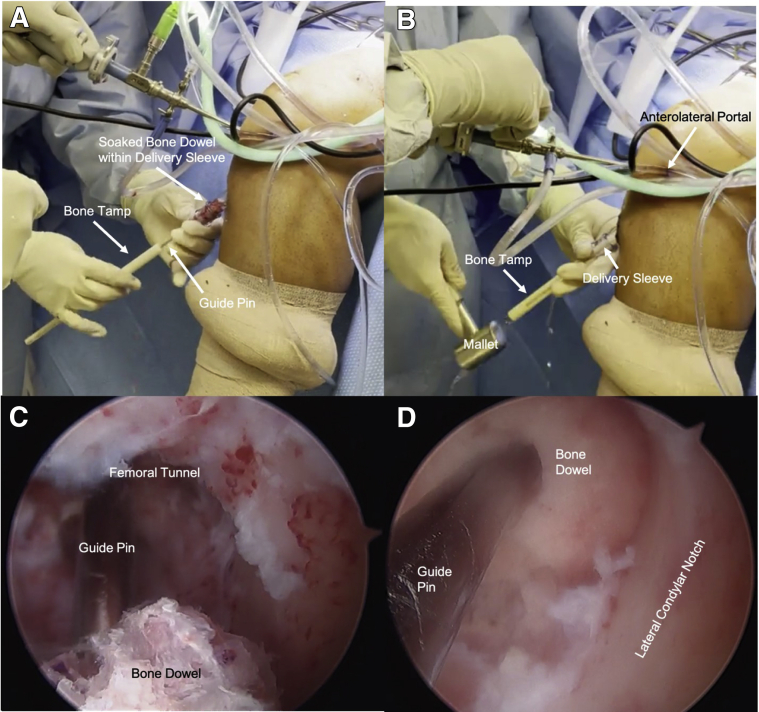
Fig 6.
Placing the bone dowel into the femoral tunnel in a left knee. While maintaining 90° of left knee flexion, the cannulated bone dowel that is soaked in bone marrow aspirate concentrate (BMAC) is inserted over the guide pin and into the delivery sleeve. The bone tamp is then inserted through the delivery sleeve behind the bone dowel (A). The bone tamp is used to advance the bone dowel into the joint space. A mallet is used to gently impact the tamp (B). Arthroscopic visualization through the anteromedial portal confirms advancement of the 10-mm bone dowel (C). Arthroscopic visualization through the anteromedial portal, confirming the 10-mm cannulated bone dowel soaked in BMAC sits slightly proud within the femoral tunnel (D).
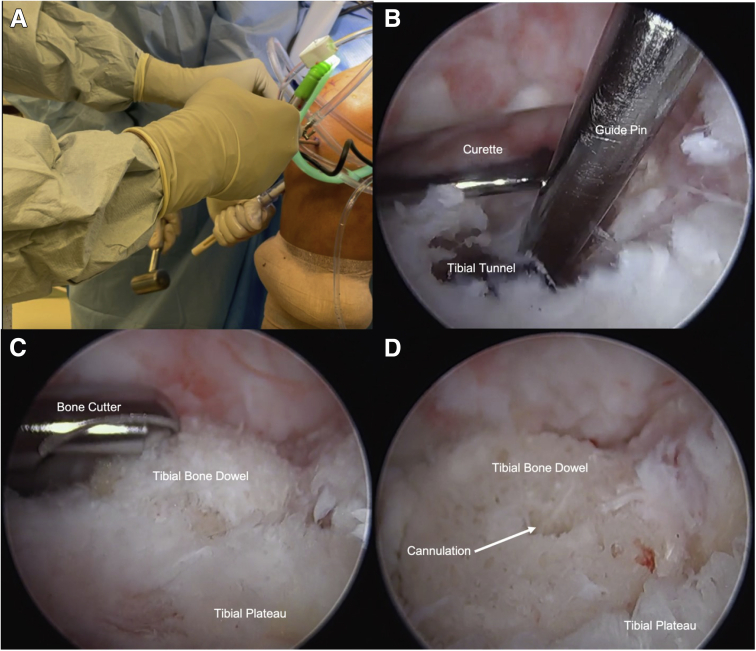
Fig 7.
Placing the bone dowels into the tibial tunnel in a left knee. Mallet is used to gently impact the bone tamp as it advances the 12-mm bone dowel into the tibial tunnel of the left knee (A). While the bone dowel is advanced into the defect, a large curette is inserted through the anteromedial portal and is placed above the proximal tibial tunnel opening to provide a roof and avoid advancing the bone dowel too far into the joint space (B). Arthroscopic visualization through the anterolateral portal of the bone cutter used to contour the proud edges of the bone dowel to sit flush against the surface of the tibial plateau (C). Arthroscopic view through the anterolateral portal of the bone dowel sitting within the tibial tunnel after the bone cutter was used to contour the proud edges (D).
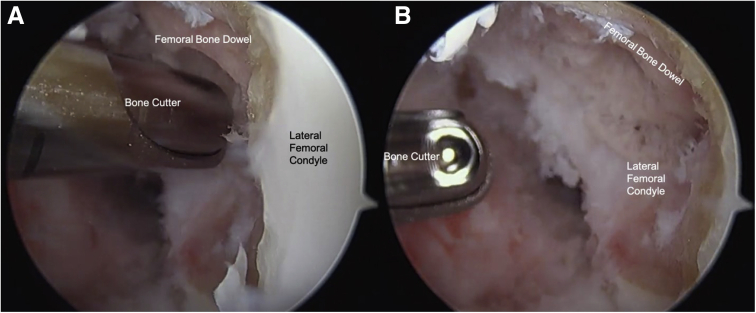
Fig 8.
Arthroscopic visualization through the anterolateral portal of the bone cutter used to contour the proud edges of the bone dowel to sit flush against the surface of the left lateral femoral condyle (A). Arthroscopic visualization through the anterolateral portal of the bone dowel sitting within the femoral defect after contouring the edges with a bone cutter (B).
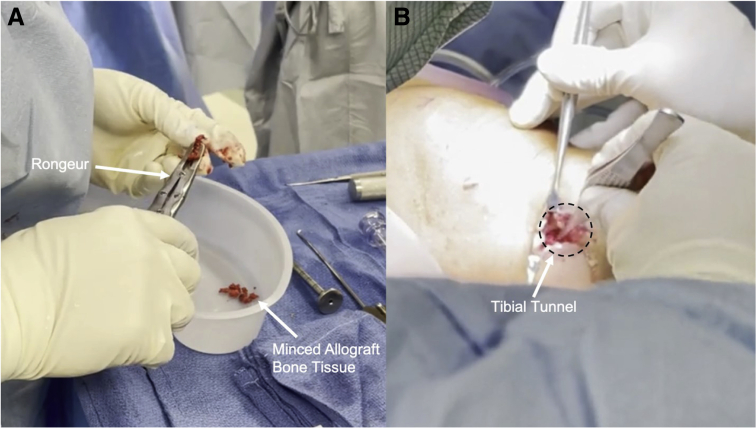
Fig 9.
A rongeur is used to mince allograft bone tissue that is soaked in bone marrow aspirate concentrate into a sterile basin (A). The minced allograft bone tissue is packed into the distal aspect of the tibial tunnel of the left leg prior to closure (B).
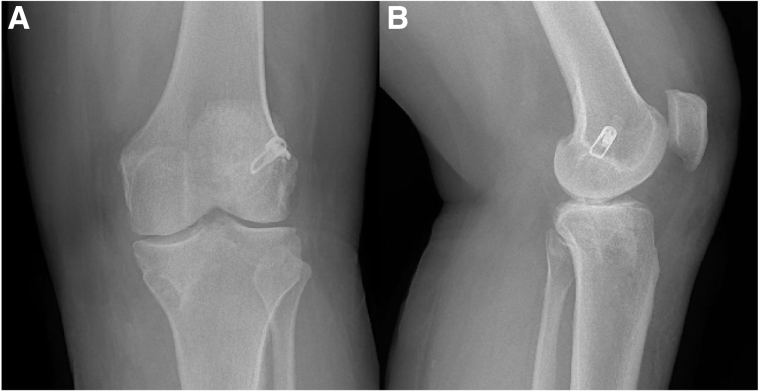
Fig 10.
Postoperative anteroposterior (AP) radiograph of the left knee (A). Postoperative lateral radiograph of the left knee (B).
Table 1.
Peals and Pitfalls of the Technique
| Pearls | Pitfalls |
|---|---|
| Using computed tomography preoperatively will help to quantify tunnel enlargement and placement. | May need to consider using another technique if tunnel widening is greater than 18 mm in diameter |
| If possible, using prior tibial incision to access tibial tunnel will avoid creating an additional scar. | An additional surgical assistant may be required if a pneumatic limb positioner is not used during surgery. |
| If primary anterior cruciate ligament reconstruction (ACLR) was done via a transtibial approach, using a transtibial approach to ream and fill the femoral tunnel will avoid the need for an accessory far medial portal. | A transtibial approach to prepare the femoral tunnel may not be possible if the femoral tunnel is in anatomic position. |
| You can recreate a fresh tunnel by overreaming to create a normal cylindrical void that will enhance allograft integration. | |
| Reaming the femoral tunnel 1-mm size smaller than the tibial tunnel will help to reach a high-located femoral tunnel through the tibial tunnel if a previous transtibial approach was used for initial ACLR | |
| Insert arthroscope through the tibial tunnel to assess for presence and location of bioabsorbable screw remnants. | |
| Clean the sclerotic and fibrous tissue out of the tunnel prior to dowel placement. | |
| Soak appropriately sized dowel in platelet-rich plasma or bone marrow aspirate concentrate to enhance healing and integration of allograft tissue. | |
| Resect prominence of bone dowel with bone cutter to ensure proper contour and a smooth notch anatomy. |
Table 2.
Advantages and Limitations of the Technique
| Advantages | Limitations |
|---|---|
| No donor site morbidity | Two-stage procedure |
| Technically simple and quick bone-grafting procedure | Transtibial approach not possible if previous femoral tunnel was in anatomic position |
| Cannulated design ensures precise and secure placement. | Expense of allograft |
| Maximizes potential for integration of allograft with the possibility to soak in platelet-rich plasma or bone marrow aspirate concentrate | High-load activity restriction after first stage |
| Replaces bony void | Increased time of return to sport due to delay of second stage |
| Optimizes bone tunnel placement for revision anterior cruciate ligament reconstruction |
Postoperative Rehabilitation:
Rehabilitation following the initial stage of this two-stage procedure is similar to standard post-ACLR protocols with minor differences. Early goals include restoring passive range of motion, restoring quadriceps muscle strength, and reducing swelling. Patients should be weight bearing as tolerated (WBAT) with crutches for 2 weeks while wearing a knee brace. There is no maximal flexion range of motion restriction. A stepwise progression is made at ∼6 weeks postoperatively when the patient demonstrates full range of motion and minimal joint effusion, in which low-load, high-repetition exercises are recommended. These exercises include walking on a treadmill, resistance biking, and swimming with short fins. It is important to avoid high-load and multiplanar activities in order to minimize risk of meniscus and cartilage damage.
The second stage of this procedure should be performed once the bone grafted tunnels demonstrate adequate healing by plain radiographs. This usually occurs at around 4 to 6 months postoperatively. However, each patient will vary depending on the size of initial ACLR tunnels. In summary, the main difference in rehabilitation between a standard ACLR and a two-staged ACLR procedure is the avoidance of high-load muscular strength exercises and increased time to return to sports in the staged procedure.
Discussion
A two-stage procedure for revision ACLR is considered when there is evidence of tunnel enlargement or nonanatomic tunnel position that will interfere with the position of the new tunnels.11.14 Evidence has shown that in these instances, the optimization of the new graft hardware and tendon bone healing is a challenge.7,15 The advantage of a staged procedure allows for an initial bone grafting procedure to replenish the bone stock.9 A study by Mitchel et al., with 88 patients, found no difference in objective outcomes and subjective patient scores and satisfaction when comparing single-stage and two-staged revision cases.16 The current bone-grafting technique using cannulated allograft bone dowels soaked in BMAC with a user-friendly delivery system is a safe and reliable method to optimize the potential for graft to bone healing and more accurate anatomic tunnel placement for the revision.
In this article, we describe a simple and efficient technique to bone grafting with cannulated bone dowels that has advantages over other techniques. First, the nature of using allograft tissue avoids donor site morbidity associated with surgical harvesting of autograft bone.3 Secondly, when tunnel expansion is present the tunnels are typically irregular.17 By overreaming the initial tunnels, a new fresh cylindrical tunnel can be created and is measured accurately to the size of an appropriate dowel. If the previous high-located femoral tunnel was created through a transtibial approach, the preparation of the femoral tunnel during the first stage can be reached through the tibial tunnel, avoiding the necessity for an accessory far medial portal. Additionally, the availability of a variety of premeasured dowels circumvents the need for preparation of allograft bone matrix or putty intraoperatively. This significantly reduces operative time and simplifies the surgical procedure. The dowel revision kit (Arthrex, Naples, FL) also comes readily available with a guide pin and delivery sleeve that allows the guide pin to stay in the tunnel during impaction. This provides secure placement of the dowel within the tunnel without creating any additional risk of releasing the dowel into the joint space. Moreover, the guide pin offers central stability during impact, as to avoid eccentric forces that can lead to improper placement or even fracture of the dowels. Additionally, the bone dowels provide immediate structure to the bony void. Finally, the bone dowels can be soaked in platelet-rich plasma (PRP) or BMAC, allowing growth factors and cells to augment the incorporation of the bone dowel scaffold.13
We recognize few limitations of this technique, including that the capacity for bone healing may be decreased in allograft bone tissue, as compared to autograft. In addition, the maximum diameter of the commercially available bone dowels is 18 mm, so the ability to use this particular biologic may be limited in defects larger than 18 mm.
In the face of a variety of treatment options, we believe this two-stage approach to revision ACLR with cannulated allograft bone dowels soaked in BMAC provides significant advantages over other options with minimal risk of complications. Additional studies are required to describe the long-term patient outcomes of this technique, which will provide meaningful guidance to optimize two-stage revision ACLR.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C. reports personal fees from Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the bone-grafting technique for a staged revision anterior cruciate ligament reconstruction using cannulated allograft bone dowels soaked in bone marrow aspirate concentrate.
References
- 1.Mall N.A., Chalmers P.N., Moric M., et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 2.Mayr R., Rosenberger R., Agraharam D., Smekal V., El Attal R. Revision anterior cruciate ligament reconstruction: An update. Archiv Orthopaed Trauma Surg. 2012;132:1299–1313. doi: 10.1007/s00402-012-1552-1. [DOI] [PubMed] [Google Scholar]
- 3.Buyukdogan K., Laidlaw M.S., Miller M.D. Two-stage revision anterior cruciate ligament reconstruction using allograft bone dowels. Arthrosc Tech. 2017;6:e1297–e1302. doi: 10.1016/j.eats.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanders T.L., Maradit Kremers H., Bryan A.J., et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med. 2016;44:1502–1507. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 5.Wilde J., Bedi A., Altchek D.W. Revision anterior cruciate ligament reconstruction. Sports Health. 2014;6:504–518. doi: 10.1177/1941738113500910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ding D.Y., Zhang A.L., Allen C.R., et al. Subsequent surgery after revision anterior cruciate ligament reconstruction: Rates and risk factors from a multicenter cohort. Am J Sports Med. 2017;45:2068–2076. doi: 10.1177/0363546517707207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamath G.V., Redfern J.C., Greis P.E., Burks R.T. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 8.Ahn J.-H., Son D.-W., Jeong H.-J., Park D.-W., Lee I.-G. One-stage anatomical revision anterior cruciate ligament reconstruction: Results according to tunnel overlaps. Arthroscopy. 2021;37:1223–1232. doi: 10.1016/J.ARTHRO.2020.11.029. [DOI] [PubMed] [Google Scholar]
- 9.Chahla J., Dean C., Cram T., et al. Two-stage revision anterior cruciate ligament reconstruction: bone grafting technique using an allograft bone matrix. Arthrosc Tech. 2016;5:e189–e195. doi: 10.1016/j.eats.2015.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Said H, Baloch K, Green M. A new technique for femoral and tibial tunnel bone grafting using the OATS harvesters in revision anterior cruciate ligament reconstruction.2006;22:796.e1-3. [DOI] [PubMed]
- 11.Thomas N.P., Kankate R., Wandless F., Pandit H. Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med. 2005;33:1701–1709. doi: 10.1177/0363546505276759. [DOI] [PubMed] [Google Scholar]
- 12.Büyükdoğan K., Laidlaw M.S., Kew M.E., Miller M.D. Allograft bone dowels show better incorporation in femoral versus tibial tunnels in 2-stage revision anterior cruciate ligament reconstruction: A computed tomography-based analysis. Arthroscopy. 2021;37:1920–1928. doi: 10.1016/J.ARTHRO.2021.01.066. [DOI] [PubMed] [Google Scholar]
- 13.Orthobiologics Next Generation in Biologics Technology. Arthrex. Updated January 2021. Available at: https://www.arthrex.com/resources/catalogs/XJUin6xx0EakTwE9WsNseg/orthobiologics-next-generation-in-biologics-technology-i-2021. Accessed May 21, 2021.
- 14.Oetgen M.E., Smart L.R., Medvecky M.J. A novel technique for arthroscopically assisted femoral bone tunnel grafting in two-stage ACL revision. Orthopedics. 2008;31:16–18. doi: 10.3928/01477447-20080101-31. [DOI] [PubMed] [Google Scholar]
- 15.Rodeo S.A., Kawamura S., Kim H.J., Dynybil C., Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: An effect of graft-tunnel motion? Am J Sports Med. 2006;34:1790–1800. doi: 10.1177/0363546506290059. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell J.J., Chahla J., Dean C.S., Cinque M., Matheny L.M., LaPrade R.F. Outcomes after 1-stage versus 2-stage revision anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:1790–1798. doi: 10.1177/0363546517698684. [DOI] [PubMed] [Google Scholar]
- 17.Battaglia T.C., Miller M.D. Management of bony deficiency in revision anterior cruciate ligament reconstruction using allograft bone dowels: Surgical technique. Arthroscopy. 2005;21 doi: 10.1016/j.arthro.2005.03.029. 767.e1-767.e5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the bone-grafting technique for a staged revision anterior cruciate ligament reconstruction using cannulated allograft bone dowels soaked in bone marrow aspirate concentrate.
This video demonstrates the bone-grafting technique for a staged revision anterior cruciate ligament reconstruction using cannulated allograft bone dowels soaked in bone marrow aspirate concentrate.