Abstract
We describe the case of a 33-year-old female smoker who presented to the Accident and Emergency department with a 1-day history of rapidly evolving airway compromise. She had no preceding illness or other objective signs/symptoms on presentation, had a history of Chronic Obstructive Pulmonary Disease (COPD) and a previous opioid addiction. Following failed endotracheal intubation, the airway was secured with an emergency surgical tracheostomy. Subsequent direct laryngoscopy revealed a severely diseased glottis and supraglottic area, from which biopsy samples revealed a multiple drug-resistant strain of Candida albicans requiring specialist microbiology input and antifungal treatment. We describe the presentation, investigation, management and outcome of this rare case, along with a literature review of the subject.
Keywords: ear, nose and throat/otolaryngology, anaesthesia
Background
Aggressive fungal disease affecting the larynx is rare and the treatment of airway obstruction secondary to any infection must first ensure that patients’ airways are stabilised and secured. Diagnostic investigation should include tissue biopsies of abnormal areas for both histological and microbiological analysis, followed by prompt treatment with targeted antimicrobial therapy. If tracheostomy has been required, plans for early decannulation should be made once the airway obstruction has been treated and reversed. Serial photographic and video documentation of the airway are essential in guiding ongoing management.
While airway obstruction secondary to this type of infection has been reported previously in the literature, the durations have been short and reversible, with Infections responding to prompt antifungal treatment. However, in this case, late presentation with a multiple-drug resistant strain of Candida albicans, delayed commencement of antifungal treatment and poor patient compliance led to chronic infection and inflammation causing irreversible airway obstruction.
Case presentation
A 33-year-old woman presented to the emergency department with a 1-day history of worsening stridor and airway compromise. There were no associated signs/symptoms and no preceding illness or antibiotic use. She had a medical history of chronic obstructive airway disease treated with salbutamol and steroid inhalers and a previous opioid addiction treated with methadone.
She had no previous contact with otolaryngology services, had no known drug allergies and was a heavy smoker and alcohol drinker.
Investigations
The patient’s symptoms did not respond to nebulised epinephrine and intravenous dexamethasone within 30 min of presenting to Accident and Emergency and due to her oxygen saturations deteriorating despite high flow oxygen, the patient was transferred to theatre for endotracheal intubation and examination in a safe environment. Members of the otolaryngology team were present should a surgical airway have been required.
Only a Cormack-Lehane grade 4 view of the larynx could be obtained by both the anaesthetic and otolaryngology team by video laryngoscopy under topical anaesthesia (10% Xylocaine) and muscle relaxants (figures 1 and 2). At this point, the supraglottis and glottis were noted to be extremely oedematous and inflamed. Unfortunately, laryngospasm was precipitated and the patient’s airway deteriorated. As attempts at intubation using a Storz rigid ventilating bronchoscope were unsuccessful, an emergency surgical tracheostomy was performed in the standard fashion.
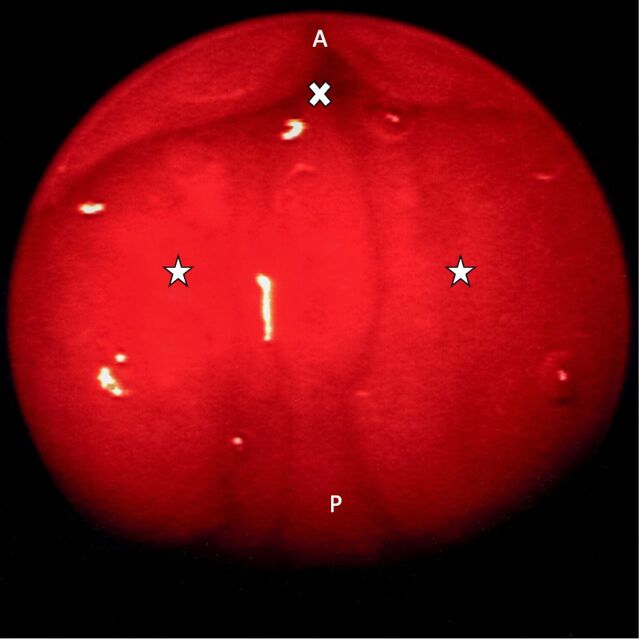
Figure 1.
Endoscopic view of the supraglottis. Stars—grossly oedematous and inflamed supraglottis, Cross—entrance to glottis. A, anterior; P, posterior.
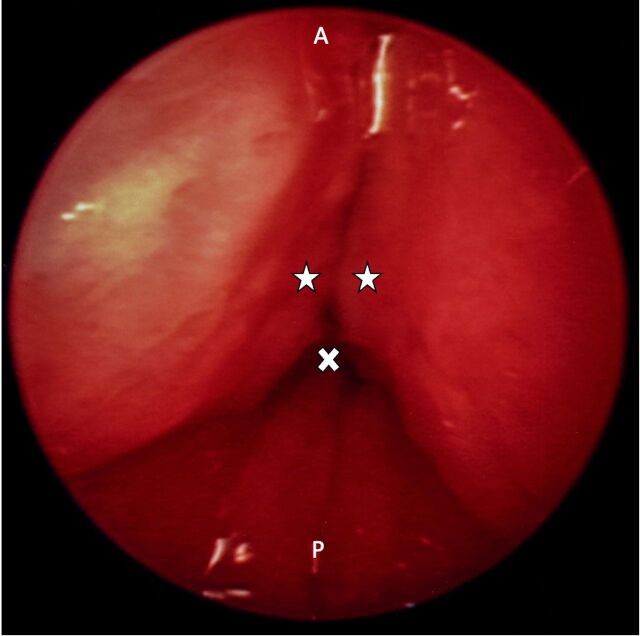
Figure 2.
Endoscopic view of the Glottis. Stars—grossly oedematous and inflamed true vocal cords, cross—Glottis. A, anterior; P, posterior.
Subsequent direct laryngoscopy revealed a grossly swollen supraglottis and neither the glottis or lower airway could be visualised. Biopsy samples were taken from the posterior commissure as well as the left and right arytenoids to investigate the underlying disease process, which was felt at this time to be either bacterial infection or malignancy.
Differential diagnosis
The principal differential diagnosis was supraglottic malignancy extending into the glottis, causing airway obstruction. This was based on the patient’s extensive smoking history and ongoing chronic obstructive pulmonary disease. Another differential diagnosis was bacterial or fugal supraglottitis based on the short history of stridor and its worsening nature.
Treatment
The patient was subsequently transferred to the intensive care unit for ventilatory support and ongoing medical management. A postoperative chest X-ray was performed to exclude subcutaneous emphysema, pneumothorax or additional pulmonary parenchymal pathology. Biopsy samples subsequently excluded malignancy and demonstrated the presence of widespread C. albicans infection (figure 3), prompting microbiology input on an extended course of antifungal medication.
Figure 3.
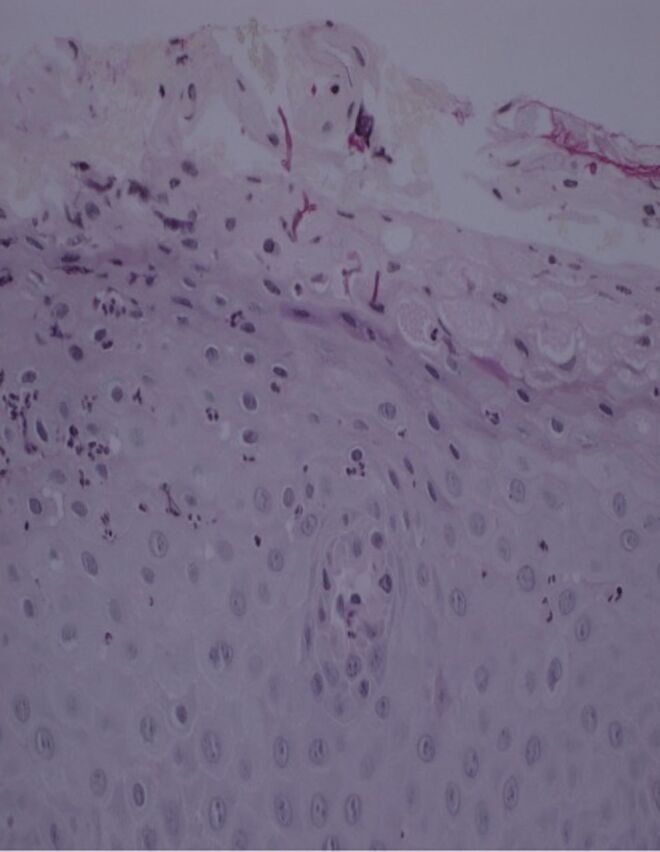
Microscopy demonstrating Candida pseudohyphae.
Outcome and follow-up
Due to the oedema caused by ongoing, chronic drug-resistant C. albicans infection, the patient remained tracheostomy dependent, failing trials of tracheostomy decannulation on four occasions due to resulting respiratory distress from chronic severe laryngeal inflammation. Unfortunately, longer-term follow-up was not possible as the patient died a few months after discharge from hospital, from unrelated causes.
Discussion
Fungal infection of the larynx is uncommon and usually develops following inhaled corticosteroid use or in those patients who are immunocompromised and at greater risk of developing rare and opportunistic infections. Airway obstruction as a consequence of laryngeal candidiasis has been reported previously, both in adults and children.1–3 Such infections are all reported to have resolved with antifungal treatment with or without interventional airway surgery. While repeated airway debridement of candidal deposits has been reported, only one report of emergency tracheostomy insertion exists.4
Airway obstruction due to laryngeal infection usually has a bacterial aetiology, with Gram positive cocci being the most commonly identified pathogen. Infections of this nature usually respond to resuscitative measures, including empirical, broad-spectrum antibiotics and corticosteroid treatment (provided either intravenously or topically). Those cases not responding to these measures are usually managed with intubation allowing further investigation and treatment to be provided in the presence of a secure airway. The option of tracheostomy insertion in a controlled environment under general anaesthetic also remains available. It is rare that genuine emergency surgical tracheostomies are required for infective airway obstruction as patients can usually be anaesthetised and intubated or tolerate tracheostomy insertion under sedation or while awake with local anaesthesia.
Laryngeal candidiasis is usually seen in conjunction with either pharyngeal or pulmonary candidiasis,5 with isolated laryngeal deposits being uncommon. The most common anatomical sites for candidal deposits are the arytenoids, vestibular folds, ventricles (as in our case) and glottis. Less commonly, deposits have been reported in the epiglottis, subglottis and trachea.1 2 6 On reviewing these individual case reports, there does not appear to be an association with the anatomical site of candidal deposits and patients’ symptoms as seen in cases of neoplastic disease.
The gold-standard management of laryngeal candidiasis is with azole antifungals and by managing any predisposing factors. These have replaced amphotericin B as first-line treatments due to their reduced hepatotoxicity and nephrotoxicity, though amphotericin can still be used in cases of aggressive or resistant disease.
A significant number of conditions are associated with development of candidiasis. Those cases of laryngeal candidiasis causing airway obstruction that have been reported discuss patients who are immunocompromised rather than those using inhaled corticosteroids to manage airway disease.2 3 7 8 The exception is a case reported by Henry et al where a young immunocompetent individual required temporary tracheostomy insertion to bypass the extent of obstruction. This obstruction resolved following antifungal treatment and decannulation was achieved at an early stage without complication, in contrast to this case.
Other fungal infections of the larynx have been reported, including blastomycosis, histoplasmosis and coccidioidomycosis. Other than candidiasis, only laryngeal aspergillosis has been reported as causing airway obstruction. Nakahira et al reported a case associated with CD4 +T lymphocyte immunodeficiency, which fully resolved following surgical excision of the deposit and 4 weeks treatment with oral itraconazole.9 Swiss et al reported a case of advanced Aspergillus infection destroying the larynx resulting in laryngotracheal separation.10 While the patient survived the infection following treatment with intravenous antibiotics, antifungals and granulocyte macrophage colony-stimulating factor, a permanent tracheo-cutaneous fistula was required to be formed.
Candidiasis can distort the appearance of the larynx to the extent that it has been mistaken for carcinoma, dysplasia, granulomatous disease or laryngopharyngeal reflux-related disease. However, long-term tracheostomy use has not been reported due to the essentially reversible nature of the infection and the high success in disease eradication encountered with antifungal treatment, avoidance of risk factors and management of patients’ immunosuppressive states.
Indeed, this case illustrates a rare presentation of aggressive fungal disease affecting the larynx requiring emergency surgical tracheostomy and a multidisciplinary approach to management over a long period of time. Due to the extent and resistance of the disease, along with certain patient factors, the patient responded poorly to treatment and was unable to be decannulated multiple times. This is rare and contrasting to the literature.
Learning points.
Undertreatment of laryngeal candidiasis can lead to airway obstruction and in rare cases, multidrug resistance.
Airway obstruction can become severe and require emergency front-of-neck access to manage situations where non-invasive ventilation or endotracheal intubation fail to overcome the obstruction.
Poor treatment compliance in cases of multiple drug-resistant candida infections can lead to chronic and irreversible laryngeal obstruction, requiring tracheostomy dependence.
A multidisciplinary team approach to cases such as this between surgeons, anaesthetics, medics and microbiology is essential in achieving positive outcomes.
Footnotes
Contributors: Case identification: SCM and DLW. Literature search: SCM, CSCGT and MB. Manuscript writing - SCM, CSCGT, DLW and MB. Manuscript proofing/checking: SCM, CSCGT, DLW and MB.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Spear RK, Walker PD, Lampton LM. Tracheal obstruction associated with a fungus ball. A case of primary tracheal candidiasis. Chest 1976;70:662–3. 10.1378/chest.70.5.662 [DOI] [PubMed] [Google Scholar]
- 2.Colman MF. Epiglottitis in immunocompromised patients. Head Neck Surg 1986;8:466–8. 10.1002/hed.2890080612 [DOI] [PubMed] [Google Scholar]
- 3.Fisher EW, Richards A, Anderson G, et al. Laryngeal candidiasis: a cause of airway obstruction in the immunocompromised child. J Laryngol Otol 1992;106:168–70. 10.1017/S0022215100118997 [DOI] [PubMed] [Google Scholar]
- 4.Henry LR, Packer MD, Brennan J. Airway-obstructing laryngeal candidiasis in an immunocompetent host. Otolaryngol Head Neck Surg 2005;133:808–10. 10.1016/j.otohns.2004.10.017 [DOI] [PubMed] [Google Scholar]
- 5.Neuenschwander MC, Cooney A, Spiegel JR, et al. Laryngeal candidiasis. Ear Nose Throat J 2001;80:138–9. 10.1177/014556130108000306 [DOI] [PubMed] [Google Scholar]
- 6.Hass A, Hyatt AC, Kattan M, et al. Hoarseness in immunocompromised children: association with invasive fungal infection. J Pediatr 1987;111:731–3. 10.1016/S0022-3476(87)80254-8 [DOI] [PubMed] [Google Scholar]
- 7.Ganesan S, Harar RP, Dawkins RS, et al. Invasive laryngeal candidiasis: a cause of stridor in the previously irradiated patient. J Laryngol Otol 1998;112:575–8. 10.1017/S0022215100141131 [DOI] [PubMed] [Google Scholar]
- 8.Jeena PM, Bobat R, Kindra G, et al. The impact of human immunodeficency virus 1 on largyngeal airway obstruction in children. Arch Dis Child 2002;87:212–4. 10.1136/adc.87.3.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakahira M, Matsumoto S, Mukushita N, et al. Primary aspergillosis of the larynx associated with CD4+ T lymphocytopenia. J Laryngol Otol 2002;116:304–6. 10.1258/0022215021910618 [DOI] [PubMed] [Google Scholar]
- 10.Swiss T, Cervantes SS, Hinni M, et al. Invasive fungal laryngopharyngitis resulting in laryngeal destruction with complete laryngotracheal separation: report of a case. Ear Nose Throat J 2017;96:E33–6. 10.1177/014556131709600105 [DOI] [PubMed] [Google Scholar]