Abstract
Patients with hypermobile Ehlers-Danlos syndrome commonly present with painful shoulder disorders mostly represented by a multidirectional instability and with often painless episode of atraumatic shoulder dislocation and/or subluxation. Because of the generalized soft tissue fragility, most of the surgical treatments of shoulder instability, as the Bankart repair or the Latarjet procedure becomes not effective, exposing a risk of failure. Then, capsular plication has to be considered in order to reduce the articular joint volume and to diminish the mobility of the joint. Two main benefits of this surgical procedure are that it doesn’t modify the anatomy or damage the labrum or cartilage that is healthy. The purpose of this Technical Note is to present the arthroscopic capsular plication for the treatment of patient with hypermobile Ehlers-Danlos syndrome, which is associated with a multidirectional shoulder instability.
Technique Video
After a first arthroscopic exploration of the glenohumeral joint, the first plication is initiated at the inferior capsule using the passing suture technique. Plications are performed with a nonabsorbable suture threads and with the arm maintained in 30° of abduction and forward flexion with a neutral rotation. The anterior capsular tissue is then assessed with the realization of two anterior plication at 3 o’clock and 5 o’clock position. Passing the arthroscope through the anterior portal, two other posterior capsular plications are then performed passing the suture thread through the posterior portal. Intraoperative drive-through test is eventually used, and additional capsular plication can be added if needed.
Introduction
Since its first description in 1892, the types of Ehlers-Danlos syndromes (EDS) have increased up to 13 different types nowadays, and the hypermobile type is the most prevalent.1 The incidence of this rare condition affecting all tissues and characterized by joint hypermobility and soft tissue fragility is estimated about 1/2,500 live births.2
The diagnostic and management of young patients with generalized ligamentous hyperlaxity in Ehlers-Danlos hypermobile (h-EDS) syndrome remain challenging. Most of these patients mostly complain of shoulder instability symptoms,3 and a shoulder dislocation is often the first symptom. In particular, EDS may be suspected after a first dislocation in a young girl, who presents painless atraumatic dislocation with pain after reduction, with a generalized hyperlaxity and possibly a shoulder hyperlaxity, formerly defined as external rotation over 85°.4 This explains why an orthopedist is often the first practitioner who diagnoses and treats this condition.
Diagnosis of general joint hyperlaxity is based on the Beighton criteria, which is only one element of h-EDS diagnosis.5,6
These patients are more prone to present clinically with a multidirectional shoulder instability (MDSI), which led to transpose the surgical treatment of these patients with the numerous procedures described for the MDSI.7 Unfortunately, it is often a failed standard surgery for shoulder instability must lead also to consider the probability of h-EDS.7,8 And because of the high failure rate, the treatment must first include a conservative management with specific physiotherapy, pain management, and multidisciplinary clinics before considering a surgical procedure.
The objective of this work is to present a stepwise approach of the realization of an arthroscopic capsular plication for multidirectional instability of the shoulder to stabilize and to purse string the whole anterior, inferior, and posterior capsule of the glenohumeral joint (Video 1). The main clinical outcome for these patients is a decrease of pain and rarely consists in a perfect stabilization of the shoulder.
Surgical Technique
Clinical Diagnosis and Imaging
The clinical exam must include a complete interrogatory of all the shoulder instability problems present by the patient. The real dislocation episodes must be separate from the recurrent shoulder instability accidents due to repetitive subluxations. The traumatic or atraumatic component of the shoulder instability must also me analyzed. The voluntary aspect of the shoulder instability episode must be researched and may compose a contraindication for this treatment. The multidirectional aspect of the shoulder instability is evaluated with the constatation of most of these following clinical signs: anterior and/ or posterior withdraw, anterior and/or posterior apprehension test, a sulcus sign, a Gagey sign and concomitant clinical signs of joint hyperlaxity according to the Beighton criteria. The indication of this procedure can be transposed to patient affected with multidirectional shoulder instability when the conservative treatment failed to stabilize the glenohumeral joint. After a standard plain X-ray radiographs to eliminate the presence of bony lesion, an arthro-CT-scan or and arthro-MRI is recommended to ensure the absence of a capsular labral complex lesion that must be treated, and the patulous redundant inferior capsule may be visualized. In this kind of patient there is not anatomical lesion.
Patient Positioning
The patient is placed in supine position to perform the procedure with the head positioned in a head-positioner. All patients have an interscalene block associated with the general anesthetic. The patient is positioned in a supine position with the whole upper limb included in the surgical field and with the medial side of the scapula resting on the operating table. A Spider 2 limb positioner (Smith & Nephew, Watford, UK) can be used to fix the upper limb of the patient during the surgical procedure and to apply specific arm positioning to facilitate the exposure during the arthroscopy. Main indications and contraindications for arthroscopic capsular plication for a patient with multidirectional shoulder instability are presented in Table 1. For those patients with fragile tissues, specific attention must be given not to pull too strongly on nerves to prevent frequent injuries. Anesthesiology is also specific regarding tissue fragility during intubation, and pain management is also challenging, as patients are in most of cases used to taking a sizable dose of painkiller.
Table 1.
Main Indications and Contraindications for Arthroscopic Capsular Plication for P:atient with Multidirectional Shoulder Instability
| Indications | Contraindications |
|---|---|
|
|
Surgical Procedure
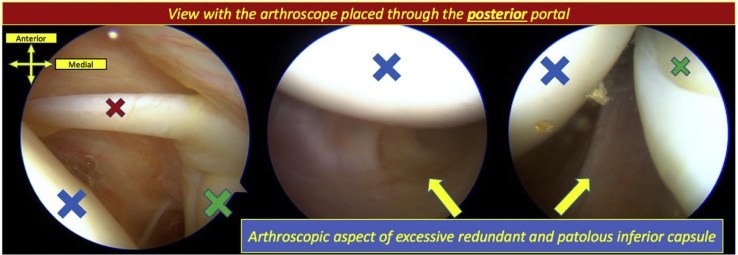
The procedure began with a complete diagnostic arthroscopy of the glenohumeral joint and the visualization of a patulous capsule using a standard posterior and anterior portal through the rotator interval (Fig 1). Palpation with the probe can help find an incompetent labrum, both anteriorly and posteriorly, and is used to search for a labral tear. A canula is used during all of the procedures to prevent the loss of the suture threads in the soft tissues during the shuttle relay techniques.
Fig 1.
First step arthroscopic exploration of the glenohumeral joint for a h-EDS patient with a multidirectional shoulder instability. A patulous and redundant inferior capsule can be visualized, and the absence of capsular labral lesion needs to be assessed. The red cross indicates the long head of the biceps, the blue cross indicates the humeral head, and the green cross indicates the glenoid cavity. The patient is positioned in a supine position, and orientation is given.
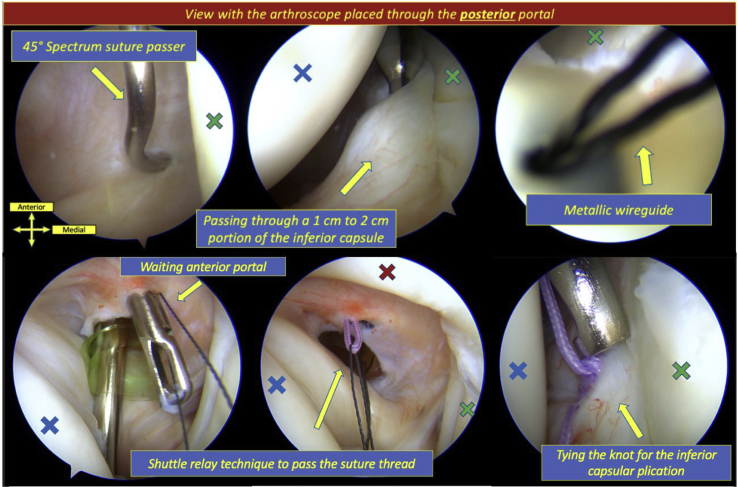
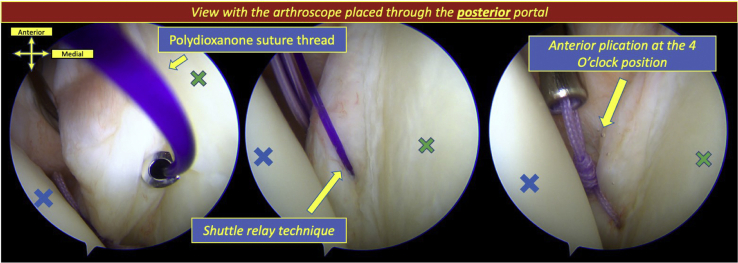
The inferior capsule is assessed first. The 45° spectrum suture passer (CONMED, New York, NY) is then used with a loaded shuttle relay to penetrate the inferior capsular tissue. A waiting anterior instrumental portal is established close to the anterior portal. A first inferior capsular plication is performed on a length of approximately 1 to 2 cm at the 6 o’clock position using a passing suture with a shuttle relay wireguide. A nonabsorbable suture (ORTHOCORD, Dupuy Synthes, West Chester, PA) is passed by the instrumental portal and then through the capsular tissue to realize the plication. At this step, it is detrimental not to go to deeper below the capsule and just under its surface, to prevent axillary nerve lesion. Several half hitch knots are performed extra-articularly, and the knot is slid to be tied intra-articularly (Fig 2). All of the plications are performed with the arm position in neutral rotation and with the upper limb maintained at 30° of forward flexion and 30° of abduction to prevent the risk of excessive postoperative loss of motion. The shuttle relay technique can either be performed using a metallic wireguide or a no. 0 polydioxanone suture thread (ETHICON, Johnson & Johnson, Cincinnati, OH) to pass the nonabsorbable suture threads (Fig 3). The anterior capsular tissue is then assessed. Using the same technique, we performed two other plications of approximately 1 cm, which were tightened approximately at the 4 o’clock and the 2 o’clock positions.
Fig 2.
The red cross indicates the long head of the biceps blue cross indicates the humeral head, and the green cross indicates the glenoid cavity. The patient is positioned in the supine position and the orientation are given.
Fig 3.
Realization of the first anterior capsular plication at the 4 o’clock position using the shuttle relay technique. The blue cross indicates the humeral head and the green cross indicates the glenoid cavity. The patient is positioned in supine position and orientation is given.
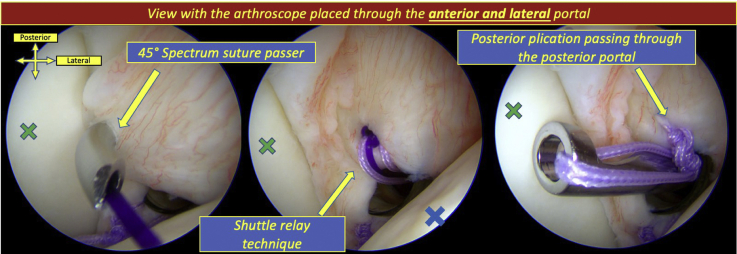
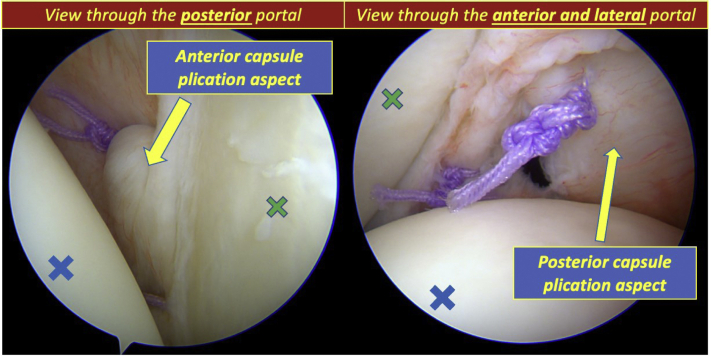
Passing the arthroscope through the anterior portal, the posterior capsular plication is performed with two other intra-articular knots. After passing a cannula through the posterior portal, the first plication is performed using the spectrum hook and passing the suture thread through the posterior portal (Fig 4). After tying the knot, a second posterior capsular plication can be performed just above at the 9 o’ clock position. After the plications, the patient is assessed with a drive-through test, and supplementary plication is performed if needed. We do not perform a closure of the rotator interval during the procedure. At the end of the procedure a good reduction of the capsular volume can be visualized (Fig 5). Main advantages and disadvantages of the arthroscopic capsular plication compared with the open techniques are presented in Table 2 as pearls and pitfalls are shown in Table 3.
Fig 4.
Realization of the first posterior capsular plication at the 7 o’clock position. The suture thread is passed through the posterior portal. The blue cross indicates the humeral head and the green cross indicates the glenoid cavity. The patient is positioned in supine position and orientation is given.
Fig 5.
Final aspect of the anterior and posterior arthroscopic capsular plication of the glenohumeral joint. The blue cross indicates the humeral head, and the green cross indicates the glenoid cavity. The patient is positioned in a supine position, and the portal used for the arthroscope is given.
Table 2.
Main Advantages and Disadvantage of the Arthroscopic Capsular Plication Compared with the Open Techniques
| Advantages | Disadvantages |
|---|---|
|
|
Table 3.
Pearls and Pitfalls of the Arthroscopic Capsular Plication for Multidirectional Shoulder Instability
| Pearls | Pitfalls |
|---|---|
|
|
Rehabilitation
Following the procedure, patients are immobilized in an abduction shoulder sling immobilizer for a total of 10 days in order to control the pain and ensure healing of the skin incision sites. Immediate range of motion exercises of the elbow and the wrist are initiated, and pendulum exercises can be started after shoulder immobilization. The follow-up includes a physical exam at the third and the sixth weeks. Physiotherapy is not systematic but may be introduced if an excessive loss of motion or a muscular disorder (especially scapular dyskinesia) are observed after the sixth week and must include active and passive stretching, muscular reinforcement, and Liotard protocol.
Discussion
Patients with MDSI associated with h-EDS are often young and active patients with high demands and expectations concerning the function of their shoulder. Most of the time, conservative management has failed, and a high rate of noncompliance has been described for these patients.9 Thus, an effective, safe, and reliable surgical technique is necessary to compensate for the low success rate that has been reported in the literature.9,10
Because of the lack of published work on the treatment of the h-EDS, most of the proposed surgeries are extrapolated from data on MDSI, and many treatments have been yielded satisfying results.7 We can find the open capsular shift, arthroscopic capsular plication, capsule reinforcement, thermal shrinkage, or even bone procedures.11,12 Because of their poor outcomes and the high rate of complications, thermal shrinkage and laser-assisted capsulorraphy techniques should no more be recommended.11,13 It has been shown that both open capsular shift and arthroscopic plication are effective for treatment of MDSI.14,15 Vavken et al. studied the outcomes of the open capsular shift for the treatment of MDSI in patients with EDS or generalized ligamentous hyperlaxity, and they found an improvement in both objective and subjective shoulder function and stability after a failed conservative treatment.16 Witney-Lagen and colleagues studied the result of the arthroscopic plication for MDI of the shoulder on 50 consecutive patients who have not improved after at least 6 months of specialized physiotherapy for symptomatic MDSI with no labral lesion.17 Their arthroscopic capsular plication was performed using purse string knot with a limb at 5 o’clock through capsular tissue, and the second limb bringing the middle glenohumeral ligament toward the labrum at 3 o’clock. Forty-seven of the patients were satisfied, and 45 of them were able to return to sport at the same level. They experienced only 2 complications (one stiffness of the shoulder and one wound infection). Wiley et al. described the arthroscopic anteroinferior capsular plication as a treatment of MDSI to address the joint laxity with a patulous axillary pouch.18 In their technique, the proceeded to the capsular plication by placing the suture through the labrum, which differ from the arthroscopic technique described here. Because of the recurrent aspect of the shoulder instability found with EDS patients, the labrum is usually deficient and may have disappeared, which led us to believe that there is no need to involve the labrum in the repair, and there is also no acute capsule tear to repair. The restoration of a satisfied labral height is useless in order to recreate a concavity-compression effect.
In our opinion, it is not sensible to proceed to a surgery that may lead to an alteration of the cartilage, which can already be altered because of the anterior pathological aspect of the shoulder. Thus, the use of an implant inserted in the glenoid rim seems aberrant.
Concerning the posterior component of the MDSI, Kim et al. reported 30 good or excellent results for one patient with recurrent instability in their series of patients treated arthroscopically with a superior shift of the posteroinferior and anteroinferior capsule associated with a rotator interval closure and a posteroinferior labroplasty.19
For patients with h-EDS, the objective of the capsular plication is to reduce the capsular volume and to allow improved proprioception. In a cadaveric study, Sekiya et al. found that glenohumeral joint volume reduction with arthroscopic capsular plication was at least as efficient as with the standard open technique.20 Similarly, Alberta et al. concluded that arthroscopic plication was effective to reduce both anterior translation and external rotation using a 10-mm anteroinferior arthroscopic suture plication.21 Despite the fact that this procedure can be criticized because of the postoperative loss of range of motion for a patient playing sports without comorbidity, this consequence become an effective surgical strategy to treat patients with h-EDS associated with a MDSI. Most of these patients usually experience a significant rate of shoulder instability events, very painful shoulders, associated with a handicap and an excessive consumption of painkillers. Thus, the loss of range of motion that follows is well accepted by the patient for whom a glenohumeral fusion may represent the only surgical strategy to treat their symptoms and to eventually stabilize the joint. We consider this surgery in most cases as a surgery that can, temporarily, decrease painkiller use and the frequency of shoulder dislocation. In our experience, the failure rate is higher than in non-h-EDS patient, but it is a shoulder surgery that must be discussed in a multidisciplinary clinic. The main objective of this procedure is to decrease the symptoms of the patient more than getting a perfectly functional shoulder at all costs. Moreover, the patients are very young, and when surgery is not performed, many older patients recover naturally with time from the shoulder disorder. Thus, this surgery can be, in very specific cases, a way to decrease symptoms before improvement occurs naturally. That is why we do not touch the labrum or the cartilage.
We consider that the closure of the rotator interval is not necessary. Even though it could be advantageous for the anterior instability22,23 and the proprioception,24 it does not seem to improve significantly the inferior and the posterior instability. The main objective of the procedure remains to perform a global volume reduction of the glenohumeral joint to optimize the postoperative rehabilitation by improving the proprioception.
The conservative treatment of the EDS with shoulder instability must remain the first step. It must include a multidisciplinary approach, a reconditioning of the function of the shoulder, which includes an adapted reeducation, orthosis, and compressive clothing may be used to manage the pain. When it fails, the arthroscopic capsular plication must be considered for these patients to prevent recurrence of shoulder instability and to relieve pain.
Conclusion
The treatment of the multidirectional shoulder instability remains challenging for all patients, and even more challenging when patients are affected with h-EDS. By restricting the range of motion of the shoulder, the arthroscopic capsular plication of the glenohumeral joint is a procedure that can help to treat this complex condition. When the patient’s shoulder symptoms become too pressing, a glenohumeral joint fusion must be considered.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: This article is funded by COS Ramsay Santé, France. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
After a first arthroscopic exploration of the glenohumeral joint, the first plication is initiated at the inferior capsule using the passing suture technique. Plications are performed with a nonabsorbable suture threads and with the arm maintained in 30° of abduction and forward flexion with a neutral rotation. The anterior capsular tissue is then assessed with the realization of two anterior plication at 3 o’clock and 5 o’clock position. Passing the arthroscope through the anterior portal, two other posterior capsular plications are then performed passing the suture thread through the posterior portal. Intraoperative drive-through test is eventually used, and additional capsular plication can be added if needed.
References
- 1.Malfait F., Francomano C., Byers P., et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175:8–26. doi: 10.1002/ajmg.c.31552. [DOI] [PubMed] [Google Scholar]
- 2.Beighton P., De Paepe A., Steinmann B., Tsipouras P., Wenstrup R.J. Ehlers-Danlos syndromes: Revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK) Am J Med Genet. 1998;77:31–37. doi: 10.1002/(sici)1096-8628(19980428)77:1<31::aid-ajmg8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 3.Rombaut L., De Paepe A., Malfait F., Cools A., Calders P. Joint position sense and vibratory perception sense in patients with Ehlers-Danlos syndrome type III (hypermobility type) Clin Rheumatol. 2010;29:289–295. doi: 10.1007/s10067-009-1320-y. [DOI] [PubMed] [Google Scholar]
- 4.Nourissat G., Vigan M., Hamonet C., Doursounian L., Deranlot J. Diagnosis of Ehlers-Danlos syndrome after a first shoulder dislocation. J Shoulder Elbow Surg. 2018;27:65–69. doi: 10.1016/j.jse.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 5.Hakim A.J., Grahame R. Joint hypermobility. Best Pract Res Clin Rheumatol. 2003;17:989–1004. doi: 10.1016/j.berh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Hakim A.J., Sahota A. Joint hypermobility and skin elasticity: the hereditary disorders of connective tissue. Clin Dermatol. 2006;24:521–533. doi: 10.1016/j.clindermatol.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Johnson S.M., Robinson C.M. Shoulder instability in patients with joint hyperlaxity. J Bone Joint Surg Am. 2010;92:1545–1557. doi: 10.2106/JBJS.H.00078. [DOI] [PubMed] [Google Scholar]
- 8.Olds M., Ellis R., Donaldson K., Parmar P., Kersten P. Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: A systematic review and meta-analysis. Br J Sports Med. 2015;49:913–922. doi: 10.1136/bjsports-2014-094342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Misamore G.W., Sallay P.I., Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven to ten-year follow-up. J Shoulder Elbow Surg. 2005;14:466–470. doi: 10.1016/j.jse.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Kiss J., Damrel D., Mackie A., Neumann L., Wallace W.A. Non-operative treatment of multidirectional shoulder instability. Int Orthop. 2001;24:354–357. doi: 10.1007/s002640000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Longo U.G., Rizzello G., Loppini M., et al. Multidirectional instability of the shoulder: A systematic review. Arthroscopy. 2015;31:2431–2443. doi: 10.1016/j.arthro.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong M.D., Smith B., Coady C., Wong I.H. Arthroscopic anterior and posterior glenoid bone augmentation with capsular plication for Ehlers-Danlos syndrome with multidirectional instability. Arthrosc Tech. 2018;7:e541–e545. doi: 10.1016/j.eats.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D’Alessandro D.F., Bradley J.P., Fleischli J.E., Connor P.M. Prospective evaluation of thermal capsulorrhaphy for shoulder instability: Indications and results, two- to five-year follow-up. Am J Sports Med. 2004;32:21–33. doi: 10.1177/0095399703258735. [DOI] [PubMed] [Google Scholar]
- 14.Caprise P.A., Jr., Sekiya J.K. Open and arthroscopic treatment of multidirectional instability of the shoulder. Arthroscopy. 2006;22:112631. doi: 10.1016/j.arthro.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Jacobson M.E., Riggenbach M., Wooldridge A.N., Bishop J.Y. Open capsular shift and arthroscopic capsular plication for treatment of multidirectional instability. Arthroscopy. 2012;28:1010–1017. doi: 10.1016/j.arthro.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Vavken P., Tepolt F.A., Kocher M.S. Open inferior capsular shift for multidirectional shoulder instability in adolescents with generalized ligamentous hyperlaxity or Ehlers-Danlos syndrome. J Shoulder Elbow Surg. 2016;25:907–912. doi: 10.1016/j.jse.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 17.Witney-Lagen C., Hassan A., Doodson A., Venkateswaran B. Arthroscopic plication for multidirectional instability: 50 patients with a minimum of 2 years of follow-up. J Shoulder Elbow Surg. 2017;26:e29–e36. doi: 10.1016/j.jse.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Wiley W.B., Goradia V.K., Pearson S.E. Arthroscopic capsular plication-shift. Arthroscopy. 2005;21:119–121. doi: 10.1016/j.arthro.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.H., Kim H.K., Sun J.I., Park J.S., Oh I. Arthroscopic capsulolabroplasty for posteroinferior multidirectional instability of the shoulder. Am J Sports Med. 2004;32:594–607. doi: 10.1177/0363546503262170. [DOI] [PubMed] [Google Scholar]
- 20.Sekiya J.K., Willobee J.A., Miller M.D., Hickman A.J., Willobee A. Arthroscopic multi-pleated capsular plication compared with open inferior capsular shift for reduction of shoulder volume in a cadaveric model. Arthroscopy. 2007;23:1145–1151. doi: 10.1016/j.arthro.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Alberta F.G., Elattrache N.S., Mihata T., McGarry M.H., Tibone J.E., Lee T.Q. Arthroscopic anteroinferior suture plication resulting in decreased glenohumeral translation and external rotation. Study of a cadaver model. J Bone Joint Surg Am. 2006;88:179–187. doi: 10.2106/JBJS.D.02974. [DOI] [PubMed] [Google Scholar]
- 22.Hewitt M., Getelman M., Snyder S.J. Arthroscopic management of multidirectional instability: Pancapsular plication. Orthop Clin North Am. 2003;34:549–557. doi: 10.1016/s0030-5898(03)00094-4. [DOI] [PubMed] [Google Scholar]
- 23.Treacy S.H., Field L.D., Savoie F.H. Rotator interval capsule closure: An arthroscopic technique. Arthroscopy. 1997;13:103–106. doi: 10.1016/s0749-8063(97)90217-6. [DOI] [PubMed] [Google Scholar]
- 24.Moon Y.L., Singh H., Yang H., Chul L.K. Arthroscopic rotator interval closure by purse string suture for symptomatic inferior shoulder instability. Orthopedics. 2011;34:269. doi: 10.3928/01477447-20110228-02. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
After a first arthroscopic exploration of the glenohumeral joint, the first plication is initiated at the inferior capsule using the passing suture technique. Plications are performed with a nonabsorbable suture threads and with the arm maintained in 30° of abduction and forward flexion with a neutral rotation. The anterior capsular tissue is then assessed with the realization of two anterior plication at 3 o’clock and 5 o’clock position. Passing the arthroscope through the anterior portal, two other posterior capsular plications are then performed passing the suture thread through the posterior portal. Intraoperative drive-through test is eventually used, and additional capsular plication can be added if needed.
After a first arthroscopic exploration of the glenohumeral joint, the first plication is initiated at the inferior capsule using the passing suture technique. Plications are performed with a nonabsorbable suture threads and with the arm maintained in 30° of abduction and forward flexion with a neutral rotation. The anterior capsular tissue is then assessed with the realization of two anterior plication at 3 o’clock and 5 o’clock position. Passing the arthroscope through the anterior portal, two other posterior capsular plications are then performed passing the suture thread through the posterior portal. Intraoperative drive-through test is eventually used, and additional capsular plication can be added if needed.