Key Points
Question
What was the burden of cancer globally and across Sociodemographic Index (SDI) groupings in 2019, and how has incidence, morbidity, and mortality changed since 2010?
Findings
In this systematic analysis, there were 23.6 million new global cancer cases in 2019 (17.2 million when excluding those with nonmelanoma skin cancer), 10.0 million cancer deaths, and an estimated 250 million disability-adjusted life years estimated to be due to cancer; since 2010, these represent increases of 26.3%, 20.9%, and 16.0%, respectively. Absolute cancer burden increased in all SDI quintiles since 2010, but the largest percentage increases occurred in the low and low-middle SDI quintiles.
Meanings
The study results suggest that increased cancer prevention and control efforts are needed to equitably address the evolving and increasing burden of cancer across the SDI spectrum.
Abstract
Importance
The Global Burden of Diseases, Injuries, and Risk Factors Study 2019 (GBD 2019) provided systematic estimates of incidence, morbidity, and mortality to inform local and international efforts toward reducing cancer burden.
Objective
To estimate cancer burden and trends globally for 204 countries and territories and by Sociodemographic Index (SDI) quintiles from 2010 to 2019.
Evidence Review
The GBD 2019 estimation methods were used to describe cancer incidence, mortality, years lived with disability, years of life lost, and disability-adjusted life years (DALYs) in 2019 and over the past decade. Estimates are also provided by quintiles of the SDI, a composite measure of educational attainment, income per capita, and total fertility rate for those younger than 25 years. Estimates include 95% uncertainty intervals (UIs).
Findings
In 2019, there were an estimated 23.6 million (95% UI, 22.2-24.9 million) new cancer cases (17.2 million when excluding nonmelanoma skin cancer) and 10.0 million (95% UI, 9.36-10.6 million) cancer deaths globally, with an estimated 250 million (235-264 million) DALYs due to cancer. Since 2010, these represented a 26.3% (95% UI, 20.3%-32.3%) increase in new cases, a 20.9% (95% UI, 14.2%-27.6%) increase in deaths, and a 16.0% (95% UI, 9.3%-22.8%) increase in DALYs. Among 22 groups of diseases and injuries in the GBD 2019 study, cancer was second only to cardiovascular diseases for the number of deaths, years of life lost, and DALYs globally in 2019. Cancer burden differed across SDI quintiles. The proportion of years lived with disability that contributed to DALYs increased with SDI, ranging from 1.4% (1.1%-1.8%) in the low SDI quintile to 5.7% (4.2%-7.1%) in the high SDI quintile. While the high SDI quintile had the highest number of new cases in 2019, the middle SDI quintile had the highest number of cancer deaths and DALYs. From 2010 to 2019, the largest percentage increase in the numbers of cases and deaths occurred in the low and low-middle SDI quintiles.
Conclusions and Relevance
The results of this systematic analysis suggest that the global burden of cancer is substantial and growing, with burden differing by SDI. These results provide comprehensive and comparable estimates that can potentially inform efforts toward equitable cancer control around the world.
The Global Burden of Diseases, Injuries, and Risk Factors Study 2019 examines cancer burden and trends globally for 204 countries and territories and by Socio-demographic Index quintiles from 2010 to 2019.
Introduction
Cancers are a major contributor to disease burden worldwide, and projections forecast that global cancer burden will continue to grow for at least the next 2 decades.1,2,3,4 The United Nations (UN) Sustainable Development Goals (SDGs) recognize the need for reducing cancer burden as part of target 3.4, stating “By 2030, reduce by one third premature mortality from noncommunicable diseases [NCDs] through prevention and treatment and promote mental health and well-being.”5 Most countries will need to accelerate their efforts to reduce NCD burden, including cancer, to meet this SDG target.6,7 Increasing the pace of progress will be particularly critical given the ongoing COVID-19 pandemic, which has led to delays and disruptions in cancer screenings, diagnosis, and treatment around the world.8,9,10,11,12
The importance of prevention and control of NCDs, including cancer, was emphasized by the third UN High-Level Meeting on NCDs in 201813 and the UN High-Level Meeting on Universal Health Coverage in 2019.14,15 World Health Organization initiatives that are focused on breast cancer,16 cervical cancer,17 and childhood cancer18 are valuable efforts toward reducing global cancer burden in combination with national-level cancer control planning and implementation. Global and local efforts require comprehensive assessments of cancer burden, information that may be sparse or unavailable in some countries.19
The Global Burden of Diseases (GBD), Injuries, and Risk Factors Study 2019 (GBD 2019) framework enables the comparable assessment of cancer burden across locations and time in terms of cancer incidence, mortality, years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life years (DALYs).20 Estimates of YLLs, YLDs, and DALYs complement incidence and mortality estimates by incorporating morbidity and mortality contributions to total cancer burden over the lifetime. Because GBD 2019 estimated disease burden across a mutually exclusive and collectively exhaustive hierarchy of diseases and injuries, cancer burden can also be systematically compared with and ranked against other causes of disease burden. Together, these qualities help GBD 2019 provide a comprehensive picture of variation in cancer burden that can potentially inform cancer control planning.
In this article, we present results for 29 cancer groups from the GBD 2019 study, globally and for 204 countries and territories, from 2010 through 2019. Results are also provided by quintiles of the Sociodemographic Index (SDI), a summary indicator of social and economic development that allows for analyses of disease burden patterns across different resource contexts.20,21 These estimates update results from the GBD 2017 study22 and supersede published estimates from previous GBD iterations.22,23,24,25
Methods
This section provides an overview of GBD 2019 cancer estimation methods. Additional detail is provided in the GBD 2019 summary publications,20,21,26 as well as in the eAppendix, eFigures 1 to 15, and eTables 1 to 18 in the Supplement. This study is compliant with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) statement (eTable 13 in the Supplement).27 The University of Washington institutional review board committee approved GBD 2019, and informed consent was waived because of the use of deidentified data. This article was produced as part of the GBD Collaborator Network and in accordance with the GBD Protocol (http://www.healthdata.org/gbd/about/protocol).
Study Design
Disease and injuries in GBD 2019 were organized into a comprehensive hierarchy of nested levels, with neoplasms as 1 of 22 level 2 groups.20 Cancers were classified into 30 level 3 cancer groups (eg, leukemia), 4 of which were further subdivided into level 4 groups (eg, chronic myeloid leukemia). While the GBD study estimates benign and in situ neoplasms as an important component of total health burden from all neoplasms broadly, this level 3 cancer group was not included in the estimates reported in this article to focus on malignant cancers (eAppendix in the Supplement). Similarly, because nonmelanoma skin cancer (NMSC) has relatively high incidence and low mortality compared with other cancers, this article presents estimates with and without NMSC.
There are 5 major ways that this iteration of the GBD study improved on the data and methods used to estimate cancer burden in GBD 201722 (eAppendix in the Supplement). First, GBD 2019 incorporated an additional 104 076 new cancer-, location-, and year-specific sources of data compared with GBD 2017 (eTable 1 in the Supplement). Second, data processing methods were improved for several cancers, particularly liver cancer, as described later. Third, the youngest age group estimated was increased or decreased for several cancers to align with cancer registry age patterns. Fourth, modeling parameters were updated to perform additional smoothing of mortality-to-incidence ratio (MIR) estimates across age and time, reducing improbable variation from sparse data. Fifth, cancer survival estimation methods were updated to improve uncertainty estimations and estimate age-specific instead of all-ages survival curves.
Results are presented by SDI, a composite indicator of income per capita, mean years of education, and fertility rate for those younger than 25 years.21 The SDI is the geometric mean of these 3 independently estimated and scaled components, with lower values representing lower development. While SDI values may change over time, for consistency of comparison, countries were grouped into quintiles according to their SDI values in 2019 (eTable 2 and eFigure 1 in the Supplement). These quintiles were termed low, low-middle, middle, high-middle, and high. More details are provided in the eAppendix in the Supplement, including the population and SDI bounds for each quintile.
Data Sources and Processing
Cancer estimation in GBD 2019 used 929 193 cancer-, location-, and year-specific sources of data, of which 767 514 (82.6%) were from vital registration systems, 155 542 (16.7%) from cancer registries, and 6137 (0.7%) from verbal autopsy reports (eTable 1 in the Supplement). The cancers presented in this analysis include malignant neoplasms or cancer as defined by the International Statistical Classification of Diseases and Related Health Problems, Ninth Revision (ICD-9) codes 140 to 209,28 or Tenth Revision (ICD-10) codes C00 to C96.29 Incidence and mortality data with these ICD codes are mapped to GBD cancer causes20 (eAppendix and eTables 3-5 in the Supplement). One processing update for GBD 2019 was the remapping of deaths coded to ICD-10 code C22.9; because this code includes unspecified primary or secondary liver cancer, a subset of these deaths were redistributed to various other cancers that metastasize to the liver.20,30,31 Kaposi sarcoma was not estimated because deaths were primarily redistributed to be of HIV/AIDS (eAppendix in the Supplement).20 The GBD NMSC estimates included squamous cell carcinoma and basal cell carcinoma. Because NMSC reporting was incomplete in many cancer registries,32 GBD 2019 additionally incorporated data from the literature and clinical sources to estimate NMSC burden (eAppendix in the Supplement).
Modeling Process
The GBD cancer mortality and YLL estimation process included 2 primary steps (eFigure 2 in the Supplement), beginning with the estimation of cancer MIRs, which provide an association between mortality and incidence estimation, maximizing data availability. The MIRs were modeled using a space-time Gaussian process regression approach26 (MIR methods are described in the eAppendix in the Supplement) using matched incidence and mortality data from cancer registries (eTable 6 in the Supplement) and the GBD-estimated health care access and quality index33 as a covariate. These estimated MIRs were then used to convert cancer registry incidence data into inputs for mortality modeling.
Estimating cancer mortality was the second step. The GBD 2019 study used a Cause of Death Ensemble model (CODEm) approach that combined data from vital registration systems, cancer registries, and verbal autopsy reports to estimate mortality across several submodels.34 Covariates provided for potential inclusion in the submodels of the ensemble, such as smoking prevalence or alcohol use, can be found in the eAppendix and eTables 7 and 8 in the Supplement. Ensemble model construction and performance was evaluated through out-of-sample predictive validity tests (eTable 9 in the Supplement). For each cancer, sex-specific CODEm models generated mortality estimates across locations, years, and age groups. These cancer mortality estimates were then scaled to align with the total mortality for all causes of death, which was separately estimated in GBD 2019 (eTable 10 in the Supplement).21 To estimate YLLs, a standard age-specific GBD life expectancy was applied to mortality estimates by age group (eAppendix in the Supplement).20
The GBD cancer incidence and YLD estimation process included 2 additional steps (eFigure 3 in the Supplement), starting with estimating incidence. Incidence was estimated by taking mortality estimates from the second step described previously and dividing by MIR estimates from the first step described previously for each cancer type, sex, location, year, and 5-year age group. Additional information can be found in the eAppendix in the Supplement.
Next, YLDs were estimated by combining prevalence estimates with disability weights associated with various phases of cancer survival. To estimate 10-year cancer prevalence, survival curves estimated from MIRs were combined with GBD-estimated background mortality and applied to incidence estimates. Additional information regarding survival and prevalence estimation can be found in the eAppendix and eFigure 3 in the Supplement. These 10-year prevalence estimates were then partitioned into 4 sequelae according to the expected person-time spent in these 4 phases of cancer survival: (1) diagnosis/treatment, (2) remission, (3) metastatic/disseminated, and (4) terminal (eTable 11 in the Supplement). Each sequela prevalence was multiplied by a sequela-specific disability weight that represented the magnitude of health loss (eTable 12 in the Supplement).20 For 5 cancer types (bladder, breast, colorectal, larynx, and prostate cancer), the total prevalence additionally included lifetime prevalence of procedure-related disability (eg, laryngectomy due to larynx cancer). These procedure-related prevalence estimates were modeled in the Bayesian meta-regression tool DisMod-MR, version 2.1,20 using medical records data on the proportion of patients with cancer who underwent these procedures and the estimated number of 10-year survivors (eAppendix in the Supplement). These procedure-related prevalence estimates were then multiplied by procedure-specific disability weights (eTable 12 in the Supplement). Total cancer-specific YLDs were estimated by summing across these sequelae. Finally, DALYs were estimated as the sum of YLDs and YLLs.20
Reporting Standards
All rates are reported per 100 000 person-years. Annualized rates of change from 2010 to 2019 represent the mean percentage change per year during this period (eAppendix in the Supplement). The GBD world population standard was used to calculate age-standardized rates (eAppendix in the Supplement).21 For all estimates, 95% uncertainty intervals (UIs) are reported. Uncertainty was propagated through each step of the cancer estimation process, with UIs representing the 2.5th and 97.5th percentiles of the distribution of 1000 draws at each step (eAppendix in the Supplement).20
Results are reported for 29 cancer groups, 204 countries and territories, and 5 SDI quintiles from 2010 to 2019. These estimates, as well as extended years (1990-2019), additional cancer groups, national and subnational locations, sex-specific estimates, and additional age groups are available from online resources (https://vizhub.healthdata.org/gbd-compare/ and http://ghdx.healthdata.org/gbd-results-tool).
Data processing and analyses were conducted using Python, version 3.7.0 (Python Software Foundation); Stata, version 15.1 (StataCorp); and R, version 3.4.1 (R Foundation). Code is available at https://ghdx.healthdata.org/gbd-2019/code.
Results
Global Estimates of Total Cancers and Cancer-Specific Burden in 2019
Across 204 countries and territories, there were 23.6 million (95% UI, 22.2-24.9 million) incident cancer cases and 10.0 million (95% UI, 9.36-10.6 million) deaths in 2019 (Table 1). Excluding NMSC, there were an estimated 17.2 million (95% UI, 15.9-18.5 million) incident cancer cases and 9.97 million (95% CI, 9.31-10.5 million) deaths (Table 1).
Table 1. Global Incidence and Deaths in 2019 for Total Cancers and 29 Cancer Groups.
| Cancer typea | Deaths, thousands (95% UI) | ASMR per 100 000 (95% UI) | Incident cases, thousands (95% UI) | ASIR per 100 000 (95% UI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | |
| Total | 10 000 (9360-10 600) | 5690 (5250-6100) | 4340 (3970-4660) | 124.7 (116.4-132.0) | 156.1 (143.9-167.2) | 99.9 (91.5-107.3) | 23 600 (22 200-24 900) | 12 900 (12 100-13 800) | 10 600 (9920-11 400) | 290.5 (274.0-307.1) | 348.7 (327.3-370.8) | 246.1 (229.8-263.1) |
| Excluding NMSC | 9970 (9310-10 500) | 5650 (5220-6 070) | 4310 (3950-4 640) | 123.9 (115.7-131.2) | 155.1 (142.9-166.1) | 99.4 (91.0-106.8) | 17 200 (15 900-18 500) | 9260 (8470-10 000) | 7960 (7280-8610) | 211.4 (195.4-226.8) | 245.9 (225.3-266.5) | 185.0 (169.4-200.2) |
| Tracheal, bronchus, and lung | 2040 (1880-2190) | 1390 (1260-1510) | 657 (590-719) | 25.2 (23.2-27.0) | 37.4 (34.1-40.7) | 15.0 (13.5-16.4) | 2260 (2070-2450) | 1520 (1370-1680) | 737 (658-814) | 27.7 (25.3-30.0) | 40.4 (36.5-44.4) | 16.8 (15.0-18.6) |
| Colon and rectum | 1090 (1000-1150) | 594 (551-638) | 492 (438-532) | 13.7 (12.6-14.5) | 16.6 (15.4-17.9) | 11.2 (10.0-12.2) | 2170 (2000-2 340) | 1240 (1130-1360) | 926 (832-1 010) | 26.7 (24.6-28.9) | 33.1 (30.2-36.2) | 21.2 (19.0-23.2) |
| Stomach | 957 (871-1030) | 612 (544-678) | 346 (308-382) | 11.9 (10.8-12.8) | 16.6 (14.8-18.3) | 7.9 (7.1-8.8) | 1270 (1150-1400) | 847 (748-963) | 423 (377-467) | 15.6 (14.1-17.2) | 22.4 (19.8-25.3) | 9.7 (8.7-10.7) |
| Breast | 701 (647-752) | 12.1 (10.7-13.3) | 689 (635-740) | 8.6 (7.9-9.2) | 0.3 (0.3-0.4) | 15.9 (14.7-17.1) | 2000 (1830-2170) | 25.1 (22.2-27.8) | 1980 (1810-2150) | 24.2 (22.1-26.2) | 0.7(0.6-0.7) | 45.9 (41.9-49.8) |
| Pancreatic | 531 (492-567) | 278 (258-299) | 253 (226-274) | 6.6 (6.1-7.1) | 7.5 (7.0-8.1) | 5.8 (5.1-6.2) | 530 (486-574) | 280 (256-303) | 250 (224-275) | 6.6 (6.0-7.1) | 7.5 (6.8-8.1) | 5.7 (5.1-6.3) |
| Esophageal | 498 (438-551) | 366 (315-415) | 133 (110-150) | 6.1 (5.4-6.8) | 9.7 (8.3-11.0) | 3.0 (2.5-3.4) | 535 (467-595) | 389 (336-444) | 146 (120-165) | 6.5 (5.7-7.2) | 10.1 (8.7-11.6) | 3.3 (2.7-3.8) |
| Prostate | 487 (420-594) | 487 (420-594) | NA | 6.3 (5.4-7.7) | 15.3 (13.0-18.6) | NA | 1410 (1230-1830) | 1410 (1230-1830) | NA | 17.4 (15.1-22.5) | 38.6 (33.6-49.8) | NA |
| Liver | 485 (444-526) | 334 (300-368) | 151 (134-167) | 5.9 (5.4-6.4) | 8.7 (7.9-9.6) | 3.5 (3.1-3.8) | 534 (487-589) | 376 (335-422) | 158 (140-176) | 6.5 (5.9-7.2) | 9.7 (8.7-10.8) | 3.6 (3.2-4.0) |
| Other malignant neoplasms | 408 (355-444) | 220 (180-249) | 188 (169-204) | 5.1 (4.5-5.6) | 5.9 (4.8-6.7) | 4.5 (4.0-4.8) | 831 (741-906) | 451 (381-504) | 381 (347-415) | 10.4 (9.3-11.4) | 11.9 (10.0-13.3) | 9.2 (8.4-10.1) |
| Leukemia | 335 (307-360) | 188 (165-208) | 146 (132-158) | 4.3 (3.9-4.6) | 5.2 (4.6-5.7) | 3.5 (3.2-3.8) | 644 (587-700) | 351 (308-390) | 293 (263-322) | 8.2 (7.5-8.9) | 9.4 (8.3-10.5) | 7.2 (6.5-8.0) |
| Cervical | 280 (239-314) | NA | 280 (239-314) | 3.4 (2.9-3.8) | NA | 6.5 (5.5-7.3) | 566 (482-636) | NA | 566 (482-636) | 6.8 (5.8-7.7) | NA | 13.4 (11.4-15.0) |
| Non-Hodgkin lymphoma | 255 (238-270) | 146 (136-155) | 109 (98.9-117) | 3.2 (3.0-3.4) | 4.0 (3.7-4.2) | 2.5 (2.3-2.7) | 457 (417-499) | 266 (241-291) | 191 (169-211) | 5.7 (5.2-6.3) | 7.2 (6.5-7.9) | 4.5 (4.0-4.9) |
| Brain and central nervous system | 246 (186-271) | 139 (99.6-157) | 108 (76.4-122) | 3.0 (2.3-3.4) | 3.6 (2.6-4.1) | 2.6 (1.8-2.9) | 348 (262-389) | 187 (135-215) | 161 (114-184) | 4.3 (3.3-4.9) | 4.8 (3.5-5.6) | 3.9 (2.8-4.5) |
| Bladder | 229 (211-243) | 169 (157-181) | 59.5 (52.3-64.6) | 2.9 (2.7-3.1) | 5.1 (4.7-5.4) | 1.4 (1.2-1.5) | 524 (476-569) | 408 (371-444) | 116 (104-128) | 6.5 (5.9-7.1) | 11.3 (10.2-12.3) | 2.7 (2.4-2.9) |
| Lip and oral cavity | 199 (182-218) | 132 (118-145) | 67.8 (60.8-75.7) | 2.4 (2.2-2.7) | 3.4 (3.1-3.8) | 1.6 (1.4-1.7) | 373 (341-404) | 243 (219-268) | 130 (117-143) | 4.5 (4.1-4.9) | 6.2 (5.6-6.8) | 3.0 (2.7-3.3) |
| Ovarian | 198 (175-218) | NA | 198 (175-218) | 2.4 (2.1-2.7) | NA | 4.6 (4.0-5.0) | 294 (261-330) | NA | 294 (261-330) | 3.9 (3.2-4.0) | NA | 6.9 (6.1-7.7) |
| Gallbladder and biliary tract | 172 (145-189) | 73.0 (59.5-80.4) | 99.5 (81.7-114.0) | 2.2 (1.8-2.4) | 2.1 (1.7-2.3) | 2.3 (1.9-2.6) | 199 (167-220) | 86.4 (69.4-95.9) | 113 (91.6-130) | 2.5 (2.1-2.7) | 2.4 (1.9-2.7) | 2.6 (2.1-3.0) |
| Kidney | 166 (155-176) | 109 (101-116) | 57.7 (52.2-61.9) | 2.1 (1.9-2.2) | 3.0 (2.8-3.2) | 1.3 (1.2-1.4) | 372 (345-402) | 241 (221-262) | 131 (120-142) | 4.6 (4.2-4.9) | 6.2 (5.7-6.8) | 3.1 (2.8-3.3) |
| Larynx | 123 (115-133) | 106 (97.8-115) | 17.8 (16.2-19.7) | 1.5 (1.4-1.6) | 2.7 (2.5-3.0) | 0.4 (0.4-0.5) | 209 (194-225) | 181 (166-196) | 28.5 (26.1-31.3) | 2.5 (2.3-2.7) | 4.6 (4.2-5.0) | 0.7 (0.6-0.7) |
| Other pharynx | 114 (103-126) | 88.0 (78.0-98.7) | 26.2 (22.5-30.5) | 1.4 (1.2-1.5) | 2.2 (2.0-2.5) | 0.6 (0.5-0.7) | 167 (153-180) | 129 (116-142) | 37.6 (33.1-42.3) | 2.0 (1.8-2.2) | 3.2 (2.9-3.5) | 0.9 (0.8-1.0) |
| Multiple myeloma | 113 (99.5-122) | 60.4 (50.7-67.1) | 53.0 (45.1-58.3) | 1.4 (1.2-1.5) | 1.7 (1.4-1.8) | 1.2 (1.0-1.3) | 156 (137-173) | 84.5 (70.9-94.9) | 71.2 (60.3-80.1) | 1.9 (1.7-2.1) | 2.3 (1.9-2.6) | 1.6 (1.4-1.8) |
| Uterine | 91.6 (82.4-101.5) | NA | 91.6 (82.4-101.5) | 1.1 (1.0-1.3) | NA | 2.1 (1.9-2.3) | 435 (397-480) | NA | 435 (397-480) | 5.2 (4.8-5.7) | NA | 10.0 (9.1-11.0) |
| Nasopharynx | 71.6 (65.4-77.6) | 51.2 (46.0-57.0) | 20.4 (18.2-22.8) | 0.9 (0.8-0.9) | 1.3 (1.2-1.4) | 0.5 (0.4-0.5) | 177 (156-200) | 127 (108-149) | 49.2 (42.6-57.0) | 2.1 (1.9-2.4) | 3.1 (2.7-3.7) | 1.2 (1.0-1.3) |
| Malignant skin melanoma | 62.8 (46.3-71.0) | 35.4 (22.0-42.7) | 27.4 (19.0-31.9) | 0.8 (0.6-0.9) | 1.0 (0.6-1.2) | 0.6 (0.4-0.7) | 290 (214-342) | 153 (89.8-193) | 137 (92.7-167) | 3.6 (2.6-4.2) | 4.0 (2.3-5.1) | 3.2 (2.2-3.9) |
| Nonmelanoma skin | 56.1 (50.4-59.8) | 33.2 (30.3-35.6) | 22.8 (19.3-25.2) | 0.7 (0.7-0.8) | 1.0 (0.9-1.1) | 0.5 (0.4-0.6) | 6350 (5810-6950) | 3680 (3350-4060) | 2670 (2430-2910) | 79.1 (72.3-86.6) | 102.8 (93.9-112.9) | 61.1 (55.8-66.7) |
| Thyroid | 45.6 (41.3-48.8) | 18.6 (16.8-20.2) | 26.9 (23.7-29.3) | 0.6 (0.5-0.6) | 0.5 (0.5-0.6) | 0.6 (0.5-0.7) | 234 (212-253) | 76.0 (68.2-82.9) | 158 (140-173) | 2.8 (2.6-3.1) | 1.9 (1.7-2.1) | 3.7 (3.3-4.1) |
| Mesothelioma | 29.3 (26.7-31.0) | 21.2 (20.0-22.5) | 8.03 (5.88-8.92) | 0.4 (0.3-0.4) | 0.6 (0.6-0.6) | 0.2 (0.1-0.2) | 34.5 (31.2-37.8) | 25.2 (22.9-27.6) | 9.34 (6.84-10.7) | 0.4 (0.4-0.5) | 0.7 (0.6-0.8) | 0.2 (0.2-0.2) |
| Hodgkin lymphoma | 27.6 (23.7-31.8) | 17.2 (13.9-21.0) | 10.4 (8.23-12.6) | 0.3 (0.3-0.4) | 0.4 (0.4-0.5) | 0.3 (0.2-0.3) | 87.5 (77.9-101.4) | 51.3 (43.6-58.7) | 36.2 (30.2-46.1) | 1.1 (1.0-1.3) | 1.3 (1.1-1.5) | 0.9 (0.7-1.1) |
| Testicular | 10.8 (9.96-11.9) | 10.8 (9.96-11.9) | NA | 0.1 (0.1-0.2) | 0.3 (0.3-0.3) | NA | 109.3 (93.4-129.5) | 109.3 (93.4-129.5) | NA | 1.4 (1.2-1.7) | 2.8 (2.4-3.3) | NA |
Abbreviations: ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; NA, not applicable; NMSC, nonmelanoma skin cancer; UI, uncertainty interval.
Rows are ordered by decreasing number of total deaths. Cancer groups are defined based on International Classification of Diseases, Ninth Revision (ICD-9) and International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes and include all codes pertaining to malignant neoplasms (ICD-9 codes 140-208 and ICD-10 codes C00-C96) except for Kaposi sarcoma (C46; eAppendix in the Supplement). eTables 3 and 4 in the Supplement detail how the original ICD codes were mapped to the Global Burden of Disease cancer cause list. Visual comparisons of cancer-specific incidence and mortality are provided in eFigures 14 and 15 in the Supplement. Detailed results for incidence and mortality by Sociodemographic Index quintile, region, and country can be accessed in eTables 16 and 17 in the Supplement and at https://vizhub.healthdata.org/gbd-compare/.
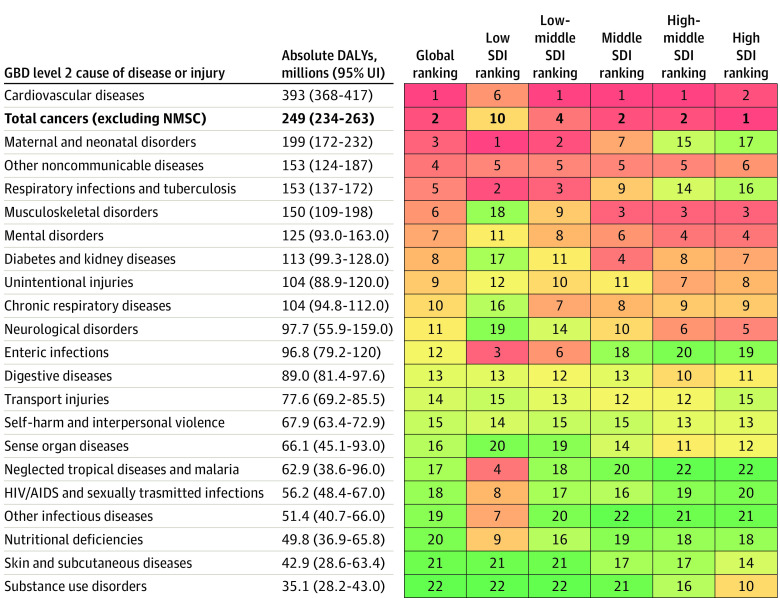
Globally, cancers were estimated to cause 250 million (95% UI, 235-264 million) DALYs in 2019 (eTable 15 in the Supplement). Of the total global DALYs, 96.9% (95% UI, 96.0%-97.7%) came from YLLs, whereas 3.1% (95% UI, 2.3%-4.0%) came from YLDs (eTable 14 and eFigure 4 in the Supplement). Among the 22 groups of diseases and injuries in level 2 of the GBD cause hierarchy (Figure 122), total cancer was the second-highest cause of DALYs, deaths, and YLLs behind cardiovascular diseases (Table 2; eTable 15 in the Supplement). As such, cancer had greater overall and fatal burden globally in 2019 than other major groups of diseases in the GBD, such as maternal and neonatal disorders, musculoskeletal disorders, and respiratory infections and tuberculosis (Figure 1).
Figure 1. Ranking of Total Cancer Absolute Disability-Adjusted Life Years (DALYs) in 2019 Among the 22 Level 2 Categories of Disease in the Global Burden of Disease (GBD) Study by Quintile of Sociodemographic Index (SDI).
Total cancers excludes nonmelanoma skin cancer. The GBD study organized diseases and injuries into a hierarchy that was mutually exclusive and collectively exhaustive. More details of this hierarchy were previously published.22 Colors represent the ranking of the cause within a given location group (eg, high SDI quintile) from red (highest ranking) to green (lowest ranking). The other noncommunicable diseases include congenital birth defects; urinary diseases and male infertility; gynecological diseases; hemoglobinopathies and hemolytic anemias; endocrine, metabolic, blood, and immune disorders; oral disorders; and sudden infant death syndrome. The other infectious diseases include meningitis; encephalitis; diphtheria; whooping cough; tetanus; measles; varicella and herpes zoster; acute hepatitis; and other unspecified infectious diseases. NMSC indicates nonmelanoma skin cancer; UI, uncertainty interval.
Table 2. Global Cancer Estimates in 2019 and Ranking Among 22 Level 2 Categories of Diseases and Injuries in the Global Burden of Disease Study Overall and by Quintile of Sociodemographic Index.
| Locationa | DALYs | Deaths | YLLs | Incident cases | YLDs | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. millions (95% UI) | Cancer rank | No. millions (95% UI) | Cancer rank | No. millions (95% UI) | Cancer rank | No. millions (95% UI) | Cancer rank | No. millions (95% UI) | Cancer rank | |
| Global | 249.0 (233.6-263.2) | 2 | 9.97 (9.31-10.5) | 2 | 241.3 (226.5-255.3) | 2 | 17.2 (15.9-18.5) | 21 | 7.72 (5.68-9.96) | 20 |
| SDI | ||||||||||
| Low | 18.0 (15.9-20.2) | 10 | 0.54 (0.48-0.60) | 5 | 17.7 (15.7-19.8) | 9 | 0.68 (0.60-0.76) | 21 | 0.26 (0.18-0.34) | 22 |
| Low-middle | 40.2 (36.8-43.7) | 4 | 1.37 (1.26-1.49) | 2 | 39.5 (36.1-43.0) | 4 | 1.81 (1.67-1.96) | 21 | 0.70 (0.52-0.92) | 22 |
| Middle | 76.3 (69.7-83.2) | 2 | 2.88 (2.62-3.15) | 2 | 74.5 (68.0-81.4) | 2 | 4.47 (4.05-4.89) | 21 | 1.85 (1.36-2.44) | 20 |
| High-middle | 63.5 (58.6-68.2) | 2 | 2.65 (2.42-2.85) | 2 | 61.4 (56.6-66.0) | 2 | 4.69 (4.29-5.09) | 21 | 2.11 (1.54-2.75) | 16 |
| High | 50.9 (48.1-52.9) | 1 | 2.53 (2.31-2.64) | 2 | 48.1 (45.5-49.7) | 1 | 5.56 (5.02-6.09) | 19 | 2.79 (2.03-3.61) | 12 |
Abbreviations: DALYs, disability-adjusted life years; SDI, Sociodemographic Index; UI, uncertainty interval; YLDs, years lived with disability; YLLs, years of life lost.
Total numbers and rankings exclude nonmelanoma skin cancer. All estimates refer to estimates in 2019. Rank refers to the relative ranking of the total cancer estimate for a given measure (eg, DALYs) and SDI quintile (eg, high SDI) compared among the 22 level 2 categories of diseases and injuries in the Global Burden of Disease Study 2019. More details on SDI quintiles, including population, are in the eAppendix in the Supplement. A version of this table using age-standardized rates is provided in eTable 18 in the Supplement.
The 5 leading causes of cancer-related DALYs for both sexes combined (Figure 2), excluding other malignant neoplasms, were tracheal, bronchus, and lung (TBL) cancer, with 18.3% (95% UI, 17.5%-19.1%) of total cancer-related DALYs; colon and rectum cancer (CRC), with 9.7% (95% UI, 9.4%-10.0%); stomach cancer, with 8.9% (8.6%-9.3%); breast cancer, with 8.2% (7.8%-8.7%); and liver cancer, with 5.0% (4.8%-5.3%).
Figure 2. Cancer Group Rankings by Disability-Adjusted Life Years (DALYs) in 2019 and Percentage Change From 2010 to 2019.
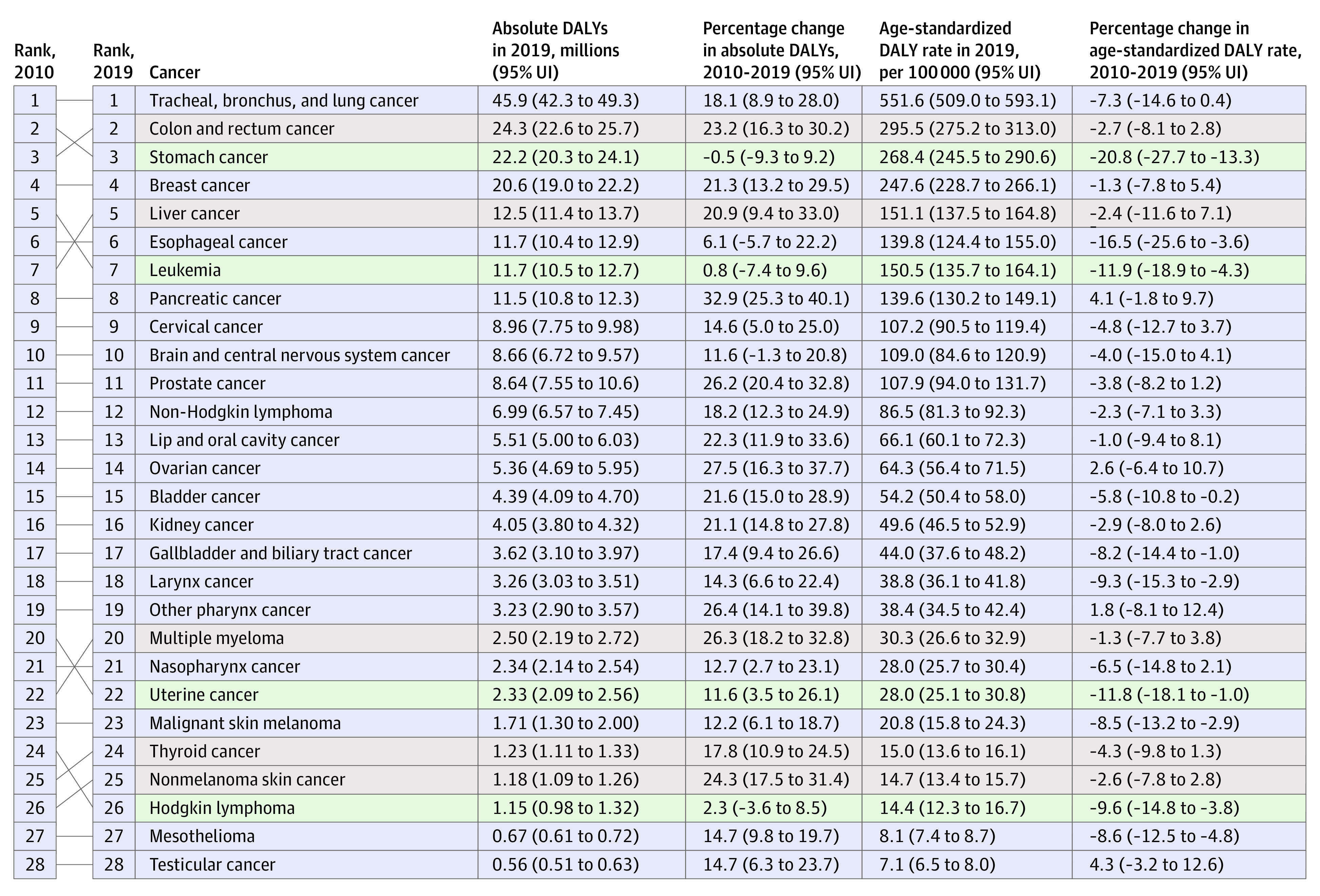
Rankings are by absolute DALYs and exclude the other malignant neoplasms cancer group. Cancers are ordered by rank in 2019, with lines connecting to their rank in 2010. Absolute DALYs and age-standardized DALY rates for 2010 can be found online at https://vizhub.healthdata.org/gbd-compare/. Colors refer to the directional change in cancer rank from 2010 to 2019: red signifies an increase in rank, blue signifies no change in rank, and green signifies a decrease in rank. UI indicates uncertainty interval.
Tracheal, bronchus, and lung cancer were estimated to cause 45.9 million (95% UI, 42.3-49.3 million) DALYs in 2019; of these, 98.8% (95% UI, 98.5%-99.1%) came from YLLs and just 1.2% (95% UI, 0.9%-1.5%) from YLDs (eTable 14 and eFigure 4 in the Supplement). In 2019, there were 2.04 million (95% UI, 1.88-2.19 million) deaths due to TBL cancer and 2.26 million (95% UI, 2.07-2.45 million) incident TBL cases (Table 1). Tracheal, bronchus, and lung cancer was the leading cause of cancer incidence and mortality in 58 and 119 countries and territories, respectively, for males (eFigures 5 and 6 in the Supplement), and 1 and 27 countries, respectively, for females (eFigures 7 and 8 in the Supplement).
Colon and rectum cancer were estimated to cause 24.3 million (95% UI, 22.6-25.7 million) DALYs in 2019; of these, 95.6% (95% UI, 94.4%-96.8%) came from YLLs and 4.4% (95% UI, 3.2%-5.6%) from YLDs (eTable 14 and eFigure 4 in the Supplement). In 2019, there were 1.09 million (95% UI, 1.00-1.15 million) deaths due to CRC and 2.17 million (95% UI, 2.00-2.34 million) incident CRC cases (Table 1). Colon and rectum cancer was the leading cause of cancer incidence and mortality in 1 country and 9 countries, respectively, for females (eFigures 7 and 8 in the Supplement) and of cancer incidence for 11 countries in males (eFigure 5 in the Supplement).
Stomach cancer was estimated to cause an estimated 22.2 million (95% UI, 20.3-24.1 million) DALYs in 2019; of these, 98.4% (95% UI, 98.0%-98.9%) came from YLLs and 1.6% (95% UI, 1.1%-2.0%) from YLDs (eTable 14 and eFigure 4 in the Supplement). There were also 957 000 (95% UI, 871 000-1 030 000) deaths and 1.27 million (95% UI, 1.15-1.40 million) incident cases of stomach cancer in 2019 (Table 1). Stomach cancer was the leading cause of cancer incidence and mortality in 5 and 11 countries, respectively, for males (eFigures 5 and 6 in the Supplement) and of cancer mortality in 6 countries for females (eFigure 8 in the Supplement).
Breast cancer was the leading cause of cancer-related DALYs, deaths, and YLLs among females globally in 2019. Most of the global breast cancer burden occurred for females, with 20.3 million (95% UI, 18.7-21.9 million) of 20.6 million (95% UI, 19.0-22.2 million) total breast cancer–related DALYs in 2019 occurring in females, of which 93.3% (95% UI, 91.1%-95.2%) came from YLLs and 6.7% (95% UI, 4.8%-8.9%) from YLDs (eTable 14 and eFigure 4 in the Supplement). Likewise, 689 000 (95% UI, 635 000-740 000) of 701 000 (95% UI, 647 000-752 000) breast cancer deaths occurred in females, and 1.98 million (95% UI, 1.81–2.15 million) of 2.00 million (95% UI, 1.83–2.17 million) incident cases of breast cancer (Table 1). For females, breast cancer was the leading cause of cancer incidence in 157 countries and deaths in 119 countries (eFigures 7 and 8 in the Supplement).
Liver cancer was estimated to cause 12.5 million (95% UI, 11.4-13.7 million) DALYs in 2019; of these, 99.0% (95% UI, 98.6%-99.3%) came from YLLs and 1.0% (95% UI, 0.7%-1.4%) from YLDs (eTable 14 and eFigure 4 in the Supplement). There were also 485 000 (95% UI, 444 000-526 000) deaths and 534 000 (95% UI, 487 000-589 000) incident cases of liver cancer in 2019 (Table 1). Liver cancer was the leading cause of cancer incidence and mortality in 6 and 8 countries, respectively, in males (eFigures 5 and 6 in the Supplement) and 1 and 2 countries, respectively, in females (eFigures 7 and 8 in the Supplement).
Sex-specific DALY rankings differed slightly from those previously described because of the higher prominence of several sex-specific cancers. Among males, TBL cancer remained the leading cause of cancer-related DALYs globally, followed by stomach, CRC, liver, and esophageal cancer, with prostate cancer sixth (eFigure 9 in the Supplement). Among females, the leading cause of cancer-related DALYs globally was breast cancer, followed by TBL, CRC, cervical, and stomach cancer, with ovarian cancer sixth (eFigure 10 in the Supplement).
Global Trends in Cancer Burden From 2010 to 2019
Globally, the number of new cancer cases increased from 18.7 million (95% UI, 18.0-19.3 million) in 2010 to 23.6 million (95% UI, 22.2-24.9 million) in 2019, an increase of 26.3% (95% UI, 20.3%-32.3%). Age-standardized incidence rates remained generally the same during this period, with a difference of −1.1% (95% UI, −5.8% to 3.5%) and an annualized rate of change of −0.1% (95% UI, −0.7% to 0.4%). Excluding NMSC, the number of incident cases increased from 13.8 million (95% UI, 13.3-14.3 million) in 2010 to 17.2 million (95% UI, 15.9-18.5 million) in 2019, a 24.6% (95% UI, 16.8%-32.6%) increase, while the age-standardized incidence rates remained the same during this period, with a difference of −1.6% (95% UI, −7.7% to 4.6%) and an annualized rate of change of −0.2% (95% UI, −0.9% to 0.5%).
Similarly, the number of global total cancer deaths increased by 20.9% (95% UI, 14.2%-27.6%) from 8.29 million (95% UI, 7.89-8.57 million) in 2010 to 10.0 million (95% UI, 9.36-10.6 million) in 2019. Cancer deaths also increased as a proportion of total deaths of all causes, rising from 15.7% (95% UI, 15.0%-16.2%) in 2010 to 17.7% (95% UI, 16.8%-18.4%) in 2019. By contrast, age-standardized mortality rates declined by −5.9% (95% UI, −11.0% to −0.9%) during this 10-year period, with an annualized rate of change of −0.7% (95% UI, −1.3% to −0.1%). During this decade, the absolute number of global cancer-related DALYs increased by 16.0% (95% UI, 9.3%-22.8%) from 216 million (95% UI, 208-223 million) in 2010 to 250 million (95% UI, 235-264 million) in 2019. The proportion of estimated total global DALYs that were due to cancer increased from 8.4% (95% UI, 7.7%-9.0%) of total DALYs from all causes in 2010 to 9.9% (95% UI, 8.9%-10.9%) in 2019. A decline is also evident in the age-standardized rates, as age-standardized cancer-related DALYs rates decreased by −6.6% (95% UI, −11.9% to −1.1%) during this period.
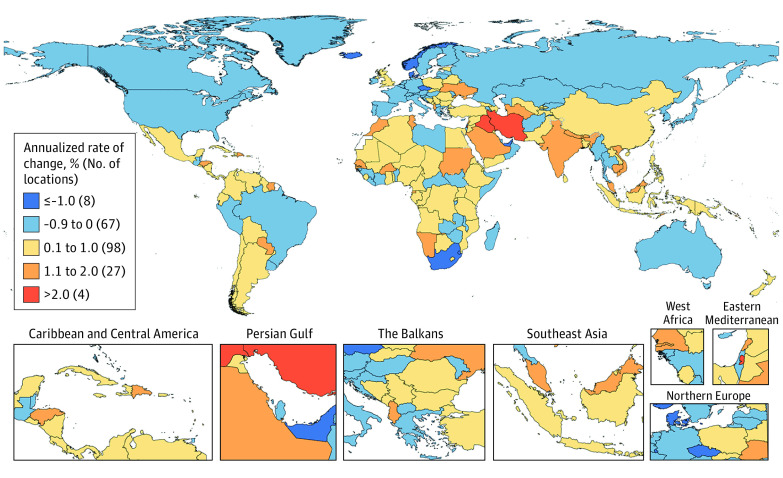
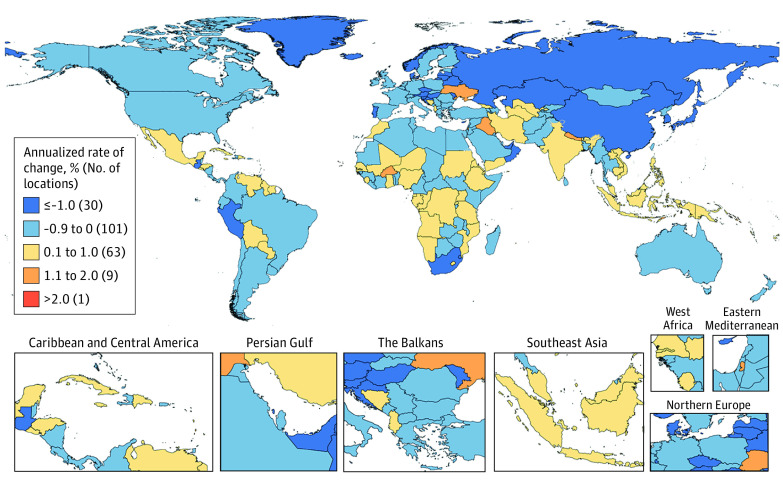
Location-specific annualized rates of change in age-standardized mortality and incidence rates from 2010 to 2019 for total cancers, excluding NMSC, varied by location. During this period, age-standardized mortality rates decreased in 131 of 204 countries and territories (64.2%; Figure 3), and age-standardized incidence rates decreased in 75 of 204 countries and territories (36.8%; Figure 4).
Figure 3. Annualized Rate of Change in Age-Standardized Total Cancer Incidence Rate From 2010 to 2019 in Both Sexes.
Total cancer excludes nonmelanoma skin cancers. Annualized rate of change from 2010 to 2019 represents the average percentage change per year during this period, with negative values indicating decreasing incidence rates and positive values indicating increasing incidence rates. There were several geographic locations where estimates were not available (eg, Western Sahara and French Guiana), as they were not modeled locations in the Global Burden of Disease 2019 Study.
Figure 4. Annualized Rate of Change in Age-Standardized Total Cancer Mortality Rate From 2010 to 2019 in Both Sexes.
Total cancer excludes nonmelanoma skin cancers. Annualized rate of change from 2010 to 2019 represents the mean percentage change per year during this period, with negative values indicating decreasing mortality rates and positive values indicating increasing mortality rates. There were several geographic locations where estimates were not available (eg, Western Sahara and French Guiana) as they were not modeled locations in the Global Burden of Disease 2019 Study.
Trends during the last decade varied by type of cancer, including several shifts in cancer group rankings by absolute DALYs (Figure 2). For example, CRC and liver cancer rose from the third and seventh leading causes of cancer-related DALYs in 2010 to second and fifth in 2019 because of large increases in the number of DALYs and small decreases in age-standardized DALY rates. In contrast, stomach cancer and leukemia dropped from second and fifth to third and seventh during the same period because of large decreases in age-standardized DALY rates and minimal changes in the number of DALYs (Figure 2).
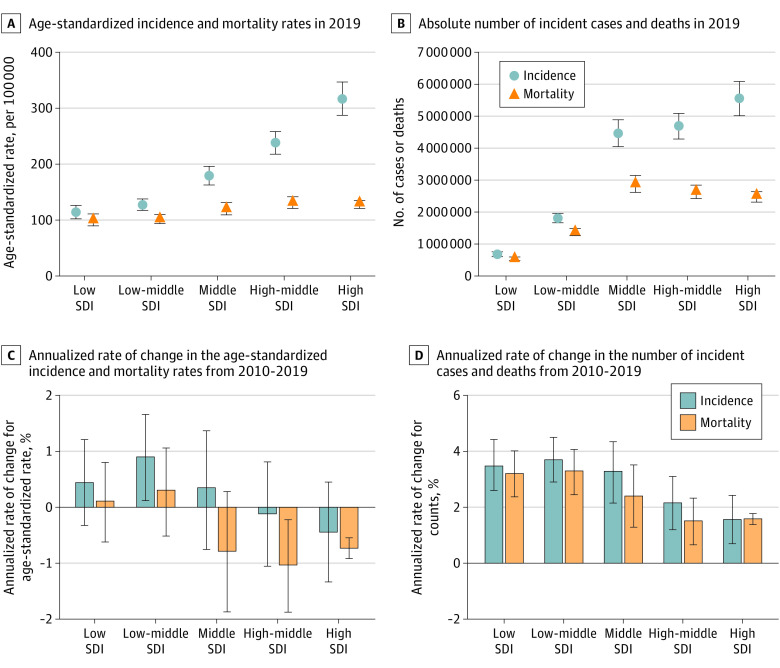
Cancer Burden by SDI
Cancer burden varied considerably across SDI quintiles in 2019 levels and rankings (Table 2 and Figure 4) and trends during the 2010 to 2019 study period (Figure 5; eTables 16 and 17 in the Supplement). The following results exclude NMSC.
Figure 5. Total Cancer Incidence and Mortality Age-Standardized Rates and Absolute Counts in 2019 and Annualized Rate of Change for Incidence and Mortality in Age-Standardized Rates and Absolute Counts From 2010 to 2019 by Sociodemographic Index (SDI) Quintile.
Panels provide global estimates for total cancers, except nonmelanoma skin cancer, stratified by SDI quintile. Annualized rate of change from 2010 to 2019 represents the mean percentage change per year during this period. Black bars represent 95% uncertainty intervals.
In the high SDI quintile in 2019, there were 50.9 million (95% UI, 48.1-52.9 million) DALYs estimated to be caused by cancer, of which 94.5% (95% UI, 93.1%-95.9%) were from YLLs and 5.5% (95% UI, 4.1%-6.9%) from YLDs. The most cases and the highest age-standardized incidence rates were in the high SDI quintile (Table 2; Figure 5). Compared with GBD level 2 groups of diseases and injuries, cancer was the leading cause of YLLs and DALYs in the high SDI quintile and was the leading or second leading cause of deaths by age-standardized rate or absolute number, respectively. In the high-middle SDI quintile, there were 63.5 million (95% UI, 58.6-68.2 million) DALYs estimated to be caused by cancer, of which 96.7% (95% UI, 95.7%-97.6%) were from YLLs and 3.3% (95% UI, 2.4%-4.3%) from YLDs. The high-middle SDI had the highest age-standardized rates of deaths and DALYs of all SDI quintiles and the second highest age-standardized incidence rate (Table 2; Figure 5).
The middle SDI quintile had the highest number of cancer-related DALYs and deaths of any SDI quintile in 2019, with 76.3 million (95% UI, 69.7-83.2 million) DALYs and 2.88 million (95% UI, 2.62-3.15 million) deaths (Table 2, Figure 5). Of the SDI quintiles, the middle SDI quintile had the largest total population (eAppendix in the Supplement). For DALYs, 97.6% (95% UI, 96.8%-98.3%) came from YLLs and 2.4% (95% UI, 1.7%-3.2%) from YLDs. In the low-middle SDI quintile, there were 40.2 million (95% UI, 36.8-43.7 million) DALYs estimated to be caused by cancer in 2019; of these, 98.2% (95% UI, 97.7%-98.7%) were from YLLs and 1.8% (95% UI, 1.3%-2.3%) from YLDs.
In the low SDI quintile, there were 18.0 million (95% UI, 15.9-20.2 million) DALYs estimated to be caused by cancer in 2019; of these, 98.6% (95% UI, 98.1%-98.9%) were from YLLs and 1.4% (95% UI, 1.1%-1.9%) from YLDs. The low SDI quintile had the lowest numbers and age-standardized rates of cancer cases and deaths (Table 2; Figure 5). In contrast to the higher rankings in other quintiles, cancer was the fifth leading cause of death in the low SDI quintile in 2019, ninth for YLLs, and tenth for DALYs.
Alongside these differences, some patterns held across most SDI quintiles. In 2019, TBL cancer had the highest number of cancer deaths and DALYs in both sexes combined in all but the low SDI quintile, in which it was breast cancer (eFigure 11 in the Supplement). Excluding NMSC, the most incident cases occurred for CRC in the high SDI quintile, TBL in the high-middle and middle SDI quintiles, and breast cancer in the low-middle and low SDI quintiles (eFigure 12 in the Supplement).
While in 2019 the largest absolute numbers of cases and deaths occurred in the middle to high SDI quintiles, from 2010 to 2019, the largest increasing annualized rates of change in the absolute numbers of cases and deaths occurred in the low-middle SDI quintile and then the low SDI quintile (Figure 5; eTables 16 and 17 in the Supplement). Changes in age-standardized rates from 2010 to 2019 also varied by SDI quintile. For mortality, age-standardized rates increased from 2010 to 2019 in the low and low-middle SDI quintiles but decreased in the middle to high SDI quintiles. For incidence, age-standardized rates increased during this period for the low to middle SDI quintiles but decreased in the high-middle and high SDI quintiles, with the largest decrease in the high SDI quintile. While there was substantial heterogeneity between countries and territories within the same SDI quintile, country-specific estimates showed similar overall trends between SDI and age-standardized incidence and mortality rates (eFigure 13 in the Supplement).
Discussion
The results of this systematic analysis demonstrate the substantial and growing global burden of cancer, with patterns of burden differing by SDI quintile. In 2019, cancer-related DALYs were second only to cardiovascular diseases in their contribution to global disease burden, and in the high SDI quintile, cancer overtook cardiovascular disease to become the leading cause of DALYs. Between 2010 and 2019, the number of new global cancer cases and deaths increased by 26.3% and 20.9%, respectively. However, the largest percentage increases in cancer incidence and mortality during the last decade occurred in the lower SDI quintiles, likely reflecting ongoing epidemiologic transitions, demographic shifts, and disparities in cancer prevention, care, and control. Together, these results provide comprehensive and comparable estimates that can potentially inform efforts for equitably reducing the evolving burden of cancer globally.
While the absolute burden of cancer grew from 2010 to 2019, global age-standardized incidence rates remained similar at −1.1% (95% UI, −5.8% to 3.5%) and mortality rates decreased by −5.9% (95% UI, −11.0% to −0.9%). These age-standardized mortality results suggest cautious optimism that some progress may have been made in early diagnosis and cancer treatment globally during the last decade. However, inequities in the distribution and growth of cancer burden around the world diminish this potential advancement and suggest that an acceleration of efforts to effectively address cancer burden are needed. Of particular concern, recent progress in reducing age-standardized incidence and mortality rates seems concentrated in higher SDI locations, while both rates are still trending upward in lower SDI locations. The increasing age-standardized incidence and mortality rates in lower SDI quintiles may reflect several factors, including shifting population age structures, increasing capacity for diagnosis and registration of cancer cases and deaths, and changes in cancer risk factors, such as metabolic, behavioral, environmental, and occupational exposures. For example, changing patterns of smoking prevalence by SDI quintile may be particularly relevant to cancer burden,35 with a need for further smoking reduction and tobacco control initiatives in many countries.36,37 These differences in cancer burden across the SDI spectrum suggest a need to tailor cancer control efforts to specific resource contexts and health system needs, incorporating local cultural and cancer context-specific knowledge.
Low and low-middle SDI locations had a higher rate of growth in the number of cases and deaths than high SDI locations during the last decade. Consistent with this trend, forecasts of cancer incidence38 and mortality1 suggest a growing burden in these locations, predicting that by 2040 more than two-thirds of the world’s cancers will occur in low-income and middle-income countries.38 Increasing cancer burden in already overburdened and underresourced settings is concerning given existing disparities in health care access and coverage.2,3,39 As many in countries within the lower SDI quintiles have insufficient access to cancer prevention services, timely diagnosis, and comprehensive treatment, efforts to strengthen cancer control infrastructure, expand workforce capacity, and increase access to universal health coverage and sufficient financial security will be crucial.3,40 The grouping of countries by SDI quintile is not meant to imply that all countries within an SDI quintile have equivalent capacity to prevent, diagnose, or treat cancers; each country has unique strengths and needs that should be considered. Further, the growing absolute number of cases and deaths in all SDI quintiles suggests that even as progress has been made in reducing age-standardized rates in some settings, globally there is an expanding need for health care infrastructure that is capable of supporting the provision of effective diagnoses and treatments for a growing number of patients with cancer.
While the traditional cancer metrics of incidence and mortality are crucial, DALY estimates provide perspective on the healthy years of life lost because of cancer morbidity and mortality globally. The GBD 2019 study found that on a global level, most cancer-related DALYs (96.9%; 95% UI, 96.0%-97.7%) in 2019 came from YLLs, suggesting that the total health loss from cancer was primarily associated with premature death. This finding is a valuable reminder of the lives that prematurely ended because of cancer globally and the importance of working toward improved global survival outcomes. While YLDs contribute less to global DALYs, the percentage of DALYs estimated to be caused by YLDs increased with increasing SDI quintiles, ranging from 1.4% (95% UI, 1.1%-1.8%) in the low SDI quintile to 5.7% (95% UI, 4.2%-7.1%) in the high SDI quintile. This greater comparative contribution of YLDs in higher SDI settings is consistent with likely improved survival,41 given generally more available access to cancer screening,42,43 diagnosis,44,45 and treatment46,47 as SDI increases. Consequently, the contribution of YLDs to health loss due to cancer would be expected to be increasingly relevant to global health planning as cancer survival improves globally, and the support needs of survivors of cancer should be considered as part of comprehensive cancer control planning efforts.48,49
The contribution of cancers to total global DALYs estimated to be caused by disease and injury has increased during the past decade, rising from third place in 2010 to second place in 2019, remaining behind only cardiovascular diseases. However, in high SDI settings, cancer-related DALYs have surpassed cardiovascular disease–related DALYs to become the leading cause of total disease burden in 2019. Other studies have described cancer’s emerging prominence as the leading cause of premature death in countries with high income50 or a high Human Development Index,4 some of which is attributed to relative decreases in cardiovascular disease deaths.4,50,51 The GBD 2019 study builds on this evolving global landscape of cancer burden by demonstrating the comparative importance of cancer in high SDI settings not just for mortality, but also when comparing the nonfatal burden of cancer and other diseases.
Together, these results suggest the need for increased cancer prevention and control efforts to reduce current burden,52 as well as the need to accelerate progress in lower SDI locations to reduce the effect of growing burden.1,2 One important step is bolstering national cancer control plans (NCCPs)53,54,55,56 that identify, plan, and evaluate a framework of cost-effective and feasible interventions, such as the World Health Organization’s best buys proposals for cancer prevention, diagnosis, and management.38 The increasing global uptake of NCCPs has demonstrated the utility of this approach in addressing cancer burden in several settings.57,58,59 However, creating and implementing effective NCCPs requires detailed knowledge about the local burden of cancer and associated risk factors, in addition to awareness of sociocultural circumstances and previous cancer control implementation efforts. Lack of information about local cancer epidemiology can be a substantial barrier in some data-sparse, and often resource-limited, locations.60,61 Cancer burden estimates, such as those in the GBD 2019 study, can potentially be helpful as part of context-specific cancer resource planning and prioritization efforts.
Limitations
Several limitations provide opportunities for improvement in future GBD iterations. An ongoing challenge is a lack of high-quality data in many locations. This includes time lags in data availability, nonspecific cause of death data from vital registration systems, and ascertainment limitations of verbal autopsy reports. The GBD addresses these data limitations through data-seeking efforts, data processing corrections, and modeling approaches that incorporate geospatial and temporal smoothing. These approaches allow the estimation of comprehensive results with appropriate uncertainty bounds. However, in years or locations where data were not available, estimates relied on covariates and modeling parameters, which may overestimate or underestimate true cancer burden. As data can be less available or reliable in locations within the lower SDI quintiles,19 estimates should be interpreted with some caution. These data limitations reinforce the need for enhancing cancer surveillance globally.61,62
Similarly, scarcity of age-specific and year-specific survival data requires using MIRs to estimate survival, which may not approximate location-specific survival trends well. Years lived with disability are currently estimated based on 10-year prevalence, which may underestimate the lifelong health loss and disability that some survivors of cancer experience, particularly for survivors of pediatric cancer.63 While the lifelong disability from treatment-related surgical procedures is currently estimated for 5 cancers, other sources of long-term disability in survivors of cancer have not yet been captured in these analyses. Finally, this study only estimated global cancer burden through 2019, and as such did not incorporate any associations of the COVID-19 pandemic with global cancer morbidity and mortality. Assessing these associations will be critical for future work on cancer burden, as the ongoing pandemic is likely to delay progress in efforts to reduce health loss from cancer globally through delays and reductions in screening, diagnosis, and treatment.8,9,10,11,12
Conclusions
This systematic analysis of the GBD 2019 study provides comprehensive and comparable estimates of cancer burden worldwide, which were updated and improved from previous GBD cycles. These estimates varied substantially by SDI quintile, highlighting global inequities in cancer burden. While the high SDI quintile had the highest estimated number of incident cases in 2019, the middle SDI quintile had the highest estimated number of deaths and DALYs. During the last decade, cancer burden has grown the fastest in the low and low-middle SDI quintiles. Such estimates are vital for improving equity in global cancer outcomes and meeting key SDG targets for reducing cancer and other noncommunicable disease burden.
eAppendix.
eTable 1. Number of site-years for cancer mortality data by source type, for GBD 2019 compared to GBD 2017
eTable 2. Socio-demographic Index groupings by geography, based on 2019 values
eTable 3. List of International Classification of Diseases (ICD) codes mapped to the Global Burden of Disease cause list for cancer incidence data
eTable 4. List of International Classification of Diseases (ICD) codes mapped to the Global Burden of Disease cause list for cancer mortality data
eTable 5. Undefined cancer code categories (ICD-10) and respective target codes for cancer registry incidence data
eTable 6. Cancer registry sources for cancer incidence and mortality-to-incidence ratio data by country, year, and registry
eTable 7. Covariates selected for CODEm for each GBD cancer group and expected direction of covariate
eTable 8. Comparison of GBD 2017 and GBD 2019 covariates used and level of covariates
eTable 9. Results for CODEm model performance testing
eTable 10. Percent change before and after CoDCorrect by cancer for all ages, both sexes combined, 2019
eTable 11. Duration of four prevalence phases by cancer
eTable 12. Disability weights
eTable 13. GATHER5 guidelines checklist
eTable 14. Contribution of YLDs and YLLs to DALYs by cancer, global, both sexes, 2019
eTable 15. Global number of incidence, prevalence, YLDs, deaths, YLLs, DALYs for both sexes, 2010 and 2019 for all level 2 GBD causes
eTable 16. Trends in incidence globally, and by SDI quintile, both sexes, 2010 to 2019
eTable 17. Trends in mortality globally, and by SDI quintile, both sexes, 2010 to 2019
eTable 18. Global age-standardized cancer estimates in 2019 and ranking among 22 level 2 categories of diseases and injuries in the Global Burden of Disease Study, overall and by quintile of socio-demographic index
eFigure 1. Socio-demographic index quintiles for the Global Burden of Disease Study 2019
eFigure 2. Flowchart GBD cancer mortality, YLL estimation
eFigure 3. Flowchart GBD cancer incidence, prevalence, YLD estimation
eFigure 4. Contribution of YLDs and YLLs to DALYs by cancer, global, both sexes, 2019
eFigure 5. Top-ranked cancers by absolute number of incident cases for all ages in males, 2019
eFigure 6. Top-ranked cancers by absolute number of deaths for all ages in males, 2019
eFigure 7. Top-ranked cancers by absolute number of incident cases for all ages in females, 2019
eFigure 8. Top-ranked cancers by absolute number of deaths for all ages in females, 2019
eFigure 9. Cancers ranked by disability-adjusted life years (DALYs) for males between 2010 and 2019
eFigure 10. Cancers ranked by disability-adjusted life years (DALYs) for females between 2010 and 2019
eFigure 11. Ranking of 29 cancer groups by mortality in 2019, by country and location group
eFigure 12. Ranking of 29 cancer groups by incidence in 2019, by country and location group
eFigure 13. Age-standardized rates and annualized rate of change for age-standardized rates for total cancers excluding non-melanoma skin cancer, all ages, both sexes
eFigure 14. Global counts of cancer-specific incidence and deaths in 2019, overall and by sex
eFigure 15. Global age-standardized cancer-specific incidence and mortality rates in 2019, overall and by sex
References
- 1.Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet. 2018;392(10159):2052-2090. doi: 10.1016/S0140-6736(18)31694-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012;13(8):790-801. doi: 10.1016/S1470-2045(12)70211-5 [DOI] [PubMed] [Google Scholar]
- 3.International Agency for Research on Cancer . World cancer report: cancer research for cancer prevention. Accessed March 1, 2021. https://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report-Cancer-Research-For-Cancer-Prevention-2020
- 4.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 71(3):209-249. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 5.United Nations . Sustainable development goals. Accessed March 3, 2021. https://sdgs.un.org
- 6.NCD Countdown 2030 Collaborators . NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. 2018;392(10152):1072-1088. doi: 10.1016/S0140-6736(18)31992-5 [DOI] [PubMed] [Google Scholar]
- 7.NCD Countdown 2030 Collaborators . NCD Countdown 2030: pathways to achieving sustainable development goal target 3.4. Lancet. 2020;396(10255):918-934. doi: 10.1016/S0140-6736(20)31761-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuderer NM, Choueiri TK, Shah DP, et al. ; COVID-19 and Cancer Consortium . Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907-1918. doi: 10.1016/S0140-6736(20)31187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023-1034. doi: 10.1016/S1470-2045(20)30388-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharpless NE. COVID-19 and cancer. Science. 2020;368(6497):1290. doi: 10.1126/science.abd3377 [DOI] [PubMed] [Google Scholar]
- 11.Addai BW, Ngwa W. COVID-19 and cancer in Africa. Science. 2021;371(6524):25-27. doi: 10.1126/science.abd1016 [DOI] [PubMed] [Google Scholar]
- 12.Sato Y, Fujiwara Y, Fukuda N, et al. ; COVID-19 Working Group of The Cancer Institute Hospital of Japanese Foundation for Cancer Research . Changes in treatment behavior during the COVID-19 pandemic among patients at a cancer hospital. Cancer Cell. 2021;39(2):130-131. doi: 10.1016/j.ccell.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.General Assembly of the United Nations . Prevention and control of non-communicable diseases. Accessed July 1, 2021. https://www.un.org/pga/72/event-latest/prevention-of-non-communicable-diseases/
- 14.United Nations . Resolution adopted by the General Assembly on 10 October 2019. Accessed March 3, 2021. https://undocs.org/en/A/RES/74/2
- 15.United Nations . The UN high-level meeting on universal health coverage. Accessed March 3, 2021. https://www.uhc2030.org/un-hlm-2019/
- 16.Anderson BO, Ilbawi AM, Fidarova E, et al. The Global Breast Cancer Initiative: a strategic collaboration to strengthen health care for non-communicable diseases. Lancet Oncol. 2021;22(5):578-581. doi: 10.1016/S1470-2045(21)00071-1 [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . Global strategy to accelerate the elimination of cervical cancer as a public health problem. Accessed February 16, 2021. https://www.who.int/publications-detail-redirect/9789240014107
- 18.World Health Organization . Global initiative for childhood cancer. Accessed July 1, 2021. https://www.who.int/publications/m/item/global-initiative-for-childhood-cancer
- 19.Bray F, Colombet M, Mery L, et al. Cancer incidence in five continents. vol XI (electronic version). Accessed March 1, 2021. https://ci5.iarc.fr
- 20.Vos T, Lim SS, Abbafati C, et al. ; GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang H, Abbas KM, Abbasifard M, et al. ; GBD 2019 Demographics Collaborators . Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1160-1203. doi: 10.1016/S0140-6736(20)30977-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fitzmaurice C, Abate D, Abbasi N, et al. ; Global Burden of Disease Cancer Collaboration . Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019;5(12):1749-1768. doi: 10.1001/jamaoncol.2019.2996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fitzmaurice C, Akinyemiju TF, Al Lami FH, et al. ; Global Burden of Disease Cancer Collaboration . Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2018;4(11):1553-1568. doi: 10.1001/jamaoncol.2018.2706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fitzmaurice C, Allen C, Barber RM, et al. ; Global Burden of Disease Cancer Collaboration . Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study. JAMA Oncology. 2017;3(4):524-548. doi: 10.1001/jamaoncol.2016.5688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitzmaurice C, Dicker D, Pain A, et al. ; Global Burden of Disease Cancer Collaboration . The global burden of cancer 2013. JAMA Oncol. 2015;1(4):505-527. doi: 10.1001/jamaoncol.2015.0735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray CJL, Aravkin AY, Zheng P, et al. ; GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-1249. doi: 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevens GA, Alkema L, Black RE, et al. ; GATHER Working Group . Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388(10062):e19-e23. doi: 10.1016/S0140-6736(16)30388-9 [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization . International Classification of Diseases: Ninth Revision, basic tabulation list with alphabetic index. Accessed March 1, 2021. https://apps.who.int/iris/handle/10665/39473
- 29.World Health Organization . International Statistical Classification of Diseases and Related Health Problems, 10th revision, 2nd edition. Accessed March 1, 2021. https://apps.who.int/iris/handle/10665/42980
- 30.Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8(1):9. doi: 10.1186/1478-7954-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Percy C, Ries LG, Van Holten VD. The accuracy of liver cancer as the underlying cause of death on death certificates. Public Health Rep. 1990;105(4):361-367. [PMC free article] [PubMed] [Google Scholar]
- 32.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166(5):1069-1080. doi: 10.1111/j.1365-2133.2012.10830.x [DOI] [PubMed] [Google Scholar]
- 33.Barber RM, Fullman N, Sorensen RJD, et al. ; GBD 2015 Healthcare Access and Quality Collaborators . Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. 2017;390(10091):231-266. doi: 10.1016/S0140-6736(17)30818-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10:1. doi: 10.1186/1478-7954-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reitsma MB, Fullman N, Ng M, et al. ; GBD 2015 Tobacco Collaborators . Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885-1906. doi: 10.1016/S0140-6736(17)30819-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reitsma MB, Kendrick PJ, Ababneh E, et al. ; GBD 2019 Tobacco Collaborators . Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet. 2021;397(10292):2337-2360. doi: 10.1016/S0140-6736(21)01169-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Flor LS, Reitsma MB, Gupta V, Ng M, Gakidou E. The effects of tobacco control policies on global smoking prevalence. Nat Med. 2021;27(2):239-243. doi: 10.1038/s41591-020-01210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization . WHO report on cancer: setting priorities, investing wisely and providing care for all. Accessed February 18, 2021. https://www.who.int/publications-detail-redirect/who-report-on-cancer-setting-priorities-investing-wisely-and-providing-care-for-all
- 39.GBD 2019 Universal Health Coverage Collaborators . Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1250-1284. doi: 10.1016/S0140-6736(20)30750-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cavalli F. Tackling cancer: time for a global response. Lancet. 2016;387(10018):e13-e14. doi: 10.1016/S0140-6736(16)00233-6 [DOI] [PubMed] [Google Scholar]
- 41.Allemani C, Matsuda T, Di Carlo V, et al. ; CONCORD Working Group . Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023-1075. doi: 10.1016/S0140-6736(17)33326-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Health. 2014;80(5):412-417. doi: 10.1016/j.aogh.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 43.Shah SC, Kayamba V, Peek RM Jr, Heimburger D. Cancer control in low- and middle-income countries: is it time to consider screening? J Glob Oncol. 2019;5:1-8. doi: 10.1200/JGO.18.00200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brand NR, Qu LG, Chao A, Ilbawi AM. Delays and barriers to cancer care in low- and middle-income countries: a systematic review. Oncologist. 2019;24(12):e1371-e1380. doi: 10.1634/theoncologist.2019-0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hricak H, Abdel-Wahab M, Atun R, et al. Medical imaging and nuclear medicine: a Lancet Oncology commission. Lancet Oncol. 2021;22(4):e136-e172. doi: 10.1016/S1470-2045(20)30751-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cortes J, Perez-García JM, Llombart-Cussac A, et al. Enhancing global access to cancer medicines. CA Cancer J Clin. 2020;70(2):105-124. doi: 10.3322/caac.21597 [DOI] [PubMed] [Google Scholar]
- 47.Martei YM, Iwamoto K, Barr RD, Wiernkowski JT, Robertson J. Shortages and price variability of essential cytotoxic medicines for treating children with cancers. BMJ Glob Health. 2020;5(11):e003282. doi: 10.1136/bmjgh-2020-003282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363-385. doi: 10.3322/caac.21565 [DOI] [PubMed] [Google Scholar]
- 49.Mollica MA, Falisi AL, Geiger AM, et al. Survivorship objectives in comprehensive cancer control plans: a systematic review. J Cancer Surviv. 2020;14(2):235-243. doi: 10.1007/s11764-019-00832-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dagenais GR, Leong DP, Rangarajan S, et al. Variations in common diseases, hospital admissions, and deaths in middle-aged adults in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2020;395(10226):785-794. doi: 10.1016/S0140-6736(19)32007-0 [DOI] [PubMed] [Google Scholar]
- 51.Roth GA, Mensah GA, Johnson CO, et al. ; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group . Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Franceschi S, Wild CP. Meeting the global demands of epidemiologic transition—the indispensable role of cancer prevention. Mol Oncol. 2013;7(1):1-13. doi: 10.1016/j.molonc.2012.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.World Health Organization . Cancer control: a global snapshot in 2015: summary of results from the 2015 WHO NCD Country Capacity Survey. Accessed July 1, 2021. https://apps.who.int/iris/handle/10665/326369
- 54.International Cancer Control Partnership . Developing a NCCP. Accessed July 1, 2021. https://www.iccp-portal.org/developing-nccp
- 55.World Health Organization . National cancer control programmes: policies and managerial guidelines. Accessed July 1, 2021. https://www.who.int/publications/i/item/national-cancer-control-programmes
- 56.Oar A, Moraes FY, Romero Y, Ilbawi A, Yap ML. Core elements of national cancer control plans: a tool to support plan development and review. Lancet Oncol. 2019;20(11):e645-e652. doi: 10.1016/S1470-2045(19)30404-8 [DOI] [PubMed] [Google Scholar]
- 57.Romero Y, Trapani D, Johnson S, et al. National cancer control plans: a global analysis. Lancet Oncol. 2018;19(10):e546-e555. doi: 10.1016/S1470-2045(18)30681-8 [DOI] [PubMed] [Google Scholar]
- 58.Stulac S, Binagwaho A, Tapela NM, et al. Capacity building for oncology programmes in sub-Saharan Africa: the Rwanda experience. Lancet Oncol. 2015;16(8):e405-e413. doi: 10.1016/S1470-2045(15)00161-8 [DOI] [PubMed] [Google Scholar]
- 59.Strasser-Weippl K, Chavarri-Guerra Y, Villarreal-Garza C, et al. Progress and remaining challenges for cancer control in Latin America and the Caribbean. Lancet Oncol. 2015;16(14):1405-1438. doi: 10.1016/S1470-2045(15)00218-1 [DOI] [PubMed] [Google Scholar]
- 60.Znaor A, Eser S, Anton-Culver H, et al. Cancer surveillance in northern Africa, and central and western Asia: challenges and strategies in support of developing cancer registries. Lancet Oncol. 2018;19(2):e85-e92. doi: 10.1016/S1470-2045(18)30019-6 [DOI] [PubMed] [Google Scholar]
- 61.WHO International Agency for Research on Cancer . The global initiative for cancer registry development. Accessed February 16, 2021. https://gicr.iarc.fr/about-the-gicr/
- 62.Piñeros M, Znaor A, Mery L, Bray F. A global cancer surveillance framework within noncommunicable disease surveillance: making the case for population-based cancer registries. Epidemiol Rev. 2017;39(1):161-169. doi: 10.1093/epirev/mxx003 [DOI] [PubMed] [Google Scholar]
- 63.Suh E, Stratton KL, Leisenring WM, et al. Late mortality and chronic health conditions in long-term survivors of early-adolescent and young adult cancers: a retrospective cohort analysis from the Childhood Cancer Survivor Study. Lancet Oncol. 2020;21(3):421-435. doi: 10.1016/S1470-2045(19)30800-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix.
eTable 1. Number of site-years for cancer mortality data by source type, for GBD 2019 compared to GBD 2017
eTable 2. Socio-demographic Index groupings by geography, based on 2019 values
eTable 3. List of International Classification of Diseases (ICD) codes mapped to the Global Burden of Disease cause list for cancer incidence data
eTable 4. List of International Classification of Diseases (ICD) codes mapped to the Global Burden of Disease cause list for cancer mortality data
eTable 5. Undefined cancer code categories (ICD-10) and respective target codes for cancer registry incidence data
eTable 6. Cancer registry sources for cancer incidence and mortality-to-incidence ratio data by country, year, and registry
eTable 7. Covariates selected for CODEm for each GBD cancer group and expected direction of covariate
eTable 8. Comparison of GBD 2017 and GBD 2019 covariates used and level of covariates
eTable 9. Results for CODEm model performance testing
eTable 10. Percent change before and after CoDCorrect by cancer for all ages, both sexes combined, 2019
eTable 11. Duration of four prevalence phases by cancer
eTable 12. Disability weights
eTable 13. GATHER5 guidelines checklist
eTable 14. Contribution of YLDs and YLLs to DALYs by cancer, global, both sexes, 2019
eTable 15. Global number of incidence, prevalence, YLDs, deaths, YLLs, DALYs for both sexes, 2010 and 2019 for all level 2 GBD causes
eTable 16. Trends in incidence globally, and by SDI quintile, both sexes, 2010 to 2019
eTable 17. Trends in mortality globally, and by SDI quintile, both sexes, 2010 to 2019
eTable 18. Global age-standardized cancer estimates in 2019 and ranking among 22 level 2 categories of diseases and injuries in the Global Burden of Disease Study, overall and by quintile of socio-demographic index
eFigure 1. Socio-demographic index quintiles for the Global Burden of Disease Study 2019
eFigure 2. Flowchart GBD cancer mortality, YLL estimation
eFigure 3. Flowchart GBD cancer incidence, prevalence, YLD estimation
eFigure 4. Contribution of YLDs and YLLs to DALYs by cancer, global, both sexes, 2019
eFigure 5. Top-ranked cancers by absolute number of incident cases for all ages in males, 2019
eFigure 6. Top-ranked cancers by absolute number of deaths for all ages in males, 2019
eFigure 7. Top-ranked cancers by absolute number of incident cases for all ages in females, 2019
eFigure 8. Top-ranked cancers by absolute number of deaths for all ages in females, 2019
eFigure 9. Cancers ranked by disability-adjusted life years (DALYs) for males between 2010 and 2019
eFigure 10. Cancers ranked by disability-adjusted life years (DALYs) for females between 2010 and 2019
eFigure 11. Ranking of 29 cancer groups by mortality in 2019, by country and location group
eFigure 12. Ranking of 29 cancer groups by incidence in 2019, by country and location group
eFigure 13. Age-standardized rates and annualized rate of change for age-standardized rates for total cancers excluding non-melanoma skin cancer, all ages, both sexes
eFigure 14. Global counts of cancer-specific incidence and deaths in 2019, overall and by sex
eFigure 15. Global age-standardized cancer-specific incidence and mortality rates in 2019, overall and by sex