Abstract
Anterior cruciate ligament (ACL) reconstruction is one of the most commonly performed orthopaedic sports procedures. Two main techniques are used for accomplishing an ACL reconstruction: transtibial and anteromedial portal techniques. The transtibial technique has been criticized for its inability to create an anatomic femoral tunnel given the intrinsic constraint of the tibial tunnel during drilling. However, technical modifications of the transtibial technique can result in anatomic tunnel entrance positioning and a properly oriented graft. This Technical Note presents our technique for anatomic transtibial ACL reconstruction.
Technique Video
This video describes our tips for a successful anatomic trans-tibial anterior cruciate ligament reconstruction (ACL). The steps highlight the technical modifications that can be implemented in the technique to help replicate the native anatomy by ensuring anatomical positioning of the tunnel entrance and proper orientation of the ACL graft.
In recent years, an increased emphasis has been placed on achieving anatomic anterior cruciate ligament (ACL) reconstruction and the techniques used to replicate the native anatomy.1 Creating the femoral tunnel through the tibial tunnel, termed transtibial (TT) reconstruction, is a common technique for ACL reconstruction. This technique is criticized for its inability to restore anatomic femoral tunnel placement because the femoral tunnel position is dependent on the orientation of the tibial tunnel. Previous cadaveric studies have demonstrated that anatomic placement of the femoral tunnel is possible but technically challenging when using the TT technique.2 Femoral tunnel placement through an anteromedial (AM) portal gained popularity because it allowed for femoral tunnel positioning independent of the tibial tunnel. Advocates of the AM technique suggest that it is better at reproducing femoral footprint anatomy and therefore coronal plane graft obliquity and results in a more anatomic graft.3 Anatomic placement of the femoral tunnel and graft obliquity in the sagittal plane are crucial to successful reconstruction. A graft that is too anterior in the sagittal plane can result in excessive tension on the graft and subsequent failure, and a vertical graft in the coronal plane has been shown to lead to suboptimal restoration of knee translation, rotational stability, and potential failure.4 This Technical Note presents our technique for arthroscopic anatomic transtibial ACL reconstruction for the treatment of a torn ACL.
Anatomic TT Surgical Technique
Preoperative Setup
The complete technique is demonstrated in a supplemental video (Video 1) and subsequent table (Table 1). The patient is positioned supine on the operative table with their operative knee overhanging the end of the operating table by approximately 6 inches depending on the patient size. The contralateral leg is abducted and placed in an operating table leg holder with the hip and knee flexed to protect the femoral and common peroneal nerves (Fig 1). After the administration of a general anesthetic, a physical examination (including Lachman, anterior drawer, and pivot shift) is performed to confirm instability of the knee and evaluate the range of motion (ROM).
Table 1.
How to Accomplish an Anatomic Anterior Cruciate Ligament Reconstruction Using a Transtibial Technique
| Tips and tricks | |
|---|---|
| Positioning | Patient at edge of the bed, with knee overhanging by ∼6 inches |
| Portals | Anterolateral and anteromedial portals will provide all the visualization needed |
| Preparation | Notchplasty increases visualization. Graft prepared and marked for easy passage |
| Tibial tunnel | Knee 90°, tibial guide 52°, guide’s outrigger arm parallel to tibial plateau Tip of guide within AM footprint of ACL |
| Femoral Tunnel | Knee 90°, 7mm offset guide introduced through tibial tunnel to the posterior aspect of the notch, rotated laterally to achieve lateral wall position Shoot for 10 o’clock in right knee, 2 o’clock in left knee Use half-fluted reamer to ream femoral tunnel |
| Placing the Graft | Notch femoral aperture anterosuperiorly Pass via pull through technique, ensuring marked deep surface of femoral bone plug is anterosuperior |
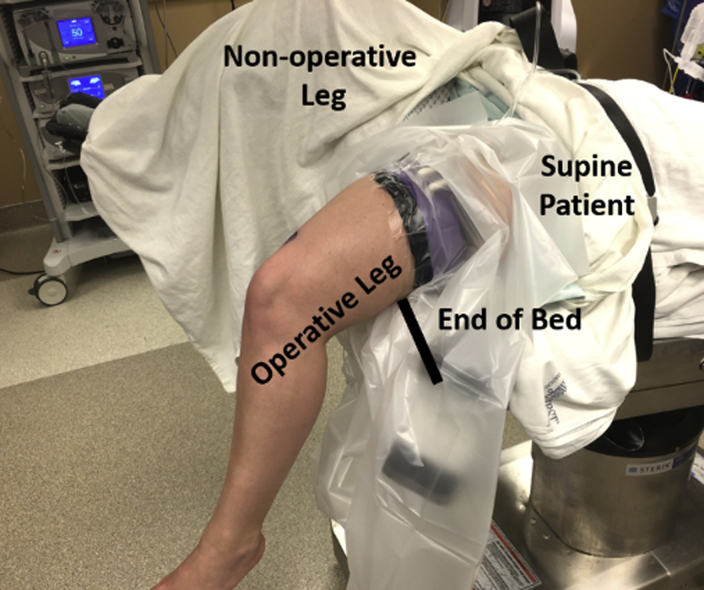
Fig 1.
The patient is positioned supine on the operative table. The waist of the table is reflexed and the foot of the table is flexed. The end of the table is removed to allow the operative leg (left leg) to hang down over the end of the bed. The nonoperative leg (right leg) is flexed, abducted and secured in an operating table leg holder. It is important to be cognizant of the resting position of the knee; the more proximal the tourniquet is placed the more the knee may be positioned in less flexion. This could result in a incorrectly positioned femoral tunnel that could result in intra tunnel “blowout.” Excessive hip extension should be avoided because it places traction on the femoral nerve.
Portal Placement and Preparation of the Knee
A standard anterolateral portal is created at the level of the distal pole of the patella and close to the edge of the patellar tendon. The anterolateral portal is used as a viewing portal for diagnostic arthroscopy and an anteromedial portal as a working portal. Knee arthroscopy begins with a general evaluation of the joint including identification of normal anatomy, loose bodies, cartilage defects, and meniscal tears. The torn ACL is documented by probing the remnant fibers. The ACL stump is debrided using a full radius shaver. A 5 mm arthroscopic bone cutter is used to perform a 2 to 3 mm notchplasty of the medial wall of the lateral femoral condyle to improve visualization. An arthroscopic ruler of 7 mm wide osteotome can be inserted to give an assessment of the amount of notchplasty needed or achieved relative to the lateral edge of the posterior cruciate ligament.
Preparing the Graft
Bone tendon bone (BTB) grafts are the authors’ preference in most cases, and this article will describe BTB preparation and passage. The BTB auto or allograft is harvested and prepared in the standard fashion, resulting in a 10 × 20 bone plug for the femoral side and a 10 × 25 mm bone plug for the tibial tunnel. The bone plugs are sized to easily fit through a 10 mm tunnel. Drill holes are placed in the femoral and tibial bone plugs of the graft with a 0.062 K-wire, 1 hole anterior to posterior on the femoral side and 2 holes medial to lateral on the tibial side (Fig 2). The femoral bone plug is marked on its deep surface with a line parallel to graft fiber orientation; this marking will later aid in the passage of the graft within the knee.
Fig 2.
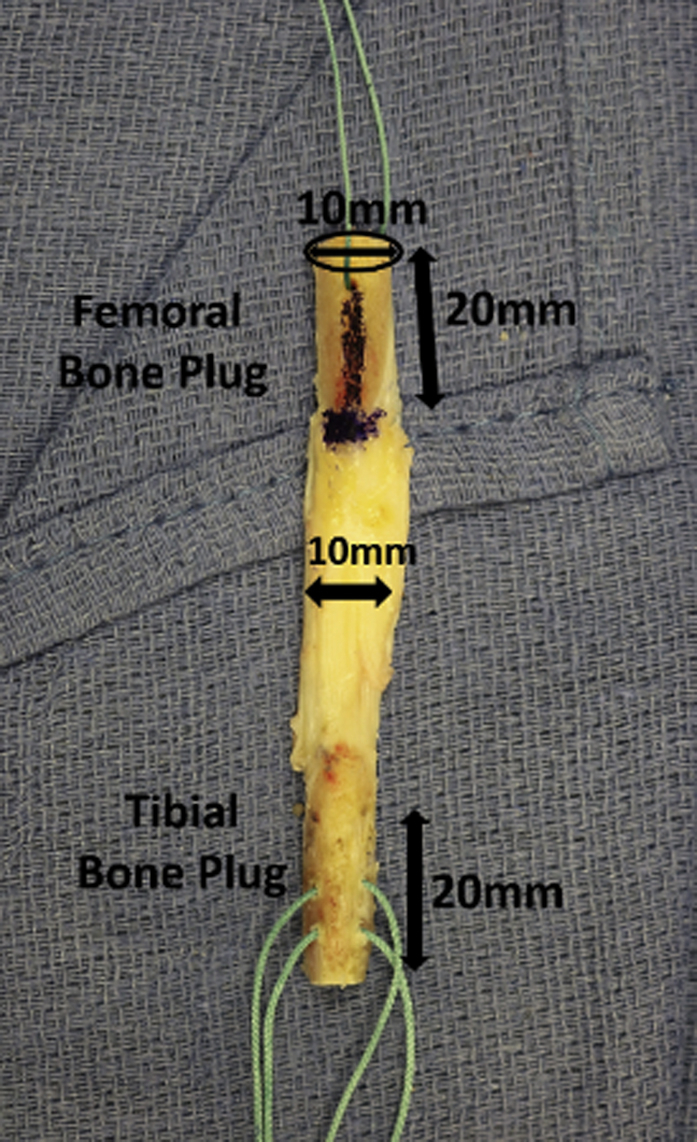
The bone-tendon-bone graft is prepared by creating a 10 mm–wide graft with 20 to 25 mm bone plugs at each end of the graft. One anterior-posterior suture is passed in the femoral bone plug and 2 medial-lateral sutures in the tibial bone plug.
Drilling the Tunnels
With the knee at 90° of flexion, the tibial drill guide (Smith & Nephew, Andover, MD) is inserted through an accessory transpatellar tendon portal. The guide is set at approximately 52° to 55° to match the native vertical orientation of the ligament and oriented such that the outrigger arm remains parallel to the tibial plateau. The external entry point of the tibial guide is placed between the anterior aspect of the medial collateral ligament and the tibial tubercle. The tip of the guide is placed within the anteromedial bundle portion of the ACL’s tibial footprint, using the inner edge of the anterior horn of the lateral meniscus and posterior cruciate ligament as landmarks. Placement is slightly more anterior compared to traditional descriptions of the transtibial technique. The goal is to have the posterior aspect of the tunnel in line with the posterior aspect of the anterior horn lateral meniscus (Fig 3). If the tunnel is placed too posteriorly, it can result in increased graft angle in the sagittal plane.
Fig 3.
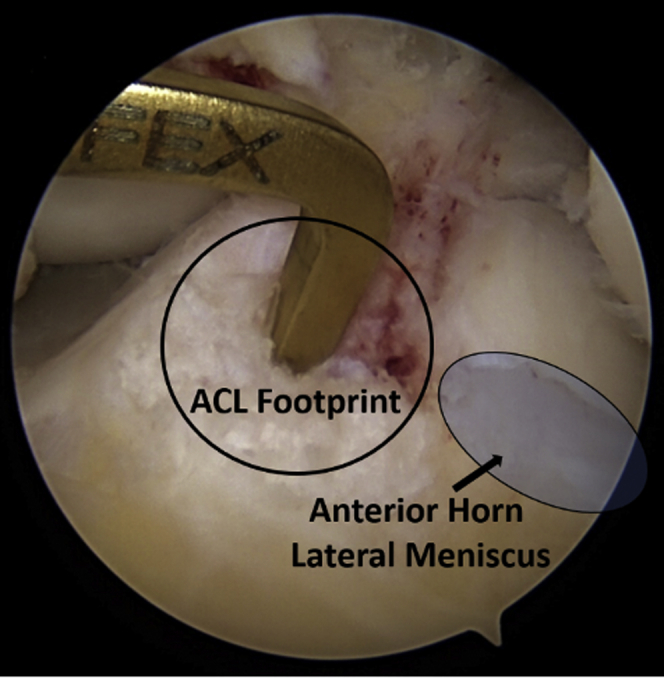
Left knee viewed arthroscopically from an anterolateral portal. The tibial drill guide is inserted into the knee through a central transpatellar tendon portal and placed in an anatomic position within the anteromedial portion of the tibial footprint with the posterior aspect of the tunnel in line with the posterior aspect of the anterior horn lateral meniscus. This aiming device is a “tip-to-tip” aimer so that the drill wire should enter the joint at the tip of the aimer stylet.
A guide pin is then drilled into the joint. After pin placement, the aiming device is removed and a cannulated reamer equal to the graft diameter is used to create the tibial tunnel (10-11 mm). One can tap the wire up into the lateral femoral wall to stabilize it while reaming.
A standardized 7 mm offset femoral guide is then introduced through the tibial tunnel and placed at the posterior aspect of the notch with the knee between 80° and 90° of knee flexion. The discrepancy between the size of the tibial tunnel and the diameter of the femoral offset guide can be taken advantage of to allow increased obliquity to access the lateral wall footprint position on the femur. Moreover, the guide can be rotated to achieve a further lateral wall position. However, as the tibial tunnel size is reduced (<8 mm), as may occur in hamstring reconstruction, the ability to reach the appropriate femoral position may be compromised.5 The femoral offset guide should be rotated laterally and slide off the “over-the-top” position confirming appropriate lateral wall position for the guide pin. A K-wire is placed in a position that has been determined by the femoral guide (usually at approximately the 10 o’clock position for the right knee or at approximately the 2 o’clock position for the left knee) (Fig 4). The K-wire is overdrilled with a half-fluted reamer corresponding to the size of the graft diameter and to a depth of 30 mm. A half-fluted reamer is used to preserve the integrity of the tibial tunnel, preventing posteriorization, while still allowing access to the femoral tunnel. The half-fluted reamer is introduced into the joint manually marinating the flutes in an anterior position. Once in the joint, the reaming can be initiated, and the tunnel is drilled. The reamer is similarly removed by hand. In doing so, the surgeon can avoid inadvertent posteriorization of the tibial tunnel aperture.
Fig 4.
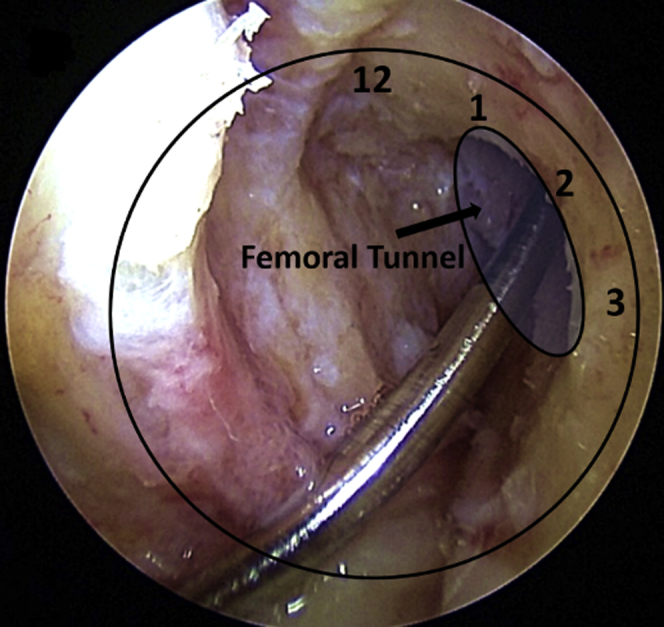
Left knee viewed arthroscopically from an anterolateral portal. When drilling the femoral tunnel through the tibial tunnel, one should aim at approximately the 10 o’clock position for the right knee or at approximately the 2 o’clock position for the left knee.
Graft Placement
The aperture of the femoral tunnel is notched anterosuperiorly using a tunnel notch to allow for easier passage of the bone plug into the femoral tunnel. The graft is passed via a pull-through technique. Before seating, the femoral bone plug is rotated such that the previously marked cancellous surface of the femoral bone plug faces anterior/superior to fit into the notched aperture (Fig 5). This also serves to place the soft tissue portion of the graft in a posterior-inferior position, allowing improved coverage of the native ACL footprint. The femoral side is then secured with a 7 × 20 mm metal interference screw. The graft is then cyclically tensioned and secured under manual tension in full extension with a 7 to 9 × 20 metal interference screw (Fig 6). If the tibial bone plug extends beyond the tibial cortex, there are 3 steps that can be taken to shorten the graft without compromising its mechanical properties: (1) recess the femoral graft up to 10 mm in the overdrilled femoral tunnel; (2) shorten the tibial bone plug, by no more than 5 mm allowing for at least 15 mm of bone plug to remain, with an oscillating Microaire saw while the graft is in place; or (3) rotate the tibial bone plug 1 full rotation to shorten the tendinous portion of the graft. If these methods do not accommodate the graft size, a free bone plug technique can be used.6 Check final graft position within the knee to ensure adequate tension and motion (Fig 7).
Fig 5.
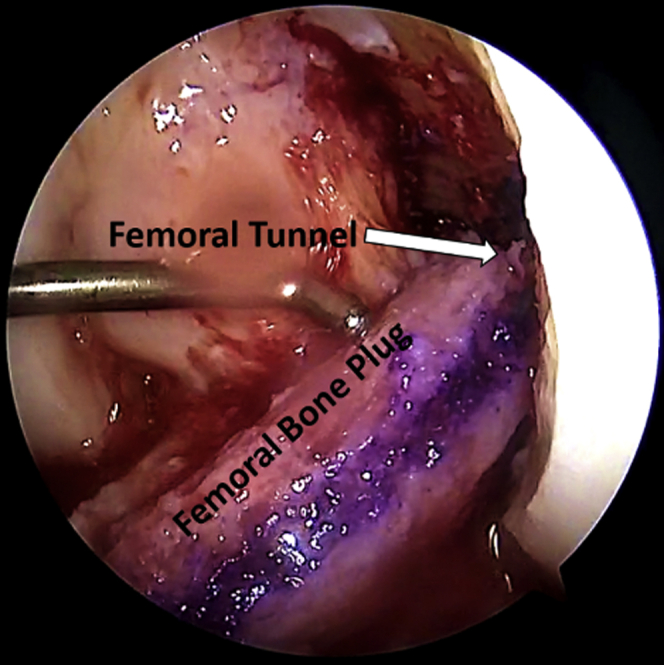
Left knee viewed arthroscopically from an anterolateral portal. During pull through of the bone-tendon-bone graft, the femoral bone plug is rotated such that the deep surface faces anteriorly and fits through the anterosuperiorly notched femoral tunnel aperture.
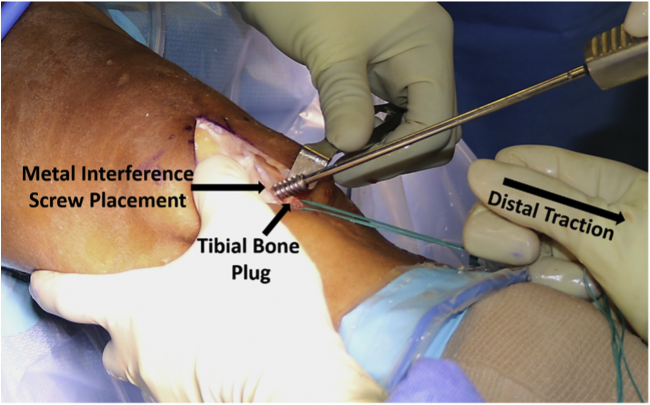
Fig 6.
Left knee in full extension, distal traction is applied to the graft. A metal interference screw is place next to the graft within the tibial tunnel.
Fig 7.
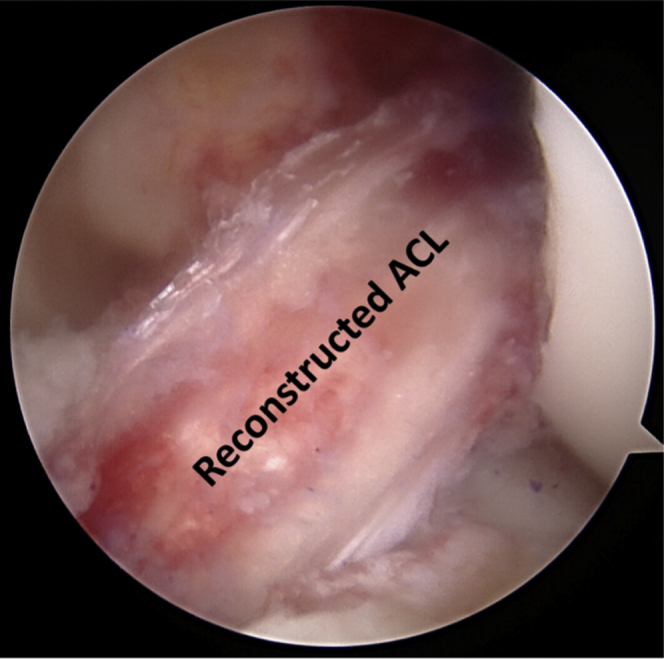
Left knee viewed arthroscopically from an anterolateral portal. Final position and tension of the graft is observed arthroscopically. Motion is also evaluated to check for graft impingement.
Rehabilitation
The knee is placed in a locking hinged knee brace that is locked in full extension. From 0 to 2 weeks, weightbearing is allowed as tolerated with the brace locked at 0° for ambulation and sleeping. ROM is allowed from 0° to 90° of flexion. At 2 weeks ROM is advanced to 0° to 125° of flexion, and the brace is unlocked, then discontinued around 4 weeks if quadriceps control is adequate. A step-up program is initiated at 2 weeks in addition to simple exercises such as weight shifts and mini-squats. At 6 weeks step-down and progressive squat programs are initiated, and exercises are advanced to leg press and lunges. Forward running and sports-specific agility drills are started around 14 weeks when 8″ step down is satisfactory. At 6 to 8 months the athlete is allowed to return to sport, at the discretion of the authors. Newer functional sports assessments now provide a good metric for readiness to return to sport.7
Discussion
The ability to produce an anatomic ACL reconstruction with the trans-tibial technique continues to be debated given the constraints of the tibial tunnel during placement of the femoral tunnel. However, with proper technique, an anatomic reconstruction can still be made with the transtibial technique.2,8 Important technical points are highlighted in Table 1 and described above. Previous literature generally reports no clinical outcome differences between transtibial and anteromedial reconstruction techniques.9 Given that literature comparing these two techniques is equivocal, the choice of technique should be based upon the operating surgeon’s comfort level and preference. There are advantages and disadvantages to both techniques that should be considered (Table 2). It is advisable to be proficient in both techniques to allow for intraoperative adjustments and deviations.
Table 2.
Advantages and Disadvantages to the Transtibial and Anteromedial Techniques for Anterior Cruciate Ligament Reconstruction
| Transtibial technique |
| Advantages |
| Isometric graft placement |
| Possibility of reaching native femoral insertion if tibial tunnel is made appropriately |
| Ease of graft passage |
| Familiarity and proven long-term outcomes |
| Disadvantages |
| Risk for non-anatomic graft placement |
| Femoral tunnel placement constrained by tibial tunnel |
| Tendency to create a vertical graft which can cause rotational instability and pivot shift if not appropriately positioned |
| Short oblique tibial tunnel in an attempt to achieve anatomic ACL reconstruction |
| Anteromedial technique |
| Disadvantages |
| Requires hyperflexion of the knee (requiring qualified assistants) |
| Can result in a short femoral tunnel |
| Can result in posterior wall blow-out due to tunnel angle |
Footnotes
The authors report the following potential conflict of interest or source of funding: B.R.B. reports grants from Arthrex, Inc, CONMED Linvatec, DJ Orthopaedics, Ossur, Smith & Nephew, and Tornier; and personal fees from SLACK Incorporated and Smith & Nephew. J.C. reports other from Arthrex, Inc, CONMED Linvatec, Ossur, and Smith & Nephew; and is a Board Member/Committee Appointments for American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine. N.N.V. reports other from the American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, Arthrex, Inc, Arthroscopy, Arthroscopy Association of North America, Breg, Cymedica, Knee, Minivasive, Omeros, Orthospace, Ossur, SLACK incorporated, Smith & Nephew, Vindico Medical-Orthopedics Hyperguide, and Wright Medical Technology, Inc. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video describes our tips for a successful anatomic trans-tibial anterior cruciate ligament reconstruction (ACL). The steps highlight the technical modifications that can be implemented in the technique to help replicate the native anatomy by ensuring anatomical positioning of the tunnel entrance and proper orientation of the ACL graft.
References
- 1.Fu F.H., van Eck C.F., Tashman S., Irrgang J.J., Moreland M.S. Anatomic anterior cruciate ligament reconstruction: A changing paradigm. Knee Surg Sports Traumatol Arthrosc. 2015;23:640–648. doi: 10.1007/s00167-014-3209-9. [DOI] [PubMed] [Google Scholar]
- 2.Piasecki D.P., Bach B.R., Jr., Espinoza Orias A.A., Verma N.N. Anterior cruciate ligament reconstruction: Can anatomic femoral placement be achieved with a transtibial technique? Am J Sports Med. 2011;39:1306–1315. doi: 10.1177/0363546510397170. [DOI] [PubMed] [Google Scholar]
- 3.Harner C.D., Honkamp N.J., Ranawat A.S. Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy. 2008;24:113–115. doi: 10.1016/j.arthro.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 4.Lee M.C., Seong S.C., Lee S., et al. Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy. 2007;23:771–778. doi: 10.1016/j.arthro.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia S., Korth K., Van Thiel G.S., et al. Effect of tibial tunnel diameter on femoral tunnel placement in transtibial single bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:51–57. doi: 10.1007/s00167-014-3307-8. [DOI] [PubMed] [Google Scholar]
- 6.Novak P.J., Wexler G.M., Williams J.S., Jr., Bach B.R., Jr., Bush-Joseph C.A. Comparison of screw post fixation and free bone block interference fixation for anterior cruciate ligament soft tissue grafts: Biomechanical considerations. Arthroscopy. 1996;12:470–473. doi: 10.1016/s0749-8063(96)90042-0. [DOI] [PubMed] [Google Scholar]
- 7.Abrams G.D., Harris J.D., Gupta A.K., et al. Functional performance testing after anterior cruciate ligament reconstruction: A systematic review. Orthop J Sports Med. 2014;2 doi: 10.1177/2325967113518305. 2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao J. Anatomic double-bundle transtibial anterior cruciate ligament reconstruction. Arthrosc Tech. 2021;10(3):e683–e690. doi: 10.1016/j.eats.2020.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chalmers P.N., Mall N.A., Cole B.J., Verma N.N., Bush-Joseph C.A., Bach B.R., Jr. Anteromedial versus transtibial tunnel drilling in anterior cruciate ligament reconstructions: A systematic review. Arthroscopy. 2013;29:1235–1242. doi: 10.1016/j.arthro.2013.02.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video describes our tips for a successful anatomic trans-tibial anterior cruciate ligament reconstruction (ACL). The steps highlight the technical modifications that can be implemented in the technique to help replicate the native anatomy by ensuring anatomical positioning of the tunnel entrance and proper orientation of the ACL graft.
This video describes our tips for a successful anatomic trans-tibial anterior cruciate ligament reconstruction (ACL). The steps highlight the technical modifications that can be implemented in the technique to help replicate the native anatomy by ensuring anatomical positioning of the tunnel entrance and proper orientation of the ACL graft.