Abstract
The Worldwide Alzheimer's Disease Neuroimaging Initiative (WW‐ADNI) is a collaborative effort to investigate imaging and biofluid markers that can inform Alzheimer's disease treatment trials. It is a public‐private partnership that spans North America, Argentina, Australia, Canada, China, Japan, Korea, Mexico, and Taiwan. In 2004, ADNI researchers began a naturalistic, longitudinal study that continues today around the globe. Through several successive phases (ADNI‐1, ADNI‐GO, ADNI‐2, and ADNI‐3), the study has fueled amyloid and tau phenotyping and refined neuroimaging methodologies. WW‐ADNI researchers have successfully standardized analyses and openly share data without embargo, providing a rich data set for other investigators. On August 26, 2020, the Alzheimer's Association convened WW‐ADNI researchers who shared updates from ADNI‐3 and their vision for ADNI‐4.
Keywords: Alzheimer's disease, amyloid, biomarkers, cerebrospinal fluid, cognitive impairment, MRI, neuroimaging, PET, Tau
1. INTRODUCTION
The Alzheimer's Disease Neuroimaging Initiative (ADNI) is an ongoing, naturalistic study to understand structural, biochemical, and cognitive changes that occur during Alzheimer's disease (AD) progression. ADNI investigators leverage imaging, blood, and cerebrospinal fluid (CSF) analysis, and clinical, genetic, and postmortem neuropathologic databases to define markers for each stage of AD. 1 Data obtained through ADNI are used to inform clinical trial design and sufficiently power trials. ADNI data can also help establish outcome measures and identify appropriate trial participants.
North American ADNI investigators are organized into distinct cores centered around: positron emission tomography (PET), magnetic resonance imaging (MRI), fluid (blood, CSF) biomarkers, genetics, biostatistics, autopsy neuropathology, and clinical data with an informatics core for widespread data sharing without embargo. More broadly, Worldwide ADNI (WW‐ADNI) now encompasses neuroimaging initiatives from nine distinct regions. It serves as the umbrella organization for North American ADNI, Argentina ADNI, Australia ADNI (AIBL), Canada ADNI, China ADNI, Japan ADNI, Korea ADNI, Mexico ADNI, and Taiwan ADNI. Biologic samples are shared and all WW‐ADNI investigators are tasked with harmonizing research methodologies so that data can be readily combined.
1.1. WW‐ADNI evolution
WW‐ADNI is the result of several successive phases. The first phase, ADNI‐1, launched in 2004. ADNI‐1 established much of the organizational structure still in place within the North American ADNI, including core facilities. 2 , 3 , 4 In total, 821 participants with and without mild cognitive impairment (MCI) or AD enrolled in ADNI‐1 across 57 study sites. 1
Two subsequent phases followed: ADNI “Grand Opportunities” (ADNI‐GO) and ADNI‐2. ADNI‐GO supported amyloid PET scans for ADNI‐1 participants plus enrollment of 200 early MCI participants. 5 ADNI‐2 further expanded the study population by 550 to include people with other forms of memory impairment.
A 5‐year competitive renewal of ADNI‐2, called ADNI‐3, began in 2016. ADNI‐3 is actively enrolling up to 1200 additional participants across the entire spectrum of AD. ADNI‐3 has moved research and study enrollment tools to the web to improve accessibility (http://adni.loni.usc.edu/) and introduced longitudinal tau PET scans. A major goal of ADNI‐3 is to validate longitudinal tau PET imaging. Considerably more that 2000 participants have been enrolled since 2004.
Although ADNI‐3 currently includes 59 study sites in North America, international collaboration continues through WW‐ADNI, with support from the Private Partner Scientific Board (PPSB). 6 WW‐ADNI's expansive, global network has produced more than 3500 publications. 1 , 5 , 7 This body of work provides a foundation for the next phase, ADNI‐4, a competitive application for renewal of ADNI‐3 slated for September 2021. In August 2020, WW‐ADNI investigators held a virtual meeting to share updates and their vision for ADNI‐4.
2. NORTH AMERICAN ADNI
Since 2004, North American ADNI investigators have enrolled more than 2000 study participants (at least 955 MCI, 350 AD, and 505 cognitively unimpaired) across 59 study sites.
2.1. PET core
The PET core has amassed thousands of brain PET scans that can be downloaded by qualified users. The scans employ 18F‐labeled tracers: florbetapir (Amyvid), florbetaben (Neuraceq), flortaucipir (Tauvid), and fluorodeoxyglucose. The core has established methods to control variability in PET scan data. 8 Longitudinal data are now available for florbetapir and flortaucipir PET scans. For example, WW‐ADNI's collection of florbetapir images, which began with ADNI‐1, now includes baseline, 1307; second, 769; third, 453; fourth, 246; fifth, 84; and sixth, 5 sequential florbetapir PET scans.
The core has established interrelationships between PET markers. Amyloid appears to drive cortical tau accumulation and is a more significant marker of tau burden than MCI diagnosis. 9 By characterizing individuals according to the current research framework, 10 individuals in ADNI were classified according to ATN (amyloid, tau, neurodegeneration) criteria. Those who were positive for all three biomarkers showed the greatest cognitive impairment. In longitudinal data, brain amyloid beta (Aβ) drives tau accumulation, and tau accumulation drives neurodegeneration. The presence of high tau and neurodegeneration is linked to cognitive decline. There is no evidence that tau levels lead to greater β‐amyloid deposition, or that neurodegeneration leads to tau deposition. Together these results are consistent with a unidirectional pathway linking amyloid, tau, and neurodegeneration in a sequential pattern leading to cognitive decline and dementia. 11
2.2. MRI core
The MRI core uses several sequences, including three‐dimensional (3D) T1 volume, 3D fluid‐attenuated inversion recovery (FLAIR), and T2* gradient echo (GRE), plus associated measurements. The core's technical capacities also include diffusion‐weighted MRI (dMRI), arterial spin labeling (ASL) in 2D and 3D, task‐free functional MRI (TF‐fMRI), and coronal high‐resolution T2 sequences. 5 , 12 The core has developed standardized protocols 5 for these sequences that can be employed across WW‐ADNI.
RESEARCH IN CONTEXT
Systematic review: The WW‐ADNI meeting provided investigators an opportunity to share updates from ADNI‐3 and a look forward to the development of ADNI‐4.
Interpretation: WW‐ADNI is a global, collaborative effort to investigate imaging and biofluid markers that can inform AD treatment trials.
Future directions: ADNI‐4 looks to build on the success of previous phases (ADNI‐1, ADNI‐GO, ADNI‐2, and ADNI‐3) through validation of emerging biomarkers, and a focus on their generalizability and their relationships to cognitive decline and dementia symptoms.
The core has developed basic and advanced protocols 9 to accommodate MRI system variability and evolving operating systems. ADNI‐3 imaging is being performed exclusively on 3T scanners. The core is performing meta‐analyses of site‐specific effects, 13 random‐effects regressions to identify scanner‐specific effects, and adjusting data before pooling 14 or encoding it to eliminate bias. 15
A newly identified risk has been the potential identification of participants based on MRI, through publicly available facial recognition software. 16 Standard MRI de‐identification removes only metadata (text). Removing or blurring face voxels can compromise other measurements, particularly in the frontal regions. 17 A committee within the MRI core is now charged with determining which defacing algorithms are most effective at anonymization while preserving data integrity.
2.3. Biomarker core
With ADNI‐3, the Biomarker core's collection of CSF, plasma, and serum grew by > 1700 samples for new enrollees and > 1600 for rollover participants. More than half (55%) of all new participants have received a lumbar puncture. The core has standardized biofluid collection and processing 18 , 19 across WW‐ADNI sites. The core has also standardized ultraperformance liquid chromatography‐tandem mass spectrometry (MS) 3 , 20 and multiplexed MS. 21 In ADNI‐3, the core revised their protocol to reduce total collection time for plasma samples to under 1 hour.
The core has worked with the Foundation for the National Institutes of Health ‐ Biomarkers Consortium (FNIH ‐ BC) to conduct a multicenter study using replicate sets of 130 ADNI plasma aliquot samples distributed to each of six participating centers. Results and analyses will be conducted in early 2021. The core has shipped >30,000 aliquots to researchers around the world who provided data for additional pathologic pathways (eg, neurogranin, Neurofilament light chain (NfL), soluable triggering receptor expressed on myeloid cells 2 (sTREM2), Neuronal Pentraxin 2 (NPTX2)) following review and approval by the WW‐ADNI Resource Allocation Review Committee (RARC). 21 , 22 , 23 , 24 RARC is made up of non‐ADNI investigators and serves as a gatekeeper for this precious resource.
In anticipation of increased plasma sample requests in ADNI‐4, the core is investigating how factors such as delayed centrifugation, aliquot size, and multiple freeze‐thaw cycles affect AD biomarker integrity. Concentration values for the core CSF biomarkers have been determined on >3000 CSF samples collected in the ADNI‐1/‐GO/‐2 and ‐3 Phases using the highly standardized automated Roche Elecsys system.
2.4. Genetics core
Although many studies that use Genetics core data focus on APOE and other risk variants, 25 ADNI‐3 has brought collaborations to study polygenic risk scores, epigenetics, transcriptomics, proteomics, and metabolomics.
For example, one group integrated data from six multicenter cohort studies (4314 participants). The group successfully identified common variants in RBFOX1 associated with early brain amyloidosis. 26 Another identified genetic determinants of hippocampal volume in 33,536 individuals. 27 For Ribonucleic acid (RNA), genomewide transcriptome analyses of ADNI core data identified novel genes dysregulated in AD pathology: CREB5, CD46, TMBIM6, IRAK3, and RPAIN. 28 An epigenome‐wide association study identified differentially methylated profiles in peripheral blood between MCI and AD participants. 29 Metabolomics researchers within the Genetics core found sex‐specific effects. APOE ε4–positive women experience greater mitochondria impairment than men do. 30 In ADNI‐4, the group plans to extend polygenic analyses. The core is also testing deep learning as an approach to analyzing multilayer ‐omics data.
2.5. Biostatistics core
This year, due to disruptions caused by the coronavirus disease 2019 (COVID‐19) pandemic, the Biostatistics core has been investigating the impact of missing data on longitudinal modeling and analyses. This includes determining whether data collected at home are comparable to clinic data. Participants in CogState studies, 14 for example, complete cognitive tests both at home and in a clinic, with significantly faster response times at home. The core is developing approaches to accommodate this factor when analyzing future cognitive testing data, including in ADNI‐4.
The core is also investigating the effects of attrition or scheduling abnormalities caused by COVID‐19. The core is determining how adjusting data collection timing (an early or late timestamp) impacts planned analyses and power. Biostatistics core simulations show that a generalized additive mixed‐models approach has more power that a mixed model for repeated measures to detect differences when there is a study hiatus, especially if the gap in data collection is long. 31 In anticipation of ADNI‐4, the core is also developing models that allow for time as a continuous (rather than categorical, or timestamped) measurement. This will support adaptations that preserve power even if there are measurement gaps due to COVID‐19 or unforeseen circumstances.
2.6. Neuropathology core
In its original funding period, ADNI‐1 did not have provisions for the neuropathologic assessment of deceased ADNI participants or for the establishment of a brain tissue resource; hence, ADNI began without a Neuropathology Core (NPC).
The ADNI NPC was established in 2007 as a “sub‐study” of ADNI‐1, with an administrative supplement from the National Institute on Aging (NIA), but with very limited resources and no authorization to maintain contact with willing, consented brain donors beyond their period of active enrollment. As a result, participant tracking was left to individual sites without financial support from ADNI. Although 33 of the 59 North American ADNI sites are associated with established Alzheimer's Disease Research Centers (ADRCs), many of the non‐ADRC sites lack independent brain donation programs and/or the capacity to secure brain donations. Consequently, ADNI's brain donation program started slowly, with only 32 sites contributing case material to the NPC by 2020.
In 2021, the ADNI NPC conducted a retrospective review of completed neuropathologic assessments (N = 81). All of these cases were evaluated according to a comprehensive, uniform protocol for Aβ deposits, tauopathy, alpha‐synucleinopathy (Lewy body disease), TDP‐43 proteinopathy, vascular disease, infarctions, and hemorrhages. Clinicopathologic correlation of those cases revealed that, among ADNI participants with a clinical diagnosis of AD dementia at expiration, 18% did not have sufficient AD neuropathology to account for dementia–in other words, their dementia was not caused by AD. In addition, 85% of the participants whose dementia likely was caused by AD pathology also exhibited features of at least one other neurodegenerative disease with the potential to have contributed to their illness. These findings underscore how essential that neuropathologic confirmation will be for ADNI to develop truly accurate biomarkers for AD and related dementias.
Recognizing the vital importance of neuropathologic confirmation and the potential value of a large brain tissue resource for the discovery and validation of molecular biomarkers of AD and other neurodegenerative pathologies, ADNI Leadership helped the NPC to secure two administrative supplements from the NIA in 2019 and 2020. The first strengthened the central infrastructure and staffing of the ADNI NPC; the second is working to bolster the brain donation program across the entire North American ADNI network.
Over the past 2 years, these investments have allowed the ADNI NPC to expand its resource to >115 brain donations, to identify at least 50 additional ADNI‐participant brain donations previously assessed at participating ADRCs, to increase support of ADNI brain donation efforts at participating sites, and to persuade several ADNI sites to join ADNI's brain donation program network for the first time.
As ADNI‐4 approaches, the ADNI‐NPC will continue its efforts to strengthen and build new connections within the ADNI brain donation network, to expand the tissue resource, and to comprehensively assess all donated specimens for relevant neuropathology. In ADNI‐4, the NPC will additionally actively promote, coordinate, and participate in the study of this resource, governed by the ADNI Neuropathology Resource Allocation Review Committee (RARC), to support the scientific initiatives and aims of ADNI and approved extramural investigations.
2.7. Clinical core
Many ADNI participants have transitioned between diagnostic groups as their disease has progressed. The Clinical core has identified participants who have transitioned from cognitively unimpaired to MCI and from MCI to AD. These subpopulations are invaluable for modeling studies designed to predict cognitive impairment. Similarly, the core has identified participants who do not progress from early to late MCI or AD, due to genetic or other factors. Table 1 details participant demographics, biomarkers, and assessment results from ADNI‐3.
TABLE 1.
ADNI‐3 participants
| Overall | CN | MCI | AD | Unknown | Combined | |
|---|---|---|---|---|---|---|
| (N = 509) | (N = 288) | (N = 109) | (N = 63) | (N = 969) | ||
| Rollover | 969 | 213 (42%) | 126 (44%) | 50 (46%) | 51 (81%) | 440 (45%) |
| Age | 969 | 73.7 (7.6) | 75.2 (8.0) | 77.6 (8.8) | 78.3 (8.8) | 74.9 (8.1) |
| APOE e4+ | 762 | 142 (32%) | 76 (39%) | 40 (59%) | 18 (35%) | 276 (36%) |
| Sex : F | 969 | 300 (59%) | 119 (41%) | 48 (44%) | 31 (49%) | 498 (51%) |
| Education | 969 | 16.8 (2.3) | 16.2 (2.6) | 15.7 (2.5) | 16.3 (2.6) | 16.5 (2.5) |
| Amyloid+ | 785 | 141 (31%) | 111 (47%) | 73 (85%) | 1 (33%) | 326 (42%) |
| Minority | 969 | 82 (16%) | 37 (13%) | 11 (10%) | 9 (14%) | 139 (14%) |
| Mini Mental State Examination (MMSE) | 922 | 29.1 (1.2) | 27.8 (2.1) | 21.8 (4.7) | 28.3 (2.6) | 27.8 (3.1) |
| Financial Capacity Instrument (FCI) | 839 | 68.1 (6.0) | 60.4 (12.1) | 39.7 (18.9) | 64.7 (8.1) | 63.0 (12.9) |
|
Clinical Dementia Rating Scale‐Sum of Boxes (CDR‐SB) |
944 | 0.073 (0.257) | 1.484 (1.218) | 5.743 (3.290) | 3.409 (5.683) | 1.309 (2.550) |
|
Alzheimer's Disease Assessment Scale‐cognitive subscale (ADAS‐cog13) |
908 | 12.7 (4.3) | 19.3 (6.5) | 34.4 (8.5) | 15.0 (8.8) | 17.3 (8.9) |
The Clinical core has identified demographic gaps in the ADNI‐3 cohort. Currently only 14% of ADNI‐3 participants identify as racial or ethnic minorities. Most identify as Caucasian and >90% have a 4‐year college education. This spurred formation of a Diversity Taskforce within WW‐ADNI. ADNI‐4 will employ targeted recruitment strategies, supported by dedicated funding for Black and Latinx participants and recruiters. These efforts will also focus on AD enrollment. Competition with treatment trials significantly impacted AD participant enrollment in ADNI‐3.
2.8. Planning for ADNI‐4
Funding for US ADNI‐3 ends August 2022, and ADNI‐4 planning is underway (Figure 1). A renewal grant for ADNI‐4 was submitted to the NIA in Oct 2021. ADNI posted a Request for Proposals on the ADNI website, and received more than 30 responses for plasma, PET, and digital biomarkers. ADNI‐4 will be similar to ADNI‐3, with several major additions: First, to make ADNI more generalizable, the exclusion criteria will be relaxed. In addition, an Engagement Core will focus on recruiting many more people from the Black, Latino, and Asian communities, and people with lower socioeconomic status. Second, because of the excitement concerning use of plasma AD markers, ADNI‐4 plans to obtain blood from 4000 participants and use the results to select 500 for referral to the ADNI clinics for in‐person evaluation, MRI, PET scans, blood tests, genetics, and lumbar puncture. Finally, ADNI is exploring greater use of digital biomarkers.
FIGURE 1.
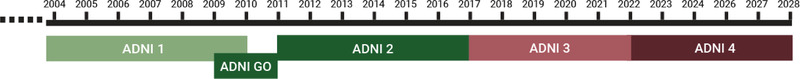
ADNI‐1 through ADNI‐4 timeline
3. WORLDWIDE ADNI
WW‐ADNI provides a larger platform for ADNI researchers to collaborate. This aligns with a major goal of ADNI throughout its evolution: to standardize protocols and analyses, and to facilitate open access to comparable, worldwide data. 3
3.1. Argentina ADNI
A Buenos Aires team has carried out the ADNI‐2 protocol 3 in 56 participants under its own financial support. The team has ended ADNI follow‐up visits and is now focused on data analysis. Several findings have been described. 3 , 32 Participant retention was strong for the 12‐ and 30‐month study visits (50 and 43 participants completed each, respectively). Of the initial cohort, 26 participants completed the final 60‐month follow‐up MRI and neuropsychiatric assessments (4 participants passed away).
Argentina ADNI researchers investigated biomarker profiles for all participants. 33 , 34 At baseline, 85% of the participants in the AD group were positive on amyloid PET scans, for CSF p‐tau, and for neurodegeneration. Whereas in the MCI group, this dropped to 50% for suspected non‐Alzheimer's pathophysiology participants who were only positive for neurodegeneration at baseline. After 5 years of follow‐up, the overall conversion rate to dementia was 21%. Cognitive testing data significantly correlated with CSF amyloid levels in participants 35 ; however, total CSF tau and p‐tau were the strongest conversion predictors. 34 , 36 The researchers have described the capacity of several biomarkers to predict cognitive impairment. 37 , 38 Notably, Argentina ADNI is the first group in Latin America to perform tau PET scans (23 performed to date).
3.2. Canada ADNI
Canada ADNI is conducting a multisite amyloid and (18)F‐fluorodeoxyglucose positron emission tomography (18F‐FDG‐PET) imaging study in 80 AD and vascular patients with severe periventricular white matter disease. Eighty ADNI‐2 participants with minimal periventricular white matter hyperintensity (WMH) provide a comparator group. The study aims to understand the additive or interactive effects of small vessel disease and AD.
At baseline and 24 months, study participants completed 3T MRI, 18F‐florbetapir, and 18F‐FDG‐PET scans, blood draws, and gait and cognitive testing. Preliminary analyses compare 57 participants with moderate to severe pvWMH to 57 ADNI‐2 MCI or AD participants with minimal pvWMH. Overall, higher pvWMH was associated with elevated brain amyloid burden by PET scan. Participants with minimal pvWMH had lower brain glucose levels. 39 Random forest machine‐learning algorithms pinpointed several brain regions associated with cognitive ability, most strikingly, the posterior cingulate gyrus. Lower amyloid burden and increased glucose in this region was associated with higher cognitive test scores. 40 Methods developed by Canada ADNI suggest that simple machine learning can help classify regions of interest in PET scans.
3.3. China ADNI
China ADNI includes several cores: Clinical, MRI, PET, Pathological, Biomarker and Genetics, Biostatistics and Informatics, and Neuropsychological. China ADNI also has a dedicated Data Storage and Processing site. Since joining WW‐ADNI in 2012, China ADNI has investigated the role of traditional Chinese medicine in AD progression.
Foundational fMRI work by China ADNI confirmed that acupuncture at two dorsal Siguan points (Tai chong on the right foot, and Hegu on the right hand) 41 activates brain regions associated with cognition in people with MCI or AD. 42 Neuroimaging shows that acupuncture at these locations improves blood perfusion, default mode network activity, 43 and hippocampal connectivity 44 , 45 in AD. A randomized, controlled trial by China ADNI found that 6 months of consistent acupuncture treatment delayed MCI disease progression. This study compared fMRI from 50 cognitively unimpaired participants to 28 with amnestic MCI. 46
China ADNI is now launching a larger, randomized controlled trial to further study Siguan acupoints and MCI progression. The study includes measurements of amyloid and tau in blood and/or CSF, a cognitive testing battery, as well as MRI and 18F‐FDG‐PET in accordance with ADNI protocols. China ADNI intends to enroll 400 amnestic MCI participants across 20 hospitals. Half of participants will receive the acupuncture intervention.
3.4. Japan ADNI
Japan ADNI launched in 2007 3 and has enrolled 537 of a targeted 600 participants in a longitudinal, observational study akin to ADNI‐1. Participants at 38 study sites have completed blood and APOE genotyping and 37% have provided a CSF sample. For neuroimaging, 37% and 63% of participants have completed 11C‐PiB and 18F‐FDG PET imaging, respectively. Japan ADNI data harmonize with North American ADNI study sites. 47 Combined analyses revealed the APOE ε4–positive and –negative participants with late MCI or mild AD experienced cognitive decline at the same speed. 48 Japan ADNI‐2, a small preclinical AD study, completed in March 2020, enrolled 28 cognitively unimpaired and 12 MCI participants. The study includes tau PET subanalyses; 15 flortaucipir scans have been completed to date.
Data collected by Japan ADNI have been released for worldwide research use (https://humandbs.biosciencedbc.jp/en/data‐use). These includes 2715 MRI and 1981 PET images, all biofluid data, as well as case report forms and cognitive testing results for cognitively unimpaired, MCI, and AD participants.
To aid recruitment, research volunteers for preclinical AD studies participate in a web‐based study (J‐TRC webstudy) to provide basic demographics, clinical histories, and complete cognitive tests. Nearly 4500 have registered. Eligible participants are then invited to a clinic to provide blood samples, undergo florbetapir or flutemetamol amyloid PET, and complete cognitive tests including PACC (J‐TRC onsite study). As a last step, risk assessment algorithms select participants most appropriate for treatment trials. This process creates a rich data set even before study enrollment. 49
3.5. Taiwan ADNI
Taiwan ADNI has five cores: Clinical, PET, MRI, Biomarkers and Genetics, and Biostatistics and Informatics. The first stage of Taiwan ADNI was similar to ADNI‐1 and completed in 2019. Six hospitals participated. Nine sites have joined stage 2 of Taiwan ADNI, which is already underway and adds a Tau Imaging core to the framework. The second stage aims to establish a longitudinal AD cohort. Beyond neuroimaging and biofluid assessments, stage 2 adds behavior, depression, diet, and sleep assessments. Neuroimaging will be assessed, in part, using deep learning algorithms. Stage 2 also includes extensive measures of early onset dementia genes. To date, Taiwan ADNI has enrolled 137 participants in stage 2.
Taiwan ADNI infrastructure has enabled researchers to assess changes in amyloid deposition due to carotid artery stenosis 50 and traumatic brain injury. 51 It has also supported PET imaging to better understand how D678H, a familial autosomal mutation common in Taiwan, may increase AD risk. 52 Similarly, Taiwan ADNI researchers have investigated how late‐life depression increases amyloid burden and MCI risk in a Taiwanese population. 53
Taiwan ADNI has employed a pre‐screening tool for use prior to selecting participants for PET scans. The tool, a simple decision tree coupled with APOE genotyping and amyloid plasma measurements, successfully predicts amyloid PET findings in MCI participants. 54 This tool could be used by other sites and in clinical trials to avoid unnecessary PET scans.
3.6. Mexico ADNI
Mexico ADNI is based in the National Institute of Neurology and Neurosurgery of Mexico. With >90,000 consultations at this site annually, there is a strong clinical demand for neuroimaging studies. The group has forged international collaborations and independently implemented ADNI‐3–compatible protocols for 3T MRI scans. In parallel, they are completing an analysis of MRI data from 70 original studies.
Several collaborations connect Mexico ADNI to the broader AD research community. Mexico ADNI is enrolling 270 participants across several consortium studies: LatAm Fingers, Dominantly Inherited Alzheimer Network (DIAN), DIAN‐trials unit, and ReDLat. All of these studies are supported by the Alzheimer's Association and follow North American ADNI protocols.
3.7. Australia ADNI
The Australian Imaging Biomarkers and Lifestyle Study of Aging (AIBL) has been the major focus of Australia ADNI for the past 14 years. The study has enrolled 2691 participants stratified by PET Centiloid level, a technique standardized by Australian and North American ADNI researchers to quantify amyloid burden. 55 This imaging biomarker identifies participants at highest risk for AD. For example, cognitively normal AIBL participants with >100 Centiloid level at baseline experienced a 50% conversion rate to prodromal AD within 5 years. 56 The first 6 years of AIBL data are available through the North American ADNI centralized database.
Preliminary analyses of AIBL tau PET MK6240 scans are underway and suggest a 0.5% per year tau increase in cognitively normal amyloid PET‐positive participants, but a 2% to 7% annual increase in AD. 56 Through international collaboration, AIBL is investigating binding of an F‐18–labeled tracer to MAO‐B, to assess reactive astrocytosis during the development of AD. 57 Australia ADNI has collaborated with industry partners to ramp up production of tau MK6240 and amyloid NAV4694 tracers at five production sites to accommodate growing research needs.
4. SUMMARY
WW‐ADNI has made major strides in amyloid and tau phenotyping, standardizing methodologies, and providing a rich data set for AD researchers around the globe. The group's efforts serve as a foundation for AD treatment trials. WW‐ADNI findings can inform participant selection criteria and deeply enhance outcome measures.
As WW‐ADNI continues, a major goal will be to validate biomarkers identified to date, with focus on their generalizability and relationships to cognitive decline and dementia symptoms. A goal shared by all WW‐ADNI researchers is to enroll more racial and ethnic minorities. To accomplish this, ADNI‐4 may relax exclusion criteria related to comorbidities across cognitively unimpaired, MCI, and AD cohorts. This may include allowing participants previously exposed to disease‐modifying treatments. Specific inclusion criteria changes will be made in collaboration with the PPSB. ADNI‐4 will also allow release of amyloid PET results to participants. This modification is based upon feedback from current study participants and is expected to further support recruitment efforts. ADNI‐4 will include a plasma‐based screening effort that selects eligible participants for imaging and CSF collection. ADNI‐4 is also expected to scale up autopsy neuropathology data collection. If funded, ADNI‐4 is expected to begin in August 2022.
FUNDING INFORMATION
CCC's WW‐ADNI project is sponsored by Chang Gung Memorial Hospital, CMRPG 8J0522. AJS receives support from multiple NIH grants related to analysis of ADNI data (P30 AG010133, R01 AG019771, R01 AG057739, U01 AG024904, R01 LM013463, R01 AG068193, and U01 AG068057). The National Centralized Repository for Alzheimer's Disease and Related Dementias (NCRAD) provides support for ADNI Genetics Core Biobanking and is supported by the NIH (U24 AG021886). CCR has received funding from the National Health and Medical Research Council of Australia. SEB has received funding from the Canadian Institutes of Health Research Foundation Grant (#159910, #142381, and #112246) and the LC Campbell Foundation. LMS has Grant support for AD biomarker studies in CSF and plasma: ADNI3 grant, Biomarker Core, U19AG024904; UPenn ADRC P30AG010124; and MJFox Foundation for Parkinson's Research, grant #005441.
CONFLICTS OF INTEREST
WJ has served as a consultant to Bioclinica, Biogen, CuraSen, Grifols, and Roche/Genentech. CRJ serves on an independent data monitoring board for Roche, has served as a speaker for Eisai, and consulted for Biogen, but he receives no personal compensation from any commercial entity. He receives research support from NIH, the GHR Foundation, and the Alexander Family Alzheimer's Disease Research Professorship of the Mayo Clinic. AJS and the Indiana University ADRC receives in‐kind PET precursor support from Avid Radiopharmaceuticals, a subsidiary of Eli Lilly. CS is a full‐time employee of Merck and Co., Inc. and owns shares in the company. CCR has received institutional research grants from Cerveau Technologies, Biogen, Eisai, Abbvie, Roche, and Janssen, and is also participating in Scientific Advisory Boards for Cerveau Technologies and Biogen Australia. LMS is supported by the NIA ADNI‐3 grant for which he provides QC oversight for CSF analyses using the Roche Elecsys automated platform and reagents, and has also received IIS grant support for AD biomarker studies from Roche.
ACKNOWLEDGMENTS
Elecsys is a registered trademark of Roche.
Weber CJ, Carrillo MC, Jagust W, et al. The Worldwide Alzheimer's Disease Neuroimaging Initiative: ADNI‐3 updates and global perspectives. Alzheimer's Dement. 2021;7:e12226. 10.1002/trc2.12226
REFERENCES
- 1. Weiner MW, Veitch DP, Aisen PS, Beckett LA, Cairns NJ, Green RC. The Alzheimer's disease neuroimaging initiative: a review of papers published since its inception. Alzheimers Dement. 2013;9(5):e111–e194. 10.1016/j.jalz.2013.05.1769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mueller SG, Weiner MW, Thal LJ, et al. The Alzheimer's disease neuroimaging initiative. Neuroimaging Clin N Am. 2005;15:869–877. 10.1016/j.nic.2005.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mueller SG, Weiner MW, Thal LJ, et al. Ways toward an early diagnosis in Alzheimer's disease: the Alzheimer's disease neuroimaging initiative. Cognition Dement. 2006;5:56–62. 10.1016/j.jalz.2005.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weiner MW, Aisen PS, Jack CR, et al. The Alzheimer's disease neuroimaging initiative: progress report and future plans. Alzheimers Dement. 2010;6(3):202–211. 10.1016/j.jalz.2010.03.007. e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jack CR Jr, Bernstein MA, Borowski BJ, et al. Update on the magnetic resonance imaging core of the Alzheimer's disease neuroimaging initiative. Alzheimers Dement. 2010;6(3):212–220. 10.1016/j.jalz.2010.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu E, Luthman J, Cedarbaum JM, Schmidt ME, Cole PE, Hendrix J. Perspective: the Alzheimer's disease neuroimaging initiative and the role and contributions of the private partner scientific board (PPSB). Alzheimers Dement. 2015;11:840–849. 10.1016/j.jalz.2015.04.001 [DOI] [PubMed] [Google Scholar]
- 7. Veitch DP, Weiner MW, Aisen PS, et al. Understanding disease progression and improving Alzheimer's disease clinical trials: recent highlights from the Alzheimer's disease neuroimaging initiative. Alzheimers Dement. 2019;15(1):106–152. 10.1016/j.jalz.2018.08.005 [DOI] [PubMed] [Google Scholar]
- 8. Schmidt ME, Chiao P, Klein G, et al. The influence of biological and technical factors on quantitative analysis of amyloid PET: points to consider and recommendations for controlling variability in longitudinal data. Alzheimers Demen. 2015;11(9):1050–1068. 10.1016/j.jalz.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 9. Tosun D, Landau S, Aisen PS, et al. Association between tau deposition and antecedent amyloid‐β accumulation rates in normal and early symptomatic individuals. Brain. 2017;140(5):1499–1512. 10.1093/brain/awx046 [DOI] [PubMed] [Google Scholar]
- 10. Jack CR Jr, Bennett DA, Blennow K, et al. NIA‐AA Research Framework: toward a biological definition of Alzheimer's disease. Alzheimers Dement. 2018;14(4):535–562. 10.1016/j.jalz.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guo T, Korman D, Baker SL, Landau SM, Jagust WJ. Alzheimer's disease neuroimaging initiative. longitudinal cognitive and biomarker measurements support a unidirectional pathway in Alzheimer's disease pathophysiology. Biol Psychiatry. 2020. 10.1016/j.biopsych.2020.06.029. S0006‐3223(20)31739‐X. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jack CR Jr, Barnes J, Bernstein MA, et al. Magnetic resonance imaging in Alzheimer's neuroimaging initiative 2. Alzheimers Dement. 2015;11(7):740–756. 10.1016/j.jalz.2015.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sten JL, Medland SE, Arias Vasquez A, et al. Identification of common variants associated with human hippocampal and intracranial volumes. Nat Genet. 2012;44(5):552–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics. 2007;8(1):118–127. 10.1093/biostatistics/kxj037 [DOI] [PubMed] [Google Scholar]
- 15. Moyer D, Ver Steeg G, Tax Chantal MW, Thompson PM. Scanner invariant representations for diffusion MRI harmonization. Magn Reson Med. 2020;84(4):2174–2189. 10.1002/mrm.28243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schwarz CG, Kremers WK, Therneau TM, et al. Identification of anonymous MRI research participants with face‐recognition software. N Engl J Med. 2019;381(17):1684–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paltoo DN, Lyman Rodriguez L, Feolo M, et al. Data use under the NIH GWAS data sharing policy and future directions. Nat Genet. 2014;46(9):934–938. 10.1038/ng.3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kang J‐H, Korecka M, Figurski MJ, et al. The Alzheimer's disease neuroimaging initiative 2 biomarker core: a review of progress and plans. Alzheimers Dement. 2015;11(7):772–791. 10.1016/j.jalz.2015.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. O'Bryant S, Gupta V, Henriksen K, et al. Guidelines for the standardization of preanalytic variables for blood‐based biomarker studies in Alzheimer's disease research. Alzheimers Dement. 2015;11(5):549–560. 10.1016/j.jalz.2014.08.099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Korecka M, Figurski MJ, Landau SM, et al. Analytical and clinical performance of amyloid‐beta peptides measurements in CSF of ADNIGO/2 participants by an LC‐MS/MS reference method. Clin Chem. 2020 Apr 1;66(4):587–597. 10.1093/clinchem/hvaa012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Spellman DS, Wildsmith KR, Honigberg LA, et al. Development and evaluation of a multiplexed mass spectrometry based assay for measuring candidate peptide biomarkers in Alzheimer's disease neuroimaging initiative (ADNI) CSF. Proteomics Clin Appl. 2015;9(7‐8):715–731. 10.1002/prca.201400178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Libiger O, Shaw LM, Watson MH, et al. Longitudinal CSF proteomics identifies NPTX2 as a prognostic biomarker of Alzheimer's disease. Alzheimers Dement. 2021. 10.1002/alz.12353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ewers M, Biechele G, Suárez‐Calvet M, et al. Higher CSF sTREM2 and microglia activation are associated with slower rates of beta‐amyloid accumulation. EMBO Mol Med. 2020;12(9):e12308. 10.15252/emmm.202012308. Epub 2020 Aug 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Portelius E, Zetterberg H, Skillbäck T, et al. Cerebrospinal fluid neurogranin: relation to cognition and neurodegeneration in Alzheimer's disease. Brain. 2015;138(Pt 11):3373–3385. 10.1093/brain/awv267. Epub 2015 Sep 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Apostolova LG, Risacher SL, Duran T, et al. Associations of the top 20 Alzheimer disease risk variants with brain amyloidosis. JAMA Neurol. 2018;75(3):328–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Raghavan NS, Dumitrescu L, Mormino E, et al. Association between common variants in RBFOX1, an RNA‐binding protein, and brain amyloidosis in early and preclinical Alzheimer disease. JAMA Neurol. 2020;77(10):1–11. 10.1001/jamaneurol.2020.1760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hibar DP, Adams Hieab HH, Jahanshad N, et al. Novel genetic loci associated with hippocampal volume. Nat Commun. 2017;8:13624. 10.1038/ncomms13624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nho K, Nudelman K, Allen M, et al. Genome‐wide transcriptome analysis identifies novel dysregulated genes implicated in Alzheimer's pathology. Alzheimers Dement. 2020;16(9):1213–1223. 10.1002/alz.12092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vasanthakumar A, Davis JW, Idler K, et al. Harnessing peripheral DNA methylation differences in the Alzheimer's disease neuroimaging initiative (ADNI) to reveal novel biomarkers of disease. Clin Epigenetics. 2020;12(1):84. 10.1186/s13148-020-00864-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Arnold M, Nho K, Kueider‐Paisley A, et al. Sex and APOE ε4 genotype modify the Alzheimer's disease serum metabolome. Nat Commun. 2020;11(1):1148. 10.1038/s41467-020-14959-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Donohue MC, Sethuraman G, Langford O, et al. Alternatives to MMRM for preclinical Alzheimer's clinical trials. [Conference presentation]. 2020.JSM 2020 Virtual Conference, online. https://ww2.amstat.org/meetings/jsm/2020/OnlineProgram/AbstractDetails.cfm?abstractid=312809
- 32. Allegri RF, Chrem Méndez P, Calandri I, et al. Prognostic value of ATN Alzheimer's biomarkers: 60‐month follow‐up results from the Argentine Alzheimer's disease neuroimaging initiative. Alzheimers Dement (Amst). 2020;12(1):e12026. 10.1002/dad2.12026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chrem Méndez P, Calandri I, Nahas F, et al. Argentina‐Alzheimer's disease neuroimaging initiative (Arg‐ADNI): neuropsychological evolution profile after one‐year follow up. Arq Neuropsiquiatr. 2018;76(4):231–240. 10.1590/0004-282x20180025 [DOI] [PubMed] [Google Scholar]
- 34. Florencia Clarens M, Crivelli L, Calandri I, et al. Neuropsychological profile of Alzheimer's disease based on amyloid biomarker findings results from a South American cohort. Appl Neuropsychol Adult. 2020: 1–6. 10.1080/23279095.2020.1756816 [DOI] [PubMed] [Google Scholar]
- 35. Harris P, Fernandez Suarez M, Surace EI, Chrem Méndez P, Eugenia Martín M, Florencia Clarens M. Cognitive reserve and Aβ1‐42 in mild cognitive impairment (Argentina‐Alzheimer's disease neuroimaging initiative). Neuropsychiatr Dis Treat. 2015;11:2599–2604. 10.2147/NDT.S84292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Allegri RF, Pertierra L, Cohen G, et al. A biological classification for Alzheimer's disease ‐ Amyloid, tau and neurodegeneration (A/T/N): results from the Argentine‐Alzheimer's disease neuroimaging initiative. Int Psychogeriatr. 2019;31(12):1837–1838. 10.1017/S1041610219000085 [DOI] [PubMed] [Google Scholar]
- 37. Chrem Méndez P, Gabriela C, Maria Julieta R, et al. Concordance between 11C‐PIB‐PET and clinical diagnosis in a memory clinic. Am J Alzheimers Dis Other Demen. 2015;30(6):599–606. 10.1177/1533317515576387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Julieta Russo M, Cohen G, Chrem Méndez P, et al. Predicting episodic memory performance using different biomarkers: results from Argentina‐Alzheimer's disease neuroimaging initiative. Neuropsychiatr Dis Treat. 2016;12:2199–2206. 10.2147/NDT.S107051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zukotynski K, Gaudet V, Kuo PH, et al. The use of random forests to identify brain regions on amyloid and FDG PET associated with MOCA score. Clin Nucl Med. 2020;45(6):427–433. 10.1097/RLU.0000000000003043 [DOI] [PubMed] [Google Scholar]
- 40. Zukotynski K, Gaudet V, Kua PH, et al. The use of random forests to classify amyloid brain PET. Clin Nucl Med. 2019;44(10):784–788. 10.1097/RLU.0000000000002747 [DOI] [PubMed] [Google Scholar]
- 41. Shan Y, Wang Z, Zhao Z, et al. An fMRI study of neuronal specificity in acupuncture: the multiacupoint siguan and its sham point. Evid Based Complement Alternat Med. 2014;2014:103491. 10.1155/2014/103491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang Z, Nie B, Li D, et al. Effect of acupuncture in mild cognitive impairment and Alzheimer's disease: a functional MRI study. PLoS One. 2012;7(8):e42730. 10.1371/journal.pone.0042730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liang P, Wang Z, Qian T, Li K. Acupuncture stimulation of Taichong (Liv3) and Hegu (LI4) modulates the default mode network activity in Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2014;29(8):739–748. 10.1177/1533317514536600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wang Z, Liang P, Zhao Z, et al. Acupuncture modulates resting state hippocampal functional connectivity in Alzheimer's disease. PLoS One. 2014;9(3):e91160. 10.1371/journal.pone.0091160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zheng W, Su Z, Liu X, et al. Modulation of functional activity and connectivity by acupuncture in patients with Alzheimer's disease as measured by resting‐state fMRI. PLoS One. 2018;13(5):e0196933. 10.1371/journal.pone.0196933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Li H, Wang Z, Yu H, et al. The long‐term effects of acupuncture on hippocampal functional connectivity in amci with hippocampal atrophy: a randomized longitudinal fMRI study. Neural Plasticity. 2020;2020:6389368. 10.1155/2020/6389368 [DOI] [Google Scholar]
- 47. Iwatsubo T, Iwata A, Suzuki K, et al. Japanese and North American Alzheimer's Disease Neuroimaging Initiative studies: harmonization for international trials. Alzheimers Dement. 2018;14(8):1077–1087. 10.1016/j.jalz.2018.03.009 [DOI] [PubMed] [Google Scholar]
- 48. Suzuki K, Hirakawa A, Ihara R, et al. Effect of apolipoprotein E ε4 allele on the progression of cognitive decline in the early stage of Alzheimer's disease. Alzheimers Dement (N Y). 2020;6(1):e12007. 10.1002/trc2.12007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sato K, Ihara R, Suzuki K, et al. Predicting amyloid risk by machine learning algorithms based on the A4 screen data: application to the Japanese Trial‐Ready Cohort study. Alzheimers Dement: Translat Res Clin Interven. 2021;7(1):e12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Huang K‐L, Lin K‐J, Ho M‐Y, et al. Amyloid deposition after cerebral hypoperfusion: evidenced on [(18)F]AV‐45 positron emission tomography. J Neurol Sci. 2012;319(1‐2):124–129. 10.1016/j.jns.2012.04.014 [DOI] [PubMed] [Google Scholar]
- 51. Yang S‐T, Hsiao I‐T, Hsieh C‐J, et al. Accumulation of amyloid in cognitive impairment after mild traumatic brain injury. J Neurol Sci. 2015;349(1‐2):99–104. 10.1016/j.jns.2014.12.032 [DOI] [PubMed] [Google Scholar]
- 52. Huang C‐Y, Hsiao I‐T, Lin K‐J, et al. Amyloid PET pattern with dementia and amyloid angiopathy in Taiwan familial AD with D678H APP mutation. J Neurol Sci. 2019;398:107–116. 10.1016/j.jns.2018.12.039 [DOI] [PubMed] [Google Scholar]
- 53. Wu K‐Y, Lin K‐J, Chen C‐H, et al. Diversity of neurodegenerative pathophysiology in nondemented patients with major depressive disorder: evidence of cerebral amyloidosis and hippocampal atrophy. Brain Behav. 2018;8(7):e01016. 10.1002/brb3.1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lin S‐Y, Lin K‐J, Lin P‐C, et al. Plasma amyloid assay as a pre‐screening tool for amyloid positron emission tomography imaging in early stage Alzheimer's disease. Alzheimers Res Ther. 2019;11(1):111. 10.1186/s13195-019-0566-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Klunk WE, Koeppe RA, Price JC, et al. The Centiloid Project: standardizing quantitative amyloid plaque estimation by PET. Alzheimer's Dement. 2015;11(1):1–15. 10.1016/j.jalz.2014.07.003. e1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. van der Kall LM, Truong T, Burnham SC, et al. Association of β‐Amyloid level, clinical progression and longitudinal cognitive change in normal older individuals. Neurology. 2020;96(5):e662‐e670. 10.1212/WNL.0000000000011222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Villemagne V, Doré V, Okamura N, et al. To tau or to MAO‐B? Most of the 18F‐THK5351 signal is blocked by selegiline. J Nucl Med. 2018;59(1):1644.30166356 [Google Scholar]


