Supplemental digital content is available in the text.
Key Words: second victim, acute care, burnout, adverse event, posttraumatic stress, patient safety, medical error
Abstract
Objectives
Health care providers that experience harm after adverse events have been termed “second victims.” Our objective was to characterize the range and context of interventions to support second victims in acute care settings.
Methods
We performed a scoping study using Arksey and O’Malley’s process. A library scientist searched PubMed, Cumulative Index of Nursing and Allied Health, EMBASE, and Cochrane Central Register of Controlled Trials in September 2017, and updated the search in November 2018. We sought gray literature (Canadian Electronic Library, Proquest and Scopus) and searched reference lists of included studies. Stakeholder organizations and authors of included studies were contacted. Two reviewers independently reviewed titles and abstracts and extracted data. A qualitative approach was used to categorize the context and characteristics of the 22 identified interventions.
Results
After screening 5634 titles and abstracts, 173 articles underwent full-text screening. Twenty-two interventions met the criteria and were categorized as providing peer support (n = 8), proactive education (n = 6), or both (n = 8). Programs came from Canada (n = 2), Spain (n = 2), and the United States (n = 18). A specific traumatic event triggered the development of 5 programs. Some programs used a standard definition of second victims, (n = 6), whereas other programs had a broader scope (n = 12). Confidentiality was explicitly assured in 9 peer support programs. Outcome measures were often not reported.
Conclusions
This is a new area of study with little qualitative data from which to determine whether these programs are effective. Many programs had a similar design, based on the structure proposed by the same small group of experts in this new field. Concerns about potential legal proceedings hinder documentation and study of program effectiveness.
Adverse events occur in 7.5 per 100 adult hospital admissions in Canada and in 9.2 per 100 pediatric admissions.1,2 Patients are the first priority after an adverse event.3 The concept of harm to health care providers (HCPs) as a result of adverse events is newer. Since 2000, HCPs who have experienced an adverse event have been termed “second victims.”4
At least half of HCPs will experience the second victim phenomenon in their career.5 In a physician cohort, Waterman et al6 reported increased anxiety, loss of confidence, sleeping difficulties, reduced job satisfaction, harm to reputation, and depression or posttraumatic stress disorder, with 90% of respondents indicating that health care organizations provided inadequate support to clinicians coping with medical errors. Scott et al7 found that 30% of clinicians reported concerns about job performance in the preceding 12 months as a result of a patient safety event and 15% of these respondents reported they seriously considered leaving their profession. In addition to compromising patient satisfaction and safety, the fallout for second victims also leads to decreases in staff retention and productivity.8,9
Previous systematic reviews have clarified the definition, prevalence, impact, and coping strategies used by second victims.5,10,11 There is a gap in the literature in terms of synthesizing the organizational policies and interventions used to support these HCPs. Although an existing systematic review examined support for nurses as second victims, it excluded quantitative evidence.12 Our objective was to characterize the range and context of interventions used to support second victims of any health profession in acute care settings and report the intervention outcomes for HCPs and the organization as a whole.
METHODS
Scoping studies are useful for assessing a broad topic addressed by heterogeneous sources to map key ideas, identify the sources and types of evidence from which ideas arise, and illuminate gaps in empirical evidence.13 We performed our scoping study using the Arksey and O’Malley14 framework. The protocol was reviewed by the Scientific Review Committee at the IWK Health Centre.
An information specialist (R.P.) developed searches in PubMed (1946 to November 2018), EMBASE via Elsevier (1947 to September 2017), the Cumulative Index of Nursing and Allied Health via EBSCOHost (1971 to September 2017), PsycINFO via EBSCOHost (1597 to September 2017), the Cochrane Central Register of Controlled Trials via Cochrane Library (Issue 9, Sept 2017), and Web of Science Core Collection via Clarivate Analytics (1900 to September 2017).
Search concepts included second victims or HCPs impacted by adverse events and acute care settings. Terms to describe second victims were compiled based on discussions with the review team and consulting a previous systematic review.5 The second victim concept was expanded to include variant index and text word terms and combinations to capture the different ways to describe burnout, depression, and other psychological impacts of medical errors or patient safety events on HCPs. Index terms and synonym text word terms were similarly identified for the acute care setting concept. Truncation and adjacency operators were used as appropriate depending on the term and the database. All databases were searched up to September 2017, and because of being the primary source for included studies, the search was updated for PubMed to retrieve results up to November 2018. In addition to the comprehensive searches restricted to acute care settings, following the methods of Arksey and O’Malley,14 iterative supplemental searches were conducted in PubMed to capture the impact of adverse events or medical errors on HCPs. See Appendix A (Supplemental Digital Content 1, http://links.lww.com/JPS/A309) for complete search strategies used in each database.
Citations resulting from the searches were imported into RefWorks (ProQuest, Bethesda, Maryland) and duplicate citations were removed before migrating the results into Covidence (Veritas Health Innovation, Melbourne, Australia), a systematic review management software, for screening.
Two reviewers independently reviewed all titles, abstracts, and websites using the following inclusion criteria:
Methods: qualitative, quantitative, mixed methods, and descriptive reports
Organizational interventions to support HCPs after an adverse event
Population: HCPs in a single discipline or multidisciplinary
Context: acute care settings
Languages: not restricted
Date: published during or since 2000§
Acute care is defined in a World Health Organization Bulletin as “all promotive, preventive, curative, rehabilitative or palliative actions, whether oriented towards individuals or populations, whose primary purpose is to improve health and whose effectiveness largely depends on time-sensitive and, frequently, rapid intervention.”15 Acute care domains include prehospital care, emergency care, critical care, trauma care and acute care surgery, urgent care, and short-term stabilization.
Titles and abstracts that seemed relevant based on the criteria listed previously were selected for full text review. Two reviewers independently reviewed the full-text articles to determine whether they fit within the inclusion criteria. Discrepancies between reviewers were resolved through consensus.
During full-text screening, the text and reference lists of included articles were screened for mentions of second victim support programs that had not been captured by the original search (backward searching). We contacted authors of included studies to request further information on these programs.
In addition, relevant stakeholder institutions and organizations were contacted and asked about documentation relating to any second victim support programs of which they were aware, as well as additional contact information. See Appendix B (Supplemental Digital Content 2, http://links.lww.com/JPS/A310) for the full list of organizations contacted.
Using a data abstraction form, the 2 reviewers independently abstracted data from included studies. We had planned to meet after extracting data from the first 10 studies; however, given the total number of included studies, we elected to meet after reviewing the full list to resolve data discrepancies. No revisions in the data abstraction form were required.
Data were collated and summarized in a chart, and programs were analyzed for common themes and characteristics.
RESULTS
The literature search yielded 5542 results: 2696 from PubMed, 1361 from EMBASE, 763 from Cumulative Index of Nursing and Allied Health, 194 from PsycINFO, 79 from Cochrane Central Register of Controlled Trials, and 449 from Web of Science. Backward searching and contacting stakeholders resulted in additional sources for full-text screening (n = 5634). There were 4056 records after duplicates were removed. Figure 1 shows the flow diagram for the study.
FIGURE 1.
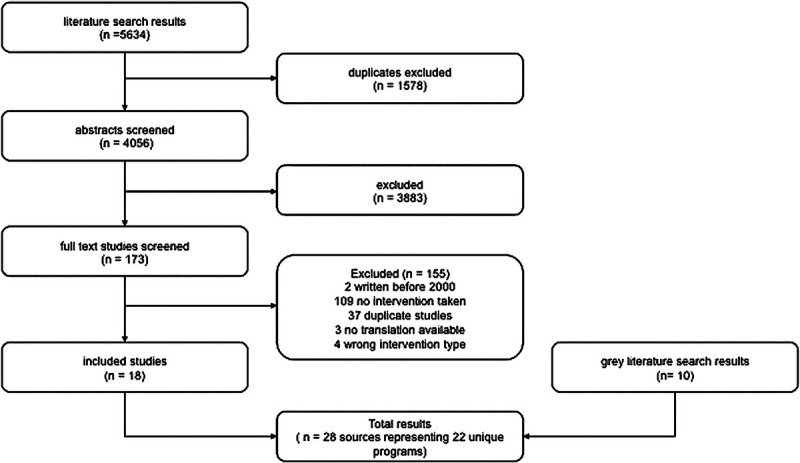
Process and results for data collection, screening, and selection. A literature search yielded a total of 5634 studies, from which 18 were included in this article. An additional 10 sources were obtained from a gray literature search.
After screening titles and abstracts, 173 articles were selected to undergo full-text screening. Full-text articles were excluded based on no intervention/strategy implemented (n = 94), duplicate study (n = 37), review of an original article/intervention (n = 15), published before 2000 (n = 2), English translation not available (n = 3), and wrong intervention (n = 4). Eighteen full-text articles met our inclusion criteria.7,8,16–31 Additional sources were identified through the gray literature search and included in data extraction.32–41 Included sources were published between 2008 and 2018 and described 22 unique organizational programs in Canada (n = 2), Spain (n = 2), and the United States (n = 18). See Table 1 for a summary of the included programs.
TABLE 1.
Summary of Included Programs
| Program Name | Reference Articles(s) | Location | Program Description | Outcome Measures |
|---|---|---|---|---|
| Code Lavender: Holistic Rapid Response | Johnson26 | Cleveland Clinic, Cleveland Ohio |
Provides emotional support to patients, family members, and hospital personnel (clinical and nonclinical) via an interdisciplinary rapid response team. Triggers include unexpected death, death or illness of staff or long-term patients. First response is within 30 min, with repeated check ins over the next 72 h. Services offered include massage, spiritual care, Reiki, Healing Touch, aromatherapy, and access to EAP. | Reported subjective perceived benefit |
| forYOU | Scott et al7 Scott38 Scott37 |
University of Missouri Health Care, Columbia, Missouri |
Rapid Response system available 24/7 to clinicians. Three-tiered model of support where tier 1 represents local or departmental support and response to promote identification and awareness of second victims. Tier 2 represents guidance and nurturing of identified second victims by specially trained peer supporters. Tier 3 represents access to professional services: chaplaincy, EAP, social work, and clinical health psychologists. | Reported Utilizations Statistics: 49 deployments in the first 10 mo. Average encounter lasting 30 min. Six team debriefings were held (average of 15 people lasting 77 min). Reasons for activations reported. Used the AHRQ-HSPOS survey 4 times. No statistical data comparing preimplementation and postimplementation. |
| Healing Beyond Today | Roesler et al31 | Methodist Hospital of Indiana, Indianapolis, Indiana, | The “Healing Beyond Today” program was launched to help transition those involved with return to work. It was a CISD-based program. Attendance was mandatory for all unit staff, and invitations were extended to ancillary personnel. Sessions were conducted offsite. | 5/6 HCPs retained their job at 1 y (1 had moved out of state). Some HCPs were resistant to attending the program and expressed feelings of ambivalence and frustrations stating that they had moved on and did not require support. |
| MITSS and the Peer Support Service (PSS) |
van Pelt8 Tobin42 |
Brigham and Women’s Hospital, Boston, Massachusetts | PSS is a rapid response model that is available to access 24 h a day, 7 d a week. The program is voluntary and separate from hospital quality assurance. There is no record keeping or documentation. Support is 1:1 and may be provided over the telephone. Referrals to the PSS may be made by the individual requiring the services, or by EAP, Risk Management, or colleagues. The program is not meant to replace formal counseling, and has a list of resources for those who require these services. MITSS also offers counseling, referrals, or telephone conversation to patients and their families. |
None reported |
| CISS Managers’ Toolkit |
Health PEI39 | Health PEI, Prince Edward Island, Canada | Toolkit outlining policies, articles, and checklists for managers responding to critical incidents. Information is listed as preincident or postincident (tier-based support). | None reported |
| RISE | Edrees et al24 Dukhanin et al22 |
Johns Hopkins Hospital, Baltimore, Maryland | Multidisciplinary team of peer supporters that can be activated through the paging system. It is available 24/7. The RISE team will page back within 30 min and arrange a meeting within the next 12 h. Group or individual support is possible. In this encounter, the RISE team member provides psychological first aid and provides a list of resources that may be helpful to the caller. All interactions are confidential. After the encounter, the peer supporter activates a debriefing, where the supporter receives support from other RISE members. |
119 calls involving 500 individuals were received in the first 52 mo. Most were from nurses, and only 4% concerned medical error. Peer responders completed self-evaluations as well as participation in a focus group. 88% of peer responders stated they had successful encounters in 88% of cases, and 83.3% of the time, they reported meeting their caller’s needs. Preprogram (2011) and postprogram (2014) surveys issued at 2011 and 2014. No significant difference in awareness of second victim phenomenon. In the post program survey more respondents perceived that organizational support was available to them (60% versus 41%), and that there was benefit to reaching out for support (94% versus 85%). 93% would recommend RISE to a colleague. |
| SWADDLE | Trent et al40 Baylor Scott & White Medical Center—Temple36 |
Baylor Scott & White Medical Center, Temple Texas | 1:1 ongoing peer support provided with psychological first aid, and referral to outside resources if needed. Based on the Scott 3-tiered model of staff support. Program provides prevention education for compassion fatigue, secondary traumatic stress, and burnout. Resilience Rounds are scheduled bi-monthly. It has both a didactic educational component, as well as a facilitated, confidential 20- to 30-min group discussion. |
None reported |
| USVIC | Bueno Domínguez et al27 | Grup SAGESSA, Tarragona, Spain | The support unit comprises a bioethicist, 2 nurses, a psychologist, and a lawyer. Provides psychological and medical support to second victims, as well as legal guidance. The unit can be activated through self-referral, or by colleagues or management. Once activated, a rapid response team will appear on scene as soon as possible. If required, more visits/telephone calls can be arranged. A root cause analysis is carried out simultaneously, and a report is made available to staff. | None reported |
| We Care | Gatzert et al43 We Care Team Family Brochure. Barnes Jewish Hospital, 2015 |
Barnes Jewish Hospital, St Louis, Missouri | Team members may proactively contact potential second victims, or may receive referrals from other HCPs via telephone or email. Debriefings may be individual or group-based. We Care Team is available 24 h a day, 7 d a week. We Care team meetings are scheduled monthly to discuss encounters and support other team members. All support is confidential and no personal or situational details are recorded. |
None reported |
| Clinician Peer Support Program | Lane et al28 | Barnes-Jewish Hospital and St. Louis Children’s Hospital | Clinicians can be referred by safety or risk management staff, peer support providers, or could self-nominate. Clinician PSP proactively contacts all physicians involved in a serious medical error or adverse event. Clinicians are matched with an available peer supporter with attempts made not to match them within the exact fields, or with those who may be in a supervisory role. Clinician PSP contacts them by email or telephone. Support is offered to the clinician, and if they decline, permission is asked to follow up in 1 week. Peer support providers debrief with a PSP director after contact with a clinician. The program conducts monthly program meetings or conference calls to share any lessons learned and program updates. |
No clinician-centered outcomes. Usage stats reported |
| YOU Matter | Krzan et l27 | Nationwide Children’s Hospital, Columbus, Ohio, | Coverage for the program is provided 24 h a day, 7 d a week. Interventions are based on the Scott 3-Tiered Model of Staff Support. Encounter forms can be accessed through SharePoint, and record only nonidentifiable data. This website also contains meeting minutes, lists of resources, and promotional materials. | Preimplementation and postimplementation surveys were conducted. 85% of those surveyed felt that the Department of Pharmacy had benefitted from the YOU Matter program. |
| CISMP of the First Nations and Inuit Health Branch | Lynch35 | First Nations and Inuit Health Branch | They have preventative and proactive education sessions. The CISM program is based on modified Mitchell Criteria and is managed by a national coordinator in Winnipeg with 2 assistant coordinators and 1.5 clerical assistants. They have access to a peer supporters and mental health professionals. Service is available 24/7 through coordinators “during working hours” and via telephone/EAP at nights and on weekends. The initial telephone call determines whether or not further intervention is required. They can bring the staff member out of the remote community for 2 sessions with the first-line provider, and up to 6 sessions over a 4-wk period with a second level provider. After this, if more support is required, they can be assessed by a psychologist. Treatment costs are covered by the program or through disability/worker’s comp. Group debriefings are rare. | Program was initiated in 1993. A follow-up survey in 1996 found 81% of respondents reported subjective benefit. 52% said without the services, they would have left their current job. 92% would use the service again, and 100% would recommend to others. |
| Provider Support Group | The Washington Patient Safety Coalition41 | The Everett Clinic, Everett, Washington |
HCPs are matched with physician mentors that have been involved in similar types of events to those that have recently experienced an adverse event/claim/lawsuit. Mentors meet monthly to address barriers. Postmentor/mentee surveys are distributed once the partnership has ended. Confidential |
None reported |
| After the Event: Care Provider Recovery Toolkit | The Washington Patient Safety Coalition41 | St Luke’s Health System, Boise, Idaho | The toolkit is a resource for managers to supplement the EAP and CISM teams after an adverse event. Toolkit includes slides, talking points, and videos. | None reported |
| Physicians Insurance Peer Support Program | The Washington Patient Safety Coalition41 | Physicians Insurance, Seattle, Washington | Program is administered by volunteer clinician members retained as consultants to the Claims Department. They contact members by telephone to offer short-term, confidential, emotional support and resources after an adverse event is reported to the Claims Department in anticipation of litigation. | None reported |
| Care for the Caregiver: Providence Peer Support Team | The Washington Patient Safety Coalition41 | Providence Everett Regional Medical Centre, Everett, Washington | A peer support program to support providers who are involved in an adverse event or “other difficult situation” | None reported |
| When Things Go Wrong | Bell et al16 | Beth Israel Deaconess Medical Centre, Harvard Medical School, Boston, Massachusetts, | Curriculum includes (1) baseline assessment of experiences, attitudes, and perceptions; (2) interactive curriculum using filmed patient narratives; and (3) implementation strategy for real-time disclosure. The curriculum was launched with separate tracks for staff physicians and residents. There is a 24-h pager number for support and communication after adverse events. |
100% of faculty physicians surveyed indicated that they felt better prepared to teach and address this topic. 79% of trainees and 92% of faculty physicians indicated that the session would affect their practice as clinicians. |
| Resident Wellness Curriculum | Arnold et al al18 | 2017 Resident Wellness Consensus Summit in Las Vegas, Nevada, | The curriculum includes a 2-module introduction to wellness; a 7-module “Self-Care Series” focusing on the appropriate structure of wellness activities and everyday necessities that promote physician wellness; a 2-module section on physician suicide and self-help; a 4-module “Clinical Care Series” focusing on delivering bad news, navigating difficult patient encounters, dealing with difficult consultants and staff members, and debriefing traumatic events in the emergency department; wellness in the workplace; and dealing with medical errors and shame. | None reported |
| Resident Educator Toolkit | Chung et al20 | 2017 Resident Wellness Consensus Summit in Las Vegas, Nevada, | Three educator toolkits were developed. The second victim syndrome toolkit has 4 modules, each with prereading material and a leader (educator) guide. In the mindfulness and meditation toolkit, there are 3 modules with a leader guide in addition to a longitudinal, guided meditation plan. The positive psychology toolkit has 2 modules, each with a leader guide and a PowerPoint slide set. These toolkits provide educators the necessary resources, reading materials, and lesson plans to implement didactic sessions in their residency curriculum. | None reported |
| Second Victim Curriculum for Nurse Anesthetists | Daniels and McCorkle21 | American Association of Nurse Anesthetists, Park Ridge, Illinois | Six basic domains including (1) define and describe second victim; (2) second victim risks for nurse anesthetists; (3) barriers for the second victim; (4) unintended consequences of the second victim; and (5) evidence-based understanding and interventions frameworks 6. Support systems |
None reported |
| MISE | Mira et al29 | Alicante-Sant Joan Health District, Alicante, Spain | The website was structured in 2 packages: demonstrative and informative. The informative package offered information on basic patient safety concepts including near misses, adverse events, and second victims. The demonstrative package included descriptions of the emotional consequences of adverse events as well as recommendations for actions after adverse events. This package had 15 videos to show what and what not to do in these situations. Information was also available through a mobile app. | Efficacy of the program was assessed with pretest and posttest. Users who finished MISE demonstrated knowledge of patient safety terminology, prevalence and impact of adverse events and clinical errors, second victim support models, and recommended actions after a severe adverse event (P < 0.001). There was no significant difference in the scores on the general knowledge test, or the demonstrative or informative test packages. The participants also completed an evaluation of MISE: HCPs rated the website 8.8/10. |
| Creating Debriefing Sessions for Perceived Medical Errors in Residency: A Step Towards Wellness | Choi et al19 | University of Illinois, Illinois, Chicago | Small groups of 9 residents and 2 facilitators (a staff and chief resident) who participate in facilitated discussions each month. Sessions were held on-campus, during noon hour, with protected time to attend. The goal of the sessions was to provide a safe space for discussion about perceived medical error, sharing coping strategies, and providing resources where necessary. |
Pre survey and postsurvey were completed. No results reported in the abstract. |
This table summarizes the names, locations, and descriptions of each program included in our scoping study, as well as outcome measures reported, where possible.
ARHQ-HSPOS, Agency for Healthcare Research and Quality Hospital Survey on Patient Safety Culture; CISD, Critical Incident Stress Debriefing; CISS, Critical Incident Staff Support; MISE, Mitigating Impact in Second Victims; PSP, Peer Support Program; USVIC, Unidad de Soporte a las Segundas Victimas del Incidente Critico.
Specific traumatic events were described as the trigger for development of 5 programs.8,18,24,31,41 Resilience in Stressful Events (RISE) was developed at Johns Hopkins Hospital after a significant adverse patient-related event involving a child in 2001.24 Healing Beyond Today was developed at Methodist Hospital of Indianapolis, where 5 infants received an overdose of heparin resulting in 3 deaths in September 2006.31 Medically Induced Trauma Support Services (MITSS) was developed after a 37-year-old woman had a cardiac arrest during an elective surgery due to accidental venous injection of bupivacaine at Brigham and Women’s Hospital in 1999.8 Care for the Caregiver: Providence Peer Support Team was triggered by a pediatric death related to a medication error where the supervising pharmacist was held responsible.41 The publication describing the resident wellness curriculum developed at a 2017 Consensus Summit communicated the death of a resident at the University of Kentucky from suicide.18
Seven programs cited a narrow definition of second victim.7,16,17,21,27,28,43 Twelve programs also extended their mandate beyond that definition to include the following: “stressful, patient-related events”24; difficult clinical outcomes or encounters27; “difficult life events”40; long-term patient death or death/illness of staff or their family26; targets of litigation or complaints40,41; violence against staff35; poor outcomes41; and self-care and wellness.18–20
All of the programs specifically supported HCPs. Code Lavender’s support was also extended to nonclinical staff.26 Three programs provided support for patients and families.26,31,42 Two programs provided support for families of affected HCPs.32,35,43
We identified 2 types of organizational interventions: peer support (n = 8)8,17,26,31,41,43 and proactive education programs (n = 6).16,18,20,21,29,41 Peer support programs included interventions whereby individuals or teams were activated in response to a specific event or a specific request for support. Proactive staff education included curricula, toolkits, and efforts to raise staff awareness about the concept of the second victim and/or coping strategies. Eight programs included both peer support and proactive staff education.7,19,24,27,28,35,39,40
Peer Support and Professional Support
Peer support was provided in a variety of models ranging from multiprofessional teams to volunteer peer supporters. Support provided by six programs was exclusively by peers,19,24,28,41 whereas 3 programs used professional staff to carry out support.17,35,42 Seven programs used a combination of both.7,26,27,31,39,40,43
Two of the programs were embedded within a Patient Safety Program24,41; 2 programs were part of a Quality Improvement Program19,41; 2 programs were associated with hospital-based Risk Management Programs40,41; 1 program was part of Occupational Health35; and 1 program was situated within the Office of Clinical Effectiveness.7 Five programs had paid staff,27,28,31,35,40 and 2 programs were exclusively volunteer based.41,43
Some programs are activated automatically in response to a specific event, some through self-referral and others by a referral from a colleague or administrator. The Clinician Peer Support Program is activated via multiple paths: a clinician can self-refer, be referred by a peer support provider, or be referred by patient safety or risk management staff.28 In the Physicians Insurance Peer Support Program, clinicians are contacted by clinician consultants who are trained by the Claims Department to provide support in anticipation of litigation.41 The RISE program can be triggered by a person involved in the event or a colleague.24 Debriefing Sessions for Perceived Medical Error in Residency was mandatory for residents as part of their educational curriculum and occurred at regular intervals irrespective of the occurrence of a specific adverse event.19
Most programs are offered for voluntary participation by second victims.7,8,17,24,26–28,35,40,41,43 Participation in Healing Beyond Today was mandatory for staff.31
Eleven programs specified that their services were provided confidentially.7,8,17,24,27,28,35,40,41,43 Four programs indicated that some level of documentation was completed: YOU Matter had a SharePoint portal where they documented interactions without identifying information27; Unidad de Soporte a las Segundas Victimas del Incidente Critico documented results of a root cause analysis where justified by the safety event17; WeCare documented interactions that lasted more than 30 minutes without recording personal or situational details43; and Critical Incident Stress Management Program (CISMP) of the First Nations and Inuit Health Branch documented the care provided.35 Most programs did not document anything and one program referred to it as “secret.”17
Eight of the programs mentioned in this article have their foundations in Critical Incident Stress Management (CISM), a technique primarily designed for first responders, to assist in coping with the psychological and physical responses to stressful events.7,8,24,27,31,35,40,43
Proactive Staff Education
Three programs described toolkits: 2 toolkits were targeted toward managers,39,41 and one toolkit was targeted toward educators.20 The manager-targeted toolkits listed resources to help managers support second victims in the workplace such as mental health first aid.39 The educator toolkit was developed by emergency physicians and listed reading materials, slide decks, and lesson plans.20
Four programs described specific curricula: a curriculum for nurse anesthetists,21 a curriculum for emergency medicine residents,18 a curriculum for medical educators and trainees,16 and Debriefing Sessions for Perceived Medical Error in Residency.19 The curricula for nurse anesthetists and emergency medicine residents described curricular content and how the content was derived. The curriculum for medical educators and trainees, “When things go wrong,” was based on a series of videos and vignettes that used real patient and family narratives, in addition to role play and exploratory questions.16 The basis for the curriculum in Debriefing Sessions for Perceived Medical Error in Residency was not explained.
One educational intervention was a website that described second victims, crisis communication, and disclosure.29 The website includes videos demonstrating these scenarios including how to support a second victim in emotional distress.
When educational interventions were bundled with peer support programs, they were largely targeted at promoting their peer support programs and raising awareness about the second victim phenomenon “to normalize the behaviour of seeking support after an adverse event.”28 For example, RISE used a website, promotional videos, internal publications, screen savers, presentations to targeted departments, and unit-level champions.24 YOU Matter and forYOU educated staff with the goal that all staff could identify and provide initial support to a second victim.7,27 This “basic awareness” training and emotional first aid formulated the basis for “tier 1” support. The educational mandate of Staff Wellbeing Assistance During Difficult Life Events (SWADDLE) and CISMP of the First Nations and Inuit Health Branch was broader than program awareness and tier 1 support.35,40 SWADDLE, for example, provided resilience-based education using seminars and “resilience rounds” to discuss compassion fatigue and mindfulness.40 Choi et al19 stated that their objectives were to recognize the personal impact of perceived errors, establish a safe discussion space, and cultivate healthy and adaptive coping strategies.
DISCUSSION
In this scoping review, we categorized programs as peer and professional support programs, or proactive staff education programs. However, even programs that were entirely focused on peer support required an educational component for implementation. The concept of HCPs as second victims is relatively new, and centers introducing the concept to their staff often cited lack of awareness, of both the concept and the local program, as implementation barriers. This suggests that educational approaches ought to be considered in designing implementation strategies for peer support programs.
Second victim research is a newer area of study, with a tight community of experts in the field. Although 22 different programs were included for analysis in this study, it is interesting to note that many programs were created with advice and oversight from the same panel of experts. This has led to a homogeneous approach to the design of peer support programs with few distinguishing features.
Seven programs specifically referred to Wu’s4 definition of a second victim. Other programs chose to broaden the mandate and support HCPs that were involved in any emotional or challenging event, whether it was related to an error or not. The term “second victim” has recently become more controversial. Some feel that the term causes organizations to avoid assigning responsibility for medical errors, and deemphasizes the effect these events have on patients. Because the term is not universally accepted, we chose to include not only programs that used Wu’s strict definition of a second victim, but also programs that supported HCPs impacted by other types of adverse patient events or outcomes. Some programs also included support for nonclinical staff, family members of CPs, and even patients and their families. Are the needs of second victims different from the needs of others who may be grieving? White et al44 suggested that programs that provide general support to employees in times of personal or work-related stress may not provide adequate support to second victims. For example, respondents from institutions with Employee Assistance Programs (EAP) only were less likely than those from programs with other support providers to report effective identification of health care workers in distress.44 In addition, support programs organized by the quality improvement or patient safety department, rather than an EAP, were associated with greater perceived efficacy.44 If the needs of a second victim are unique, do second victim support programs need to be unique as well?
Four programs were initiated in response to significant adverse events that occurred in a hospital. All programs that were reactionary to devastating adverse events were peer support programs rather than educational programs. This may suggest that those who had already experienced a significant adverse event did not see stand-alone educational programs as adequate.
Few programs published robust postimplementation outcome data and program evaluations. For proactive staff education or curriculum-based programs, it is difficult to determine how much lead time would be required to appropriately measure impact and retention of knowledge and skills. Although it seems intuitive that peer support programs would be beneficial, there is little evidence as to the benefit or harm of these programs for HCPs. Reported outcomes focused on the peer supporter perspective, largely in an effort to protect privacy and confidentiality around these sensitive events. Adverse events in hospitals have potential legal implications. For this reason, there is little to no documentation by peer support programs about triggering events. Second victim support programs could benefit from legal immunity similar to how “apology laws” have enhanced disclosure of adverse events to patients and their families.45
Critical Incident Stress Management is a technique initially designed to help first responders cope with stressful events and prevents. We identified 8 programs that used these principles.7,8,24,27,31,35,40,43 Recent literature reviews and meta-analyses suggest that reliving these traumatic events via CISM techniques may actually increase the rate of posttraumatic stress disorder in this population and cause more harm than benefit.46 If there is, at best, controversial and contradictory evidence to show that CISM provides benefit, outcome data are needed to assess the impact of the second victim support programs that were created using these principles.
This area of research needs robust outcome data. This community would benefit from establishing common nomenclature, definitions, and consistency in reporting outcome data.47 A consensus among this community of experts would facilitate building a body of evidence to evaluate these interventions at both the provider and organizational levels, as well as ensuring the feasibility of meta-analyses. Potential outcomes include the following: staff retention, staff sick time, occurrence of serious safety events, and workplace satisfaction. Preimplementation and postimplementation data would be helpful in institutions that are implementing new programs. The Second Victim Experience and Support Tool developed by Burlison et al48 is a survey designed to assess physical and mental signs and symptoms of second victims as well as the desirability or need for potential resources that could become available. It is intended to assess the adequacy of support for second victims and to be used to monitor progress when changes to the supports are made. Tools like the Second Victim Experience and Support Tool could provide a standard way to assess needs and monitor impact after implementation.
Second victim research is a relatively new area of study, with a small community of experts in the field. Although 22 different programs were included in our analysis, most of these were created with advice and oversight from the same experts, namely, Susan Scott, Albert Wu, Rick van Pelt, Linda Kenney, and Hanan Edrees. As a result, the pool of programs is relatively homogeneous. Our scoping review partly relied on forward and backward searching, and reaching out to known programs for information on other programs. This may introduce a degree of bias, in that it may identify programs that are similar in nature or from similar geographic or academic communities. This field of study is growing rapidly, and we expect that there are many other programs that have yet to be published or are in development. Some programs are likely advertised on organizational intranets and protected access domains, which would make them difficult to identify with our search strategies. Some documents we found were not academic in nature (e.g., a brochure) and did not report outcomes or development methodology. Including these studies enabled us to include a greater breadth of second victim support programs at the cost not being able to discuss or address the methodological quality.25
CONCLUSIONS
This is a new area of study with few reported outcomes. Scientific study has been hindered by concerns about confidentiality and protection of HCPs from legal consequences. As a result, there is little scientific rigor from which to determine whether these programs are indeed meeting their goals and objectives. Consensus about target audiences for organizational interventions and the triggers for activating peer support would facilitate aggregating results for broader program evaluation. Without the type of protection afforded by legislation in the patient safety domain, it will not be possible to report intervention outcomes for HCPs.
Supplementary Material
ACKNOWLEDGMENTS
We are grateful to the IWK Health Centre, who funded this study through a Category A Research Grant, and the Canadian Patient Safety Institute, who supported translating non-English articles from our search.
The rationale for this is that the term “second victim” was first coined in the literature by Dr Albert Wu in 2000.4
Funding for the project was provided through an IWK Health Centre Category A Grant, August 2017.
The authors disclose no conflict of interest.
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.journalpatientsafety.com).
Contributor Information
Laura Wade, Email: laura.wade@dal.ca.
Eleanor Fitzpatrick, Email: eleanor.fitzpatrick@iwk.nshealth.ca.
Natalie Williams, Email: nataliew@ns.sympatico.ca.
Robin Parker, Email: robin.parker@dal.ca.
REFERENCES
- 1.Baker GR Norton PG Flintoft V, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170:1678–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matlow AG Baker GR Flintoft V, et al. Adverse events among children in Canadian hospitals: the Canadian Paediatric Adverse Events Study. CMAJ. 2012;184:E709–E718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conway J Federico F Stewart K, et al. Respectful Management of Serious Clinical Adverse Events (Second Edition). IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2011. [Google Scholar]
- 4.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ. 2000;320:726–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seys D Wu AW Van Gerven E, et al. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof. 2013;36:135–162. [DOI] [PubMed] [Google Scholar]
- 6.Waterman AD Garbutt JF Hazel EF, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33:467–476. [DOI] [PubMed] [Google Scholar]
- 7.Scott SD Hirschinger LE Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010;36:233–240. [DOI] [PubMed] [Google Scholar]
- 8.van Pelt F. Peer support: healthcare professionals supporting each other after adverse medical events. Qual Saf Health Care. 2008;17:249–252. [DOI] [PubMed] [Google Scholar]
- 9.Burlison JD Quillivan RR Scott SD, et al. The effects of the second victim phenomenon on work-related outcomes: connecting self-reported caregiver distress to turnover intentions and absenteeism. J Patient Saf. 2016. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seys D Scott S Wu A, et al. Supporting involved health care professionals (second victims) following an adverse health event: a literature review. Int J Nurs Stud. 2013;50:678–687. [DOI] [PubMed] [Google Scholar]
- 11.Sirriyeh R Lawton RF Gardner PF, et al. Coping with medical error: a systematic review of papers to assess the effects of involvement in medical errors on healthcare professionals’ psychological well-being. Qual Saf Health Care. 2010;19:e43. [DOI] [PubMed] [Google Scholar]
- 12.Cabilan CJ, Kynoch K. Experiences of and support for nurses as second victims of adverse nursing errors: a qualitative systematic review. JBI Database System Rev Implement Rep. 2017;15:2333–2364. [DOI] [PubMed] [Google Scholar]
- 13.Joanna Briggs Institute . The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. Australia: The Joanna Briggs Institute; 2015. [Google Scholar]
- 14.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 15.Hirshon JM Risko N Calvello EJ, et al. Health systems and services: the role of acute care. Bull World Health Organ. 2013;91:386–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bell SK, Moorman DW, Delbanco T. Improving the patient, family, and clinician experience after harmful events: the “when things go wrong” curriculum. Acad Med. 2010;85:1010–1017. [DOI] [PubMed] [Google Scholar]
- 17.Bueno Domínguez M Briansó Florencio M Colomés Figuera L, et al. Experiencia de unidad de soporte a las segundas víctimas (USVIC). Rev Calid Asis. 2016;31(Suppl 2):49–52. [DOI] [PubMed] [Google Scholar]
- 18.Arnold J Tango J Walker I, et al. An evidence-based, longitudinal curriculum for resident physician wellness: the 2017 Resident Wellness Consensus Summit. West J Emerg Med. 2018;19:337–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi N, McGoldrick J, Borgetti S. Creating debriefing sessions for perceived medical errors in residency: a step towards wellness. J Gen Intern Med. 2017;32(Suppl 2):83–808.28397154 [Google Scholar]
- 20.Chung AS Smart J Zdradzinski M, et al. Educator toolkits on second victim syndrome, mindfulness and meditation, and positive psychology: the 2017 Resident Wellness Consensus Summit. West J Emerg Med. 2018;19:327–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daniels RG, McCorkle R. Design of an evidence-based “second victim” curriculum for nurse anesthetists. AANA J. 2016;84:107–113. [PubMed] [Google Scholar]
- 22.Dukhanin V Edrees HH Connors CA, et al. Case: a second victim support program in pediatrics: successes and challenges to implementation. J Pediatr Nurs. 2018;41:54–59. [DOI] [PubMed] [Google Scholar]
- 23.Edrees H Brock DM Wu AW, et al. The experiences of risk managers in providing emotional support for health care workers after adverse events. J Healthc Risk Manag. 2016;35:14–21. [DOI] [PubMed] [Google Scholar]
- 24.Edrees H Connors C Paine L, et al. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6:e011708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edrees HH, Wu AW. Does one size fit all? Assessing the need for organizational second victim support programs. J Patient Saf. 2017. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26.Johnson B. Code Lavender: initiating holistic rapid response at the cleveland clinic. Beginnings. 2014;34:10–11. [PubMed] [Google Scholar]
- 27.Krzan KD Merandi J Morvay S, et al. Implementation of a “second victim” program in a pediatric hospital. Am J Health Syst Pharm. 2015;72:563–567. [DOI] [PubMed] [Google Scholar]
- 28.Lane MA Newman BM Taylor MZ, et al. Supporting clinicians after adverse events: development of a clinician peer support program. J Patient Saf. 2018;14:e56–e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mira JJ Carrillo I Guilabert M, et al. The second victim phenomenon after a clinical error: the design and evaluation of a website to reduce caregivers’ emotional responses after a clinical error. J Med Internet Res. 2017;19:e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pratt S Kenney L Scott SD, et al. How to develop a second victim support program: a toolkit for health care organizations. Jt Comm J Qual Patient Saf. 2012;38:235–240. [DOI] [PubMed] [Google Scholar]
- 31.Roesler R, Ward D, Short M. Supporting staff recovery and reintegration after a critical incident resulting in infant death. Adv Neonatal Care. 2009;9:163–171. [DOI] [PubMed] [Google Scholar]
- 32.BJC Healthcare . We Care Team: Family Resources. St. Louis, MO: Barnes-Jewish Hospital; date unknown. [Google Scholar]
- 33.BJC Healthcare . We Care Team: Providing Care and Support to Our Staff. St. Louis, MO: Barnes-Jewish Hospital; date unknown. [Google Scholar]
- 34.Calder L. Physician Health and Wellness Meeting. Lecture presented at: The Ottawa Hospital; 2013.
- 35.Lynch G. Operational Report of the Critical Incident Stress Management Program of First Nations and Inuit Health Branch. Wingate Consulting: Kanata, Ontario; 2004. [Google Scholar]
- 36.Baylor Scott and White Medical Center—Temple. House Staff Handbook [PDF]. January 2018. Available at: https://www.bswhealth.med/education/Documents/temple/house-staffhandbook.pdf. Accessed November 11, 2018.
- 37.Scott SD. Building a Clinician Support Program: Assessment Worksheet/Planner [PDF]. Columbia, MO: Health Care University of Missouri Health System; 2010. [Google Scholar]
- 38.Scott S. Second victim support: Implications for patient safety attitudes and perceptions. Patient Safety &. Qual Healthc. 2015;12:26–31. [Google Scholar]
- 39.Health PEI. Critical Incident Staff Support (CISS) Managers™ Toolkit [PDF]. 2012 March 21. Available at: http://www.gov.pe.ca/photos/original/src_ciss_tkit.pdf. Accessed November 11, 2018.
- 40.Trent M Waldo K Wehbe-Janek H, et al. Impact of health care adversity on providers: lessons learned from a staff support program. J Healthc Risk Manag. 2016;36:27–34. [DOI] [PubMed] [Google Scholar]
- 41.Washington Patient Safety Coalition (WPSC). Northwest Second Victim Programs. Seattle, WA: Foundation for Health Care Quality; 2013. [Google Scholar]
- 42.Tobin WN. MITSS: Supporting Patients and Families for More Than a Decade [Internet]. 2013. Available at: https://www.psqh.com/analysis/mitss-supporting-patients-and-families-for-more-than-a-decade/. Accessed April 24, 2020.
- 43.Gatzert M, Wobbe A, York L. We Care Team: Caring for the Care Giver. Barnes-Jewish Hospital: St. Louis, MO; 2015. [Google Scholar]
- 44.White AA Brock DM McCotter PI, et al. Risk managers’ descriptions of programs to support second victims after adverse events. J Healthc Risk Manag. 2015;34:30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robbennolt JK. Apologies and medical error. Clin Orthop. 2009;467:376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bledsoe BE. Critical Incident Stress Management (CISM): benefit or risk for emergency services? Prehosp Emerg Care. 2003;7:272–279. [DOI] [PubMed] [Google Scholar]
- 47.Idris AH Bierens JJLM Perkins GD, et al. 2015 Revised Utstein-style recommended guidelines for uniform reporting of data from drowning-related resuscitation: an ILCOR advisory statement. Resuscitation. 2017;118:147–158. [DOI] [PubMed] [Google Scholar]
- 48.Burlison JD Scott SD Browne EK, et al. The second victim experience and support tool: validation of an organizational resource for assessing second victim effects and the quality of support resources. J Patient Saf. 2017;13:93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


