Abstract
The current outbreak of coronavirus disease 2019 (COVID-19) across the world forced universities to suspend learning to limit the spread of the virus. Many medical schools have shifted to online education as an information delivery mechanism where the educator and learner are separated in space and potentially also in time. This systematic review aims to explore and understand the variety of distance learning strategies in medical students in the contexts of COVID-19. A systematic review was conducted in Web of Sciences, PubMed, Educational Resources and Information Center, and Scopus from December 2019 to July 2020. Eight sets of terminology were used, combining “Distance learning” AND “Medical education” AND “Pandemic.” Studies were reviewed independently by two reviewers. Data were extracted and quality appraised using QualSyst tools, and synthesized by performing thematic analysis. A total of 473 articles were identified after removing duplicates and 314 records were screened, of which 125 were included in this study. The primary articles were 52 primarily qualitative articles. Five learning strategies consisted of technology-enhanced learning (TEL), simulation-based learning, technology-based clinical education, mobile learning, and blended learning. Tools, methods, and learning resources associated with these five learning strategies were extracted from the articles. Our review highlights that TEL and simulation-based learning were more commonly used than others in distance learning in medical education during the COVID-19 pandemic. These strategies have the potential to improve learners’ level of knowledge and performance through making online learning resources such as Massive Open Online Courses, virtual clinical cases, and blended sources accessible.
Keywords: COVID-19, distance education, educational technology, handheld computers, medical students, simulation training
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a major challenge in every aspect of health care. Due to lockdowns and social distancing, teaching opportunities for trainees in medical education have been drastically reduced and changed.[1]
The novel COVID-19 outbreak was reported as a public health emergency on January 30, 2020.[2] Subsequently, the World Health Organization declared COVID-19 a pandemic after 200,000 cases had been detected with 8000 deaths across 160 countries.[3] The rapid spread of COVID-19 has had an enormous impact on many aspects of human life, including social development and education, and has caused many countries to activate emergency risk management.[4,5] Any crisis in a nation will always have an impact on education in one way or the another. Students’ right to education is threatened in times of crisis caused by natural disasters such as earthquakes, tsunamis, cyclones, war, and disease outbreak.[6]
The current outbreak of COVID-19 across the world forced universities to suspend learning to limit the spread of the virus. Medical schools have applied a variety of policies that stopped face-to-face students’ education around the world. Most medical institutions have discontinued student clinical rotations and modified undergraduate and postgraduate education by drastically limiting hospital exposure hours. The resulting decreased number of procedures has been of great concern to medical students, residents, and fellows.[7]
This crisis has forced the universities to think of new and alternative strategies to engage students.[8] Many medical schools have shifted to online education to ensure continuity of teaching–learning processes.[6]
Hence, it is time to think of “distance or online learning” as an information delivery mechanism where the educator and learner are separated in space and potentially also in time.[9]
The study by Cook and Dupras introduced a potentially effective way to create an online learning platform in medical education.[10] They emphasized the importance of a user-friendly website design and integration of self-assessment for students.[10]
More recently, Virginia Gewin provided useful tips in the transition to online learning.[11] She describes the utility of live video-conferencing for follow-up on the previously described self-learning module.[10,11,12] In some evidence, lectures have quickly been delivered online by technologically enhanced approaches.[3] These new technologies appear to have many advantages compared with traditional formats; they are more cost-effective, give high levels of access to students, and facilitate more flexible teaching and learning methods, thus increasing educational opportunities.[13]
Another strategy is webinars or online teaching platforms, ensuring that all medical students can access webinars regardless of their actual location.[14]
This systematic review aims to explore and understand the variety of distance learning strategies as a new or innovative way of teaching medical students in the contexts of the COVID-19 pandemic. This paper will address the following two main questions:
What strategies have been deployed in medical education?
What strengths and weaknesses do the instant move to online learning bring?
Materials and Methods
This systematic review includes studies on under- and postgraduate medical education published between December 2019 and July 2020. The COVID-19 pandemic started around December 2019 and related articles were selected in this period.
Search strategy
The following databases were searched: Web of Sciences (Thomson Reuters), PubMed, Educational Resources and Information Center (ERIC), and Scopus.
Primary search terms were distance learning (all synonyms) and COVID-19 (all synonyms) and (medical student) (all synonyms) using MESH terms, employing Boolean operators and truncations such as (education, distance) OR (computer-assisted instruction) OR (digital education) OR (digital learning) OR (e-learning) OR (M-learning) OR (mobile learning) OR (m learning)) OR (u-learning)) OR (ubiquitous learning) OR (simulation training) OR (digital learning) AND (medical students) OR (education, medical) AND ([Pandemics] OR [Coronavirus Infections]) OR (COVID-19). A total of 473 articles were identified after removing duplicates and 314 records were screened, of which 125 were included in this study.
Inclusion and exclusion criteria
The search was restricted to distance learning studies implemented since the onset of the COVID-19 pandemic. A comprehensive search was performed for articles which were published in peer-reviewed journals in English language from December 2019. Articles based on primary studies were also included. The exclusion criteria were: (i) articles not covering distance learning during the COVID-19 pandemic; (ii) articles based on secondary studies; (iii) articles published in nonpeer-reviewed journals; (iv) studies not including medical students; and (v) studies not published in English language.
Selection of studies
Two independent researchers searched the databases by first reviewing each title and abstract matching the inclusion criteria.
Full-text studies were reviewed based on relevant abstracts. In case of any disagreement regarding eligibility, a third independent researcher was involved. The PRISMA guideline (Preferred Reporting Items for Systematic Review and Meta-Analysis) was followed [Figure 1].[15]
Figure 1.
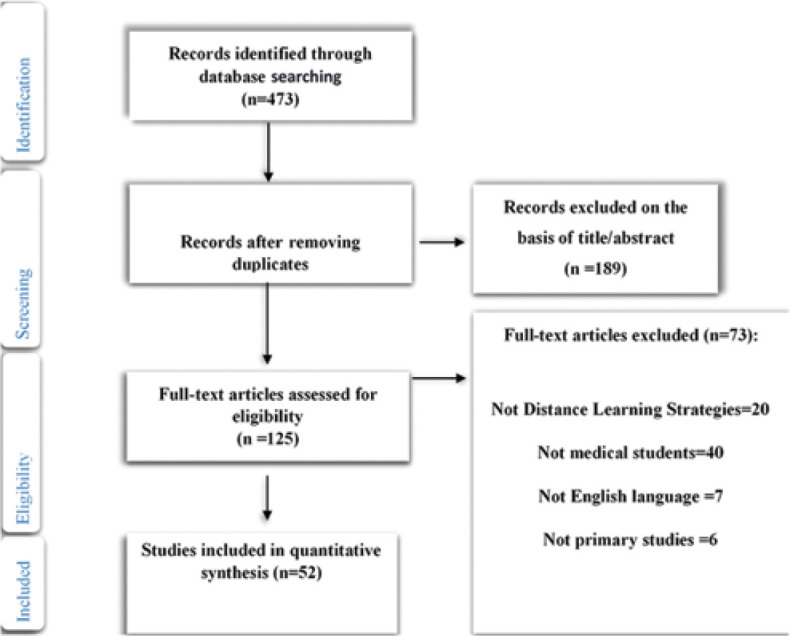
PRISMA flowchart on inclusion of studies
Data analysis and synthesis
Fifty-two articles were included in the review. Statistical integration of the data was not possible because there was no consistency in distance learning strategies and methodologies. In the case of heterogeneity in methodology, the synthesis of findings must be integrated through narrative synthesis.[16,17]
Tabulating the included studies
The authors (MK, N Kh) extracted the following data using a purpose-built, standardized data extraction tool: teaching strategies or methods (tool, technology, and educational platforms), type of study, study country, and participants; disagreements were resolved by involving a third independent researcher (MA).
Quality assessment
The quality of the included studies was assessed by two authors (MK, NKh) using standardized critical appraisal tools from the QualSyst checklist.[18] This scoring system was useful to clearly demonstrate the process and to evaluate the quality of the included papers.[19]
The QualSyst checklist consists of 10 items for qualitative studies. A score of 0–2 is assigned to each question, and the final score is calculated by summing up the total score of each item and dividing them by the total maximum sum.[19,20] A cutoff point of 55% as the threshold for studies was made.[20]
Results
A total of 473 articles were identified after removing duplicates and 314 records were screened, of which 125 were included in this study. The primary articles were 52 primarily qualitative articles [Figure 1]. Most studies were published in 2020. Participants were mostly undergraduate and postgraduate students (medical student, resident, or fellow). Most articles originated from North America (n = 30, 60%) [Figure 2]. A summary of data extraction is provided in Additional File 1. Distribution of studies according to type of publication is illustrated in Figure 3.
Figure 2.
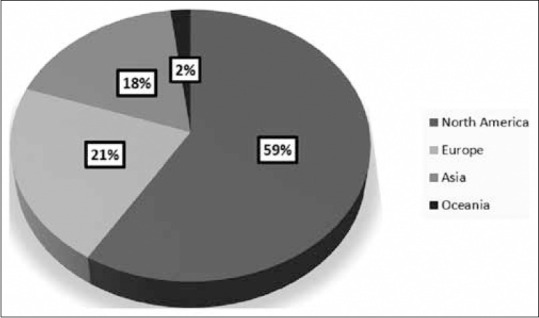
Studies divided by continent
Figure 3.
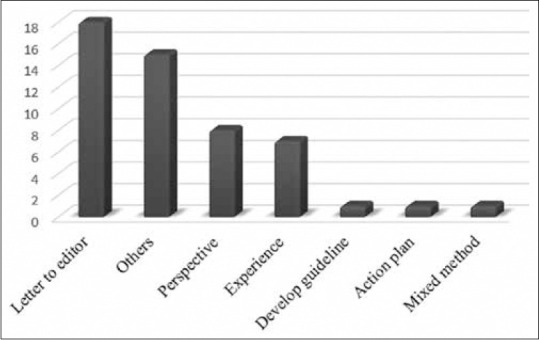
Type of articles
Regarding the type of participants in educational contexts, the most frequently studied sample included residents and fellows (n = 30; 55%), followed by medical students (n = 21; 38%) and academic staffs (n = 4; 7%) [Figure 4].
Figure 4.

Participants
In this review, tools, methods, and learning resources based on each learning strategy are shown in Table 1. Learning strategies consisted of technology-enhanced learning (TEL), simulation-based learning, technology-based clinical education, mobile learning, and blended learning.
Table 1.
Summary of learning strategies, tools, methods, and learning resource associated with distance learning
| Learning strategies | Tools | Methods | Learning resource |
|---|---|---|---|
| TEL | Webinars, [1,14,21,22,23] virtual whiteboards,[21] Blogs,[21] Google classroom, [21,24] virtual classroom,[21,22,25,26,27] videoconferencing,[26,28,29,30] videocast,[31] website,[32] online conference platforms[33] | YouTube-based lecture series,[1] E-seminars[21] local web-based lectures,[34] video-based education,[34] virtual classroom discussions,[26] synchronous tele-education,[35] virtual “review” session,[36] online team-based learning,[37] feedback via online learning advisors,[37] online peer teaching,[38] asynchronous problem-solving activities,[39] synchronous interactive small groups sessions,[39] asynchronous interactive lecture,[40] video lectures[24] | Online learning modules[36] MOOCs [21,24] electronic books[41] subspecialty tele-conferences[27] PowerPoints with voice-over, Elsevier free online teaching-learning resources[24] |
| Simulation-based learning | Endoscopy simulators (mechanical and virtual reality versions),[7] virtual reality simulator models,[34] operating room simulation,[42] endovascular simulation[43] | ||
| Technology-based clinical education | Video [27,28,44,45] telephone,[28] telephone hotlines,[28] telehealth clinics[27] | Endoscopy video rounds,[7] virtual grand rounds,[25,28,33] bedside clinical teaching via Zoom,[37] remote/web-based learning,[44,45,46] virtual or web scenario-based learning,[44] virtual team discussions,[44] web-based discussions,[44] virtual morning report,[28] virtual professors’ rounds,[28] virtual journal club,[28] telephone or phone or video visits,[28,45,47] virtual discussion rounds,[45] remote surgical learning,[42] image-guided surgical E-learning,[42] virtual clerkship,[48] virtual clinic visits[40] | Virtual clinical case,[24] virtual lab[24] |
| Mobile learning | Kahoot app,[21] web-based calls,[44] Jabber app,[28] secure cloud systems,[49] group chat application,[49] smartphone or tablet-based videoconferencing application,[45] telemedicine application[51] | ||
| Blended learning | Flipped virtual classroom[27] | Hybrid learning[21] | Blended courses[42] |
MOOCs=Massive open online courses, TEL=Technology-enhanced learning
TEL can use it to promote information and communication technologies in education and training.[52]
Some researchers focused their studies on tools related to these learning strategies. Kaup et al.[21] introduced various tools to maintain education during this pandemic, such as virtual classroom, webinars, and Blogs. They report that the real classroom has been changed into a virtual classroom with E-seminars, case-based discussions, and Journal clubs, which can be successfully conducted using virtual classrooms. Various medical education methods within TEL can be used during COVID-19, including the 14 teaching methods mentioned in Table 1.[1,6,21,22,25,26,34,35,36,37,38]
Furthermore, six studies mentioned resources for TEL, most of which are free online resources such as Massive Open Online Courses (MOOCs).[6,21,27,36,37,41]
Simulation-based learning can help develop medical students’ knowledge, skills, and attitudes, while maintaining patient safety. Simulation-based medical education may reduce ethical issues and resolve dilemmas. Simulation-based learning techniques, tools, and strategies can be used in designing learning experiences and have previously been broadly applied as an educational strategy in aviation, anesthesiology, and military. Simulators help to decrease errors and maintain safety.[31,53,54]
Studies included in the current study have used four teaching tools in simulation-based learning, namely virtual reality simulator models, operating room simulation, endovascular simulation, and endoscopy simulators (mechanical and virtual reality versions).[24,25,35,36] Virtual reality simulator technology provides the possibility of performing some types of surgery remotely, such as endoscopies. Based on this model, technical, cognitive, and integrative skills (e.g. communication) in surgical training have been developed to ensure the transfer of skills to clinical practice.[34]
Technology-based clinical education is defined as the attainment of clinical education skills via computers which can display combinations of text, images, video, and voice.[55]
Agarwal et al.[28] and Chick et al.[27] used telephone, video, telephone hotlines, and telehealth clinics as clinical education tools during COVID-19.
Some studies suggest 16 learning methods for technology-based clinical education, of which the following three are the most widely used: virtual grand rounds, web-based learning, and phone or video visits. Agarwal et al.[28] used online journal clubs, grand round lectures, case-based morning reports, and educational rounds to increase accessibility for learners from anywhere. Furthermore, residency education continued at the clinic through video visits. Using this method has made lectures more readily accessible, leading to participant participation among residents, fellows, and faculties. Chris Roberts developed “bedside clinical teaching via Zoom” as a new method to protect students’ safety during this medical crisis.
Virtual clinical case and virtual labs are introduced as a resource in this strategy.[56]
Mobile learning is any type of learning that occurs in learning environments that considers the portability of technology, learners, and learning.[57]
Plancher et al. stated that mobile devices or handheld computers could rapidly access learning resources such as journals, e-books, and videos on surgical performances. Use of mobile devices through social media can help young surgeons treat hard cases and make significant long-term contacts with experienced practitioners.[58]
Mobile-based applications (apps) are also an important tool for learning.[59] A variety of mobile apps can help share voice, pictures, slides, and other materials.[32] Agarwal et al.[28] and Kaup et al.[21] used a diversity of tools to present mobile-learning strategies such as the Jabber app and the Kahoot app.[29,32,45,49,50]
García Vazquez et al. reported that operating room simulation could be accessed through mobile phone applications, promoting online surgical training.[42]
Blended learning means that traditional teaching is complemented by electronic formats. It is characterized by combining traditional face-to-face learning and e-learning[51] with additional multimedia options; E-learning environments will also meet different student learning styles.[60]
Because of the risk of infection experienced during COVID-19, both faculty and students were restricted from attending in-person on-site meetings, and blended learning is a way to accommodate these restrictions. Kekkonen-Moneta and Moneta suggested that if interactive learning courses are designed accurately, they can promote higher-order learning outcomes based on students’ different learning styles.[61]
Chen et al., Chick et al., and Kaup et al.[21,27,62] suggested a flipped classroom tool in this strategy. In “flipped classrooms,” students study content online before working with educators to apply knowledge in the classroom (e.g. through problem-based learning). Moreover, compared to lectures, flipped classrooms produce better learning outcomes.
Only one study used hybrid learning as a method of blended learning; they considered surgical education as a robust educational method for experienced surgeons during the COVID-19 crisis.[51]
The findings revealed that the blended courses are resources for this learning strategy.[51]
Table 2 summarizes each study in this review, including social media and platforms.
Table 2.
Social media and platforms related to learning strategies
| Learning strategies | Social media | Platform |
|---|---|---|
| TEL, blended learning, mobile learning, technology-based clinical education | Twitter, WhatsApp, Facebook, Skype, Viber, FaceTime, YouTube live, Periscope | Virtual learning platform using Microsoft teams, Zoom (Zoom, San Jose, California), Slack, cloud-based platforms, Adobe Connect, E-class platform, boot camps, Google Hangouts meet, CiscoWebEx, Elias, Moodle, Canvas, Blackboard, Epolls, Google Forms, webcast, podcasts, asynchronous discussion boards, Google Voice, asynchronous discussion forums, VoxVote, online Meded, E-portfolio platforms like “Mahara,” “FolioSpaces,” online learning management system |
Some studies mentioned eight types of social media and 24 platforms. Most studies had introduced Zoom. Zoom is a videoconferencing service, which has expanded rapidly expansion during the COVID-19 crisis. It is currently an application available for use on desktop or mobile devices. Zoom can be used for one-to-one or group videoconferencing and applies two-way audio and video capacity.
The advantage of Zoom in comparison to other videoconferencing platforms is the availability of a free version, ease of accessibility and use, the ability to share screens, and adaptability with a multitude of devices, including mobile options.[49]
Discussion
This review is, to the best of our knowledge, the first systematic review examining and synthesizing distance learning strategies in medical education during the COVID-19 pandemic. We included and analyzed 52 articles and found five learning strategies commonly applied during the pandemic. Most of the studies have introduced tools, methods, and learning resources associated with these five learning strategies.
Most studies mentioned the use of TEL. The pandemic has shifted attention toward TEL implemented through the design of webinars, virtual classroom, videoconference, and teleconference, and the various learning resources via E-seminar and online team-based learning and synchronous interactive small group sessions. These techniques have been implemented to enhance problem-solving and critical thinking, improve clinical skills, and encourage self-directed learning.[63] Barberio et al. indicated that these strategies could help develop clinical skills and holistic noncognitive characteristics, such as flexibility and cooperation among medical students, residents, and fellows.[34]
Another strategy was simulation-based learning. All of the studies using this strategy concerned residency training. This strategy may develop health professionals’ knowledge, skills, and attitudes while maintaining patient safety.
Simulation-based training techniques, tools, and strategies can be applied in designing structured learning experiences and used as a measurement tool for competences and learning objectives. It helps to decrease errors and maintain a culture of safety.[31,53,64] Simulation-based learning has not only been used during the COVID-19 pandemic,[65,66] but COVID-19 has made us apply this strategy more quickly. One of the challenges of medical education in COVID-19 is skills training, which is not possible due to social distancing. Kononowicz's systematic review indicated improving knowledge and procedural skills and improving clinical reasoning by using a virtual patient.[67]
Clinical education will be increasingly complemented by computers with combinations of multimedia elements, and new strategies for using technologies for education. This result Refers to the concept of technology-based clinical education.
During this medical crisis, clinical education needs to rapidly manage the increasing number of patient cases while being careful of protecting care providers and continuing educational activities. Agarwal et al. reported that using technology-based clinical education to convert continuity in clinical patient visits to virtual options, transforming didactics to online platforms.[28]
Some methods suggested in Agarwal's study were Journal clubs, case-based morning reports, and professors’ rounds, which were formerly available via videoconferencing and now been changed to an online-only platform.[28]
Another learning strategy in this review was mobile learning. Mobile learning is still a developing area, but it already offers many advantages compared with other strategies such as mobility, portability and small size, price, coordination, knowledge base, and access to multimedia. Despite these benefits, there are some disadvantages: small screens, the use of these devices results in the disruption of other activities, mobile portability increases the risk of theft, and loss of information.[68]
Some studies have shown that handheld technologies can improve the use of evidence-based medicine and clinical decision-making.[69] Furthermore, there is a growing interest in using handheld technologies to improve preclinical learning.[70,71] and clinical learning.[72,73]
To properly utilize mobile technologies, medical educators need to grasp the underlying principles governing their social and pedagogical use and create an environment where these technologies can be used effectively. In this way, medical educators can better utilize the advantages of using mobile technologies and prepare learners for practice in a world in which mobile technology use is pervasive and transformative.[74]
The restrictions caused by the COVID-19, and to ensure continuity of learning for medical students, mobile learning is a suitable strategy in higher education as students can learn at anytime, anywhere.
Blended learning has also been used during the pandemic. Most studies on these strategies were conducted among medical students and less among residents.
Blended learning by integrating online instruction has been shown to overcome the limitations of time and space, support instructional methods that are hard to achieve using textbooks, and reach a larger number of students without increasing the need for resources.[48,75] Kaveevivitchai et al. stated a significant difference favoring blended learning for performance and skill acquisition compared with online learning alone.[76]
A potentially positive result of the pandemic has been greater access to online educational platforms and social media for medical students worldwide. Chatziralli stated that they used several platforms, that is, Zoom®, Skype, for teaching because lectures had been rapidly converted from face-to-face to online video conferences. This approach allows faculty and residents/fellows to attend education at more convenient times based on their schedules. Besides, basic versions of many online platforms and social media are currently free of charge and allow for invited national and international speakers to participate at reduced costs.[26]
Limitations and recommendation
One limitation of this review was the lack of original studies. Therefore, it is possible that some studies were conducted by focusing on primary studies. Second, our search was restricted to the following four databases: PubMed, Web of Science, Scopus, and ERIC databases. Thus, we suggested that some studies be carried out in other databases. Third, in our search, eight sets of terminology were used, combining (“Distance learning” OR “Mobile learning” OR “Ubiquitous Learning” OR “Simulation training” OR “Digital education”) AND (“Medical student” OR “Medical education”) AND “Pandemic.” Other terminology could be searched by authors. Moreover, some studies may have emphasized other keywords to describe them. Fourth, this study included only English-language articles, and therefore seven out of 73 studies were excluded. It is also possible that other languages are included in future studies. Finally, the study lacked meta-analysis because of the dissimilar nature of the results. It is recommended that some studies be prepared in different study designs.
Conclusions
Our review highlights that TEL and simulation-based learning were more commonly used than others in distance learning in medical education during the COVID-19 pandemic. These strategies have the potential to improve learners’ level of knowledge and performance through making online learning resources such as MOOCs, virtual clinical cases, and blended courses accessible to learners regardless of their contexts and timescale.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank reviewers for their helpful comments.
References
- 1.Hughes BA, Stallard J, West CC. The use of WhatsApp® as a way to deliver Plastic Surgery Teaching during the COVID-19 pandemic. J Plast Reconstr Aesthet Surg. 2020;73:e1–e2. doi: 10.1016/j.bjps.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–6. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spinelli A, Pellino G. COVID-19 pandemic: Perspectives on an unfolding crisis. Br J Surg. 2020;107:785–7. doi: 10.1002/bjs.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C, Cheng Z, Yue XG, McAleer M. Risk management of COVID-19 by universities in China. J Risk Financ Manag. 2020;13:36. [Google Scholar]
- 5.Yusoff MS, Hadie SN, Mohamad I, Draman N, Muhd Al-Aarifin I, Wan Abdul Rahman WF, et al. Sustainable medical teaching and learning during the COVID-19 pandemic: Surviving the new normal. Malays J Med Sci. 2020;27:137–42. doi: 10.21315/mjms2020.27.3.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zayabalaradjane Z. COVID-19: Strategies for online engagement of remote learners. Online Submission. 2020;9:1–1. [Google Scholar]
- 7.Siddiqui UD, Aslanian HR. The new virtual reality: Advanced endoscopy education in the COVID-19 Era. Dig Dis Sci. 2020;65:1888–91. doi: 10.1007/s10620-020-06386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Longhurst GJ, Stone DM, Dulohery K, Scully D, Campbell T, Smith CF. Strength, Weakness, Opportunity, Threat (SWOT) analysis of the adaptations to anatomical education in the united kingdom and republic of Ireland in response to the COVID-19 pandemic. Anat Sci Educ. 2020;13:301–11. doi: 10.1002/ase.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Billings DM. Distance education in nursing: 25 years and going strong. Comput Inform Nurs. 2007;25:121–3. doi: 10.1097/01.NCN.0000270044.67905.4a. [DOI] [PubMed] [Google Scholar]
- 10.Cook DA, Dupras DM. A practical guide to developing effective web-based learning. J Gen Intern Med. 2004;19:698–707. doi: 10.1111/j.1525-1497.2004.30029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gewin V. Five tips for moving teaching online as COVID19 takes hold. Nature. 2020;580:295–6. doi: 10.1038/d41586-020-00896-7. [DOI] [PubMed] [Google Scholar]
- 12.Schneider SL, Council ML. Distance learning in the era of COVID-19. Arch Dermatol Res. 2020;8:1–2. doi: 10.1007/s00403-020-02088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oliver R. Exploring strategies for online teaching and learning. Distance Educ. 1999;20:240–54. [Google Scholar]
- 14.Sandhu P, de Wolf M. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online. 2020;25:1764740. doi: 10.1080/10872981.2020.1764740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clarke M. Overview of methods. In: Webb C, Roe B, editors. Reviewing Research Evidence for Nursing Practice: Systematic Reviews. Oxford: Blackwell Publishing Ltd; 2007. pp. 1–8. [Google Scholar]
- 17.Rodgers M, Sowden A, Petticrew M, Arai L, Roberts H, Britten N, et al. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews. Eval. 2009;15:47–71. [Google Scholar]
- 18.Kmet LM, Lee RC, Cook LS. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. Canada: Alberta Heritage Foundation for Medical Research (AHFMR); 2004. [Last accessed on 2019 Oct 30]. Available from: https://www.biomedcentral.com/content/supplementary/1471-2393-14-52-s2.pdf . [Google Scholar]
- 19.Lee L, Packer TL, Tang SH, Girdler S. Self-management education programs for age-related macular degeneration: A systematic review. Australas J Ageing. 2008;27:170–6. doi: 10.1111/j.1741-6612.2008.00298.x. [DOI] [PubMed] [Google Scholar]
- 20.Maharaj S, Harding R. The needs, models of care, interventions and outcomes of palliative care in the Caribbean: A systematic review of the evidence. BMC Palliat Care. 2016;15:9. doi: 10.1186/s12904-016-0079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaup S, Jain R, Shivalli S, Pandey S, Kaup S. Sustaining academics during COVID-19 pandemic: The role of online teaching-learning. Indian J Ophthalmol. 2020;68:1220–1. doi: 10.4103/ijo.IJO_1241_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mishra D, Nair AG, Gandhi RA, Gogate PJ, Mathur S, Bhushan P, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India – Outcomes of a survey. Indian J Ophthalmol. 2020;68:999–1004. doi: 10.4103/ijo.IJO_1067_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaveevivitchai C, Chuengkriankrai B, Luecha Y, Thanooruk R, Panijpan B, Ruenwongsa P. Enhancing nursing students’ skills in vital signs assessment by using multimedia computer-assisted learning with integrated content of anatomy and physiology. Nurse Educ Today. 2009;29:65–72. doi: 10.1016/j.nedt.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 24.Zayapragassarazan Z. COVID-19: Strategies for engaging remote learners in medical education [version 1; not peer reviewed] F1000Res. 2020;9:273. [Google Scholar]
- 25.Anwar A, Seger C, Tollefson A, Diachun CA, Tanaka P, Umar S. Medical education in the COVID-19 era: Impact on anesthesiology trainees. J Clin Anesth. 2020;66:109949. doi: 10.1016/j.jclinane.2020.109949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bloom DA, Reid JR, Cassady CI. Education in the time of COVID-19. Pediatr Radiol. 2020;50:1055–8. doi: 10.1007/s00247-020-04728-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chick RC, Clifton GT, Peace KM, Propper BW, Hale DF, Alseidi AA, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–32. doi: 10.1016/j.jsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agarwal S, Sabadia S, Abou-Fayssal N, Kurzweil A, Balcer LJ, Galetta SL. Training in neurology: Flexibility and adaptability of a neurology training program at the epicenter of COVID-19. Neurology. 2020;94:e2608–14. doi: 10.1212/WNL.0000000000009675. [DOI] [PubMed] [Google Scholar]
- 29.Roy SF, Cecchini MJ. Implementing a structured digital-based online pathology curriculum for trainees at the time of COVID-19. J Clin Pathol. 2020;73:444. doi: 10.1136/jclinpath-2020-206682. [DOI] [PubMed] [Google Scholar]
- 30.Zuo L, Dillman D, Miller Juvé A. Learning at home during COVID-19: A multi-institutional virtual learning collaboration. Med Educ. 2020;54:664–5. doi: 10.1111/medu.14194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;13(Suppl 1):i2–10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mukhopadhyay S, Booth AL, Calkins SM, Doxtader EE, Fine SW, Gardner JM, et al. Leveraging technology for remote learning in the era of COVID-19 and social distancing: Tips and resources for pathology educators and trainees. Arch Pathol Lab Med. 2020;144:1027–36. doi: 10.5858/arpa.2020-0201-ED. [DOI] [PubMed] [Google Scholar]
- 33.Lewis CT, Zeineddine HA, Esquenazi Y. Challenges of neurosurgery education during the coronavirus disease 2019 (COVID-19) pandemic: A U.S. perspective. World Neurosurg. 2020;138:545–7. doi: 10.1016/j.wneu.2020.04.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chatziralli I, Ventura CV, Touhami S, Reynolds R, Nassisi M, Weinberg T, et al. Transforming ophthalmic education into virtual learning during COVID-19 pandemic: A global perspective. Eye (Lond) 2020;10:1–8. doi: 10.1038/s41433-020-1080-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barberio B, Massimi D, Dipace A, Zingone F, Farinati F, Savarino EV. Medical and gastroenterological education during the COVID-19 outbreak. Nat Rev Gastroenterol Hepatol. 2020;17:447–9. doi: 10.1038/s41575-020-0323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Regier DS, Smith WE, Byers HM. Medical genetics education in the midst of the COVID-19 pandemic: Shared resources. Am J Med Genet Part A. 2020;182:1302–8. doi: 10.1002/ajmg.a.61595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberts C. How medical education can help in a COVID-19 crisis. Clin Teach. 2020;17:241. doi: 10.1111/tct.13183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts V, Malone K, Moore P, Russell-Webster T, Caulfield R. Peer teaching medical students during a pandemic. Med Educ Online. 2020;25:1772014. doi: 10.1080/10872981.2020.1772014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pather N, Blyth P, Chapman JA, Dayal MR, Flack NA, Fogg QA, et al. Forced disruption of anatomy education in Australia and New Zealand: An acute response to the COVID-19 pandemic. Anat Sci Educ. 2020;13:284–300. doi: 10.1002/ase.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mousa AY, Broce M. The impact of COVID-19 on vascular training. J Vasc Surg. 2020;72:380–1. doi: 10.1016/j.jvs.2020.04.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chong A, Kagetsu NJ, Yen A, Cooke EA. Radiology residency preparedness and response to the COVID-19 pandemic. Acad Radiol. 2020;27:856–61. doi: 10.1016/j.acra.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.García Vazquez A, Verde JM, Dal Mas F, Palermo M, Cobianchi L, Marescaux J, et al. Image-guided surgical e-learning in the post-COVID-19 pandemic Era: What is next? J Laparoendosc Adv Surg Tech A. 2020;30:993–7. doi: 10.1089/lap.2020.0535. [DOI] [PubMed] [Google Scholar]
- 43.Kesselman A, Lamparello NA, Malhotra A, Winokur RS, Pua BB. Endovascular simulation as a supplemental training tool during the COVID-19 national emergency. Clin Imaging. 2020;67:72–3. doi: 10.1016/j.clinimag.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ashokka B, Ong SY, Tay KH, Loh NH, Gee CF, Samarasekera DD. Coordinated responses of academic medical centres to pandemics: Sustaining medical education during COVID-19. Med Teach. 2020;42:762–71. doi: 10.1080/0142159X.2020.1757634. [DOI] [PubMed] [Google Scholar]
- 45.Codispoti CD, Bandi S, Moy JN, Mahdavinia M. Running a virtual allergy division and training program in the time of COVID-19 pandemic. J Allergy Clin Immunol. 2020;145:1357–9. doi: 10.1016/j.jaci.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Comer BT, Gupta N, Mowry SE, Malekzadeh S. Otolaryngology education in the setting of COVID-19: Current and future implications. Otolaryngol Head Neck Surg. 2020;163:70–4. doi: 10.1177/0194599820923621. [DOI] [PubMed] [Google Scholar]
- 47.Carvalho VO, Conceição LS, Gois MB., Jr COVID-19 pandemic: Beyond medical education in Brazil. J Card Surg. 2020;35:1170–1. doi: 10.1111/jocs.14646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCutcheon K, Lohan M, Traynor M, Martin D. A systematic review evaluating the impact of online or blended learning vs. face-to-face learning of clinical skills in undergraduate nurse education. J Adv Nurs. 2015;71:255–70. doi: 10.1111/jan.12509. [DOI] [PubMed] [Google Scholar]
- 49.Almarzooq ZI, Lopes M, Kochar A. Virtual learning during the COVID-19 pandemic: A disruptive technology in graduate medical education. J Am Coll Cardiol. 2020;75:2635–8. doi: 10.1016/j.jacc.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yuen JC, Gonzalez SR. Addressing the surgical training gaps caused by the COVID-19 pandemic: An opportunity for implementing standards for remote surgical training. Plast Reconstr Surg. 2020;146:109e–10. doi: 10.1097/PRS.0000000000007074. [DOI] [PubMed] [Google Scholar]
- 51.Kim K, Bonk CJ, Oh E. The present and future state of blended learning in workplace learning settings in the United States. Perf Improv. 2008;47:5–16. [Google Scholar]
- 52.Kirkwood A, Price L. Technology-enhanced learning and teaching in higher education: what is ‘enhanced’ and how do we know? A critical literature review. Learn Media Technol. 2014;39:6–36. [Google Scholar]
- 53.Jha AK, Duncan BW, Bates DW. Making Health Care Safer: A Critical Analysis of Patient Safety Practices. United States: Agency for Health care, Research and Quality. U.S. Dept of Health and Human Services; 2001. Simulator based training and patient safety; pp. 511–8. [Google Scholar]
- 54.Lateef F. Simulation-based learning: Just like the real thing. J Emerg Trauma Shock. 2010;3:348–52. doi: 10.4103/0974-2700.70743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Henderson JV. Comprehensive, technology-based clinical education: The “virtual practicum”. Int J Psychiatry Med. 1998;28:41–79. doi: 10.2190/NQEN-KRT8-19GA-R0BV. [DOI] [PubMed] [Google Scholar]
- 56.Guragai M. Nepalese medical students in the COVID-19 pandemic: Ways forward. J Nepal Med Assoc. 2020;58:352–4. doi: 10.31729/jnma.4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.El-Hussein MO, Cronje JC. Defining mobile learning in the higher education landscape. J Educ Technol Soc. 2010;13:12–21. [Google Scholar]
- 58.Plancher KD, Shanmugam JP, Petterson SC. The changing face of orthopaedic education: Searching for the new reality after COVID-19. Arthrosc Sports Med Rehabil. 2020;2:e295–e298. doi: 10.1016/j.asmr.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moran J, Briscoe G, Peglow S. Current technology in advancing medical education: Perspectives for learning and providing care. Acad Psychiatry. 2018;42:796–9. doi: 10.1007/s40596-018-0946-y. [DOI] [PubMed] [Google Scholar]
- 60.Wang FL, Fong J, Kwan R. Handbook of Research on Hybrid Learning Models: Advanced Tools, Technologies, and Applications. New York: Information Science Reference; 2010. [Google Scholar]
- 61.Kekkonen-Moneta S, Moneta GB. E-Learning in Hong Kong: Comparing learning outcomes in online multimedia and lecture versions of an introductory computing course. Br J Educ Technol. 2002;33:423–33. [Google Scholar]
- 62.Chen CH, Mullen AJ. COVID-19 can catalyze the modernization of medical education. JMIR Med Educ. 2020;6:e19725. doi: 10.2196/19725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilder S. Impact of the problem-based learning on high school academic achievement: A systematic review. Educ Rev. 2015;67:414–35. [Google Scholar]
- 64.Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;13(Suppl 1):i2–10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zardosht R, Karimi Moonaghi H, Etezad Razavi M, Ahmady S. Educational concern of surgical technology students in the operating room: A grounded theory study. J Educ Health Promot. 2020;9:58. doi: 10.4103/jehp.jehp_348_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–58. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 67.Kononowicz AA, Woodham LA, Edelbring S, Stathakarou N, Davies D, Saxena N, et al. Virtual patient simulations in health professions education: Systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res. 2019;21:e14676. doi: 10.2196/14676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ellaway R, Masters K. AMEE Guide 32: E-Learning in medical education Part 1: Learning, teaching and assessment. Med Teach. 2008;30:455–73. doi: 10.1080/01421590802108331. [DOI] [PubMed] [Google Scholar]
- 69.Leung GM, Johnston JM, Tin KY, Wong IO, Ho LM, Lam WW, et al. Randomised controlled trial of clinical decision support tools to improve learning of evidence based medicine in medical students. BMJ. 2003;327:1090. doi: 10.1136/bmj.327.7423.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dolan B. Nine Medical Schools that Support Mobile Learning. Mobihealthnews. Obtenido De. 2011. [accessed 19 May 2015]. Available from: http://mobihealthnews.com/12346/nine-medical-schoolsthat-support-mobile-learning/
- 71.George P, Dumenco L, Doyle R, Dollase R. Incorporating iPads into a preclinical curriculum: A pilot study. Med Teach. 2013;35:226–30. doi: 10.3109/0142159X.2012.735384. [DOI] [PubMed] [Google Scholar]
- 72.Katibeh M, Sabbaghi H, Kalantarion M, Nikkhah H, Mousavi B, Beiranvand R, et al. Eye care utilization in a community-oriented mobile screening programme for improving eye health in Iran: A cluster randomized trial. Ophthalmic Epidemiol. 2020;27:417–28. doi: 10.1080/09286586.2020.1768552. [DOI] [PubMed] [Google Scholar]
- 73.Mosa AS, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67. doi: 10.1186/1472-6947-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Masters K, Ellaway RH, Topps D, Archibald D, Hogue RJ. Mobile technologies in medical education: AMEE Guide No.105. Med Teach. 2016;38:537–49. doi: 10.3109/0142159X.2016.1141190. [DOI] [PubMed] [Google Scholar]
- 75.Mosalanejad L, Ahmady S. Implementation of blended learning with native systems: A new model for the application of new technology in Iranian medical education. J Educ Health Promot. 2019;8:239. doi: 10.4103/jehp.jehp_402_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kaveevivitchai C, Chuengkriankrai B, Luecha Y, Thanooruk R, Panijpan B, Ruenwongsa P. Enhancing nursing students’ skills in vital signs assessment by using multimedia computer-assisted learning with integrated content of anatomy and physiology. Nurse Educ Today. 2009;29:65–72. doi: 10.1016/j.nedt.2008.06.010. [DOI] [PubMed] [Google Scholar]


