Abstract
Perceiving that one has grown in positive ways following highly stressful experiences (perceived posttraumatic growth; PPTG) is common and sometimes--but not always--related to psychological wellbeing. However, PPTG is typically studied cross-sectionally and well after the stressful experience has passed; how PPTG might relate to wellbeing over time in an unprecedented, ongoing worldwide disaster such as the COVID-19 pandemic remains unknown. Thus, the current study sought to answer whether, in the midst of the pandemic, PPTG relates to subsequent wellbeing, broadly defined. Participants were N = 1544 MTurk workers who completed a five-wave (T1-T5) six-month longitudinal study. Current analyses focused on T2-T5 (ns = 860–712). At each time point, participants completed self-report measures of PPTG and wellbeing (depression, anxiety, stress, positive states of mind, alcohol use, posttraumatic stress). In cross-lagged panel models, PPTG was largely unrelated to subsequent wellbeing. Somewhat more evidence was found that increasing distress led to increases in PPTG, suggesting perceptions of growth may serve as a coping mechanism. PPTG does not appear to benefit adjustment to the COVID-19 pandemic and may simply reflect efforts to manage distress.
Keywords: COVID-19, Distress: posttraumatic growth, Adjustment, Coping
Perceived posttraumatic growth (PPTG) refers to positive life changes that people commonly report experiencing following highly stressful events (Park, 2009), such as developing closer relationships with significant others, appreciating life more, and developing a deeper spiritual perspective. This phenomenon has been studied in the context of a wide variety of different types of traumatic events, including cancer and other health conditions such as heart disease and multiple sclerosis, motor vehicle accidents, combat, shipwrecks, bereavement, and sexual assault (Mangelsdorf et al., 2019).
Much of this work has been conducted with individuals experiencing personal traumas, but PPTG is also commonly reported in communal traumas such as earthquakes, hurricanes, floods, and terrorist attacks (Park and Blake, 2020). Thus, reports of PPTG might be expected to also be common in the context of the COVID-19 pandemic, and indeed early studies have documented fairly high levels of PPTG in samples around the world, including in China (Li et al., 2021), Greece (Koliouli et al., 2021), Germany (Büssing et al., 2020), Spain (Prieto-Ursúa et al., 2020; Vazquez et al., 2021), Portugal and the UK (Stallard et al., 2021), Turkey (Ikizer et al., 2021), Taiwan (Chen et al., 2021), Canada, France and Israel (Uziel et al., 2021), and the US (Pietrzak et al., 2021).
Research has established that PPTG is common following highly stressful and traumatic events, including the COVID-19 pandemic. The universal and enduring impact of the pandemic provides a rare opportunity to examine these questions in a population that has collectively experienced substantial disruption to their lives. The present study aimed to examine whether PPTG related to better psychological adjustment in the months following the initial lockdowns of the COVID-19 pandemic in the US.
1. Relations of PPTG with better psychological adjustment
PPTG is often assumed to be a marker of positive adjustment to the trauma and of restored psychological functioning (e.g., Tedeschi et al., 2018). Indeed, clinical researchers have begun to test interventions to facilitate PPTG based on this assumption (e.g., Ramos et al., 2018; Roepke et al., 2018; Ye et al., 2018). Yet findings regarding PPTG and psychological adjustment following trauma are decidedly mixed. PPTG is sometimes positively associated with measures of positive aspects of well-being (e.g., positive affect), especially in cross-sectional studies (CasellasGrau et al., 2017), but is often unrelated, especially in longitudinal studies (e.g., Eisma et al., 2019). In addition, PPTG is quite inconsistently related--sometimes favorably, sometimes unfavorably, and sometimes unrelated--to negative trauma outcomes such as depression and anxiety (Helgeson et al., 2006; Long et al., 2021). Further, PPTG is fairly consistently positively related to posttraumatic stress symptoms (PTSS; for meta-analyses, see Helgeson et al., 2006; Liu et al., 2017; Schubert et al., 2016). Even using longitudinal designs to examine cross-lagged relationships, some studies showed higher Time 1 PPTG predicting higher T2 PTSS (Engelhard et al., 2015; Zalta et al., 2017), some finding lower (e.g., Chen et al., 2015), and others finding no associations (Eisma et al., 2019). Clearly, relationships between PPTG and PTSS are complicated and likely influenced by numerous moderating variables. In summary, PPTG is often either unrelated or positively related to aspects of negative trauma-related adjustment.
Similar inconsistent findings regarding PPTG and psychological adjustment have been reported in the pandemic. Positive associations of PPTG and distress have been reported in a community sample in Spain (PTSS; Vazquez et al., 2021), a sample of nurses in Taiwan (burnout; Chen et al., 2021), a sample of dental personnel in Canada, France and Israel (depression and worry; Uziel et al., 2021), a sample of community residents in Greece (perceived stress; Koliouli and Canellopoulos, 2021), a national sample of US veterans (PTSD symptoms; Pietrzak et al., 2021), a snowball sample of people in Turkey (PTSS and perceived depreciation; Ikizer et al., 2021), and an online sample in the US (mental health; Kowalski et al., 2021). In China, a study of nurses and the general population found PPTG was unrelated to anxiety (Li et al., 2021) and another of high school graduates found PPTG unrelated to anxiety or depression (Yu et al., 2021). In one study, of a German community sample, PPTG was positively associated with life satisfaction (Büssing et al., 2020) and in another, of caregivers of children in Portugal and the UK, PPTG was related to higher wellbeing but unrelated to anxiety (Stallard et al., 2021). All of these studies were cross-sectional, however, and salutary associations between PPTG and psychological adjustment following the pandemic may take time to manifest. A further consideration worthy of study is the role time played over the course of the COVID-19 pandemic – specifically, the impact evolving stresses had on perceptions of growth and depreciation (Taku et al., 2021) as the virus surged over multiple waves over the course of 2020.
The inconsistent findings between PPTG and various aspects of adjustment and wellbeing across diverse populations dealing with a wide range of outcomes has been attributed to the notion that PPTG largely comprises coping efforts, signaling distress rather than being an outcome of stressful experiences (Zoellner and Maercker, 2006). Perceiving that one has grown as a result of traumatic experiences can function as a form of coping by viewing the situation in more positive ways (i.e., reappraisal), particularly as a pathway through which one has been able to make positive changes. PPTG is consistently and strongly associated with positive reinterpretation coping (e.g., HamamaRaz et al., 2019; Shand et al., 2015); such links would be expected if PPTG was simply another form of coping (i.e., of trying to see an event as less threatening/more favorable)—that is, the event seems less terrible because it was an occasion for some positive outcomes to occur (Finkelstein-Fox, Park, & Kalichman, 2019). This coping process of searching for some positive outcomes of traumatic events has also been termed “benefit finding” (Tennen and Affleck, 2002).
Thus, in the present study we aimed to examine, in a national sample experiencing a long-term pandemic and associated life disruptions, whether PPTG would be associated with subsequent adjustment and to examine these relationships repeatedly as the pandemic wore on and people adapted to their altered circumstances, vaccines were developed and administered, and societal reopening was underway. Further, because PPTG demonstrates inconsistency across different measures of adjustment and wellbeing, we examined a host of wellbeing measures, including general and trauma-specific distress, positive states of mind, and--a behavioral aspect of adjustment highly relevant during the pandemic (Schmits and Glowacz, 2021) but rarely studied in the context of PPTG in any population (cf. McDiarmid et al., 2017)--alcohol use. We hypothesized that PPTG at a given time point would subsequently be associated with lower depression, anxiety, stress, PTSS, and alcohol use. We also hypothesized that it would be related to higher levels of positive states of mind. However, we rendered these hypotheses tentatively, acknowledging the high likelihood of finding inconsistency.
1.1. Open practices statement
Analyses for this study were preregistered following data collection. The preregistration can be accessed at:
[https://osf.io/tv4de/?view_only=bc5cb5454596415e9268ad9edaf695c4].
2. Method
2.1. Participants
Participants were recruited from the Amazon MTurk online worker pool. Eligible participants were aged 18 or older, residing in the US, and able to read English. After following best practice guidelines for online data cleaning at each timepoint to screen out suspicious or poor-quality responses (e.g., removal of inattentive cases and responses originating outside valid locations in the US, ensuring unique human responders as opposed to computerized bot responses), 1544 high quality unique responses were available at baseline (T1), of whom 860 provided high quality data at T2, 816 at T3, 744 at T4 and 712 at T5. Cases were validated through the use of time to completion or “fast-responder” analysis that eliminated any response completed in less than 10 min, Captcha screening, and location verification through GPS coordinate confirmation.
Studies using MTurk have found the data to be high quality, replicable, and valid across comparisons with frequently used academic platforms (Bartneck et al., 2015; Sheehan & Pitman, 2016). Although some studies suggests that MTurk respondents report slightly higher levels of depression than the general population (e.g., Ophir et al., 2020), others indicate mental health (as assessed by the DASS-21, also used in the present study) of MTurk workers approximates that of the general US population (e.g., Kim and Hodgins, 2017; Mortensen and Hughes, 2018).
3. Data collection
The university IRB approved all study materials (X20-057). Participants volunteered for the study on the MTurk homepage and provided informed consent prior to screening and completing T1 questionnaires. The project was advertised as an anonymous, longitudinal study of the impact of Covid-19 on daily life, providing participants with $2 for completing the T1 survey and $3 for subsequent surveys. Data presented here are drawn from the T1 survey, administered from April 8-25, 2020 (approximately 3 weeks after widespread US shelter-in-place recommendations were first issued), the T2 survey, administered from May 15-29, at which point many areas of the US had begun to implement reopenings, the T3 survey, June 30-July 14, a period of additional reopenings but also sporadic viral surges, reclosures, and increased uncertainty, the T4 survey (August 24 to September 10, 2020), a period of continued concern and closures and an up-coming contentious general election further politicizing the pandemic, and the Time 5 survey immediately following the election (November 12-29, 2020), when holiday surges were expected and effective COVID-19 vaccines were expected within a matter of months.
3.1. Measures
3.1.1. Demographics
At T1, participants reported on their location by state, financial security, whether they were a primary caregiver for a dependent, partner status, gender, sexual orientation, race, ethnicity, and age.
3.1.2. Perceived posttraumatic growth
From Time 2 onward, we administered the CAIR (Complementary and Integrative Research Lab)-Pandemic Impact Questionnaire (C-PIQ) Positive Impact scale (Lang, 2020) as recommended by NIH in the early days of the pandemic (NIH, 2020). This scale is a version of the PTGI (Tedeschi and Calhoun, 1996) modified for the Covid-19 Pandemic, asking participants “Has the COVID-19 pandemic led to any of the following positive changes in your life IN THE PAST TWO WEEKS?” and presents five items (e.g., “created spiritual change” and “strengthened your relationships with others or your community”) rated from “not at all” (1) to “extremely” (5). Cronbach's alphas for each time point used in the analyses were: T2 (0.85), T3 (0.86), T4 (0.88), and T5 (0.89).
3.1.3. General distress
Past-week general distress was assessed at T2-T5 using the 21-item version of the Depression, Anxiety, and Stress Scales (DASS-21; Lovibond and Lovibond, 1995). Items are rated from 0 (“Did not apply to me at all”) to 3 (“Applied to me very much or most of the time”). Summed scores are multiplied by 2 to create separate subscales, each ranging from 0 to 42). The DASS-21 demonstrated good psychometric properties in samples of Chinese during the COVID-19 pandemic (Wang et al., 2020) and MTurk workers (e.g., Arditte et al., 2016). Cronbach's alphas in the present sample at T2, T3, T4, and T5 were, respectively, 0.93, 94, and 0.94 for depression; 0.89, 0.90, and for anxiety, and 0.90, 0.90, and 0.91 for stress.
3.1.4. General positive states
From Time 2 onward, the 7-item Positive States of Mind Scale (PSOM; Horowitz et al., 1988) assessed participants' ability to experience desired positive psychological states (e.g., focused attention, restful repose), in reference to the past week. Items were rated from 0 (“unable to experience this even though I have wanted to”) to 3 (“easy to experience”), with an additional option to mark items as “not relevant/have not wanted to experience” (these response options were excluded from the calculation of item mean scores). Cronbach's alpha for the PSOM was .89 at T3 in the current sample, with total possible scores ranging from 0 to 3.
3.1.5. Alcohol use
An item from the AUDIT-C (Bradley et al., 2003) asked participants about number of days in the past month that they consumed alcohol.
3.1.6. Covid-19-specific posttraumatic distress
From Time 2 onward, the Impact of Events Scale-Revised (IES-R; Weiss and Marmar, 1997) was administered. The IES-R is a 22-item scale that assesses psychological distress due to a traumatic life event reflected in three types of symptoms: Avoidance (8 items), Intrusion (8 items) and Hyperarousal (6 items). Instructions read, “The following is a list of difficulties people sometimes have after stressful life events. Please read each item and then indicate how distressing each difficulty has been for you during the past 7 days with respect to the COVID-19 pandemic. How much were you distressed or bothered by these difficulties?” using a 5-point Likert scale (0 “Not at all” to 4 “Extremely” (e.g., “Pictures about it popped into my mind”; “I had trouble falling asleep”). The IES-R has extensively been used in clinical and nonclinical populations and shows good psychometric properties (Creamer et al., 2003; Weiss, 2004), as in the current sample (αfor each time point = .95). A total score is calculated by summing items, ranging from 0 to 88, with scores above 33 indicating probable PTSD diagnoses (Creamer et al., 2003).
3.2. Data analytic plan
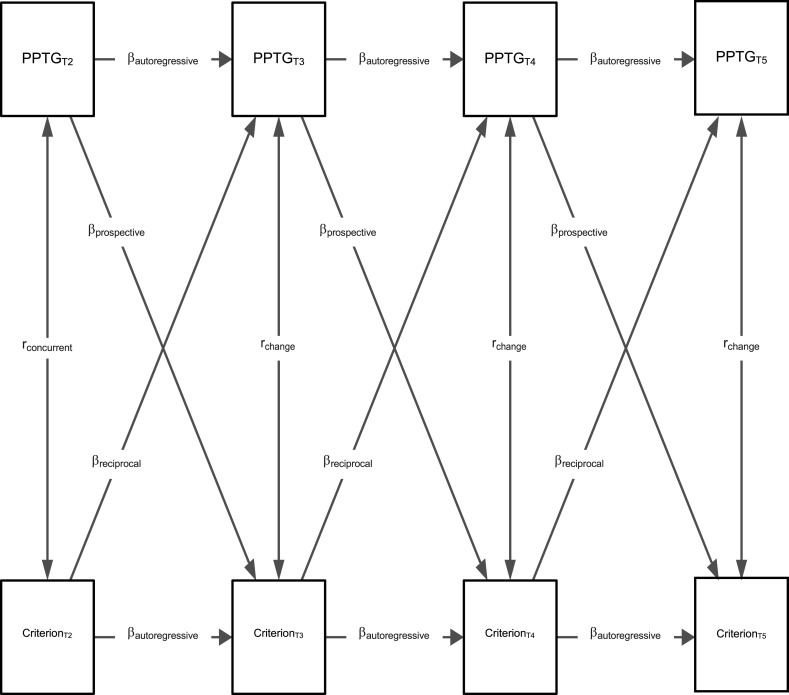
Analyses excluded Time 1 data because many of the key variables were only assessed at T2 onwards. After examining systematic attrition and computing descriptive statistics, we used the lavaan package (Rosseel, 2012) within R (R Core Team, 2021) to conduct six separate cross-lagged panel models (CLPMs) relating PPTG scale scores to each of the criterion variables described in the Measures subsection (see Fig. 1 ).1 Each CLPM estimated rank-order stability effects for each variable from T to T+1 (ß autoregressive), concurrent correlations at T2 (r concurrent), correlations of changes in scores over time at T3, T4, and T5 (r change), regressions of criterion variables at T+1 based on T (ß prospective), and reciprocal regressions of criterion variables at T on predictors at T+1 (ß reciprocal). Not shown in Fig. 1 (for the sake of simplicity) but estimated in the model were regressions for each variable from T+2 and T+3 on T. Stability and reciprocal effects were estimated. For example, PPTG and criterion variables at T4 were regressed on PPTG and criterion variables at T2. Therefore, all variables were related to each other and thus the models were fully saturated (i.e., χ 2 (0) = 0, p = 1.00). We treated the data as continuous and used maximum likelihood with robust standard errors (MLR) estimation. CLPMs handled missing data using full information maximum likelihood (FIML).
Fig. 1.
Conceptual representation of bivariate cross-lagged panel models.
Note. PPTG = Perceived Posttraumatic Growth scores. We estimated separate models for each of the 7 Criterion variables. Models estimated concurrent correlations at T2, autoregressive paths for each variable across time, correlations of change, prospective regression paths from PPTG to criterion variables, and reciprocal regression paths from outcome variables to predictors. To facilitate interpretation, the figure omits regressions of variables at T+2 and T+3 on T (e.g., PPTGT4 on PPTGT2).
4. Results
4.1. Participant description
The participants comprised male (n = 358, 42.6%) and female (n = 468, 55.6%) gender, with an additional 15 (1.8%) participants endorsing another choice (i.e.., non-binary, transgender, self-described, or prefer not to say). Participants were an average of 39.3 years old (SD = 14.15, range = 20–88) and primarily White (n = 683, 81.2%) and non-Hispanic/Latinx (n = 782, 93.0%). The sample included African-Americans (n = 105, 12.5%), Asian/Asian-Americans (n = 103, 12.0%), Native Hawaiian/Other Pacific Islanders (n = 41; 4.9%), and American Indian/Alaskan Natives (n = 52; 6.2%). Most participants identified as straight/heterosexual (n = 751, 87.3%); 3.9% identified as gay or lesbian (n = 33), 4.6% as bisexual (n = 39), and 2.1% preferred to self-describe or not say (n = 18). Most were married (n = 338, 40.2%) or single (n = 293, 34.8%); others were cohabiting with a significant other they were not married to (n = 119, 14.1%), divorced (n = 69, 8.2%), widowed (n = 14, 1.7%), or separated (n = 8, 1.0%). Nearly one-fourth (n = 197; 23.4%) reported being a caregiver in their home. Locations were reported across the US (as categorized into four distinct regions based on divisions used in the US Census (2020), n = 132, 19.6% in the Northeast; n = 127, 18.9% in the Midwest; n = 153, 22.7% in the West; and n = 261, 38.7% in the South).
4.2. Attrition/complete vs. incomplete data
To examine systematic attrition, we compared participants with complete PPTG data (n = 448; participants with data for PPTG at all timepoints from T2-T5) to participants who provided PPTG data at one to three time points (n = 389). Note that all participants were included in other analyses described below. Attrition analyses compared subgroups to determine whether dropout was dependent upon providing complete PPTG data. We compared participants on PPTG and all adjustment variables across time points. Independent groups t-tests showed that complete responders did not differ from incomplete responders on PPTG at any time point (ps > .05), but complete responders showed lower levels (ps < .05) of depression, anxiety, stress, and posttraumatic stress at each time point, as well as higher levels of PSOM at each time point. Thus, complete responders tended to have similar levels of PPTG but higher levels of mental health throughout the duration of the study.
4.3. Descriptive statistics
Mean item levels of PPTG and of the criterion variables at Time 2 are shown in Table 1 . Levels of PPTG were similar to that reported in other studies of PPTG during the pandemic (e.g., Ikizer et al., 2021).
Table 1.
Descriptive statistics for PPTG and criterion variables at baseline (T2).
| Variable | N | M | SD | skew | kurtosis |
|---|---|---|---|---|---|
| Perceived Posttraumatic Growth | 858 | 6.00 | 4.70 | 0.73 | −0.14 |
| Depression | 860 | 4.29 | 5.38 | 1.25 | 0.54 |
| Anxiety | 860 | 2.22 | 3.81 | 2.13 | 4.25 |
| Stress | 860 | 4.63 | 4.78 | 1.01 | 0.22 |
| Positive States of Mind | 666 | 22.46 | 4.77 | −0.71 | −0.13 |
| PTSD Symptoms | 822 | 17.06 | 16.08 | 1.23 | 1.34 |
| Days Consumed Alcohol in Past Month | 860 | 2.58 | 1.79 | 0.96 | −0.20 |
4.4. Cross-lagged panel models
Supplemental Table 1 shows estimates of stability. High stability was evidenced from T2 to T3 (30-day lag; β range = 0.71 to 0.85) and moderate-to-high stability was evidenced from T3 to T4 (30-day lag; β range = 0.38 to 0.65). Stability estimates over a 60-day lag (T2 to T4; β range = 0.26 to 0.50) and 90-day lag (T4 to T5; β range = 0.27 to 0.47) tended to be in the moderate range. Estimates over the longer lags of 120 days (T3 to T5; β range = 0.25 to 0.41) and 150 days (T2 to T5; β range = 0.10 to 0.31) were mostly moderate with some lower estimates as well. These results generally reflect an autoregressive structure, in which stability is higher over timepoints spaced more closely together.
Table 2 shows results pertaining to our hypotheses. The vast majority of results contradicted our hypotheses. Only two effects were statistically significant in the predicted direction: the concurrent association and T2 to T3 prospective association with PSOM. Finally, for completeness, Table 3 shows estimates of reciprocal effects from mental health variables to PPTG across one time point lags (apart from the positive associations between T3 PPTG and T2 anxiety and posttraumatic stress, no associations were statistically significant).2
Table 2.
Standardized path coefficients from cross-lagged panel models relevant to hypotheses relating perceived posttraumatic growth to criterion variables.
| Path |
Concurrent |
Correlation of Changes |
Prospective (T+1) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Association between Timepoints |
T2↔ T2 |
T3↔T3 |
T4↔T4 |
T5↔T5 |
T2→ T3 |
T3→T4 |
T4→T5 |
|||||||
| β | p | β | p | β | p | β | p | β | p | β | p | β | p | |
| Mental Health Variables | ||||||||||||||
| Depression | -.09 | .006 | -.05 | .28 | .00 | .97 | .01 | .81 | -.01 | .61 | .02 | .55 | -.01 | .72 |
| Anxiety | .17 | <.001 | .04 | .39 | .04 | .32 | .18 | .002 | .01 | .76 | .05 | .08 | -.01 | .73 |
| Stress | .06 | .13 | .00 | .97 | .09 | .07 | .04 | .39 | -.02 | .43 | .01 | .68 | .01 | .77 |
| Days Consumed Alcohol in Past Month | -.06 | .06 | -.02 | .69 | .04 | .44 | -.04 | .36 | -.02 | .29 | .02 | .51 | -.02 | .70 |
| Positive States of Mind | .17 | <.001 | .02 | .68 | -.10 | .10 | .06 | .21 | .07 | .04 | .03 | .48 | .06 | .24 |
| PTSD Symptoms | .20 | <.001 | .15 | <.001 | .10 | .01 | .07 | .11 | .05 | .05 | .02 | .63 | .05 | .18 |
Note. Column 1 is concurrent, columns 2–4 are correlation of changes, and columns 5–7 are prospective. Sample sizes for variables ranged from 552 to 860, which explains why similar β values sometimes had discrepant p-values.
Table 3.
Standardized path coefficients from cross-lagged panel models for T+1 reciprocal effects.
| Path |
Reciprocal (T+1) |
|||||
|---|---|---|---|---|---|---|
| Association between Timepoints |
T2→T3 |
T3→T4 |
T4→T5 |
|||
| β | p | β | p | β | p | |
| Depression | .02 | .50 | .01 | .86 | .09 | .13 |
| Anxiety | .08 | .01 | .07 | .15 | .03 | .72 |
| Stress | .04 | .18 | .03 | .30 | .07 | .30 |
| Days Consumed Alcohol in Past Month | -.01 | .88 | .04 | .43 | -.09 | .12 |
| Positive States of Mind | .03 | .19 | .01 | .85 | -.07 | .37 |
| PTSD Symptoms | .07 | .01 | -.02 | .63 | .09 | .08 |
5. Discussion
Overall, participants reported moderately high levels of PPTG at each time point; these levels of PPTG are fairly consistent with those previously reported in various samples during the Covid pandemic (e.g., Vasquez et al., 2021) as well as other samples dealing with other types of stressful or traumatic situations (Helgeson et al., 2006). Our longitudinal design allowed us to repeatedly measure PPTG in a fairly large group of participants dealing with a stressful situation. Although some change in PPTG was apparent over time, its rank-order stability was high at timepoints spaced 30 days apart and tended to be moderate over 60- and 90-day lags, suggesting that a substantial component of PPTG is stable. To date, relatively little research has assessed PPTG over time with the same event, so little is known about this aspect of PPTG, which may represent either stability in growth assessed at many time points or a traitlike tendency to report growth. Our findings suggest that this aspect may be an important direction for future work to better understand the nature of PPTG.
Contrary to some previous literature linking PPTG to better adjustment in community-wide disasters, however, we found little evidence that PPTG was related to better subsequent psychological adjustment or wellbeing. Even at our baseline (T2), while higher PPTG related to lower depression and amount of alcohol consumed and higher positive states of mind, it was also associated with more anxiety and PTSS, and was unrelated to stress, or days of drinking. These cross-sectional findings are consistent with the mixed cross-sectional findings that studies have reported in which PPTG may relate to some aspects of doing well (e.g., depression) but is typically related to higher PTSS as well (Helgeson et al., 2006).
In terms of our primary research question, we found virtually no evidence that PPTG related favorably to subsequent wellbeing (in only 1 of 24 comparisons, with higher PPTG at previous timepoint related to subsequent higher levels of positive states of mind at T3; at this timepoint as well, however, PPTG was also related to higher PTSS). Based on previous research, these findings are perhaps unsurprising in that longitudinal studies have reported highly inconsistent results, with some studies reporting salutary longitudinal relations (e.g., lower subsequent distress; Chen et al., 2015), while others report the opposite (e.g., Engelhard et al., 2015; Zalta et al., 2017). On the other hand, these findings may be surprising in the stark lack of relations—either favorable or unfavorable.
One explanation for the lack of associations may be due to a somewhat traitlike nature of PPTG, which would render it relatively unrelated to fluctuations in adjustment measures. In addition, PPTG is often considered a form of reappraisal or self-enhancement coping (Zoellner and Maercker, 2006; Finkelstein-Fox et al., 2020) and there was some evidence that PPTG might be functioning as coping in our sample. Specifically, there were more significant relationships for reverse direction effects that indicated distress predicting subsequent PPTG than vice-versa. These correlations of change across time periods show that increasing PTSS was associated with increasing PPTG at all three subsequent time points, while T2 to T3 increased anxiety predicted subsequent increased PPTG. Further, increased PPTG from T3 to T4 was related to lower subsequent positive states of mind and increased PPTG from T4 to T5 was related to more subsequent anxiety. Thus, PPTG may have served a coping role for some participants when feeling particularly distressed by allowing them to focus on perceived benefits that served as a coping mechanism but did not have actual substance or impact on mental health (Tennen and Affleck, 2002).
We included a range of adjustment outcomes including general and COVID-19-specific measures, positive and negative measures, and psychological and substance-use indicators to broadly characterize wellbeing; thus, the general lack of associations appears pervasive across domains of psychological adjustment to COVID-19. The potential for associations of PPTG with less substance use and misuse has been examined in only a few prior studies, with promising findings (e.g., Arpawong et al., 2015, 2016; McDiarmid et al., 2017). Thus, given high levels of alcohol use and misuse widely reported on from multiple studies during the pandemic (e.g., Pollard et al., 2020), and considering the high rates of heavy drinking in this sample (e.g., Fendrich et al., 2021), the lack of relations of PPTG and alcohol use found here are particularly disappointing.
Limitations of the current study must be noted. Our sample of MTurk workers do not comprise a nationally representative sample of Americans, although they are a useful group in which to model trends and associations (Walters et al., 2018). Our attrition analyses indicated that our sample of completers had higher levels of mental health than those participants who missed some assessment timepoints. This result is consistent with other results pertaining to mental health and attrition and may be due to people with lower levels of mental health finding the study to be too burdensome to complete on top of their emotional difficulties (Graaf et al., 2000). Though it is theoretically plausible that attrition would affect associations, previous research shows this not to be the case (Saiepour et al., 2019). Thus, we are confident that our results generalize reasonably well across levels of mental health.
As is true for all observation studies, our longitudinal design, while allowing some modeling of temporal ordering, does not allow for determining causality. The PPTG measure used here was a shortened version and although its psychometric properties were good, use of the full PTGI or other measures of PPTG might have resulted in different findings. In addition, the generalizability of these results to stressful situations outside of the COVID-19 pandemic is unclear. Because the PPTG assessed here referenced the pandemic broadly, it is unclear what specific difficult circumstances (e.g. marital problems) respondents might be referring to when responding.
In spite of these limitations, the present study advances our understanding of PPTG and wellbeing in a national sample of Americans during a community-wide—in this case, worldwide---disaster by repeatedly examining associations of these constructs, revealing a general lack of association. At least with regard to living through a pandemic, perceiving one has grown as a result of it does not lead to feeling less distressed or enhance one's wellbeing. Instead, it appears that PPTG is in large part stable and perhaps even traitlike, and that it may also serve as a coping function, as described in previous work (e.g., Infurna and Jayawickreme, 2019). These findings suggest that interventions to promote PPTG (e.g., Roepke et al., 2018; Ye et al., 2018) may be premature or misguided in that the value of PPTG remains unclear. Future work is needed to discern the meaning and importance of PPTG vis-à-vis wellbeing and adjustment to highly stressful situations.
Funding
This study was funded by support from the National Institute of Alcohol and Alcoholism (1R34AA027455, PIs: Park, Fendrich, Russell) and a Covid-19 Seed Grant from UCONN Institute for Collaboration on Health, Intervention, and Policy (PIs: Park, Fendrich, Russell).
Contributors
All authors have approved the final article in its current form.
The current work is part of a larger study of Covid-19 resilience.
CLP, BSR and MRF, developed the initial concept and design of the study.
CLP conducted the literature searches and wrote the first draft of the manuscript.
JW designed and conducted statistical analysis and wrote results.
All authors reviewed and edited drafts of the paper.
Declaration of competing interest
The authors report no conflicts of interest with the content of the manuscript. The content of this manuscript does not necessarily reflect the views of the funding agencies and reflects the views of the authors.
Acknowledgements
None.
Footnotes
In the preregistration, we specified a plan for conducting bivariate latent autoregressive models (BLAMs) relating PPTG latent variables (defined by the 5 items from the adapted PTGI) to latent variables composed of items from the multi-item criterion measures. We also planned to relate the PPTG latent variables to the three separate, one-item variables assessing alcohol use. These models estimated identical paths to those in the CLPMs presented herein with the exception of stability paths across more than one time point (i.e., the BLAMs had a true autoregressive structure). However, BLAMs imposing longitudinal measurement invariance constraints across timepoints (for item loadings, intercepts, and residuals) did not achieve good fits to the data. The configural models allowing item loadings to vary across timepoints did achieve good fit statistics, but we opted to present results at the scale level over the configural models because: (a) most researchers will use scale scores rather than latent variables when modeling these variables, and (b) the latent constructs in the configural models are slightly different conceptually across timepoints, which may complicate interpretation and reduce replicability of the findings. Further, substantive interpretation of results did not differ across the two analytical methods, with one possible exception. In the BLAMs, stability estimates from T to T+1 all tended to be high (pT to T+1 > 0.70). This discrepancy was likely due to excluding stability paths across more than one time point.
These analyses were conducted a second time to include age and gender as covariates and results were essentially unchanged.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.12.040.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Arditte K.A., Çek D., Shaw A.M., Timpano K.R. The importance of assessing clinical phenomena in Mechanical Turk Research. Psychol. Assess. 2016;28(6):684–691. doi: 10.1037/pas0000217. [DOI] [PubMed] [Google Scholar]
- Arpawong T.E., Sussman S., Milam J.E., Unger J.B., Land H., Sun P., Rohrbach L.A. Psychol. Health. 2015;30(4):475–494. doi: 10.1080/08870446.2014.979171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpawong T.E., Rohrbach L.A., Milam J.E., Unger J.B., Land H., Sun P., Spruijt-Metz D., Sussman S. Stressful life events and predictors of post-traumatic growth among high-risk early emerging adults. J. Posit. Psychol. 2016;11(1):1–14. doi: 10.1080/17439760.2014.994223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartneck C., Duenser A., Moltchanova E., Zawieska K., Voracek M. Comparing the similarity of responses received from studies in Amazon's Mechanical Turk to studies conducted online and with direct recruitment. PLoS One. 2015;10(4):1–23. doi: 10.1371/journal.pone.0121595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley K.A., Bush K.R., Epler A.J., Dobie D.J., Davis T.M., Sporleder J.L., Kivlahan D.R. Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT): validation in a female veterans affairs patient population. Arch. Intern. Med. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Büssing A., Rodrigues Recchia D., Hein R., Dienberg T. Perceived changes of specific attitudes, perceptions and behaviors during the Corona pandemic and their relation to wellbeing. Health Qual. Life Outcome. 2020;18:374. doi: 10.1186/s12955-020-01623-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CasellasGrau A., Ochoa C., Ruini C. Psychological and clinical correlates of posttraumatic growth in cancer: a systematic and critical review. Psycho Oncol. 2017;26(12):2007–2018. doi: 10.1002/pon.4426. [DOI] [PubMed] [Google Scholar]
- Chen J., Zhou X., Zeng M., Wu X. Post-traumatic stress symptoms and post-traumatic growth: evidence from a longitudinal study following an earthquake disaster. PLoS One. 2015;10(6) doi: 10.1371/journal.pone.0127241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Sun C., Chen J.‐J., Jen H.‐J., Kang X.L., Kao C.‐C., Chou K.‐R. A large‐scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID‐19 Pandemic. Int. J. Ment. Health Nurs. 2021;30:102–116. doi: 10.1111/inm.12796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the impact of event scale-revised. Behav. Res. Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Eisma M.C., Lenferink L.I., Stroebe M.S., Boelen P.A., Schut H.A. No pain, no gain: cross-lagged analyses of posttraumatic growth and anxiety, depression, posttraumatic stress and prolonged grief symptoms after loss. Hist. Philos. Logic. 2019;32(3):231–243. doi: 10.1080/10615806.2019.1584293. [DOI] [PubMed] [Google Scholar]
- Engelhard I.M., Lommen M.J., Sijbrandij M. Changing for better or worse? Posttraumatic growth reported by soldiers deployed to Iraq. Clin. Psychol. Sci. 2015;3(5):789–796. [Google Scholar]
- Fendrich M., Becker J., Park C., Russell B., Finkelstein-Fox L., Hutchison M. Associations of alcohol, marijuana, and polysubstance use with non-adherence to COVID-19 public health guidelines in a US sample. Subst. Abuse. 2021;42(2):220–226. doi: 10.1080/08897077.2021.1891603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein-Fox L., Park C.L., Kalichman S.C. Health benefits of positive reappraisal coping among people living with HIV/AIDS: a systematic review. Health Psychol. Rev. 2020;14(3):394–426. doi: 10.1080/17437199.2019.1641424. [DOI] [PubMed] [Google Scholar]
- Graaf R.D., Bijl R.V., Smit F., Ravelli A., Vollebergh W.A. Psychiatric and sociodemographic predictors of attrition in a longitudinal study The Netherlands mental health survey and incidence study (NEMESIS) Am. J. Epidemiol. 2000;152(11):1039–1047. doi: 10.1093/aje/152.11.1039. [DOI] [PubMed] [Google Scholar]
- HamamaRaz Y., Pat‐Horenczyk R., Roziner I., Perry S., Stemmer S.M. Can posttraumatic growth after breast cancer promote positive coping?—a cross‐lagged study. Psycho Oncol. 2019;28(4):767–774. doi: 10.1002/pon.5017. [DOI] [PubMed] [Google Scholar]
- Helgeson V.S., Reynolds K.A., Tomich P.L. A meta-analytic review of benefit finding and growth. J. Consult. Clin. Psychol. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Horowitz M., Adler N., Kegeles S. A scale for measuring the occurrence of positive states of mind: a preliminary report. Psychosom. Med. 1988;50(5):477–483. doi: 10.1097/00006842-198809000-00004. [DOI] [PubMed] [Google Scholar]
- Ikizer G., Karanci A.N., Gul E., Dilekler I. Post-traumatic stress, growth, and depreciation during the COVID-19 pandemic: evidence from Turkey. Eur. J. Psychotraumatol. 2021;12(1):1872966. doi: 10.1080/20008198.2021.1872966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna F.J., Jayawickreme E. Fixing the growth illusion: new directions for research in resilience and posttraumatic growth. Curr. Dir. Psychol. Sci. 2019;28(2):152–158. [Google Scholar]
- Kim H.S., Hodgins D.C. Reliability and validity of data obtained from alcohol, cannabis, and gambling populations on Amazon's Mechanical Turk. Psychol. Addict. Behav. 2017;31:85–94. doi: 10.1037/adb0000219. [DOI] [PubMed] [Google Scholar]
- Koliouli F., Canellopoulos L. Dispositional optimism, stress, post-traumatic stress disorder and post-traumatic growth in Greek general population facing the COVID-19 crisis. Eur. J. Trauma Dissociation. 2021 doi: 10.1016/j.ejtd.2021.100209. 100209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalski R.M., Carroll H., Britt J. Finding the silver lining in the COVID-19 crisis. J. Health Psychol. 2021 doi: 10.1177/1359105321999088. 1359105321999088. [DOI] [PubMed] [Google Scholar]
- Lang A. CAIR (Complementary and Integrative Research Lab) Pandemic Impact Questionnaire (C-PIQ) 2020. https://www.nlm.nih.gov/dr2/COVID-19_BSSR_Research_Tools.pdf
- Li L., Mao M., Wang S., Yin R., Yan H.O., Jin Y., Cheng Y. Posttraumatic growth in Chinese nurses and general public during the COVID-19 outbreak. Psychol. Health Med. 2021:1–11. doi: 10.1080/13548506.2021.1897148. [DOI] [PubMed] [Google Scholar]
- Liu A.N., Wang L.L., Li H.P., Gong J., Liu X.H. Correlation between posttraumatic growth and posttraumatic stress disorder symptoms based on Pearson correlation coefficient: a meta-analysis. J. Nerv. Ment. Dis. 2017;205(5):380–389. doi: 10.1097/NMD.0000000000000605. [DOI] [PubMed] [Google Scholar]
- Long L.J., Phillips C.A., Glover N., Richardson A.L., D'Souza J.M., Cunningham-Erdogdu P., Gallagher M.W. A meta-analytic review of the relationship between posttraumatic growth, anxiety, and depression. J. Happiness Stud. 2021:1–26. doi: 10.1037/bul0000173. [DOI] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Mangelsdorf J., Eid M., Luhmann M. Does growth require suffering? A systematic review and meta-analysis on genuine posttraumatic and postecstatic growth. Psychol. Bull. 2019;145(3):302–338. doi: 10.1037/bul0000173. [DOI] [PubMed] [Google Scholar]
- McDiarmid L., Taku K., Phillips M. Posttraumatic growth associated with perceived changes in health values and reduced alcohol use among bereaved college students. Traumatology. 2017;23(4):309–316. doi: 10.1037/trm0000120. [DOI] [Google Scholar]
- Mortensen K., Hughes T.L. Comparing Amazon's Mechanical Turk platform to conventional data collection methods in the health and medical research literature. J. Gen. Intern. Med. 2018;33:533–538. doi: 10.1007/s11606017-4246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ophir Y., Sisso I., Asterhan C., Tikochinski R., Reichart R. The Turker blues: hidden factors behind increased depression rates in Amazon's Mechanical Turk. Clin. Psychol. Sci. 2020;8:65–83. doi: 10.1177/2167702619865973. [DOI] [Google Scholar]
- Park C.L. In: Positive Life Change in the Context of Medical Illness: Can the Experience of Serious Illness Lead to Transformation? Park C.L., Lechner S., Antoni M.H., Stanton A, editors. American Psychological Association; Washington, DC: 2009. Overview of theoretical perspectives; pp. 11–30. [Google Scholar]
- Park C.L., Blake E.B. In: Positive Psychological Approaches to Disaster: Meaning, Resilience, and Posttraumatic Growth. Schulenberg S.E., editor. Springer; New York, NY: 2020. Resilience and recovery following disasters: the meaning making model; pp. 9–25. [Google Scholar]
- Pietrzak R.H., Tsai J., Southwick S.M. Association of symptoms of posttraumatic stress disorder with posttraumatic psychological growth among US veterans during the COVID-19 Pandemic. JAMA Netw. Open. 2021;4(4) doi: 10.1001/jamanetworkopen.2021.4972. e214972-e214972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.22942. e2022942-e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PrietoUrsúa M., Jódar R. Finding meaning in hell. The role of meaning, religiosity and spirituality in posttraumatic growth during the coronavirus crisis in Spain. Front. Psychol. 2020;11:567836. doi: 10.3389/fpsyg.2020.567836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing. 2021. R: a language and environment for statistical computing.http://www.R-project.org [Google Scholar]
- Ramos C., Costa P.A., Rudnicki T., Marôco A.L., Leal I., Guimarães R., Tedeschi R.G. The effectiveness of a group intervention to facilitate posttraumatic growth among women with breast cancer. Psycho Oncol. 2018;27(1):258–264. doi: 10.1002/pon.4501. [DOI] [PubMed] [Google Scholar]
- Roepke A.M., Benson L., Tsukayama E., Yaden D.B. Prospective writing: Randomized controlled trial of an intervention for facilitating growth after adversity. J. Posit. Psychol. 2018;13(6):6. [Google Scholar]
- Rosseel Y. lavaan: an R Package for structural equation modeling. J. Stat. Software. 2012;48(2):1–36. [Google Scholar]
- Saiepour N., Najman J.M., Ware R., Baker P., Clavarino A.M., Williams G.M. Does attrition affect estimates of association: a longitudinal study. J. Psychiatr. Res. 2019;110:127–142. doi: 10.1016/j.jpsychires.2018.12.022. [DOI] [PubMed] [Google Scholar]
- Schmits E., Glowacz F. Changes in alcohol use during the COVID-19 pandemic: impact of the lockdown conditions and mental health factors. Int. J. Ment. Health Addiction. 2021:1–12. doi: 10.1007/s11469-020-00432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert C.F., Schmidt U., Rosner R. Posttraumatic growth in populations with posttraumatic stress disorder—a systematic review on growth‐related psychological constructs and biological variables. Clin. Psychol. Psychother. 2016;23(6):469–486. doi: 10.1002/cpp.1985. [DOI] [PubMed] [Google Scholar]
- Shand L.K., Cowlishaw S., Brooker J.E., Burney S., Ricciardelli L.A. Correlates of post‐traumatic stress symptoms and growth in cancer patients: a systematic review and meta‐analysis. Psycho Oncol. 2015;24(6):624–634. doi: 10.1002/pon.3719. [DOI] [PubMed] [Google Scholar]
- Sheehan K.B., Pittman M. Melvin & Leigh; Irvine, CA: 2016. Amazon's Mechanical Turk for Academics: the HIT Handbook for Social Science Research. [Google Scholar]
- Stallard P., Pereira A.I., Barros L. Post-traumatic growth during the COVID-19 pandemic in carers of children in Portugal and the UK: cross-sectional online survey. BJPsych Open. 2021;7(1):e37. doi: 10.1192/bjo.2021.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taku K., Tedeschi R.G., Shakespeare-Finch J., Krosch D., David G., Kehl D., et al. Posttraumatic growth (PTG) and posttraumatic depreciation (PTD) across ten countries: global validation of the PTG-PTD theoretical model. Pers. Indiv. Differ. 2021;169:110222. [Google Scholar]
- Tedeschi R.G., Calhoun L.G. The posttraumatic growth inventory: Measuring the positive legacy of trauma. J. Trauma Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Tedeschi R.G., Shakespeare-Finch J., Taku K., Calhoun L.G. Routledge; New York: 2018. Post-traumatic Growth: Research, Theory, and Applications. [Google Scholar]
- Tennen H., Affleck G. In: Handbook of Positive Psychology. Snyder C.R., Lopez S.J., editors. Oxford University Press; London, Tucker: 2002. Benefit-finding and benefit-reminding; pp. 584–597. [Google Scholar]
- Uziel N., Gilon E., Meyerson J., Levin L., Khehra A., Emodi-Perlman A., Eli I. Dental personnel in Israel, Canada, and France during the COVID-19 pandemic: attitudes, worries, emotional responses, and posttraumatic growth. Quintessence Int. 2021:444–453. doi: 10.3290/j.qi.b936999. [DOI] [PubMed] [Google Scholar]
- Vazquez C., Valiente C., García F.E., Contreras A., Peinado V., Trucharte A., Bentall R.P. Post-traumatic growth and stress-related responses during the COVID-19 pandemic in a national representative sample: the role of positive core beliefs about the world and others. J. Happiness Stud. 2021;1–21 doi: 10.1007/s10902-020-00352-3. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters K., Christakis D.A., Wright D.R. Are Mechanical Turk worker samples representative of health status and health behaviors in the US? PLoS One. 2018;13(6) doi: 10.1371/journal.pone.0198835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1–25. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D.S. In: Assessing Psychological Trauma and PTSD: A Practitioner's Handbook. second ed. Wilson J.P., Keane T.M., editors. Guilford; New York: 2004. The impact of event scale - revised; pp. 168–189. [Google Scholar]
- Weiss D.S., Marmar C.R. In: Assessing Psychological Trauma and PTSD. Wilson J.P., Keane T.M., editors. Guilford; New York: 1997. The impact of event scale-revised; pp. 399–411. [Google Scholar]
- Ye Z., Yu N.X., Zhu W., Chen L., Lin D. A randomized controlled trial to enhance coping and posttraumatic growth and decrease posttraumatic stress disorder in HIV-infected men who have sex with men in Beijing, China. AIDS Care. 2018;30(6):793–801. doi: 10.1080/09540121.2017.1417534. [DOI] [PubMed] [Google Scholar]
- Yu Y., Yu Y., Hu J. COVID-19 among Chinese high school graduates: psychological distress, growth, meaning in life and resilience. J. Health Psychol. 2021 doi: 10.1080/10615806.2016.1229467. 1359105321990819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta A.K., Gerhart J., Hall B.J., Rajan K.B., Vechiu C., Canetti D., Hobfoll S.E. Self-reported posttraumatic growth predicts greater subsequent posttraumatic stress amidst war and terrorism. Hist. Philos. Logic. 2017;30(2):176–187. doi: 10.1080/10615806.2016.1229467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner T., Maercker A. Posttraumatic growth in clinical psychology—a critical review and introduction of a two component model. Clin. Psychol. Rev. 2006;26:626–653. doi: 10.1016/j.cpr.2006.01.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.