Abstract
Histopathological features are important for the practicing hair transplant surgeon to ensure proper case selection, diagnosis, choice of proper treatment, and successful outcome. While the primary focus of the hair transplant surgeon is androgenetic alopecia (AGA), it is important to be aware of other conditions that can mimic AGA, whose treatment may be different. This article outlines some of these conditions such as scarring alopecias, alopecia areata, etc., and how to distinguish them. Proper identification will ensure proper treatment and avoid potential missteps in management.
Keywords: Alopecia, histopathology, Hair follicle, Androgenetic alopecia
Introduction
Alopecias are a complicated subject clinically and histologically, as it involves multiple variations. 1 The recent advent of dermoscopy has provided a simple and valuable bedside tool for diagnosis. However, scalp biopsies provide a basis for confirmation of definitive diagnoses and thereby help in management. The hair transplantation surgeon needs to understand the simulators of androgenetic alopecia (AGA), their clinical and histological features, biopsy procedure, clinicopathological correlation, and prognosis to ensure satisfactory outcome after surgery.
The objective is to give a brief outline of relevant entities to the hair transplant surgeon and an algorithmic approach to the diagnosis of these conditions.
Normal Hair Anatomy and Hair Cycle
Two types of hair are present in adult humans: Vellus hair which is the short fine brown hair present all over the body, and terminal hair, which is the thick black hair present on the scalp, face, chest, pubic area, etc. 2 Terminal hairs become clinically vellus type after miniaturization in AGA, but still differ histologically from the true vellus hairs in having an arrectores pilorum muscle.
Normal hair follicle ( Fig. 1 ) consists of three segments: infundibulum (above the attachment of sebaceous gland), isthmus (between the attachments of sebaceous gland and arrectores muscle), and the inferior segment (below the attachment of arrectores muscle). Each hair undergoes a cycle with three phases ( Table 1 ): anagen, catagen hair, and telogen hair. During catagen phase, the inferior segment disappears to regrow again during anagen. Thus, the inferior segment is temporary and is loosely attached to the surrounding tissue. The stem cells are located largely in the bulge, the site of attachment of the arrectores muscle. These facts are of importance in the logic of follicular unit excision (FUE). The normal scalp has 90% of hairs in the anagen phase (anagen to a nonanagen ratio of 9:1). Duration of hair cycle varies from one area to another, such as scalp, beard, and body, and this knowledge is essential in nonscalp donor harvesting in hair transplant.
Fig. 1.
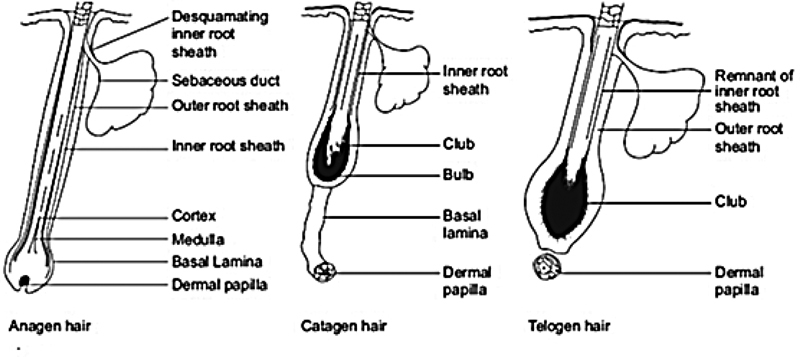
Normal hair anatomy and hair cycle
Table 1. Histological changes during different stages of hair cycle.
| Feature | Anagen | Catagen | Telogen |
|---|---|---|---|
| Location of root | Lower dermis | Mid/lower dermis | Mid/upper dermis |
| Root | Bulbous, fully formed | Small | Club-shaped |
| Pigmentation of root | Pigmented | No melanocytes | No melanocytes |
| Inferior segment | Present | Replaced by epithelial cord | Replaced by fibrous cord |
| Mitotic figures | Present | Absent | Absent |
| Colloid bodies | Absent | Present | Absent |
| Vitreous sheath | Absent | Thick | Absent |
| Dermal papilla | Large, flame-shaped | Small | small |
Scalp Biopsy
Recent advent of trichoscopy as a reliable simpler outpatient tool has somewhat decreased the need for more invasive scalp biopsy . However, scalp is still very useful in several situations mentioned below. Therefore, it is essential to know all aspects of a biopsy: when to do it, how to do it, where to do it, how to send biopsy, etc.
Indications
a) Female pattern hair loss versus chronic telogen effluvium (TE).
b) Chronic diffuse alopecia areata in men versus male pattern hair loss (MPHL).
c) Lymphocytic scarring alopecias, particularly frontal fibrosing alopecia.
d) Some cases of trichotillomania.
e) Growths.
f) Medicolegal purpose before hair transplant to assess activity in cicatricial alopecia or longstanding alopecia areata.
Scalp biopsy technique: Scalp biopsy is a simple outpatient procedure under local anesthesia. 3 The biopsy needs to be a deep biopsy, extending to subcutis, to include terminal hair bulbs. Adequate amount of lignocaine with adrenaline is needed to ensure tumescence and vasoconstriction, in order to prevent bleeding during surgery. The biopsy can either be a punch or incisional biopsy and should be of 4 to 6 mm width (which has 20–40 hair follicles/10–12 units).
The site of biopsy should be the active part of the lesion, as old residual areas of alopecia may not show typical histology. Hence, biopsy from the edge of the lesion, which still has hairs, is preferred and not from the central atrophic area. The biopsy should be performed with the punch oriented parallel to the direction of hair growth, in order to avoid transecting the hair. Two biopsies are needed, one for horizontal sections and the other for vertical sections. A third biopsy may be needed if direct immunofluorescence (DIF) is planned to distinguish discoid lupus erythematosus from pseudopelade and lichen plano pilaris.
Hematoxylin and eosin are the primary stains. Elastic tissue stains, periodic acid-Schiff (PAS), and mucin stains are optional.
A biopsy allows both qualitative interpretation (morphology of follicles, inflammation, fibrosis, etc.) and quantitative information (no. of units, number of hairs). Much of this data can only be obtained from transverse sections.
Importance of Transverse Sections (Horizontal Sectioning)
Headington, in a landmark paper in 1984, demonstrated the value of transverse sectioning of biopsies in alopecias. 4 The technique has the following advantages:
Gives a better idea of hair follicle cycle dynamics, which is so relevant in nonscarring alopecias.
Allows measurement of follicle diameter with a micrometer.
Allows study of follicular units.
Helps calculate the hair density in a given area.
However, transverse sections have the following limitations: 5 6
Multiple levels have to be studied.
Are technically more difficult to section and need an experienced technician.
Epidermal changes are not well-appreciated. Hence, vertical sections are preferred for alopecia associated with epidermal changes, such as lupus erythematosus
Therefore, it is preferable to perform both types of sections for two biopsies.
The Follicular Unit
Headington demonstrated that hair follicles, sebaceous glands, arrectores pilorum muscle, and the surrounding connective tissue occur in specialized anatomical units known as follicular units. 4 The follicular unit consists of the following:
One to four terminal follicles.
One or, rarely, two vellus follicle(s).
Associated sebaceous lobules and insertions of the arrector pili.
Perifollicular vascular plexus and neural net.
Perifollicular collagen.
The follicular unit is pyramidal in shape, with hairs splaying at the inferior segment and narrowest at the isthmus, with arrectores holding the hairs together. The inferior segment is loosely held, and hence loosening the hold of arrectores loosens the unit. This concept of the follicular unit has become the cornerstone of recent hair transplantation techniques, both strip and excision techniques. It is remarkable that a histopathological concept has had so much impact on a cosmetic surgical technique. 7 8
Classification of Alopecias
Traditionally, alopecias have been classified into nonscarring and scarring types( Table 2 ). The classification is based on the presence or absence of hair follicle's destruction, as indicated by the presence or absence of the follicular ostia clinically and its replacement by fibrous tissue histologically. 9 This classification is of prognostic significance and nonscarring alopecias have poorer prognosis. Dermoscopy can help with not only identifying scarring but also in indicating the site for biopsy. 10
Table 2. Classification of alopecias.
| Nonscarring alopecias | Scarring alopecias |
|---|---|
| • Congenital alopecias • Premature catagen/telogen: TE • Premature telogen with anagen arrest (alopecia areata) • Vellus follicle formation (AGA) • Anagen effluvium • Hair shaft abnormalities |
A primary scarring alopecias: • Lymphocyte-mediated scarring alopecia: lichen planus, chronic cutaneous lupus erythematosus, pseudopelade, central centrifugal cicatricial alopecia, alopecia mucinosa, keratosis follicularis, and spinulosa decalvans. • Neutrophilic scarring alopecia: folliculitis decalvans and dissecting folliculitis. • Mixed: folliculitis keloidalis, folliculitis (acne) necrotica, and erosive pustular dermatosis. Secondary scarring alopecias: burns, injury, surgery, radiation etc. |
Abbreviations: AGA, androgenetic alopecia; TE, Telogen effluvium.
Among the entities which are listed above, the alopecias which can mimic AGA and are hence of importance to a hair transplant surgeon are as follows:
Chronic TE, particularly in women.
Alopecia areata, particularly the diffuse variant.
Traction alopecia and some cases of trichotillomania.
Frontal fibrosing alopecia.
Alopecia areata may also cause confusion with postoperative donor anagen effluvium after strip excision. These include primary scarring alopecias such as lichen plano pilaris, Pseudopelade, and discoid lupus erythematosus. A biopsy in these situations can help establish the histological activity of the disease and be considered medicolegally prudent if surgery is being planned.
Androgenic Alopecia ( Fig. 2 )
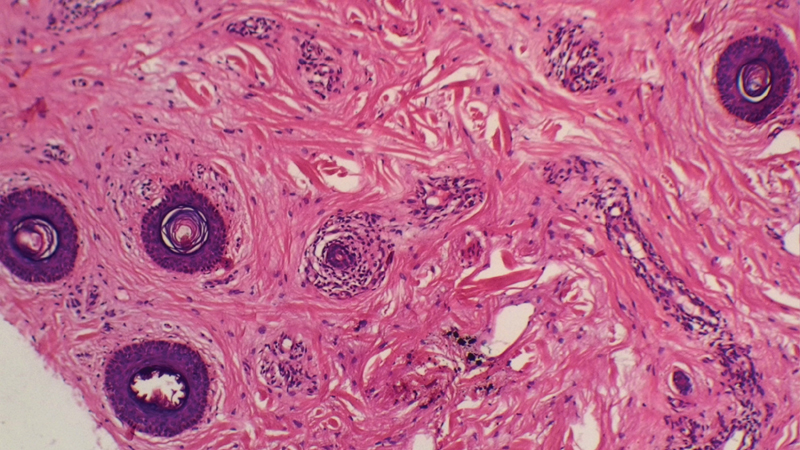
Fig. 2.

Androgenetic alopecia (AGA) showing multiple miniaturized follicles in middermis and a fibrous tract extending into subcutis. Note the oversized sebaceous glands.
With the increasing popularity of hair transplantation, particularly FUE with mega sessions, proper case selection has become paramount to achieving good results. Particularly diffuse types of AGA, which show miniaturization in the occipital area, is a challenge for both diagnosis and donor harvesting. 11
The hallmark of AGA is miniaturization, indicated by the presence of small bulbs of hairs located high in the upper dermis. As miniaturization progresses, the size of the hair progressively decreases, and the location of the hair bulb is shifted higher and higher in the dermis. The anagen to catagen ratio is reversed with many catagen and telogen hairs but fewer anagen hairs in the dermis. The presence of a thin vascular connective tissue streamer beneath the hair root, and absence of significant inflammatory infiltrate, are characteristic features. 11 Sebaceous glands appear large and out of proportion to the small miniaturized hair. 12
Telogen Effluvium
TE is a very common nonscarring alopecia almost always diagnosed clinically and through dermoscopy. However, chronic TE is sometimes difficult to differentiate from diffuse type of AGA, particularly in women, and hence may need a biopsy, particularly while planning transplantation.
Histology shows plenty of telogen follicles (reversal of anagen telogen ratio), which are identified by trichilemmal keratinization of the most proximal portion of the hair shaft, absence of miniaturization, and minimal inflammation. 13
Alopecia Areata ( Fig. 3 )
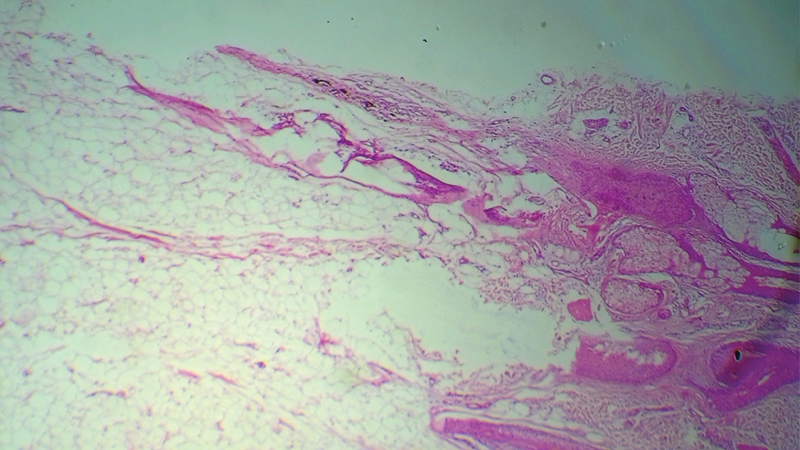
Fig. 3.

Alopecia areata showing hair follicle at the level of isthmus with lymphocytes surrounding the hair follicle with a fibrous tract beneath it (10 × ).
It is an autoimmune condition, histologically characterized by a dense lymphocytic infiltrate directed at the inferior segment of the anagen hair (referred to as swarm of bees appearance), ( Fig. 4 ), causing abrupt cessation of anagen, precipitate entry into catagen and rapid shedding. 14 15 Early lesions ( Figs 3 and 4 ) of alopecia areata are characterized by increased number of telogen hairs and presence of dystrophic anagen hair, which is seen as a small miniaturized hair with root in middermis just 2 mm below the epidermis, in contrast to normal anagen hair root, which is located 3.5 mm below epidermis. 14
Fig. 4.
Alopecia areata. Horizontal section of scalp at the level of sebaceous gland showing perifollicular lymphocytic infiltrate in a “swarm of bees appearance” (10 × ).
Late lesions show minimal infiltrate and many miniature hairs, which are anagen hairs that have been miniaturized by repeated episodes of inflammation and are referred to as nanogen hairs. At this stage, the condition may resemble AGA due to the presence of miniaturized hairs. However, the presence of small atrophic sebaceous glands, clumps of melanin (pigment casts) within the dermal papilla, and presence of eosinophils around the bulb and within the thin fibrous stellae are useful clues. 16 17 18
Trichotillomania ( Fig. 5 )
Fig. 5.
Trichotillomania showing damaged hair shaft and empty hair follicle (10 × ).
Trichotillomania is a condition characterized by repeated pulling of the hairs in stress-prone individuals, particularly young females. While clinical and dermoscopic diagnosis as seen by the presence of short stubs of broken hairs' different lengths in a localized patch is characteristic, biopsy is sometimes needed to confirm the diagnosis where history is unreliable. A similar entity is traction alopecia, often seen in the frontal area, which may cause confusion in diagnosis with AGA. The most important criterion for diagnosis is the evidence of damage to the hair follicle, which is demonstrated by a broken shaft, trichomalacia (softening or clumping of hair), ruptured hair follicles with clefts around hair follicles, hemorrhage around hair follicle, empty hair follicle, release of pigment into the surrounding dermis and in hair papilla, and increased number of telogen hairs 19 . Infiltrate of lymphocytes, although present, is mild. Hamburger sign, indicating vertically oriented split in the hair shaft containing proteinaceous material and erythrocytes, may also be seen. 20
Primary Scarring Alopecia or Cicatricial Alopecia
Primary scarring alopecias need to be recognized early, as the destruction of hair may be reversible by medical treatment. A biopsy is therefore useful in early diagnosis and prompt medical management. 21 Hair transplantation is not a routine treatment for this condition, but can be considered in a late stable lesion after careful counselling, clinicopathological coordination, and dermatological opinion.
Primary scarring alopecias were classified by Sperling ( Table 2 ), according to the predominant cell type (lymphocytic, neutrophilic, and mixed) 19 22 23 Histological features of destruction of hair follicle are common to all types of scarring alopecia and are as follows:
Hair follicle is destroyed, and it is replaced by a thick fibrous tract, which is avascular 23 This fibrous tract is different from fibrous stellae seen in AGA and alopecia areata, which appears as a thin loose collection of fine collagen fibers, with blood vessels at the site of hair follicle.
Remnants of hair follicles such as shaft are seen in early lesions and may be totally absent in late lesions. However, arrectores pilorum persists, even in late lesions, provide an important clue.
A foreign body giant cell reaction can often be seen around these remnants.
Elastic tissue fibers seen by Verrof Van Gieson stain (VVG) are destroyed.
Lymphocytic Scarring Alopecias
These include lichen plano pilaris, discoid lupus erythematosus, scleroderma, pseudopelade of Brocq, frontal fibrosing alopecia, and central centrifugal alopecia. 22 24 25 26 27 28 29 They all show varying degrees of lymphocytic infiltrate with or with out basal cell degeneration, which leads to destruction of the hair follicle. The degree of infiltrate can be a sign of histological activity. Of these conditions, only frontal fibrosing alopecia mimics AGA and is considered in detail.
Frontal Fibrosing Alopecia
This entity, occurring commonly in menopausal women, manifests with frontal alopecia, which strikingly mimics AGA . On close examination, there is mild scarring with dilated blood vessels. Even though clinical and dermoscopic features are fairly diagnostic, biopsy is needed and can be helpful in selected cases. 30 31 Biopsy shows a lichenoid histopathology characterized by dense inflammatory lymphocytic infiltrate involving the isthmus and infundibulum of the hair follicles, apoptotic cells in the external root sheath, and a concentric fibrosis surrounding the hair follicles. Association of frontal fibrosing alopecia (FFA) with lichen planus has also been reported 32 33 34 35 36
Other types of lymphocytic alopecia such as central centrifugal cicatricial alopecia and alopecia mucinosa are uncommon and are beyond the purview of this article. 37 38 39
Neutrophilic Scarring Alopecias
These are characterized by recurrent pustules, leading to the destruction of hairs. They are easily diagnosable clinically and managed mostly by medical modalities. However, surgical treatment may be needed for drainage of abscesses and excision of cysts. 40
Folliculitis Decalvans
This chronic condition is characterized by recurrent pustules and results in scarring and alopecia. There may be epidermal hyperkeratosis, follicular plugging, and evidence of tufting of hairs. The lesion shows polymorphonuclear cells within hair follicle, often as abscesses. 40 Dermis shows scarring, remnants of hair shafts surrounded by mixed inflammatory infiltrate of neutrophils, plasma cells and lymphocytes around appendages and foreign body giant cells.
A summary of histopathological findings of different types of alopecias is presented in Table 3 .
Table 3. Summary of findings in alopecias.
| Diseases | Important pathological features |
|---|---|
| Nonscarring alopecia: persistence of follicular ostia, absence of destruction, | |
| Alopecia areata | Lymphocytic infiltrate around hair bulbs (“swarm of bees”), dystrophic anagen |
| Trichotillomania | “Torn” catagen follicles ± hemorrhage, Hamburger sign, pigment cast |
| AGA | Miniaturization of hair, reversed anagen telogen ration, pauci-inflammatory |
| Chronic TE | Reversed anagen telogen ration, absence of infiltrate and miniaturization |
| Scarring alopecia: destruction of hair follicle with replacement by fibrous tract | |
| Lichen plano pilaris | Follicle replaced by fibrotic tract, follicular basal cell degeneration with dense lymphocytic infiltrate, apoptotic bodies, sparing of the intervening skin |
| Discoid lupus erythematosus | Perifollicular lymphocytic infiltrate, basal cell degeneration, follicular plugging, PAS + basement membrane thickening, dermal mucin |
| Scleroderma | Dense collagen, hyalinization of dermis and subcutaneous fat (pulled up appearance) |
| Pseudopelade of Brocq | Columns of fibrosis with persistent elastic fibers, mild infiltrate at isthmus |
| FFA | Follicular basal cell degeneration with dense lymphocytic infiltrate, few apoptotic bodies |
| Central centrifugal cicatricial alopecia | Premature desquamation of inner root sheath |
| Alopecia mucinosa | Vacuolate hair follicle (Alcian blue positive) |
| Folliculitis decalvans | Fibrosis with neutrophilic and lymphocytic infiltrate |
Abbreviations: AGA, androgenic alopecia; FFA, frontal fibrosing alopecia; PAS, periodic acid-Schiff; TE, telogen effluvium.
Approach to Diagnosis of Alopecias
Diagnosis of alopecias is complex and needs a multifaceted approach of thorough clinical examination, trichoscopy, histopathology, and clinicopathological correlation to obtain satisfactory results. 41 42 The hair transplant surgeon should not hesitate to consult a dermatologist in all doubtful cases. Any interpretation of skin biopsy in alopecia should answer the following questions:
Is it scarring or nonscarring alopecia?
If nonscarring, which type?
If scarring, which type?
Is there a possibility of hair growth?
Can surgery be done?
While the first three questions can be answered with certainty, the last need consideration of several factors, including duration of disease, previous clinical course, precise diagnosis, previous treatment and duration of treatment, need for future treatment of the primary condition, emotional needs of the patient, and histopathological assessment of the stability of the condition.
The algorithmic approach is a simplified diagnostic approach popularized by Ackerman, shown in Figs. 6 and 7 43
Fig. 6.

Algorithm for the diagnosis of nonscarring alopecias.
Fig. 7.

Algorithm showing approach to scarring alopecias. Reproduced from Mysore V. Fundamentals of Pathology of Skin. 4th ed. Wolters Kluwer: Delhi; 2012
Summary
Proper diagnosis of alopecias needs a multifaceted approach of thorough clinical examination, trichoscopy, histopathology, and proper clinicopathological correlation. This is particularly important as hair transplantation is sought for many of these cases. The hair transplant surgeon should be aware of these conditions.
Acknowledgment
The authors wish to acknowledge the role of Dr. Arpitha Argya, MD and Dr Pooja K, MD, for her help in copy editing
Funding Statement
Funding None declared.
Footnotes
Conflicts of Interest None declared.
References
- 1.Yeliur I K, Tirumalae R. Histopathologic approach to alopecia. Indian Journal of Dermatopathology and Diagnostic Dermatology. 2018;5(02):79. [Google Scholar]
- 2.Mysore V.Chapter 2. Fundamentals of Pathology of Skin 4th ed.Delhi: Wolters Kluwer; 2012:6–20 [Google Scholar]
- 3.Knopp E. The scalp biopsy for hair loss and its interpretation. Semin Cutan Med Surg. 2015;34(02):57–66. doi: 10.12788/j.sder.2015.0144. [DOI] [PubMed] [Google Scholar]
- 4.Headington J T. Transverse microscopic anatomy of the human scalp. A basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120(04):449–456. [PubMed] [Google Scholar]
- 5.Solomon A R.The transversely sectioned scalp biopsy specimen: the technique and an algorithm for its use in the diagnosis of alopecia Adv Dermatol 19949127–157., discussion 158 [PubMed] [Google Scholar]
- 6.Böer A, Hoene K. Transverse sections for diagnosis of alopecia? Am J Dermatopathol. 2005;27(04):348–352. doi: 10.1097/01.dad.0000154398.60712.11. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein R M, Rassman W R.The logic of follicular unit transplantation Dermatol Clin 19991702277–295., viii, discussion 296 [DOI] [PubMed] [Google Scholar]
- 8.IADVL Dermatosurgery Task Force Patwardhan N, Mysore V.Hair transplantation: standard guidelines of care Indian J Dermatol Venereol Leprol 200874(Suppl):S46–S53. [PubMed] [Google Scholar]
- 9.Sellheyer K, Bergfeld W F. Histopathologic evaluation of alopecias. Am J Dermatopathol. 2006;28(03):236–259. doi: 10.1097/00000372-200606000-00051. [DOI] [PubMed] [Google Scholar]
- 10.Miteva M, Tosti A. Dermoscopy guided scalp biopsy in cicatricial alopecia. J Eur Acad Dermatol Venereol. 2013;27(10):1299–1303. doi: 10.1111/j.1468-3083.2012.04530.x. [DOI] [PubMed] [Google Scholar]
- 11.Ekmekci T R, Sakiz D, Koslu A. Occipital involvement in female pattern hair loss: histopathological evidences. J Eur Acad Dermatol Venereol. 2010;24(03):299–301. doi: 10.1111/j.1468-3083.2009.03411.x. [DOI] [PubMed] [Google Scholar]
- 12.Whiting D A.Diagnostic and predictive value of horizontal sections of scalp biopsy specimens in male pattern androgenetic alopecia J Am Acad Dermatol 199328(5 Pt 1):755–763. [DOI] [PubMed] [Google Scholar]
- 13.Werner B, Mulinari-Brenner F. Clinical and histological challenge in the differential diagnosis of diffuse alopecia: female androgenetic alopecia, telogen effluvium and alopecia areata–part II. An Bras Dermatol. 2012;87(06):884–890. doi: 10.1590/S0365-05962012000600010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whiting D A. Histopathologic features of alopecia areata: a new look. Arch Dermatol. 2003;139(12):1555–1559. doi: 10.1001/archderm.139.12.1555. [DOI] [PubMed] [Google Scholar]
- 15.Chaitra V, Rajalakshmi T, Kavdia R. Histopathologic profile of alopecia areata in Indian patients. Int J Trichology. 2010;2(01):14–17. doi: 10.4103/0974-7753.66906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elston D M, McCollough M L, Bergfeld W F, Liranzo M O, Heibel M. Eosinophils in fibrous tracts and near hair bulbs: a helpful diagnostic feature of alopecia areata. J Am Acad Dermatol. 1997;37(01):101–106. doi: 10.1016/s0190-9622(97)70219-6. [DOI] [PubMed] [Google Scholar]
- 17.Whiting D. The histopathology of alopecia areata in vertical and horizontal sections. Dermatol Ther. 2001;14:297–305. [Google Scholar]
- 18.Goyal M, Khandpur S, Ramam M, Sharma V K, Singh M K. A study of the histopathological features of alopecias on transverse sections of scalp biopsies. Indian J Dermatol. 2019;64(01):47–54. doi: 10.4103/ijd.IJD_477_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muller S A. Trichotillomania: a histopathologic study in sixty-six patients. J Am Acad Dermatol. 1990;23(01):56–62. doi: 10.1016/0190-9622(90)70186-l. [DOI] [PubMed] [Google Scholar]
- 20.Royer M C, Sperling L C. Splitting hairs: the 'hamburger sign' in trichotillomania. J Cutan Pathol. 2006;33 02:63–64. doi: 10.1111/j.1600-0560.2006.00526.x. [DOI] [PubMed] [Google Scholar]
- 21.Dogra S, Sarangal R. What's new in cicatricial alopecia? Indian J Dermatol Venereol Leprol. 2013;79(05):576–590. doi: 10.4103/0378-6323.116726. [DOI] [PubMed] [Google Scholar]
- 22.Sperling L C, Cowper S E. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25(01):41–50. doi: 10.1016/j.sder.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Sperling L C, Solomon A R, Whiting D A. A new look at scarring alopecia. Arch Dermatol. 2000;136(02):235–242. doi: 10.1001/archderm.136.2.235. [DOI] [PubMed] [Google Scholar]
- 24.Horenstein M G, Jacob J S. Follicular streamers (stelae) in scarring and non-scarring alopecia. J Cutan Pathol. 2008;35(12):1115–1120. doi: 10.1111/j.1600-0560.2008.00987.x. [DOI] [PubMed] [Google Scholar]
- 25.Workshop on Cicatricial Alopecia . Olsen E A, Bergfeld W F, Cotsarelis G. Summary of North American Hair Research Society (NAHRS)-sponsored workshop on cicatricial alopecia, Duke University Medical Center, February 10 and 11, 2001. J Am Acad Dermatol. 2003;48(01):103–110. doi: 10.1067/mjd.2003.68. [DOI] [PubMed] [Google Scholar]
- 26.Zelger B G, Zelger B. Lichen planopilaris-histologic criteria & clues in vertical sections. Hair Ther Transplant. 2013;3:1. [Google Scholar]
- 27.Hordinsky M. Cicatricial alopecia: discoid lupus erythematosus. Dermatol Ther. 2008;21(04):245–248. doi: 10.1111/j.1529-8019.2008.00205.x. [DOI] [PubMed] [Google Scholar]
- 28.Pierre-Louis M, Sperling L C, Wilke M S, Hordinsky M K. Distinctive histopathologic findings in linear morphea (en coup de sabre) alopecia. J Cutan Pathol. 2013;40(06):580–584. doi: 10.1111/cup.12124. [DOI] [PubMed] [Google Scholar]
- 29.Al-Zaid T, Vanderweil S, Zembowicz A, Lyle S. Sebaceous gland loss and inflammation in scarring alopecia: a potential role in pathogenesis. J Am Acad Dermatol. 2011;65(03):597–603. doi: 10.1016/j.jaad.2010.09.774. [DOI] [PubMed] [Google Scholar]
- 30.Somani N, Bergfeld W F. Cicatricial alopecia: classification and histopathology. Dermatol Ther. 2008;21(04):221–237. doi: 10.1111/j.1529-8019.2008.00203.x. [DOI] [PubMed] [Google Scholar]
- 31.Alzolibani A A, Kang H, Otberg N, Shapiro J. Pseudopelade of Brocq. Dermatol Ther. 2008;21(04):257–263. doi: 10.1111/j.1529-8019.2008.00207.x. [DOI] [PubMed] [Google Scholar]
- 32.Zinkernagel M S, Trüeb R M. Fibrosing alopecia in a pattern distribution: patterned lichen planopilaris or androgenetic alopecia with a lichenoid tissue reaction pattern? Arch Dermatol. 2000;136(02):205–211. doi: 10.1001/archderm.136.2.205. [DOI] [PubMed] [Google Scholar]
- 33.Amato L, Chiarini C, Berti S, Bruscino P, Fabbri P. Case study: fibrosing alopecia in a pattern distribution localized on alopecia androgenetica areas and unaffected scalp. Skinmed. 2004;3(06):353–355. doi: 10.1111/j.1540-9740.2004.03687.x. [DOI] [PubMed] [Google Scholar]
- 34.Kossard S. Postmenopausal frontal fibrosing alopecia. Scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130(06):770–774. [PubMed] [Google Scholar]
- 35.Kossard S, Lee M S, Wilkinson B. Postmenopausal frontal fibrosing alopecia: a frontal variant of lichen planopilaris. J Am Acad Dermatol. 1997;36(01):59–66. doi: 10.1016/s0190-9622(97)70326-8. [DOI] [PubMed] [Google Scholar]
- 36.Faulkner C F, Wilson N J, Jones S K. Frontal fibrosing alopecia associated with cutaneous lichen planus in a premenopausal woman. Australas J Dermatol. 2002;43(01):65–67. doi: 10.1046/j.1440-0960.2002.00558.x. [DOI] [PubMed] [Google Scholar]
- 37.Whiting D A, Olsen E A. Central centrifugal cicatricial alopecia. Dermatol Ther. 2008;21(04):268–278. doi: 10.1111/j.1529-8019.2008.00209.x. [DOI] [PubMed] [Google Scholar]
- 38.Rajalakshmi T, Inchara Y K, Antony M. Follicular mycosis fungoides - A report of four Indian cases. Indian J Med Paediatr Oncol. 2009;30(03):108–112. doi: 10.4103/0971-5851.64257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Böer A, Guo Y, Ackerman A B. Alopecia mucinosa is mycosis fungoides. Am J Dermatopathol. 2004;26(01):33–52. doi: 10.1097/00000372-200402000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Otberg N, Kang H, Alzolibani A A, Shapiro J. Folliculitis decalvans. Dermatol Ther. 2008;21(04):238–244. doi: 10.1111/j.1529-8019.2008.00204.x. [DOI] [PubMed] [Google Scholar]
- 41.Stefanato C M. Histopathology of alopecia: a clinicopathological approach to diagnosis. Histopathology. 2010;56(01):24–38. doi: 10.1111/j.1365-2559.2009.03439.x. [DOI] [PubMed] [Google Scholar]
- 42.Stefanato C, Asher R, Craig P, Orchard G. The multiteam approach in the newly introduced alopecia protocol: the St. John's experience. J Cutan Pathol. 2008;35:137–138. [Google Scholar]
- 43.Ackerman A B, Boer A, Bennin B, Gottlieb G.An algorithmic method based on pattern analysis 3rd ed.New York: Ardor Scribendi; 2005. Histologic diagnosis of inflammatory skin diseases [Google Scholar]


