Abstract
Patterned hair loss which includes both male pattern hair loss (MPHL) or androgenic alopecia (AGA) and female pattern hair loss (FPHL) is the most common indication for hair transplant surgery. However, not all such patients are candidates for hair transplants. There are eight conditions that cause patients to not be appropriate candidates. These are: diffuse unpatterned alopecia (DUPA), cicatricial alopecia (CA), patients with unstable hair loss, patients with insufficient hair loss, very young patients, patients with unrealistic expectations, patients with psychologic disorders such as body dysmorphic disorder (BDD) and trichotillomania, and patients who are medically unfit. In addition, there are patients who are poor candidates and who should undergo hair transplantation only if they understand and accept limited results. The key to identifying these patients involves performing careful and detailed history and examination at the time of consultation.
Keywords: candidacy, pattern hair loss, hair transplant, hair restoration surgery, patient selection, long-term treatment plan, progressive condition
Introduction
A successful hair transplant depends on the appropriate selection of patients by the surgeon. Not every balding person is a candidate for hair restoration. Missed diagnoses can lead to poor surgical outcomes.
The most common indication for hair transplantation in both men and women is patterned alopecia. Patterned alopecia incudes male pattern hair loss (MPHL), which is also known as androgenic alopecia (AGA), and female pattern hair loss (FPHL). Fig. 1 shows the widely used Norwood–Hamilton classification of MPHL and Fig. 2 shows the Ludwig classification of FPHL. 1 2 A minority of women will have frontotemporal hair loss in patterns similar to the Norwood–Hamilton patterns.
Fig. 1.
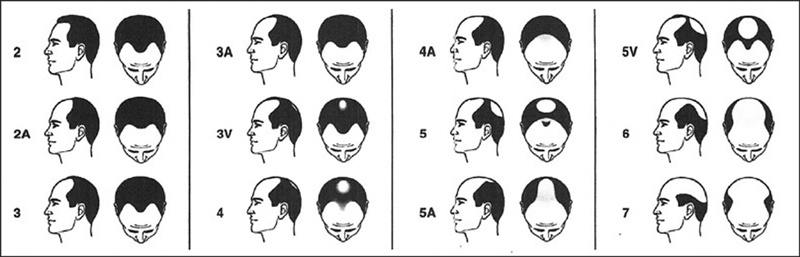
Norwood classification of male pattern hair loss (MPHL).
Fig. 2.
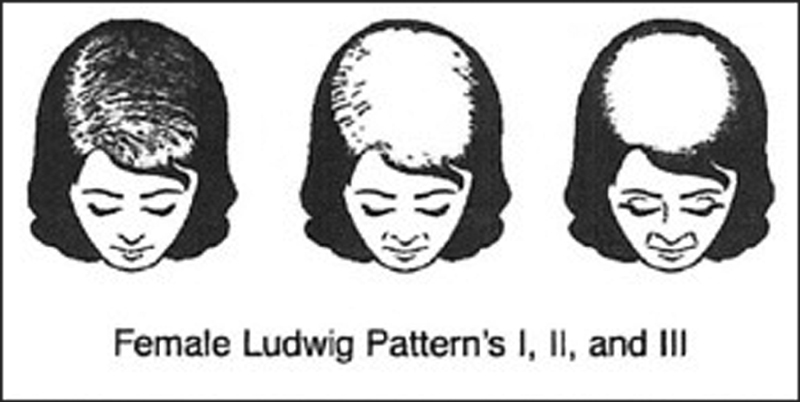
Ludwig classification of female pattern hair loss (FPHL).
The majority of patients with pattern hair loss, at some point in the course of their condition, will be candidates for transplantation. A hair transplant can be performed for any person with sufficient hair loss, good donor area hair, a healthy scalp, in good general health, and who has reasonable expectations. 3 When the hair transplant is done by a well-qualified, trained, and experienced surgeon, results are natural and enduring.
Diagnosis and Determining Surgical Candidacy
The key to identifying and excluding patients with PHL, who are not candidates for hair transplantation, is being able to perform a competent and thorough general medical and scalp-specific history and examination. A hair surgeon must be fully trained and experienced in performing this evaluation. It is relatively easy to identify many cases of poor candidacy, but some of these cases are subtle and can be missed without detailed and knowledgeable evaluation.
Essential questions to determine candidacy
Is there a pattern to the hair loss?
Is there greater than 50% hair loss in any part of the scalp?
Does the scalp appear healthy?
What is the quality and quantity of hair in the donor region?
Is the hair loss unstable?
Does the patient have realistic expectations?
Are there any medical or dermatologic conditions that could interfere with the surgery?
Caveats to Avoid Misdiagnosis
For all patients:
Take a thorough general medical history.
Take a thorough hair loss-specific history.
Examine the entire scalp, both donor and recipient areas of both the hair and the scalp. In men, examine the nonscalp donor areas of the beard and body.
Routinely use dermoscopy/densitometry.
Have a high index of suspicion—get consultations/biopsies if anything unusual.
In each consultation, get a thorough current and past medical history to identify any conditions that could be contributing to hair loss or which could impact on surgery. A detailed history of the development and character of the hair loss must be obtained. When did the hair loss start? Is it now stable or worsening slowly or rapidly? Is there a family history of hair loss; if so, who and what patterns? What treatments have been used? Diagnoses by other doctors who were consulted.
Examine the entire scalp thoroughly. This means combing through the whole scalp while looking at the condition of the scalp and quality and density of the hair. During this examination, pay attention to miniaturization of hair (which is the hallmark of PHL), variations in density, scaling or redness of the scalp, and loss of follicular ostia and shininess. Is there gross evidence of hair loss? Note the degree of loss for each location. Is the loss patchy? Diffuse?
Routinely use dermoscopy/densitometry in both the recipient and donor areas to determine density and the degree of miniaturization, percentage of loss density, and further characterize any scalp findings.
Hair of 60 to 65 microns is considered fine hair, 65- 80 microns is considered medium hair, and greater than 80 microns is considered coarse hair. Less than 60 follicular units (FUs)/cm 2 in the donor region is considered low density.
If this examination shows only findings consistent with PHL, if the donor area is of good density and condition, and if the there are areas of sufficiently developed balding, hair transplantation can be undertaken.
On the other hand, if there are scalp findings or unusual patterns of hair loss and/or miniaturization in the donor area, further evaluation is needed before undertaking transplantation. This means possible biopsy and dermatology consultation.
Contraindications to Transplantation in Patterned Hair Loss
While there are few absolute contraindications to hair restoration surgery, there are several relative contraindications.
Avoid Performing Hair Transplant Surgery in These Eight Patient Categories
1. Diffuse unpatterned alopecia
It is essential to identify patients who do not have a patterned alopecia, but rather they have a diffuse unpatterned alopecia (DUPA). The key aspect in making this differentiation is that the miniaturization and loss of density is not confined to the top of the head, but also involves the temporal, parietal, and occipital scalp ( Fig. 3 ). The concept of donor dominance is at the heart of hair transplantation. To produce an enduring result with hair transplantation, the donor follicles must be taken from the portion of the scalp which is spared by the pattern of alopecia and commonly referred to as the safe donor area. If there is no such donor area, as in DUPA, transplantation will not be successful and should not be performed. The loss of density and miniaturization in many cases of DUPA is readily evident upon gross inspection. But in earlier stages of the condition, magnified scalp examination with dermoscopy or trichoscopy is necessary to identify excess miniaturization. Diagnosis can be confirmed by scalp biopsies taken from the sides or back of the head as well as the top of the scalp. Medications are the treatment of choice for DUPA and not surgery. The degree of miniaturization that defines DUPA is not fully defined. Dr. Jose Lorenzo has suggested greater than 15% is a warning sign (personal communication). Devroye has suggested the threshold of 35% as an absolute contraindication to surgery. 3 Anything in between is certainly cause for caution. 4 5 6
Fig. 3.

Patient with diffuse unpatterned alopecia (DUPA) (Courtesy of Seema Garg).
Diffuse Patterned Alopecia
DPA is to be differentiated from DUPA. In DPA, the hair loss does follow a pattern and is confined to the top of the head, but the thinning is present throughout the entire pattern rather than focused on specific regions, as in the Norwood patterns ( Fig. 4 ). Those with DPA are potential candidates for hair transplantation.
Fig. 4.

Patient with diffuse patterned alopecia (DPA) (Courtesy of Seema Garg).
2. Cicatricial Alopecias
CAs may mimic PHL or may occur along with PHL. Hair transplantation is not indicated with active CAs, as not only is there a high risk of failure but hair transplant surgery can also exacerbate the disease. Cicatricial alopecias include lichen plano pilaris (LPP), CCCA, discoid lupus erythematosus (DLE), and others. 7 8 In scalp examination, look for patchy hair loss, redness around the base of hair follicles as they exit the skin, loss of follicular ostia, shininess of the skin, scarring of the scalp, or hair loss without miniaturization ( Fig. 5 ). There can be underlying PHL and superimposed CA. These lesions can occur anywhere throughout the scalp—recipient and donor areas. In the presence of any of these signs, dermoscopy and scalp biopsy are indicated before proceeding with hair transplantation. Although controversial, hair transplantation may be undertaken when the CA is burned out, no active disease for two or more years, or biopsy confirmed. Yield may be suboptimal due to the scarring, and results may be only temporary.
Fig. 5.

Patient with cicatricial alopecia (CA) (Courtesy of Seema Garg).
3. Alopecia areata
An autoimmune variant that affects hair follicles, AA may coexist with PHL. Patchy hair loss may occur anywhere in the scalp, beard, or body hair 9 ( Fig. 6 ). Detection of such a patch or multiple patches necessitates a high index of suspicion and should be followed by dermoscopy, biopsy, and possible dermatology referral. Hair transplant is contraindicated in the presence of active AA, even if there is also PHL. Surgery may precipitate a recurrence and the transplanted hair may be affected by AA. If there has been no active disease for an extended period (2 or more years), the risk with hair transplant is diminished but not eliminated.
Fig. 6.

Patient with alopecia areata (AA) (Courtesy of Seema Garg).
4. Patients with unstable hair loss
It is essential during the initial consultation that the practitioner develop an assessment of the stability of the patient's condition. If the history indicates that the condition has not been changing or accelerating recently, and if there is not a high degree of miniaturization in the area to be transplanted (less than 15%), it is safe to proceed with surgery. On the other hand, if the history indicates rapid deterioration and progression and the recipient area has greater than 15% miniaturization, it is better to initiate medical therapy for 6 to 12 months to stabilize the patient before proceeding with surgery. A patient with a high degree of miniaturization in the recipient area is at high risk of experiencing shock loss with transplantation that may be permanent. 10 Patients who experience this kind of hair loss from the surgery are likely to be unhappy and feel that the surgery has made them worse rather than better. A total of 6 to 12 months of medical therapy with finasteride, minoxidil, low-level laser therapy (LLLT), and platelet-rich plasma (PRP) is likely to reverse some of the miniaturization and lessen the impact of shock loss secondary to the surgery.
5. Patients with insufficient hair loss
Most patients with PHL will present with some of the areas of the top of the head with readily visible loss of hair density and the scalp showing through the hair. In these areas, over 50% of the native hair density has been lost. This is generally held as the threshold at which hair transplantation can be performed without risking damage to the native hair in the recipient area. Some patients will present without any areas of the scalp showing such thinning. Nevertheless, closer examination with trichoscopy will reveal the presence of PHL and miniaturization. Such patients are not yet candidates for hair transplantation. Rather, medical therapy is indicated along with ongoing monitoring until such time that loss of hair density reaches the threshold for transplantation.
6. Beware the young patient!
Surgeons must be particularly cautious when dealing with young male patients in their late teens to early 20s. 11 12 Often when PHL develops at such a young age, it is both rapidly progressive and emotionally devastating to the patient. When these patients present for the consultation, there is often a sense of urgency on the part of the patient and sometimes his parents to “fix” the problem, and they come to the office convinced that getting a hair transplant is what will resolve the situation. In many instances, their hairline has receded. This recession may have converted their juvenile low and flat hairline to the level of a normal adult male hairline. They show you a picture of their favorite pop star with a very thick head of hair and a low, flat hairline and squared-off temples, declaring that this is what they want. Or they may have a balding vertex and want it restored to the original density. These patients often have very unstable hair loss, and they are undergoing rapid progression of their balding. Most will, without intervention, end up with Norwood class 5–6 balding by age 30, if not before. While tempting to the surgeon, performing a hair transplant at this early stage is the wrong way to treat these young patients. Giving the patient that low flat hairline and/or overutilizing donor supply to make the vertex hair thick will jeopardize the future for these patients and come back to haunt both them and the surgeon.
Proper care for these patients means that the surgeon will spend time explaining the progressive nature of the balding process and the need for ongoing treatment throughout adulthood. Medical treatment will be recommended with the goal being stabilizing the progression of balding and perhaps restoring some lost density prior to performing a hair transplant. This means deferring consideration of hair transplanting for at least a year. During that year, the patient should be seen two to four times to monitor medical therapy effects and side effects, with the goal of helping the patient get the best results. It is essential that the patient be fully informed about the medications prescribed and understand that effects take months to develop fully.
Some patients will reject medical therapy and insist on transplantation. Rather than bowing to this pressure, the best course for the surgeon is not to do the surgery but to invite the patient to get further consultations with reputable and ethical surgeons and to return for a second consultation. Without medical therapy, it is probable that these patients will be chasing their progressing balding with a series of surgeries until their donor supply, their doctor, and they are exhausted and unsatisfied.
7. The patient with unrealistic expectations
Apropos the discussion above of the pitfalls of transplanting in young patients, there also lies the issue of examining the problem of the patient with unrealistic expectations. The patient who is showing you the picture of their favorite pop star, movie star, or professional athlete typically has unrealistic expectations. Our goal with transplantation is not to create a superdensity as great or greater than the prebalding level. Rather, we aim for cosmetic density that creates the appearance of density without actually restoring or surpassing the original density. A patient who expects to see no scalp at all after transplantation is going to be very difficult to satisfy. At the same time, a patient who expects that there will be “zero” scarring after surgery will be equally at risk for dissatisfaction. It is the surgeon's responsibility to be able to educate the patient with reasonable expectations and be convinced that they understand and accept these limitations. If not, proceeding with surgery can be risky and problematic.
8. Patients with psychological disorders
The most complex psychological disorder is BDD. These patients will often present with very trivial defects, sometimes not even evident to the examining surgeon. They will report a fixation of this defect, constantly looking in the mirror and believing that others are aware of the defect and staring because of it. It is a mistake to transplant these patients. They are at high risk of being dissatisfied, seeking a never-ending stream of “corrective” surgeries and also being litigious. They may not readily accept a refusal to perform surgery, and they may not accept recommended psychological counseling.
Another risky patient to transplant is the patient with trichotillomania, an obsessive-compulsive disorder of incessant hair pulling and plucking. A patient may have this coexisting with PHL, or they may produce a balding pattern that mimics pattern hair loss ( Fig. 7 ).
Fig. 7.

Patient with trichotillomania (Courtesy of Seema Garg).
Inquiring about hair pulling needs to be a routine part of the consultation, as does an examination of the balding area for broken hairs. Sometimes patients will deny hair pulling, making diagnosis more challenging. Trichotillomania is not an absolute contraindication to hair transplantation, but transplantation should be deferred, pending psychological treatment and stabilization.
Anxiety and/or depression are not contraindications and transplantation may help in treating these conditions. It is important for the surgeon to support the patient in receiving psychological treatment for these disorders in conjunction with hair loss treatment.
Proceed with Caution
Patients with Medical Conditions that Complicate Surgery
Patients who smoke regularly are at risk of having poor yield from their hair transplant because of the vascular effects of smoking. The best situation is for the patient to completely stop smoking a month or two before the transplant and not resume smoking afterward. If this is not possible, then cessation 3 weeks before and after can reduce the risks. But if the patient cannot or will not do either of these, the best course is to not perform surgery. If surgery is performed on a smoker, without cessation, he/she should give written acknowledgment of being informed that the result may be suboptimal.
Patients with long-standing diabetes with microvascular damage or patients with extensive solar damage to the scalp are also at risk of suboptimal yield and should be so advised prior to surgery. Perhaps, the best course for these patients is to do smaller treatments with somewhat lower density.
Other patients with chronic medical conditions such as hypertension, heart disease, diabetes, excessive alcohol use, immune deficiency, anticoagulation, and others can undergo hair transplantation if these conditions are fully recognized and managed before and during surgery.
Relatively Poor Candidacy
Some patients will have poor quality or limited donor hair, making them relatively poor candidates for surgery, particularly if they have advanced balding. They will be able to only cover a part of the balding area (usually frontal forelock) and achieve lower density of coverage. This does not mean that they cannot have surgery, but that they must be aware of and accept the limitations of what can be achieved ( Fig. 8 ).
Fig. 8.

Poor Candidates for hair transplantation.
Key Points
Not all persons with PHL are suitable candidates for hair transplantation.
PHL is a progressive condition; therefore, rarely is a single transplant session adequate.
Great care must be taken with the younger patient because of potential unrealistic expectations and the uncertain extent of balding.
Great care must be taken with the patient who has unstable, rapidly progressing hair loss.
Donor hair quality and density must be adequate to undertake restoration.
Coexisting dermatologic and medical conditions must be excluded or fully controlled with ongoing treatment.
Thorough history and examination are needed to make correct diagnoses and treatment plans.
Conclusion
Most patients who present for hair transplantation are suitable candidates. However, some patients should not undergo transplantation for a variety of reasons. It is incumbent for the hair transplant surgeon be able to identify these patients and advise against surgery. This requires that thorough history, examination, and testing are routine. The surgeon must be familiar with the hair loss and scalp conditions as well as the medical and psychological conditions that are contraindications to hair transplantation.
Footnotes
Conflict of Interest None.
References
- 1.Hamilton J B. Patterned loss of hair in man; types and incidence. Ann N Y Acad Sci. 1951;53(03):708–728. doi: 10.1111/j.1749-6632.1951.tb31971.x. [DOI] [PubMed] [Google Scholar]
- 2.Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977;97(03):247–254. doi: 10.1111/j.1365-2133.1977.tb15179.x. [DOI] [PubMed] [Google Scholar]
- 3.Konior R J, Simmons C. Patient selection, candidacy, and treatment planning for hair restoration surgery. Facial Plast Surg Clin North Am. 2013;21(03):343–350. doi: 10.1016/j.fsc.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Devroye J. New York: Informa Healthcare; 2011. An overview of the donor area: basic principles; pp. 248–262. [Google Scholar]
- 5.Bernstein R M, Rassman W R.Follicular transplantation. Patient evaluation and surgical planning Dermatol Surg 19972309771–784., discussion 801–805 [PubMed] [Google Scholar]
- 6.Seery G. More on Guidelines. Hair Transplant Forum Int. 1998;8(04):14. [Google Scholar]
- 7.Harris J A.New methodology and instrumentation for follicular unit extraction: lower follicle transection rates and expanded patient candidacy Dermatol Surg 2006320156–61., discussion 61–62 [DOI] [PubMed] [Google Scholar]
- 8.Ross E K, Shapiro J. Berlin: Springer; 2008. Primary cicatricial alopecia; pp. 187–220. [Google Scholar]
- 9.Sinclair R, Banfield C, Dawber R. Hoboken, NJ: Wiley-Blackwell Science; 1999. Handbook of Diseases of the Hair and Scalp. [Google Scholar]
- 10.Pia Freyschmidt P, Hoffmann R, McElwee K J. New Delhi: Springer; 2010. Alopecia areata; pp. 311–328. [Google Scholar]
- 11.True R H, Dorin R J. A protocol to prevent shock loss. Hair Transplant Forum Int. 2005;15(06):197–199. [Google Scholar]
- 12.Cohen I. Guidelines for hair transplantation in the young patient. Hair Transplant Forum Int. 2001;11(05):131–133. [Google Scholar]


