Abstract
Follicular unit extraction (FUE), now named as follicular unit excision, is one of the methods of harvesting hair follicles from the donor area for implanting in the recipient area. The occipital scalp area is the most common donor area, but nonscalp donor areas like beard, chest, and other hairy body parts can be used as donor hair follicle area. The extraction of the hair follicle leaves a tiny circular scar over the donor area. Over the past 20 years, various devices for FUE have been developed, starting from manual, simple motorized to highly advanced motors with rotation, oscillation, and vibration. Similarly, different types of punch are used: dull, sharp, ultrasharp, serrated, hybrid and specially designed punch blade for long hair follicles harvesting in various diameters from 0.7 mm to 1.1 mm. The follicles can be harvested either by manual method or by motorized method.
Keywords: FUE, follicular unit strip surgery, FUT, oscillation, punch
Introduction
Follicular unit extraction (FUE), now called “follicular unit excision,” is one of the methods for hair follicle harvesting in hair transplantation 1 2 . It involves harvesting hair follicles from the safe donor area, using a circular hollow blade called “punch.” The scalp is a commonly used donor area, and other donor areas include the beard, chest, and other body parts. 3 The extraction leaves a circular wound that heals with primary intention, leaving only a tiny scar. The procedure has achieved increasing popularity compared with the strip method of follicle harvesting, widely known as follicular unit transplantation (FUT) or follicular unit strip surgery (FUSS), as there is no linear scar.
Historical Perspective
The first hair transplant was done by a Japanese doctor, Shoji Okuda, in 1937. 4 The modern era of FUE began with the work of several surgeons such as Woods, Rassman, Cole, Harris, and Rose. The term “follicular unit extraction” was coined by William Rassman in 2002. 5 Dr. Paul Rose suggested the term “follicular isolation technique” (FIT) to denote the possibility that an extracted graft does not always include all the follicles of the follicular unit (FU) or at times have follicles from more than one FU. 6
Over the past 20 years, a variety of automated devices have evolved to assist with the speed of incisions and reduction in transections, such as the SAFER System, Neograft, Smart Graft, Vortex, PCID, WAW system, 3 Step FUE, Rote core, Mamba, and other devices. 7 8 9 10 Now, robots are in use for FUE as well as implantation. 7
Current Nomenclature of FUE
As per International Society of Hair Restoration Surgery (ISHRS), the appropriate definition of FUE is as follows: “follicular unit excision is the surgical technique that refers to circumferential incision of the skin around the follicular unit bundle or group of hair follicles to extract a full-thickness skin graft containing hair follicle (s), intradermal fat, dermis, and epidermis.” 11
The Logic of FUE
As explained by Headington, the FU comprises one to four terminal hair follicles (now modified to be one to five terminal hair follicles), their arrector pili muscle, surrounding connective tissue, nerves, and vessels ( Fig. 1 ). 12 The logic of FUE involves excising a column of tissue or a circular skin flap having hair and all layers of skin by releasing the fold of arrestors and severing the adherence of surrounding dermal collagen through a circular punch. Since the shape of the FU is pyramidal, it is the narrowest in the upper part till the attachment of arrectors; hence, a small punch of less than 1 mm is enough to excise the unit. This small size would then heal easily and quickly without a significant scar.
Fig. 1.
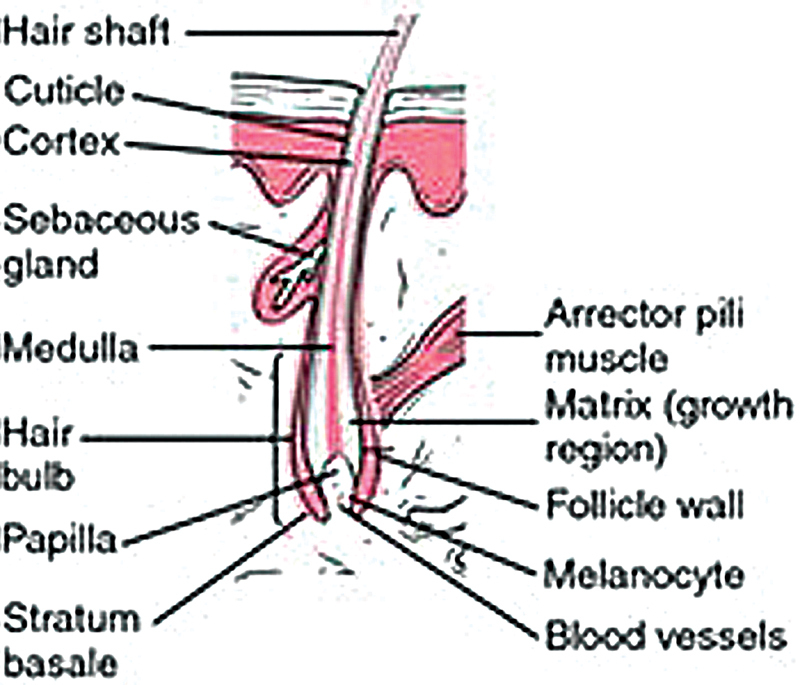
Hair follicle.
The inferior segment of hair, below the arrestors, is loosely held, and hence the unit pops up once the hold of arrectors is released ( Fig. 2 ). Such grafts would, then, not need any further dissection and be ready to be taken out of the hole. However, the pyramidal shape of the unit with splaying of hairs in the lower segment (figure of graft) and the varying level of attachment of arrectors would also lead to a more significant level of damage to the follicles, mainly because the introduction of punch is blind.
Fig. 2.

Popping out of graft once the arrector pili is cut.
One of the challenges in FUE donor harvesting is the variability of the FUE donor area. The viscoelastic properties of the skin are essential factors in FUE donor harvesting and contribute to the unpredictability of donor harvesting. The tissue characteristics of the skin vary from one patient to another. The viscoelastic characteristics of skin impart biomechanical properties similar to the elastic properties of solids and viscous properties of fluids. The patient-to-patient variations in the epidermis, dermal-epidermal junction, and subcutaneous tissue contribute to the challenges of donor harvesting and obtaining low-follicular transaction rates
Science behind FUE
There are two surgical events and four technical steps in the FUE method. The scoring of the epidermis to get inside the deeper tissue, and dissection of follicle separating the follicle unit from surrounding dermis, subcutaneous tissue, arrector pili muscle, and neurovascular structures. ( Fig. 3 ). The scoring of epidermis and dissection of follicle together are known as “excision of follicles.” The three surgical steps are as follows: alignment of punch, engagement of punch, and advancement of punch. The fourth step is the extraction or removal of the dissected follicle.
Fig. 3.
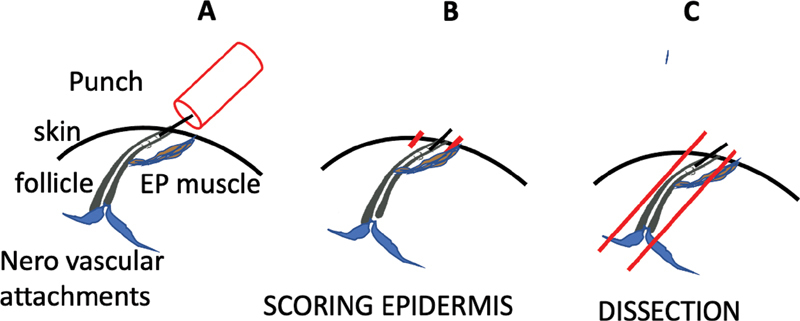
Surgical events. ( A ) Follicle with its attachments. ( B ) Scoring of the epidermis by the punch. ( C ). Dissection means separation of the follicle from its attachments.
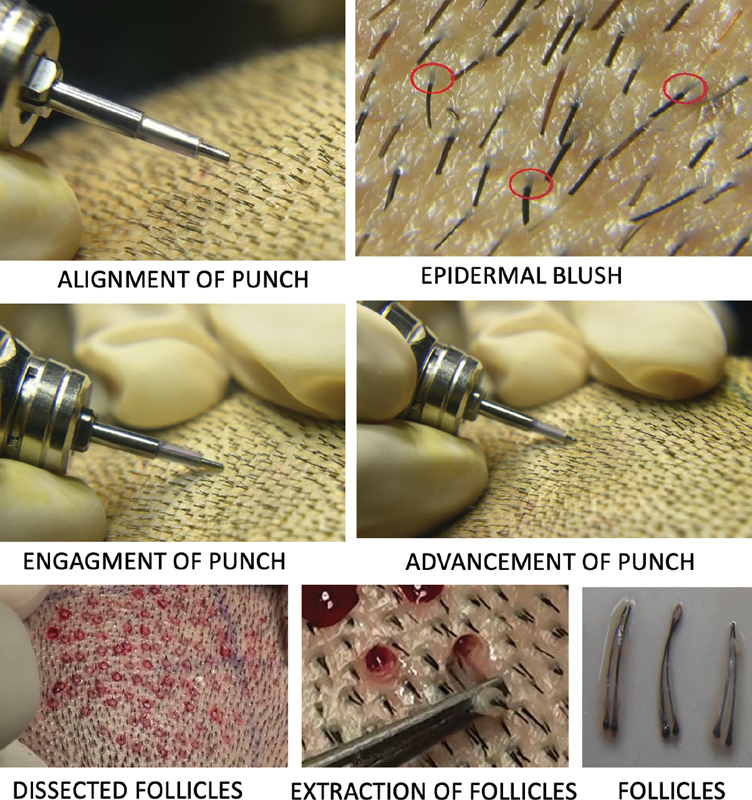
The first step—Alignment of punch means keeping the long axis of the punch axis along or parallel to the hair shaft ( Fig. 4 A ).
Fig. 4.

Steps of follicular unit extraction (FUE) ( A ) Step I—Alignment of punch to the hair shaft. ( B ) Step II—Engagement of punch to epidermal blush or exit point of hair. ( C ) Step III—Advancement of punch in deeper tissue for dissection of follicle unit. ( D ) Step IV—Removal or extraction of dissected follicle.
The second step—The engagement of punch is a process in which the punch cutting edge is fixed over the skin surface for scoring the epidermis. The punch is centered on the exit point of hair or preferably the epidermal blush. The epidermal blush is the intraepidermal part of hair shaft which is seen under magnification ( Fig. 4 B ).
The third step—With the help of advancement using rotatory or oscillatory movement, combined with the axial force, the punch is advanced deeper to separate the follicles from all their surrounding attachments, which is collectively known as the dissection of the follicle unit ( Fig. 4 C ).
The fourth step—Once the follicle unit is freed from surrounding attachments, then the dissected follicle unit is removed, which is called extraction. Extraction of the dissected follicle can be done either by a surgeon or a trained assistant ( Fig. 4 D ).
The precise depth insertion of punch is the key to harvesting an intact FU. The attachment of the follicle to the surrounding tissues is termed as “tethering.” Tethering is in all probability the major factor explaining the broad range of results obtained with the different FUE techniques and the variations recorded from one patient to another. The tethering is linked to the existence of various lateral connections between the dermal sheaths, the sebaceous gland, the arrector pili muscle, and connective tissue of the surrounding hypodermis. There is also a deep tethering between the hair follicle and the subcutaneous fat tissue at the bottom of the follicle unit (neurovascular attachments).
To have smooth extraction, there is a need to cut the majority of the lateral attachments. Consequently, the vertical force required to extract the follicle will be small enough to avoid injuries linked to the traction (like capping, splitting, crushing, breakage). The only way to cut attachments is to cut deep enough. For extraction, there is a need to use two forceps: one pulling the graft and other forceps pushes the skin in the opposite direction. If the graft comes out with just one forceps, it means the punch went too deep. There are exceptions. It is possible to remove the graft without a contra force, just by pulling, even if the scoring was shallow.
Instrumentations for FUE
There are two necessary instruments needed to perform follicular unit excision. 13 One is a circular hollow blade to dissect the FU from its surrounding structures, the so-called “FUE punch.” The other is a device over which the punch is mounted to use it for follicular unit dissection, the so-called “FUE punch handle.” There are a wide range of punches and punch holding handles available to perform the FUE. 13
FUE Punch
Diameter of Punch
The punch size varies from 0.7 mm to 1.2 mm in diameter. The commonly used ones are 0.9 to 1.00 mm for the scalp and 0.7 to 0.8 mm for the body hair follicle harvesting. The larger punch will reduce transection rates but lead to more scar volume and greater vascular compromise of the donor area. When the diameter is reduced, it may increase transection, but lead to thinner grafts, fewer follicles per FUs and less donor scar volume.
Edge of the Punch
Dr. John Cole, with the help of sharp punches, has simplified the biomechanics of extraction to support his theory. 14 When force is applied over the skin to cut, then there is compression of the skin and follicle underneath it as one unit. The dull punch needs more force to cut the skin, which leads to distortion of follicles and skin, thereby increasing the transaction and more buried grafts. If the sharp punch is used, less force will be required to cut the skin, so there will be no or minimal distortion of the skin and follicle unit. He extended his concept further by reducing the contact surface of the punch to the skin, in order to decrease the frictional injury to tissue. Keeping both concepts, he devised an ultrasharp serrated punch. The potential problem with a sharp punch is increased transaction rate, which is an important aspect and should be taken care of. The increased transaction because of sharp punch can be controlled by practice and depth precision.
A sharp punch is required to cut the skin, while to dissect follicles from surrounding, a dull punch is good enough. 13 Based on this concept, a variety of punches are designed with the intention to reduce transection. The flat punch mechanics do precisely the same. At 90 degrees, a flat punch acts sharply to the skin, but after piercing, it acts like a dull punch. By using a flat punch, we can penetrate deep enough without damaging the follicle.
The hybrid punch is flared (trumpet-shaped) at the end with a sharp outer edge and dull inner edge. 13 The sharp outer edge is to score the epidermis, and dull inner punch is to dissect the hair follicle from surrounding structures. This design helps in reducing the transection of hair follicles.
FUE Handle
The handle is a device over which the punch is mounted. This is used to create an axial, rotational, and/or oscillatory force to score the epidermis and finally dissect the follicle from its surrounding attachments. The handle can be manual and motorized ( Fig. 5 ).
Fig. 5.

Basic motorized system for follicular unit extraction (FUE). The basic console of motor and foot paddle to control speed and a motor in handle for holding the punch.
Methods of Follicular Unit Excision
The “FUE handle” can be manual or motorized. On this basis, the FUE is performed by two methods: the manual and the motorized method.
Manual Method of FUE
The punch is mounted on a handle, and the scoring of epidermis and dissection of the follicular unit is done using the axial and oscillatory forces of the hand. First, the epidermis is scored, followed by advancing deeper to dissect the follicles from surrounding dermis and subcutaneous tissue. The continuous oscillatory controlled force is applied along the axis of the follicle.
Technique
The manual FUE can be done either as a single-step or two-step technique. 15
Two-step Manual FUE Technique
The first step involves scoring epidermis. A sharp punch is mounted on a handle and aligned to the hair shaft, engaging the exit point or epidermal blush, and scoring the epidermis using oscillating force.
The second step—Replace the sharp punch and mount the dull punch over the handle. Insert the punch through the same incision created by the previous sharp punch. Maintaining the same angle, advance the punch in deeper tissue by oscillating and axial force. Once the arrector muscle is cut, there is a feeling of giving way. At this point, stop the punch movement and remove it; using forceps, remove the popped-out FU, examine this for transection, and adjust the depth and angle of punch accordingly.
Single-step Manual FUE
In this, the scoring of epidermis and dissection of the follicle unit is done using the same punch and in one step.
Motorized FUE
In the motorized method of FUE, the punch is mounted on a motorized handle. The device motor uses either electricity or battery power. 16 17 The motor makes revolution at a speed of 100 to 20,000 RPM. Initially, the revolutions were unidirectional, but in the advanced systems, oscillatory movements were added, like Mumba and Devroye FUE device. 13 Harris developed a safe system that utilizes blunt Hex punch, using two-step motorized handle. 18
Instruments for Motorized FUE
The motorized device and a punch, and the latter may be sharp or dull with variable diameter. ( Fig. 5 ).
Steps of Motorized FUE Method ( Fig. 6 )
Fig. 6.
Steps of follicular unit extraction (FUE).
Select motorized device, punch, and magnification loupe (3.5X to 5X).
Hold the handle in a pen-holding position, and stabilize the grip. Adjust the RPM of the motor and check the magnifying loupe.
Target the follicle to be harvested.
Start the rotation of the punch.
Align the punch to the exit angle of hair.
The center of punch is focused on the exit point of a hair or preferably epidermal blush. The epidermal blush is the show of the epidermal part of the hair shaft, which can be identified under magnification and good light ( Fig. 6 ).
Fix the punch over the skin surface, remember the motor is in motion, and score the epidermis.
After scoring the epidermis, advance the punch with controlled, steady pressure and allow the punch to dissect to the full depth (the depth has already been controlled by using a depth guard over the punch). The depth of punch can be decided as per the length of the follicle. For this, a few follicles are extracted to measure the length of the follicle ( Fig. 7 ).
During advancement of punch, speed of the motor is adjusted, as per the feeling of resistance from the tissue.
Initially, only a few grafts are harvested and evaluated for transection and graft burial.
Adjust the speed and angle as per the above observations.
Fig. 7.

Use of depth guard for depth precision of punch. ( A ) The first few test grafts are harvested, and the length of graft is assessed. ( B ) Infant feeding tube or other silicone tube is taken ( C ). The silicone tube guard is mounted over the punch, so the punch reaches just above the level of bulb of the hair follicle.
The simplest motorized system is a hand motor over which a punch can be mounted, and a motor is attached to a speed controlling console ( Fig. 5 ). A foot paddle can control the speed of the motor. The most common motor is one which a maxillofacial surgeon uses, but in FUE, the speed shall be within the range of 1000 to 2000 RPM. Over a period, many modifications in motorized systems have been incorporated.
Candidacy for FUE
A patient of hair loss desiring aesthetic correction, with a suitable donor area, otherwise fit for surgery and having reasonable expectations, can undergo a hair transplant. A young patient whose hair loss is not yet stable is a better candidate for medical treatment rather than surgery. Contrary to this, a patient with a very high grade of baldness, expecting a full head of hair and not willing for extra scalp donor hair harvesting, or when extra scalp donor hair is not available, is not a candidate for hair transplant. A patient having body dysmorphic disorder is a contraindication for hair transplants. Any candidate who has diffuse unpatterned hair loss, and the vellus hair is more than 30%, is not the right candidate for hair transplant. Such a patient shall be treated for the cause first.
There are few conditions where FUE can be a preferred choice over the strip method of hair transplant.
A person wishes to keep his hair short; the follicular unit excision is preferred as the long linear scar of strip surgery (FUSS) may show through the short hair.
There are cases in which the scalp laxity is less, and strip surgery might lead to a wide scar; patients with a history of hypertrophic scar or keloid tendencies are better candidates for FUE.
For patients having a low pain threshold and wanting to get back to his job earlier, the FUE option is good.
For cases which have already undergone strip surgery and the second strip is not possible, or they do not want the second strip, the FUE is a choice.
The FUE is the only method to harvest follicles from other than the scalp donor areas like the beard, chest, and other body parts.
The FUE is also done along with the strip method as a combination method of hair transplant.
Contraindications for FUE Surgery
There are a few conditions in which the FUE procedure is not a preferred procedure.
Patient with extensive scarring of the donor area.
Patients having a high curl of hair, where very high transection of follicles are expected.
The surgeon is not trained enough.
The patient is not willing for FUE.
The patient is not willing for head shaving, which is required in FUE; otherwise, unshaven FUE is the option.
Female patients who do not prefer shaving of the donor area, the strip method is the choice; otherwise, unshaven FUE is another option.
Safe Donor Area
The “SAFE donor area” of scalp means donor area from where the follicles, when harvested and implanted, remain unaffected by androgenetic factors which are responsible for miniaturization and hair loss. The safe donor area is the occipital area of scalp ( Fig. 8 ). The donor area other than the scalp donor area is also available for hair transplant. 19 20 21 22 It is mandatory that all grafts shall be harvested from safe donor area only.
Fig. 8.
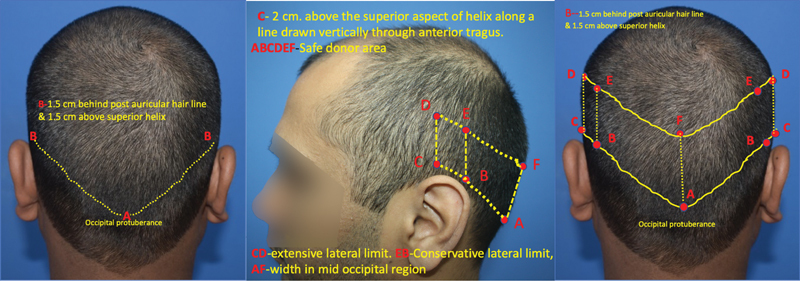
Scalp SAFE donor area—Width of safe donor area at the most anterior (lateral) limit is 6 to 7 cm wide. In the center of safe zone, width is decided by taking a horizontal line drawn from point “C,” (i.e., 2 cm above superior helix in a plane anterior to helix) which will intersect midline of occiput.
Anesthesia and Tumescence for Donor Area of Scalp
The commonly used anesthetic agents are lidocaine, bupivacaine, and ropivacaine. The nerve block using lidocaine and ropivacaine is used to block bilateral greater occipital and lesser occipital nerve. 23 After nerve block or ring block, the tumescence solution is infiltrated above galea for hemostasis and smooth, long-lasting anesthesia. 24
Few Essentials for FUE
Safe Excision Density
Safe excision density means the number of extracted grafts without compromising the visual density of donor area. 25 26 27 Most FUE experts recommend 10 to 15 excisions/cm 2 as a safe single pass density in a person with a baseline average density of 65 to 75 grafts per square centimeters. 26 Dr. James Harris reported a routine use of higher excision density in the range of 20 to 25 grafts per square centimeters without problems. 19 The author conducted a study of donor area density using Trico scan in Indian patients. He found average donor site density 89.67 FU/cm. 2 As part of the routine, the author took an average donor density of five points, and 20% of existing graft units were harvested in one session of follicular unit excision (that is in Caucasian patients who have higher donor density).
Position of Patient
The position of the surgeon, as well as the patient, should be very comfortable for easy and safe extraction. Massage chair or modified dental chair, prone and lateral position with frequent change of position of the patient, will ensure maximum cooperation from patient 28 . The author used a Thai massage chair, modified dental chair, and modified routine operating table, depending on procedure and comfort of patient, as shown in Fig. 9 .
Fig. 9.
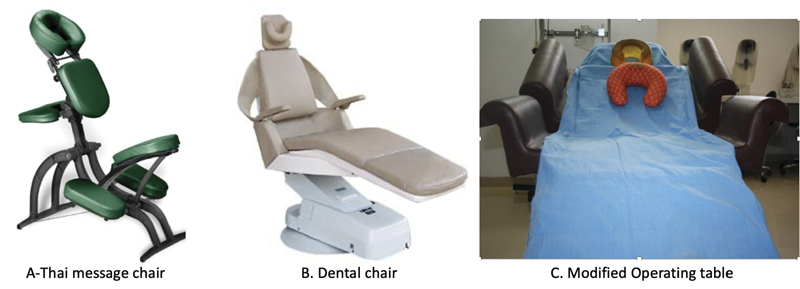
( A ) Thai massage chair, ( B ) modified dental chair, ( C ) operating table attached to the cushioned handle, extra cushion, and neck pillow.
Graft Out of Body Time (Ischemia Time)
The graft out of body time affects hair growth in terms of quality and quantity. 29 The graft out of body time to have maximum benefit is preferably within 2 hours. Kim and Hwang did a study which showed that grafts kept out of the body in saline for less than 2 hours have a similar survival rate compared with freshly harvested grafts reimplanted immediately. 30 For this period, the grafts can be kept in normal saline; other graft solutions do not have better results. Kim found normal saline at 4 degrees centigrade did not improve graft health unless more than 6 hours out of the body. The out of body time that is optimal for good growth should not exceed 2 hours. The reduction in graft out of body time can be made in two ways. One way is simultaneously extract and implant grafts in premade recipient sites. 31 Another way which the author followed was to have short sessions of graft extractions and implantations within 2 hours of graft extraction.
Common Beginner Mistakes and Tips to Avoid
Attempting a case size that is too large for the surgeon's experience level. It creates too much pressure to get more grafts, thereby compromising graft quality.
Inexperience with the device or technique being used. First, master one set of instruments and technique, get proper training, and start with small cases. After mastering one technique, then if required, change to another technique and/or instruments.
Use of low-quality loupes with less magnification for dissection. Obtain high-quality prismatic surgical loupes of at least 3.5X magnification. The author advises 4.5X and above magnification.
Using the same handling protocols with FUE grafts as used with strip grafts. FUE grafts are delicate and fragile as compared with strip grafts.
Precise control of the depth of punch using a guard.
Control speed and amount of extraction of grafts as per capability.
Conclusions
FUE method of hair transplant is the most demanding procedure. If done correctly, it is a safe procedure. The disadvantages of FUE can be reduced with experience, depth precision and use of better quality of instruments.
Footnotes
Conflict of Interest None declared.
References
- 1.Bernstein R M, Rassman W R, Szaniawski W, Halperin A. Follicular transplantation. Int J Aesthetic Restorative Surg. 1995;3:119–132. [Google Scholar]
- 2.Bernstein R M, Rassman W R. The aesthetics of follicular transplantation. Dermatol Surg. 1997;23(09):785–799. doi: 10.1111/j.1524-4725.1997.tb00419.x. [DOI] [PubMed] [Google Scholar]
- 3.Poswal A. Body hair transplant: an additional source of donor hair in hair restoration surgery. Indian J Dermatol. 2007;52:104–105. [Google Scholar]
- 4.Inui S, Itami S. Dr Shoji Okuda (1886-1962): the great pioneer of punch graft hair transplantation. J Dermatol. 2009;36(10):561–562. doi: 10.1111/j.1346-8138.2009.00704.x. [DOI] [PubMed] [Google Scholar]
- 5.Rassman W R, Bernstein R M, McClellan R, Jones R, Worton E, Uyttendaele H. Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28(08):720–728. doi: 10.1046/j.1524-4725.2002.01320.x. [DOI] [PubMed] [Google Scholar]
- 6.Kingsley S. Sharing experiences of follicular isolation technique? Follicular unit extraction. Hair Transplant Forum Int. 2004;14:15–16. [Google Scholar]
- 7.Rassman W R, Bernstein R M. New York: Marcel Dekker, Inc; 2002. Automation of hair transplantation past, present, and future; pp. 489–502. [Google Scholar]
- 8.Gökrem S, Baser N T, Aslan G. Follicular unit extraction in hair transplantation: personal experience. Ann Plast Surg. 2008;60(02):127–133. doi: 10.1097/SAP.0b013e318056d69a. [DOI] [PubMed] [Google Scholar]
- 9.Ekrem C, Aksoy M, Koc E, Aksoy B. Evaluation of three instruments used in FUE. Hair Transplant Forum Int. 2009;19(01):14–15. [Google Scholar]
- 10.Bernstein R M, Rassman W R. New instrumentation for three-step follicular unit extraction. Hair Transplant Forum Int. 2006;16:229–237. [Google Scholar]
- 11.Mejia R. Redefining the “E” in FUE: Excision = Incision + Extraction. Hair Transplant Forum Int. 2018;28(01):1–6. [Google Scholar]
- 12.Headington J T. Transverse microscopic anatomy of the human scalp. A basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120(04):449–456. [PubMed] [Google Scholar]
- 13.Mohebi P.The terminology used in follicular unit excision, Recommendation of FUE committee ISHRS Forum International 2019, Volume 29, Number 3. Doi: doi.org/10.33589/29.3.98
- 14.Cole J. 5th ed. London, UK: Informa Healthcare; 2011. Commentary- donor area harvesting; pp. 296–298. [Google Scholar]
- 15.Harris J A. 5th ed. London, UK: Informa Healthcare; 2011. Conventional FUE; pp. 291–92. [Google Scholar]
- 16.Onda M, Igawa H H, Inoue K, Tanino R. Novel technique of follicular unit extraction hair transplantation with a powered punching device. Dermatol Surg. 2008;34(12):1683–1688. doi: 10.1111/j.1524-4725.2008.34346.x. [DOI] [PubMed] [Google Scholar]
- 17.Ors S, Ozkose M, Ors S. Follicular unit extraction hair transplantation with micromotor: eight years experience. Aesthetic Plast Surg. 2015;39(04):589–596. doi: 10.1007/s00266-015-0494-8. [DOI] [PubMed] [Google Scholar]
- 18.Harris J A.Follicular unit extraction: the SAFE system Hair Transplant Forum Int 200414157,163–4 [Google Scholar]
- 19.Unger W. Delineating the safe donor area for hair transplanting. J Am Acad Cosmet Surg. 1994;4:239–243. [Google Scholar]
- 20.Bernstein R M, Rassman W R.Follicular transplantation. Patient evaluation and surgical planning Dermatol Surg 19972309771–784., discussion 801–805 [PubMed] [Google Scholar]
- 21.Rassman W R, Carson S. Micrografting in extensive quantities. The ideal hair restoration procedure. Dermatol Surg. 1995;21(04):306–311. [PubMed] [Google Scholar]
- 22.Cole J, Devroye J. A calculated look at the donor area. Hair Transplant Forum Intl. 2001;11:150–154. [Google Scholar]
- 23.Swinehart J M. Local anesthesia in hair transplant surgery. Dermatologic Surgery. 2002;28(12):1189. doi: 10.1046/j.1524-4725.2002.02127.x. [DOI] [PubMed] [Google Scholar]
- 24.Wolf B R. 5th ed. London, UK: Informa Healthcare; 2011. Overview of anaesthesia; pp. 227–243. [Google Scholar]
- 25.Bernstein R M, Rassman W R, Anderson K W.Follicular unit extraction mega sessions: evolution of a technique Hair Transplant Forum Int. 20041497–99.. doi:https://doi.org/10.33589/28.1.0001a [Google Scholar]
- 26.Keene S A, Rassman W R.Determining safe excision limits in FUE Hair Transplant Forum Int 2018287,8–10 [Google Scholar]
- 27.Devroye J. 5th ed. London, UK: Informa Healthcare; 2011. Donor Area Harvesting; pp. 247–248. [Google Scholar]
- 28.Miao Y, Fan Z X, Jiang W, Hu Z Q. Patient in the sitting position to improve comfort in follicular unit extraction. Plast Reconstr Surg Glob Open. 2016;4(11):e1141. doi: 10.1097/GOX.0000000000001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Limmer R. St. Louis: Mosby; 1996. Micrograft survival; pp. 147–9. [Google Scholar]
- 30.Kim J C, Hwang S. 4th ed. New York: Marcel Dekker; 2004. The effects of dehydration, preservation temperature and time, and hydrogen peroxide on hair grafts; pp. 285–286. [Google Scholar]
- 31.Sethi P, Bansal A. Direct hair transplantation: a modified follicular unit extraction technique. J Cutan Aesthet Surg. 2013;6(02):100–105. doi: 10.4103/0974-2077.112672. [DOI] [PMC free article] [PubMed] [Google Scholar]


