Abstract
Objective:
To examine the association of disease activity and disability with rehabilitation utilization in African Americans with rheumatoid arthritis (RA).
Methods:
We analyzed cross-sectional baseline data from the Consortium for the Longitudinal Evaluation of African Americans with RA (CLEAR) I and CLEAR II Registry. Disease activity was quantified with the Disease Activity Score 28 with C-Reactive Protein. Disability was measured with the Health Assessment Questionnaire. Rehabilitation utilization was determined by self-reported recall of physical therapy or occupational therapy visits in the prior 6 months or ever. We examined the association of disease activity and disability with rehabilitation utilization using separate binary logistic regression models to estimate odds ratios and 95% confidence intervals and adjusted for potential confounders. We repeated the analyses with the sample stratified by disease duration: early RA and established RA.
Results:
Of 1067 participants, 14% reported utilizing rehabilitation in the prior 6 months, and 41% reported ever utilizing rehabilitation. Rehabilitation utilization in the prior 6 months was similar among those with early and established RA (12% vs. 16%). A greater proportion of those with established RA reported any past rehabilitation utilization (28% vs. 50%). Among those with established RA but not early RA, worse disability was associated with rehabilitation utilization in the prior 6 months. Disease activity was not associated with either outcome.
Conclusion:
Among African Americans with RA, rehabilitation utilization in the 6 months prior to assessment was low and associated with disability, but not disease activity. Factors driving rehabilitation utilization are unclear.
Considerable advances in pharmacological care for adults with rheumatoid arthritis (RA) over the last 25 years, including emphasis on a treat-to-target approach and the introduction of biologic drugs, have resulted in lower disease activity and less joint destruction.(1, 2) However, disability has not improved to the same extent.(1-3) Functional limitation remains a prevalent consequence of RA.(1, 3) Rehabilitation, including physical therapy (PT) and occupational therapy (OT), is recommended to address disability and functional limitations in adults with RA(4), yet utilization of rehabilitation for adults with RA in the United States (US) is low.(5)
The current understanding of why and when rehabilitation is used among people with RA in the US is limited. Factors associated with OT utilization in the US are unknown, while there is a single study that investigated factors associated with PT utilization.(5) Using data from a registry of patients with RA, Iversen et al.(5) observed that 15% of adults with RA utilized PT in a 6-month period. Factors associated with utilization of PT were greater disease activity, higher levels of formal education, stronger social networks, and receiving disability pension. While this study provided novel insight on which patients with RA are more likely to receive PT, generalizability was limited as the sample was predominantly white (98%) and insured (98%), with higher socioeconomic status (67% with income >$50,000; 26% with a graduate degree or some graduate education).(5)
Racial and ethnic disparities exist in rehabilitation utilization for musculoskeletal conditions. African American and Hispanic adults with a musculoskeletal condition, including arthritis, have lower odds of receiving outpatient rehabilitation services compared to White adults.(6) In RA, lower disease activity and disability were associated with less utilization of rehabilitation services in white adults with RA, but it is unclear if associations are similar in African Americans. The purpose of this study was to examine the association of disease activity and disability with rehabilitation utilization in African Americans with RA, adjusting for other potential confounders. We hypothesized that greater disease activity and disability would be associated with rehabilitation utilization. A secondary purpose of the study was to examine if these associations differed among adults with early or established RA.
METHODS.
Design.
We conducted a cross-sectional analysis of data from the Consortium for the Longitudinal Evaluation of African Americans with RA (CLEAR) I and CLEAR II Registries. CLEAR I was a longitudinal cohort of African Americans with early RA (disease duration <2 years). Data from the baseline visit of CLEAR I were included in this analysis. CLEAR II was a cross-sectional cohort of African Americans with RA with no restriction on disease duration. Participant data for both CLEAR I and CLEAR II were collected at one of five southeastern US institutions (University of Alabama at Birmingham, Birmingham, Alabama; Emory University, Atlanta, Georgia; Medical University of South Carolina, Charleston, South Carolina; University of North Carolina at Chapel Hill, Chapel Hill North Carolina; Washington University, Saint Louis, Missouri).
Sample.
The shared inclusion criteria for the CLEAR I and CLEAR II cohorts were [1] self-identified as African American, [2] met the American College of Rheumatology 1987 criteria for RA(7), [3] ability and intent to provide informed consent, and [4] no concurrent diagnosis of rheumatic diseases other than osteoarthritis. Additional inclusion criteria for the CLEAR I cohort were RA disease duration <2 years and willingness to regularly participate in follow-up visits at year 3 and 5 disease duration. CLEAR I recruitment occurred from 2002 to 2005, and CLEAR II recruitment occurred from 2006 to 2011.
Measures.
The primary variables of interest were disease activity and disability. Disease activity was defined by the Disease Activity Score 28 with C-Reactive Protein (DAS28-CRP). The DAS28-CRP is a validated measure of RA disease activity and includes 28 tender and swollen joint counts, a patient assessment of disease activity on a visual analog scale, and serum levels of CRP with a range of 0-9.4.(8, 9) Disability was assessed with the Health Assessment Questionnaire Disability Index (HAQ). The HAQ is a valid, sensitive, and commonly used self-reported measure of physical function in adults with RA.(10, 11) The HAQ addresses eight functional domains including dressing, arising, eating, walking, hygiene, reaching, gripping, and usual activities.
Other participant characteristics were collected as potential confounders, including age (years), sex, body mass index (BMI, kg/m2; calculated from measured height and weight), disease duration (months from self-reported date of diagnosis to date of study entry), current use of conventional (e.g., methotrexate and leflunomide) or biologic disease modifying anti-rheumatic drugs (DMARD; self-reported yes/no), comorbidities (number of self-reported comorbid conditions from a list), household income (>$30k vs. ≤$30k), current employment (yes/no), and education (more than high school vs. high school graduate or less). The list of comorbidities were anemia; asthma, bronchitis, or emphysema; back or spine problems; depression; diabetes; fibromyalgia; heart disease such as angina, heart attack, hardening of arteries; high blood pressure or hypertension; inflammatory bowel disease (Crohn’s disease or ulcerative colitis); kidney stones or kidney disease; liver disease; osteoporosis; parathyroid disease; psoriasis; stomach ulcer, stomach or intestinal surgery; tumor, cyst, or cancer; vascular disease or stroke. In addition, participants could report any unlisted comorbidities.
Outcomes.
The primary outcomes were rehabilitation utilization in the 6 months prior to the study visit and any prior rehabilitation utilization. Participants were asked if they had seen a physical therapist or occupational therapist for help with their arthritis or other problems in the prior 6 months or ever. A response of “yes” was classified as rehabilitation utilization in each time frame respectively.
Multiple Imputation.
Data were missing for 227 (21.3%) participants, primarily due to missing values for DAS28-CRP (n=157, 14.7% missing). Thus, we used the multiple imputation procedure (SAS 9.4; PROC MI) to impute the relevant missing variables. We included all measures in Table 1 as variables in the imputation models. Twenty imputed datasets were created with 20 burn-in iterations before each imputation. The multiple imputation was conducted by fully conditional specification (FCS) logistic methods for binary covariates, and using FCS regression Predicted Mean Matching (REGPMM) method, which does not assume normality, for continuous variables. FCS was used because it performs well for assumptions for data missing at random and missing proportions lower than 0.5 [http://www2.sas.com/proceedings/sugi30/113-30.pdf].
Table 1.
Participant Characteristics
| Full Sample | Early RA | Established RA | ||
|---|---|---|---|---|
| Mean ± SD or Median [IQR] or % (n) | p-value ^ | |||
| n | 1067 | 445 | 622 | |
| Age, years | 54.2 ± 12.2 | 51.3 ± 13.0 | 56.3 ± 11.2 | <0.001 |
| Sex, women | 85% (916) | 84% (373) | 87% (543) | 0.10 |
| BMI, kg/m2 | 31.6 ± 7.6 | 31.6 ± 7.8 | 31.6 ± 7.5 | 0.95 |
| Education, more than HS | 44% (465) | 43% (191) | 44% (273) | 0.77 |
| Employed, yes | 30% (322) | 41% (184) | 22% (139) | <0.001 |
| Household income, >$30k | 25% (262) | 30% (130) | 21% (132) | 0.002 |
| Comorbidities, number | 3 [2, 5] | 3 [2, 4] | 3 [2, 5] | <0.001 |
| Disease duration, months | 37 [13, 138] | 11 [6, 17] | 117.5 [60, 213] | n/a |
| DMARD use, yes | 85% (904) | 82% (365) | 87% (539) | 0.04 |
| Disease Activity (DAS28-CRP), score | 3.9 ± 1.4 | 4.0 ± 1.5 | 3.8 ± 1.3 | 0.10 |
| Disability (HAQ), score | 1.4 ± 0.8 | 1.5 ± 0.9 | 1.3 ± 0.7 | 0.002 |
| Rehabilitation utilization in the prior 6 months, yes | 14% (150) | 12% (53) | 16% (97) | 0.10 |
| Rehabilitation utilization ever, yes | 41% (434) | 28% (126) | 50% (308) | <0.001 |
comparison of Early RA & Established RA using independent t-test, Mann-Whitney U test or Chi-squared
Abbreviations: BMI, body mass index; DAS28-CRP, Disease Activity Scale 28 with C-Reactive Protein; DMARD, disease-modifying anti-rheumatic drug; HAQ, Health Activity Questionnaire; HS, high school; RA, rheumatoid arthritis; Ref, reference
Statistical Analysis.
We calculated summary statistics for all participant characteristics and outcomes of interest. We examined the association of disease activity and disability with rehabilitation utilization using separate binary logistic regression models to estimate odds ratios and 95% confidence intervals. We adjusted for the potential confounders and also reported the association of these variables with the outcome. We repeated the analyses with the sample stratified by disease duration: early RA (<2 years) and established RA (≥2 years). Separate analyses were carried out in each of the 20 imputed datasets, then estimated parameters from all imputed datasets were synthesized to generate a single estimate according to Rubin’s rules. All tests were two-sided and considered statistically significant at the 0.05 level. All analyses were conducted using the statistical software package SAS version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS.
Of 1067 participants, 14% reported utilizing rehabilitation in the prior 6 months, and 41% reported ever utilizing rehabilitation (Table 1). The proportion of the sample reporting rehabilitation utilization in the prior 6 months was similar among those with early and established RA (12% vs. 16%), however a greater proportion of those with established RA reported any past rehabilitation utilization (28% vs. 50%; p < 0.001).
In the full sample, disease activity was not associated with rehabilitation utilization in the prior 6 months or ever, in unadjusted and adjusted models (Figure 1, Table 2). Worse disability was associated with higher odds of rehabilitation utilization in the prior 6 months or ever in unadjusted models, but only the association with rehabilitation utilization in the last 6 months persisted in the adjusted model. Among the other factors, older age was associated with higher odds of rehabilitation in the prior 6 months in adjusted models, while older age, higher number of comorbidities, and current employment were associated with higher odds of any prior rehabilitation utilization.
Figure 1.
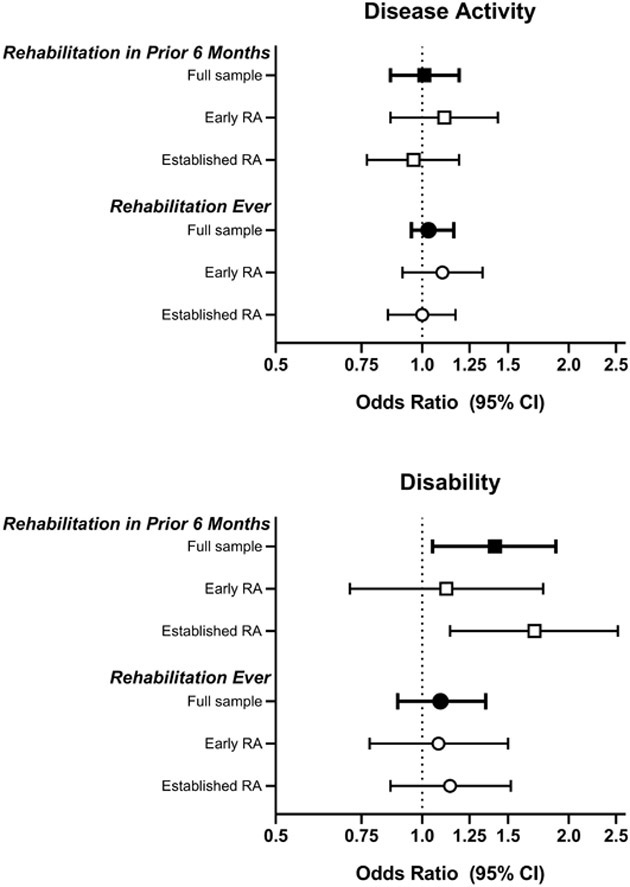
Association of disease activity and disability with rehabilitation utilization in the prior 6 months (squares) and ever (circles) in the full sample (black filled square or circle) and in the stratified samples (white filled square or circle).
Table 2.
Factors associated with rehabilitation utilization in the prior 6 months or ever in the full sample and stratified by RA disease duration
| Utilization in the last 6 months | Utilization ever | |||
|---|---|---|---|---|
| Unadjusted model OR (95% CI) |
Adjusted model OR (95% CI) |
Unadjusted model OR (95% CI) |
Adjusted model OR (95% CI) |
|
| Full Sample | ||||
| Disease Activity (per unit increase in DAS28-CRP) | 1.07 (0.94, 1.22) | 1.01 (0.86, 1.19) | 1.04 (0.95, 1.14) | 1.03 (0.92, 1.16) |
| Disability (per unit increase in HAQ) | 1.40 (1.12, 1.74) | 1.41 (1.05, 1.88) | 1.18 (1.01, 1.38) | 1.09 (0.89, 1.35) |
| Age (per year) | 1.03 (1.02, 1.05) | 1.03 (1.01, 1.05) | 1.03 (1.02, 1.04) | 1.02 (1.01, 1.03) |
| BMI (per 1kg/m2) | 1.02 (0.99, 1.04) | 1.02 (0.99, 1.04) | 1.02 (1.00, 1.03) | 1.02 (1.00, 1.03) |
| Gender (Ref: Women) | 0.91 (0.70, 1.18) | 1.04 (0.78, 1.37) | 0.87 (0.73, 1.04) | 1.02 (0.83, 1.24) |
| Disease duration (per year) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.01 (1.00, 1.01) | 1.00 (1.00, 1.01) |
| Comorbidities (per increase in number) | 1.18 (1.09, 1.27) | 1.07 (0.98, 1.17) | 1.30 (1.22, 1.39) | 1.20 (1.11, 1.29) |
| DMARD use (Ref: yes) | 1.08 (0.86, 1.36) | 1.06 (0.83, 1.35) | 0.94 (0.80, 1.12) | 0.95 (0.79, 1.15) |
| Household income (Ref: <$30k) | 1.02 (0.83, 1.24) | 1.19 (0.94, 1.50) | 0.97 (0.84, 1.12) | 1.14 (0.96, 1.36) |
| Employed (Ref: no) | 1.39 (1.12, 1.73) | 1.18 (0.93, 1.52) | 1.41 (1.23, 1.63) | 1.21 (1.02, 1.43) |
| Education (Ref: > HS) | 0.88 (0.74, 1.05) | 0.84 (0.69, 1.02) | 0.89 (0.79, 1.01) | 0.88 (0.76, 1.02) |
| Early RA Subsample | ||||
| Disease Activity (per unit increase in DAS28-CRP) | 1.08 (0.88, 1.31) | 1.11 (0.86, 1.43) | 1.06 (0.92, 1.22) | 1.10 (0.91, 1.33) |
| Disability (per unit increase in HAQ) | 1.04 (0.75, 1.44) | 1.12 (0.71, 1.77) | 1.08 (0.85, 1.37) | 1.08 (0.78, 1.50) |
| Age (per year) | 1.04 (1.02, 1.07) | 1.05 (1.02, 1.08) | 1.04 (1.02, 1.05) | 1.05 (1.03, 1.07) |
| BMI (per 1kg/m2) | 1.01 (0.97, 1.05) | 1.02 (0.98, 1.06) | 1.02 (0.99, 1.04) | 1.01 (0.98, 1.04) |
| Gender (Ref: Women) | 1.14 (0.78, 1.65) | 1.21 (0.80, 1.21) | 0.94 (0.71, 1.26) | 1.02 (0.74, 1.40) |
| Disease duration (per year) | 0.96 (0.92, 1.01) | 0.97 (0.92, 1.01) | 1.03 (1.00, 1.07) | 1.04 (1.01, 1.08) |
| Comorbidities (per increase in number) | 1.06 (0.91, 1.24) | 0.98 (0.82, 1.16) | 1.17 (1.04, 1.31) | 1.08 (0.95, 1.22) |
| DMARD use (Ref: yes) | 0.85 (0.56, 1.28) | 0.80 (0.52, 1.23) | 0.76 (0.56, 1.02) | 0.72 (0.52, 0.99) |
| Household income (Ref: <$30k) | 1.21 (0.89, 1.64) | 1.23 (0.83, 1.82) | 1.12 (0.89, 1.40) | 1.12 (0.85, 1.50) |
| Employed (Ref: no) | 1.10 (0.81, 1.48) | 1.00 (0.69, 1.45) | 1.07 (0.86, 1.33) | 0.91 (0.70, 1.19) |
| Education (Ref: > HS) | 0.80 (0.60, 1.07) | 0.76 (0.54, 1.08) | 0.81 (0.66, 1.00) | 0.76 (0.60, 0.98) |
| Established RA Subsample | ||||
| Disease Activity (per unit increase in DAS28-CRP) | 1.08 (0.90, 1.29) | 0.96 (0.77, 1.19) | 1.07 (0.94, 1.21) | 1.00 (0.85, 1.17) |
| Disability (per unit increase in HAQ) | 1.93 (1.41, 2.66) | 1.70 (1.14, 2.52) | 1.46 (1.16, 1.82) | 1.14 (0.86, 1.52) |
| Age (per year) | 1.02 (1.00, 1.04) | 1.02 (0.99, 1.04) | 1.02 (1.01, 1.03) | 1.00 (0.99, 1.02) |
| BMI (per 1kg/m2) | 1.02 (0.99, 1.05) | 1.02 (0.99, 1.05) | 1.02 (1.00, 1.04) | 1.02 (0.99, 1.04) |
| Gender (Ref: Women) | 0.76 (0.52, 1.11) | 0.86 (0.57, 1.29) | 0.86 (0.68, 1.09) | 1.01 (0.77, 1.31) |
| Disease duration (per year) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) |
| Comorbidities (per increase in number) | 1.22 (1.11, 1.34) | 1.11 (1.00, 1.24) | 1.34 (1.23, 1.45) | 1.26 (1.15, 1.38) |
| DMARD use (Ref: yes) | 1.28 (0.96, 1.70) | 1.23 (0.91, 1.68) | 1.17 (0.93, 1.48) | 1.19 (0.92, 1.54) |
| Household income (Ref: <$30k) | 0.91 (0.69, 1.21) | 1.11 (0.81, 1.51) | 0.95 (0.78, 1.15) | 1.14 (0.90, 1.44) |
| Employed (Ref: no) | 1.73 (1.21, 2.48) | 1.43 (0.97, 2.10) | 1.54 (1.26, 1.88) | 1.40 (1.10, 1.77) |
| Education (Ref: > HS) | 0.94 (0.75, 1.16) | 0.89 (0.69, 1.14) | 0.94 (0.80, 1.11) | 0.95 (0.78, 1.14) |
Abbreviations: BMI, body mass index; DAS28-CRP, Disease Activity Scale 28 with C-Reactive Protein; DMARD, disease-modifying anti-rheumatic drug; HAQ, Health Activity Questionnaire; HS, high school; Ref, reference
When the results were stratified by disease duration, the association of disability with rehabilitation utilization in the prior 6 months was magnified among those with established RA and was not present in those with early RA (Figure 1, Table 2). Disease activity remained not associated with rehabilitation utilization in both groups and in either time frame. Among participants with early RA, older age was associated with rehabilitation utilization in the prior 6 months and any prior rehabilitation utilization in unadjusted and adjusted models. In addition, higher number of comorbidities was associated with any prior rehabilitation in the unadjusted model only, while longer disease duration, DMARD use, and more than high school graduation were associated with higher odds of any prior rehabilitation utilization in the adjusted model only. Among participants with established RA, a higher number of comorbidities and current employment were associated with both outcomes in the unadjusted models, and remained associated with any prior rehabilitation utilization in the adjusted model. Older age was associated with any prior rehabilitation utilization in the unadjusted model only.
DISCUSSION.
Contrary to our hypothesis, disease activity was not associated with rehabilitation utilization in the prior 6 months or any prior rehabilitation utilization in the full sample. In partial support of our hypothesis, worse disability was associated with rehabilitation utilization in the prior 6 months or ever, however only the association with utilization in the prior 6 months persisted in the adjusted model. This remained true among those with established RA, but not among those with early RA. Iversen et al. also previously reported that worse function and disability were associated with higher odds for physical therapy utilization in the prior 6 months. In contrast to our findings, Iversen et al. reported greater disease activity was associated with rehabilitation utilization, though they used a different measure of disability (Rheumatoid Arthritis Disease Activity Index; RADAI) which may contribute to the discrepancy.(5) Additionally, function was not significantly associated when considered alongside disease activity and disability.(5) Considerable differences in sample characteristics may also account for some of the discrepancy, as their sample was predominantly white with higher socioeconomic status and less comorbidity.(5) Taken together, it remains unclear why and when rehabilitation is utilized for African-American adults with RA, though disability is a contributor in those with established disease.
Beyond a description of factors associated with rehabilitation utilization, this analysis was the first to shed light on rehabilitation utilization reported among African Americans with RA. In the CLEAR I and II cohorts, 14% of participants reported utilizing either PT or OT in the prior 6 months. It remains unclear if this rehabilitation utilization is different than white adults with RA. Iversen et al.(5) reported 15% of adults with RA utilized PT in the 6 month period; OT utilization was not included in the estimate. Thus, it is unclear how overall rehabilitation utilization compares between the samples, with differences in sample characteristics notwithstanding. Sandstrom et al. reported that Black adults with arthritis were 34% less likely to utilize office-based therapy compared to non-Black/non-Hispanic adults with arthritis, however the type of arthritis (RA vs. osteoarthritis) and type of office-based therapy (PT vs. OT vs. other) was not specified in this analysis.(6) Further research is needed to understand the extent to which disparities exist regarding rehabilitation utilization for adults with RA.
Despite consistent recommendations for rehabilitation and exercise in the management of RA(4), rehabilitation utilization was low. In the CLEAR I and II cohorts, lifetime rehabilitation utilization (i.e., any prior utilization) was 41%, and 48% among those with established RA and a median disease duration of nearly 10 years. These are likely overestimates of actual rehabilitation utilization for RA as participants may have reported rehabilitation utilization for problems that were unrelated to RA, such as after a sport injury. Overall, these results are consistent with previous reports that rehabilitation utilization over one year is lower in the United States (24%(5, 12)) compared to other countries (40-46%(13, 14)). Reasons for this difference in rehabilitation utilization are unclear.
The results of this study and prior studies suggest rehabilitation is potentially underutilized in RA management for adults in the United States. Disability and functional limitation remain a prevalent issue among adults with RA, despite considerable improvements in disease management and joint preservation with the proliferation of DMARDs and biologics drugs.(1-3) As a complement to pharmacologic strategies, rehabilitation is needed to address disability and functional limitation. Prior analyses in CLEAR indicated that socioeconomic disparities in disease activity, disability, and other self-reported health outcomes exist among African Americans with RA.(15) Higher household income was associated with rehabilitation utilization in the prior 6 months and current employment was associated with any prior rehabilitation utilization in this analysis (Table 2), which may further contribute to these health disparities. Future research must consider barriers to accessing rehabilitation and advance approaches to integrating rehabilitation into routine RA care in the United States to preserve function and delay disability in adults with RA.
The results should be considered in light of several limitations. First, rehabilitation utilization estimates used self-reported recall, combined PT and OT, and were not necessarily specific to RA as the participants may have seen a rehabilitation professional for problems other than RA. Analyses of administrative and electronic medical record data are needed to more accurately estimate PT and OT utilization for clinical issues related to RA. Other variables, such as comorbidities and medications, were also based on self-reported recall. This analysis was cross-sectional, so causality cannot be inferred. Rehabilitation utilization preceded the measures of disease activity and disability, so we cannot exclude the possibility that these clinical measures improved following rehabilitation. The CLEAR cohort includes participants recruited from academic medical centers in the southeastern US in the early 2000s, which may limit generalizability beyond the region and practice type, as well as to current clinical practice. Biologics were an emerging treatment in the early 2000s and their use was likely not consistent across institutions or across the enrollment period. It is unclear how this could affect referral to rehabilitation, though we know that functional limitations remain a prevalent consequence of RA in the era of biologics.(1, 3). Finally, we did not have information regarding insurance coverage, location, transportation availability, which may impact rehabilitation utilization.
CONCLUSION.
Among African Americans with RA, rehabilitation utilization was low (14%) in the 6 months prior to enrollment into CLEAR, was not associated with disease activity, and was only associated with disability among those with established disease. Factors driving rehabilitation utilization in African Americans with RA remain unclear and should be a focus of future research to facilitate delivery of appropriate and effective rehabilitation services.
Supplementary Material
SIGNIFICANCE & INNOVATIONS:
This is the first report of rehabilitation utilization among African American adults with RA in the United States
Rehabilitation utilization was low among African Americans adults with RA
Rehabilitation utilization was associated with disability but not disease activity, particularly in adults with established RA
ACKNOWLEDGEMENTS.
The authors thank the following investigators in the Consortium for the Longitudinal Evaluation of African Americans with Rheumatoid Arthritis (CLEAR): Doyt Conn, MD – Emory University School of Medicine; Richard Brasington, MD – Washington University School of Medicine; Larry W. Moreland, MD - University of Colorado University of Colorado School of Medicine. We are also very grateful to the participants in the CLEAR Registry.
FUNDING:
CLEAR registry supported by NIH contract N01-AR-02247; other support NIH/NIAMS Office of Research on Women's Health grant R01-AR056717-02 and P30AR072580.
REFERENCES.
- 1.Andersson MLE, Forslind K, Hafström I. Patients with Early Rheumatoid Arthritis in the 2000s Have Equal Disability and Pain Despite Less Disease Activity Compared with the 1990s: Data from the BARFOT Study over 8 Years. The Journal of Rheumatology. 2017;44(6):723–31. [DOI] [PubMed] [Google Scholar]
- 2.Hallert E, Bjork M, Dahlstrom O, Skogh T, Thyberg I. Disease activity and disability in women and men with early rheumatoid arthritis (RA): an 8-year followup of a Swedish early RA project. Arthritis Care Res (Hoboken). 2012;64(8):1101–7. [DOI] [PubMed] [Google Scholar]
- 3.Carpenter L, Barnett R, Mahendran P, Nikiphorou E, Gwinnutt J, Verstappen S, et al. Secular changes in functional disability, pain, fatigue and mental well-being in early rheumatoid arthritis. A longitudinal meta-analysis. Semin Arthritis Rheum. 2020;50(2):209–19. [DOI] [PubMed] [Google Scholar]
- 4.Excellence NIfHaC. Rheumatoid arthritis in adults: management. NICE; 2018. [Google Scholar]
- 5.Iversen MD, Chhabriya RK, Shadick N. Predictors of the Use of Physical Therapy Services Among Patients With Rheumatoid Arthritis. Physical Therapy. 2011;91(1):65–76. [DOI] [PubMed] [Google Scholar]
- 6.Sandstrom R, Bruns A. Disparities in Access to Outpatient Rehabilitation Therapy for African Americans with Arthritis. Journal of Racial and Ethnic Health Disparities. 2017;4(4):599–606. [DOI] [PubMed] [Google Scholar]
- 7.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24. [DOI] [PubMed] [Google Scholar]
- 8.Wells G, Becker JC, Teng J, Dougados M, Schiff M, Smolen J, et al. Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythr. Annals of the Rheumatic Diseases. 2009;68(6):954–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.England BR, Tiong BK, Bergman MJ, Curtis JR, Kazi S, Mikuls TR, et al. 2019 Update of the American College of Rheumatology Recommended Rheumatoid Arthritis Disease Activity Measures. Arthritis Care Res (Hoboken). 2019;71(12):1540–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis & Rheumatism. 1980;23(2):137–45. [DOI] [PubMed] [Google Scholar]
- 11.Lane CY, Givens DL, Thoma LM. General Functional Status: Common Outcome Measures for Adults With Rheumatic Disease. Arthritis Care & Research. 2020;72(S10):431–51. [DOI] [PubMed] [Google Scholar]
- 12.Desai RJ, Solomon DH, Weinblatt ME, Shadick N, Kim SC. An external validation study reporting poor correlation between the claims-based index for rheumatoid arthritis severity and the disease activity score. Arthritis research & therapy. 2015;17(1):83–. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huscher D, Mittendorf T, von Hinuber U, Kotter I, Hoese G, Pfafflin A, et al. Evolution of cost structures in rheumatoid arthritis over the past decade. Ann Rheum Dis. 2015;74(4):738–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobi CE, Triemstra M, Rupp I, Dinant HJ, van den Bos GAM. Health care utilization among rheumatoid arthritis patients referred to a rheumatology center: unequal needs, unequal care? Arthritis Care & Research. 2001;45(4):324–30. [DOI] [PubMed] [Google Scholar]
- 15.Baldassari AR, Cleveland RJ, Jonas BL, Conn DL, Moreland LW, Bridges SL Jr., et al. Socioeconomic disparities in the health of african americans with rheumatoid arthritis from the southeastern United States. Arthritis Care Res (Hoboken). 2014;66(12):1808–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


