Summary
Sinonasal teratocarcinosarcoma is a rare aggressive malignant tumor with a primary setting involving the nasal cavity followed by the ethmoid sinus and maxillary sinus. It accounts for approximately 3% of all head and neck cancers and less than 1% of all tumors. Nasal obstruction, recurrent epistaxis and headache represent the typical clinical presentation. Imaging shows the presence of a mass in the nasal cavity. The treatment usually consists of surgery and adjuvant intensity modulated radiotherapy. The rarity and the variability of the histological features make its diagnosis particularly difficult.
In this paper, we report a case of sinonasal teratocarcinosarcoma in a 62-year-old male treated with a multidisciplinary approach. As an alternative to intensity modulated radiotherapy, we proposed proton beam therapy for the first time. The patient benefited from the new and personalized protocol that provided excellent results and few adverse effects. At 45 months follow-up there is no evidence of relapse and the patient is in good health.
Key words: teratocarcinosarcoma, paranasal sinus neoplasm, radiotherapy, proton therapy
Introduction
Sinonasal teratocarcinosarcoma (SNTCS) is a malignant tumor with an aggressive behavior, a poor prognosis, a high risk of recurrence and poor survival 1. It arises in the nasal cavity, involving the ethmoid sinus in half of the patients and the maxillary sinus in a quarter of patients. Primary settings in the nasopharynx and oral cavity have also been reported. Moreover, an intracranial extension is also possible given the aggressive nature of the disease. SNTCS is a rare malignancy with 127 cases reported in the literature 2-3. It was first described in 1983 by Shanmugaratnam with the name of “carcinosarcoma”. Only a year later Heffner and Hyams coined the term “teratocarcinosarcoma” 4 and from 2005 it is recognized as a distinct entity in the WHO Classification of Head and Neck Tumors 1,6, representing approximately 3% of all malignancies of the region and less than 1% of all cancers. Patients (7:1 male to female ratio) are generally middle-aged men with a mean age at diagnosis of 54.5 years 1. The typical onset consists of nasal obstruction, recurrent epistaxis and headache. Neurological symptoms are rare and reported only in case of intracranial extension. The etiopathogenesis is still unknown.
Histologically they are heterogeneous lesions characterized by cells of different embryonic derivation (ectodermal, mesodermal and endodermal), in multiple degrees of differentiation 4. The most widely used therapeutic approach is a combination of surgery and adjuvant intensity modulated radiotherapy (IMRT), but there are no official guidelines or consensus 7. As an alternative to IMRT, proton beam therapy (PBT) is nowadays used to treat several head and neck tumors. In this report, the use of PBT for the treatment of a stage 3 SNTCS is discussed. It represents the first application to the best of our knowledge.
Case report
In June 2017, a 62-year-old male came to the Emergency Unit of the San Paolo Hospital (Milan) reporting a 12 hours unstoppable right-sided epistaxis. The patient experienced recurrent episodes of sinusitis, epistaxis, nasal obstruction, cacosmia and headache in the last four months. The symptoms were progressive and refractory to medical therapy. The patient stopped smoking in January 2017 (history of 4 cigarettes/day for 20 years - 4 pack/year history). Physical examination and the routine blood tests were non-contributory. During ear, nose and throat (ENT) examination, nasal endoscopy was performedwhich revealed a large mass in the right nasal cavity (Fig. 1A, 1B). A computed tomography (CT) scan with contrast showed that the mass completely obliterated the right nasal cavity and maxillary sinus, extending to the nasopharynx; the remain sinuses were uninvolved and no intracranial extension was identified (Fig. 1C). Endoscopic sinus surgery (ESS) with radical intent was performed. The intraoperative examination was inconclusive for the histological diagnosis, although margins were negative. The patient was discharged at day 1 in good health.
Figure 1.
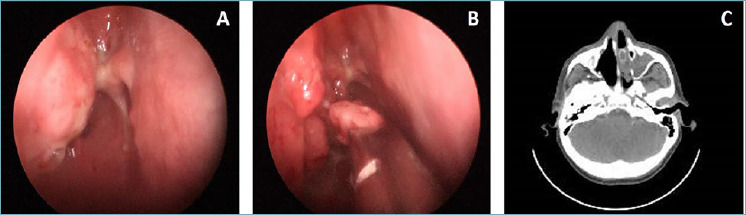
(A) Flexible fiber optic endoscopy shows the polypoidal mass in the right nasal cavity. (B) Biopsy performed during endoscopic sinus surgery (ESS). (C) Pre-surgical maxillo-facial CT shows a mass that completely obliterates the right nasal cavity, the ipsilateral maxillary sinus, and expands posteriorly toward the right nasopharynx.
Histologic examination revealed a heterogeneous admixture of epithelial, mesenchymal and neuroectodermal components. The first varied from small rounded elements, partly organized in solid nests with peripheral palisade cells (Fig. 2A), sometimes with clear cytoplasm, to elements with squamous differentiation and shadow cells (Fig. 2B). There were micro-cystic and cystic formations, some of which with necrotic centers, and more rarely tubule/glandular structures, sometimes with ciliated cylindrical epithelium. The mesenchymal component was for the most part made up of rhabdomyoblastic elements (Fig. 3A) with the typical streak (Fig. 3B), with atypia from mild to moderate and some atypical mitosis. Finally, there were spindle elements of medium size which tended to crowd around the epithelial structures, mixed with fibro-mixoid areas. Necrosis and hemorrhage were present in about 30% of the sample. Neuroepithelium and elements of neuroectodermal origin were not clearly detectable based on hematoxylin and eosin staining.
Figure 2.
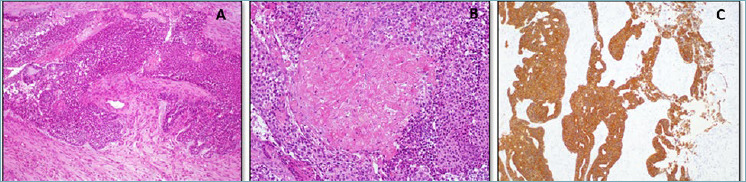
(A) Epithelial component, histology; small rounded elements partly organized in solid nests and peripheral palisade cells (H-E; 4x). (B) Epithelial component, histology; there are elements with different degrees of squamous differentiation and shadow cells (H-E; 10x). (C) Epithelial component, immunohistochemistry; it is positive for cytokeratins (AE1/AE3, Monoclonal mouse; DAKO; ready to use).
Figure 3.
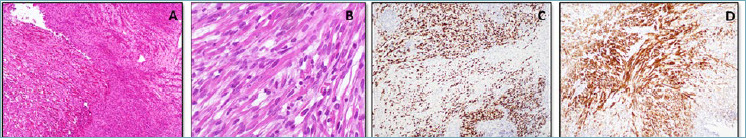
(A) Mesenchymal component, histology; it is for the most part made up of rhabdomyoblastic elements (H-E; 10x). (B) Mesenchymal component, histology; rhabdomyoblastic elements with the typical streak (H-E; 40x). (C) Mesenchymal component, immunohistochemistry; rhabdomyosarcoumatous component positive for myogenin (F5D, Monoclonal mouse; DAKO; ready to use). (D) Mesenchymal component, immunohistochemistry; rhabdomyosarcoumatous component positive for desmin (D33, Monoclonal mouse; DAKO; ready to use).
Immunohistochemistry revealed positivity for myogenin (Fig. 3C) and desmin (Fig. 3D) in the rhabdomyosarcomatous component and pan-cytokeratin positivity in the epithelial component (Fig. 2C). The spindle elements crowded around the epithelial structures were GFAP positive (Fig. 4A, 4B).
Figure 4.
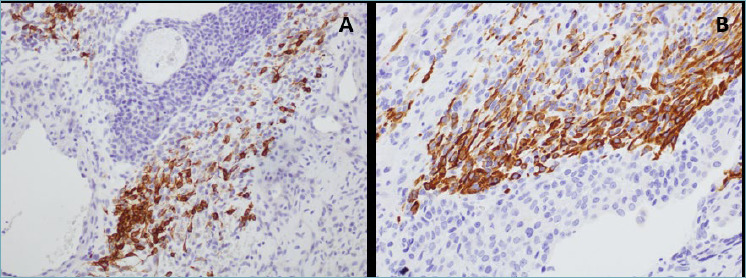
(A, B) Neuroectodermal component, immunohistochemistry; spindle elements crowded around the epithelial structures GFAP positive (6F2, Monoclonal mouse; DAKO).
The combination of morphology and immunohistochemistry made possible the final diagnosis of teratocarcinosarcoma.
Two months after resection, positron emission tomography (PET) examination revealed an accumulation of radiopharmaceutical at the level of the right nasal fossa, confirmed by magnetic resonance imaging (MRI). A subsequent ENT evaluation revealed a polypoid lesion of the right posterior ethmoid sinus. Histologic examination confirmed a residual SNTCS. A multidisciplinary treatment approach was planned and the patient underwent 33 PBT sessions. Treatment was administered 5 days a week from January to March 2018 at Centro Nazionale di Adroterapia Oncologica (CNAO) in Pavia (Italy). The patient received 66 Gy in 2 Gy daily fractions and the radiation dose delivered to the adjacent healthy tissue did not exceed 5 Gy. In January 2019 (18 months after diagnosis), a follow-up PET examination was performed with no evidence of recurrence. In April 2020 (34 months after diagnosis), the patient underwent a head and neck MRI, which was negative for relapse or nodal metastases. During the treatment the patient reported loss of the right eyebrow and beard, actinic rhinitis and hyposmia (the latter only in the last two weeks of treatment). To date (45 months after diagnosis), the patient has only moderate post-actinic vestibulitis.
Discussion
SNTCS is an extremely rare malignant tumor mostly located in maxillary and ethmoid sinus (50% and 25% respectively) 1,8. Orbit, oral cavity, pharynx and anterior cranial fossa are rare localizations, while bone erosion and extracranial extension are anecdotal, especially at onset 9. Moreover, intracranial extension is also possible.
Macroscopically, these tumors present as bulky reddish masses. Histologically, epithelial, mesenchymal and neuroectodermal components include the teratoid component of the tumor 10. The epithelial structures can vary from poorly differentiated cell nests to well differentiated squamous cells with formation of horny pearls and glands focally containing mucin. The “fetal-appearing” squamous epithelium is a common feature, consisting in squamous cells with clear cytoplasm. It has been described in the literature in about 50% 8 to 75% 5 of the tumors. The mesenchymal component can be composed of cartilage, bone, striated muscle and smooth muscle, usually with cytologic atypia and immaturity 10. The neuroectodermal component can be organized into rosettes and pseudorosettes 9,12.
The rarity of the tumor and the microscopic variability make the diagnosis difficult and challenging. A combination of carcinosarcoma and teratoma are required 10 and immunohistochemistry is fundamental to support the diagnosis. The epithelial component shows positivity for pan-cytokeratins, the neuroectodermal elements show variable positivity for GFAP, S-100, NSE, CD99, chromogranin and synaptophysin and the mesenchymal component results positive for vimentin and/or myogenin and/or desmin 8. SNTCS should be put in the differential diagnosis with multiple malignancies including poorly differentiated squamous carcinoma, sarcomas, malignant craniopharyngioma, small cell carcinoma and undifferentiated sinus carcinoma, from which it differs in the coexistence of carcinomatous, sarcomatoid and neuroectodermal elements. SNTCS for its typical undifferentiated round-shaped cells mimics the olfactory neuroblastoma; these two tumors have a similar neuroectodermal differentiation, but they can be distinguished by the evident epithelial differentiation and by the presence of neoplastic mesenchymal components that characterize SNTCS. Another possible differential diagnosis is with malignant teratoma, but it should be considered that teratomas are mainly found in the reproductive system and in other parts of the body (mediastinum, retroperitoneum), while the location of teratocarcinosarcoma is well-defined in the head and neck district. Furthermore, malignant teratoma lacks immature squamous cell nests (clear cell nests or blastic cells) and does not have carcinomatous features 12. Carcinosarcoma is distinguished because this tumor consists of a single malignant epithelial component and a single malignant mesenchymal component 8. Moreover, it is important to put in differential diagnosis lymphoma and melanoma, but the negativity for the specific tumor markers excludes these entities. Considering all these possible differential diagnoses, it is easy to understand how biopsy specimens of limited dimensions may represent a problem for the diagnosis, either for the insufficient representativeness of the sample and for insufficient material necessary for immunohistochemistry.
The most relevant review of SNTCS was published in 2014 by Misra and colleagues 1, who identified surgery and neoadjuvant IMRT as the most common treatment (survival rate of 56.5% and relapse rate of 26.1%). Among radiation treatments, PBT has a promising potential in disease control in patients with head and neck cancer, particularly sinonasal cancer 13. PBT has fewer side effects and improves quality of life. Hence, its use has increased in recent years and it shows a potential superiority over classical photon therapy, reducing toxicity and side effects 13. PBT is a type of external radiotherapy that produces a concentrated proton beam focused on a specific target 14. The main characteristic of protons is the absence of an exit dose outside the target and a sharper lateral dose distribution due to the heavier mass of the protons. This distinguishes proton therapy from conventional photon therapy 13. Several studies report on dose reduction to non-target structures, preservation of normal tissues and potential improvement in tumor control in patients receiving proton beam therapy compared to patients receiving conventional radiotherapy 14-18. However, proton therapy has some limitations including limited availability and costs (2-3 times higher than traditional radiotherapy) 19-25. Due to the benefits of PBT and its efficacy on other sinonasal tumors 26-28, our group decided to propose it to the patient. More than 40 months after diagnosis, our patient is in good health, ESS and PBT have been well tolerated and there are no signs of recurrence or metastases.
Conclusions
SNTCS is an aggressive tumor often misdiagnosed due to its rarity, histologic complexity and variability. Recent studies demonstrate how a combined approach with surgery followed by radiotherapy and chemotherapy can improve the prognosis. Further studies are needed with a larger sample size for a better understanding of the best multidisciplinary management of the disease. It would be also interesting to investigate the positive outcomes that proton therapy can have when substituted to conventional radiation therapy, improving the survival rate and limiting the side effects of radiation in selected patients.
Figures and tables
Acknowledgements
We would like to thank Dr. Laura Moneghini, which contribution was precious to achieve this difficult diagnosis.
References
- 1.Misra P, Husain Q, Svider PF, et al. Management of sinonasal teratocarcinosarcoma: Asystematic review. Am J Otolaryngol 2014;35:5-11. https://doi.org/10.1016/j.amjoto.2013.04.010. Epub 2013 Jun 2. 10.1016/j.amjoto.2013.04.010 [DOI] [PubMed] [Google Scholar]
- 2.Budrukkar A, Agarwal JP, Kane S, et al. Management and clinical outcome of sinonasal teratocarcinosarcoma: single institution experience. J Laryngol Otol 2010;124:739-743. https://doi.org/10.1017/S0022215109992866. Epub 2010 Feb 16. 10.1017/S0022215109992866 [DOI] [PubMed] [Google Scholar]
- 3.Chapurin N, Totten DJ, Morse JC, et al. Treatment of sinonasal teratocarcinosarcoma: a systematic review and survival analysis. Am J Rhinol Allergy 2020:1945892420959585. https://doi.org/10.1177/1945892420959585. Epub ahead of print. 10.1177/1945892420959585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanmugaratnam K, Kunaratnam N, Chia KB, et al. Teratoid carcinosarcoma of the paranasal sinuses. Pathology 1983;15:413-419. https://doi.org/10.3109/00313028309085168 10.3109/00313028309085168 [DOI] [PubMed] [Google Scholar]
- 5.Heffner DK, Hyams VJ. Teratocarcinosarcoma (malignant teratoma?) of the nasal cavity and paranasal sinuses. A clinicopathologic study of 20 cases. Cancer 1984;53:2140-2154. https://doi.org/10.1002/1097-0142(19840515)53:10<2140::aid-cncr2820531025>3.0.co;2-y [DOI] [PubMed] [Google Scholar]
- 6.Cardesa A, Luna MA. Sinonasal teratocarcinosarcoma. In: Barnes L, Eveson JD, Reichart P, Sidransky D, eds. World Health Organization Classification of Tumors. Pathology and Genetics of Head and Neck Tumors. Lyon: IARC Press, 2005. pp. 76-77. [Google Scholar]
- 7.Tandon S, Gairola M, Ahlawat P, et al. Sinonasal teratocarcinosarcoma treated with surgery followed by volumetric modulated radiotherapy: a case report with review of literature. Radiat Oncol J 2018;36:341-347. doi:10.3857/roj.2018.00304. 10.3857/roj.2018.00304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pai SA, Naresh KN, Masih K, et al. Teratocarcinosarcoma of the paranasal sinuses: a clinicopathologic and immunohistochemical study. Hum Pathol 1998;29:718-722. https://doi.org/10.1016/s0046-8177(98)90281-7 10.1016/s0046-8177(98)90281-7 [DOI] [PubMed] [Google Scholar]
- 9.Smith SL, Hessel AC, Luna MA, et al. Sinonasal teratocarcinosarcoma of the head and neck: A report of 10 patients treated at a single institution and comparison with reported series. Arch Otolaryngol Head Neck Surg 2008;134:592-595. https://doi.org/10.1001/archotol.134.6.592 10.1001/archotol.134.6.592 [DOI] [PubMed] [Google Scholar]
- 10.Wei S, Carroll W, Lazenby A, et al. Sinonasal teratocarcinosarcoma: report of a case with review of literature and treatment outcome. Ann Diagn Pathol 2008;12:415-425. https://doi.org/10.1016/j.anndiagpath.2007.05.003. Epub 2007 Oct 24. 10.1016/j.anndiagpath.2007.05.003 [DOI] [PubMed] [Google Scholar]
- 11.Salem F, Rosenblum MK, Jhanwar SC, et al. Teratocarcinosarcoma of the nasal cavity and paranasal sinuses: Report of 3 cases with assessment for chromosome 12p status. Hum Pathol 2008; 39:605-609. https://doi.org/10.1016/j.humpath.2007.09.002. Epub 2008 Mar 4. 10.1016/j.humpath.2007.09.002 [DOI] [PubMed] [Google Scholar]
- 12.Yang S, Sun R, Liang J, et al. Sinonasal teratocarcinosarcoma: a clinical and pathological analysis. Int J Surg Pathol 2013;21:37-43. https://doi.org/10.1177/1066896912457202. Epub 2012 Aug 24. 10.1177/1066896912457202 [DOI] [PubMed] [Google Scholar]
- 13.Blanchard P, Gunn GB, Lin A, et al. Proton therapy for head and neck cancers. Semin Radiat Oncol 2018;28:53-63. https://doi.org/10.1016/j.semradonc.2017.08.004 10.1016/j.semradonc.2017.08.004 [DOI] [PubMed] [Google Scholar]
- 14.Kim JK, Leeman JE, Riaz N, et al. Proton therapy for head and neck cancer. Curr Treat Options Oncol 2018;19:28. https://doi.org/10.1007/s11864-018-0546-9 10.1007/s11864-018-0546-9 [DOI] [PubMed] [Google Scholar]
- 15.Kandula S, Zhu X, Garden AS, et al. Spot-scanningbeamprotontherapy vs intensity-modulated radiation therapy for ipsilateral head and neck malignancies: a treatment planning comparison. Med Dosim 2013;38:390-394. https://doi.org/10.1016/j.meddos.2013.05.001. Epub 2013 Aug 2 10.1016/j.meddos.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 16.Holliday EB, Kocak-Uzel E, Feng L, et al. Dosimetric advantages of intensity-modulated proton therapy for oropharyngeal cancer compared with intensity-modulated radiation: a case-matched control analysis. Med Dosim 2016;41:189-194. [DOI] [PubMed] [Google Scholar]
- 17.Apinorasethkul O, Kirk M, Teo K, et al. Pencil beam scanning proton therapy vs rotational arc radiation therapy: A treatment planning comparison for postoperative oropharyngeal cancer. Med Dosim 2017;42:7-11. https://doi.org/10.1016/j.meddos.2016.09.004. Epub 2016 Nov 7. 10.1016/j.meddos.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 18.Eekers DBP, Roelofs E, Jelen U, et al. Benefit of particle therapy in reirradiation of head and neck patients. Results of a multicentric in silico ROCOCO trial. Radiother Oncol 2016;121:387-394. https://doi.org/10.1016/j.radonc.2016.08.020. Epub 2016 Sep 14. 10.1016/j.radonc.2016.08.020 [DOI] [PubMed] [Google Scholar]
- 19.Ramaekers BLT, Grutters JPC, Pijls-Johannesma M, et al. Protons in head- and-neck cancer: bridging the gap of evidence. Int J Radiat Oncol Biol Phys 2013;85:1282-1288. https://doi.org/10.1016/j.ijrobp.2012.11.006. Epub 2012 Dec 27 10.1016/j.ijrobp.2012.11.006 [DOI] [PubMed] [Google Scholar]
- 20.Pommier P, Zucca L, Näslund I, et al. Light ion facility projects in Europe: methodological aspects for the calculation of the treatment cost per protocol. Radiother Oncol. 2004;73 Suppl 2:S183-5. https://doi.org/10.1016/s0167-8140(04)80045-8 10.1016/s0167-8140(04)80045-8 [DOI] [PubMed] [Google Scholar]
- 21.Lundkvist J, Ekman M, Ericsson SR, et al. Proton therapy of cancer: potential clinical advantages and cost-effectiveness. Acta Oncol 2015;44:850-861. https://doi.org/10.1080/02841860500341157 10.1080/02841860500341157 [DOI] [PubMed] [Google Scholar]
- 22.Pijls-Johannesma M, Pommier P, Lievens Y. Cost-effectiveness of particle therapy: current evidence and future needs. Radiother Oncol 2008;89:127-134. https://doi.org/10.1016/j.radonc.2008.07.015. Epub 2008 Aug 15 10.1016/j.radonc.2008.07.015 [DOI] [PubMed] [Google Scholar]
- 23.Peeters A, Grutters JPC, Pijls-Johannesma M, et al. How costly is particle therapy? Cost analysis of external beam radiotherapy with carbon-ions, protons and photons. Radiother Oncol 2010;95:45-53. https://doi.org/10.1016/j.radonc.2009.12.002. Epub 2010 Jan 26 10.1016/j.radonc.2009.12.002 [DOI] [PubMed] [Google Scholar]
- 24.Pommier P, Lievens Y, Feschet F, et al. Simulating demand for innovative radiotherapies: an illustrative model based on carbon ion and proton radiotherapy. Radiother Oncol 2010;96:243-249. https://doi.org/10.1016/j.radonc.2010.04.010. Epub 2010 May 7 10.1016/j.radonc.2010.04.010 [DOI] [PubMed] [Google Scholar]
- 25.Thaker NG, Frank SJ, Feeley TW. Comparative costs of advanced proton and photon radiation therapies: Lessons from time-driven activity- based costing in head and neck cancer. J Comp Eff Res 2015; 4:297-301. https://doi.org/10.2217/cer.15.32 10.2217/cer.15.32 [DOI] [PubMed] [Google Scholar]
- 26.Romesser PB, Cahlon O, Scher E, et al. Proton beam radiation therapy results in significantly reduced toxicity compared with intensity-modulated radiation therapy for head and neck tumors that require ipsilateral radiation. Radiother Oncol 2016;118:286-292. https://doi.org/10.1016/j.radonc.2015.12.008. Epub 2016 Feb 8 10.1016/j.radonc.2015.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDonald MW, Liu Y, Moore MG, Johnstone PA. Acute toxicity in comprehensive head and neck radia- tion for nasopharynx and paranasal sinus cancers: cohort comparison of 3D conformal proton therapy and intensity modulated radiation therapy. Radiat Oncol 2016;11:32. https://doi.org/10.1186/s13014-016-0600-3 10.1186/s13014-016-0600-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel SH, Wang Z, Wong WW, et al. Charged particle therapy versus photon therapy for paranasal sinus and nasal cavity malignant diseases: a systematic review and meta-18. analysis. Lancet Oncol 2014;15:1027-1038. https://doi.org/10.1016/S1470-2045(14)70268-2. Epub 2014 Jun 26. 10.1016/S1470-2045(14)70268-2 [DOI] [PubMed] [Google Scholar]


