Abstract
Objectives:
To describe indications for scleral contact lens (ScCL) evaluation, previous treatments, and outcomes of patients prescribed ScCL at a tertiary referral center.
Methods:
This retrospective study reviewed 133 patients evaluated for ScCL between January 1, 2010, and December 31, 2015, at the University of Illinois at Chicago (UIC) Contact Lens Service. Patient demographics, ocular history, indications for evaluation, previous treatments, presence of punctate epithelial erosions, number of lenses ordered, follow-up visits, best-corrected visual acuity before ScCL, and visual acuity with ScCL were evaluated. Patients were categorized based on primary indication for ScCL evaluation as ocular surface disease (OSD) or corneal irregularity (CI). The primary outcome was visual acuity.
Results:
Visual acuity improved from logarithm of the minimal angle of resolution 0.3±0.4 at presentation to 0.1±0.2 with ScCL in all eyes (n=223, P=0.0001), and from 0.3±0.5 to 0.1±0.2 (n=164, P=0.001) in the OSD group and 0.5±0.4 to 0.2±0.2 (n=59, P=0.0001) in the CI group. Seventy percent of patients were evaluated for bilateral ScCL evaluation. Indication for ScCL evaluation was OSD in 71% (n=95) of patients, with 20% having a secondary diagnosis of CI. Corneal irregularity was the primary diagnosis in 29% of patients (n=38), with 50% having a secondary diagnosis of OSD.
Conclusions:
Ocular surface disease was common in this tertiary referral patient population and was a primary or secondary indication for ScCL evaluation in 85.7% (n=114) of patients evaluated for ScCL. Scleral contact lenses improved visual outcomes in patients with both primary diagnoses of CI and OSD.
Keywords: Corneal irregularity, Keratoconus, Ocular surface disease, Scleral contact lens
Scleral contact lenses (ScCL) are important tools in the management of ocular surface disease (OSD) and corneal irregularity (CI) when other management options fail. With the increase in available lens designs in recent years, their use continues to become more widespread. A ScCL provides a smooth front surface, masking irregular corneal astigmatism and improving visual quality, benefiting patients with corneal scarring, postkeratoplasty, or corneal ectasia from keratoconus or pellucid marginal degeneration.1 In addition, they are therapeutic for patients with severe keratoconjunctivitis sicca because they provide protection from dryness and mechanical factors while the tear reservoir continuously lubricates the eye.2
Recent studies have reported ScCL fitting trends. In 2015, ScCL prescribers surveyed by the SCOPE study group estimated they were fitting 74% of their patients for CI, 16% for OSD, and 10% for uncomplicated refractive error.3 A follow-up 2017 cross-sectional study reported an even higher rate of 87% of ScCL fittings for the management of CI and only 8% for OSD.3,4 In this study, we describe patient characteristics, indications for ScCL evaluation, previous treatments, and outcomes of patients at a hospital-based tertiary referral center.
METHODS
This retrospective cohort study reviewed 133 patients who were evaluated for and ordered ScCL between January 1, 2010, and December 31, 2015, at the University of Illinois at Chicago (UIC) Illinois Eye and Ear Infirmary. All patients were fit in-office with a trial ScCL before lens ordering. Individuals were fit with commercial lenses (Jupiter lens design; Essilor Contact Lenses, Dallas, TX) or The BostonSight PROSE (Boston Foundation for Sight; Needham, MA). Patient demographics, ocular history, indications for evaluation, previous treatments, clinical findings, number of devices ordered, number of follow-up visits, best-corrected visual acuity before ScCL, and visual acuity with ScCL were examined. Inclusion criteria included new evaluation and dispensing of ScCL. This study was approved by the University of Illinois at Chicago Institutional Review Board.
Patients were categorized by primary indication for evaluation as OSD or CI. In patients with both OSD and CI, the primary indication was determined by the patient’s ocular history, chief complaint, and treatment goals. The primary outcome for both OSD and CI groups was visual acuity. Visual acuity was measured using a projected Snellen acuity chart and converted to logarithm of the minimal angle of resolution (logMAR) for data analysis. A secondary outcome was the presence or absence of punctate epithelial erosions. The CI group was further categorized by severity (mild <45D, moderate 45–52D, and steep >52D) based on the CLEK study keratometry criteria.5 Data were analyzed using SAS Institute Inc 2018 (SAS 9.4M6, Cary, NC). Descriptive statistics as well as t tests and one-way analysis of variance tests were used to compare variables with a significance level of 0.05.
RESULTS
Mean patient age at presentation was 49 years (range 18–87; Table 1). About half of patients presenting for new ScCL evaluations were male (52%) and the majority were Caucasian (74%). Seventy percent of patients were evaluated for bilateral ScCL evaluation. Visual acuity improved from logMAR 0.3±0.4 at presentation to 0.1±0.2 with ScCL in all eyes (n=223, P=0.0001; Table 2). There were 95 patients with a primary indication of OSD, 38 patients with CI, and none with uncomplicated refractive error. Ocular surface disease was a primary or secondary indication for ScCL evaluation in 85.7% (n=114) of patients evaluated for ScCL. The percentage of patients with corneal punctate staining decreased after 6 weeks of ScCL use from 86% to 31% of right eyes (n=81), and 82% to 29% of left eyes with OSD (n=84). In addition, corneal punctate staining also decreased after 6 weeks of ScCL use from 23% to 7% of right eyes (n=30), and from 24% to 10% of left eyes with CI (n=29).
TABLE 1.
Patient Demographics
| Demographics | |||
|---|---|---|---|
| OSD n (%) | CI n (%) | Total n (%) | |
| Gender | |||
| Male | 48 (51%) | 21 (55%) | 69 (52%) |
| Female | 47 (49%) | 17 (45%) | 64 (48%) |
| Race | |||
| Caucasian | 74 (78%) | 25 (66%) | 99 (74%) |
| African American | 3 (3%) | 6 (16%) | 9 (7%) |
| Hispanic | 5 (5%) | 3 (8%) | 8 (6%) |
| Asian | 3 (3%) | 0 (0%) | 3 (2%) |
| Other/unknown | 10 (11%) | 4 (10%) | 14 (11%) |
| Mean age | 49 | 49 | 49 |
| Mean distance from clinic (miles) | 165 | 32 | 129 |
| Eye evaluated for ScCL | |||
| OD | 9 (9.5%) | 9 (23.7%) | 18 (13.5%) |
| OS | 14 (14.7%) | 8 (21.1%) | 22 (17.5%) |
| OU | 72 (75.8%) | 21 (55.3%) | 93 (70%) |
CI, corneal irregularity; OSD, ocular surface disease; ScCL, scleral contact lens.
TABLE 2.
Visual Acuity by OSD Versus CI and Severity of CI, and Presence of Punctate Epithelial Erosions at Baseline and 6-Week Follow-Up in Patients With OSD
| Visual Acuity | Entering BCVA, logMAR (Snellen) | BCVA With ScCL, logMAR (Snellen) | Significance (α=0.05) |
|---|---|---|---|
| OSD | 0.3±0.5 (20/40) | 0.1±0.2 (20/24) | 0.001a |
| CI | 0.5±0.4 (~20/59) | 0.2±0.2 (~20/28) | 0.0001a |
| All | 0.3±0.4 (20/43) | 0.1±0.2 (20/25) | 0.0001a |
| CI Visual Improvement by Severity (D)a | Entering BCVA (range) | BCVA With ScCL (range) | Significance (α=0.05) |
| Mild (<45.00) | 0.35 (0–0.88) | 0.18 (0–0.60) | 0.082 |
| Moderate (45.00–52.00) | 0.36 (0–1.0) | 0.13 (0–0.30) | 0.028a |
| Severe (>52.00) | 0.69 (0–1.3) | 0.13 (0–0.40) | <0.001a |
| OSD Presence of PEE | Baseline Visit | Significance (α=0.05) | Significance (α=0.05) |
| OD | 70 (46 PROSE, 25 commercial ScCL) | 25 (13 PROSE, 12 commercial ScCL) | 0.03a |
| OS | 69 (49 PROSE, 20 commercial ScCL) | 24 (12 PROSE, 12 commercial ScCL) | 0.02a |
Steep keratometry in diopters (D).
CI, corneal irregularity; logMAR, logarithm of the minimal angle of resolution; OSD, ocular surface disease.
Ocular Surface Disease
Of the 95 patients with a primary indication of OSD, 20% (n=19) also had a secondary CI diagnosis. The most common diagnosis in the OSD group was chronic ocular graft versus host disease, followed by dry eye syndrome and neurotrophic keratitis (Fig. 1), and most patients were evaluated for ScCL in both eyes (76%). Secondary diagnoses of CI in this group included corneal scarring, post-LASIK ectasia, and status post penetrating keratoplasty. Visual acuity improved from logMAR 0.3±0.5 to 0.1±0.2 (P=0.001), and 64% of right eyes and 65% of left eyes that initially presented with punctate epithelial erosions had resolution after 6 weeks of ScCL wear (P=0.03, P=0.02; Table 2). The average number of previous treatments in this population was 4.4 (Fig. 2). On average, 6.7 PROSE devices were ordered compared to 4.5 commercial lenses during a fitting period for patients with OSD. Similarly, PROSE patients averaged 7.4 follow-up visits compared to 6.5 in commercial ScCL wearers. It is also notable that patients with OSD fit with PROSE were more symptomatic, with 46% of patients fit with PROSE reporting pain at baseline in comparison to 17% of those fit with commercial scleral lenses.
FIG. 1.
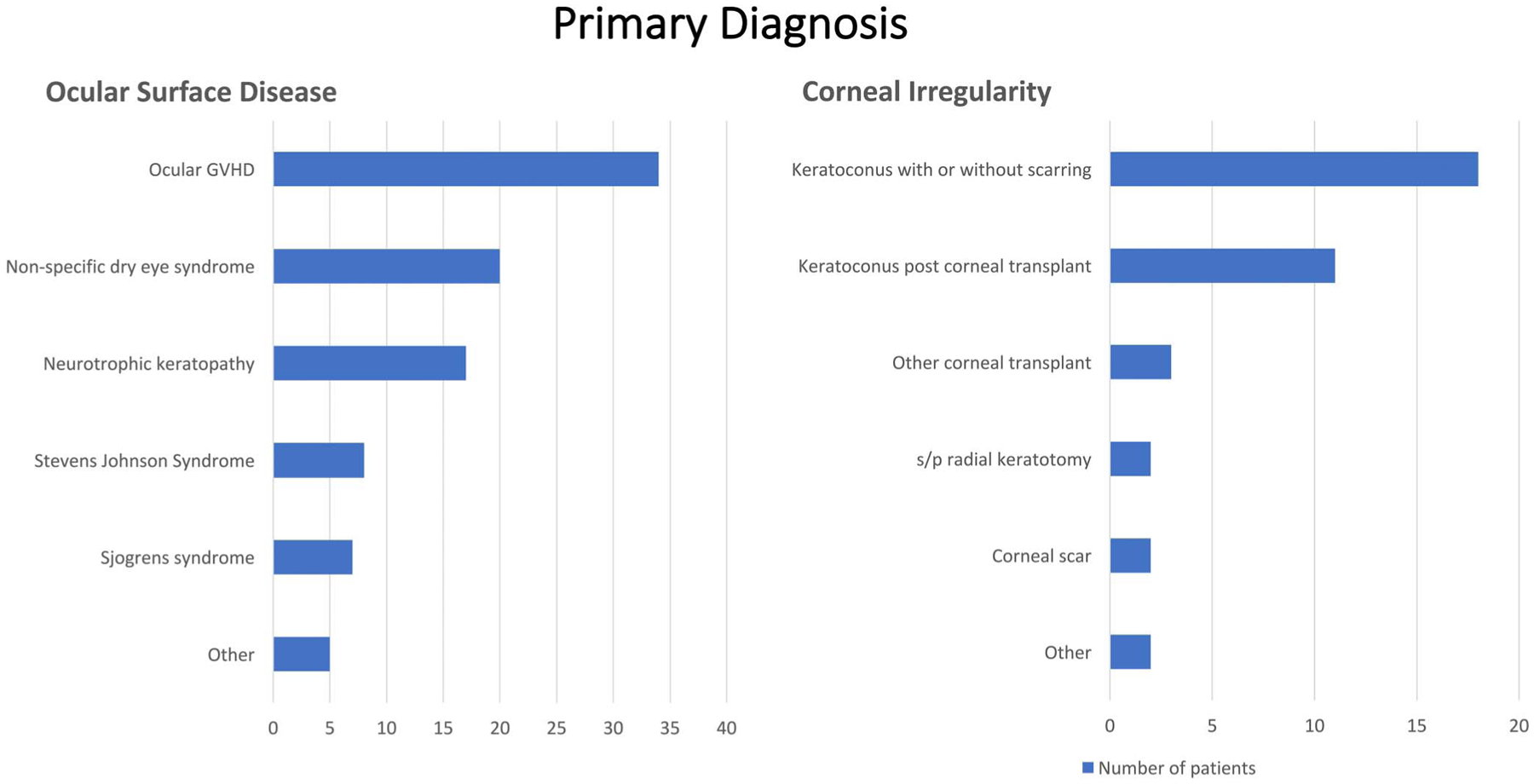
Primary diagnosis in individuals with ocular surface disease and corneal irregularity.
FIG. 2.
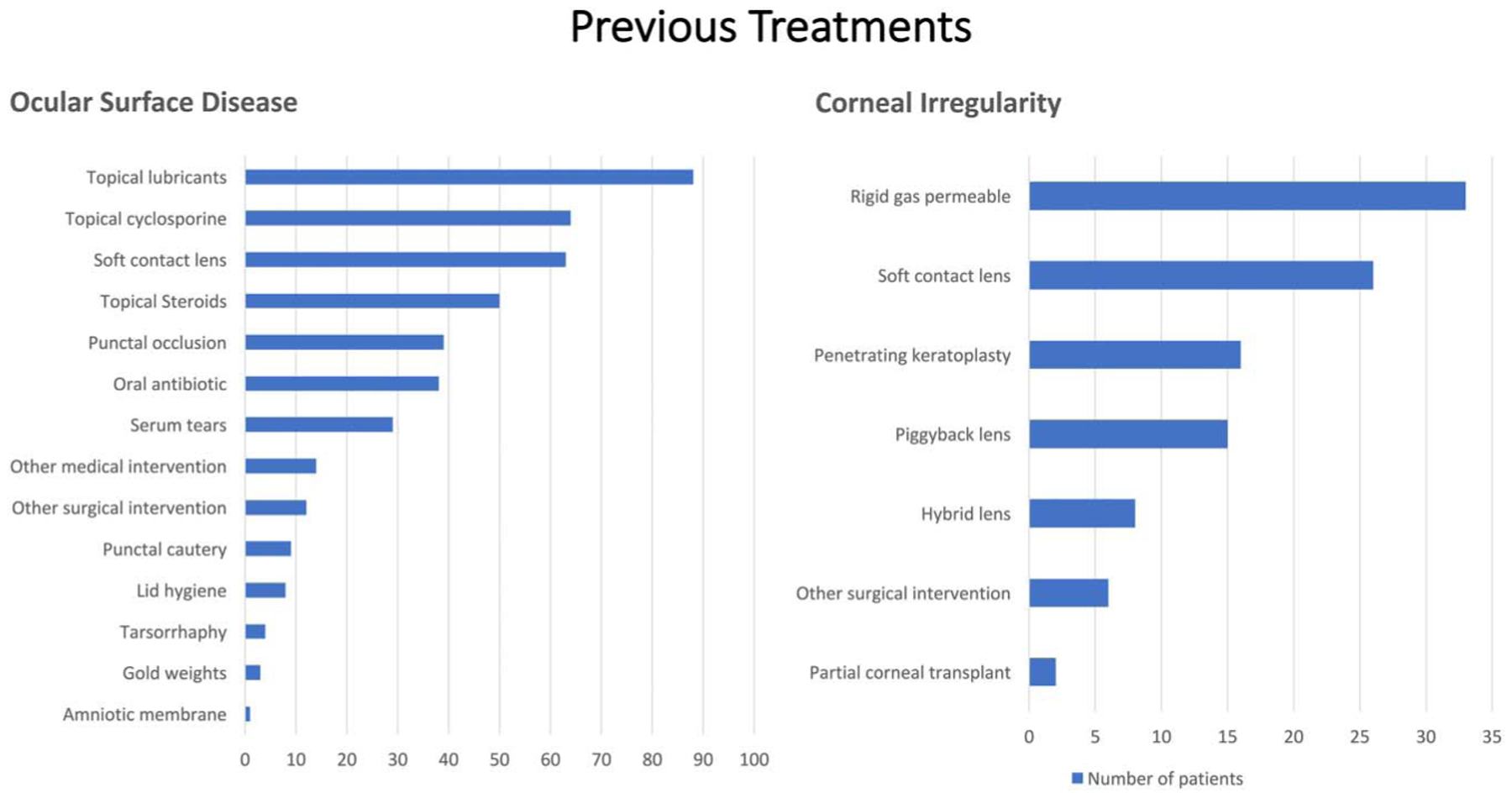
Previous treatments in patients with primary indication of ocular surface disease and corneal irregularity.
Corneal Irregularity
Of 38 patients with a primary indication of CI, 50% (n=19) also had a secondary diagnosis of OSD. The most frequent diagnosis in the CI group was keratoconus followed by keratoconus status after keratoplasty (Fig. 1). Secondary diagnoses of OSD included dry eye syndrome and Sjogrens syndrome. Visual acuity improved from 0.5±0.4 to 0.2±0.2 (P=0.0001) with ScCL. When further categorizing this group by severity, eyes with moderate (45.00–52.00D) and severe (>52.00D) irregularity showed statistically significant visual improvement (P=0.028, P<0.001; Table 2). The average number of prior treatments in this population was 2.8 (Fig. 2). On average, six PROSE devices were ordered compared to 3.8 commercial lenses during a fitting period for patients with CI. Similarly, PROSE patients averaged 7.5 follow-up visits compared to 3.9 in commercial ScCL wearers.
DISCUSSION
In this study, we assessed ScCL trends in a tertiary referral center. Ocular surface complaints and disease were very common in this patient population. The majority (71%) of patients evaluated had a primary indication of OSD; however, OSD was a primary or secondary indication for ScCL evaluation in most patients. This demonstrates that our study population was different from general prescribers surveyed in the SCOPE studies with 74% and 87% of prescribers fitting patients for the indication of CI.3,4 However, this is consistent with a previous report that prescribers in hospital-based practices fit more patients for OSD than community-based prescribers.3 This could be due to seeing more patients referred with OSD as a tertiary care center, and who have potentially already failed first-line therapies. This discrepancy could also be due to the fitting philosophy of our providers, preferring to use corneal gas-permeable lenses for patients with CI and reserving ScCL for more advanced cases.
Individuals with OSD were commonly referred for evaluation when other treatments were unsuccessful. For example, 93% of patients were previously treated with topical lubricants, 67% with topical cyclosporine, and 53% had used topical steroids. In addition, 66% of these patients had been previously prescribed therapeutic soft lenses, and patients had previously tried an average of 4.4 interventions. This is similar to Schornack et al.6 who reported an average of 3.2 treatments before ScCL evaluation, the most common being lubricating drops and punctal plugs. A survey of ScCL prescribers ranked ScCL as the fifth choice in the management of OSD, after topical lubricants, topical cyclosporines, topical corticosteroids, and punctal occlusion.7 However, 20% of hospital-based practitioners ranked ScCL as their first, second, or third treatment of choice for OSD.7 Currently, there lacks a clinical consensus on when ScCL should be used for the management of OSD. In our practice, we tend to manage OSD with traditional therapies first with the exception of neurotrophic or exposure keratopathies in which we often prescribe ScCL earlier.
Of patients evaluated for ScCL with history of CI, 68% had previously used soft contact lenses and 87% had used corneal gas-permeable lenses, with an average of 2.8 treatments before ScCL evaluation. This differs from the study by Shorter et al.7 in which eye care providers ranked ScCL as their second treatment of choice, only after corneal gas-permeable lenses for the management of CI, followed by custom hydrogel/silicone hydrogels, hybrid lenses, piggyback lenses, and standard hydrogel/silicone hydrogels. Again, this could be due to our prescriber’s fitting philosophy in which we often use custom soft, corneal gas-permeable, and piggyback lens systems first before prescribing ScCL for patients with CI. In our population, 50% of patients with a primary indication of CI had a secondary diagnosis of OSD. Ocular surface complaints and disease likely augmented the use of ScCL in this population.
We found that visual acuity significantly improved with ScCL overall. Although there was improvement of 0.2 logMAR units in the OSD group with ScCL, there was larger improvement, 0.3 logMAR unit, in the CI group. The greater than three-line improvement in CI patients we found is consistent with previous studies.8,9 In addition, we found that when further categorizing by severity of irregularity based on the CLEK study,5 only those with moderate and severe irregularity showed statistically significant visual improvement. Individuals with mild CI also had better baseline visual acuity using traditional spectacles, soft lenses, or corneal gas-permeable lenses. In our population, patients fit with ScCL had previously failed other lens options, and ScCL were considered before recommending surgery. Kopen et al.10 previously reported successfully avoiding surgery by managing over three quarters of eyes with severe keratoconus with long-term ScCL use. Deloss et al.11 also reported that patients with stage 4 ectasia (mean keratometry >55.00 D) fit with PROSE devices had better visual outcomes and more rapid visual rehabilitation than those who underwent keratoplasty, suggesting that nonsurgical intervention should be considered in all individuals before keratoplasty. Given the significant improvement in vision in the severe CI group, we highly recommend ScCL evaluation before keratoplasty.
Our patients with OSD had, on average, a greater than 1.5 Snellen line improvement in visual acuity with ScCL use. In this group, many eyes had resolution of corneal staining after six weeks of ScCL use. This is consistent with previous studies that demonstrated a decrease in corneal staining with PROSE device use in individuals with chronic ocular GVHD.12 Patients with OSD were more likely to travel from further distances for ScCL evaluation and more likely to be fit with PROSE devices (Table 1). This is not surprising because PROSE treatment is currently limited to 12 institutions in the United States.13 Although this was a retrospective study and was not designed to evaluate differences between commercial ScCL and PROSE devices, there were a few trends observed. This study is unique in that we included all patients who were prescribed PROSE and ScCL. There were differences in the number of lenses ordered in both OSD and CI groups as well as the number of follow-up visits in the OSD group. This discrepancy could be in part due to PROSE treatment and device remake periods extending up to 180 days, whereas other ScCL are generally limited to 90 days. It is also possible that although commercially available ScCL allow for some modifications, more PROSE remakes may have been made due to the ability to customize more precisely with the highly customizable PROSE design. In this series, PROSE patients had an average of 7.4 visits in the OSD group and 7.5 in the CI group. This is similar to DeLoss et al.11 who reported an average of six visits for PROSE patients with CI, and slightly less than Kornberg et al.14 who reported an average of 12.3 in patients with OSD and 10.7 visits for those with CI fit with PROSE. The number of PROSE devices ordered in our study was 6.7 for OSD and 6.0 for CI, similar to Kornberg et al.14 with 5.8 for OSD and 5.2 for CI. Previous reports of commercial scleral lenses in academic medical centers reported lesser numbers with 3.2 lenses per eye over 6 visits8 and 1.4 lenses/eye over an average of 3 visits.6
A limitation to our study was that as a retrospective design, documentation was not standardized and data collection was dependent on existing medical records. In addition, this was a small sample size, which limited statistical testing. Future prospective studies may better identify individual factors that suggest the need for ScCL evaluation earlier in the treatment sequence.
In conclusion, ScCL were an effective therapy in this tertiary care patient population improving vision and decreasing corneal punctate keratopathy. Ocular surface disease was very common and was a primary or secondary indication for ScCL evaluation in 85.7% of patients evaluated.
Acknowledgments
Supported by an unrestricted grant to the Department of Ophthalmology and Visual Sciences from Research to Prevent Blindness and an NIH/NEI EY001792 (UIC) Core grant.
Footnotes
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: A review. Contact Lens Anterior Eye 2014;37:240–250. [DOI] [PubMed] [Google Scholar]
- 2.Barnett M, Johns KJ. Contemporary scleral lenses: Theory and application. Optom Vis Sci 2018;95:687. [Google Scholar]
- 3.Nau CB, Harthan J, Shorter E, et al. Demographic characteristics and prescribing patterns of scleral lens fitters: The SCOPE study. Eye Contact Lens 2018;44(Suppl 1):S265–S272. [DOI] [PubMed] [Google Scholar]
- 4.Schornack M, Nau C, Nau A, et al. Visual and physiological outcomes of scleral lens wear. Cont Lens Anterior Eye 2019;42:3–8. [DOI] [PubMed] [Google Scholar]
- 5.Zadnik K, Barr JT, Edrington TB, et al. Baseline findings in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Invest Ophthalmol Vis Sci 1998;39:2537–2546. [PubMed] [Google Scholar]
- 6.Schornack MM, Pyle J, Patel SV. Scleral lenses in the management of ocular surface disease. Ophthalmology 2014;121:1398–1405. [DOI] [PubMed] [Google Scholar]
- 7.Shorter E, Harthan J, Nau CB, et al. Scleral lenses in the management of corneal irregularity and ocular surface disease. Eye Contact Lens 2018;44: 372–378. [DOI] [PubMed] [Google Scholar]
- 8.Pecego M, Barnett M, Mannis MJ, et al. Jupiter scleral lenses: The UC davis eye center experience. Eye Contact Lens 2012;38:179–182. [DOI] [PubMed] [Google Scholar]
- 9.Arumugam AO, Rajan R, Subramanian M, et al. PROSE for irregular corneas at a tertiary eye care center. Eye Contact Lens 2014;40:71–73. [DOI] [PubMed] [Google Scholar]
- 10.Koppen C, Kreps EO, Anthonissen L, et al. Scleral lenses reduce the need for corneal transplants in severe keratoconus. Am J Ophthalmol 2018;185: 43–47. [DOI] [PubMed] [Google Scholar]
- 11.DeLoss KS, Fatteh NH, Hood CT. Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) scleral device compared to keratoplasty for the treatment of corneal ectasia. Am J Ophthalmol 2014;158:974–982. [DOI] [PubMed] [Google Scholar]
- 12.Theophanous C, Irvine JA, Parker P, et al. Use of prosthetic replacement of the ocular surface ecosystem scleral lenses in patients with ocular chronic graft-versus-host disease. Biol Blood Marrow Transpl 2015;21: 2180–2184. [DOI] [PubMed] [Google Scholar]
- 13.BostonSight. PROSE network. BostonSight 2017. 2019. Available at: https://www.bostonsight.org/PROSE/PROSE-providers/Find-a-Clinic. [Google Scholar]
- 14.Kornberg DL, Dou E, Wang Y, et al. Clinical experience with PROSE fitting: Significance of diagnosis and age. Eye Contact Lens 2016;42: 124–128. [DOI] [PubMed] [Google Scholar]


