Highlights
-
•
Low back pain information offered on YouTube ™ is often not evidence based.
-
•
Available information prioritizes interventions rather than inform on condition.
-
•
Factors related to engagement with content on YouTube ™ remain uncertain.
Keywords: Health information, Low back pain, YouTube
Abstract
Background
Quality of low back pain (LBP) information offered on YouTube ™ is unclear.
Objective
To describe the current low back pain information available on YouTube ™ and determine if these videos report information that aligns with clinical guidelines. Further analysis explored whether specific features of the videos explain their popularity.
Methods
A cross-sectional observational study was conducted on videos related to LBP on YouTube™ with the 200 most viewed videos using the term “low back pain.” The videos were independently viewed and assessed by two researchers for specific video characteristics, LBP specific content, and compliance with guidelines. The association between video characteristics or content with popularity (i.e., views, likes, dislikes, and comments) was investigated using regression models.
Results
The median number of views was 2 018 167. Only 59 (29.5%) of the videos reported at least one diagnostic recommendation from clinical guidelines, and only 100 (50%) reported a treatment recommendation that aligned with clinical guidelines. Apart from year of upload, no variables were identified that were independently associated with popularity or engagement of the videos.
Conclusion
The information related to LBP offered on YouTube™ is often not evidence-based and there is the tendency to prioritize information on interventions rather than understanding the LBP process. Factors related to engagement with content about LBP on YouTube™ remains uncertain, indicating further need for knowledge translation in this field.
Introduction
Low back pain (LBP) is prevalent worldwide, with 540 million people experiencing this health condition at any time.1, 2, 3 Disability related to LBP brings an enormous direct and indirect cost to the population and health systems around the world.4 Although there are multiple clinical guidelines for assessing and treating different forms of LBP,5 there remains a difference between clinical practice and current scientific evidence6 and, currently, many health professionals are not using quality scientific evidence to support their clinical practice.7 Disseminating health information on social media is becoming more prevalent, making it important to explore if information available on social media also differs from current scientific evidence. This presents an important area of concern as the general public is also affected by difficulty accessing the best health information, as well as a lack of knowledge on how to access information easily.7,8
With over one billion views per month,9 YouTube™ is a video sharing platform which has increasingly become a way to obtain health care information.10 There is no information about the exact number of people that use YouTube™ as a health care information source, but some studies show that a large percentage of health decisions are influenced by searches through online platforms.9 A systematic review of health care information on YouTube™ found that a large amount of health-related information is searched on the platform, and some information is misleading or incorrect.10 Over the past five years, studies have evaluated the quality of the health care content on YouTube™8,9,11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 and the relationship between video characteristics with viewer engagement.8,13,17
Currently, research on the quantity and quality of the information on LBP in online platforms is scarce.10 Taking into account the impact that LBP has and the widespread access to health information through social media platforms such as YouTube™, it is important to clarify the quantity and quality of the available information.
This study aims to describe the current LBP information available on YouTube™ and determine if these videos report information that aligns with current clinical guidelines.5 A secondary analysis explored whether specific features of the videos explain their popularity based on video engagement. The identification of factors that can improve popularity of videos may be important for health information dissemination and to improve interventions using social media platforms.
Methods
Study design and data collection
A cross-sectional observational study was conducted using a convenience sample of videos related to LBP on YouTube™ (sharing site: http://www.youtube.com). The protocol for the study was prospectively published on the Open Science Framework (https://osf.io/ne6kj/). Two trained and independent researchers (LBM and JPS) conducted a search on YouTube™ in Brazil following the same steps: i) researchers were instructed to sign out of their personal Google™ accounts and use a new account created specifically for them to perform the search; ii) they searched using the term ‘‘low back pain’’ to identify videos, applying the filter ‘‘view count’’; and iii) they selected the first 200 most viewed videos related to LBP (based on previous studies that analyzed descriptive characteristics8 and correlations).17 As two researchers performed this search in parallel, the search results were combined and a final selection of the most popular 200 videos was made. Between-reviewer consensus solved potential discrepancies. The first 50 videos identified by both searches are available in the Supplemental Online Material to show the similarity in the search results. A pilot search was done on February 24th, 2020 to identify possible issues with collection and to ensure that there were no differences between the two searches. The final search used in this study was made on March 25th, 2020. This study follows the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology)26 reporting guidelines.
Eligibility criteria and data extraction
Videos related to LBP were considered for inclusion if they were recorded in English, Portuguese, or Spanish without restriction on the date of uploading. Partial or total duplicates were excluded with the most viewed video maintained in the results. The Universal Resource Locator (URL) link for each video was saved for assessment by the researchers.13
Video features
The videos were viewed by two reviewers independently (LBM and JPS), descriptive information were extracted and the LBP content was evaluated for compliance with a 2018 updated overview of 15 LBP guidelines (eg, from the National Guideline Clearinghouse and National Institute for Health and Clinical Excellence–NICE) associated with searches in some databases (MEDLINE and PEDro).5 Between-reviewer consensus solved potential discrepancies.
Independent variables
The independent variables extracted for each video were: 1) type of video (could be categorized as video class, lecture, videoconference, program or interview, podcast, event, documentary, or animation); 2) year (the year of uploading to YouTube™); 3) duration (in minutes); 4) Source of content (the presence of conflict of interest); 5) category of speaker (the person sharing the information categorized as physical therapist, physical educator, massage therapist, physician, or layperson; 6) language (could be English, Portuguese, or Spanish); 7) source (channel or individual as uploader of the videos); and 8) intention (was the goal of the video to inform about diagnosis, prognosis, epidemiology, risk factors, interventions, or none. A video could be classified into more than one category of intention).
Compliance with guidelines5 was assessed using one point for each recommendation based on the latest update of clinical practice guidelines for LBP (total of six diagnostic recommendations and 11 treatment recommendations).5 The rules for scoring video compliance with the guidelines are explained in Table 1.
Table 1.
Guidelines based classification.
| Diagnostic recommendations | |
| Classification | 1 point |
| History taking and physical examination | 1 point |
| Red flags | 1 point |
| Neurological examination | 1 point |
| Imaging only considered if red flags are present | 1 point |
| Yellow flags | 1 point |
| Treatment recommendations | |
| Avoiding bed rest for acute low back pain (LBP) | 1 point |
| Advice to maintain normal activities for acute LBP | 1 point |
| Reassuring that LBP is not a serious illness | 1 point |
| Reassuring on the favorable prognosis of acute LBP | 1 point |
| Use of NSAIDs for acute/chronic LBP | 1 point |
| Antidepressants for chronic LBP when necessary | 1 point |
| Indication for referral to specialist | 1 point |
| Referral to a specialist if there is no improvement 4 weeks to 2 years | 1 point |
| Multidisciplinary rehabilitation | 1 point |
| Psychosocial strategies in chronic LBP | 1 point |
| Exercise therapy in chronic LBP | 1 point |
NSAIDs: nonsteroidal anti-inflammatory drugs.
Dependent variables
The dependent variables were extracted through the available information on YouTube™: 1) views (how many people watched each video); 2) likes (the site allows viewers to rate each video through positive engagement); 3) dislikes (negative engagement); and 4) comments (the number of comments on each video as a measure of engagement).
Data analysis
Descriptive statistics were performed for video characteristics (i.e., independent variables) reporting frequency, median, and interquartile range as data were not normally distributed. Compliance with guidelines5 was assessed using descriptive analysis reporting the frequency of: i) the number of videos identified reporting on each diagnostic and treatment recommendation, and ii) the number of recommendations reported by each video.
To investigate which features are associated with popularity and engagement, a Spearman test was used to describe the association between dependent (i.e., views, likes, dislikes, and comments) and continuous independent variables of interest (i.e., year, duration). Chi-squared (χ2) test was used for categorical independent variables (i.e., video type, category of speaker, language, source, and diagnostic and treatment recommendations). For this correlation analysis, the compliance with guidelines was dichotomized as ‘‘evidence-based video’’ if the video reported at least one guideline recommendation or ‘‘non-evidence-based video’’ if the video did not report any guideline recommendation.
All independent variables which were associated with one of the dependent variables (i.e., with a p-value ≤ 0.20)27,28 were included in a univariate linear regression model to explain popularity and engagement. Standardized beta coefficients (β), 95% confidence intervals (CI) and p-values were presented for all independent variables included in the model. Final multivariate regression model was planned to explain the dependent variables including all independent variables with a p-value ≤ 0.05.
Kappa coefficients was used to investigate the researchers’ agreement,29 considering a value < 0 as no agreement, 0–0.20 as slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1 as almost perfect agreement.29 We evaluated the agreement of classification of the variables “type,” “diagnostic recommendations,” and “treatment recommendations.” All analyses were performed in the Statistical Package for the Social Sciences Inc. (SPSS), Chicago, IL, USA (v.20).
Results
Characteristics of included videos
The characteristics of the 200 most viewed LBP videos showed that ‘’program or interview’’ was the most common type of video (93.5%), the videos were uploaded 4 years ago (median = 2016), and the median duration was 10 min and 18 s. The source of the content could not be determined for almost half of the videos (49%) and was business-related in 47.5%. The median number of views was 2 018 167 and the videos had a median number of 537 likes, 283 dislikes, and 404 comments. The most common category of speaker in the videos was physical therapists (40%) and the main language of the videos was English (99.5%). The variable ‘‘intention’’ presented videos classified into more than one category, and the most common intention category was ‘‘inform about intervention’’ (100%). One video hid information about likes and dislikes, and seven videos hid information about comments. The Kappa coefficients were at least 95.9 and showed almost perfect agreement between the two reviewers. Detailed characteristics of the videos are presented in Table 2.
Table 2.
Characteristics of YouTube™ videos (n = 200) related to low back pain.
| Type | |
| Animation | 13 (6.5%) |
| Program or interview | 187 (93.5%) |
| Years uploaded, | 4 (2–7) |
| Duration (min) | 10 (5–15) |
| Source of content | |
| Business-related | 95 (47.5%) |
| Associations/researchers | 7 (3.5%) |
| Not available | 98 (49%) |
| Category of speaker | |
| Physical therapist | 80 (40.0%) |
| Physical educator | 62 (31.0%) |
| Massage therapist | 24 (12.0%) |
| Physician | 24 (12.0%) |
| Layperson | 10 (5.0%) |
| Language | |
| English | 199 (99.5%) |
| Portuguese | 1 (0.5%) |
| Source | |
| Channel | 145 (72.5%) |
| Individual | 55 (27.5%) |
| Intention* | |
| Inform on diagnosis | 28 (14.0%) |
| Inform on prognosis | 2 (2.0%) |
| Inform on epidemiology | 6 (3.0%) |
| Inform on risks | 3 (1.5%) |
| Inform on intervention | 200 (100.0%) |
| None of the above | 4 (2.0%) |
| Diagnostic recommendations | |
| No recommendation | 127 (63.5%) |
| At least one recommendation | 73 (36.5%) |
| Treatment recommendations | |
| No recommendation | 100 (50.0%) |
| At least one recommendation | 100 (50.0%) |
| Views | 2 018 167 (1 372 712–3 651 597) |
| Likes | 537 (415–818) |
| Dislikes | 283 (156–498) |
| Comments | 404 (168–950) |
Data are median (25th–75th percentiles) and frequency (proportion).
There are videos with more than one intention. This variable was used just in the descriptive analysis.
Primary analysis–compliance of included videos with the current guidelines
Diagnostic recommendations
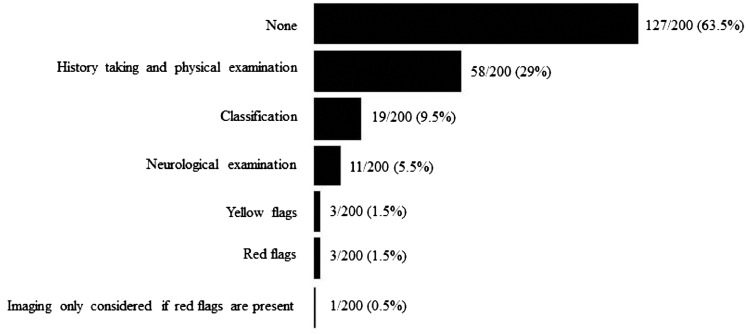
Of the 200 most viewed videos: 127 (63.5%) reported no diagnostic recommendations; 59 (29.5%) reported one diagnostic recommendation; 10 (5%) reported two recommendations; three (1.5%) reported three recommendations; and one (0.5%) reported all six diagnostic recommendations. In summary, 36.5% of the videos reported at least one guideline recommendation on diagnosis and 63.5% did not report any recommendations. The reporting of each diagnostic recommendation is provided in Fig. 1.
Fig. 1.
Number of videos classified on each diagnostic recommendation; n/200 (%).
Treatment recommendations
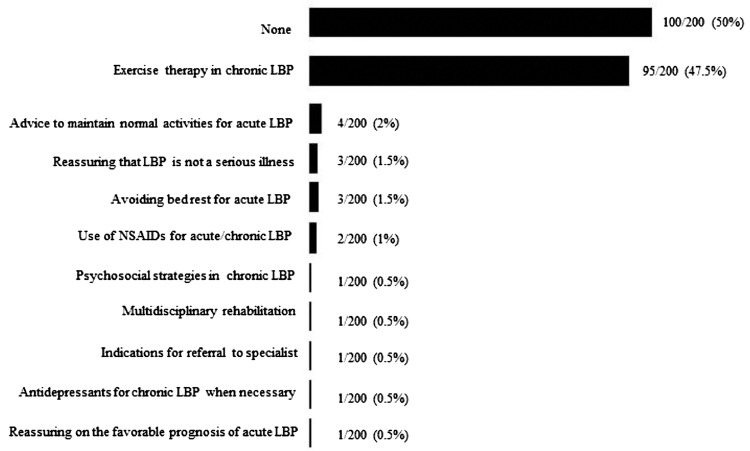
Of the 200 most viewed videos, 100 (50%) reported no treatment recommendations; 88 (44%) reported one recommendation; eight (4%) reported two recommendations; one (0.5%) reported three recommendations; one (0.5%) reported four recommendations; one (0.5%) reported six recommendations; and one (0.5%) reported seven treatment recommendations. In summary, 50% of the videos reported at least one guideline recommendation on treatment and 50% did not report any. Some examples of nonevidence-based treatments found in the videos were: passive interventions (treatments based only on manual therapy such as osteopathy or massage), traction table, and natural remedies. The reporting of each treatment recommendation is provided in Fig. 2.
Fig. 2.
Number of videos classified on each treatment recommendation; n/200 (%).
Secondary analysis–factors associated with popularity of low back pain videos
The secondary analysis showed a significant correlation (p < 0.20) between the number of views and the type of video as well as between the number of comments and the category of speaker. The results of Spearman correlation for continuous variables showed a correlation (p < 0.20) between the number of likes and the year; the number of likes and the video duration; the number of dislikes and the year; the number of dislikes and the video duration; the number of comments and the year; as well as the number of comments and the video duration. Results for the correlation analyses are presented in the Supplemental Online Material.
Univariate linear regressions only showed a significant relationship between the independent variable ‘’year’’ with the dependent variables: ‘’likes’’; ‘’dislikes’’; and ‘’comments.’’ Older videos were more likely to have more likes, dislikes, and comments over time: one year is likely to increase 1794.5 likes, 79.8 dislikes, and 117.7 comments on videos. All the other independent variables were not associated with any of the four outcomes of interest (p > 0.05). Univariate regression models are presented in Table 3.
Table 3.
Linear regression analyses (n = 200).
|
Views |
Likes |
Dislikes |
Comments |
|||||
|---|---|---|---|---|---|---|---|---|
| B (95% CI) | β | B (95% CI) | β | B (95% CI) | β | B (95% CI) | β | |
| Year | – | – | 1794.5* (68.9, 3520.2) | 0.14 | 79.8* (1.35, 158.3) | 0.14 | 117.7* (8.42, 227.1) | 0.15 |
| Duration | – | – | 97.2 (−423.3, 617.8) | 0.03 | −2.6 (−26.3, 21.1) | 0.01 | 13.9 (−18.8, 46.7) | 0.06 |
| Diagnostic recommendations | – | – | −1083.9 (−7621.8, 5453.9) | 0.02 | – | – | – | – |
| Treatment recommendations | – | – | 4112.9 (−1594.7, 9820.7) | 0.10 | – | – | 8.3 (−356.5, 373.3) | 0.00 |
| Type | −344,036.8 (−2,315,465, 1,627,391) | 0.02 | – | – | – | – | – | |
| Category of speaker | – | – | – | – | – | −146.0 (−415.1, 123.0) | 0.08 | |
CI, confidence interval; -, no correlation of variables; β, standardized beta coefficients; B, rate of change per unit of variable; *, statistically significant association (p-value ≤ 0.05).
Discussion
In our study we found very low compliance of LBP videos on YouTube ™ with the current guidelines for both diagnostic and treatment recommendations. We also identified a tendency to explain and give more information about interventions, with fewer videos about diagnosis, prognosis, epidemiology, or risk factors. Taking into account the popularity analysis, only one variable (year) explained the greater or lesser popularity of these videos. Videos that have been on the site the longest tend to have the most views, likes, dislikes, and comments.
We can contextualize the results about compliance with guidelines using the concept of evidence-based practice that includes the use of current best evidence, clinical expertise, and patient values in the health care context.30,31 When observing videos related to LBP on YouTube™, a range of different types of intervention and non-standardized clinical reasoning in the choice of diagnostics or treatments for LBP are evident. Following the recommendations of evidence-based practice, the great majority of the videos seem to focus on the clinical expertise of the person speaking in the video with some consideration of patient values, however, ignoring the use of the available best evidence. These results are similar to reports of videos for other health conditions.9,17 With regard to the greater number of videos about interventions we can surmise that there is a focus on ‘’solving” LBP instead of explaining or informing about the condition, even though there is evidence to support interventions such as health education for individuals with LBP.5,32,33 Taking into account the popularity of the videos, the results from the current analysis do not add much insight, considering that it is already expected that the older a video is, the greater the number of views, likes, dislikes, and comments it will have.
The strengths of the current study are the systematic evaluation of health information available on YouTube™ which has highlighted the lack of current and easily accessible evidence for LBP management. The fact that the platform receives a large amount of videos from various sources without specific criteria favors this scenario of great divergence from the current clinical guidelines.
There are a few limitations of this study which included videos in English, Spanish, or Portuguese language only and the search term “low back pain” in English due to feasibility. Future studies should investigate whether there are specific cultural differences using appropriate language and descriptors. Our findings suggested that the variable ‘’year’’ is a confounding factor when evaluating popularity and engagement. Future studies should clarify whether other factors such as “influential people,” “production value,” “audiovisual aspects,” or “simplicity” could influence popularity independently from the year of video upload. Investigation of whether funding and conflicts of interest would influence popularity and engagement of videos was not possible in our study because this information is not available on YouTube ™ videos. An important potential limitation is the influence of the YouTube™ algorithm that may influence the number of views, likes, dislikes, and comments (e.g., sponsorship). Another limitation is that geotargeted searches on YouTube™ may also influence the results of this analysis. Future research should attempt to investigate the potential influence of these factors. In addition, potential limitation is the use of a dichotomizing approach to classify the videos into “evidence-based” or “non-evidence based” that can overestimate the evidence-based characteristics of some videos; however, even using this approach, the majority of videos did not show even one evidence-based recommendation.
We can consider this study to assess barriers to knowledge and it appears that a main barrier is the low compliance of LBP videos with the current guidelines. The next step could be the selection and implementation of interventions with participation of professionals who speak more on current scientific evidence on the management of LBP in YouTube™ videos, with a focus on making regular and accessible updates.
The attempt to facilitate the transmission of the scientific research for the general population is known as knowledge translation. Knowledge translation ‘’is about turning knowledge into action and encompasses the processes of both knowledge creation and knowledge application.’’34 Future studies could investigate the effects of online health education on LBP management and the impact of new evidence-based online health programs on knowledge translation for patients and even for professionals on YouTube ™.
Conclusion
The quality of the LBP information offered on YouTube™ is often not evidence-based and there is a tendency to prioritize information on interventions rather than understanding the LBP process. Factors related to engagement with content about LBP on YouTube™ remain uncertain, so knowledge translation needs to be optimized.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.bjpt.2021.06.009.
Appendix. Supplementary materials
References
- 1.Disease G.B.D., Injury I., Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pierobon A., Villalba F., Ferreira G., Maher C. Insights into low back pain management in Argentina. Braz J Phys Ther. 2021 doi: 10.1016/j.bjpt.2021.02.005. S1413-3555(21)000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silva E.S., Vieira Y.P., Saes M.O., et al. Epidemiology of chronic back pain among adults and elderly from Southern Brazil: a cross-sectional study. Braz J Phys Ther. 2021;25(3):344–351. doi: 10.1016/j.bjpt.2020.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maniadakis N., Gray A. The economic burden of back pain in the UK. Pain. 2000;84(1):95–103. doi: 10.1016/s0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 5.Oliveira C.B., Maher C.G., Pinto R.Z., et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27(11):2791–2803. doi: 10.1007/s00586-018-5673-2. [DOI] [PubMed] [Google Scholar]
- 6.Buchbinder R., van Tulder M., Öberg B., et al. Low back pain: a call for action. Lancet. 2018;391(10137):2384–2388. doi: 10.1016/S0140-6736(18)30488-4. [DOI] [PubMed] [Google Scholar]
- 7.de Souza F.S., Ladeira C.E., Costa L.O.P. Adherence to back pain clinical practice guidelines by Brazilian physical therapists: a cross-sectional study. Spine. 2017;42(21):E1251–E1258. doi: 10.1097/BRS.0000000000002190. [DOI] [PubMed] [Google Scholar]
- 8.Heathcote L.C., Pate J.W., Park A.L., et al. Pain neuroscience education on YouTube. PeerJ. 2019;7:e6603. doi: 10.7717/peerj.6603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong M., Desai B., Bautista M., Kwon O., Kolodychuk N., Chimento G. YouTube is a poor source of patient information for knee arthroplasty and knee osteoarthritis. Arthroplasty Today. 2019;5(1):78–82. doi: 10.1016/j.artd.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madathil K.C., Rivera-Rodriguez A.J., Greenstein J.S., Gramopadhye A.K. Healthcare information on YouTube: a systematic review. Health Inform J. 2015;21(3):173–194. doi: 10.1177/1460458213512220. [DOI] [PubMed] [Google Scholar]
- 11.Ortiz-Martínez Y., Acosta-Fernandez C.H., Losada-Manchola D.A., Marulanda-Satizabal J.A. Analysis of YouTube as a source of information about Tuberculosis. Indian J Tuberc. 2017;64(4):343–344. doi: 10.1016/j.ijtb.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Liu M., Cardenas V., Zhu Y., Enguidanos S. YouTube videos as a source of palliative care education: a review. J Palliat Med. 2019;22(12):1568–1573. doi: 10.1089/jpm.2019.0047. [DOI] [PubMed] [Google Scholar]
- 13.Van den Eynde J., Crauwels A., Demaerel P.G., et al. YouTube videos as a source of information about immunology for medical students: cross-sectional study. JMIR Med Educ. 2019;5(1):e12605. doi: 10.2196/12605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abedin T., Ahmed S., Al Mamun M., et al. YouTube as a source of useful information on diabetes foot care. Diabetes Res Clin Pract. 2015;110(1):e1–e4. doi: 10.1016/j.diabres.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Lashari B.H., Chan V., Shoukat U., et al. YouTube as a source of patient education in idiopathic pulmonary fibrosis: a media content analysis. J Community Hosp Intern Med Perspect. 2019;9(2):98–102. doi: 10.1080/20009666.2019.1593779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruppert L., Køster B., Siegert A.M., et al. YouTube as a source of health information: analysis of sun protection and skin cancer prevention related issues. Dermatol Online J. 2017;23(1) [PubMed] [Google Scholar]
- 17.Gokcen H.B., Gumussuyu G. A quality analysis of disc herniation videos on YouTube. World Neurosurg. 2019 doi: 10.1016/j.wneu.2019.01.146. [DOI] [PubMed] [Google Scholar]
- 18.Staunton P., Baker J., Green J., Devitt A. Online curves: a quality analysis of scoliosis videos on YouTube. Spine. 2015;40:1857–1861. doi: 10.1097/BRS.0000000000001137. [DOI] [PubMed] [Google Scholar]
- 19.Delli K., Livas C., Vissink A., Spijkervet F.K. Is YouTube useful as a source of information for Sjögren's syndrome? Oral Dis. 2016;22(3):196–201. doi: 10.1111/odi.12404. [DOI] [PubMed] [Google Scholar]
- 20.Leong A.Y., Sanghera R., Jhajj J., Desai N., Jammu B.S., Makowsky M.J. Is YouTube useful as a source of health information for adults with type 2 diabetes? A south Asian perspective. Can J Diabetes. 2018;42(4):395–403. doi: 10.1016/j.jcjd.2017.10.056. e394. [DOI] [PubMed] [Google Scholar]
- 21.Ortiz-Martinez Y., Ali-Salloum W., González-Ferreira F., Molinas-Argüello J. HIV videos on YouTube: helpful or harmful? Sex Transm Infect. 2017;93(7):481. doi: 10.1136/sextrans-2017-053197. [DOI] [PubMed] [Google Scholar]
- 22.Erdem M.N., Karaca S. Evaluating the Accuracy and Quality of the Information in Kyphosis Videos Shared on YouTube. Spine. 2018;43(22):E1334–E1339. doi: 10.1097/BRS.0000000000002691. [DOI] [PubMed] [Google Scholar]
- 23.Smeeton B., Wormald J.C.R., Plonczak A.M., Butler D., Hamilton S. A critical review of melanoma self-screening tools on YouTube–a missed opportunity? J Plast Reconstr Aesthet Surg. 2018;71(6):e11–e12. doi: 10.1016/j.bjps.2018.01.037. [DOI] [PubMed] [Google Scholar]
- 24.Tang W., Olscamp K., Choi S.K., Friedman D.B. Alzheimer's disease in social media: content analysis of YouTube videos. Interact J Med Res. 2017;6(2):e19. doi: 10.2196/ijmr.8612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mueller S.M., Jungo P., Cajacob L., Schwegler S., Itin P., Brandt O. The absence of evidence is evidence of non-sense: cross-sectional study on the quality of psoriasis-related videos on YouTube and their reception by health seekers. J Med Internet Res. 2019;21(1):e11935. doi: 10.2196/11935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tanha K., Mohammadi N., Janani L. P-value: what is and what is not. Med J Islam Repub Iran. 2017;31:65. doi: 10.14196/mjiri.31.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Babyak M.A. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66:411–421. doi: 10.1097/01.psy.0000127692.23278.a9. [DOI] [PubMed] [Google Scholar]
- 29.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 30.Jennings B.M., Loan L.A. Misconceptions among nurses about evidence-based practice. J Nurs Scholarsh. 2001;33(2):121–127. doi: 10.1111/j.1547-5069.2001.00121.x. [DOI] [PubMed] [Google Scholar]
- 31.Hughes R.G., Advances in Patient Safety . Agency for Healthcare Research and Quality (US); Rockville (MD): 2008. Patient Safety and Quality: an Evidence-Based Handbook for Nurses. [PubMed] [Google Scholar]
- 32.Khodadad B., Letafatkar A., Hadadnezhad M., Shojaedin S. Comparing the Effectiveness of cognitive functional treatment and lumbar stabilization treatment on pain and movement control in patients with low back pain. Sports Health. 2020;12(3):289–295. doi: 10.1177/1941738119886854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bailey J., Agarwal V., Zheng P., et al. Digital care for chronic musculoskeletal pain: a 10,000 user longitudinal observational study (Preprint) J Med Internet Res. 2020;22 doi: 10.2196/18250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Graham I.D., Logan J., Harrison M.B., et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.