Abstract
Objectives:
Vaccination is one of the most significant public health achievements of humanity. However, a significant portion of the population remains hesitant about vaccine safety, efficacy, and necessity. This study aimed to determine COVID-19 vaccination intention and factors affecting their decision among the general population in the Kurdistan region, Iraq.
Methods:
A cross-sectional survey was conducted online during (April-May 2021), and a total of 1171 participants provided complete and valid answers were enrolled. Data collection was done through online questionnaire through Google Forms. We used binary regression analysis to identify factors associated with COVID-19 vaccination intention.
Results:
The majority (53.6%) of the participants were female. Willingness to accept COVID-19 vaccine was low (33 %) of the participants. We found that vaccine hesitancy/resistance was high which was evident for (32%) and (34.9%) of surveyed populations, respectively. Vaccination intention may associate with age, education, and occupation. Furthermore, several factors were associated with hesitancy/resistance: Adverse effects of the vaccine and loss of family members during the pandemic.
Conclusions:
More than half of the study participants refused or were hesitant to have the COVID-19 vaccine, so that Governments and health authorities should improve communication and increase trust.
Keywords: COVID-19 vaccines, Iraq, Kurdistan region, vaccination intention
Introduction
In December 2019 from Wuhan city in China, the novel coronavirus infection outbreak known as Coronavirus disease (COVID)-19 has emerged.[1] The coronavirus has been spread steadily and within a period emerged in other countries, including the Iraqi Kurdistan region.[2] COVID-19 was declared a public health emergency of international concern by the World Health Organization on January 30, 2020, and a pandemic on March 11, 2020.[3] According to the World Health Organization, there were 264,815,815 confirmed COVID-19 cases and a total of 5,249,793 deaths worldwide by December 7, 2021.[4]
The first human case of SARS was reported in Guangdong province, South China, in 2002. In 2012, the MERS coronavirus was transmitted to humans by a camel in Saudi Arabia.[5] The SARS-CoV-2 virus is a new spherical virus with mushroom-shaped proteins known as spikes that give it the look of a crown.[6] Fever, dry cough, shortness of breath, and pneumonia are all common symptoms. Headache, diarrhea, productive cough, runny nose, and hemoptysis are some of the less prevalent clinical symptoms.[7]
Preventive measures, such as lockdown and social distancing, are effective measures for controlling the COVID-19 spread in different nations.[8,9] Vaccination, on the other hand, is still the safest and most efficient technique of preventing infectious diseases and is often regarded as one of the greatest successes in global health.[10] Two COVID-19 vaccines with higher than 90% effectiveness in reducing the risk of symptomatic infection have been licensed in the EU as of January 6, 2021.[11] Its benefit depends on the acceptance of individuals to be vaccinated.[12] However, to achieve heard immunity COVID-19 vaccine hesitancy might represent the main barrier.[13] Understanding socio-demographic characteristics that influence vaccine decision-making is critical to improving vaccine acceptance.[14]
In Kurdistan Regional Government (KRG), three COVID-19 vaccines have been approved recently namely, (Pfizer/BioNTech, Oxford-AstraZeneca, Sinopharm). As of 20 October, 13% of people received vaccines;[15] however, Kurdish health authorities aimed to get at least 20% fully vaccinated community by the end of the year.[16] Therefore, the objective of this study is to determine the COVID-19 vaccination acceptance, refusal, and hesitancy rates and factors behind vaccination intention in the Kurdistan region of Iraq.
Methods
Study design and survey questionnaire
A cross-sectional study design was conducted in Kurdistan Regional Government (KRG) of Iraq; the survey was performed around two weeks during April/May 2021. A total of 1171 samples were enrolled in the present study. Eligibility criteria included being age 18 or >55, currently living in the Kurdistan Region, and not getting the COVID-19 vaccine at the time of the study. Participation was voluntary, provided informed consent on the survey platform before they could proceed to the completion of the questionnaire. The survey questionnaire was composed of 18 questions and divided into three parts. The first section contained sociodemographic characteristics namely (age, gender, occupation, province, and education). While in the second section, participants responded to the structured questionnaire (Whether they accept, hesitant/rejecting to take COVID-19 vaccine, types of vaccines, previous infection, losing family, etc.). Respondents were asked to indicate how important a series of four factors were in their decision, as a third part of the questionnaire. Initially, the clarity and comprehensibility of questions and answers were verified by the pilot study on a group of individuals. The questionnaire was in English and translated to Kurdish Languages to be understandable by all and the survey took 5 minutes for each participant to complete questions.
Study setting
Erbil, Sulaymaniyah, Halabja, and Duhok are the four governorates that made up Iraqi Kurdistan. Figure 1 showed the governorates of Iraqi Kurdistan on a map.[17] SARS-CoV-2 emerged in Iraqi Kurdistan on March 1, 2020, in the Sulaymaniyah Governorate, infecting a family and a woman who had recently returned from Iran. The confirmed cases were also confirmed in the governorates of Halabja and Erbil.[18] COVID-19 prevalence in the Kurdistan region was 1.9%, which is comparable to neighboring countries and the rest of the world from March 2020 to March 2021. The mortality rate was 59 per 100,000 populations.[19] As a result, travelers to the Iraqi Kurdistan Region must provide a PCR certificate valid for at least 48 hours or proof of the second dose of vaccine.[20]
Figure 1.
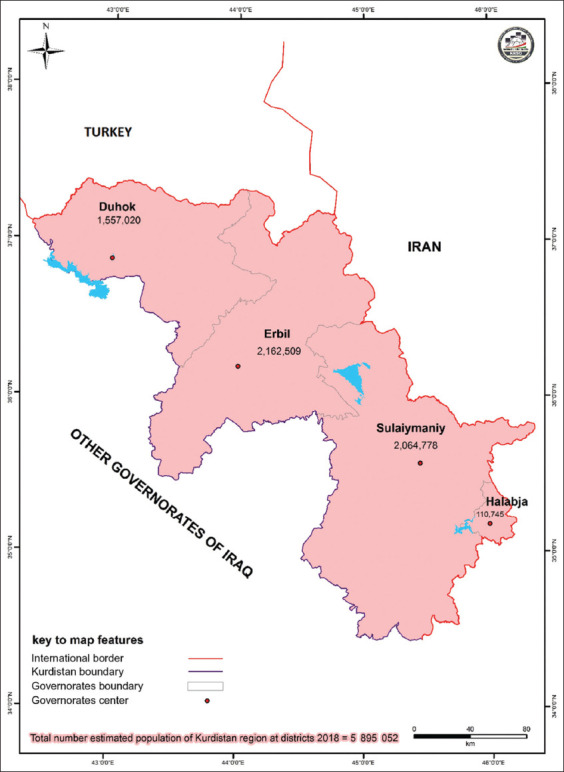
Map of Kurdistan Region with its Estimated Population at Governorate Level, 2018
Data collection
As a result of the COVID-19 pandemic, an online Google form was preferred, as it was thought to be a safer option for both participants and researchers to avoid face-to-face contact and limit the chance of infection. The structured questionnaire was used to enroll participants which consisted of two sections. In the first section, researchers asked about basic sociodemographic characteristics including (age, gender, occupation, level of education. While in the second section the questions concerning vaccination intentions and factors that affect their decision regarding vaccination were asked. Participants who did not complete the questions of the survey were excluded from the study. The online link was sent to the target population randomly using social media platforms such as Viber, Facebook, messenger, pages, and WhatsApp groups.
Statistical analysis
Primarily, descriptive tests (frequency and percentage) were used for demographic characteristics (gender, age, occupation, education, and province), and a Chi-square test was used to indicate p-value. Variables associated with vaccine acceptance and refusal were assessed through Binary logistic regression analysis providing crude odds ratio (OR) and 95% confidence intervals (CI). In a subsequent step, we performed a graph to determine the intention to types of vaccine. Version 23 of IBM SPSS Statistics was used (IBM Corporation, Armonk, New York, USA).
Results
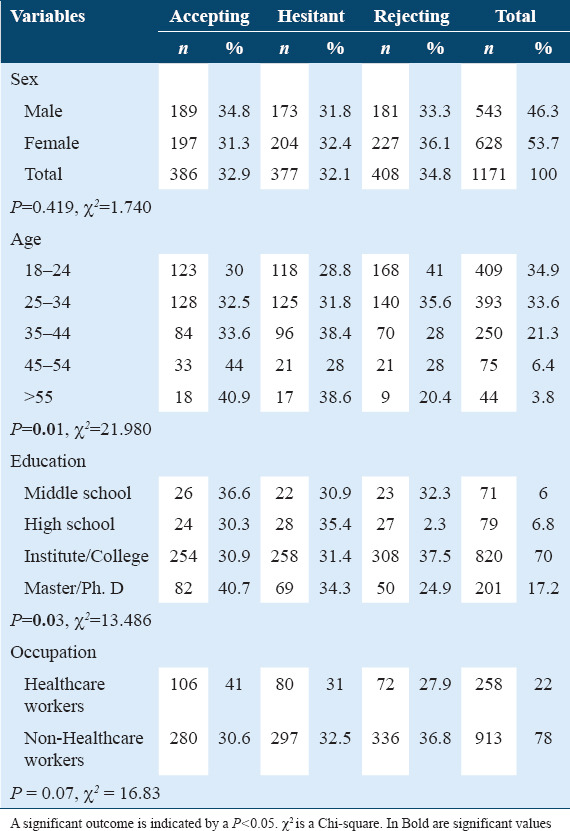
Of the 1171 participants who participated in the current study, (46.3%) were males and (53.7%) were females. Regarding vaccination intention, there was no significant association between both genders. The majority of males and females were hesitant (31.8%) (32.4%) and rejected to be vaccinated (33.3%) (36.1%), respectively. While (34.8%) of males and (32.9) of females declared that they would accept the vaccine. A strong relationship (p<0.01) was found among age groups, the younger individuals 18-44 years were more hesitant and refused to have vaccines as compared to elder age groups. The study revealed a strong relationship (p<0.03) among education levels, Masters and Ph. D individuals had higher rates of accepting vaccines (40.7%) compared to those with high school and under. Furthermore, it is important to highlight that the vast majority (41%) of healthcare workers revealed that they would accept to take the vaccine and a lower percentage (27.9%) would reject to take the vaccine as compared to other occupations [Table 1].
Table 1.
Vaccine intention according to sociodemographic characteristics
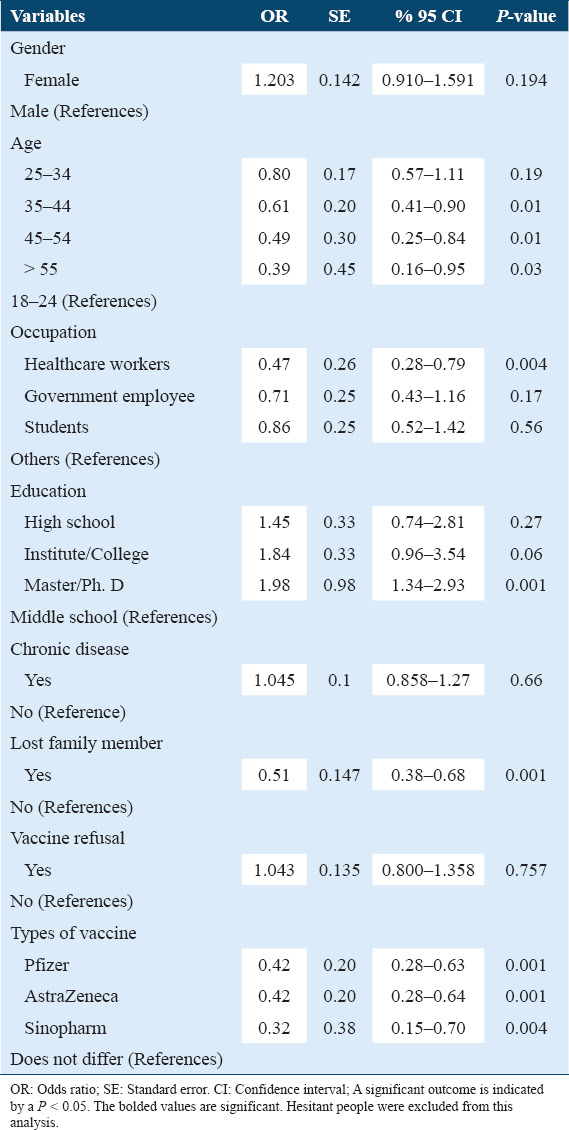
Logistic regression analysis was used to assess independent variables to evaluate vaccine acceptance and rejection. The study revealed that there was no significant association between males and females (OR: 1.20% 95% Cl 0.910-1.591) for accepting and rejecting vaccines. While middle-aged individuals (35-55) were strongly (p<0.01) associated with accepting or rejecting vaccines compared to younger age groups. The lower odds (OR: 0.47% 95% Cl 0.28-0.79) were found among health care workers with significant association (P<0.004) as compared to other occupations with greater odds. The adjusted odds were greater among the participants with higher education with a highly significant association Master/Ph.D. degree (OR: 1.98% 95% Cl 1.34–2.93) in contrast to less-educated participants.
Meanwhile, losing a family member due to the COVID-19 was significantly associated with vaccination intention (P < 0.001; OR: 0.51% 95% Cl 0.38–0.68). Furthermore, significant association (P < 0.001, P < 0.004) was found for available vaccines Pfizer, AstraZeneca, and Sinopharm, respectively. While other factors such as having a chronic disease and a history of vaccine refusal were not significantly associated with the COVID-19 vaccine [Table 2].
Table 2.
Binary regression analyses for Covid-19 vaccine admission
Regarding, reasons behind rejecting or being hesitant to get the COVID-19 vaccine, more than half percent (52%), and almost (48%) were hesitant or refused to get vaccinated. It is mentioned that the majority of hesitant participants (45%) and that rejected vaccination (50.1%) was due to adverse effects of the vaccine. And about (12.7), (15.6) did not accept to take the vaccine due to time of building vaccine were short as compared to other vaccines. Only about (7) and (8.7) their reasons for not being vaccinated were fear of vaccine needle or reinfection after vaccination, respectively [Table 3].
Table 3.
Reasons behind refusing or being hesitant toward COVID-19 vaccination (n=785)
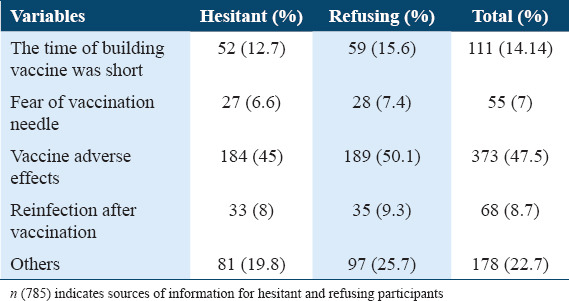
Figure 2 illustrates a strong relationship between types of vaccine and vaccination intention. The majority of participants (40%) would accept the Sinopharm vaccine, followed by Pfizer (36.34%), and AstraZeneca vaccine as the least acceptable (35%). Pfizer (33.02%) and AstraZeneca (32.47%) were also mentioned as the vaccine that people would refuse to get it. Only roughly a quarter of participants (28%) said they would refuse the Sinopharm vaccine. When it comes to vaccine hesitancy, practically all survey people were nearly equally hesitant, ranging from 30% to 32% for available vaccines offered in the Kurdistan region.
Figure 2.
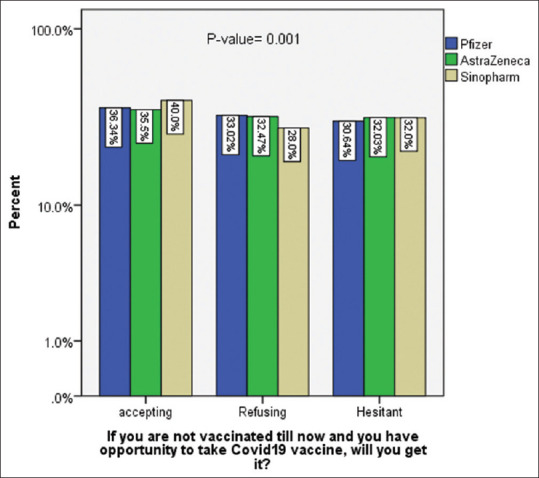
Types of vaccine and COVID-19 vaccination intention
Discussion
Vaccination is widely regarded as one of the most achievements of science; however, vaccine hesitancy continues to persist.[21] As of December 2020, two approved vaccines have been demonstrated to be highly effective and safe for the vast majority of people.[22] The COVID-19 pandemic has reached alarming proportions in Iraq, with thousands of new cases reported daily and hundreds of deaths reported weekly.[23] Iraqi government employed partial curfew in case of increasing COVID-19 cases, improved personal protective measures and announced for vaccines campaign.[24] In this situation, vaccines are the most effective way to combat COVID-19. Therefore, this study was conducted to investigate COVID-19 vaccine acceptance, hesitancy, and refusal, and associated factors among the Kurdish population.
Our data demonstrate that of 1171 respondents, (33%) accepted the vaccine while the majority (32.7%) was hesitant and (34.8%) rejected the COVID-19 vaccines. The available research indicated that COVID-19 vaccinations have been accepted at varying rates in other parts of the world. For instance, the acceptance rate was 90% in China,[25] 76.5% in Canada,[26] (58%) to (69%) in the USA, and (55%) in Russia.[25,27,28] Furthermore, recent researches were following our findings, in a study conducted among the Middle Eastern population, a substantial percentage of people were hesitant (26.4%) or refused the COVID-19 vaccine (36.7%), according to our findings.[29] Furthermore, in neighboring countries including, Iraq.[30,31] As a general low COVID-19 coverage was reported in the Middle East countries during this study. This variation between countries could be attributed to several factors, namely COVID-19 prevalence and mortality rates in the local community, the economies of the countries, social and political conditions, education and public awareness, and the people’s trust in their government and national health organizations.[26,32]
In terms of age and education level, there was a significant relationship (P < 0.01) and (P < 0.03) respectively, when compared to other variables such as gender and occupation. This was in line with other studies done in Iraq[33] and in Saudi Arabia,[34] while these findings were quite different from a study done in Canada.[35] In our results of binary regression analysis for accepting and rejecting vaccines, we found that there was no difference (P < 0.19) between genders. Meta-analysis research found that men (58.3%) were more likely to get vaccinated.[36,37]
However, a strong relationship was revealed with middle-aged adults (ages 35–55 years) and health care workers compared to other occupations. Participants with higher educational levels, such as a Master’s, Ph. D holders, showed strong relation (P < 0.001). These results were following other studies in Iraq.[33] In Saudi Arabia[34] and Greek,[38] as evidenced by being a health care worker increases the willingness to get vaccinated.[39] On the other hand, other studies done in different parts of the world declared different findings.[30,40]
Importantly, we found that having chronic diseases and a history of vaccine refusal was not associated with COVID-19 vaccination intention in our study. Besides, losing a family member due to the COVID-19 was strongly associated with the COVID-19 vaccination. In contrast to the present study in a study done in Scotland, there was a higher intention to take the COVID-19 vaccine among those underlying medical conditions.[41] One reason could be due to that the majority of the participants were young and they lack chronic conditions in the present research. A study done in Saudi Arabia revealed that Participants were less likely to have an intention to be vaccinated if they had a history of vaccine refusal.[42] This contradicts the current result. Moreover, many studies during the COVID-19 pandemic observed a connection between COVID-19 and losing family members.[43,44] Concerning the main reasons for refusing or being hesitant about the COVID-19 vaccine were adverse effects of vaccines this is consistent with accumulating evidence that the main reason for not accepting COVID-19 vaccinations were adverse effects of vaccine.[38,44]
The present study found that participants’ desire to receive or reject COVID-19 vaccination was closely similar to available vaccines (AstraZeneca, Pfizer, Sinopharm). One factor could be that the majority of people were hesitant or refused vaccination regardless of the type of vaccine. Another reason could be that social media plays a significant influence on vaccination intention. However, the Oxford-AstraZeneca COVID-19 vaccine, on the other hand, was perceived to be far less safe than the Pfizer-BioNTech vaccine, a distinction that was especially obvious among vaccine-hesitant people.[45] In research conducted in Egypt, the mRNA-based vaccine was found to be the most trusted.[31] The mechanism of action of mRNA vaccines was given more consideration by expert groups, resulting in a higher level of understanding and acceptance.[46]
Strength and limitations
One of the study’s strengths is the large sample size, which decreases the influence of existing bias. Another strong aspect of the present study is that at the time of the study three types of vaccine were available so that their intention for vaccination would be more accurate. This research has various limitations that should be mentioned. Firstly, because our research is cross-sectional, we can only provide you a snapshot of vaccination intentions at a certain point in time. Furthermore, because this is an online questionnaire survey, the samples are prone to recall and selection bias. As a result of the internet-based nature of the survey, the vast majority of respondents were young adults, with the elderly having less opportunity to participate than younger adults. The previous study has proven, however, that web-based research is a cost-effective approach for generating a sample that is representative of the entire population for a fraction of the expense.[47] Moreover, it has been suggested that as the worldwide number of Internet users grows, the sociodemographic features of web-based survey participants will resemble the broader population.[48]
Conclusions
In the present study, more than half of the participants were hesitancy/resistance to take the COVID-19 vaccine. The vaccine’s adverse effects and losing family members are the primary reason for the unwillingness to the vaccine. Following the conclusions of the study, a more comprehensive approach must be exhibited by all stakeholders to enhance trust in COVID-19 vaccines uptake as well as educational programs concerning health problems and how communities should respond to a health crisis.
Authors’ Declaration Statements
Ethics approval and consent to participate
The ethical approval of the present study was obtained from the University of Duhok, College of Nursing. The author asked participants whether they agree to participate in this online survey at the beginning of the questionnaire. All participants’ rights to privacy and secrecy were maintained.
Availability of data and material
The data used in this study are available and will be provided by the corresponding author on a reasonable request.
Competing interests
None.
Funding
None.
Authors Contributions
According to the corresponding author, all authors whose names were mentioned in the study contributed sufficiently to the data collection, design, review, and analysis. The final paper was approved by all authors.
Acknowledgments
We would like to thank everyone who took the time to participate in our online survey; their involvement is greatly appreciated.
ORCID of corresponding author: https://orcid.org/0000-0003-4788-2402.
References
- 1.Merza MA, Aswad SM, Sulaiman HM, Abdulah DM, Rasheed WS, Taib NI. Clinical and epidemiological characteristics and outcomes of coronavirus disease-19 patients in a large longitudinal study. IJHS. 2021;15:29. [PMC free article] [PubMed] [Google Scholar]
- 2.Merza MA, Al Mezoris AA, Mohammed HM, Abdulah DM. COVID-19 outbreak in Iraqi Kurdistan:The first report characterizing epidemiological, clinical, laboratory, and radiological findings of the disease. Diabet Metab Synd Clin Res Rev. 2020;14:547–54. doi: 10.1016/j.dsx.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balkhair AA. COVID-19 pandemic:A new chapter in the history of infectious diseases. Oman Med J. 2020;35:e123. doi: 10.5001/omj.2020.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. COVID-19 Weekly Epidemiological Update. Geneva: World Health Organization; 2020. Availabe from: https://C:/Users/botan%20pc/Downloads/20211207_Weekly_Epi_Update_69-(1).pdf . [Google Scholar]
- 5.Omrani AS, Al-Tawfiq JA, Memish ZA. Middle East respiratory syndrome coronavirus (MERS-CoV):Animal to human interaction. Pathog Global Health. 2015;109:354–62. doi: 10.1080/20477724.2015.1122852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vankadari N, Wilce JA. Emerging COVID-19 coronavirus:Glycan shield and structure prediction of spike glycoprotein and its interaction with human CD26. Emerg Microbes Infect. 2020;9:601–4. doi: 10.1080/22221751.2020.1739565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period:A scoping review. Infect Dis Poverty. 2020;9:1–12. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahmud I, Al-Mohaimeed A. COVID-19:Utilizing local experience to suggest optimal global strategies to prevent and control the pandemic. IJHS. 2020;14:1. [PMC free article] [PubMed] [Google Scholar]
- 9.Alabdulmonem W, Shariq A, Rasheed Z. COVID-19:A global public health disaster. Int J Health Sci (Qassim) 2020;14:7–8. [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Health Topics:Vaccines 2019. [Last accessed on 2019 Nov 09]. Available form: https://www.who.int/topics/vaccines/en .
- 11.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France:A survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6:e210–21. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it?A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hogan AB, Winskill P, Watson OJ, Walker PG, Whittaker C, Baguelin M, et al. Report 33:Modelling the Allocation and Impact of a COVID-19 Vaccine. London: Imperial College London; 2020. [Google Scholar]
- 14.Petravić L, Arh R, Gabrovec T, Jazbec L, Rupčić, Starešinič N, et al. Factors affecting attitudes towards COVID-19 vaccination:An online survey in Slovenia. Vaccines. 2021;9:247. doi: 10.3390/vaccines9030247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shakir L. 2021. Available from: https://www.rudaw.net/english/kurdistan/201020212 .
- 16.Sherwani H, Catherine J. COVID-19:Plans for new vaccination card as Kurdistan Region reaches 4,500 total deaths. 2021. Available from: https://www.kurdistan24.net/en/story/24920-COVID-19 .
- 17.Kurdistan Region Statistics Office. Kurdistan Map. 2015. [Last accessed on 2020 Mar 17]. Available form: http://www.krso.net/Default.aspx?page=category&c=kurdistan .
- 18.Abdulah DM, Qazli SS, Suleman SK. Response of the public to preventive measures of COVID-19 in Iraqi Kurdistan. Disaster medicine and public health preparedness. 2020:1–9. doi: 10.1017/dmp.2020.233. Doi:10.1017/dmp.2020.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sidiq K. Prevalence of COVID-19 and possible antigenic drifts in SARS-CoV-2 spike protein in Kurdistan region-Iraq. Passer J Basic Appl Sci. 2021;3:27. [Google Scholar]
- 20.U.S. Embassy and Consulates in Iraq. COVID-19 Information. 2020. Available form: https://iq.usembassy.gov/“U.S. Embassy &Consulates in Iraq. Covid-19 information. 2020. https://iq.usembassy.gov/covid-19-information .
- 21.Greenwood B. The contribution of vaccination to global health:Past, present and future. Philos Trans R Soc B Biol Sci. 2014;369:20130433. doi: 10.1098/rstb.2013.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384:403–16. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uctu R. Use of generic medicines in the Middle East:Knowledge, perceptions and experiences of the Sulaimani population, KRI, Iraq. Journal of Generic Medicines. 2021;17:206–213. [Google Scholar]
- 24.Government of Iraq. Iraq continues anti-COVID vaccination campaign as latest Pfizer shipment arrives. Available from: https://gds.gov.iq/iraq-continues-anti-covid-vaccination-campaign-as-latest-pfizer-shipment-arrives/
- 25.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–8. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frank K, Arim R. Canadians'Willingness to Get a COVID-19 Vaccine when One Becomes Available:What Role Does Trust Play? 2020. [Accessed 9/1/2021]. Available from: https://www150.statcan.gc.ca/ n1/pub/45-28-0001/2020001/article/00073-eng.htm .
- 27.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine:A survey of US adults. Ann Intern Med. 2020;173:964–73. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health. 2021;9:34. doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abu Farha RK, Alzoubi KH, Khabour OF, Alfaqih MA. Exploring perception and hesitancy toward COVID-19 vaccine:A study from Jordan. Hum Vaccin Immunother. 2021;17:2415–20. doi: 10.1080/21645515.2021.1888633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mohamed-Hussein AA, Makhlouf H, Abd El Aal H, Kholief K, Saad MM, Abdellal DA. A national survey of potential acceptance of COVID-19 vaccines in healthcare workers in Egypt. MedRxiv. 2021. Available from: https://www.medrxiv.org/content/about-medrxiv .
- 32.Guidry JP, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49:137–42. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghazi HF, Taher TM, Alfadhul SA, Al-Mahmood S, Hassan SA, Hamoudi TA, et al. Acceptance of Covid-19 vaccine among general population In Iraq. Iraqi Natl J Med. 2021;3:9. [Google Scholar]
- 34.Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia:A web-based national survey. J Multidiscip Healthc. 2020;13:1657. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dzieciolowska S, Hamel D, Gadio S, Dionne M, Gagnon D, Robitaille L, et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers:A multicenter survey. Am J Infect Control. 2021;49:1152–7. doi: 10.1016/j.ajic.2021.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zintel S, Flock C, Arbogast AL, Forster A, von Wagner C, Sieverding M. Gender Differences in the Intention to Get Vaccinated Against COVID-19-a Systematic Review and Meta-analysis. 2021. Available from: https://www.ssrn.com/abstract=3803323 . [DOI] [PMC free article] [PubMed]
- 37.Callaghan T, Moghtaderi A, Lueck JA, Hotez PJ, Strych U, Dor A, et al. Correlates and disparities of COVID-19 vaccine hesitancy. Soc Sci Med. 2021;272:113638. doi: 10.1016/j.socscimed.2020.113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Papagiannis D, Rachiotis G, Malli F, Papathanasiou IV, Kotsiou O, Fradelos EC, et al. Acceptability of COVID-19 vaccination among Greek health professionals. Vaccines. 2021;9:200. doi: 10.3390/vaccines9030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qattan A, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8:83. doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ditekemena JD, Nkamba DM, Mavoko AM, Hypolite M, Siewe Fodjo JN, Luhata C, et al. COVID-19 vaccine acceptance in the democratic republic of Congo:A cross-sectional survey. Vaccines. 2021;9:153. doi: 10.3390/vaccines9020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams L, Flowers P, McLeod J, Young D, Rollins L. Social patterning and stability of intention to accept a COVID-19 vaccine in Scotland:Will those most at risk accept a vaccine? Vaccines. 2021;9:17. doi: 10.3390/vaccines9010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alfageeh EI, Alshareef N, Angawi K, Alhazmi F, Chirwa GC. Acceptability of a COVID-19 vaccine among the Saudi population. Vaccines. 2021;9:226. doi: 10.3390/vaccines9030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Y, Xie S, Wang P, Wang G, Zhang L, Cao X, et al. Factors influencing mental health of medical workers during the COVID-19 outbreak. Front Public Health. 2020;8:491. doi: 10.3389/fpubh.2020.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers:Rapid review and meta-analysis. BMJ. 2020;369:1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sønderskov KM, Dinesen PT, Østergaard SD. Sustained COVID-19 vaccine willingness after safety concerns over the Oxford-AstraZeneca vaccine. Dan Med J. 2021;68:A03210292. [PubMed] [Google Scholar]
- 46.Rzymski P, Zeyland J, Poniedziałek B, Małecka I, Wysocki J. The perception and attitudes toward COVID-19 vaccines:A cross-sectional study in Poland. Vaccines. 2021;9:382. doi: 10.3390/vaccines9040382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines:A rapid systematic review. Vaccines. 2021;9:16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study are available and will be provided by the corresponding author on a reasonable request.


